Abstract
Background:
Endoscopic sleeve gastroplasty (ESG) is a restrictive endoscopic bariatric procedure providing promising results. In this short case series, we analyze the technical aspects and short-term outcomes of the redo ESG.
Methods:
A retrospective analysis was done on a prospective database of all patients that were selected by a multidisciplinary team that underwent ESG between March 2017 and May 2019. Patients that underwent a redo ESG because of a progressive loss of satiety, weight regain, or insufficient weight loss due to high baseline body mass index were included. Percentage of excess weight loss (%EWL), percentage of total body weight loss (%TBWL), and the Bariatric Analysis and Reporting Outcome System (BAROS) questionnaire were evaluated during follow-up.
Results:
A total of 120 ESG procedures were performed with mean %EWL of 44.4% (± 19.5), mean %TBWL of 18.3% (± 6.7), and mean BAROS of 4.5 (± 1.7) at 12 months. Of those, four patients that underwent a redo ESG were identified. A total of three of them had a redo ESG after 12 months from the first ESG, whereas one of them had a redo ESG after 7 months. During the second procedure, old threads were removed with scissors and new stitches were positioned following a triangular pattern and avoiding overlap with the previous stitches. No adverse events were reported during the redo ESG. Six month follow-up was available for three patients, mean %EWL and %TBWL were 44.2% and 20.4%, respectively; BAROS questionnaire mean score was 6.3. One patient had only 1 month follow-up with a mean %EWL and %TBWL of 33.3% and 12.2%, respectively; BAROS questionnaire reported score was 6. All included patients reported excellent satiety feeling after redo ESG.
Conclusions:
The redo ESG short-term outcomes are completely satisfying in terms of safety and efficacy. The need to perform a redo ESG should not be considered as a failure of the previous procedure, but it can be considered as a second step of the endoscopic treatment strategy.
Keywords: bariatric endoscopy, endoscopic sleeve gastroplasty, obesity
Introduction
Obesity is a pathological clinical condition characterized by abnormal weight gain that represents a worldwide growing challenge for public health. It requires a multidisciplinary approach in both prevention and treatment. The latest clinical evidences suggest that several specialists, such as gastroenterologists, surgeons, psychiatrists, endocrinologists, and nutritionists, should collaborate with the aim of giving rise to a multidisciplinary obesity path.1 The specific type of treatment chosen for each obese patient must therefore be individualized and adapted to the comorbidity complex affecting the patient. Although bariatric surgical techniques have scientifically proven efficacy and safety, they are not suitable as a therapeutic strategy for all patients suffering from obesity. Personal limitations, lack of precise indications for surgical treatment, comorbidities associated with obesity, excessive perioperative risk, contraindications to surgery, and patient’s refusal of surgery are the main limitations of bariatric surgery. Therefore, a promising alternative in these cases is bariatric endoscopy. Endoscopic sleeve gastroplasty (ESG) is a restrictive endoscopic bariatric procedure that provides a gastric tubulization obtained by placing full-thickness stitches. It has a double mechanism of action: the first is restriction of the gastric cavity and the second is alteration of gastric peristalsis. The result is a long-lasting feeling of satiety.2 In recent years, this technique has provided excellent results: it proved to be safe (1% complication rate), quick, and statistically effective in ensuring weight loss and comorbidities improvement.3–6 The reported mean percentage of total body weight loss (%TBWL) is 17.2% at 12 months and 20.2% at 24 months, on average (Table 1).2,3,6–13 If weight resumption after surgery is considered a real failure of the technique, the need to perform a redo ESG in selected patients should not be considered as a failure of the previous procedure. ESG is repeatable per definition, likewise for every endoscopic procedure. A redo ESG can then be considered as a second step of the endoscopic treatment strategy. In this short case series, we analyze the technical aspects and short-term outcomes of the redo ESG.
Table 1.
