Abstract
Aims
It is unknown whether kinematic alignment (KA) objectively improves knee balance in total knee arthroplasty (TKA), despite this being the biomechanical rationale for its use. This study aimed to determine whether restoring the constitutional alignment using a restrictive KA protocol resulted in better quantitative knee balance than mechanical alignment (MA).
Methods
We conducted a randomized superiority trial comparing patients undergoing TKA assigned to KA within a restrictive safe zone or MA. Optimal knee balance was defined as an intercompartmental pressure difference (ICPD) of 15 psi or less using a pressure sensor. The primary endpoint was the mean intraoperative ICPD at 10° of flexion prior to knee balancing. Secondary outcomes included balance at 45° and 90°, requirements for balancing procedures, and presence of tibiofemoral lift-off.
Results
A total of 63 patients (70 knees) were randomized to KA and 62 patients (68 knees) to MA. Mean ICPD at 10° flexion in the KA group was 11.7 psi (SD 13.1) compared with 32.0 psi in the MA group (SD 28.9), with a mean difference in ICPD between KA and MA of 20.3 psi (p < 0.001). Mean ICPD in the KA group was significantly lower than in the MA group at 45° and 90°, respectively (25.2 psi MA vs 14.8 psi KA, p = 0.004; 19.1 psi MA vs 11.7 psi KA, p < 0.002, respectively). Overall, participants in the KA group were more likely to achieve optimal knee balance (80% vs 35%; p < 0.001). Bone recuts to achieve knee balance were more likely to be required in the MA group (49% vs 9%; p < 0.001). More participants in the MA group had tibiofemoral lift-off (43% vs 13%; p < 0.001).
Conclusion
This study provides persuasive evidence that restoring the constitutional alignment with KA in TKA results in a statistically significant improvement in quantitative knee balance, and further supports this technique as a viable alternative to MA.
Cite this article: Bone Joint J. 2020;102-B(1):117–124
Keywords: Kinematic alignment, Constitutional alignment, Mechanical alignment, Total knee arthroplasty, Soft tissue balance
Introduction
The causes of dissatisfaction following total knee arthroplasty (TKA) are likely to be multifactorial, with surgical factors such as instability, malalignment, patellofemoral maltracking, and stiffness reported to be significant contributors.1-4 Such dissatisfaction has led some surgeons to question the focus on creating the theoretically ideal mechanically aligned environment for the implant,5-8 suggesting instead ways to accurately recreate the constitutional (or pre-arthritic) alignment of the knee9 with a goal of improving patient satisfaction.10-12
The kinematic alignment (KA) method13 aims to restore the constitutional knee joint by creating bone resections parallel to the pre-disease surface of distal femur, posterior femur, and proximal tibia, as opposed to cuts oriented perpendicular to the long axis of each bone. The rationale is that a knee aligned to the patient’s native anatomy will be better balanced and therefore will require little, if any, adjustment of the soft-tissue envelope to more closely approximate normal knee kinematics.10 It remains unclear whether such kinematic techniques improve quantitatively measured knee balance when compared with mechanical alignment (MA), despite evidence that this technique may contribute to improved patient outcomes.13-17
The aim of this study was to assess whether restoring the patient’s constitutional alignment during TKA using a restrictive KA protocol results in better quantitative soft-tissue balance when compared with the conventional method of MA. The null hypothesis was that there would be no difference in mean intercompartmental pressure difference (ICPD) at 10° of knee flexion in patients who underwent TKA performed with a restrictive safe zone KA protocol when compared with those having surgery using MA. Additionally, we wished to test null hypotheses that a restrictive KA protocol would result in no difference in mean ICPDs at higher degrees of knee flexion, on the proportion of balanced knees, number of balancing procedures, and number of cases of tibiofemoral lift-off when compared with MA.
Methods
Study design
We conducted a randomized, controlled, parallel-group superiority trial comparing intraoperative soft-tissue balance in TKAs implanted using kinematic versus MA with a 1:1 ratio. Participants, assessors and statisticians were blinded in order to enable unbiased collection and analysis of patient-reported and functional outcomes. Allocation was performed via sequentially numbered, sealed opaque envelopes. Randomization was undertaken using computer-generated permuted blocks of four, with surgeons unaware of block size. Bilateral procedures were included and randomized once, with both sides being assigned to the same group. The study protocol was approved by Bellberry Ethics Committee (#2017-12-911) and was prospectively registered with the Australian New Zealand Clinical Trials Registry (#ACTRN12617001627347).
Participants
Between February and August 2018, consecutive patients listed at our knee clinic to undergo primary TKA were screened for eligibility resulting in 125 participants and 138 knees (74 males, 51 females; mean age 67.5 years (36 to 89)). Patients were considered eligible for inclusion if they were scheduled for primary, unilateral or bilateral TKA for osteoarthritis, inflammatory arthritis, or post-traumatic osteoarthritis. Two knee arthroplasty surgeons (SJM, DBC) performed all procedures at one private hospital in Sydney, Australia. Each surgeon has been in clinical practice for 13 years and performs between 200 and 300 TKAs annually. Both surgeons routinely performed mechanically aligned TKAs, and prior to commencement of the study performed approximately 20 navigated KA TKAs to avoid a potential impact of the surgical learning curve on the study.
