Abstract
Background:
Proximal humeral fractures are relatively common in pediatric patients. These injuries are usually treated nonoperatively in younger children or children with minimally displaced fractures. However, closed reduction or open reduction followed by percutaneous pinning is recommended for older children with displaced fractures. Percutaneous pinning has several advantages, but there are limited reports of a safe and reliable surgical technique in the literature.
Description:
Patients are positioned in a modified beach-chair position to allow orthogonal imaging. The injured extremity is draped free from the remainder of the body. Closed reduction, which comprises a combination of traction, abduction, and rotation, is attempted. Internal or external rotation may be required, depending on the fracture line and deforming forces. If an anatomic closed reduction cannot be obtained, a block to reduction should be suspected and open reduction should be performed via a deltopectoral approach. Once the fracture is reduced, two 2.5-mm threaded Kirschner wires from the small external fixator set are used to percutaneously fix the fracture. Any small external fixator set can be used, and if not available, individual threaded wires of similar size can be used. Alternatively, Kirschner wires can be advanced to the fracture site prior to reduction and then advanced into the humeral epiphysis once the fracture is reduced. Care is taken to avoid the axillary nerve, which is reliably within 6 cm of the anterolateral aspect of the acromion, and wires are placed distal to this site. Once pin position has been confirmed radiographically, the construct is secured with pin-to-pin clamps to improve rigidity and further decrease the risk of pin migration. A soft dressing and shoulder immobilizer are placed postoperatively. Patients are followed with biweekly radiographs, and pins are removed in the outpatient office or under conscious sedation at 4 weeks. Leaving pins for a longer period may increase the risk of skin irritation and potentially infection.
Alternatives:
Alternatives to closed reduction or open reduction and percutaneous pinning include nonoperative management and elastic intramedullary nailing. Nonoperative treatment is a reliable option for most patients. However, it is not suitable for older children with severely displaced fractures because of diminished remodeling potential. Elastic intramedullary nailing is a good option for distal fractures. However, it is not suitable for proximal fractures, and it has been associated with longer operative times and more blood loss than percutaneous pinning. It also requires a second procedure.
Rationale:
This procedure allows for anatomic fixation of proximal humeral fractures and provides a rigid construct to maintain reduction. It is not technically challenging, requires limited postoperative immobilization, and decreases the risk of a second general anesthetic.
Introductory Statement
Percutaneous pinning is an effective, safe, and reliable technique to fix displaced pediatric proximal humeral fractures.
Indications & Contraindications
Indications
-
Absolute
-
○
Open fractures.
-
○
Fractures associated with neurovascular compromise.
-
○
Skin tenting or risk of impending open fracture.
-
○
-
Relative
-
○
Severe displacement (Neer-Horwitz grade III or IV1; Table I) or angulation, particularly in children >11 years old.
-
○
Inadequate reduction in patients approaching skeletal maturity (Table II).
-
○
Displaced or unstable fractures in patients who cannot tolerate immobilization (polytrauma, neuromuscular disorders, etc.).
-
○
Adolescent athletes involved in overhead-throwing activities.
-
○
Polytrauma.
-
○
TABLE I.
Neer-Horwitz Classification for Pediatric Proximal Humeral Fractures1
| Grade | Classification Description |
| I | Displaced <5 mm |
| II | Displaced ≤1/3 humeral shaft width |
| III | Displaced >1/3 but ≤2/3 humeral shaft width |
| IV | Displaced >2/3 humeral shaft width, including total separation |
TABLE II.
Indications for Surgical Intervention
| Study | Age Range (yr) | Indications for Surgical Intervention |
| Bahrs et al.6 | ≥10 | Full displacement, >30° angulation, and 10° valgus deformity |
| <10 | Full displacement and >60° angulation | |
| Binder et al.7 | All ages | >30° angulation |
| Burgos-Flores et al.2 | >13 | >30% angulation and >50% displacement |
| Dobbs et al.8 | ≥12 | >45° angulation |
| 8-11 | >60° angulation | |
| ≤7 | >75° angulation | |
| Hohloch et al.9 | ≥13 | Displacement of >1/3 shaft width and >20° angulation |
| 10-12 | Same indications as for those who are ≥13 years, comparable with nonoperative management (may attempt closed reduction) | |
| Hutchinson et al.5 | ≥12 | Neer-Horwitz grade-IV fractures and >40° angulation |
Contraindications
Birth fractures of the proximal part of the humerus.
Closed fractures with acceptable alignment.
Step-by-Step Description of Procedure
Step 1: Fracture Reduction (Figs. 1 and 2, Video 1)
Fig. 1.
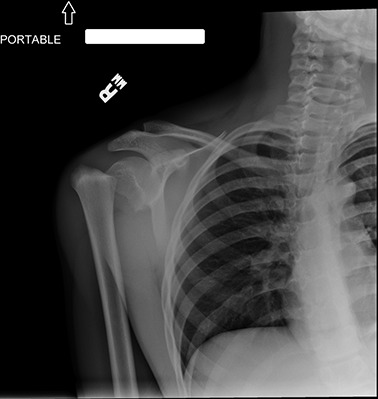
Preoperative radiograph showing displaced proximal humeral fracture.
