Abstract
Background
Laminectomy is commonly used in the treatment of lumbar spine pathology. Laminectomies are increasingly being performed in outpatient settings, but patient safety concerns remain.
Questions/Purposes
We aimed to describe trends in outpatient lumbar laminectomy between 2008 and 2016 and to identify factors associated with successful same-day discharge.
Methods
We identified patients who underwent single-level lumbar laminectomy between 2008 and 2016 in the American College of Surgeons’ National Surgical Quality Improvement Program database and divided them into two groups according to their admission status, either inpatient or outpatient. Inpatient and outpatient groups were further divided according to actual length of stay (LOS): did not remain in the hospital overnight (LOS = 0) or stayed in the hospital overnight or longer (LOS ≥ 1). We then analyzed patient characteristics and complications for significance and to identify factors associated with successful same-day discharge.
Results
We identified 85,769 patients, 41,149 classified as outpatient status and 44,620 as inpatient status. Between 2008 and 2016, the proportion of procedures performed on an outpatient basis increased from 24.1 to 56.74%. Overall, 27.3% of all patients were discharged on the day of surgery, representing 52.8% of outpatients and 3.8% of inpatients. Older age and longer duration of surgery predicted that patients were less likely to have same-day discharge. Patients with a primary diagnosis other than intervertebral disk disorder, Hispanic ethnic background, or an American Society of Anesthesiologists physical status classification of III were less likely to achieve same-day discharge. Patients under the care of orthopedic surgeons (as opposed to neurosurgeons) were more likely to be discharged on the day of surgery. We also found an association between sex and day of discharge, with female patients being less likely to be discharged on the day of surgery.
Conclusions
Laminectomy is increasingly being performed in the outpatient setting. Younger, healthier non-Hispanic male patients undergoing uncomplicated surgery have a higher likelihood of successful same-day discharge.
Keywords: ambulatory, laminectomy, trend of practice, predictor, same-day discharge
Introduction
Lumbar spine surgery improves quality of life in suitable patients [19, 34]. The demand for lumbar spine surgery has grown rapidly over the past 40 years [9, 10], which can be attributed to improvements in surgical and anesthetic techniques and enhanced diagnostic technology [10, 34]. In the era of growing healthcare costs, increased demand for services necessitates strategies to balance clinical needs and cost-effective care of surgical spine patients.
Outpatient surgery, when clinically appropriate, is more cost-effective than inpatient surgery. This may, in part, account for the progressive transition from inpatient to outpatient spine surgery [3, 10, 29]. Research has supported the use of outpatient surgery in microdiscectomy [6], anterior cervical discectomy and fusion (ACDF) [35], lumbar fusion [31], and vertebroplasty [16]. Nonetheless, discussion continues regarding the most appropriate setting—inpatient hospital, outpatient hospital, or true ambulatory care facility—in which to perform such procedures [17].
The safety and feasibility of outpatient lumbar decompression surgery (hemi-laminectomy and laminectomy) are poorly defined. Although the available data suggest successful outcomes overall, most series have been small [2, 24], retrospective [7], or conducted when outpatient laminectomy was very uncommon [15]. Therefore, we determined to study single-level ambulatory lumbar laminectomy in recent years using data from the American College of Surgeons’ National Surgical Quality Improvement Program (NSQIP) to understand recent trends in practice. In addition, we investigated factors associated with successful same-day discharge after surgery. We hypothesized that selective ambulatory (same-day) laminectomy would not compromise patient safety, as compared with inpatient surgery. These data should assist healthcare providers and policy makers as they seek to balance clinical practice and cost-effectiveness of care in patients undergoing lumbar decompression surgery; it should also help with patient selection.
Patients and Methods
This study was exempted by the institutional review board at our institution.
Study Sample
We acquired 2008 to 2016 data from the NSQIP. The NSQIP prospectively collects data on more than 140 variables, including demographic information, comorbidities, pre-operative laboratory results, intra-operative variables, 30-day mortality rates, and 30-day post-operative complications.
