Abstract
Background:
A modified Lemaire lateral extra-articular tenodesis (LET) is a procedure that is designed to address anterolateral complex (ALC) deficiency. The procedure is performed as an augmentation to anterior cruciate ligament reconstruction (ACLR) to reduce anterolateral rotatory laxity. Studies have demonstrated improved rotational control and reduced failure rates of ACLR when LET is added. This is particularly helpful in young patients with high-grade rotatory laxity returning to contact pivoting sport, and in the revision ACLR scenario.
Description:
A 6-cm skin incision is placed just posterior to the lateral epicondyle. The subcutaneous tissue is dissected down to the iliotibial band (ITB). A 1-cm-wide by 8-cm-long strip of the posterior half of the ITB is fashioned, leaving the distal attachment at Gerdy’s tubercle intact. The free end is whipstitched with number-1 Vicryl suture, tunneled deep to the fibular collateral ligament (FCL), and attached to the metaphyseal flare of the lateral femoral condyle at the insertion of the distal Kaplan fibers of the ITB. Fixation is performed with a staple, with the graft tensioned to no more than 20 N (by simply holding it taut and not “tensioned”), with the knee held at 60° of flexion and neutral rotation of the tibia.
Alternatives:
A number of procedures to address ALC deficiency have been described. The most common methods currently are variations of the ITB LET (Lemaire [ITB graft detached proximally, passed under the FCL, and attached to the femur] or Ellison [ITB graft detached distally, passed deep to the FCL, and reattached at Gerdy’s tubercle]) or anterolateral ligament reconstructions. No clinical studies have been performed that demonstrate that one technique is superior to another.
Rationale:
Current ACLR procedures focus on intra-articular graft placement to replace the ACL. Unfortunately, high rates of graft failure and persistent rotatory laxity (pivot shift) have been observed, particularly in young, high-demand individuals returning to contact pivoting sport. ALC deficiency has been shown to be a major cause of high-grade anterolateral rotatory laxity. The LET procedure is therefore designed to augment ACLR and reduce anterolateral rotation. The aim of adding LET to ACLR is to reduce the strain on the ACLR graft, reduce the prevalence of the pivot shift, and thereby potentially reduce the rate of ACLR graft failure.
Introductory Statement
The modified Lemaire lateral extra-articular tenodesis (LET) has been shown to reduce anterolateral rotatory laxity in the anterior cruciate ligament (ACL)-reconstructed knee1 and hence may be important to help reduce failure of ACL reconstruction (ACLR) in young patients returning to contact pivoting sports who are at a high risk of graft failure, or in the revision ACLR scenario2.
Indications & Contraindications
Indications
The following indications were developed from a recent International ALC [Anterolateral Complex] Consensus Group Meeting2 and represent the current thinking as to when LET may be added to ACLR:
Revision ACLR.
High-grade rotational laxity (a grade-2 or 3 pivot shift).
Generalized ligamentous laxity or genu recurvatum of >10°.
A young patient (<25 years old) returning to a contact pivoting sport.
Contraindications
There are no specific contraindications; however, caution should be observed in patients with:
Posterolateral corner injury.
Lateral compartment osteoarthritis.
Step-by-Step Description of Procedure
Step 1: Completion of ACLR
The ACLR is completed prior to performing a modified Lemaire LET.
Pass, tension, and fix the ACL graft in a standard manner. When the ACLR is complete, perform a modified Lemaire LET (Video 1).
Video 1.
Modified Lemaire extra-articular tenodesis surgical technique.
Step 2: Lateral Skin Incision
Perform the lateral skin incision.
Position the leg with the knee at approximately 80° of flexion.
Make a minimum 6-cm longitudinal incision 1 cm posterior to the lateral femoral epicondyle, starting 2 cm proximal to Gerdy’s tubercle (Figs. 1-A and 1-B).
If greater visualization is required, particularly in patients with abundant subcutaneous tissue, extend the incision proximally.
Dissect the subcutaneous fat down to the iliotibial band (ITB) and sweep the fat posteriorly to identify the posterior border of the ITB, enabling palpation of Gerdy’s tubercle distally.
Figs. 1-A and 1-B With the knee positioned at 80° of flexion (Fig. 1-A), a lateral skin incision is placed just posterior to the lateral epicondyle (Fig. 1-B).
Fig. 1-A.