Patients were excluded if they had prior grade 3 ligamentous knee injury to posterolateral corner or lateral collateral ligament. Patients with previous grade 3 medial collateral ligament injuries treated conservatively were included if they were deemed by the surgeon to have healed with a maximum of grade 1 laxity. Patients with prior femoral, tibial, or patellofemoral osteotomies, or extra-articular femoral or tibial malunions with deformity greater than 5° in any plane were excluded.
Preoperative plans and groups
Surgical planning was undertaken with weight-bearing, long leg alignment radiographs as per Paley.18 The hip-knee-ankle (HKA) angle, lateral distal femoral angle (LDFA), and medial proximal tibial angle (MPTA) were measured using a software-based measurement tool as per Bellemans et al.9
In the control group (MA), initial femoral and tibial bone resections were positioned perpendicular to the mechanical axis of each bone and at an HKA angle of 0°.5-8,19 Femoral component rotation was set parallel to the surgical transepicondylar axis with secondary rotational referencing perpendicular to the anteroposterior sulcus axis and 3° externally rotated to the posterior condylar axis.
In the intervention group (KA), bone resections were undertaken within a restrictive alignment safe zone of 4° valgus to 3° varus for recreation of the LDFA, 3° valgus to 4° varus for the MPTA, and 5° varus to 4° valgus for the HKA. If the preoperative plan required LDFA and MPTA resections that would lead to an HKA outside the safe zone, then LDFA and MPTA were incrementally adjusted until the final HKA did not exceed the boundaries of the safe zone. To reduce the risk of subsidence of the implant, patients with a history of medically treated osteoporosis, insufficiency fractures, or those aged over 80 years had the safe zones for LFDA and MPTA narrowed to 3° valgus to 3° varus, and HKA narrowed to 4° varus to 3° valgus. The angles bounding these safe zones were centred on means describing the normal distribution of these angles,9 as well as studies examining implant alignment in the context of survivorship.6-8,20 Femoral component rotation was initially set parallel to the native posterior condylar axis. If the planned tibial resection angle was reduced in order to bring it within the safe zone, the femoral component was externally rotated by the same amount in order to rebalance the flexion gap.
Surgical technique
A posterior-stabilized, fully cemented total knee prosthesis was used with patellar resurfacing in all cases (Legion; Smith & Nephew, Memphis, Tennessee, USA). All TKAs were implanted using computer-assisted navigation (OrthoMap Precision Navigation; Stryker, Kalamazoo, Michigan, USA) to improve accuracy as well as to ensure consistency between groups. All implants were aligned according to group allocation. Trial components were inserted prior to any soft-tissue releases. During trialling, the surgeon determined the most suitable tibial insert size. The extensor mechanism was approximated using towel clips, and the knee cycled through a range of motion.21
ICPD assessments and balance
The pressure sensor insert (VERASENSE; OrthoSensor, Dania Beach, Florida, USA) recorded initial knee ICPDs at 10°, 45°, and 90°, confirmed with computer-assisted navigation. Compartment pressures were recorded by the operating surgeon and surgical assistant. The absolute mean ICPD of the two readings constituted the primary endpoint.
The surgeon then undertook final balancing by standard surgical techniques, and utilizing the sensor as per Gustke et al.22 All knees were considered balanced if they achieved an ICPD of 15 psi or less at all three flexion angles.23,24 Improved one-year functional and satisfaction scores have been reported in patients with ICPDs less than 15 psi.24,25 Further bony resection was performed if the absolute pressure in one compartment was greater than 60 psi, or an ICPD was greater than 40 psi. If the ICPD was between 16 psi and 40 psi, a soft-tissue release was performed. The aim was to achieve a final ICPD of 15 psi or less, with a single compartmental pressure of 40 psi or less at the three flexion angles.
Endpoints at surgery and postoperative outcomes
The primary endpoint with respect to improved knee balance was the difference of the mean ICPD at 10° of flexion between groups. This was recorded with trial implants in situ and prior to balancing procedures. A flexion of 10° was chosen as the primary endpoint as this is the position in which weight acceptance occurs during the gait cycle and walking on level ground is the most common activity after TKA. Additionally, the planning for KA was performed in the coronal plane to give distal femoral and proximal tibial resections and resultant extension gap, as opposed to a posterior femoral resection determining flexion gap balance. A primary endpoint measured at 10° (near extension) would therefore better reflect the different surgical technique in the KA cohort.
Secondary endpoints of mean ICPDs at 45° and 90° corresponded to mid- and high-flexion activities such as stair-climbing and rising from a seated position. We recorded the need for subsequent balancing procedures (further bony resection or soft-tissue releases) once pressures were recorded. We determined the proportions in each group that were balanced and recorded tibiofemoral ‘lift-off’ (no contact in one compartment with at least 20 psi of pressure in the contralateral compartment, agreed by both observers) as an indicator of significant imbalance.26,27 The requirement for a 20 psi minimum pressure of the contralateral side was to ensure that the zero reading was not due to an overall reduced joint tension, and instead reflected significant tightness of the collateral ligament on the contralateral side of the lift-off.26 Total operative time in minutes from skin incision to wound closure was recorded.
Radiological assessment of postoperative alignment was undertaken with CT using the Perth protocol.28,29 We analyzed the final postoperative CT alignment in both groups with respect to neutral MA and final target alignments (± 2° and ± 3°) for HKA, LDFA, and MPTA.