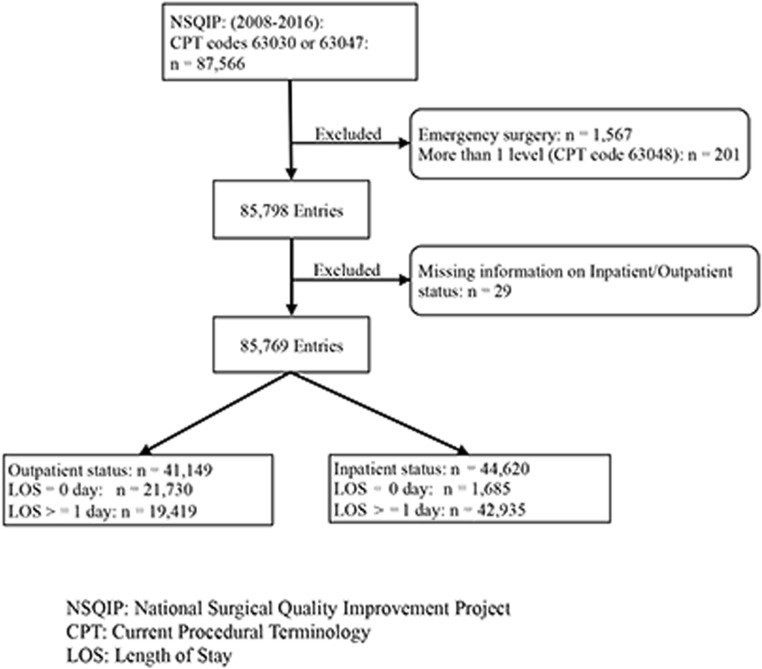
To define our study cohort while minimizing bias related to procedure type, we included patients with only the two most commonly reported Current Procedural Terminology (CPT) codes for hemi-laminectomy and laminectomy (CPT 63030 and 63047). The total number of entries was 87,566. After excluding emergency cases (1567 entries), patients with an additional level (or levels) of spine surgery (CPT 63048; 201 entries), and cases with missing information on length of stay (LOS; 29 entries), the final cohort included 85,769 subjects (Fig. 1).
Fig. 1.
Patient selections.
Study Variables
We first examined trends in specific variables over time: percentages of subjects scheduled for outpatient surgery (outpatients) and those scheduled for inpatient surgery (inpatients); age, sex, and race; comorbidity burden; mortality rates; and incidence of readmission.
We categorized patients according to their scheduled LOS: outpatient or inpatient. The inpatient and outpatient groups were then divided according to actual LOS: same-day discharge (LOS = 0 day) or a stay of 1 day or longer (LOS ≥ 1 day). We used pairwise comparisons and multivariable regression analyses to examine factors relating to successful same-day discharge: patient demographics, comorbidity variables, and practice characteristics. Independent variables included age, body mass index, sex, race or ethnicity, American Society of Anesthesiologists (ASA) physical status classification, diabetes, chronic obstructive pulmonary disease, congestive heart failure, coronary artery disease, end-stage renal disease, central nervous system disease, paraplegia or quadriplegia, functional status, steroid use, and year in which surgery was performed. In addition, we also included surgeon specialty, primary diagnosis, and total operative time in the regression model.
Statistical Analysis
All data analysis was executed using STATA 14.2 statistical software (StataCorp LP, College Station, TX, USA). We analyzed continuous variables using the Student t test, and categorical variables using the χ2 test. For the regression analysis, we conducted both univariable regression and multivariable logistic regression analyses. The results were comparable in regard to significance of variables; for the sake of simplification, we therefore elected to report the results of the multivariable regression analysis, which we conducted using LOS = 0 day patients as the reference. Adjusted odds ratios, 99% confidence intervals, and statistical significance (a p value of 0.05 or lower) are reported.
Results
The final study cohort included 85,769 entries, including 41,149 outpatients and 44,620 inpatients. The numbers of subjects discharged on same day as surgery were 21,730 (52.8%) and 1685 (3.8%), respectively, within the two groups.
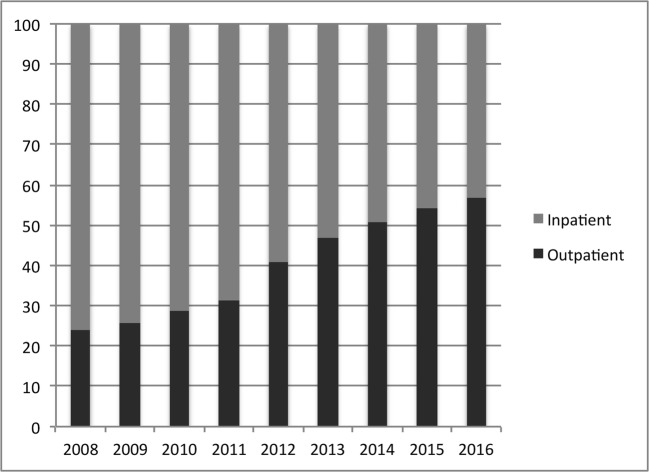
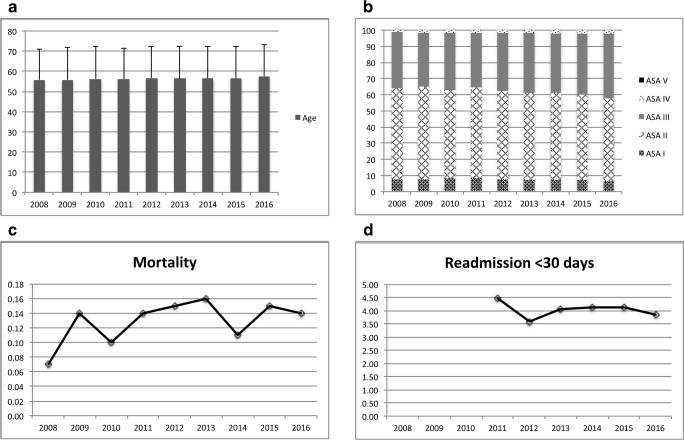
The percentage of procedures scheduled as outpatient surgery rose steadily during the study period, from 24.1% in 2008 to 56.74% in 2016 (Fig. 2). In contrast, age, ASA status, mortality, and readmission within 30 days were largely unchanged during the study period (Fig. 3).