Fig. 1-B.

Step 3: Fashioning of ITB Graft
Fashion the ITB graft.
Harvest an 8-cm-long by 1-cm-wide strip of ITB from the posterior half of the ITB, ensuring that the most posterior fibers of the deep ITB (capsulo-osseous layer) remain intact (Figs. 2-A, 2-B, and 3).
Leave the distal attachment at Gerdy’s tubercle intact.
Release the deep attachments to the vastus lateralis off the proximal 6 cm of the graft and place a whipstitch with number-1 Vicryl suture (Ethicon) in the free end.
Figs. 2-A and 2-B In fashioning the ITB graft, a strip of ITB is harvested from the posterior half of the ITB (Fig. 2-A), making sure that the most posterior fibers of the deep ITB (capsulo-osseous layer) remain intact (Fig. 2-B).
Fig. 2-A.

Fig. 2-B.
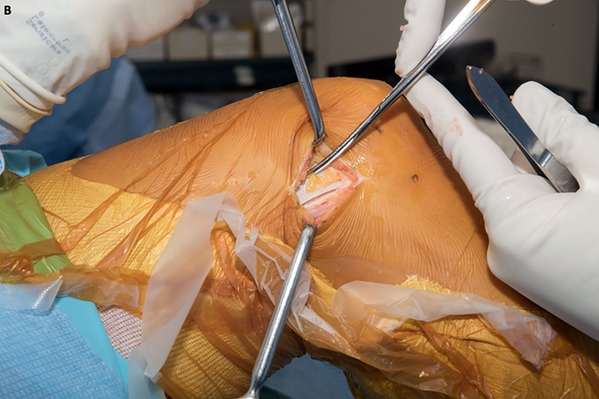
Fig. 3.

The ITB graft measures 8 cm long and 1 cm wide.
Step 4: Passage of the ITB Graft Deep to the Fibular Collateral Ligament (FCL)
Pass the ITB graft beneath the FCL.
Identify the FCL by palpation. Place the leg in a figure-of-4 position to aid in identification.
Make small capsular incisions anterior and posterior to the proximal portion of the FCL and place Metzenbaum scissors deep to the FCL from anterior to posterior to bluntly dissect out a tract for graft passage.
Attempt to remain extracapsular, while ensuring there is no iatrogenic damage to the popliteus or FCL.
Then pass the ITB graft beneath the FCL from distal to proximal using a right-angled clamp (Fig. 4).
Fig. 4.

The ITB graft is tunneled under the femoral attachment of the FCL.
Step 5: Fixation of ITB Graft to Femur
Fix the ITB graft to the femur.
Using electrocautery, clear the lateral femoral supracondylar area of the small fat pad found proximal to the lateral head of the gastrocnemius.
Cauterize the superolateral genicular artery, which may be found here, to avoid unwanted bleeding.
Identify the attachment site just anterior and proximal to the lateral head of the gastrocnemius tendon, on the lateral metaphyseal flare of the lateral femoral condyle.
Clear the periosteum using a Cobb elevator on the metaphyseal flare of the lateral femoral condyle.
Take care not to damage ACL femoral fixation as the suspensory loop button is often found close to this location.
Then hold the graft taut, but not overtensioned (<20 N), with the knee at 60° of flexion and the foot in neutral rotation to avoid lateral compartment overconstraint.
Secure the graft using a small Richards staple (Smith & Nephew) and then fold the graft back distally and suture it onto itself using a whipstitch with number-1 Vicryl suture (Figs. 5 and 6).
Fig. 5.

Fixation of the ITB graft with a staple. The knee is at 60° of flexion and neutral tibial rotation.
Fig. 6.