Finally, we recorded preoperative and one-year postoperative patient-reported outcome scores using the Knee Injury and Osteoarthritis Outcome Score 4 (KOOS4), the aggregated mean score of the subscales that are most specific to TKA recovery: pain, symptoms, function in daily living, and knee-related quality of life30,31 along with all five subscales of KOOS. In addition, we recorded the Forgotten Joint Score-12 (FJS-12), which focuses on patients’ awareness of their knees in everyday life,32 and the EuroQol five-dimension five-level questionnaire (EQ-5D-5L) as a standard measure of overall health status.33,34
Sample size
We analyzed the ICPDs of 280 consecutive mechanically aligned TKAs and found a mean initial 10° ICPD of 30 psi (SD 30) prior to knee balancing. Given the recommended value of 15 psi in order to consider the knee balanced, we decided that a reduction of 15 psi would represent a clinically meaningful difference to achieve using KA prior to releases being performed. Using a 5% significance, a SD of 30 and an 80% power to detect a mean pressure reduction of 15 psi between groups, a sample size of 125 was required. As the primary endpoint was an intraoperative measurement, no loss to follow-up was included in the calculation.
Statistical analysis
Independent-samples and paired t-tests were used to compare mean differences between continuous variables and reported with 95% confidence intervals (CIs). The Mann-Whitney U test was used to compare mean differences for non-normally distributed data. Chi-squared tests were used to compare proportions between groups. Intraclass correlation coefficients with 95% CIs were used to assess absolute agreement between the two observers with a two-way mixed effects model. Poor reliability was considered for values under 0.5, moderate reliability for 0.5 to 0.75, good reliability for 0.75 to 0.9, and excellent above 0.9. Statistical significance was set at p < 0.05.
Results
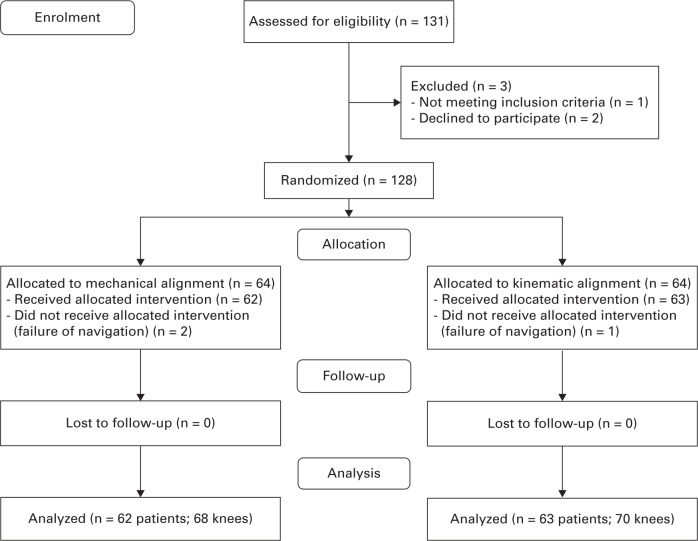
A total of 131 consecutive patients were eligible for inclusion. Two patients refused to participate, one patient did not meet the inclusion criteria, and three patients were excluded from final analysis due to inability to assess the primary endpoint. There were 62 patients (68 knees) in the MA group and 63 patients (70 knees) in the KA group who received the allocated intervention and were included in statistical analysis (Figure 1). There were no significant preoperative differences between groups (Table I).
Table I.
Patient demographics and radiological characteristics for each group.
| Characteristic | MA | KA | p-value |
|---|---|---|---|
| Patients, n | 62 | 63 | N/A |
| Total knee arthroplasty cases, n | 68 | 70 | N/A |
| Bilateral cases, n | 6 | 7 | N/A |
| Mean age, yrs (range) | 69.0 (56 to 86) | 67.4 (36 to 89) | 0.322* |
| Sex ratio, male:female, n | 28:34 | 23:40 | 0.225† |
| Side, left:right, n | 26:42 | 34:36 | 0.221† |
| Body mass index, kg/m2 | 30.1 | 30.2 | 0.883* |
| Mean preoperative HKA angle, ° (range) | -3.7 (-17.6 to +14.7) | -2.8 (-16.0 to +19.9) | 0.505* |
| Mean preoperative LDFA, ° (range) | 87.6 (81.6 to 95.4) | 87.5 (80.0 to 92.2) | 0.886* |
| Mean preoperative MPTA, ° (range) | 87.3 (81.6 to 91.5) | 87.8 (80.1 to 94.2) | 0.259* |
Independent samples t-test.
Chi-squared test.
HKA, hip-knee-ankle angle; KA, kinematic alignment; LDFA, lateral distal femoral angle; MA, mechanical alignment; MPTA, medial proximal tibial angle; N/A, not applicable.
Fig. 1.
Study enrolment flow diagram.
Intercompartmental sensor pressure agreement between observers
Intraclass correlation coefficients for ICPD measures showed excellent agreement between the two observers. Mean ICCs were 0.970 (95% CI, 0.958 to 0.979), 0.962 (95% CI, 0.947 to 0.973), and 0.923 (95% CI, 0.892 to 0.945), at 10°, 45°, and 90°, respectively (p < 0.001 at all angles).
Primary outcome – mean intercompartmental pressure difference at 10°
The mean ICPD at 10° in the MA group was 32.0 psi (SD 28.9; 0 to 138), which was nearly three times more than the KA group ICPD of 11.7 psi (SD 13.1; 0 to 63; p < 0.001, independent samples t-test).