Fig. 2.

Operating table setup showing patient and image intensifier positioning.
Perform closed reduction of the fracture with traction, abduction, and rotation.
Perform closed reduction using traction, abduction, and rotation; in some patients, a milking maneuver, analogous to closed reduction of supracondylar humeral fractures, is helpful.
Confirm reduction with orthogonal imaging.
As acceptable reduction parameters vary by age, ensure that angulation is <60° in children between 10 and 12 years and <45° in older children (Table II).
-
If the fracture is not reducible, perform open reduction via a deltopectoral approach.
-
○
Make an incision from the coracoid along the deltopectoral groove.
-
○
Mobilize the cephalic vein medially or laterally.
-
○
Retract the deltoid laterally and the pectoralis major medially.
-
○
Retract the short head of the biceps and coracobrachialis medially.
-
○
Note that common blocks to reduction include the biceps tendon and periosteum.
-
○
Video 1.
Surgical setup and technique.
Step 2: Pin Fixation
Use pin fixation to maintain fracture reduction.
Mark the axillary nerve, which is reliably within 6 cm of the anterolateral acromion.
Place 2 threaded 2.5-mm threaded Kirschner wires from the small external fixator set.
If needed, place a third pin anteriorly, posteriorly, proximally, or distally, depending on the position of the first 2 pins, for additional fixation and stability.
Place pins distal to the axillary nerve and advance to the epiphysis.
Alternatively, advance pins to the fracture site prior to fracture reduction and then advance into the epiphysis once the fracture is reduced.
Step 3: Confirm Reduction and Fixation (Figs. 3 and 4)
Fig. 3.
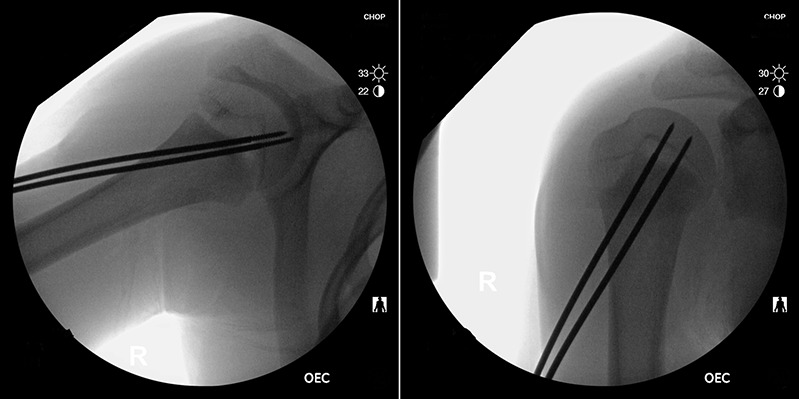
Intraoperative fluoroscopic images showing pin trajectories.
Fig. 4.
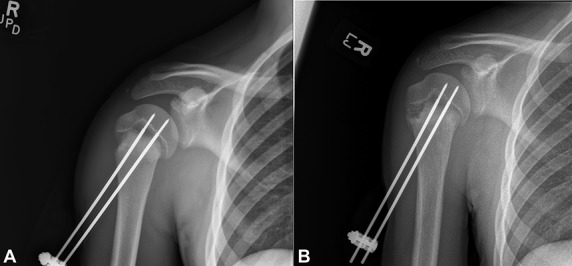
Postoperative radiographs showing the fracture at 4 days (Fig. 4-A) and 3 weeks (Fig. 4-B) after surgery.
Perform radiographic evaluation to confirm reduction and fixation.
Make anteroposterior and scapular Y radiographs to confirm reduction and fixation.
Confirm pin placement with live fluoroscopy or an approach-withdraw technique, which shows pins getting closer and further away from the articular surface and confirms that pins are not intra-articular.
Step 4: Improve Rigidity of Construct (Fig. 5)
Fig. 5.

Clinical photograph of pin and clamp construct.
Connect pins with pin-to-pin clamp to improve rigidity of the construct.
Apply a pin-to-pin clamp and tighten it.
Make relaxing incisions at the skin-pin interface if needed.
Step 5: Surgical Dressing
Apply a soft dressing and shoulder immobilizer.
Dress pin sites with Xeroform gauze (Kendall) and bulky gauze dressing.
Apply a shoulder immobilizer.
The elbow and wrist may be removed from the immobilizer as needed to allow distal range of motion. The shoulder immobilizer may be removed starting at 2 weeks for gentle range of motion (pendulum exercises) and self-care.
