Abstract
Background and Purpose:
To assess the anterior (aAL) and caudal (cAL) extensions of Anterior loop (AL) of Inferior alveolar nerve (IAN) using Digital Panoramic (DP) and Cone Beam Computed Tomography (CBCT) for its presence and dimensions in various age groups, genders, right and left sides of the mandible and between dentulous and edentulous patients.
Methods:
A 1-year retrospective comparative study between DP and CBCT to assess the extensions of AL of IAN was conducted on individuals referred to a private imaging center located in Bengaluru, South India. 360 mandibular sites were examined using DP and CBCT to assess the presence and dimensions of AL.
Results:
Results showed higher frequency of AL in CBCT compared to DP. Also there was a decreasing frequency of AL with increasing age and an insignificant difference in frequency between males and females. Bilateral looping was most common, aAL was more frequent on the left side and cAL on the right of the mandible. Statistically higher frequency in dentate group compared to edentulous. A decreasing mean value with increasing age and higher mean values in CBCT than DP. No significant difference in mean values among males and females or between the dentulous and edentulous groups. Higher mean values in CBCT compared to DP on the left side of the mandible compared to the right.
Conclusion:
Choosing mental foramen as reference for termination of IAN could result in injury to AL; low sensitivity and specificity of DP compared to CBCT in assessing frequency and extent of AL underlines its inadequacy, while CBCT can be performed with comparable resolution, to accurately analyze AL.
Keywords: Anterior loop, cone-beam computed tomography, digital panoramic, implants, inferior alveolar nerve
Introduction
Anterior loop (AL) of the inferior alveolar nerve (IAN) is where the mental neurovascular bundle crosses anterior to the mental foramen (MF), then doubles back to exit the MF.[1] Consideration of this anatomic variation is important before planning surgical procedures of the anterior mandible.[2,3] Placement of dental implants, osteotomy, bone harvesting, although considered safe elective procedures, sensory disturbances have been reported as a complication in up to 31% of patients in the first 2 weeks following surgery, with 10%–15% of patients continuing to complain of sensory disturbances after 15 months.[3,4] A direct surgical trauma to the AL can result in paresthesia, anesthesia, or even disabling dysesthesia most often affecting the lip and the chin region.[5,6] With studies showing a wide range in both the frequency and mean of the AL, there exists a risk of violation of the loop. In view of these potential complications, preoperative radiographic examination is essential before surgical procedures involving the mandible.[7,8] Digital panoramic (DP) remains the most commonly used method of radiologic diagnosis for planning mandibular surgeries. In recent years, cone-beam computed tomography (CBCT) has gained an increasingly important role in dental diagnosis, primarily because of its effectiveness in any type of bone, higher resolution images, at lower radiation doses.[9,10] The present study is an attempt to assess the presence and dimensions of anterior (aAL) and caudal (cAL) extensions of the AL of IAN in various age groups, genders, right and left sides of mandible and between dentulous and edentulous patients in DP and CBCT.
Methods
This 1-year retrospective comparative study between DP and CBCT to assess the AL of IAN was conducted on individuals referred to a private imaging center located in Bengaluru, South India. These individuals were subjected to CBCT examination for reasons such as presurgical implant planning and third molar impactions. The study was conducted between July 2, 2015 and June 29, 2016. 360 mandibular sites from 180 images (90 DP and 90 CBCT images) of 90 patients above the age of 18 were obtained with demographic details. Inclusion criteria for the study were DP and CBCT images of subjects over 18 years and the exclusion criteria was – mixed dentition and/or incomplete eruption of mandibular teeth, mandibular lesions, mandibular fractures, and mandibular asymmetry as these situations may obfuscate the region of interest.
