Abstract
Multiple sclerosis is a chronic autoimmune disease of the central nervous system. It is the main cause of non-traumatic neurological disability in young adults. Multiple sclerosis mostly affects people aged 20–50 years; however, it can occur in young children and much older adults. Factors identified in the distribution of MS include age, gender, genetics, environment, and ethnic background. Multiple sclerosis is usually associated with progressive degrees of disability. The disease involves demyelination of axons of the central nervous system and causes brain and spinal cord neuronal loss and atrophy. Diagnosing multiple sclerosis is based on a patient’s medical history including symptoms, physical examination, and various tests such as magnetic resonance imaging, cerebrospinal fluid and blood tests, and electrophysiology. The disease course of multiple sclerosis is not well correlated with the biomarkers presently used in clinical practice. Blood-derived biomarkers that can detect and distinguish the different phenotypes in multiple sclerosis may be advantageous in personalized treatment with disease-modifying drugs and to predict response to treatment. The studies reviewed have shown that the expression levels of a large number of miRNAs in peripheral blood, serum, exosomes isolated from serum, and cerebrospinal fluid are altered in multiple sclerosis and can distinguish the disease phenotypes from each other. Further studies are warranted to independently validate these findings so that individual or pairs of miRNAs in serum or cerebrospinal fluid can be used as potential diagnostic markers for adult and pediatric multiple sclerosis and for monitoring disease progression and response to therapy.
Keywords: clinically isolated syndrome, CSF, disease progression, exosomes, humans, microRNA, multiple sclerosis, peripheral blood, phenotypes, serum
Introduction
Multiple sclerosis (MS) is a chronic autoimmune disease of the central nervous system (CNS). It is the main cause of non-traumatic neurological disability in young adults. MS mostly affects people aged 20–50 years, although it can occur in young children and much older adults. An estimated 2.5 million people in the world have MS and it is at least 2–3 times more common in women than in men. Other factors identified in the distribution of MS include age, genetics, environment, and ethnic background (Olsson et al., 2017). It is likely lifestyle factors that have changed over time and people tending to live longer with MS will have affected the rates of prevalence and incidence of MS (Multiple Sclerosis Trust, 2018; National MS Society, 2018).
MS is usually associated with progressive degrees of disability, in which chronic inflammation gives rise to multifocal demyelination of axons in both white and gray matter of the CNS (Kutzelnigg and Lassmann, 2014). The disease involves axonal degeneration and causes brain and spinal cord neuronal loss and atrophy (Geurts et al., 2012). Diagnosis of MS commonly involves finding lesions (plaques) in at least two separate areas of the CNS, including the brain, spinal cord, and optic nerves (Paul et al., 2019). However, diagnosing MS is often difficult and is based on a patient’s medical history including symptoms, physical examination, and various tests such as magnetic resonance imaging (MRI), cerebrospinal fluid (CSF) and blood tests, and electrophysiology (Katz Sand, 2015; National MS Society, 2018), and which are incorporated into the 2010 revised McDonald diagnostic criteria for MS (Polman et al., 2011). The frequency and duration of symptoms can differ between individuals, and from time to time in the same individual. These may include fatigue, tingling, pain or numbness, difficulties with balance and walking, changes in vision, depression/mood changes, impaired cognitive ability, poor muscle coordination, sexual dysfunction, slurred speech and stuttering, tremors, bladder and bowel problems. The signs of MS which may be revealed by a physical examination include irregular eye movement, changes in the way a patient talks, lack of coordination, sensory disturbances, changes in reflexes, and weakness/spasticity in arms or legs. Disability and MS severity are rated according to the Expanded Disability Status Scale (EDSS) (Kurtzke, 1983, 2015), and the Multiple Sclerosis Severity Score (MSSS) (Roxburgh et al., 2005), respectively. EDSS scores range from low (0) to high disability (10). MSSS is the decile of the EDSS within the range of patients who have had the disease for the same disease duration. It ranges from 0 to 10. At present there is no cure for MS.