Fig. 2.
Laminectomy scheduling over time. Comparison of inpatient with outpatient surgery in the National Surgical Quality Improvement Program (NSQIP) database, 2008–2016.
Fig. 3.
Changes over time, 2008–2016. a Average age; b distribution of American Society of Anesthesiologists (ASA) classification; c mortality; d readmission within 30 days of surgery (the National Surgical Quality Improvement Program did not collect this information before 2011). ASA classifications: I = normal health; II = mild systemic disease; III = severe systemic disease; IV = severe systemic disease that is a constant threat to life; V = a moribund state with severe systemic disease that is a constant threat to life.
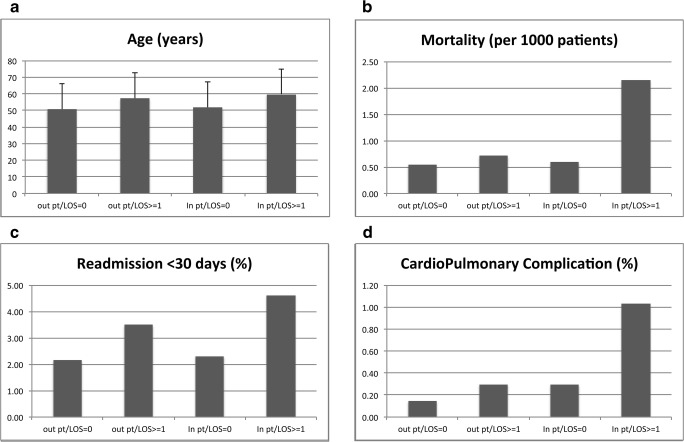
Subgroup analyses showed that outpatients were younger and healthier than inpatients, and LOS = 0 day patients were much younger than the LOS ≥ 1 day patients (Table 1, Fig. 4a; p < 0.001 for both). There was no increase in mortality with outpatient surgery or among LOS = 0 day patients (Fig. 4b). Similar findings were seen in rates of readmission within 30 days of surgery (Fig. 4c) and in cardiopulmonary complications across subgroup comparisons (Fig. 4d).
Table 1.
Demographic information and baseline characteristics
| Outpatients (n = 41,149) | Inpatients (n = 44,620) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| LOS = 0 (n = 21,730; 52.8%) | LOS ≥ 1 (n = 19,419; 48.2%) | p value | LOS = 0 (n = 1685; 3.8%) | LOS ≥ 1 (n = 42,935; 96.2%) | p value | |||||
| Mean or number | SD or % | Mean or number | SD or % | Mean or number | SD or % | Mean or number | SD or % | |||
| Mean age in years | 50.7 | ±15.2 | 57.1 | ±15.6 | < 0.001 | 51.7 | ±15.6 | 59.8 | ±15.2 | < 0.001 |
| Sex | < 0.001 | < 0.001 | ||||||||
| Female | 8685 | 40.0 | 8637 | 44.5 | 651 | 38.6 | 19,872 | 46.3 | ||
| Male | 13,041 | 60.0 | 10,780 | 55.5 | 1034 | 61.4 | 23,046 | 53.7 | ||
| Race or ethnicity | < 0.001 | < 0.001 | ||||||||
| White | 17,118 | 85.8 | 16,135 | 86.0 | 1272 | 86.4 | 32,217 | 82.1 | ||
| African American | 1094 | 5.5 | 1210 | 6.5 | 80 | 5.4 | 3218 | 8.2 | ||
| Hispanic | 1072 | 5.4 | 1038 | 5.5 | 59 | 4.0 | 2440 | 6.2 | ||
| Others | 678 | 3.4 | 380 | 2.0 | 62 | 4.2 | 1369 | 3.5 | ||
| ASA classification | < 0.001 | < 0.001 | ||||||||
| I | 2787 | 12.8 | 1133 | 5.8 | 191 | 11.4 | 2068 | 4.8 | ||
| II | 13,350 | 61.5 | 10,475 | 54.0 | 1020 | 60.6 | 21,094 | 49.2 | ||
| III | 5403 | 24.9 | 7478 | 38.5 | 458 | 27.2 | 18,671 | 43.5 | ||
| IV | 161 | 0.7 | 323 | 1.7 | 14 | 0.8 | 1049 | 2.5 | ||
| V | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | ||
| Total operation time in minutes | 74.3 | ±35.8 | 88.9 | ±46.8 | < 0.001 | 90.1 | ±45.9 | 139.7 | ±82.8 | < 0.001 |
LOS length of stay, SD standard deviation, ASA American Society of Anesthesiologists
Fig. 4.
