Abstract
Background:
Molar incisor hypomineralization (MIH) is an esthetic setback for the patient as well as for the dentist, treatment options for MIH includes minimally invasive techniques like microabrasion which has a limited literature of its effect. Furthermore, the effect of remineralizing such as casein phosphopeptide–amorphous calcium phosphate (CPP-ACP) agent on MIH-affected teeth is minimally studied.
Aim:
Comparative evaluation of the esthetic after microabrasion and microabrasion followed by Tooth Mousse Plus on hypomineralized incisors of MIH-affected patients.
Settings and Design:
The study was a randomized clinical trial.
Materials and Methods:
The study comprised Grade I MIH patients in the age strata of 7–16 years having lesions on incisors. As per inclusion criteria, 46 lesions were divided into two groups of microabrasion and microabrasion followed by CPP-amorphous calcium fluoride phosphate (ACFP). Photographs were obtained before treatment, just after treatment, and 6 months after treatment. The photographic evaluation was done using the CIE L*a*b* scoring method.
Statistical Analysis Used:
ANOVA and posthoc Tukey's test were applied to compare the difference in lightness ΔL and total color change ΔE of these two groups.
Results:
In microabrasion group, the overall change in ΔL of white tooth discoloration came −0.9 standard deviation (SD) 7.3. In microabrasion followed by CPP-ACFP group, statistically significant difference was found between both these groups with P value of P ≤ 0.001.
Conclusions:
Microabrasion followed by the remineralizing agent can improve the esthetics of white tooth discoloration with time.
Keywords: Casein phosphopeptide–amorphous calcium fluoride phosphate, microabrasion, molar incisor hypomineralization
Introduction
Molar incisor hypomineralization (MIH) is a disease as its name implies hypomineralized white or yellow demarcated opacities on permanent incisors and all or few permanent molars rendering the enamel with reduced strength, mechanical properties, and esthetics. The first case of MIH was described in Sweden as “idiopathic enamel hypomineralization” in 1987.[1]
MIH as the name suggests hypomineralization of partial or entire enamel. This qualitative defect makes enamel rough and plaque retentive, hypersensitive, with a high risk of caries development, as well as the risk of posteruption breakdown.
Correspondingly, treatment options accessible to improve esthetics of this stubborn hypomineralized discoloration are enamel microabrasion, bleaching, composite resin bonding, and prosthetic rehabilitation, depending on the graveness of the disease.[2]
One of the conservative techniques is enamel microabrasion treatment, advocated for esthetic rehabilitation of enamel discolorations limited to its outer layer.[3] Techniques most widely used is employing a combination of hydrochloric acid (HCL) 18% and abrasives such as pumice[4] or HCL (6.6% and 10%)[5,6] with silica carbide, or even phosphoric acid (37%) gel,[7] with pumice in equal proportions of volume.
On the contrary, nonoperative procedures are gaining attention for controlling demineralization process and simultaneously remineralizing them. Novel agents are available, namely, casein phosphopeptide-amorphous calcium phosphate (CPP-ACP), sodium–calcium–phosphosilicate, bioactive glass, SensiStat, Xylitol carrier, nanohydroxyapatite, alpha-tricalcium phosphate, and calcium sucrose phosphate.[8]
Likewise, GC Tooth Mousse, containing Recaldent CPP-ACP[9] binds to plaque, enamel crystals, localizing calcium and phosphate, and thus helping in remineralization of porosities of enamel crystals.[9,10]
Minimally invasive procedures are increasingly accepted through the advent of new techniques and materials.[11] However, there is an obvious need for extensive long-term clinical studies so that they can easily be a part of day-to-day clinical practice. Henceforth, the purpose of this research is to do a comparative evaluation of the esthetic after microabrasion and microabrasion followed by Tooth Mousse Plus on MIH-affected incisor.