The ITB graft is folded over the staple and is sutured onto itself.
Step 6: Closure of the ITB
Perform partial closure of the ITB.
Irrigate the wound, confirm hemostasis, and perform closure in layers.
Close the posterior aspect of the ITB with interrupted number-1 Vicryl sutures up to the level of the transverse retinacular ligament.
Do not close the ITB completely to avoid overtightening the lateral patellofemoral joint.
Step 7: Postoperative Rehabilitation
Postoperatively, manage the patient with weight-bearing and range of motion performed as tolerated.
Postoperative rehabilitation is the same as for any ACLR. Manage the patient with weight-bearing and range of motion performed as tolerated so long as there is no substantial meniscal repair.
Results
The modified Lemaire LET has recently been shown to reduce anterolateral rotatory laxity in the ACL-reconstructed knee1. A number of early studies comparing ACLR with or without a lateral tenodesis showed promising results with respect to lower rates of failure with the addition of the LET3,4; however, concerns were raised with regard to restriction of external rotation, pain, and subsequent overconstraint5. This led to the procedure being mostly abandoned in the United States. In Europe, many centers continued to utilize the technique with great success6,7.
This has been illustrated by recent systematic reviews showing improved anterolateral and anteroposterior stability as measured by the pivot-shift test and the Lachman test and/or KT-1000 arthrometer (Medmetric), respectively, when LET was combined with ACLR1,8-10. However, pooled functional scores did not show superiority. Devitt et al. found that LET is not beneficial when used in early primary ACLR (≤1 year), but it does reduce postoperative pivot-shift in delayed ACLR (>1 year)10. They also showed in a 2017 systematic review that LET with ACLR did not result in increased rates of osteoarthritis, as has previously been suggested11. Instead, meniscal involvement at the time of injury was a greater predictor of osteoarthritis. This finding has also been observed by Ferretti et al.12 and Marcacci et al.6 in their long-term follow-up studies. The notion that LET may be graft-protective has previously been demonstrated by Engebretsen et al., who showed that the forces going through the ACL graft may be reduced by 43% in vitro13.
Pitfalls & Challenges
While the FCL is usually readily palpable, in some cases it can be difficult to palpate. The knee can be placed into a figure-of-4 position to stretch the FCL and increase its tautness, thereby making it easier to palpate.
The region of the femoral metaphyseal flare proximal and lateral to the lateral gastrocnemius head should be cleared of fat using electrocautery because branches of the superolateral genicular artery and its venae comitantes are in proximity.
Care must be taken to identify the suspensory loop femoral fixation of the ACL graft (if one is used) as it is typically close to the desired attachment site for the LET graft.
While biomechanical studies have suggested that the flexion angle can be between 30° and 70° of flexion14, our preference is for the LET graft to be held taut during femoral fixation (tensioned <20 N) with the knee placed at 60° of flexion and the foot in neutral rotation to avoid overconstraining the lateral compartment.
Footnotes
Investigation performed at the Department of Surgery, Fowler Kennedy Sport Medicine Clinic, Western University, London, Ontario, Canada
Disclosure: The authors indicated that no external funding was received for any aspect of this work. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJSEST/A274).
Published outcomes of this procedure can be found at: Arthroscopy. 2015 Oct;31(10):2022-34.
References
- 1.Hewison CE, Tran MN, Kaniki N, Remtulla A, Bryant D, Getgood AM. Lateral extra-articular tenodesis reduces rotational laxity when combined with anterior cruciate ligament reconstruction: a systematic review of the literature. Arthroscopy. 2015. October;31(10):2022-34. Epub 2015 Jun 24. [DOI] [PubMed] [Google Scholar]