The figure plots the summary information of four study groups: outpatient with LOS = 0 day (out pt./LOS = 0), outpatient with LOS ≥ 1 day (out pt./LOS ≥ 1), inpatient with LOS = 0 day (in pt./LOS = 0), and inpatient with LOS ≥ 1 day (in pt./LOS ≥ 1). a age; b mortality; c readmission within 30 days of surgery (NSQIP did not collect this data before 2011); d cardiopulmonary complications.
Multivariable regression analyses (Table 2) show that patients who were older and had a longer duration of surgery were less likely to be discharged on the day of surgery. Patients with a primary diagnosis (such as spinal stenosis) other than intervertebral disk disorder, patients with Hispanic ethic background, and patients with ASA III status (severe systemic disease that is not life threatening) were less likely to be discharged on the day of surgery. Patients under the care of orthopedic surgeons (as compared with neurosurgeons) and male patients were more likely to be discharged on the day of surgery.
Table 2.
Odds of unsuccessful same-day discharge, on multivariable regression analysis
| Outpatients | Inpatients | |||||
|---|---|---|---|---|---|---|
| Odds ratio | 99% CI | p value | Odds ratio | 99% CI | p value | |
| Surgeon specialty | ||||||
| Neurosurgery | 1 | |||||
| Orthopedics | 0.5 | 0.40 – 0.64 | < 0.001 | |||
| Primary diagnosis | ||||||
| Intervertebral disc disorder | 1 | 1 | ||||
| Spinal stenosis | 1.46 | 1.13 – 1.89 | < 0.001 | 1.15 | 0.78 – 1.71 | 0.355 |
| Other spine condition | 1.47 | 0.94 – 2.29 | 0.027 | 1.74 | 0.86 – 3.54 | 0.044 |
| Age | ||||||
| ≥ 18 to < 40 years | 1 | 1 | ||||
| ≥ 40 to < 50 years | 1.1 | 0.82 – 1.48 | 0.409 | 0.96 | 0.57 – 1.61 | 0.830 |
| ≥ 50 to < 60 years | 1.11 | 0.82 – 1.51 | 0.367 | 0.88 | 0.52 – 1.48 | 0.525 |
| ≥ 60 to < 70 years | 1.42 | 1.01 – 2.00 | 0.009 | 1.00 | 0.57 – 1.75 | 0.993 |
| ≥ 70 to < 80 years | 1.48 | 0.97 – 2.26 | 0.017 | 2.01 | 1.01 – 3.98 | 0.009 |
| ≥ 80 to < 90 years | 1.81 | 0.96 – 3.42 | 0.016 | 3.99 | 1.22 – 13.0 | 0.003 |
| ≥ 90 years | . | 1.25 | 0.08 – 20.2 | 0.837 | ||
| BMI | ||||||
| ≥ 18.5 to < 30 | 1 | 1 | ||||
| ≥ 30 to < 40 | 1.14 | 0.92 – 1.42 | 0.119 | 1.61 | 1.10 – 2.34 | 0.001 |
| ≥ 40 | 1 | 0.66 – 1.52 | 0.982 | 1.64 | 0.74 – 3.62 | 0.110 |
| < 18.5 | 0.81 | 0.29 – 2.26 | 0.598 | 1.25 | 0.26 – 6.02 | 0.711 |
| Total duration of surgery | ||||||
| < 60 mins | 1 | 1 | ||||
| ≥ 60 to < 90 mins | 1.34 | 1.05 1.71 | 0.002 | 1.77 | 1.17 – 2.69 | < 0.001 |
| ≥ 90 to < 120 mins | 1.73 | 1.30 – 2.30 | < 0.001 | 2.42 | 1.51 – 3.88 | < 0.001 |
| ≥ 120 to < 150 mins | 2.50 | 1.69 – 3.70 | < 0.001 | 3.06 | 1.74 – 5.39 | < 0.001 |
| ≥ 150 to < 180 mins | 3.21 | 1.75 – 5.87 | < 0.001 | 5.55 | 2.37 – 13.0 | < 0.001 |
| ≥ 180 to < 210 mins | 8.01 | 2.63 – 24.4 | < 0.001 | 15.81 | 3.42 – 73.0 | < 0.001 |
| ≥ 210 to < 240 mins | 6.62 | 1.43 – 30.6 | 0.001 | 27.81 | 2.05 – 376.5 | 0.001 |
| ≥ 240 to < 270 mins | 1.00 | 11.68 | 1.81 75.4 | 0.001 | ||
| ≥ 270 to < 300 mins | 11.21 | 0.63 – 199.6 | 0.031 | . | ||
| ≥ 300 mins | 7.35 | 0.41 – 130.2 | 0.074 | . | ||
| Sex | ||||||
| Female | 1 | 1 | ||||
| Male | 0.77 | 0.63 – 0.95 | 0.001 | 0.64 | 0.46 – 0.90 | 0.001 |
| Race or ethnicity | ||||||
| White | 1 | 1 | ||||
| African American | 1.35 | 0.86 – 2.11 | 0.083 | 1.52 | 0.69 – 3.34 | 0.175 |
| Hispanic | 2.07 | 1.30 – 3.30 | <0.001 | 1.84 | 0.75 – 4.55 | 0.081 |
| Other | 1.81 | 0.82 – 3.98 | 0.053 | 1.18 | 0.39 – 3.60 | 0.701 |
| ASA classification | ||||||
| I | 1 | 1 | ||||
| II | 0.98 | 0.71 – 1.36 | 0.898 | 1.07 | 0.61 – 1.87 | 0.754 |
| III | 1.52 | 1.02 – 2.28 | 0.008 | 0.99 | 0.51 – 1.94 | 0.984 |
| IV | 2.62 | 0.54 – 12.83 | 0.118 | 1.03 | 0.19 – 5.64 | 0.959 |
| Other factors | ||||||
| Diabetes | 0.95 | 0.75 – 1.20 | 0.542 | 1.33 | 0.84 – 2.10 | 0.111 |
| History of severe COPD | 1.05 | 0.58 – 1.92 | 0.826 | 0.55 | 0.25 – 1.24 | 0.058 |
| Congestive heart failure | 1.00 | |||||
| Coronary artery disease | 1.05 | 0.67 – 1.66 | 0.764 | 1.46 | 0.70 – 3.04 | 0.184 |
| Renal disease | 0.85 | 0.05 – 14.5 | 0.884 | |||
| Central nervous system disease | 1.24 | 0.69 – 2.22 | 0.346 | |||
| Paraplegia or quadriplegia | 4.71 | 0.74 – 30.0 | 0.031 | |||
| Functional health status before surgery | 1.65 | 0.82 – 3.34 | 0.161 | 0.97 | 0.42 – 2.25 | 0.937 |
| Steroid use for chronic condition | 1.22 | 0.75 – 1.98 | 0.423 | 1.24 | 0.44 – 3.47 | 0.588 |