Materials and Methods
The present in vivo study is a randomized controlled trial done in the Department of Pedodontics and Preventive Dentistry at H. P. Government Dental College, Shimla. The study comprised patients in the age strata of 7–16 years, attending the outpatient department. Written consent was obtained from the parents after explaining the treatment procedure. The ethical approval was obtained from the College Ethical Committee Board. In the present study, a total number of 43 lesions on incisors MIH patients as per inclusion criteria were divided into two groups, that is, microabrasion and microabrasion followed by Tooth Mousse Plus. Grade I (mild) lesions were taken in the study. Criteria for selection were established according to the European Academy of Pediatric Dentistry criteria's given in 2010.[12] Any lesion with isolated opacities, discoloration of permanent incisors, and demarcated enamel opacities without a breakdown of the enamel were included in the study. Exclusion criteria were kept as the patient having any active decay, loss of the enamel or dentin structure, clinical symptoms of irreversible pulpitis such as spontaneous pain or persisting pain, and previous use of bleaching agent.
Group A: For the microabrasion group
Teeth were entirely isolated to protect the gums from coming into contact with the acid (37% phosphoric acid). The pumice acid slurry was then applied to the teeth using cotton and rubbed with a very slow-speed rubber cup. Using a slow-speed handpiece (1000 rpm), a bristle brush cup was used to rub the pumice acid slurry for five separate applications of 10 s each. After the completion of the microabrasion technique, the enamel surfaces were polished with a cup-shaped polishing rubber and with a prophylactic paste containing fluoride to smoothen and polish the enamel surface. Standardized clinical photographs[13] were taken before the procedure (T1), immediately after the procedure (T2), and 6 months after procedure (T3) infiltration. For standardizing the photographic conditions, the camera was placed at the equidistance from the tooth. To prevent the change of refractive index by moisture, 30 s of drying was done of the lesion. Photographs were captured using a digital camera (EOS 700D camera; Canon, Tokyo, Japan), macro lens, and flash, such that photographic quality remains same [Figures 1 and 2].
Figure 1.

Photograph of before microabrasion (T1), immediately after microabrasion (T2), and 6 months after microabrasion (T3) (top to bottom)
Figure 2.

Photograph of before microabrasion (T1), immediately after microabrasion (T2), and 6 months after microabrasion (T3) (top to bottom)
Group B: For the microabrasion followed by Tooth Mousse Plus group
After microabrasion procedure same as done for Group A, Tooth Mousse Plus application was done by the patient. Microabrasion technique was followed by application of Tooth Mousse Plus® by patients over the teeth for 6 months. They were asked to leave the paste for 2–6 min at night after brushing their teeth and were also asked to spit and not to swallow or to rinse their teeth after using the cream for half an hour. Standardized clinical photographs[2] were taken before the procedure (T1), immediately after the procedure (T2), and 6 months after procedure (T3) [Figures 3 and 4].
Figure 3.

Photograph of before microabrasion (T1), immediately after microabrasion (T2), and 6 months after microabrasion (T3) (top to bottom)
Figure 4.

Photograph of before microabrasion (T1), immediately after microabrasion (T2), and 6 months after microabrasion (T3) (top to bottom)
Evaluation of color changes
The photographic evaluation was done by two trained examiners; photographs were randomly designated to bypass measuring bias. Subsequently, the white tooth discolorations were outlined on the screen and the colors of white tooth discolorations at three points (at the center, at the periphery, and one between these two points on the lesion) were taken to obtain an average scoring and was measured using color space CIELAB method (Commission Internationale de l’E’ clairage) [Figure 5].[14]
Figure 5.