Based on age, the images were divided into three study groups (18–38, 39–58, and 59 and above) with 30 DP and 30 CBCT images in each group; 15 males and 15 females in each age group, respectively. 90 DP radiographs of patients of three different age groups were taken using Siemens Orthophos (Sirona, Bensheim, Germany) machine. The DP radiographs were recorded using the following exposure parameters - tube potential settings ranging from 64 kVp to 74 kVp, exposure times between 8.2 s and 19.0 s, tube current values between 4 mA and 7 mA. The magnification factors reported by the manufacturers were 1.2 and 1.25, respectively. The 90 CBCT images of the same patients were obtained using 3D (three-dimensional) Carestream 9300 CBCT machine with sensor type – thin film transistor, scan mode – Continuous and pulse, scanning time 12–28 s (± 10%), grayscale 16384–14 bits, voxel size (μm) 90–500, and field of view (cm) 10 × 5, 10 × 10, 17 × 13.5, tube voltage 60–90 kV, and tube current 2–15 mA. A single 360° scan was used. The sagittal, coronal, and axial sections of image were reconstructed from the projection data. Images with positional errors and artifacts were omitted. Only panoramic radiographs where the MF and canal were visible were considered in the study. All images were assessed under optimal viewing conditions with appropriate image viewing software (MicroDicom for DP images and Carestream 3D imaging software for the panoramic reconstructions of CBCT). In the toolbar for the Carestream 3D software, the nerve canal tool was used to isolate the nerve and trace up to the MF. The measurement command tool was then used to measure the aAL and cAL. Measurement tool in toolbar of MicroDicom software was used to measure the distances in DP images.
The images in each group were independently inspected by two oral radiologists with 3 years of experience in evaluation of DP and CBCT to assess the AL. aAL and cAL were measured on the panoramic images and panoramic reconstruction of CBCT images as follows: aAL: distance between the anterior border of the MF and the anterior border of AL [Figure 1] and cAL: Distance between the lower border of the MF and the lowest point of the mandibular canal. The aAL and cAL were assessed in DP [Figure 2] and CBCT [Figure 3] with regard to age, gender, sides of the mandible, and between dentulous and edentulous patients.
Figure 1.
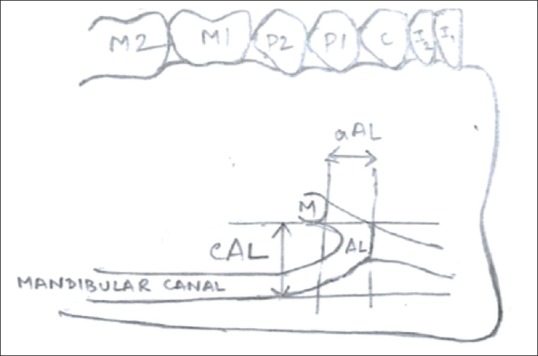
aAL: distance between anterior border of MF and the anterior border of AL; cAL: distance between lower border of MF and the lowest point of the mandibular canal
Figure 2.

Digital panoramic image showing the anterior and caudal extensions of the anterior loop of Inferior alveolar nerve on the right and left sides
Figure 3.
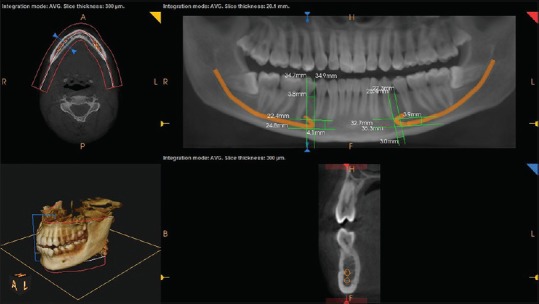
Panoramic reconstruction of cone-beam computed tomographic image, showing the anterior and caudal extensions of the anterior loop on the right and left sides of mandible. Cross-sectional view shows anterior loop identified by the presence of two separate canals
Results
Results showed a significant difference between the two imaging techniques; (P < 0.05). The test showed a statistically higher frequency of the AL (aAL and cAL) in CBCT compared to DP. Out of the 180 mandibular sites assessed by DP and CBCT, 67 sites showed AL in DP (37.2%) and 102 sites (56.67%) in CBCT. The results showed a decreasing frequency of the aAL and cAL with increase in age (Chi-square test, P < 0.05). There was no significant difference in the frequency of the AL (aAL and cAL) between males and females (Chi-square test, P > 0.05). Results showed that bilateral looping was the most common; aAL was more frequent on the left side of the mandible and the cAL on the right side of the mandible. There was statistically a higher frequency of the AL in the dentate group compared to the edentulous group in DP and CBCT imaging. P < 0.05 was found statistically significant, suggesting a decreasing mean value of aAL and cAL in both DP and CBCT with increasing age and higher mean values in CBCT compared to DP. There was a statistically insignificant difference in the mean values (P>0.05) of aAL and cAL in DP and CBCT between males and females. Kappa statistic was used to test the interobserver variability. Kappa value (κ = 1.0000) and P = 0.0001, which was statistically significant suggested a 100% agreement between the two observers.