Outcomes of endoscopic sleeve gastroplasty.
| Study | Number of patients (n) | Mean age (years) | Mean BMI | 6 months %TBWL | 12 months %TBWL | 24 months %TBWL |
|---|---|---|---|---|---|---|
| Lopez-Nava et al.8 | 55 | 43.5 ± 8.1 | 37.7 ± 4.5 | 18.9 ± 9.5 | NA | NA |
| Abu Dayyeh et al.2 | 25 | 47.6 ± 10 | 35.5 ± 2.6 | 53 ± 17 | 54 ± 40§ | 45 ± 41*§ |
| Lopez-Nava et al.3 | 154 | NA | 38.3 ± 5.5 | 15.8 ± 7.1 | 20.2 ± 12.2 | 21.3 ± 13.4 |
| Lopez-Nava et al.9 | 248 | 44.5 ± 10 | 37.8 ± 5.6 | 15.2 | NA | 18.6 |
| Sharaiha et al.10 | 91 | 43.86 ± 11.26 | 40.7 ± 7 | 14.4 | 17.6 | 20.9 |
| Alqahtani et al.6 | 1000 | 34.4 ± 9.5 | 33.3 ± 4.5 | 13.7 ± 6.8 | 15.0 ± 7.7 | 14.8 ± 8.5** |
| Fayad et al.7 | 54 | 48 | 43.1 | 17.2 | NA | NA |
| Sartoretto et al.11 | 112 | 45.1 ± 11.7 | 37.9 ± 6.7 | 14.9 ± 6.1 | NA | NA |
| Saumoy et al.12 | 128 | 43.6 | 38.9 | 13.43 | 15.8 | NA |
| Kumar et al.13 | 77 | 41.3 ± 1.1 | 36.1 ± 0.6 | 16.2 ± 0.7 | 17.4 ± 1.1 | NA |
BMI: body mass index; %EWL: percentage of excess weight loss; NA: not available; %TBWL: percentage of total body weight loss.
%EWL.
20 month follow-up.
18 month follow-up.
Methods
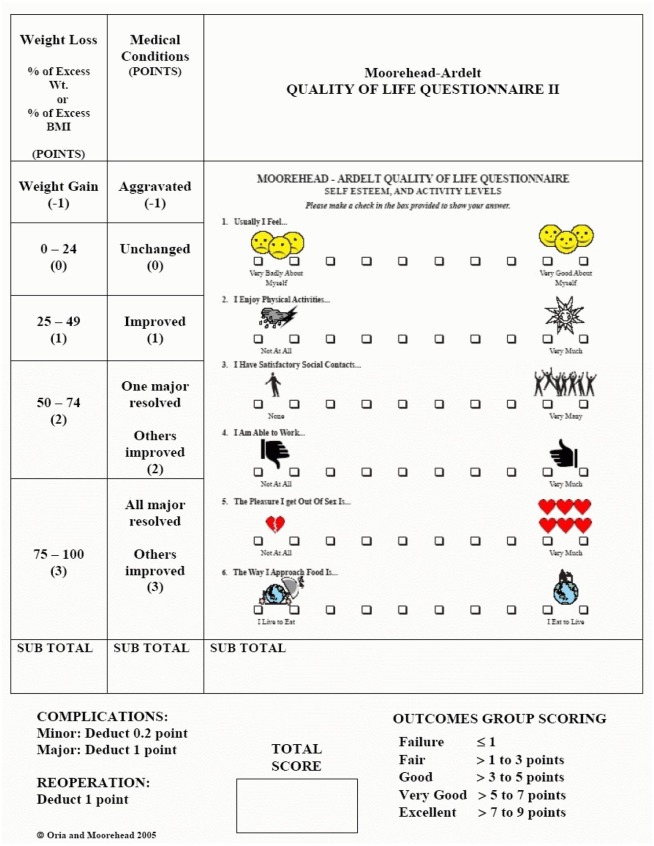
A retrospective analysis was performed on a prospective database collecting data on all patients that were selected for bariatric endoscopy by a multidisciplinary team and who underwent ESG between March 2017 and May 2019. Patients were evaluated for percentage of excess weight loss (%EWL), %TBWL and the Bariatric Analysis and Reporting Outcome System (BAROS) questionnaire (Figure 1) at 1, 3, 6, 9, and 12 months after the first ESG. Patients that registered progressive loss of satiety, weight regain or insufficient weight loss due to a high baseline body mass index (BMI) underwent a redo ESG and were included in this case series. %EWL, %TBWL and BAROS questionnaire were again evaluated after the second procedure in order to analyze short-term outcomes of the redo ESG. Indications for redo ESG were the same as for the first procedure: BMI between 30 kg/m² and 40 kg/m² (with or without comorbidities), inability to lose or maintain weight loss through diet, lifestyle change or medication intake, refusal of surgery, and contraindications to bariatric surgery. Written informed consent was obtained before the procedures for every patient. The study was approved by the ethics committee (2083/2018) of the Fondazione Policlinico Universitario Agostino Gemelli IRCCS.