Results
Among several studies that have examined functional outcomes after percutaneous pinning of pediatric proximal humeral fractures2-4, Burgos-Flores et al. reported good functional outcomes in 20 of 22 pediatric patients undergoing percutaneous pinning, specifically in those under the age of 13 years with less residual displacement and angulation2. In comparison, patients at least 13 years old were noted to have a higher frequency of stiffness and dysmetria. Chaus et al. retrospectively compared percutaneous pinning and nonoperative management in 14 patients with Neer-Horwitz grade III or IV fractures3. There were no differences in functional outcomes, complications, or rate of return to preinjury activity; however, less than desirable outcomes were noted in patients at least 12 years old who were managed nonoperatively. Kraus et al., in a retrospective study, compared percutaneous pinning and intramedullary nailing in 31 pediatric patients also with Neer-Horwitz grade-III or IV proximal humeral fractures4. Their results showed no difference in functional or radiographic outcomes; however, percutaneous pinning led to both a shorter hospital stay and shorter time to implant removal.
Compared with intramedullary nailing, percutaneous pinning has the advantage of being relatively simple and often requires less operative time5. Furthermore, intramedullary nailing is not suitable for very proximal fractures, can require larger incisions, is associated with more blood loss, and has the added requirement of a second procedure under anesthesia. However, percutaneous pinning is associated with complications such as pin-site infection, decreased shoulder mobility, rotator cuff muscle irritation, and pin migration2-5. In our experience at a level-I trauma center and tertiary-care children’s hospital, where we typically perform surgery on 8 to 12 pediatric proximal humeral fractures per year, there have been no instances of pin migration with the use of threaded pins and a small external fixator. Similarly, the risk of pin-site infection is small since most pins are removed by 4 weeks; however, if infection occurs, it can be managed with oral antibiotics or pin removal. Currently, all surgeons at our institution use this construct, with reliable clinical and radiographic outcomes.
Pitfalls & Challenges
Avoiding the axillary nerve is critical during percutaneous pin placement.
It is important to avoid penetrating the articular surface with the threaded Kirschner wires.
The pin trajectory needs to be relatively acute or vertical in order to reach the epiphysis from the lateral cortex.
Relaxing skin incisions may be needed to avoid skin necrosis at the site of pin insertion.
Pin migration can occur but is unlikely with threaded Kirschner wires.
Pin care and close observation are required to avoid pin-site infection.
Footnotes
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSEST/A264).
Published outcomes of this procedure can be found at: Int Orthop. 1993;17(1):16-9, J Pediatr Orthop. 2015 Apr-May;35(3):234-9, and J Shoulder Elbow Surg. 2014 Oct;23(10):1462-7.
References
- 1.Neer CS, 2nd, Horwitz BS. Fractures of the proximal humeral epiphysial plate. Clin Orthop Relat Res. 1965. Jul-Aug;41:24-31. [PubMed] [Google Scholar]
- 2.Burgos-Flores J, Gonzalez-Herranz P, Lopez-Mondejar JA, Ocete-Guzman JG, Amaya-Alarcón S. Fractures of the proximal humeral epiphysis. Int Orthop. 1993;17(1):16-9. [DOI] [PubMed] [Google Scholar]
- 3.Chaus GW, Carry PM, Pishkenari AK, Hadley-Miller N. Operative versus nonoperative treatment of displaced proximal humeral physeal fractures: a matched cohort. J Pediatr Orthop. 2015. Apr-May;35(3):234-9. [DOI] [PubMed] [Google Scholar]
- 4.Kraus T, Hoermann S, Ploder G, Zoetsch S, Eberl R, Singer G. Elastic stable intramedullary nailing versus Kirschner wire pinning: outcome of severely displaced proximal humeral fractures in juvenile patients. J Shoulder Elbow Surg. 2014. October;23(10):1462-7. Epub 2014 Apr 13. [DOI] [PubMed] [Google Scholar]
- 5.Hutchinson PH, Bae DS, Waters PM. Intramedullary nailing versus percutaneous pin fixation of pediatric proximal humerus fractures: a comparison of complications and early radiographic results. J Pediatr Orthop. 2011. September;31(6):617-22. [DOI] [PubMed] [Google Scholar]
- 6.Bahrs C, Zipplies S, Ochs BG, Rether J, Oehm J, Eingartner C, Rolauffs B, Weise K. Proximal humeral fractures in children and adolescents. J Pediatr Orthop. 2009. Apr-May;29(3):238-42. [DOI] [PubMed] [Google Scholar]
- 7.Binder H, Schurz M, Aldrian S, Fialka C, Vécsei V. Physeal injuries of the proximal humerus: long-term results in seventy two patients. Int Orthop. 2011. October;35(10):1497-502. Epub 2011 May 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dobbs MB, Luhmann SL, Gordon JE, Strecker WB, Schoenecker PL. Severely displaced proximal humeral epiphyseal fractures. J Pediatr Orthop. 2003. Mar-Apr;23(2):208-15. [PubMed] [Google Scholar]
- 9.Hohloch L, Eberbach H, Wagner FC, Strohm PC, Reising K, Südkamp NP, Zwingmann J. Age- and severity-adjusted treatment of proximal humerus fractures in children and adolescents. A systematical review and meta-analysis. PLoS One. 2017. August 24;12(8):e0183157. [DOI] [PMC free article] [PubMed] [Google Scholar]