Discussion
With a rapid increase in the use of implants to treat edentulousness, there is a corresponding increase in the need to identify important anatomical features as the AL of the IAN to avoid postoperative sensory disturbances. Various techniques have been used to assess extensions of AL from cadaveric studies, to use of radiographic techniques.[1,11,12] Large variations in frequency and measurement of aAL in literature probably are due to different definitions and methods of measurement.[13] While cadaveric studies employ surgical exposure of MF and probing the loop with Naber's probe,[14] the disadvantage is an inability to distinguish aAL and incisive canal.[13]
In periapical radiographs,[1,15] the film is highly flexible, its processing often suboptimal, with deleterious consequences to image quality. Moreover, when the MF is located at a lower position, periapical film or digital sensor cannot locate it.[16] DP can provide wide coverage of oral structures, at relatively low radiation and moderately low expense of equipment and still continues to be widely used before mandibular surgeries. Recently, CBCT has gained an increasingly important role in dental diagnosis with benefits of reduced radiation exposure compared to CT[15] at comparable resolution and accuracy and has become widely available and affordable.[2]
In literature, widely differing values are provided for the frequency of aAL. In cadaveric studies, they widely range from 0%[15] to 88%.[14] In panoramic studies, the prevalence varied from 6.25%[17] to 56%.[18] In CBCT studies, the range is 48%[19]–84%.[20] In our study using DP, out of 180 mandibular sites assessed, aAL was evident in 67 mandibular sites (37.2%) [Table 1] and coinciding with results in the literature.[17,18] The higher incidence of AL, in our study, could be due to the use of newer panoramic machines, providing higher resolution images. Using CBCT, [Table 1] out of 180 mandibular sites, aAL was evident in 102 mandibular sites (56.66%) and coincides with the results in literature.[2,19] The observations in our study have shown a relatively less frequency of the AL in DP compared to the CBCT. This can be explained by the fact that, the radiographic length of the AL can only be measured in radiographs, where the entire course of the mental canal can be visualized, from the mandibular canal to the MF.[21,22,23] Furthermore, the relatively low frequency of AL in DP could be due to the difference in the bone quality.[23,24,25] The prevalence of AL determined by DP was prominently lower in poor bone quality. One of the disadvantages of DP is the two-dimensional view of image, presence of overlapping structures, and geometric distortion of anatomic structures.[25] Distortions in the horizontal and vertical plane, especially in the anterior region, depend on the anatomical variations between arch curvatures and accurate patient positioning in the radiographic machine,[26,27] which could result in overestimation or underestimation of the AL.[22] Panoramic radiographs have shown the evident deficiencies, depending on corticalization quality of the canal wall. Anderson et al.[28] reported that as the IAN approaches the MF, the decrease in the definite bone walls of the mandibular canal can affect panoramic measurements. The relatively less frequency of AL in our study in DP compared to CBCT shows that the reliability of using DP to assess the AL may be limited. These findings also suggest the low specificity and sensitivity of DP compared to CBCT.
Table 1.
Frequency of the anterior loop of inferior alveolar nerve in digital panoramic and cone-beam computed tomography by McNemar test
| Sides | Variables | DP (%) | CBCT (%) | Mc Nemar |
|---|---|---|---|---|
| Right | aAL | 31 (34.44) | 52 (57.78) | 0.0001* |
| cAL | 32 (35.56) | 52 (57.78) | 0.0001* | |
| Left | aAL | 36 (40.00) | 50 (55.56) | 0.0001* |
| cAL | 36 (40.00) | 50 (55.56) | 0.0001* |
*P<0.05. DP: Digital panoramic; CBCT: Cone-beam computed tomography; AL: Anterior loop; aAL: Anterior AL; cAL: Caudal AL
In the current study, DP and panoramic reconstruction of the CBCT images were used to assess the cAL. The frequency of cAL in DP was 37.78%, and in the CBCT imaging, the frequency was 56.67% [Table 1]. A study by Filo et al.[2] showed a 100% occurrence of cAL, where the cAL was measured in cross-sections between the marking of the lower border of the MF in the scan with the largest vertical diameter and the cross-section with the lowest point of the mandibular canal.[2] In our study, the frequency of cAL in CBCT was 56.67% and in DP was 37.78% [Table 1]. This could be because our study was a comparison between DP and CBCT and we used panoramic reconstruction of CBCT to assess cAL. However, a point which can be suggested is that further studies using cross-sectional view could prove to be more appropriate to assess cAL.