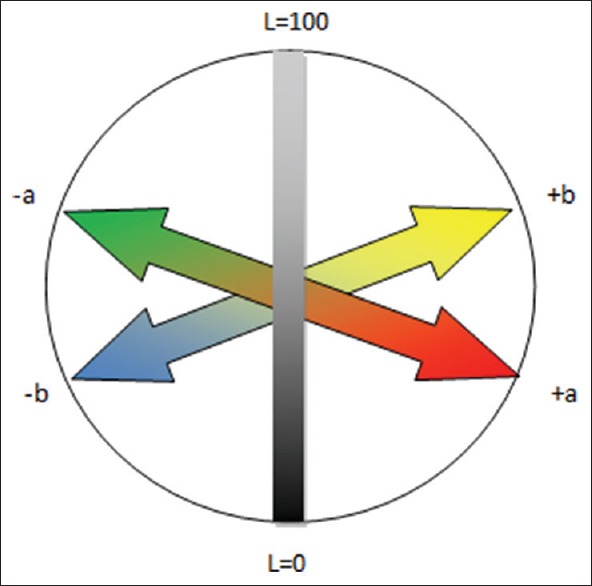
Illustrating the CIELAB color in three-dimensional color space with three axes, that is, L*, a*, and b* where L* = lightness of an object; L* 0 = perfect black; and L* value of 100 = perfect reflecting diffuser. Positive a* = redness; negative a* = greenness; positive b* = yellowness; negative b* = blueness
The CIELAB color space resembles a uniform color space, with equal distances analogous to equal perceived color differences. These three axes are L*, a*, and b*. The L* value is a measure of the lightness of an object and is measured such that a total black represents L* value of zero and a total reflecting diffuser represents L* value of 100. The a* value stands for redness (positive a*) or greenness (negative a*). The b* value stands for yellowness (positive b*) or blueness (negative b*).[15] Data were extracted from photographs. From T1 photograph for every group, three readings were obtained as L1, a1, and b1. Similarly, From T2 photograph for every group, three readings were obtained as L2, a2, and b2 and from T3 photograph for every group, three readings were obtained as L3, a3, and b3. Changes in the reading of L*, a*, and b* were calculated between every time point, to obtain ΔL, Δa, and Δb. The difference in total color, ΔE, given by the Euclidean distance in CIELAB space, can be obtained by the following equation ΔE = (ΔL*2 + Δa*2 + Δb*2)½.[16] Means of each parameter such as ΔL, Δa, Δb, and ΔE values taken from photographs of white tooth discoloration at every time points for each group were calculated, and ANOVA in conjunction with Tukey's post hoc test was used to calculate the means, that are significantly different from each other.
Results
In Group A and B, value of the mean of difference in lightness (ΔL1) of white tooth discoloration obtained from before procedure photograph (T1) and just after procedure photograph (T2) are similar, that is, 1.4 standard deviation (SD) 0.7 and − 0.9 SD 0.5, respectively, with no statically significant difference (P = 0.45) [Table 1].
Table 1.
Specific P values obtained from Tukey’s post hoc test of mean of difference in lightness (ΔL) and total color change (ΔE) of white tooth discoloration, obtained from before treatment photograph (T1), just after treatment photograph (T2), and 6 months after treatment photograph (T3) of Group A and Group B
| Parameter compared | P value between Group A and Group B |
|---|---|
| ΔL1 | 0.45 |
| ΔL2 | <0.001* |
| ΔL3 | <0.001* |
| ΔE1 | 0.07 |
| ΔE2 | <0.001* |
| ΔE3 | <0.001* |
*Level of significance P < 0.05
In Group A, value of mean of difference in lightness (ΔL2) of white tooth discoloration between different groups obtained from just after procedure photograph (T2) and 6 months after procedure photograph (T3) came to be positive, that is, 0.9 SD 0.3, which signifies increase in lightness of white tooth discoloration from after treatment to 6 months after treatment. Whereas, in Group B, the (ΔL2) value came -7.4, SD 2.1 with a statistically significant difference between both the groups [Table 1]. This signifies decrease in lightness of white tooth discoloration more in Group B than Group A.
In Group A, the value of the mean of difference in lightness (ΔL3) of white tooth discoloration between different groups obtained from before procedure photograph (T1) and 6 months after procedure photograph (T3) came to be lowest negative, that is, −0.9 SD 7.3, which signifies the least decrease in the lightness of white tooth discoloration overall. Whereas in Group B, (ΔL2) value came -7.4, SD 6.6 with statistically significant difference between both the groups [Table 1].
In Group A and B, value of the mean of difference total color change (ΔE1) of white tooth discoloration obtained from before procedure photograph (T1) and just after procedure photograph (T2) is 5.9 SD 4.3 and 7.4 SD 4.7, respectively, with no statically significant difference (P = 0.07).
