SUMMARY:
Metal hardware serves as a common artifact source in spine CT imaging in the form of beam-hardening, photon starvation, and streaking. Postprocessing metal artifact reduction techniques have been developed to decrease these artifacts, which has been proved to improve visualization of soft-tissue structures and increase diagnostic confidence. However, metal artifact reduction reconstruction introduces its own novel artifacts that can mimic pathology.
Metal artifacts are an obstacle to obtaining high-fidelity CT images in postoperative spine imaging, which is increasingly problematic as the number of instrumented spinal fusions grows. There were approximately 463,200 spinal fusions in 2014 in the United States,1 a 12% increase compared with 20112 and nearly triple the amount from 1998.3 Unfortunately, up to one-third of patients experience no improvement or worsening of symptoms following surgical intervention4 and require appropriate spine imaging.4–7
The main artifacts introduced by metallic spinal implants include beam-hardening, photon starvation, and streaking,8 which diminish overall image quality and impair the identification of pathology.9,10 Metal artifact reduction (MAR; GE Healthcare, Milwaukee, Wisconsin) postprocessing techniques have been developed11 to recover image quality and detail in affected areas and to diminish the artifacts themselves.12 Unfortunately, MAR introduces different artifacts that can mimic pathology, which radiologists need to recognize.12,13 The purpose of this article was to review MAR-related artifacts seen on GE Healthcare scanners. While only 1 manufacturer is included in this article, many of the concepts are applicable to different vendor products that use similar techniques.
MAR Technique and Its Benefits
MAR is an automated postprocessing, projection-based technique developed by GE Healthcare that addresses metal artifacts in 3 stages. First, metal artifacts are identified in the source tomogram projection using a density threshold. Second, the data lost from metal artifacts are reconstructed into an inpainted projection with corrected data, which is generated by estimation from artifact-free areas. Finally, the corrected projection is formed by combining the inpainted projection and the original projection, which reveal details of structures obscured by artifacts.14,15
MAR reconstruction has been shown to significantly improve visualization of obscured soft-tissue structures and diagnostic confidence compared with the standard weighted filtered back-projection reconstruction method.12 Paraspinal soft tissues adjacent to the fusion hardware are obscured on traditional images, while the MAR image allows adequate visualization of the underlying structures (Fig 1). Despite the clear benefits of applying MAR to decrease metal artifacts, MAR introduces its own unique artifacts.
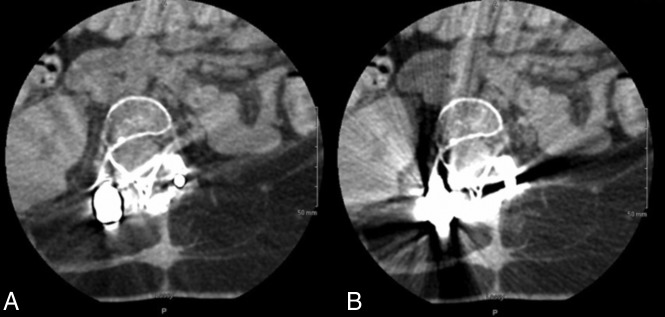
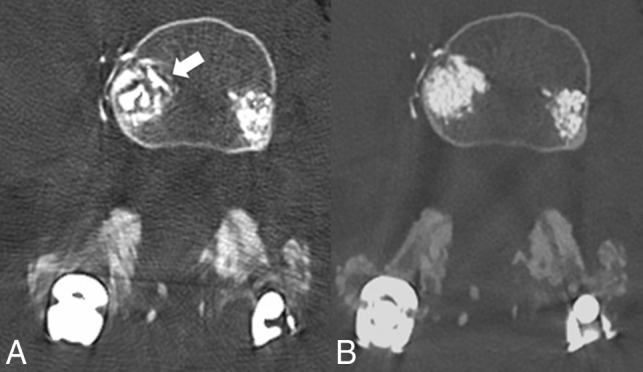
Fig 1.