In our study, we observed a trend toward decreasing frequency of aAL and cAL with increasing age, as the samples in the study were equally divided in each age group [Table 2]. A similar finding of a decreasing frequency of the AL with increasing age was reported by Ngeow et al.[29] This decrease in the frequency with increasing age could be a result of reduced corticalization quality of the canal wall. With an increase in age, the bone undergoes changes both quantitatively and qualitatively, with slower remodeling with an increase in age. These findings were especially appreciated in the age group above 59 years of age, which could be due to a marked increase in cortical porosity and the percentage of Haversian canals showing resorption. As a result of this resorption, the marrow space enlarges and disordered trabeculae form affecting the identification of AL. This may explain the decreased frequency of the AL with an increase in age, as the bony canal walls are likely to have become radiolucent.[30,31]
Table 2.
Comparison of frequency of anterior loop of inferior alveolar nerve between different age groups in digital panoramic and cone-beam computed tomography by Chi-square test
| Methods | Sides | Variables | 18-38 (%) | 39-58 (%) | 59+ (%) | Total (%) | χ2 | P |
|---|---|---|---|---|---|---|---|---|
| Digital panoramic | Right | aAL | 15 (50.00) | 10 (33.33) | 6 (20.00) | 31 (34.44) | 6.0030 | 0.0500* |
| cAL | 16 (53.33) | 10 (33.33) | 6 (20.00) | 32 (35.56) | 7.3710 | 0.0250* | ||
| Left | aAL | 17 (56.67) | 13 (43.33) | 6 (20.00) | 36 (40.00) | 8.6110 | 0.0130* | |
| cAL | 17 (56.67) | 13 (43.33) | 6 (20.00) | 36 (40.00) | 8.6110 | 0.0130* | ||
| CBCT | Right | aAL | 23 (76.67) | 13 (43.33) | 16 (53.33) | 52 (57.78) | 7.1960 | 0.0270* |
| cAL | 23 (76.67) | 13 (43.33) | 16 (53.33) | 52 (57.78) | 7.1960 | 0.0270* | ||
| Left | aAL | 24 (80.00) | 16 (53.33) | 10 (33.33) | 50 (55.56) | 13.3200 | 0.0010* | |
| cAL | 24 (80.00) | 16 (53.33) | 10 (33.33) | 50 (55.56) | 13.3200 | 0.0010* |
*P<0.05. CBCT: Cone-beam computed tomography; AL: Anterior loop; aAL: Anterior AL; cAL: Caudal AL
In our study, we could not assess any gender influence on the frequency of aAL and cAL in DP and CBCT [Table 3] similar to findings in literature.[2] These findings suggest that the AL has no importance in sexual dimorphism.
Table 3.