Biomarkers currently used in clinical practice for diagnosing MS include glycoproteins, chemokines, IgG and IgM antibodies, and cell surface markers of inflammation (Harris et al., 2017). However, the disease course of MS is very variable and the diversity in disease phenotype is not well correlated with these biomarkers. Thus, it is imperative to identify new specific biomarkers that can aid in distinguishing the clinical phenotypes of MS, predict disease progression, and provide a correlate with disability (Housley et al., 2015; Regev et al., 2018). Due to its proximity to the CNS, the most direct source of biomarkers is CSF. However, lumbar puncture to collect CSF is an invasive procedure, requires a clinical specialist to perform it, and can lead to adverse effects. It is likely the emergence of accurate and reliable CSF biomarkers, together with the development of safe and effective intrathecal therapies, will result in CSF analysis becoming a routine part of optimal MS clinical management (Harris et al., 2017). Collections of peripheral blood are less invasive and more easily obtained than collections of CSF. Blood-derived biomarkers able to detect disease activity in MS and distinguish the different disease phenotypes may be advantageous in personalized MS treatment with disease-modifying drugs and to predict response to treatment.
MicroRNAs (miRNAs) are small, single-stranded, non-coding RNAs that repress the expression of target genes via post-transcriptional mechanisms by binding to complementary sequences in the 3′ or 5′ UTR (untranslated) region of the target messenger RNA (Lytle et al., 2007). However, more recently it has been shown that miRNAs may mediate both activation and inhibition of transcription of a target gene (Catalanotto et al., 2016). The remarkable stability of miRNAs in body fluids, together with sensitive methods for their detection and quantitation, has led to circulating miRNAs being investigated as biomarkers for various human diseases and disorders (Peplow et al., 2019), including neurodegenerative diseases and other neurologic pathologies (Sheinerman and Umansky, 2013). Increasing evidence has revealed an altered pattern of expression of miRNAs in autoimmune diseases. Further understanding of miRNA dysregulation and its mechanisms during the development of different autoimmune diseases has enormous potential to develop novel therapeutic targets or strategies, as well as identifying novel circulating or exosomal miRNA biomarkers (Long et al., 2018). Exosomes are membrane bound vesicles shed by almost all cell types and contain, amongst others, miRNAs. A significant increase in circulating exosome concentration occurs in many inflammatory diseases (Momen-Heravi et al., 2015; Lee et al., 2016). As exosomes can cross the blood-brain barrier, some of the circulating exosomes in MS patients may be derived from affected CNS cells or the associated inflammatory environment (Pusic et al., 2014).
In a review on miRNAs, Fawaz et al. (2015) wrote “Recently, recognizing the importance of biofluid biomarkers for enhancing our understanding of MS, it has been discussed their inclusion in the McDonald diagnostic criteria improves the sensitivity and specificity of diagnosis. However, the insufficient evidence of a reliable link between MS clinical course and biological markers, as well as considerable population and interlaboratory variability, and a lack of standardized procedures did not allow their inclusion at this time. Further advances in technology, development of sensitive biomarker assays and clinical validation studies are necessary”. The review listed dysregulated miRNAs in MS patients reported in research articles published in the years 2009–2013; however, for many of the miRNAs the type of samples assayed (blood, serum, plasma, specific cell types) was not indicated. We have performed a PubMed search of articles on miRNAs in blood and CSF of MS patients published in the period January 2016–December 2018 to determine to what extent they confirm and extend the findings on dysregulated miRNAs in MS, are able to distinguish between the different MS phenotypes, and meet some of the concerns expressed by Fawaz et al. (2015).
Clinical Phenotypes of Multiple Sclerosis
A first neurological event suggestive of MS usually experienced by patients is known as clinically isolated syndrome (CIS). It lasts for > 24 hours, with symptoms and signs indicating either a single lesion (monofocal) or several lesions (multifocal) within the CNS (Kappos et al., 2006). On experiencing CIS a person may or may not develop MS, with the likelihood being greater in someone who has lesions on a MRI scan similar to those seen in MS (National MS Society, 2018).
Three clinical phenotypes of MS have been recognized (Lublin and Reingold, 1996; Bayer US, 2018; National MS Society, 2018) and serve for disease staging in the progression of MS. They are:
-
1)
Relapsing-remitting MS (RRMS): About 85% of people with adult-onset MS are initially diagnosed with this condition. Individuals with RRMS have clearly defined relapses (also called attacks or exacerbations), lasting from days to weeks and then subsiding, with full or partial recovery and no apparent disease progression between attacks. True attacks must last over 24 hours, with the interval between attacks lasting at least 30 days (Kacperska et al., 2015). The relapses are caused by reactive autoimmune cells, which cause focal inflammation and demyelination often seen on MRI. As inflammation decreases and remyelination occurs, relapses are followed by periods of clinical remission. In a recent study, 52% of patients with CIS developed RRMS within a 1-year study period (Ahlbrecht et al., 2016).
