Abstract
A 53-year-old female appeared with pain in the right mandible ramus, for the past 9 months, after tooth extraction. Clinical and radiological examination using conventional and advanced computerized tomography diagnostic imaging led to a provisional diagnosis of multiple complex odontomas. Complete conservative excision of the lesion was performed. The clinical diagnosis was confirmed histopathologically. Postoperative period was uneventful with no evidence of recurrence. According to an extensive literature review, this report describes the oldest patient ever diagnosed with multiple odontomas in the literature.
Keywords: Complex odontoma, hamartoma, mandible, multiple odontomas, odontogenic tumor
Introduction
Odontomas are mixed odontogenic tumors since they are composed of both epithelial and mesenchymal dental hard tissues.[1,2] Single odontomas are one of the most common odontogenic tumors and can be classified as compound or complex. Complex odontoma is a hamartoma in which enamel and dentin, and sometimes cementum and pulp, are present.[2] It is primarily diagnosed in children, adolescents, and young adults. Both compound and complex odontomas mostly occur as solitary lesions in the jaw. On the other hand, multiple odontomas (MOs) are characterized by numerous odontomas involving from one to all four quadrants of the jaws. A literature review disclosed 15 cases of MOs, of them 9 were complex. Because it is a rare pathologic entity, little is known about clinical features of MOs. This report describes a rare case of multiple complex odontoma in a 53-year-old female. This is the first report of MOs in a 53-year-old patient.
Procedure
A 53-year-old female patient presented with a noncontributory medical and dental history, and there was no significant medical history. Her chief complaint was pain in the right mandible ramus, for the past 9 months, after tooth extraction. The intraoral examination showed swelling on the buccal side of the right horizontal body of the mandible with permanent mandibular right first premolar mesially displaced. The swelling was hard on palpation, the overlying mucosa was normal, the adjacent premolar had mobility, and there was no neck lymphadenopathy.
Panoramic radiography and computerized tomography [Figures 1–3] revealed two well-defined radiopaque lesions on the right mandible's body. The posterior lesion slightly expanded the premolar and molar external and lingual mandibular wall with thinning of the lingual cortex and small disruption of the buccal cortex. The major lesion measured 31 mm × 23 mm in the larger sectional axes. The remaining path of the inferior alveolar nerve canal seemed to be below the lesion. Both lesions were intraosseous and independent. The anterior one slightly disrupts and surrounds the mental foramen. Taking into account the pathologic and radiologic presentations, a provisional diagnosis of multiple complex odontomas was made. Compound odontoma, osteoma, ameloblastic fibro-odontoma, and cemento-ossifying fibroma were considered for differential diagnosis.[1,2]
Figure 1.
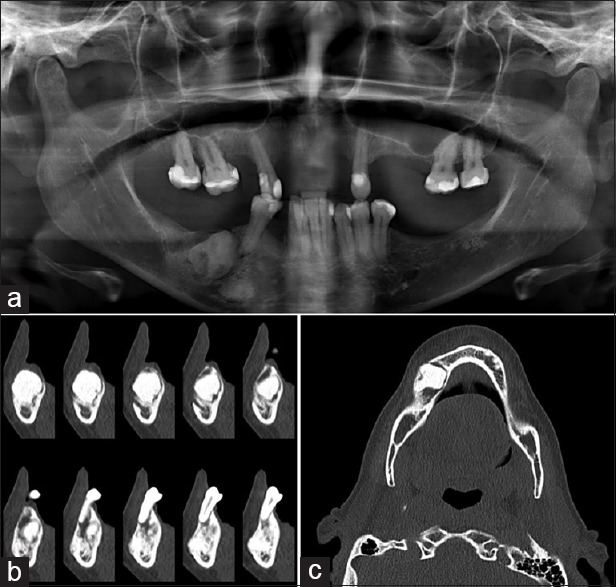
Preoperative panoramic radiograph and computerized tomography images. (a) Panoramic radiograph. (b) Coronal plane. (c) Axial plane
Figure 3.