Axial lumbar CT images of a 15-year-old boy with spinal muscular atrophy type II who underwent posterior spinal fusion of T2–L5 due to severe scoliosis. A, MAR images demonstrating improved visualizations of soft tissues surrounding the hardware. B, Uncorrected images show artifacts covering soft tissues surrounding the hardware.
MAR-Related Artifacts and Limitations
MAR-induced artifacts have been described in the hip and elbow,15 but there are limited descriptions of these artifacts in the spine12,16 where MAR artifacts frequently mimic pathology. The primary artifacts include the following: perihardware lucency, pedicle screw lucency, factitious subarachnoid material on myelography, and misrepresentation of intraosseous cement.
Perihardware Lucency.
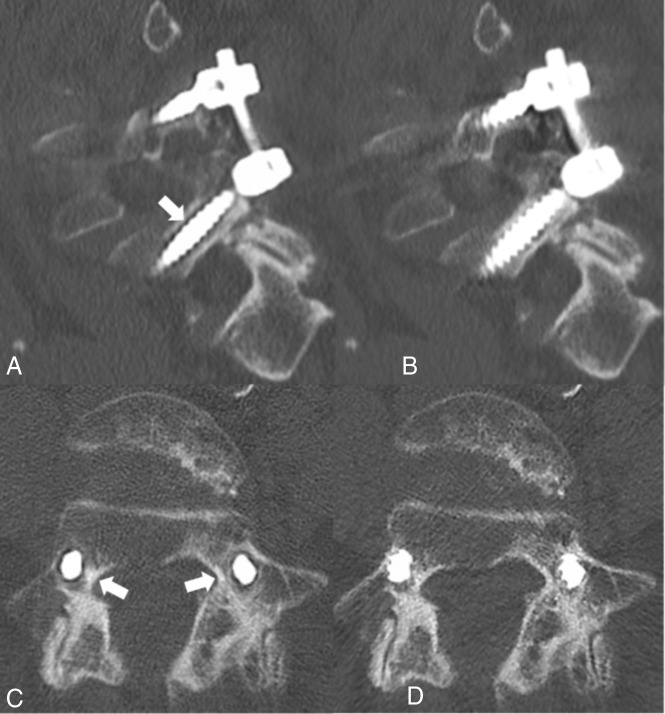
Perihardware lucency (Fig 2A, white arrow) is concerning because it usually signifies loosening of the hardware; however, this is not visualized in the non-MAR images (Fig 2B). More troublesome is that these artifacts persist in multiple planes as shown in the axial plane (Fig 2C, -D).
Fig 2.
A, Sagittal CT image of posterior lumbar spinal fusion with the MAR technique applied shows lucency surrounding the L5 pedicle screw as indicated by the white arrow. B, Image A without the MAR protocol applied, C, Axial CT image shows bilateral pedicle screws with the MAR technique applied, demonstrating lucency surrounding the bilateral pedicle screws (white arrows). If the MAR images were viewed alone, these lucencies could be mistaken for hardware loosening. D, Image C without the MAR protocol applied.
Pedicle Screw Lucency.
Pedicle screw lucency occurs when the implanted hardware fatigues and fractures (Fig 3A, white arrow), which is not seen on the non-MAR image (Fig 3B). This artifact is not uniform throughout the MAR series, and adjacent images demonstrate that adjacent screws are unaffected.
Fig 3.
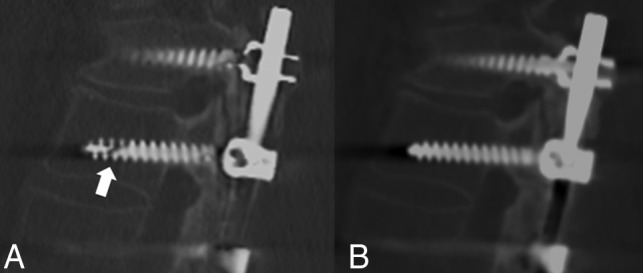
A, Sagittal CT image of posterior spinal fusion of the MAR protocol demonstrating lucency through the pedicle screw (white arrow). This lucency clearly mimics a fracture, hence could be called a “pseudofracture” if non-MAR images are not available. B, Image without the MAR application shows a normal appearance of the pedicle screw.