-
2)
Secondary-progressive MS (SPMS): After 10–20 years of disease, > 50% of RRMS patients will transition to SPMS, characterized by relapses without any recovery. Chronic inflammation with scar formation (sclerosis), increasing axonal damage and brain atrophy, and inhibition of remyelination occurring over time cause the progressive worsening of disabilities.
-
3)
Primary-progressive MS (PPMS): In this phenotype of MS, the disease is progressive from clinical onset and occurs in ~15% of people with MS. It is characterized by slowly worsening symptoms from the beginning, without a preceding relapsing-remitting phase. It is clinically indistinguishable from SPMS.
Early-onset, juvenile or pediatric MS is defined as MS with an onset before the age of 16 years; 3–10% of MS patients present under 16 years of age and < 1% under 10 years of age (Boiko et al., 2002). The disease course in pediatric MS is different to that in adults, with 98% of pediatric MS patients presenting with a RRMS course, and less likely to develop PPMS or SPMS in childhood (Renoux et al., 2007; Alroughani and Boyko, 2018). Furthermore, the relapse rate is higher than in adult-onset MS (Benson et al., 2014).
MicroRNAs in Multiple Sclerosis and Disease Progression
Dysregulated expression of miRNAs associated with the MS phenotypes has been found previously in blood and CSF. Expression of miR-145 was upregulated while that of miR-660 and miR-939 was downregulated in plasma of MS patients (Søndergaard et al., 2013). Also, miR-22, miR-30e, miR-140-3p, miR-210, miR-500, miR-574-3p were upregulated in the plasma of RRMS patients compared to healthy controls (HC), and miR-92a-1*, miR-135a, miR-454, miR-500 and miR-574-3p were upregulated in the plasma of RPMS patients compared to SPMS patients (Gandhi et al., 2013). Furthermore, miR-15b, miR-23a, and miR-223 were downregulated in serum of both RRMS and PPMS, with no differences found between the MS phenotypes (Fenoglio et al., 2013). MiR-181c and miR-633 were upregulated whereas miR-922 was downregulated in the CSF of MS patients compared to patients with other neurologic diseases, and with miR-181c and miR-633 differentiating RRMS from SPMS patients (Haghikia et al., 2012). Earlier studies also found associations between the expression of miRNAs and MS disability or disease progression (Gandhi et al., 2013; Huang et al., 2016).
The steps involved in the review and its contents are shown (Figure 1). A total of 16 research articles were found. Thirteen of these had measured miRNAs in blood (two had used peripheral blood, one had used peripheral blood leukocytes, seven had used serum, and three had used exosomes isolated from serum) (Table 1) and three had analyzed miRNAs in CSF (Table 2). Ten of the studies utilizing blood had used qPCR to analyze/validate miRNAs, and all three of the studies with CSF had used qPCR. While most of the studies had used quite large cohorts of MS patients and HC (≥ 30/group), there were a few that had used much smaller cohorts (< 30/group). All of the studies reported on composition of the groups in terms of gender (mainly female) and age, which were similar between MS patients and HC. Diagnosis of MS was based on the 2010 revised McDonald criteria (Polman et al., 2011). The mean duration of disease from diagnosis ranged from 2.2 to 20.4 years for RRMS, from 8.0 to 20.4 years for SPMS, and from 7.6 to 16.6 years for PPMS. In addition, the mean EDSS scores, which are a measure of ambulatory disabililty, ranged from 0.5 to 6.3 for RRMS, from 4.5 to 6.6 for SPMS, and from 5.1 to 5.9 for PPMS. In some studies none of the MS patients had received disease-modifying treatment (DMT) for a considerable period of time prior to study entry, while in others, patients were receiving treatment at the time of blood sample collection. Administration of DMT medications during the course of the study may constitute a confounding factor. Eleven of the studies had used receiver operating characteristics (ROC) analysis with area under curve (AUC) values to establish which miRNAs are good or fair tests to distinguish MS and its subtypes from HC and to distinguish between the various MS subtypes. The studies were performed in several different countries, although only one study had indicated the race of the participants (Magner et al., 2016).
Figure 1.