Intercompartmental pressure difference at all knee flexion angles
The mean ICPD in the MA group was almost twice that of patients undergoing the KA protocol at 45° and 90° of flexion of the knee (Table II).
Table II.
Mean intercompartmental pressure difference at 10°, 45°, and 90° of knee flexion for mechanical and kinematic alignment groups.
| Knee angle, ° | Intercompartmental pressure difference | |||
|---|---|---|---|---|
| Mean MA, psi | Mean KA, psi | Mean difference, psi (95% CI) | p-value* | |
| 10 | 32.0 | 11.7 | 20.3 (12.8 to 27.8) | < 0.001† |
| 45 | 25.2 | 14.8 | 10.3 (3.4 to 17.2) | 0.004† |
| 90 | 19.1 | 11.7 | 7.4 (2.9 to 12.0) | 0.002† |
Independent samples t-test.
Statistically significant.
CI, confidence interval; KA, kinematic alignment; MA, mechanical alignment.
Proportion of balanced knees between groups
The proportion of knees that were unbalanced in each group was determined in order to calculate absolute risk, absolute risk reduction, and relative risk reduction. More than twice as many knees were balanced in the KA group at 10° (80%; 56/70 knees) when compared with the MA group (35%; 24/68 knees; p < 0.001, chi-squared test). The absolute and relative risks of having an unbalanced knee at each flexion angle are presented in Table III. In patients undergoing TKA with KA, there was a relative risk reduction of knee imbalance of 69%, 27%, and 48% at 10°, 45°, and 90°, respectively, when compared with MA group of patients. There was a significant relative risk reduction by undertaking a KA procedure at 10° and 90° of knee flexion compared with MA.
Table III.
The absolute and relative risks of an unbalanced knee when comparing mechanical alignment (MA) and kinematic alignment (KA) techniques in total knee arthroplasty.
| Knee angle, ° | MA absolute risk of being unbalanced, % (n) | KA absolute risk of being unbalanced, % (n) | Absolute risk reduction, % | Relative risk reduction, % | p-value* |
|---|---|---|---|---|---|
| 10° | (65) 44 | (20) 14 | 45 | 69 | < 0.001† |
| 45° | (54) 37 | (40) 28 | 14 | 27 | 0.090 |
| 90° | (47) 32 | (24) 17 | 23 | 48 | 0.005† |
Chi-squared test.
Statistically significant.
KA, kinematic alignment; MA, mechanical alignment.
Requirements for subsequent knee balancing procedures
Additional bony resection to alter the final alignment of the knee were more likely to be required in the MA group to achieve optimal knee balance (49% MA group, 9% KA group; p < 0.001, chi-squared test). The majority of such resections were made on the tibia (Table IV). A higher proportion of resections required additional soft tissue balancing in the MA group.
Table IV.
Difference in requirements for knee balancing procedures during total knee arthroplasty using either mechanical alignment (MA) or kinematic alignment techniques.
| Knee balancing intervention | MA, n (%); n = 68 | KA, n (%); n = 70 | p-value |
|---|---|---|---|
| Type of knee balancing intervention | |||
| Patients requiring soft-tissue releases only | 11 (16) | 16 (23) | 0.439† |
| Patients requiring bone recuts only | 18 (26) | 1 (1) | < 0.001* † |
| Patients requiring both bone recuts and soft-tissue releases | 15 (22) | 5 (7) | 0.013* † |
| Proportion of bone recuts | |||
| Patients requiring any bone cuts | 33 (49) | 6 (9) | < 0.001* † |
| Tibial recuts only | 24 (35) | 4 (6) | < 0.001* † |
| Femoral recuts only | 5 (7) | 2 (3) | 0.271‡ |
| Both tibial and femoral recuts | 4 (6) | 0 (0) | 0.056‡ |
Statistically significant.
Chi-squared test.
Fisher’s exact test.
KA, kinematic alignment; MA, mechanical alignment.
Presence of lift-off
Prior to knee balancing, there was a significantly higher proportion of patients with lift-off in the MA group in at least one position (43% MA, 13% KA; p < 0.001, chi-squared test). The majority of these phenomena were noted in the lateral compartment (23/29 cases in MA group, 1/9 cases in KA group). When comparing two or more positions with lift-off, 27% had lift-off in the MA group compared with 4% in the KA group (p < 0.001, chi-squared test).
Operative time
The mean total operative time was 78 minutes in the MA group (SD 12.3; 58 to 120) and 79 minutes in the KA group (SD 17.0; 58 to 160; p = 0.907; independent samples t-test).
Alignment
The postoperative alignment was within 3° of the surgically recorded computer-assisted navigation resections in 94% of cases for both groups (Table V). The LDFA in the KA group had a greater mean valgus angulation (KA 89.2° (SD 1.8°; 85° to 93°), MA 90.6° (SD 1.5°; 86° to 93°); p < 0.001, independent samples t-test). By contrast, the MPTA in the KA group had a greater mean varus angulation (KA 88.9° (SD 1.8°; 84° to 95°), MA 90.0° (SD 1.9°; 85° to 94°; p = 0.003, independent samples t-test). There was no significant difference in the mean hip-knee-ankle (HKA) or the percentage of cases within ± 2° and ± 3° of neutral MA when comparing KA with MA with secondary balancing (including bone recuts).
Table V.