Subarachnoid Material on Myelography.
Factitious subarachnoid material can be seen on myelograms when MAR is applied, particularly in areas of concentrated intrathecal contrast. There is hypodense material in the dorsal spinal canal (Fig 4A, white arrow), which is not seen on the non-MAR image (Fig 4B). This artifact could be mistaken for arachnoiditis, tumor, or layering debris and may lead to unnecessary further work-up.
Fig 4.
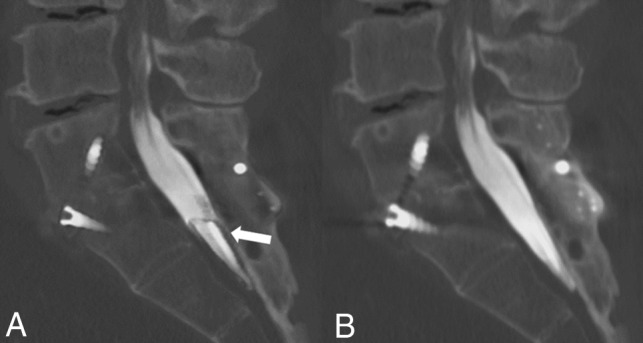
A, Sagittal MAR CT image with fusion hardware in the lumbar and sacral spine demonstrates apparent hypodense material (white arrow) in the dorsal spinal canal not seen in the non-MAR image. This filling defect could be mistaken for arachnoiditis, tumor, or layering debris and lead to unnecessary further work-up. B, Non-MAR image without evidence of material within the spinal canal.
Intraosseous Cement Abnormal Distribution.
Postvertebroplasty cement configuration can appear irregular and fragmented with indistinct margins (Fig 5A, white arrow) and an internal heterogeneous pattern of vertebral body filling; however, in the non-MAR image (Fig 5B), the bone cement has a normal uniform distribution with clearly defined margins.
Fig 5.
A, Axial CT image with MAR applied demonstrating an irregular fragmented appearance of bone cement with indistinct margins (white arrow). B, Non-MAR counterpart image with normal appearance of bone cement with accurate representation of vertebral filling.
Conclusions
MAR is a useful imaging reconstruction technique that can minimize metal artifacts, thus improving soft-tissue visualization and diagnostic confidence in the setting of spinal hardware;12 however, it is critical to understand the generated artifacts to render a correct interpretation. One limitation of this article is that we exclusively used GE Healthcare scanners. While MAR techniques of different vendors may have overlap in method (ie, projection modification is used by GE Healthcare and Philips Healthcare), each vendor ultimately has its own proprietary algorithm.17 All can potentially simulate undersampling due to oversmoothing by the MAR algorithm in areas where dense objects interface with bone, as shown in previous phantom modeling demonstrating distortion of hardware.17
At our institution, we include a set of standard images along with the MAR postprocessed images (from a single CT acquisition) on the PACS to allow confident identification of MAR artifacts and true pathology or postoperative complication. Given the widespread use of MAR techniques and the implication of misinterpreting artifacts, it is crucial that radiologists recognize these artifacts exist.
ABBREVIATION:
- MAR
metal artifact reduction
Footnotes
Disclosures: Allison M. Grayev—UNRELATED: Royalties: McGraw Hill, Comments: Author.
Paper previously presented at: Zachary Clark Radiology Research Symposium, May 4, 2019, Madison, Wisconsin; and Annual Meeting of the American Society of Neuroradiology, May 18–23, 2019, Boston, Massachusetts.