In Group B, the value of mean of difference in total color change (ΔE2) of white tooth discoloration between different groups obtained from just after procedure photograph (T2) and 6 months after procedure photograph (T3) came to be highest, that is, 10.9 SD 5.5 which signifies maximum clinically detectable change in total color of white tooth discoloration from after treatment until 6 months. In Group A, (ΔE2) value came to be 6.2, SD 5.5. A statistically significant difference was noticed [Table 1]. A significant difference between the groups was noted (P ≤ 0.001*).
In Group A, the value of the mean of difference in total color change (ΔE3) of white tooth discoloration between different groups obtained from before procedure photograph (T1) and 6 months after procedure photograph (T3) came to be lowest, that is, 8.8 SD 6.0 which signifies the least decrease in total color of white tooth discoloration overall. Whereas in Group B, value came 11.4 SD 6.2, respectively, signifying that decrease in the lightness of white tooth discoloration was highest in Group A.
Discussion
Microabrasion is an acid abrasive removal and not the dissolution of enamel stain.[5] It is a technique that was proposed as a treatment modality for esthetic results in enamel opacities; brown, orange, or yellow enamel spots; and fluorotic white streaks.[17]
The effect of microabrasion is limited to a discoloration which is no more than 100 μm deep.[18] Each application of this technique removes 10 μm of enamel surface and hence only up to a maximum of 10 applications can be done to remove the stain; however, if the stain persists after 10 application of microabrasion, the lesion must be considered to be deep for this technique to be employed.[19] In addition, Waggoner et al.[20] concluded that the preliminary 1-min application causes nearly 12 μm of enamel loss and add-on 26 μm is lost with every subsequent application.
Most commonly used acid in microabrasion is phosphoric acid and hydrochloric acid. Sheoran et al.[21] noticed no difference clinically among these techniques despite differences in their concentration. Moreover, Hoeppner et al.[18] reported that after the microabrasion with 35% phosphoric acid enamel layer was found to be more resistant to demineralization up to 4 months. Hence, in our study, we used 35% phosphoric acid with pumice for microabrasion treatment. However, 18% or 35% phosphoric acid or 6.6% HCL with abrasive resulted in rough enamel surface, and there was a reduction in microhardness.[7,22,23] Nonetheless, both above-mentioned effects of microabrasion could be reverted back by the polishing of enamel or after saliva exposure.[22,23] Hence, in this study after micro-abrasion treatment, polishing of the treated lesion was done using fluoride containing prophylactic paste.
Segura et al.[24] in his study found that microabraded enamel layer, when treated with 1% sodium fluoride, were found to be more resistant to demineralization when compared to enamel layer that was treated with fluoride alone or when microabraded alone.
Similarly, Bishara[25] in 2008 found that when fluoride in high concentration is used to treat demineralized enamel, it only remineralizes superficial layer leaving the subsurface enamel porous, and thus leaving visible white spot posing an esthetic risk in anterior teeth. Thus, he concluded that to remineralize such white spot, low concentration of calcium and fluoride ions should be used to be penetrated into subsurface enamel porosities. A systemic review has concluded that the use of fluoride and CPP-ACP in reducing white spot lesion WSL during and after orthodontic treatment is significantly efficacious. Howsoever, for minimization of WSL, CPP-ACP can be more advantageous when compared to fluoride alone.[26]
Foremostly, Ardu et al.[17] recommended in office application and a following at-home application protocol of CPP-ACP following microabrasion to gain desired esthetic results.
Reynolds[27] established that the casein phosphopeptides can stabilize and maintain calcium and phosphate ions over the enamel surface and hence helping in remineralization of the same. This stabilization product is called as CPP-ACP and can remineralize enamel at concentrations of 0.5% and 1.0% in vitro.
Cross et al.[28] in 2004 reported that CPP could also stabilize fluoride ions along with calcium and phosphate ions. They established that CPP-amorphous calcium fluoride phosphate (ACFP) had better potential for caries prevention than CPP-ACP. Similar results were observed in a study by Reynolds et al.[29] they established that fluoride alone was able to remineralize the surface layer alone, on contrary CPP-ACP or combination of these two was able to remineralize the subsurface porosities as well. Commercial products such as Tooth Mousse Plus or MI Paste Plus demonstrate above-mentioned synergistic effect as they comprise CPP-ACP along with 900 ppm fluoride.[30] Hence in our study, we included Tooth Mousse Plus GC Recaldent containing sodium fluoride 0.20% W/W 900 ppm fluoride.