Figure 1.
Bariatric Analysis and Reporting Outcome System BAROS (Morehead-Ardelt quality of life questionnaire - this instrument is copyright protected and require licensing that can be obtained from Dr. Melodie Kay Moorehead at drmoorehead.com).
Results
A total of 120 ESG procedures were performed, resulting in a mean %EWL 44.4% (± 19.5), mean %TBWL 18.3% (± 6.7), and mean BAROS score of 4.5 (± 1.7) at 12 months. Of those, four patients that underwent redo ESG (two males, two females, mean age 41 years) were identified. The first ESG had been performed with the Apollo OverStitch suturing system and with a double channel gastroscope (Olympus 2TGIF-160) under general anesthesia and with insufflation of CO2. Sutures were placed using the standard ‘U’ pattern and 4–7 stitches were placed per patient. The mean procedure time was 45 min (range 35–56). No peri-procedural complications were reported during the first ESG (Table 2). Patient 1 was a 27-year-old female with an initial BMI of 62.4 kg/m² that refused surgery and did not reach the goal in terms of weight loss after the first ESG. Patients 2, 3 and 4 before the first ESG had a mean BMI of 36 kg/m², but after initial weight loss they progressively felt less satiety and regained weight. An esophagogastroduodenoscopy was then performed in these patients, with evidence of loose threads and partial reopening of the sutures (Figure 2). Therefore, after a new multidisciplinary evaluation, the four patients were scheduled for a redo ESG.
Table 2.
Characteristics of the four patients who underwent a redo endoscopic sleeve gastroplasty.
| Patient | Age (years) | Sex | Initial BMI | First ESG n° of stiches | First ESG procedural time | First ESG complications | BMI before second ESG | Time between the two ESG procedures (months) | Second ESG n° of stiches | Second ESG procedural time | Second ESG complications | Follow-up after second ESG (months) | BMI at follow-up | %EWL at follow-up | %TBWL at follow-up | BAROS at follow-up |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 27 | F | 62.4 | 7 | 46 | None | 52.3 | 12 | 4 | 31 | None | 6 | 49.8 | 30.5 | 20.1 | 6 |
| 2 | 31 | M | 37.9 | 4 | 39 | None | 35.4 | 7 | 5 | 32 | None | 6 | 28.7 | 59.1 | 24.5 | 7 |
| 3 | 65 | M | 36.9 | 6 | 56 | None | 34.9 | 12 | 4 | 37 | None | 6 | 30.8 | 42.9 | 16.7 | 6 |
| 4 | 52 | F | 33.3 | 5 | 35 | None | 30.9 | 12 | 4 | 27 | None | 1 | 29 | 33.3 | 12.2 | 6 |
BAROS: bariatric analysis and reporting outcome system; BMI: body mass index; ESG: endoscopic sleeve gastroplasty; %EWL: percentage of excess weight loss; %TBWL: percentage of total body weight loss.
Figure 2.

Partial reopening of the sutures placed during the first ESG. Visible suture threads were cut with endoscopic seizures.
Technical features, short-term outcomes, and timing of the redo ESG
A total of three patients underwent a redo ESG after 12 months from the first ESG whereas one patient underwent the second procedure after 7 months. All second ESG procedures were again performed with the Apollo OverStitch suturing system and with a double channel gastroscope (Olympus 2TGIF-160), under general anesthesia and with insufflation of CO2. On average, 4–5 stitches were placed in 32 min (range 27–37). As the ESG procedure is inducing serosa-to-serosa or mucosa-to-mucosa adhesions with mucosal bridges (Figure 3), the gastric wall is less elastic in these patients. Therefore, in order to avoid perforations, the redo ESG procedure was performed in a technically different manner compared with the first one. Before re-suturing, all remaining old stitches were removed with endoscopic scissors and the new stitches were positioned following a triangular pattern; the rule was to place a maximum of three bites per suture line, avoiding overlap with the stitches positioned during the first ESG and without pulling too much on the tissue helix and the threads (Figure 4). No peri-procedural complications were reported during the second procedure. After the redo ESG, the patients were followed-up at 1 month, 3 months and 6 months; %EWL, %TBWL, and BAROS questionnaire were evaluated during each of these examinations. The 6-month follow-up was available for three patients: mean %EWL and %TBWL were 44.2% (range 30.5–59.1%) and 20.4% (range 16.7–24.5%), respectively, BAROS questionnaire mean score was 6.3 (range 6–7). Only one patient had a 1-month follow-up: mean %EWL and %TBWL were 33.3% and 12.2%, respectively, BAROS questionnaire reported score was 6. Every patient reported excellent satiety feeling. On average, the time elapsed between the two procedures was 10.3 months (range 7–12 months).