Gross specimens excised
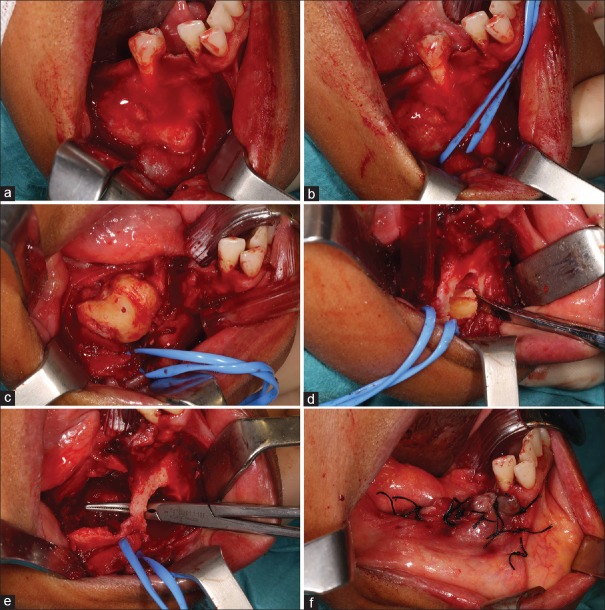
Figure 2.
Excision procedure. (a) Exposure of both lesions. (b) After nerve localization, it was wrapped with a silicon tube. (c) Excision of the posterior lesion en bloc and extraction of the second left lower premolar. (d) Separation of the anterior lesion in two portions to ease the excision. (e) After removing both lesions, it was possible to preserve a thin portion of buccal bone. (f) Sutures and final aspect
It was performed a total conservative excision procedure under general anesthesia [Figures 4 and 5]. The posterior lesion was excised en bloc. It was not possible to maintain the second left lower premolar due to the lesion extension and periodontal status. The anterior lesion was separated into two portions to enable the excision [Appendix 3]. After excision, a thorough curettage was made, and the lesions were submitted for histopathological analysis.
Figure 4.
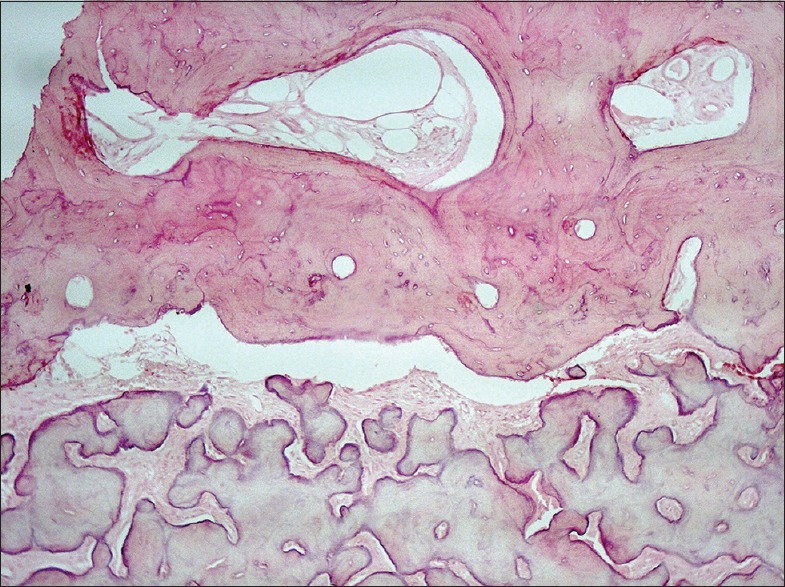
Multiple complex odontomas, microscopic findings. The core exhibits decreased cellularity, smaller fibroblastic nuclei, dispersed and amorphous dentin, dispersed enamel and cementum, and low vascularization (H and E, ×400)
Figure 5.
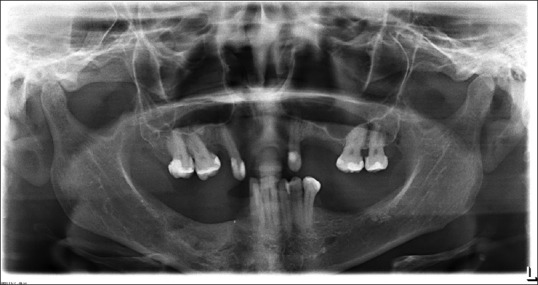
Panoramic radiograph of 14-month follow-up showing no recurrence
As a potential rare pathological entity in a 53-year-old patient, histopathological analysis was made in two independent laboratories. Both laboratories confirmed the diagnosis of complex odontoma.