Under acidic conditions, the dental plaque and tooth surface attached CCP-ACFP complexes release calcium and phosphate ions, thus maintaining a supersaturated mineral environment, which inhibits enamel demineralization and enhances remineralization. After CPP-ACP or CPP-ACFP penetrates into the voids of enamel crystals, they liberate loosely attached calcium and phosphate and fluoride ions to form hydroxyapatite or fluorhydroxyapatite.[31]
The current study seek to examine the effectiveness of microabrasion and also the effect of the mineralizing agent after microabrasion. Until now there have been no studies done to compare micro-abrasion and innovative micro-abrasion technique on MIH. The current research evaluated the results from standardized clinical photographs and image analyzing software. Only one concern is that the camera should be positioned in the same orientation and light source should be constant. Studies had proven that this method is an objective, reliable and valid technique.[32,33,34,35]
There is no specific LAB for anterior maxillary teeth as there have been many studies showing a vast range in L*, a*, and b* values. Hence, the comparison was made with baseline LAB score of every white tooth discoloration of the tooth.[16]
In this study, little reduction in the whiteness of white tooth discoloration and also a small change in total color was appreciated just after treatment, following microabrasion treatment. On the contrary, increase in the whiteness of white tooth discolorations and also a slight change in total color was observed 6 months after treatment, following microabrasion treatment.
Hence, it is clear that after microabrasion treatment, the whiteness decreased to some extent only, but it eventually increased or came near to baseline. Contrary results were observed by Murphy et al.[36] in his study. He noted that the microabrasion technique significantly reduced visible enamel WSLs with a mean reduction in lesion size of 83%. However, Murphy et al. in his study treated post orthodontic WSL. While in the present study treatment was done on MIH lesion which are usually of varying depth. Micro-abrasion exposes these lesions for remineralization but, some of these lesion were much deeper, and it doesn’t get remineralized to full extent. It was reported that microabrasion could favorably remove the stain if it is confined to an enamel layer no more than 100 μm in depth.[5,19] However, sometimes when the white spot discoloration is more in-depth than 100 μm, some stains may be left and clinically visible. The accompanying acid erosion and abrasion of enamel crystals may compact mineralized tissue inside the organic area, substituting the outer surface layer of prism-rich enamel with a highly compacted, prism-free region.[37]
Distinctively, Schmidlin et al.[38] concluded that after microabrasion of demineralized lesions luminescence and fluorescence of enamel surface decreased when compared with the untreated demineralized enamel. Unusually, microabrasion is not as likely to prevail in deeper porosities.
In the present study, small reduction in whiteness and also a slight change in total color were appreciated of white tooth discolorations just after treatment, following microabrasion treatment which was to be followed by Tooth Mousse Plus as a remineralizing agent up till 6 months.
Surprisingly, marked reduction in whiteness, and also a drastic change in total color of white tooth discolorations, was seen following microabrasion treatment which was followed by tooth mousse plus as a remineralizing agent up till 6 months bringing the desired results. This can be explained by the remineralizing effect of CPP-ACFP after microabrasion removed the hypermineralized layer exposing the subsurface porosities for remineralization.
Similar results were observed by Ardu et al.[17] they described a modified technique in which microabrasion was combined with the CPP-ACP cream for the treatment of WSLs in postorthodontic patients. In this modified technique, microabrasion reactivates superficial enamel by mechanical and chemical abrasion, increasing porosity of the enamel lesion allowing better penetration of ions required for remineralization.[39] A similar result was found by Torres et al.[40] in 2011 and Paris et al.[41] in 2013 where microabrasion could not bring lightness to the baseline values. Contrary results were observed by Pliska et al.,[42] they concluded that microabrasion treatment, with or without CPP-ACP, improved the fluorescence and thus reduced WSLs. Some of the limitations observed in the study were that the application of Tooth Mousse Plus is compliance based. Second, the effect of the microabrasion could have been compared with a different type of white tooth discolorations, that is, enamel opacities, fluorosis, postorthodontic white spot discolorations. Finally, further studies are required with longer time duration.