| Year of operation | 0.95 | 0.90 – 1.00 | 0.070 | |||
BMI body mass index (weight in kilograms divided by the square of the height in meters), ASA American Society of Anesthesiologists, COPD chronic obstructive pulmonary disease
Discussion
With the growing emphasis on value-based care in the USA, there is increasing focus on balancing high-quality care with appropriate healthcare resource use. Several studies support the safety and feasibility of outpatient spine surgery without compromising clinical outcomes [2, 7, 15, 24]. However, larger-scale safety studies of more-invasive procedures (including lumbar decompression surgery) are lacking. Consequently, there is minimal evidence to guide safe practices regarding outpatient lumbar laminectomy. Our study of NSQIP data from 2008 to 2016 with 85,769 patients indicates that in practice laminectomy is shifting toward the use of outpatient surgery (56.74% outpatient surgery 2016, with 27.3% of patients discharged to home on the day of surgery). Overall, the evidence suggests that suitable patients can be discharged on the day of surgery without compromising safety. Younger, healthier male patients undergoing uncomplicated surgery are more likely to have a successful same-day discharge. Primary diagnosis, surgeon specialty, and race also affect same-day discharge.
Our study has several limitations. First, our study is limited by its design, being a retrospective analysis of prospectively collected data. Second, analysis is limited to those data elements that were available in the NSQIP database. For example, the NSQIP did not collect 30-day readmission data until 2011, so no comparisons were feasible before then. Likewise, other important variables, such as opioid consumption, antidepressant use, employment and education status, surgical approach, and details of intra-operative care were not available in the NSQIP. Third, even though some variables, such as the year of surgery, trended toward being significant predictors of same-day discharge, those trends were likely related to changes in practice patterns. Within the field, we have become more comfortable with discharging older and sicker patients on the day of surgery. However, such correlations need further study.
It is not surprising that age was associated with extended LOS. Age has been described as a predictor of extended LOS in several spine surgery cohorts. In an early (2002) report of 112 patients undergoing revision posterior lumbar fusion, advanced age was the only significant predictor of a greater LOS [36] among the factors we studied. These findings were confirmed in a more recent analysis of NSQIP-derived data that identified age as an independent predictor of extended LOS after primary elective posterior lumbar fusion [4]. Two other series concluded that age over 80 was associated with greater LOS after lumber decompression [23] or discectomy [25]. Our study found age over 60 years to be significantly associated with extended LOS. Advanced age likely carries additional and cumulative risk factors for prolonged hospital stay, as represented by the step-wise increase in odds ratios with advancing age (Table 2).
Our study did not indicate any single comorbidity as a significant factor affecting the likelihood of same-day discharge in the outpatient group. However, we did find that assignment of ASA classification III was associated with successful same-day discharge. To our knowledge, this is the first report linking ASA classification with same-day discharge after lumbar decompression surgery. There are several studies linking an ASA classification of III to other generalized complications, such as prolonged admission and higher incidence of unplanned 90-day readmission [33], greater use of hospital resources after spine surgery of varying complexity [13], and (in an analysis of NSQIP data on 15,668 patients) unplanned 30-day readmission after all types of lumbar surgery [27]. In those undergoing adult spinal deformity correction, higher ASA classification was shown to be an independent risk factor for death, reoperation within 30 days, and LOS greater than 5 days [32]. ASA classification accounts for combinations of comorbidities and their cumulative influence on health status in ways that assessing individual diagnoses does not. Therefore, it is not surprising that our study showed a similar result.