No evidence of recurrence was observed at 14-month follow-up. The patient was requested to make regular follow-up visits to our hospital.
Discussion and Conclusion
In the past few years, numerous epidemiological studies were made on the prevalence of odontogenic tumors. According to the published greatest series, odontomas are one of the most common odontogenic tumors, along with ameloblastoma and keratocystic odontogenic tumor.[3,4,5,6,7] In spite of the high prevalence of odontomas, MOs are extremely rare in humans with an unknown prevalence.[8] A review of the English language literature found 15 cases of MOs [Table 1],[8,9,10,11,12,13,14,15,16,17,18,19,20] of them only 9 were complex odontomas. The cases presented by Browne,[21] Malik and Khalid,[22] and Mani[23] were not included in this analysis due to the absence of a histological diagnosis. MOs are mainly diagnosed in the first two decades, with only one case of a 42-year-old female.[16] Therefore, this rare case in a 53-year-old female patient represents the oldest patient ever diagnosed with MOs and the tenth case of multiple complex odontomas described.
Table 1.
Multiple odontomas reported in the literature
| Author (year) | Gender/age | Location | Radiographic diagnosis | Histological diagnosis | Size | Other abnormality | Treatment |
|---|---|---|---|---|---|---|---|
| Bader 1967 | Female/0-5 | 4 quadrants | Compound and complex | Confirmed | Extensive in maxilla; localized in mandible | Stenosis of esophagus | Two-staged operation |
| Schmidseder and Hausamen 1975 | Male/4 | 4 quadrants | Compound | Confirmed | Localized | Stenosis of esophagus | Two-session surgical excision |
| Melnick 1975 | Male/20 | 4 quadrants | Compound | Confirmed | Localized | No | Excision |
| Iwamoto 1999 | Female/15 | 2 quadrants (Bilateral mandible) | Compound and developing complex | Confirmed | Localized | No | Excision |
| Ajike 2000 | Female/15 | 4 quadrants | Compound | Confirmed | Extensive | No | Excision |
| Bordini 2008 | Male/17 | 4 quadrants | Compound | Confirmed | Extensive in right maxilla, localized in other 3 quadrants | No | Excision |
| Hammoudeh et al., 2009 | Female/4 | 2 quadrants (Bilateral mandible) | Complex | Confirmed | Localized | Pierre-robin syndrome | Excision |
| Maleewong et al., 2011 | Male/15 | 4 quadrants | Complex | Confirmed | Extensive | No | Excision |
| Female/19 | 4 quadrants | Complex | Confirmed | Extensive | No | Excision | |
| Srivastava 2012 | Female/42 | 2 quadrants | Complex | Confirmed | Localized | No | Excision |
| Kumazawa et al., 2014 | Female/4 | 4 quadrants | Complex and Compound | Confirmed | Extensive | No | Excision |
| Erdogan 2014 | Male/27 | 4 quadrants | Compound | Confirmed | Extensive | Mild mental retardation sight disorder, severe myopia | Partial excision |
| Guledgud et al., 2014 | Male/13 | 4 quadrants | Complex | Confirmed | Extensive | No | Excision |
| Gujjar et al., 2015 | Male/45 | 4 quadrants | Compound | Confirmed | Localized | No | Excision |
| Liu et al., 2017 | Female/9 | 1 quadrant (left mandible) | Complex | Confirmed | Localized | Otodental syndrome | Excision |
| Botelho et al., 2018 | Female/53 | 1 quadrant (right mandible) | Complex | Confirmed | Localized | No | Excision |
In general, odontomas are asymptomatic, although they can appear in any age they are primarily found in the second decade, and they are not gender related.[24] The most prevalent symptoms are impaction of permanent tooth, swelling of the jaw, and adjacent teeth displacement. Pain and tooth malpositioning are not so common.[24] In this case report, the patient complained of jaw's swelling and pain that started after the extraction of the lower right first molar, 9 months before her first appointment with us.
The etiology of odontomas remains unclear. However, they have been associated with environmental (traumas, infections, or inflammation) and genetic causes (cleidocranial dysostosis, Gardner's syndrome, Hermann's syndrome, and Pierre–Robin syndrome).[14,25,26,27] Recently, a study suggested a possible genetic etiology for MOs since the partial duplication of chromosome 11 q13.3 may confer a gain of function of the FGF3 and FGF4 genes.[28] In this case, there was no familiar history, and she was the first known case of MOs in the family.