Conclusion
Microabrasion alone could not be considered as an option for developmental enamel defects like Grade I MIH lesions, as it increases the whiteness of the same, and may cause further demineralization
Microabrasion followed by the remineralizing agent can improve the esthetics of Grade I MIH lesions with time, which is merely not an improvement in refractive index alone, there is added remineralization of subsurface enamel crystals
Microabrasion could be followed by a remineralizing agent such as CPP-ACFP, to bring esthetic results.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Koch G, Hallonsten AL, Ludvigsson N, Hansson BO, Holst A, Ullbro C, et al. Epidemiologic study of idiopathic enamel hypomineralization in permanent teeth of swedish children. Community Dent Oral Epidemiol. 1987;15:279–85. doi: 10.1111/j.1600-0528.1987.tb00538.x. [DOI] [PubMed] [Google Scholar]
- 2.Kim S, Kim EY, Jeong TS, Kim JW. The evaluation of resin infiltration for masking labial enamel white spot lesions. Int J Paediatr Dent. 2011;21:241–8. doi: 10.1111/j.1365-263X.2011.01126.x. [DOI] [PubMed] [Google Scholar]
- 3.Sundfeld RH, Sundfeld-Neto D, Machado LS, Franco LM, Fagundes TC, Briso AL, et al. Microabrasion in tooth enamel discoloration defects: Three cases with long-term follow-ups. J Appl Oral Sci. 2014;22:347–54. doi: 10.1590/1678-775720130672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Croll TP, Cavanaugh RR. Enamel color modification by controlled hydrochloric acid-pumice abrasion. II. Further examples. Quintessence Int. 1986;17:157–64. [PubMed] [Google Scholar]
- 5.Croll TP. Enamel microabrasion: The technique. Quintessence Int. 1989;20:395–400. [PubMed] [Google Scholar]
- 6.Sundfeld RH, Rahal V, Croll TP, De Aalexandre RS, Briso AL. Enamel microabrasion followed by dental bleaching for patients after orthodontic treatment – case reports. J Esthet Restor Dent. 2007;19:71–7. doi: 10.1111/j.1708-8240.2007.00069.x. [DOI] [PubMed] [Google Scholar]
- 7.Rodrigues MC, Mondelli RF, Oliveira GU, Franco EB, Baseggio W, Wang L, et al. Minimal alterations on the enamel surface by micro-abrasion:In vitro roughness and wear assessments. J Appl Oral Sci. 2013;21:112–7. doi: 10.1590/1678-7757201302117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cai F, Shen P, Walker GD, Reynolds C, Yuan Y, Reynolds EC, et al. Remineralization of enamel subsurface lesions by chewing gum with added calcium. J Dent. 2009;37:763–8. doi: 10.1016/j.jdent.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 9.Hegde MN, Moany A. Remineralization of enamel subsurface lesions with casein phosphopeptide-amorphous calcium phosphate: A quantitative energy dispersive X-ray analysis using scanning electron microscopy: An in vitro study. J Conserv Dent. 2012;15:61–7. doi: 10.4103/0972-0707.92609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Balakrishnan A, Jonathan R, Benin P, Kuumar A. Evaluation to determine the caries remineralization potential of three dentifrices: An in vitro study. J Conserv Dent. 2013;16:375–9. doi: 10.4103/0972-0707.114347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kielbassa AM, Muller J, Gernhardt CR. Closing the gap between oral hygiene and minimally invasive dentistry: A review on the resin infiltration technique of incipient (proximal) enamel lesions. Quintessence Int. 2009;40:663–81. [PubMed] [Google Scholar]