We found that prolonged duration of surgery (90 min or longer) was less likely to be associated with same-day discharge. Longer operative duration has been reported as a risk factor for complications up to 30 days after lumbar decompression [18] and for extended LOS after posterior lumbar fusion [4]. This may be explained by longer operative times’ generally being associated with higher surgical and anesthetic complexity and more intra-operative complications [26]. Longer intra-operative time is linked to greater volumes of intravenous fluid administration and blood transfusion, which in turn, are independent risk factors for extended LOS after spine surgery [12, 30].
The effect of race and ethnicity on patterns of clinical practice and outcomes has been an interesting topic across various medical specialties. However, there has been very limited information on Hispanic patient populations and none reporting LOS outcomes. Our study showed that patients with Hispanic background were less likely to be discharged on the day of surgery. This could be related to patterns of clinical practice or the cultures of Hispanic patients. Future studies are indicated.
Unexpectedly, we found that same-day discharge was associated with care provided by orthopedic surgeons, as compared with neurosurgeons. Several retrospective studies describe relationships between subspecialty and outcomes after spine surgery. We identified one trial comparing LOS after lumbar procedures of varying complexity performed by orthopedic surgeons or neurosurgeons. In contrast to our results, patients cared for by an orthopedic surgeon had slightly greater odds of prolonged LOS [28]. Two additional population-based studies suggest that spine surgeons achieve equivalent outcomes irrespective of specialty [18, 21]. Two studies have suggested that undergoing spine surgery performed by an orthopedic surgeon was associated with as much as twice the risk of needing perioperative blood transfusion, as compared with those treated by neurosurgeons, even after adjustment for patient differences [21, 29]. These differences may be accounted for by heterogeneity in the patient populations investigated. For example, whereas our study was restricted to lumbar decompression only, the investigation by Seicean et al. included all lumbar procedures, including complex cases [28]. Alternatively, there may have been differences in patient acuity represented between the specialties in our study, whereby healthier patients may have been cared for by orthopedic surgeons. This is consistent with a large retrospective analysis of patients undergoing ACDF, in which patients under the care of neurosurgeons had more comorbidities compared with patients under the care of orthopedic surgeons [22].
Finally, we found an association between male sex and greater likelihood of same-day discharge after lumbar decompression surgery. There is mixed evidence regarding the influence of sex on outcomes after spine surgery. Basques et al. described a greater risk of adverse events among male patients after ACDF [5]. The authors attributed these results to a stronger baseline association between medical comorbid burden and male sex than between that and female sex. In contrast, other data have failed to show any effect of sex on complications or morbidity after adult spinal deformity surgery [8], or reported that female sex strongly predicted a discharge destination other than home [1]. There are several explanations for these discrepant results. There may be sex-based differences in quality of life and pain perception, which in turn could affect readiness for discharge after a procedure scheduled as outpatient. Recent research has shown that women have more baseline dysfunction, more pain, and lower quality-of-life scores before elective lumbar surgery, which translated into lower satisfaction and poorer functional recovery at 1 year [12]. Important psychosocial variables may also interact with sex to contribute to LOS and discharge destination. In a recent prospective analysis of resource use after lumbar surgery, female sex, depression, anxiety, and poor social support were all associated with extended LOS [20]. Finally, post-operative nausea and vomiting (PONV) is a major factor limiting same-day discharge after all types of surgery [14]. PONV affects women more often than men and was not controlled for in our study. Thus, PONV may represent an underlying explanation for the sex-based differences found here [14].
In conclusion, our findings provide data supporting the practice of outpatient spine surgery in select patients, specifically those who are younger than 60 years and with better baseline health status (ASA I [normal health] or II [mild systemic disease]). A shorter operating time (under 90 min) and non-Hispanic ethic background were also associated with successful outpatient laminectomy and should be considered clinical decisions. Because the study uncovered associations between sex and race or ethnicity and outcomes after ambulatory lumbar laminectomy, further study is needed to clarify the underlying biological, clinical, and social factors contributing to these factors and whether they are amenable to intervention. Overall, the results suggest that a tailored, patient-specific approach may be necessary in pre-operative planning and communication of risks to patients.