Radiographically, complex odontomas appear as a spherical or ovoid radiopacity with a fine radiating periphery, surrounded by a radiolucent zone, which may be broader in a developing complex odontoma. Differential diagnosis from a compound odontoma or even an osteoma may not be possible radiographically.[2]
Mandible multiple complex odontomas constitute a therapeutic challenge,[29] since, in some cases, lesions are located nearby vital anatomic structures. In this case, to prevent the injury of the mental nerve, after the detachment and lesion recognition, we localized and wrapped the nerve with a silicon tube [Figure 5]. Thus, we readily identified this structure during all surgeries, decreasing the postsurgical risks. The patient had no complication after surgery.
In conclusion, after an extensive literature review and in light of the existing information, this report describes the oldest patient ever diagnosed with MOs in the literature.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Regezi J, Sciubba J. 5th ed. St. Louis: Saunder; 2007. Oral Pathology: Clinical Pathologic Correlations. [Google Scholar]
- 2.Barnes L, Eveson JW, Reichart P, Sidransky D. WHO Press; 2005. Pathology and Genetics of Head and Neck Tumours: World Health Organization Classification Tumour: 163. [Google Scholar]
- 3.Buchner A, Merrell PW, Carpenter WM. Relative frequency of central odontogenic tumors: A study of 1,088 cases from Northern California and comparison to studies from other parts of the world. J Oral Maxillofac Surg. 2006;64:1343. doi: 10.1016/j.joms.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 4.Jing W, Xuan M, Lin Y, Wu L, Liu L, Zheng X, et al. Odontogenic tumours: A retrospective study of 1642 cases in a Chinese population. Int J Oral Maxillofac Surg. 2007;36:20–5. doi: 10.1016/j.ijom.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 5.Luo HY, Li TJ. Odontogenic tumors: A study of 1309 cases in a Chinese population. Oral Oncol. 2009;45:706–11. doi: 10.1016/j.oraloncology.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Avelar RL, Primo BT, Pinheiro-Nogueira CB, Studart-Soares EC, de Oliveira RB, Romulo de Medeiros J, et al. Worldwide incidence of odontogenic tumors. J Craniofac Surg. 2011;22:2118–23. doi: 10.1097/SCS.0b013e3182323cc7. [DOI] [PubMed] [Google Scholar]
- 7.Siriwardena BS, Tennakoon TM, Tilakaratne WM. Relative frequency of odontogenic tumors in Sri Lanka: Analysis of 1677 cases. Pathol Res Pract. 2012;208:225–30. doi: 10.1016/j.prp.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 8.Bordini J, Jr, Contar CM, Sarot JR, Fernandes A, Machado MA. Multiple compound odontomas in the jaw: Case report and analysis of the literature. J Oral Maxillofac Surg. 2008;66:2617–20. doi: 10.1016/j.joms.2007.08.027. [DOI] [PubMed] [Google Scholar]
- 9.Bader G. Odontomatosis. Oral Pathol. 1967;23:770. doi: 10.1016/0030-4220(67)90368-4. [DOI] [PubMed] [Google Scholar]
- 10.Schmidseder R, Hausamen JE. Multiple odontogenic tumors and other anomalies. An autosomal dominantly inherited syndrome. Oral Surg Oral Med Oral Pathol. 1975;39:249–58. doi: 10.1016/0030-4220(75)90226-1. [DOI] [PubMed] [Google Scholar]
- 11.Melnick M. Odontomatosis. Oral Surg Oral Med Oral Pathol Oral Radiol. 1975;40:163. doi: 10.1016/0030-4220(75)90362-x. [DOI] [PubMed] [Google Scholar]
- 12.Iwamoto O, Harada H, Kusukawa J, Kameyama T. Multiple odontomas of the mandible: A case report. J Oral Maxillofac Surg. 1999;57:338–41. doi: 10.1016/s0278-2391(99)90685-7. [DOI] [PubMed] [Google Scholar]
- 13.Ajike SO, Adekeye EO. Multiple odontomas in the facial bones. Int J Oral Maxillofac Surg. 2000;29:443. [PubMed] [Google Scholar]