- 12.Lygidakis NA, Wong F, Jälevik B, Vierrou AM, Alaluusua S, Espelid I, et al. Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): An EAPD policy document. Eur Arch Paediatr Dent. 2010;11:75–81. doi: 10.1007/BF03262716. [DOI] [PubMed] [Google Scholar]
- 13.Arends J, Christoffersen J. The nature of early caries lesions in enamel. J Dent Res. 1986;65:2–11. doi: 10.1177/00220345860650010201. [DOI] [PubMed] [Google Scholar]
- 14.Joiner A, Luo W. Tooth colour and whiteness: A review. J Dent. 2017;67S:S3–S10. doi: 10.1016/j.jdent.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 15.O’Brien WJ, Hemmendinger H, Boenke KM, Linger JB, Groh CL. Color distribution of three regions of extracted human teeth. Dent Mater. 1997;13:179–85. doi: 10.1016/S0109-5641(97)80121-2. [DOI] [PubMed] [Google Scholar]
- 16.Joiner A, Hopkinson I, Deng Y, Westland S. A review of tooth colour and whiteness. J Dent. 2008;36(Suppl 1):S2–7. doi: 10.1016/j.jdent.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Ardu S, Castioni NV, Benbachir N, Krejci I. Minimally invasive treatment of white spot enamel lesions. Quintessence Int. 2007;38:633–6. [PubMed] [Google Scholar]
- 18.Hoeppner MG, Mauro SJ, Alexandre RS, Sundefeld ML, Sundfeld RH. Evaluation “in situ” of tag formation in dental enamel submitted to microabrasion technique. Effect of two etching times. Acta Odontol Latinoam. 2010;23:153–7. [PubMed] [Google Scholar]
- 19.Bishara SE, Denehy GE, Goepferd SJ. A conservative postorthodontic treatment of enamel stains. Am J Orthod Dentofacial Orthop. 1987;92:2–7. doi: 10.1016/0889-5406(87)90288-5. [DOI] [PubMed] [Google Scholar]
- 20.Waggoner WF, Johnston WM, Schumann S, Schikowski E. Microabrasion of human enamel in vitro using hydrochloric acid and pumice. Pediatr Dent. 1989;11:319–23. [PubMed] [Google Scholar]
- 21.Sheoran N, Garg S, Damle SG, Dhindsa A, Opal S, Gupta S, et al. Esthetic management of developmental enamel opacities in young permanent maxillary incisors with two microabrasion techniques – A split mouth study. J Esthet Restor Dent. 2014;26:345–52. doi: 10.1111/jerd.12096. [DOI] [PubMed] [Google Scholar]
- 22.Meireles SS, Andre Dde A, Leida FL, Bocangel JS, Demarco FF. Surface roughness and enamel loss with two microabrasion techniques. J Contemp Dent Pract. 2009;10:58–65. [PubMed] [Google Scholar]
- 23.Fragoso LS, Lima DA, de Alexandre RS, Bertoldo CE, Aguiar FH, Lovadino JR, et al. Evaluation of physical properties of enamel after microabrasion, polishing, and storage in artificial saliva. Biomed Mater. 2011;6:035001. doi: 10.1088/1748-6041/6/3/035001. [DOI] [PubMed] [Google Scholar]
- 24.Segura A, Donly KJ, Wefel JS. The effects of microabrasion on demineralization inhibition of enamel surfaces. Quintessence Int. 1997;28:463–6. [PubMed] [Google Scholar]
- 25.Bishara SO. White spot lesions: Formation, prevention, and treatment. Semin Orthod. 2008;14:174–82. [Google Scholar]
- 26.Lopatiene K, Borisovaite M, Lapenaite E. Prevention and treatment of white spot lesions during and after treatment with fixed orthodontic appliances: A systematic literature review. J Oral Maxillofac Res. 2016;7:e1. doi: 10.5037/jomr.2016.7201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reynolds EC. Remineralization of enamel subsurface lesions by casein phosphopeptide-stabilized calcium phosphate solutions. J Dent Res. 1997;76:1587–95. doi: 10.1177/00220345970760091101. [DOI] [PubMed] [Google Scholar]