- 2.Getgood A, Brown C, Lording T, Amis A, Claes S, Geeslin A, Musahl V; ALC Consensus Group. The anterolateral complex of the knee: results from the International ALC Consensus Group Meeting. Knee Surg Sports Traumatol Arthrosc. 2019. January;27(1):166-76. Epub 2018 Jul 25. [DOI] [PubMed] [Google Scholar]
- 3.Noyes FR, Barber SD. The effect of an extra-articular procedure on allograft reconstructions for chronic ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 1991. July;73(6):882-92. [PubMed] [Google Scholar]
- 4.Anderson AF, Snyder RB, Lipscomb AB., Jr Anterior cruciate ligament reconstruction. A prospective randomized study of three surgical methods. Am J Sports Med. 2001. May-Jun;29(3):272-9. [DOI] [PubMed] [Google Scholar]
- 5.O’Brien SJ, Warren RF, Wickiewicz TL, Rawlins BA, Allen AA, Panariello R, Kelly AM. The iliotibial band lateral sling procedure and its effect on the results of anterior cruciate ligament reconstruction. Am J Sports Med. 1991. Jan-Feb;19(1):21-4; discussion 24-5. [DOI] [PubMed] [Google Scholar]
- 6.Marcacci M, Zaffagnini S, Giordano G, Iacono F, Presti ML. Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: a prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am J Sports Med. 2009. April;37(4):707-14. Epub 2009 Feb 3. [DOI] [PubMed] [Google Scholar]
- 7.Pernin J, Verdonk P, Si Selmi TA, Massin P, Neyret P. Long-term follow-up of 24.5 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am J Sports Med. 2010. June;38(6):1094-102. Epub 2010 Mar 19. [DOI] [PubMed] [Google Scholar]
- 8.Rezende FC, de Moraes VY, Martimbianco AL, Luzo MV, da Silveira Franciozi CE, Belloti JC. Does combined intra- and extraarticular ACL reconstruction improve function and stability? A meta-analysis. Clin Orthop Relat Res. 2015. August;473(8):2609-18. Epub 2015 Apr 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song GY, Hong L, Zhang H, Zhang J, Li Y, Feng H. Clinical outcomes of combined lateral extra-articular tenodesis and intra-articular anterior cruciate ligament reconstruction in addressing high-grade pivot-shift phenomenon. Arthroscopy. 2016. May;32(5):898-905. Epub 2015 Oct 30. [DOI] [PubMed] [Google Scholar]
- 10.Devitt BM, Bell SW, Ardern CL, Hartwig T, Porter TJ, Feller JA, Webster KE. The role of lateral extra-articular tenodesis in primary anterior cruciate ligament reconstruction: a systematic review with meta-analysis and best-evidence synthesis. Orthop J Sports Med. 2017. October 24;5(10):2325967117731767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devitt BM, Bouguennec N, Barfod KW, Porter T, Webster KE, Feller JA. Combined anterior cruciate ligament reconstruction and lateral extra-articular tenodesis does not result in an increased rate of osteoarthritis: a systematic review and best evidence synthesis. Knee Surg Sports Traumatol Arthrosc. 2017. April;25(4):1149-60. Epub 2017 Mar 13. [DOI] [PubMed] [Google Scholar]
- 12.Ferretti A, Monaco E, Ponzo A, Basiglini L, Iorio R, Caperna L, Conteduca F. Combined intra-articular and extra-articular reconstruction in anterior cruciate ligament-deficient knee: 25 years later. Arthroscopy. 2016. October;32(10):2039-47. Epub 2016 May 4. [DOI] [PubMed] [Google Scholar]
- 13.Engebretsen L, Lew WD, Lewis JL, Hunter RE. The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med. 1990. Mar-Apr;18(2):169-76. [DOI] [PubMed] [Google Scholar]
- 14.Geeslin AG, Moatshe G, Chahla J, Kruckeberg BM, Muckenhirn KJ, Dornan GJ, Coggins A, Brady AW, Getgood AM, Godin JA, LaPrade RF. Anterolateral knee extra-articular stabilizers: a robotic study comparing anterolateral ligament reconstruction and modified Lemaire lateral extra-articular tenodesis. Am J Sports Med. 2018. March;46(3):607-16. Epub 2017 Dec 21. [DOI] [PubMed] [Google Scholar]