- 14.Hammoudeh JA, Kleiber GM, Nazarian-Mobin SS, Urata MM. Bilateral complex odontomas: A rare complication of external mandibular distraction in the neonate. J Craniofac Surg. 2009;20:973–6. doi: 10.1097/SCS.0b013e3181a2e327. [DOI] [PubMed] [Google Scholar]
- 15.Maleewong S, Ajiravudh JT, Chasiree S. Atypical four-quadrant complex odontomas: Report of two cases in siblings. Korn Kaen University Dental Journal. 2011;14:107. [Google Scholar]
- 16.Srivastava A, Annaji AG, Nyamati SB, Singh G, Shivakumar GC, Sahana S. Complex odontoma in both the jaws: A rare case report. J Orofac Res. 2012;56:60. [Google Scholar]
- 17.Kumazawa Y, Kawai T, Shirase T, Yagishita H, Yoshida K, Yosue T. Multiple calcifying lesions in the maxilla and mandible of a 4-year-old girl: Report of a rare case and literature review. Oral Radiol. 2014;30:259. [Google Scholar]
- 18.Guledgud M, Degala S, Patil K, Keshari D. Multiple extensive complex odontomas of the jaws. Int J Dent Sci Res. 2014;2:128. [Google Scholar]
- 19.Gujjar PK, Sahni P, Pereira T, Zingade J. Multiple compound odontomas in the jaws: A Rare case report. J Clin Diagn Res. 2015;9:ZD05–6. doi: 10.7860/JCDR/2015/15468.6927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu A, Wu M, Guo X, Guo H, Zhou Z, Wei K, et al. Clinical, pathological, and genetic evaluations of Chinese patient with otodental syndrome and multiple complex odontoma: Case report. Medicine (Baltimore) 2017;96:e6014. doi: 10.1097/MD.0000000000006014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Browne WG. Familial compound composite odontomes. Oral Surg Oral Med Oral Pathol. 1970;29:428–30. doi: 10.1016/0030-4220(70)90145-3. [DOI] [PubMed] [Google Scholar]
- 22.Malik S, Khalid M. Odontomatosis (Multile Odontomas) – A case report. Br J Oral Surg II. 1974;262:264. doi: 10.1016/0007-117x(74)90112-7. [DOI] [PubMed] [Google Scholar]
- 23.Mani NJ. Odontoma syndrome: Report of an unusual case with multiple multiform odontomas of both jaws. J Dent. 1974;2:149–52. doi: 10.1016/0300-5712(74)90043-8. [DOI] [PubMed] [Google Scholar]
- 24.Hidalgo-Sánchez O, Leco-Berrocal MI, Martínez-González JM. Metaanalysis of the epidemiology and clinical manifestations of odontomas. Med Oral Patol Oral Cir Bucal. 2008;13:E730–4. [PubMed] [Google Scholar]
- 25.Ferrer Ramírez MJ, Silvestre Donat FJ, Estelles Ferriol E, Grau García Moreno D, López Martínez R. Recurrent infection of a complex odontoma following eruption in the mouth. Med Oral. 2001;6:269–75. [PubMed] [Google Scholar]
- 26.Amado Cuesta S, Gargallo Albiol J, Berini Aytés L, Gay Escoda C. Review of 61 cases of odontoma. Presentation of an erupted complex odontoma. Med Oral. 2003;8:366–73. [PubMed] [Google Scholar]
- 27.Iatrou I, Vardas E, Theologie-Lygidakis N, Leventis M. A retrospective analysis of the characteristics, treatment and follow-up of 26 odontomas in Greek children. J Oral Sci. 2010;52:439–47. doi: 10.2334/josnusd.52.439. [DOI] [PubMed] [Google Scholar]
- 28.Ziebart T, Draenert FG, Galetzka D, Babaryka G, Schmidseder R, Wagner W, et al. The original family revisited after 37 years: Odontoma-dysphagia syndrome is most likely caused by a microduplication of chromosome 11q13.3, including the FGF3 and FGF4 genes. Clin Oral Investig. 2013;17:123–30. doi: 10.1007/s00784-012-0676-6. [DOI] [PubMed] [Google Scholar]
- 29.Ferreira JJ, Zagalo CM, Oliveira ML, Correia AM, Reis AR. Mandible reconstruction: History, state of the art and persistent problems. Prosthet Orthot Int. 2015;39:182–9. doi: 10.1177/0309364613520032. [DOI] [PubMed] [Google Scholar]