Comparison of frequency of anterior loop of inferior alveolar nerve between genders in digital panoramic and cone-beam computed tomography by Chi-square test
| Methods | Sides | Variables | Male (%) | Female (%) | Total (%) | χ2 | P |
|---|---|---|---|---|---|---|---|
| Digital panoramic | Right | aAL | 18 (40.00) | 13 (28.89) | 31 (34.44) | 1.2300 | 0.2670 |
| cAL | 18 (40.00) | 14 (31.11) | 32 (35.56) | 0.7760 | 0.3780 | ||
| Left | aAL | 21 (46.67) | 15 (33.33) | 36 (40.00) | 1.6670 | 0.1970 | |
| cAL | 21 (46.67) | 15 (33.33) | 36 (40.00) | 1.6670 | 0.1970 | ||
| CBCT | Right | aAL | 28 (62.22) | 24 (53.33) | 52 (57.78) | 0.7290 | 0.3930 |
| cAL | 28 (62.22) | 24 (53.33) | 52 (57.78) | 0.7290 | 0.3930 | ||
| Left | aAL | 31 (68.89) | 19 (42.22) | 50 (55.56) | 6.4800 | 0.0110* | |
| cAL | 31 (68.89) | 19 (42.22) | 50 (55.56) | 6.4800 | 0.0110* |
*P<0.05. CBCT: Cone-beam computed tomography; AL: Anterior loop; aAL: Anterior AL; cAL: Caudal AL
The results of our study showed statistically significant difference in AL by mandibular side, consistent with findings in the literature.[19] The study found that bilateral looping was the most common similar to the results in relevant works.[7,32] aAL was more frequent on the left side of the mandible coinciding with literature[32] and the cAL on the right side of the mandible. A higher frequency of aAL was evident on the left side of mandible in DP, compared to CBCT. This finding could suggest the assessing of the AL by DP could result in false-positive results and an overestimation of AL. These findings suggest the low specificity of the DP compared to CBCT. Although false-positive and false-negative results have been reported in the use of DP,[9,10] an overestimation of the AL by false-positive result could result in the surgeon unable to use the maximum available interforaminal area.
The AL of the IAN was assessed in dentate and edentate patients. Images of partially edentulous patients were of those who were edentulous in the region of the premolar. As this region of the mandible is associated with the presence of MF. Several studies have located the MF in the horizontal plane, usually by the apex of the second mandibular premolar or between the apices of the premolars.[14,33,34] In our study, we found a frequency of the AL in edentate group was 11.11% in DP and 19.44% in CBCT, respectively, which was lesser than the frequency in the dentate group who had a frequency of 26.11% and 37.22% in DP and CBCT, respectively, congruent with findings in literature[7,22,29] We chose to study the AL in dentate and partially or completely edentate patients as the visualization and the course of AL has known to become variable with the alveolar bone resorption that happens following the loss of teeth.[35] Resorption of the residual alveolar ridges in edentulous patients may progress to an extent that the mental canal is resorbed and the mental neurovascular bundle is exposed. Kuzmanovic et al.[22] reported that radiographic visualization of the mental canal may be adversely affected by poor bone quality in edentulous patients.
There also is a wide range in the mean values and the maximum aAL found in the literature. In cadaver studies, researchers found averages of 1.5 mm[36]–5.0 mm.[37] In panoramic studies, mean values range from 0.11[22] to 5 mm.[16] Findings of studies involving CBCT showed mean values between 0.89 mm[19] and 3.54 mm[20] and a maximum of 5.7 mm.[19] The mean value of aAL in panoramic in our study in the three age groups using DP was, 1.6 mm, 1.1 mm, and 0.4 mm, respectively, coinciding with the values of literature,[22] and using CBCT imaging, the mean values in the three age groups were 2.2 mm, 1.3 mm, and 0.9 mm, respectively. These findings in our study suggest that not only the AL of IAN has shown a decrease in frequency with increasing age as suggested by Ngeow et al.[29] but also a decrease in the mean values of the aAL with increasing age [Graph 1]. The findings in our study have shown a higher mean values of aAL in CBCT compared to DP.
Graph 1.
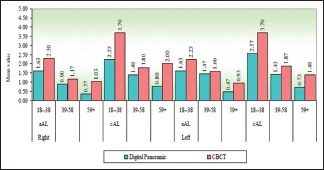
Comparison of mean scores of anterior loop in different age groups in digital panoramic and cone-beam computed tomography by Krusal–Wallis ANOVA
The cAL has shown mean values 2.4 mm, 1.4 mm, and 0.7 mm, respectively, in DP, and 3.7 mm, 1.8 mm, and 1.7 mm in CBCT in the three age groups. There is little in the literature which deals with the caudal extension of the AL. Therefore, a comparative discussion is difficult. The decrease in the mean values of cAL with an increase in age, was evident. Furthermore, our study has shown lower mean values of aAL compared to cAL in both DP and CBCT, which suggests that the AL shows a greater caudal extension compared to the anterior extension.
In our study, we could not assess any gender influence on the mean values of the AL in DP and CBCT [Graph 2].
Graph 2.