- 28.Cross KJ, Huq NL, Stanton DP, Sum M, Reynolds EC. NMR studies of a novel calcium, phosphate and fluoride delivery vehicle-alpha(S1)-casein(59-79) by stabilized amorphous calcium fluoride phosphate nanocomplexes. Biomaterials. 2004;25:5061–9. doi: 10.1016/j.biomaterials.2004.01.045. [DOI] [PubMed] [Google Scholar]
- 29.Reynolds EC, Cai F, Cochrane NJ, Shen P, Walker GD, Morgan MV, et al. Fluoride and casein phosphopeptide-amorphous calcium phosphate. J Dent Res. 2008;87:344–8. doi: 10.1177/154405910808700420. [DOI] [PubMed] [Google Scholar]
- 30.Gupta R, Prakash V. CPP-ACP complex as a new adjunctive agent for remineralisation: A review. Oral Health Prev Dent. 2011;9:151–65. [PubMed] [Google Scholar]
- 31.Cochrane NJ, Saranathan S, Cai F, Cross KJ, Reynolds EC. Enamel subsurface lesion remineralisation with casein phosphopeptide stabilised solutions of calcium, phosphate and fluoride. Caries Res. 2008;42:88–97. doi: 10.1159/000113161. [DOI] [PubMed] [Google Scholar]
- 32.Benson PE, Pender N, Higham SM. Enamel demineralisation assessed by computerised image analysis of clinical photographs. J Dent. 2000;28:319–26. doi: 10.1016/s0300-5712(00)00002-6. [DOI] [PubMed] [Google Scholar]
- 33.Cochran JA, Ketley CE, Sanches L, Mamai-Homata E, Oila AM, Arnadóttir IB, et al. A standardized photographic method for evaluating enamel opacities including fluorosis. Community Dent Oral Epidemiol. 2004;32(Suppl 1):19–27. doi: 10.1111/j.1600-0528.2004.00135.x. [DOI] [PubMed] [Google Scholar]
- 34.Willmot DR, Benson PE, Pender N, Brook AH. Reproducibility of quantitative measurement of white enamel demineralisation by image analysis. Caries Res. 2000;34:175–81. doi: 10.1159/000016586. [DOI] [PubMed] [Google Scholar]
- 35.Benson PE, Shah AA, Willmot DR. Measurement of white lesions surrounding orthodontic brackets: Captured slides vs. digital camera images. Angle Orthod. 2005;75:226–30. doi: 10.1043/0003-3219(2005)075<0222:MOWLSO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 36.Murphy TC, Willmot DR, Rodd HD. Management of postorthodontic demineralized white lesions with microabrasion: A quantitative assessment. Am J Orthod Dentofacial Orthop. 2007;131:27–33. doi: 10.1016/j.ajodo.2005.04.041. [DOI] [PubMed] [Google Scholar]
- 37.Donly KJ, O’Neill M, Croll TP. Enamel microabrasion: A microscopic evaluation of the “abrosion effect”. Quintessence Int. 1992;23:175–9. [PubMed] [Google Scholar]
- 38.Schmidlin PR, Zehnder M, Pasqualetti T, Imfeld T, Besek MJ. Penetration of a bonding agent into de- and remineralized enamel in vitro . J Adhes Dent. 2004;6:111–5. [PubMed] [Google Scholar]
- 39.Cochrane NJ, Cai F, Huq NL, Burrow MF, Reynolds EC. New approaches to enhanced remineralization of tooth enamel. J Dent Res. 2010;89:1187–97. doi: 10.1177/0022034510376046. [DOI] [PubMed] [Google Scholar]
- 40.Rocha Gomes Torres C, Borges AB, Torres LM, Gomes IS, de Oliveira RS. Effect of caries infiltration technique and fluoride therapy on the colour masking of white spot lesions. J Dent. 2011;39:202–7. doi: 10.1016/j.jdent.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 41.Paris S, Schwendicke F, Keltsch J, Dörfer C, Meyer-Lueckel H. Masking of white spot lesions by resin infiltration in vitro . J Dent. 2013;41(Suppl 5):e28–34. doi: 10.1016/j.jdent.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 42.Pliska BT, Warner GA, Tantbirojn D, Larson BE. Treatment of white spot lesions with ACP paste and microabrasion. Angle Orthod. 2012;82:765–9. doi: 10.2319/111611-710.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