Postoperative CT radiological alignment for mechanical alignment (MA) and kinematic alignment (KA) groups with subsequent knee balancing if indicated. Negative values represent varus and positive values represent valgus for HKA angle range; ± 2° and ± 3° alignment range is inclusive of upper and lower boundaries and centred around neutral MA.
| Angle | MA group alignment | KA group alignment | p-value |
|---|---|---|---|
| HKA angle | |||
| Mean angle, ° (SD; range) | -0.6 (2.3; -6 to 4) | -0.2 (2.3; -5 to 5) | 0.322* |
| Within ± 2° of zero mechanical alignment, % | 71 | 71 | 0.913† |
| Within ± 3° of zero mechanical alignment, % | 84 | 86 | 0.757† |
| Within ± 2° of final navigation alignment, % | 87 | 83 | 0.679† |
| Within ± 3° of final navigation alignment, % | 94 | 94 | 0.966† |
| LDFA | |||
| Mean, ° (SD; range) | 90.6 (1.5; 86 to 93) | 89.2 (1.8; 85 to 93) | < 0.001* ‡ |
| Within ±2° of zero mechanical alignment, % | 85 | 80 | 0.412† |
| Within ± 3° of zero mechanical alignment, % | 99 | 96 | 0.324† |
| Within ± 2° of final navigation alignment, % | 94 | 83 | 0.039† ‡ |
| Within ± 3° of final navigation alignment, % | 100 | 97 | 0.160† |
| MPTA | |||
| Mean, ° (SD; range) | 90.0 (1.9; 85 to 94) | 88.9 (1.83; 84 to 95) | 0.003* ‡ |
| Within ± 2° of zero mechanical alignment, % | 84 | 79 | 0.430† |
| Within ± 3° of zero mechanical alignment, % | 96 | 87 | 0.078† |
| Within ± 2° of final navigation alignment, % | 87 | 89 | 0.747† |
| Within ± 3° of final navigation alignment, % | 97 | 99 | 0.542† |
Independent samples t-test.
Chi-squared test.
Statistically significant.
HKA, hip-knee-ankle; KA, kinematic alignment; LDFA, lateral distal femoral angle; MA, mechanical alignment; MPTA, medial proximal tibial angle.
Clinical outcomes
Table VI presents a summary of patient-reported outcome scores. There were no statistically significant differences between groups when comparing baseline with one-year postoperative scores. It should be noted that a significant proportion of participants assigned to MA and KA groups underwent subsequent alignment changes and soft-tissue balancing procedures based on sensor pressures if required, hence these outcomes do not represent a direct comparison of MA and KA.
Table VI.
Patient-reported outcome scores for mechanical alignment and kinematic alignment groups comparing preoperative and one-year postoperative scores.
| Score | Preoperative mean, psi (SD) | Postoperative mean, psi (SD) | Mean score change, psi (SD) | Mean difference (MA - KA), psi (95% CI) | p-value* |
|---|---|---|---|---|---|
| KOOS4 | -1.2 (-8.5 to 6.0) | 0.735 | |||
| MA | 40.0 (16.7) | 79.6 (14.7) | 39.6 (20.6) | ||
| KA | 41.5 (13.5) | 82.2 (16.4) | 40.8 (21.2) | ||
| KOOS Symptoms | -5.5 (13.6 to 2.6) | 0.180 | |||
| MA | 45.9 (21.6) | 77.0 (14.6) | 31.2 (23.2) | ||
| KA | 43.8 (16.2) | 80.5 (16.5) | 36.7 (23.1) | ||
| KOOS Pain | 0.8 (-7.0 to 8.6) | 0.845 | |||
| MA | 41.8 (19.6) | 85.4 (16.0) | 43.6 (22.9) | ||
| KA | 43.9 (13.8) | 86.7 (16.1) | 42.8 (21.7) | ||
| KOOS ADL | 1.4 (-6.6 to 9.4) | 0.736 | |||
| MA | 46.9 (18.8) | 84.5 (16.4) | 37.6 (23.6) | ||
| KA | 50.3 (16.9) | 86.5 (15.2) | 36.2 (22.2) | ||
| KOOS Sports | -9.8 (-21.1 to 1.5) | 0.088 | |||
| MA | 23.8 (27.4) | 57.4 (29.1) | 33.6 (36.7) | ||
| KA | 18.9 (17.8) | 62.3 (25.4) | 43.4 (27.3) | ||
| KOOS QoL | -1.6 (-10.9 to 7.7) | 0.733 | |||
| MA | 25.5 (16.1) | 71.5 (21.8) | 46.0 (26.1) | ||
| KA | 27.5 (17.5) | 75.1 (22.6) | 47.6 (27.2) | ||
| FJS-12 | -6.8 (-16.2 to 2.6) | 0.155 | |||
| MA | 15.5 (16.4) | 56.8 (26.0) | 41.2 (28.1) | ||
| KA | 15.9 (13.2) | 63.9 (26.6) | 48.0 (25.8) | ||
| EQ-5D-5L | -1.4 (-6.8 to 4.0) | 0.610 | |||
| MA | 75.0 (14.5) | 82.3 (13.3) | 7.4 (16.3) | ||
| KA | 75.3 (18.4) | 84.1 (15.2) | 8.8 (14.6) |
Independent samples t-test.
ADL, function in activity of daily living subscale; CI, confidence interval; EQ-5D-5L, EuroQol five-dimension five-level questionnaire; FJS-12, Forgotten Joint Score-12; KA, kinematic alignment group with subsequent knee balancing; KOOS, Knee injury and Osteoarthritis Outcome Score; KOOS4, aggregated mean score of subscales of pain, symptoms, function in daily living, and knee-related quality of life; MA, mechanical alignment group with subsequent knee balancing; QoL, quality of life subscale.