Figure 3.

Mucosal bridges induced by the first ESG.
Figure 4.

Suggested sites for re-biting the gastric wall (blue circles) during the redo ESG to avoid high-tension-related perforation.
Discussion
Bariatric endoscopy is proposed as a minimally invasive strategy to offer an adequate loss of body weight. ESG is a restrictive endoscopic bariatric procedure that provides a reduction of the gastric volume. This technique has provided very good results also in our recent experience. The overall mean %TBWL at 12 months of the 121 patients that were treated in our center is in accordance with other studies (Table 1).2,3,6–13 As in all endoscopic procedures, ESG is repeatable per definition and the need to perform a redo ESG should not be considered as a failure of the previous procedure, but in selected patients it can be contemplated as a second-step endoscopic treatment approach. Indications for redo ESG are the same as for the first procedure. The main reason that leads to a redo ESG is weight regain and loss of satiety feeling. Another indication to redo ESG could be the need of further weight loss in super obese patients that refuse surgery. In addition, facing the possibility to perform a redo ESG, every case should be revised by the multidisciplinary team in order to guarantee a tailored and personalized therapeutic approach. The role of the psychiatrist is essential in the multidisciplinary panorama of specialists dealing with obesity management; the most important contraindication to a redo ESG is in fact the lack of a patient’s psychological and educational compliance. Patients with dysfunctional eating habits not properly treated should first undergo a psycho-educational therapeutic course and only after should a redo ESG be considered. In our experience, only four patients needed to undertake a second procedure; three patients reported progressive loss of satiety and weight regain after the first ESG and one patient did not reach the goal in terms of weight loss due to high baseline BMI. Considering the very low rate of redo ESG performed in our experience (only 4 patients out of 121), we attribute this success to the role of the multidisciplinary team, and to the selected proper treatment strategy. These results however, are probably also influenced by the small sample (121 patients) and the short follow-up period after the primary ESG. The endoscopic technique used for the redo ESG was slightly different than that used to perform the first procedure. In our experience, the first ESG was performed by placing stitches in a traditional ‘U’ pattern between the anterior gastric wall, the great curvature, and the posterior gastric wall, while the redo ESG was performed by placing the stitches following a triangular pattern and avoiding the sutures already placed. Our case series experience, even if very limited, proved the redo ESG to be well tolerated because no peri-procedural complications were reported, and effective not only in terms of weight loss, but also in terms of the patient’s quality of life. Optimal timing between the first and the second procedure should be 6–12 months, first of all to let mucosal and submucosal tissues consolidate, but most of all to have sufficient follow-up time to evaluate the need of a second-step procedure. If also after the redo ESG the patient registers weight regaining and loss of satiety after meals, a surgical strategy needs to be considered.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: Professor Guido Costamagna is consultant for Olympus, Cook Medical and Boston Scientific. Dr. Ivo Boškoski is a research grant holder from Apollo Endosurgery and is consultant for Apollo Endosurgery, Cook Medical and Boston Scientific. Dr. Vincenzo Bove, Camilla Gallo, Valerio Pontecorvi and Lucrezia Laterza have nothing to declare.
ORCID iD: Ivo Boškoski  https://orcid.org/0000-0001-8194-2670
https://orcid.org/0000-0001-8194-2670
Contributor Information
Ivo Boškoski, Fondazione Policlinico Universitario Agostino Gemelli IRCSS, Largo A. Gemelli, 8 Rome 00168, Italy; Università Cattolica del Sacro Cuore di Roma, Center for Endoscopi Research Therapeutics and Training (CERTT), UK.
Valerio Pontecorvi, Digestive Endoscopy Unit, Fondazione Policlinico Universitario Agostino Gemelli IRCSS, Rome, Italy; Università Cattolica del Sacro Cuore di Roma, Center for Endoscopi Research Therapeutics and Training (CERTT), UK.
Camilla Gallo, Digestive Endoscopy Unit, Fondazione Policlinico Universitario Agostino Gemelli IRCSS, Rome, Italy; Università Cattolica del Sacro Cuore di Roma, Center for Endoscopi Research Therapeutics and Training (CERTT), UK.