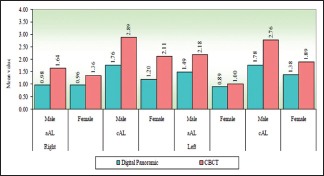
Comparison of mean scores of anterior loop among males and females in digital panoramic and cone-beam computed tomography by Mann–Whitney U test
The findings in our study suggest that the mean of the aAL is more on the left side, in both DP and CBCT, with higher mean values in CBCT compared to DP [Graph 3]. The mean of the cAL is more on the left side, in both DP and CBCT, with higher mean values in CBCT. This suggests that not only is there a higher frequency of the AL on the left side but also a higher mean values on the left side of the mandible.
Graph 3.
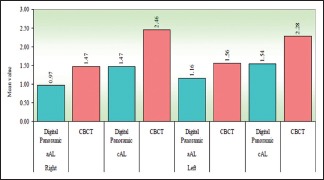
Comparison of mean scores of anterior loop on the right and left sides of the mandible in digital panoramic and cone-beam computed tomography by z-test
The results of our study showed no significant difference in the mean values of the aAL and cAL between the dentate and the edentate group.
The longest loop length in our study was 8.2 mm. The longest loop length recorded in literature was 11 mm.[14] Although various reliable safety margins have been suggested anterior to MF, for safe surgical procedures, there is always the possibility that a long AL may be encountered.
Conclusion
In conclusion to the current study, DP has shown a frequent overestimation or underestimation of AL compared to CBCT, which underlines the inadequacy of DP to form the basis for recommendations for default safety margins. While an underestimation of AL results in the risk of injuring IAN, an overestimation could result in the surgeon unable to utilize the maximum available space in the interforaminal area. The significantly higher frequency and measurement of the aAL and cAL in CBCT suggest the higher sensitivity and specificity of the imaging technique. With an exploding increase in the use of implants for replacement of teeth, it becomes more essential to identify this important anatomical feature.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bavitz JB, Harn SD, Hansen CA, Lang M. An anatomical study of mental neurovascular bundle-implant relationships. Int J Oral Maxillofac Implants. 1993;8:563–7. [PubMed] [Google Scholar]
- 2.Filo K, Schneider T, Locher MC, Kruse AL, Lübbers HT. The inferior alveolar nerve's loop at the mental foramen and its implications for surgery. J Am Dent Assoc. 2014;145:260–9. doi: 10.14219/jada.2013.34. [DOI] [PubMed] [Google Scholar]
- 3.Jacobs R, Mraiwa N, vanSteenberghe D, Gijbels F, Quirynen M. Appearance, location, course, and morphology of the mandibular incisive canal: An assessment on spiral CT scan. Dentomaxillofac Radiol. 2002;31:322–7. doi: 10.1038/sj.dmfr.4600719. [DOI] [PubMed] [Google Scholar]
- 4.Rosa MB, Sotto-Maior BS, Machado Vde C, Francischone CE. Retrospective study of the anterior loop of the inferior alveolar nerve and the incisive canal using cone beam computed tomography. Int J Oral Maxillofac Implants. 2013;28:388–92. doi: 10.11607/jomi.2648. [DOI] [PubMed] [Google Scholar]
- 5.Khan I, Halli R, Gadre P, Gadre KS. Correlation of panoramic radiographs and spiral CT scan in the preoperative assessment of intimacy of the inferior alveolar canal to impacted mandibular third molars. J Craniofac Surg. 2011;22:566–70. doi: 10.1097/SCS.0b013e3182077ac4. [DOI] [PubMed] [Google Scholar]
- 6.Worthington P. Injury to the inferior alveolar nerve during implant placement: A formula for protection of the patient and clinician. Int J Oral Maxillofac Implants. 2004;19:731–4. [PubMed] [Google Scholar]
- 7.Uchida Y, Noguchi N, Goto M, Yamashita Y, Hanihara T, Takamori H, et al. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region: A second attempt introducing cone beam computed tomography. J Oral Maxillofac Surg. 2009;67:744–50. doi: 10.1016/j.joms.2008.05.352. [DOI] [PubMed] [Google Scholar]