Discussion
This randomized controlled trial confirmed that recreating the constitutional alignment of the knee within a restrictive safe zone via kinematic alignment results in a lower mean ICPD at 10° of flexion compared with mechanical alignment. Significantly lower ICPDs were also seen at higher knee flexion angles in the KA group. At all knee positions, knees were found to have more equal mediolateral compartmental loads when KA was used, compared with MA. The ICPD decreased slightly between groups with increasing knee flexion. This may have been as a result of the coronal nature of the radiological planning of kinematic bone resections, leading to more pronounced differences near full extension than when in flexion.
The high rate of knee balancing noted in the current study is most likely multifactorial. The sensor may overestimate the requirement to undertake knee balancing because an optimal ICPD that correlates with patient outcomes has not been demonstrated by high-quality studies.25,35,36 Additionally, surgeon-defined assessment of knee balance is a poor predictor of the true soft-tissue balance compared with sensor data.37 Generally, it is likely that a high proportion of knees are left unbalanced despite surgeon assessment of appropriate balance.
Severe knee imbalance in this study was evidenced by the presence of lift-off, which indicates significant collateral ligament tightness on the contralateral side of the tibiofemoral joint separation and secondary unicompartmental load bearing.26,27,38,39 Although some degree of lateral tibiofemoral laxity is recognized to occur normally in flexion,40 the lift-offs recorded using our pre-defined criterion of high sensor pressures in the opposite compartment, particularly in extension, indicate that this phenomenon was most likely pathological. The rate of lift-off in our MA group using sensors was similar to that in other studies using different measures. The majority were noted to occur in the lateral compartment. This may suggest that iatrogenic overtightening of the medial collateral ligament results when a knee with constitutional varus develops relative valgus when positioned in neutral MA. Dennis et al26 fluoroscopically examined 40 successful TKAs and noted lift-off in 70% of cruciate-retaining and 80% of posterior-stabilized designs. Insall et al27 noted fluoroscopically demonstrated lift-off in 40% of TKAs in flexion, and Kim et al38 reported lift-off with axial radiographs in 18% of navigated and 45% of non-navigated TKAs.
Vandekerckhove et al41 examined 95 retrieved polyethylene inserts and noted more insert wear laterally in varus knees, which they felt may be due to lateral condylar lift-off inducing impact and shear loading. Li et al42 also reported that postoperative varus alignment predisposes to wear of both medial and lateral sides of retrieved polyethylene inserts, which may support the theory of lateral condylar lift-off as a cause of impaction wear. Although there is a concern regarding increased alignment outliers with KA,43 it is possible that the technique may actually reduce polyethylene wear through reduced incidence of lift-off. Our study did not find an increase in outliers with KA when compared with MA, despite KA significantly reducing lift-off.
The current study has several limitations. First, the one-year clinical results do not represent a true comparison of the two methods as both groups underwent balancing if indicated, due to the ethical conflict inherent in failing to address a knee confirmed by instrumentation to be unbalanced. Nearly half of all mechanically aligned knees subsequently underwent further bony resections that likely aligned them closer to their constitutional alignment. The results do indicate that both alignment strategies with subsequent knee balancing using sensor technology may produce similar early clinical outcomes. Kinematic alignment may, however, provide a potential surgical efficiency advantage in the absence of sensor technology as initial balance was achieved more readily and required significantly fewer balancing procedures. We used only one type of knee prosthesis with a posterior-stabilized design. As such, the results of this study may not be applicable to other implant designs, especially those with differing levels of stability or more anatomical articulations, as it is known that flexion laxities are altered with resection of the posterior cruciate ligament.44-47 Although patient blinding was undertaken, the surgeon was not blinded when sensor measures were recorded, and hence we cannot exclude measurement or treatment bias. For this reason, a second observer was used and intraclass correlations showed high levels of agreement between measures, thereby reducing the risk of measurement bias. Knee balancing procedures were performed based on the predefined sensor pressures, aiming to reduce the risk of treatment bias. The cost of the sensor technology used to determine and undertake knee balancing may prohibit widespread adoption. For the purposes of this study, however, the sensors provided an objective, quantifiable measure of knee balance.
The results of this study provide persuasive evidence that restoration of the patient’s constitutional alignment within a restrictive kinematic safe zone significantly improves knee balance, reduces knee balancing procedures, and may more closely restore native soft-tissue tension when compared with MA. Further high-quality randomized trials with long-term follow-up to evaluate efficacy, safety, and subsequent revision risk are needed to confirm the validity and efficacy of this approach.
Take home message
- Restoring the constitutional alignment of the knee using a restrictive kinematic protocol improves quantitative knee balance when compared to mechanical alignment.
- Twice as many patients undergoing kinematic alignment will have an optimally balanced knee when compared to mechanical alignment.
- Kinematic alignment significantly reduces the rate of tibiofemoral lift-off and the requirement for knee balancing procedures.