Vincenzo Bove, Digestive Endoscopy Unit, Fondazione Policlinico Universitario Agostino Gemelli IRCSS, Rome, Italy; Università Cattolica del Sacro Cuore di Roma, Center for Endoscopi Research Therapeutics and Training (CERTT), UK.
Lucrezia Laterza, Digestive Endoscopy Unit, Fondazione Policlinico Universitario Agostino Gemelli IRCSS, Rome, Italy; Università Cattolica del Sacro Cuore di Roma, Center for Endoscopi Research Therapeutics and Training (CERTT), UK.
Guido Costamagna, Digestive Endoscopy Unit, Fondazione Policlinico Universitario Agostino Gemelli IRCSS, Rome, Italy; Università Cattolica del Sacro Cuore di Roma, Center for Endoscopi Research Therapeutics and Training (CERTT), UK.
References
- 1. Apovian CM. Obesity: definition, comorbidities, causes, and burden. Am J Manag Care 2016; 22(Suppl. 7): s176–s185. [PubMed] [Google Scholar]
- 2. Abu Dayyeh BK, Acosta A, Camilleri M, et al. Endoscopic sleeve gastroplasty alters gastric physiology and induces loss of body weight in obese individuals. Clin Gastroenterol Hepatol 2017; 15: 37–43. [DOI] [PubMed] [Google Scholar]
- 3. Lopez-Nava G, Galvão MP, Bautista-Castaño I, et al. Endoscopic sleeve gastroplasty for obesity treatment: two years of experience. Arq Bras Cir Dig 2017; 30: 18–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Storm AC, Abu Dayyeh BK. Endoscopic sleeve gastroplasty for obesity: defining the risk and reward after more than 1600 procedures. Gastrointest Endosc 2019; 89: 1139–1140. [DOI] [PubMed] [Google Scholar]
- 5. Sharaiha R. Endoscopic sleeve gastroplasty for obesity management. Gastroenterol Hepatol (N Y) 2019; 15: 390–392. [PMC free article] [PubMed] [Google Scholar]
- 6. Alqahtani A, Al-Darwish A, Mahmoud AE, et al. Short-term outcomes of endoscopic sleeve gastroplasty in 1000 consecutive patients. Gastrointest Endosc 2019; 89: 1132–1138. [DOI] [PubMed] [Google Scholar]
- 7. Fayad L, Adam A, Schweitzer M, et al. Endoscopic sleeve gastroplasty versus laparoscopic sleeve gastrectomy: a case-matched study. Gastrointest Endosc 2019; 89: 782–788. [DOI] [PubMed] [Google Scholar]
- 8. Lopez-Nava Breviere G, Bautista-Castano I, Fernandez-Corbelle JP, et al. Endoscopic sleeve gastroplasty (the Apollo method): a new approach to obesity management. Rev Esp Enferm Dig 2016; 108: 201–206. [DOI] [PubMed] [Google Scholar]
- 9. Lopez-Nava G, Sharaiha RZ, Vargas EJ, et al. Endoscopic sleeve gastroplasty for obesity: a multicenter study of 248 patients with 24 months follow-up. Obes Surg 2017; 27: 2649–2655. [DOI] [PubMed] [Google Scholar]
- 10. Sharaiha RZ, Kumta NA, Saumoy M, et al. Endoscopic sleeve gastroplasty significantly reduces body mass index and metabolic complications in obese patients. Clin Gastroenterol Hepatol 2017; 15: 504–510. [DOI] [PubMed] [Google Scholar]
- 11. Sartoretto A, Sui Z, Hill C, et al. Endoscopic sleeve gastroplasty (ESG) is a reproducible and effective endoscopic bariatric therapy suitable for widespread clinical adoption: a large, international multicenter study. Obes Surg 2018; 28: 1812–1821. [DOI] [PubMed] [Google Scholar]
- 12. Saumoy M, Schneider Y, Zhou XK, et al. A single-operator learning curve analysis for the endoscopic sleeve gastroplasty. Gastrointest Endosc 2018; 87: 442–447. [DOI] [PubMed] [Google Scholar]
- 13. Kumar N, Abu Dayyeh BK, Lopez-Nava Breviere G, et al. Endoscopic sutured gastroplasty: procedure evolution from first-in-man cases through current technique. Surg Endosc 2018; 32: 2159–2164. [DOI] [PMC free article] [PubMed] [Google Scholar]