- 8.Kaya Y, Sencimen M, Sahin S, Okcu KM, Dogan N, Bahcecitapar M, et al. Retrospective radiographic evaluation of the anterior loop of the mental nerve: Comparison between panoramic radiography and spiral computerized tomography. Int J Oral Maxillofac Implants. 2008;23:919–25. [PubMed] [Google Scholar]
- 9.Kuribayashi A, Watanabe H, Imaizumi A, Tantanapornkul W, Katakami K, Kurabayashi T, et al. Bifid mandibular canals: Cone beam computed tomography evaluation. Dentomaxillofac Radiol. 2010;39:235–9. doi: 10.1259/dmfr/66254780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koong B. Cone beam imaging: Is this the ultimate imaging modality? Clin Oral Implants Res. 2010;21:1201–8. doi: 10.1111/j.1600-0501.2010.01996.x. [DOI] [PubMed] [Google Scholar]
- 11.Rothman SL, Chaftez N, Rhodes ML, Schwarz MS. CT in the preoperative assessment of the mandible and maxilla for endosseous implant surgery. Work in progress. Radiology. 1988;168:171–5. doi: 10.1148/radiology.168.1.3380955. [DOI] [PubMed] [Google Scholar]
- 12.Todorovic VS, Postma TC, van Zyl AW. Assessment of the anterior loop of the inferior alveolar nerve using reformatted computed tomography: A retrospective study. Br J Oral Maxillofac Surg. 2018;56:186–91. doi: 10.1016/j.bjoms.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 13.Greenstein G, Tarnow D. The mental foramen and nerve: Clinical and anatomical factors related to dental implant placement: A literature review. J Periodontol. 2006;77:1933–43. doi: 10.1902/jop.2006.060197. [DOI] [PubMed] [Google Scholar]
- 14.Neiva RF, Gapski R, Wang HL. Morphometric analysis of implant-related anatomy in Caucasian skulls. J Periodontol. 2004;75:1061–7. doi: 10.1902/jop.2004.75.8.1061. [DOI] [PubMed] [Google Scholar]
- 15.Benninger B, Miller D, Maharathi A, Carter W. Dental implant placement investigation: Is the anterior loop of the mental nerve clinically relevant? J Oral Maxillofac Surg. 2011;69:182–5. doi: 10.1016/j.joms.2010.07.060. [DOI] [PubMed] [Google Scholar]
- 16.Juodzbalys G, Wang HL, Sabalys G. Anatomy of mandibular vital structures. Part I: Mandibular canal and inferior alveolar neurovascular bundle in relation with dental implantology. J Oral Maxillofac Res. 2010;1:e2. doi: 10.5037/jomr.2010.1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vujanovic-Eskenazi A, Valero-James JM, Sánchez-Garcés MA, Gay-Escoda C. A retrospective radiographic evaluation of the anterior loop of the mental nerve: Comparison between panoramic radiography and cone beam computerized tomography. Med Oral Patol Oral Cir Bucal. 2015;20:e239–45. doi: 10.4317/medoral.20026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arzouman MJ, Otis L, Kipnis V, Levine D. Observations of the anterior loop of the inferior alveolar canal. Int J Oral Maxillofac Implants. 1993;8:295–300. [PubMed] [Google Scholar]
- 19.Apostolakis D, Brown JE. The anterior loop of the inferior alveolar nerve: Prevalence, measurement of its length and a recommendation for interforaminal implant installation based on cone beam CT imaging. Clin Oral Implants Res. 2012;23:1022–30. doi: 10.1111/j.1600-0501.2011.02261.x. [DOI] [PubMed] [Google Scholar]
- 20.Parnia F, Moslehifard E, Hafezeqoran A, Mahboub F, Mojaver-Kahnamoui H. Characteristics of anatomical landmarks in the mandibular interforaminal region: A cone-beam computed tomography study. Med Oral Patol Oral Cir Bucal. 2012;17:e420–5. doi: 10.4317/medoral.17520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.do Couto-Filho CE, de Moraes PH, Alonso MB, Haiter-Neto F, Olate S, de Albergaria-Barbosa JR, et al. Accuracy in the diagnosis of the mental nerve loop. A Comparative study between panoramic radiography and cone beam computed tomography. Int J Morphol. 2015;33:327–32. doi: 10.4067/S0717-95022015000100051. [DOI] [PubMed] [Google Scholar]