Author contributions
S. J. MacDessi: Conceived and designed the study, Produced the manuscript, Analyzed the data, Gave final approval.
W. Griffiths-Jones: Designed the study, Produced the manuscript.
D. B. Chen: Designed the study, Produced the manuscript.
S. Griffiths-Jones: Produced the manuscript, Planned kinematic alignment.
J. A. Wood: Coordinated the study, Collected the data, Produced the manuscript.
A. D. Diwan: Interpreted the data, Produced the manuscript.
I. A. Harris: Interpreted the data, Produced the manuscript, Gave final approval.
Funding statement
The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
S. J. MacDessi and D. B. Chen report institutional grants (paid to Sydney Knee Specialists) from Smith & Nephew not related to this study. S. J. MacDessi, W. Griffiths-Jones, and D.B. Chen hold a personal pending patent in knee alignment not related to this study.
Ethical review statement
The study protocol was approved by Bellberry Ethics Committee (#2017-12-911).
Trial registration number
This study was prospectively registered with the Australian New Zealand Clinical Trials Registry (#ACTRN12617001627347).
Open access statement
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
This article was primary edited by P. Page.
References
- 1.Dalury DF, Pomeroy DL, Gorab RS, Adams MJ. Why are total knee arthroplasties being revised? J Arthroplasty. 2013;28(8 Suppl):120–121. [DOI] [PubMed] [Google Scholar]
- 2.Lombardi AV Jr, Berend KR, Adams JB. Why knee replacements fail in 2013: patient, surgeon, or implant? Bone Joint J. 2014;96-B(11 Supple A):101–104. [DOI] [PubMed] [Google Scholar]
- 3.Schroer WC, Berend KR, Lombardi AV, et al. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011. J Arthroplasty. 2013;28(8 Suppl):116–119. [DOI] [PubMed] [Google Scholar]
- 4.Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J. Why are total knee arthroplasties failing today—has anything changed after 10 years? J Arthroplasty. 2014;29(9):1774–1778. [DOI] [PubMed] [Google Scholar]
- 5.Aglietti P, Buzzi R. Posteriorly stabilised total-condylar knee replacement. Three to eight years’ follow-up of 85 knees. J Bone Joint Surg Br. 1988;70-B(2):211–216. [DOI] [PubMed] [Google Scholar]
- 6.Berend ME, Ritter MA, Meding JB, et al. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. 2004;428:26–34. [DOI] [PubMed] [Google Scholar]
- 7.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24(6 Suppl):39–43. [DOI] [PubMed] [Google Scholar]
- 8.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed] [Google Scholar]
- 9.Bellemans J, Colyn W, Vandenneucker H, Victor J.. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res. 2012;470(1):45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res. 2013;471(3):1000–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsumoto T, Takayama K, Ishida K, Hayashi S, Hashimoto S, Kuroda R. Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Joint J. 2017;99-B(5):640–646. [DOI] [PubMed] [Google Scholar]
- 12.McEwen P, Balendra G, Doma K. Medial and lateral gap laxity differential in comput er-assisted kinematic total knee arthroplasty. Bone Joint J. 2019;101-B(3):331–339. [DOI] [PubMed] [Google Scholar]
- 13.Howell SM, Kuznik K, Hull ML, Siston RA. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics. 2008;31(9):857–863. [DOI] [PubMed] [Google Scholar]
- 14.Delport H, Labey L, Innocenti B, De Corte R, Vander Sloten J, Bellemans J. Restoration of constitutional alignment in TKA leads to more physiological strains in the collateral ligaments. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2159–2169. [DOI] [PubMed] [Google Scholar]
- 15.Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG. Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics. 2012;35(2):e160–e169. [DOI] [PubMed] [Google Scholar]
- 16.Howell SM, Papadopoulos S, Kuznik KT, Hull ML. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2271–2280. [DOI] [PubMed] [Google Scholar]
- 17.Hutt J, Masse V, Lavigne M, Vendittoli PA. Functional joint line obliquity after kinematic total knee arthroplasty. Int Orthop. 2016;40(1):29–34. [DOI] [PubMed] [Google Scholar]
- 18.Paley D. Principles of Deformity Correction. Heidelberg: Springer-Verlag; 2003. [Google Scholar]
- 19.Bargren JH, Blaha JD, Freeman MA. Alignment in total knee arthroplasty. Correlated biomechanical and clinical observations. Clin Orthop Relat Res. 1983;173:178–183. [PubMed] [Google Scholar]
- 20.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92-A(12):2143–2149. [DOI] [PubMed] [Google Scholar]
- 21.Schnaser E, Lee YY, Boettner F, Gonzalez Della Valle A. The Position of the Patella and Extensor Mechanism Affects Intraoperative Compartmental Loads During Total Knee Arthroplasty: A Pilot Study Using Intraoperative Sensing to Guide Soft Tissue Balance. J Arthroplasty. 2015;30(8):1348–1353 e3. [DOI] [PubMed] [Google Scholar]
- 22.Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR. A Targeted Approach to Ligament Balancing Using Kinetic Sensors. J Arthroplasty. 2017;32(7):2127–2132. [DOI] [PubMed] [Google Scholar]
- 23.Chow J, Wang K, Elson L, Anderson C, Roche M. Effects of Cementing on Ligament Balance During Total Knee Arthroplasty. Orthopedics. 2017;40(3):e455-e459. [DOI] [PubMed] [Google Scholar]
- 24.Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR. A new method for defining balance: promising short-term clinical outcomes of sensor-guided TKA. J Arthroplasty. 2014;29(5):955–960. [DOI] [PubMed] [Google Scholar]
- 25.Gustke KA, Golladay GJ, Roche MW, Jerry GJ, Elson LC, Anderson CR. Increased satisfaction after total knee replacement using sensor-guided technology. Bone Joint J. 2014;96-B(10):1333–1338. [DOI] [PubMed] [Google Scholar]
- 26.Dennis DA, Komistek RD, Walker SA, Cheal EJ, Stiehl JB. Femoral condylar lift-off in vivo in total knee arthroplasty. J Bone Joint Surg Br. 2001;83-B(1):33–39. [DOI] [PubMed] [Google Scholar]
- 27.Insall JN, Scuderi GR, Komistek RD, Math K, Dennis DA, Anderson DT. Correlation between condylar lift-off and femoral component alignment. Clin Orthop Relat Res. 2002;402:143–152. [DOI] [PubMed] [Google Scholar]
- 28.Chauhan SK, Clark GW, Lloyd S, Scott RG, Breidahl W, Sikorski JM. Computer-assisted total knee replacement. A controlled cadaver study using a multi-parameter quantitative CT assessment of alignment (the Perth CT Protocol). J Bone Joint Surg Br. 2004;86-B(6):818–823. [DOI] [PubMed] [Google Scholar]
- 29.Sikorski JM. Alignment in total knee replacement. J Bone Joint Surg Br. 2008;90-B(9):1121–1127. [DOI] [PubMed] [Google Scholar]
- 30.No authors listed The 2012 User’s Guide to: Knee injury and Osteoarthritis Outcome Score KOOS. 2012. http://www.koos.nu/index.html (date last accessed 18 October 2019).