Compliance with Ethical Standards
Conflict of Interest
Ellen M. Soffin, MD, PhD, James D. Beckman, MD, Jonathan C. Beathe, MD, Gregory A. Liguori, MD, and Jiabin Liu, MD, PhD, declare that they have no conflicts of interest. Federico P. Girardi, MD, reports royalties from Lanx, Inc., Depuy Synthes Spine, Nuvasive, Inc., and Ortho Development Corp.; fees as a consultant from Ortho Development Corp., Spineart USA, Nuvasive, Inc., Depuy Synthes Spine, Lanx, Inc., and EIT Emerging Implant Technologies; ownership interest in Healthpoint Capital Partners, Paradigm Spine, LLC, Centinel Spine, Inc., Spinal Kinetics, Inc., and Liventa Bioscience; and other personal fees from Aesculap, MiMedx Group, Inc., and Nuvasive, Inc., outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Level III: Retrospective cohort study
References
- 1.Aldebeyan S, Aoude A, Fortin M, et al. Predictors of discharge destination after lumbar spine fusion surgery. Spine (Phila Pa 1976) 2016;41(19):1535–1541. doi: 10.1097/BRS.0000000000001575. [DOI] [PubMed] [Google Scholar]
- 2.An HS, Simpson JM, Stein R. Outpatient laminotomy and discectomy. J Spinal Disord. 1999;12(3):192–196. [PubMed] [Google Scholar]
- 3.Baird EO, Brietzke SC, Weinberg AD, et al. Ambulatory spine surgery: a survey study. Global Spine J. 2014;4(3):157–160. doi: 10.1055/s-0034-1378142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basques BA, Fu MC, Buerba RA, Bohl DD, Golinvaux NS, Grauer JN. Using the ACS-NSQIP to identify factors affecting hospital length of stay after elective posterior lumbar fusion. Spine (Phila Pa 1976)\ 2014;39(6):497–502. doi: 10.1097/BRS.0000000000000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Basques BA, Hijji FY, Khechen B, et al. Sex differences for anterior cervical fusion: complications and length of stay. Spine (Phila Pa 1976) 2017;43(15):1025–1030. doi: 10.1097/BRS.0000000000002512. [DOI] [PubMed] [Google Scholar]
- 6.Best NM, Sasso RC. Success and safety in outpatient microlumbar discectomy. J Spinal Disord Tech. 2006;19(5):334–337. doi: 10.1097/01.bsd.0000210119.47387.44. [DOI] [PubMed] [Google Scholar]
- 7.Best NM, Sasso RC. Outpatient lumbar spine decompression in 233 patients 65 years of age or older. Spine (Phila Pa 1976) 2007;32(10):1135–1139. doi: 10.1097/01.brs.0000261486.51019.4a. [DOI] [PubMed] [Google Scholar]
- 8.Bumpass DB, Lenke LG, Gum JL, et al. Male sex may not be associated with worse outcomes in primary all-posterior adult spinal deformity surgery: a multicenter analysis. Neurosurg Focus. 2017;43(6):E9. doi: 10.3171/2017.9.FOCUS17475. [DOI] [PubMed] [Google Scholar]
- 9.Deyo RA, Mirza SK. Trends and variations in the use of spine surgery. Clin Orthop Relat Res. 2006;443:139–146. doi: 10.1097/01.blo.0000198726.62514.75. [DOI] [PubMed] [Google Scholar]
- 10.Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 2005;30(12):1441–1445. doi: 10.1097/01.brs.0000166503.37969.8a. [DOI] [PubMed] [Google Scholar]
- 11.Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303(13):1259–1265. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elsamadicy AA, Reddy GB, Nayar G, et al. Impact of gender disparities on short-term and long-term patient reported outcomes and satisfaction measures after elective lumbar spine surgery: a single institutional study of 384 patients. World Neurosurg. 2017;107:952–958. doi: 10.1016/j.wneu.2017.07.082. [DOI] [PubMed] [Google Scholar]
- 13.Farshad M, Bauer DE, Wechsler C, Gerber C, Aichmair A. Risk factors for perioperative morbidity in spine surgeries of different complexities: a multivariate analysis of 1009 consecutive patients. Spine J. 2018;18(9):1625–1631. doi: 10.1016/j.spinee.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Gan TJ, Diemunsch P, Habib AS, et al. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2014;118(1):85–113. doi: 10.1213/ANE.0000000000000002. [DOI] [PubMed] [Google Scholar]
- 15.Gray DT, Deyo RA, Kreuter W, et al. Population-based trends in volumes and rates of ambulatory lumbar spine surgery. Spine (Phila Pa 1976) 2006;31(17):1957–1963. doi: 10.1097/01.brs.0000229148.63418.c1. [DOI] [PubMed] [Google Scholar]
- 16.Gray DT, Hollingworth W, Onwudiwe N, Jarvik JG. Costs and state-specific rates of thoracic and lumbar vertebroplasty, 2001-2005. Spine (Phila Pa 1976) 2008;33(17):1905–1912. doi: 10.1097/BRS.0b013e31817bb0a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Idowu OA, Boyajian HH, Ramos E, Shi LL, Lee MJ. Trend of spine surgeries in the outpatient hospital setting versus ambulatory surgical center. Spine (Phila Pa 1976) 2017;42(24):E1429–E1436. doi: 10.1097/BRS.0000000000002180. [DOI] [PubMed] [Google Scholar]