References
- 1. McDermott KW, Freeman WJ, Elixhauser A. Overview of Operating Room Procedures During Inpatient Stays in U.S. Hospitals, 2014: Statistical Brief #233. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville: Agency for Healthcare Research and Quality; 2017 [PubMed] [Google Scholar]
- 2. Weiss AJ, Elixhauser A, Andrews RM. Characteristics of Operating Room Procedures in U.S. Hospitals, 2011: Statistical Brief #170. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville: Agency for Healthcare Research and Quality; 2014 [PubMed] [Google Scholar]
- 3. Rajaee SS, Bae HW, Kanim LEA, et al. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine 2012;37:67–76 10.1097/BRS.0b013e31820cccfb [DOI] [PubMed] [Google Scholar]
- 4. Skolasky RL, Wegener ST, Maggard AM, et al. The impact of reduction of pain after lumbar spine surgery: the relationship between changes in pain and physical function and disability. Spine 2014;39:1426–32 10.1097/BRS.0000000000000428 [DOI] [PubMed] [Google Scholar]
- 5. Chan C, Peng P. Failed back surgery syndrome. Pain Med 2011;12:577–606 10.1111/j.1526-4637.2011.01089.x [DOI] [PubMed] [Google Scholar]
- 6. Young PM, Berquist TH, Bancroft LW, et al. Complications of spinal instrumentation. Radiographics 2007;27:775–89 10.1148/rg.273065055 [DOI] [PubMed] [Google Scholar]
- 7. Baber Z, Erdek MA. Failed back surgery syndrome: current perspectives. J Pain Res 2016;9:979–87 10.2147/JPR.S92776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Barrett JF, Keat N. Artifacts in CT: recognition and avoidance. Radiographics 2004;24:1679–91 10.1148/rg.246045065 [DOI] [PubMed] [Google Scholar]
- 9. Stradiotti P, Curti A, Castellazzi G, et al. Metal-related artifacts in instrumented spine: techniques for reducing artifacts in CT and MRI: state of the art. Eur Spine J 2009;18:102–08 10.1007/s00586-009-0998-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. White LM, Buckwalter KA. Technical considerations: CT and MR imaging in the postoperative orthopedic patient. Semin Musculoskelet Radiol 2002;06:5–17 10.1055/s-2002-23160 [DOI] [PubMed] [Google Scholar]
- 11. Gjesteby L, Man BD, Jin Y, et al. Metal artifact reduction in CT: where are we after four decades? IEEE Access 2016;4:5826–49 10.1109/ACCESS.2016.2608621 [DOI] [Google Scholar]
- 12. Kotsenas AL, Michalak GJ, DeLone DR, et al. CT metal artifact reduction in the spine: can an iterative reconstruction technique improve visualization? AJNR Am J Neuroradiol 2015;36:2184–90 10.3174/ajnr.A4416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhou P, Zhang C, Gao Z, et al. Evaluation of the quality of CT images acquired with smart metal artifact reduction software. Open Life Science 2018;13:155–62 10.1515/biol-2018-0021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. GE Healthcare. GE Healthcare. Smart Metal Artifact Reduction (MAR). 2013. https://www.gehealthcare.com/products/computed-tomography/radiation-therapy-planning/metal-artifact-reduction. Accessed May 30, 2019
- 15. Katsura M, Sato J, Akahane M, et al. Current and novel techniques for metal artifact reduction at CT: practical guide for radiologists. Radiographics 2018;38:450–61 10.1148/rg.2018170102 [DOI] [PubMed] [Google Scholar]
- 16. Wang Y, Qian B, Li B, et al. Metal artifacts reduction using monochromatic images from spectral CT: evaluation of pedicle screws in patients with scoliosis. Eur J Radiol 2013;82:e360–66 10.1016/j.ejrad.2013.02.024 [DOI] [PubMed] [Google Scholar]
- 17. Huang JY, Kerns JR, Nute JL, et al. An evaluation of three commercially available metal artifact reduction methods for CT imaging. Phys Med Biol 2015;60:1047–67 10.1088/0031-9155/60/3/1047 [DOI] [PMC free article] [PubMed] [Google Scholar]