- 31.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hamilton DF, Loth FL, Giesinger JM, et al. Validation of the English language Forgotten Joint Score-12 as an outcome measure for total hip and knee arthroplasty in a British population. Bone Joint J. 2017;99-B(2):218–224. [DOI] [PubMed] [Google Scholar]
- 33.EuroQol Group EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. [DOI] [PubMed] [Google Scholar]
- 34.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chow JC, Breslauer L. The Use of Intraoperative Sensors Significantly Increases the Patient-Reported Rate of Improvement in Primary Total Knee Arthroplasty. Orthopedics. 2017;40(4):e648-e651. [DOI] [PubMed] [Google Scholar]
- 36.Meneghini RM, Ziemba-Davis MM, Lovro LR, Ireland PH, Damer BM. Can Intraoperative Sensors Determine the “Target” Ligament Balance? Early Outcomes in Total Knee Arthroplasty. J Arthroplasty. 2016;31(10):2181–2187. [DOI] [PubMed] [Google Scholar]
- 37.MacDessi SJ, Gharaibeh MA, Harris IA. How Accurately Can Soft Tissue Balance Be Determined in Total Knee Arthroplasty? J Arthroplasty. 2019;34(2):290–294. e1. [DOI] [PubMed] [Google Scholar]
- 38.Kim SH, Lee HJ, Jung HJ, Lee JS, Kim KS. Less femoral lift-off and better femoral alignment in TKA using computer-assisted surgery. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2255–2262. [DOI] [PubMed] [Google Scholar]
- 39.Schmidt R, Komistek RD, Blaha JD, Penenberg BL, Maloney WJ. Fluoroscopic analyses of cruciate-retaining and medial pivot knee implants. Clin Orthop Relat Res. 2003;410:139–147. [DOI] [PubMed] [Google Scholar]
- 40.Freeman MA, Pinskerova V. The movement of the normal tibio-femoral joint. J Biomech. 2005;38(2):197–208. [DOI] [PubMed] [Google Scholar]
- 41.Vandekerckhove PTK, Teeter MG, Naudie DDR, Howard JL, MacDonald SJ, Lanting BA. The Impact of Coronal Plane Alignment on Polyethylene Wear and Damage in Total Knee Arthroplasty: A Retrieval Study. J Arthroplasty. 2017;32(6):2012–2016. [DOI] [PubMed] [Google Scholar]
- 42.Li Z Esposito CI, Koch CN, Lee YY, Padgett DE, Wright TM. Polyethylene Damage Increases With Varus Implant Alignment in Posterior-stabilized and Constrained Condylar Knee Arthroplasty. Clin Orthop Relat Res. 2017;475(12):2981–2991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nakamura S, Tian Y, Tanaka Y, et al. The effects of kinematically aligned total knee arthroplasty on stress at the medial tibia: A case study for varus knee. Bone Joint Res. 2017;6(1):43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chaiyakit P, Meknavin S, Hongku N. Effects of posterior cruciate ligament resection in total knee arthroplasty using computer assisted surgery. J Med Assoc Thai. 2009;92(Suppl 6):S80-S84. [PubMed] [Google Scholar]
- 45.Matsueda M, Gengerke TR, Murphy M, Lew WD, Gustilo RB. Soft tissue release in total knee arthroplasty. Cadaver study using knees without deformities. Clin Orthop Relat Res. 1999;366:264–273. [DOI] [PubMed] [Google Scholar]
- 46.Matziolis G, Mehlhorn S, Schattat N, et al. How much of the PCL is really preserved during the tibial cut? Knee Surg Sports Traumatol Arthrosc. 2012;20(6):1083–1086. [DOI] [PubMed] [Google Scholar]
- 47.Park SJ, Seon JK, Park JK, Song EK. Effect of PCL on flexion-extension gaps and femoral component decision in TKA. Orthopedics. 2009;32(10 Suppl):22–25. [DOI] [PubMed] [Google Scholar]