- 18.Kim BD, Smith TR, Lim S, Cybulski GR, Kim JY. Predictors of unplanned readmission in patients undergoing lumbar decompression: multi-institutional analysis of 7016 patients. J Neurosurg Spine. 2014;20(6):606–616. doi: 10.3171/2014.3.SPINE13699. [DOI] [PubMed] [Google Scholar]
- 19.Lurie JD, Tosteson TD, Tosteson A, et al. Long-term outcomes of lumbar spinal stenosis: eight-year results of the Spine Patient Outcomes Research Trial (SPORT) Spine (Phila Pa 1976) 2015;40(2):63–76. doi: 10.1097/BRS.0000000000000731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mancuso CA, Duculan R, Craig CM, Girardi FP. Psychosocial variables contribute to length of stay and discharge destination after lumbar surgery independent of demographic and clinical variables. Spine (Phila Pa 1976) 2018;43(4):281–286. doi: 10.1097/BRS.0000000000002312. [DOI] [PubMed] [Google Scholar]
- 21.McCutcheon BA, Ciacci JD, Marcus LP. Thirty-day perioperative outcomes in spinal fusion by specialty within the NSQIP database. Spine (Phila Pa 1976) 2015;40(14):1122–1131. doi: 10.1097/BRS.0000000000000599. [DOI] [PubMed] [Google Scholar]
- 22.Minhas SV, Chow I, Patel AA, Kim JY. Surgeon specialty differences in single-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2014;39(20):1648–1655. doi: 10.1097/BRS.0000000000000499. [DOI] [PubMed] [Google Scholar]
- 23.Murphy ME, Gilder H, Maloney PR, et al. Lumbar decompression in the elderly: increased age as a risk factor for complications and nonhome discharge. J Neurosurg Spine. 2017;26(3):353–362. doi: 10.3171/2016.8.SPINE16616. [DOI] [PubMed] [Google Scholar]
- 24.Newman MH. Outpatient conventional laminotomy and disc excision. Spine (Phila Pa 1976) 1995;20(3):353–355. doi: 10.1097/00007632-199502000-00017. [DOI] [PubMed] [Google Scholar]
- 25.Nie H, Hao J, Peng C, Ou Y, Quan Z, An H. Clinical outcomes of discectomy in octogenarian patients with lumbar disc herniation. J Spinal Disord Tech. 2013;26(2):74–78. doi: 10.1097/BSD.0b013e318236b92d. [DOI] [PubMed] [Google Scholar]
- 26.Phan K, Kim JS, Kim JH, et al. Anesthesia duration as an independent risk factor for early postoperative complications in adults undergoing elective ACDF. Global Spine J. 2017;7(8):727–734. doi: 10.1177/2192568217701105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S. Causes and risk factors for 30-day unplanned readmissions after lumbar spine surgery. Spine (Phila Pa 1976) 2014;39(9):761–768. doi: 10.1097/BRS.0000000000000270. [DOI] [PubMed] [Google Scholar]
- 28.Seicean A, Alan N, Seicean S, Neuhauser D, Benzel EC, Weil RJ. Surgeon specialty and outcomes after elective spine surgery. Spine (Phila Pa 1976) 2014;39(19):1605–1613. doi: 10.1097/BRS.0000000000000489. [DOI] [PubMed] [Google Scholar]
- 29.Shapiro FE, Punwani N, Urman RD. Office-based surgery: embracing patient safety strategies. J Med Pract Manage. 2013;29(2):72–75. [PubMed] [Google Scholar]
- 30.Siemionow K, Pelton MA, Hoskins JA, Singh K. Predictive factors of hospital stay in patients undergoing minimally invasive transforaminal lumbar interbody fusion and instrumentation. Spine (Phila Pa 1976) 2012;37(24):2046–2054. doi: 10.1097/BRS.0b013e31825c6688. [DOI] [PubMed] [Google Scholar]
- 31.Smith WD, Wohns RN, Christian G, Rodgers EJ, Rodgers WB. Outpatient minimally invasive lumbar interbody: fusion predictive factors and clinical results. Spine (Phila Pa 1976) 2016;41(Suppl 8):S106–S122. doi: 10.1097/BRS.0000000000001479. [DOI] [PubMed] [Google Scholar]
- 32.Somani S, Capua JD, Kim JS, et al. ASA classification as a risk stratification tool in adult spinal deformity surgery: a study of 5805 patients. Global Spine J. 2017;7(8):719–726. doi: 10.1177/2192568217700106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wadhwa RK, Ohya J, Vogel TD, et al. Risk factors for 30-day reoperation and 3-month readmission: analysis from the quality and outcomes database lumbar spine registry. J Neurosurg Spine. 2017;27(2):131–136. doi: 10.3171/2016.12.SPINE16714. [DOI] [PubMed] [Google Scholar]
- 34.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT) Spine (Phila Pa 1976) 2008;33(25):2789–2800. doi: 10.1097/BRS.0b013e31818ed8f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wohns R. Safety and cost-effectiveness of outpatient cervical disc arthroplasty. Surg Neurol Int. 2010;1:77. doi: 10.4103/2152-7806.73803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zheng F, Cammisa FP, Jr, Sandhu HS, Girardi FP, Khan SN. Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation. Spine (Phila Pa 1976) 2002;27(8):818–824. doi: 10.1097/00007632-200204150-00008. [DOI] [PubMed] [Google Scholar]