- 22.Kuzmanovic DV, Payne AG, Kieser JA, Dias GJ. Anterior loop of the mental nerve: A morphological and radiographic study. Clin Oral Implants Res. 2003;14:464–71. doi: 10.1034/j.1600-0501.2003.00869.x. [DOI] [PubMed] [Google Scholar]
- 23.Yosue T, Brooks SL. The appearance of mental foramina on panoramic radiographs. I. Evaluation of patients. Oral Surg Oral Med Oral Pathol. 1989;68:360–4. doi: 10.1016/0030-4220(89)90224-7. [DOI] [PubMed] [Google Scholar]
- 24.Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988;17:232–6. doi: 10.1016/s0901-5027(88)80047-x. [DOI] [PubMed] [Google Scholar]
- 25.Lekholm U, Zarb GA. Tissue-Integrated Prostheses: Osseointegration in Clinical Dentistry. Chicago, IL: Quintessence Publishing Co., Inc.; 1985. Patient selection and preparation; pp. 199–209. [Google Scholar]
- 26.Schiff T, D’Ambrosio J, Glass BJ, Langlais RP, McDavid WD. Common positioning and technical errors in panoramic radiography. J Am Dent Assoc. 1986;113:422–6. doi: 10.14219/jada.archive.1986.0212. [DOI] [PubMed] [Google Scholar]
- 27.Truhlar RS, Morris HF, Ochi S. A review of panoramic radiography and its potential use in implant dentistry. Implant Dent. 1993;2:122–30. doi: 10.1097/00008505-199305000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Anderson LC, Kosinski TF, Mentag PJ. A review of the intraosseous course of the nerves of the mandible. J Oral Implantol. 1991;17:394–403. [PubMed] [Google Scholar]
- 29.Ngeow WC, Dionysius DD, Ishak H, Nambiar P. A radiographic study on the visualization of the anterior loop in dentate subjects of different age groups. J Oral Sci. 2009;51:231–7. doi: 10.2334/josnusd.51.231. [DOI] [PubMed] [Google Scholar]
- 30.Yaghmaei M, Mashhadiabbas F, Shahabi S, Zafarbakhsh A, Yaghmaei S, Khojasteh A, et al. Histologic evaluation of inferior alveolar lymphatics: An anatomic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:564–7. doi: 10.1016/j.tripleo.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 31.Hu KS, Yun HS, Hur MS, Kwon HJ, Abe S, Kim HJ, et al. Branching patterns and intraosseous course of the mental nerve. J Oral Maxillofac Surg. 2007;65:2288–94. doi: 10.1016/j.joms.2007.06.658. [DOI] [PubMed] [Google Scholar]
- 32.do Nascimento EH, Dos Anjos Pontual ML, Dos Anjos Pontual A, da Cruz Perez DE, Figueiroa JN, Frazão MA, et al. Assessment of the anterior loop of the mandibular canal: A study using cone-beam computed tomography. Imaging Sci Dent. 2016;46:69–75. doi: 10.5624/isd.2016.46.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sankar DK, Bhanu SP, Susan PJ. Morphometrical and morphological study of mental foramen in dry dentulous mandibles of South Andhra population of India. Indian J Dent Res. 2011;22:542–6. doi: 10.4103/0970-9290.90290. [DOI] [PubMed] [Google Scholar]
- 34.Santini A, Alayan I. A comparative anthropometric study of the position of the mental foramen in three populations. Br Dent J. 2012;212:E7. doi: 10.1038/sj.bdj.2012.143. [DOI] [PubMed] [Google Scholar]
- 35.Kieser J, Kuzmanovic D, Payne A, Dennison J, Herbison P. Patterns of emergence of the human mental nerve. Arch Oral Biol. 2002;47:743–7. doi: 10.1016/s0003-9969(02)00067-5. [DOI] [PubMed] [Google Scholar]
- 36.Uchida Y, Yamashita Y, Goto M, Hanihara T. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region. J Oral Maxillofac Surg. 2007;65:1772–9. doi: 10.1016/j.joms.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 37.Hwang K, Lee WJ, Song YB, Chung IH. Vulnerability of the inferior alveolar nerve and mental nerve during genioplasty: An anatomic study. J Craniofac Surg. 2005;16:10–4. doi: 10.1097/00001665-200501000-00004. [DOI] [PubMed] [Google Scholar]