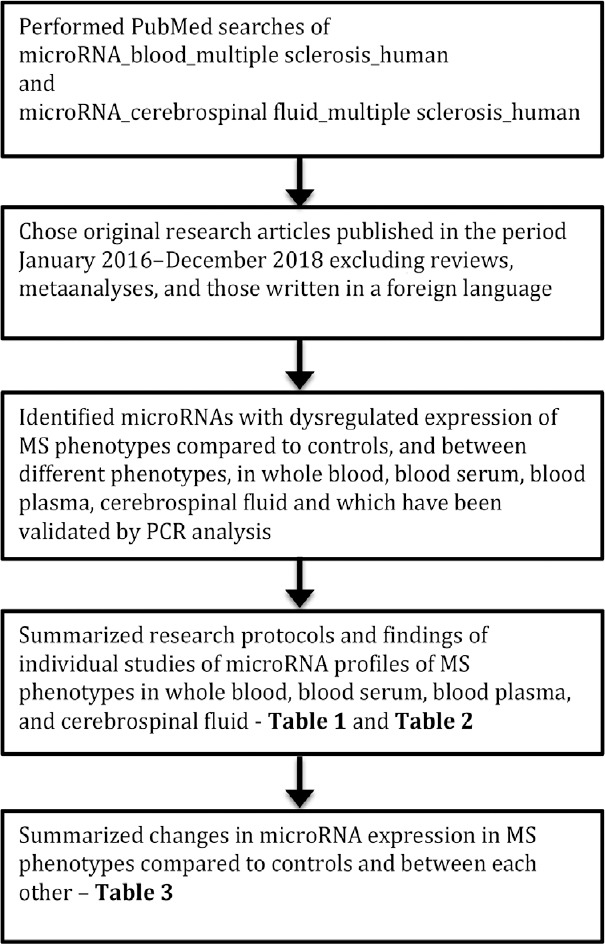
Flow diagram to show how the review was performed and its contents.
Table 1.
MicroRNAs in blood of human patients with MS
| Authors, country | Number of patients, gender, ages | Comparison | Changes in miRNAs in DR patients | Functional outcomes | Conclusion | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Peripheral blood | ||||||||||||||
| Nuzziello et al., 2018; Italy | 58 MS patients with adult onset of the disease (AOMS), 16 M/42 F, 37.8 ± 11.3 yrs, disease duration 13.4 ± 9.3 yrs, MS course 54 RR/4 SP/0 PP, EDSS 2.7 ± 1.1, DMT 56 Y/2 N. Peripheral blood samples were collected and frozen at –20oC. | 20 HC, 6 M/14 F, 43.2 ± 3.1 yrs. They were recruited among volunteers who did not show clinical signs or instrumental evidences of inflammatory or neurological diseases, and who had negative family histories for MS and other neurodegenerative diseases. | The 13 miRNAs that were differentially expressed in pediatric MS were analyzed by qPCR in the AOMS patients. Six miRNAs (miR-320a, miR-125a-5p, miR-652-3p, miR-185-5p, miR-942-5p, miR-25-3p) were significantly dysregulated in AOMS compared to HC. The qPCR analysis showed statistically significant upregulation of miR-320a (fold change, FC = 1.79), miR-125a-5p (FC = 1.89), miR-652-3p (FC = 1.51), miR-185-5p (FC = 1.5), miR-942-5p (FC = 1.67), and miR-25-3p (FC = 1.49) in AOMS compared to HC. | By ROC analysis, AUC values for the validated miRNAs ranged from 0.701 to 0.735 for miR-320a, miR-185-5p, miR-125a-5p and miR-652-3p, discriminating AOMS patients from HC and with miR-320a having the best AUC of 0.735. Using databases containing experimentally validated miRNA-target interactions (miRtarbase and DIANA-Tarbase), 155 miRNA-target pairs were validated by reporter gene assays. Several target genes (TP53, SLC4A10, CDKN1A, EKBB2, ATRX, ST6GAL2, PTEN, FAM160B1, SMAD7, IKZF4, PHLPP2, MCL1, KCNS3, NFATC3, AR, IGF1R, PCDHA4, TANC2, ZNF704, WWC2, NTRK3, NCAN, VEGFA, MSI1, LCOR, and RBM20) were shared by two of the following miRNAs: miR-125a-5p, miR-320a, miR-25-3p, and miR-185-5p. | MiR-320a, miR-125a-5p, miR-652-3p, miR-185-5p, miR-942-5p, miR-25-3p were significantly upregulated in AOMS and may be considered as circulating biomarkers of the disease. | |||||||||
| Liguori et al., 2018; Italy | 19 patients with pediatric MS (PedMS), 9 M/10 F, 15.5 ± 2.7 yrs, disease duration 2.8 ± 3.3 yrs, MS course RR, EDSS 2.7 ± 1.1, DMT 9 Y/ 10 N, education 9.6 ± 2.5 yrs, cognitive abilities 7 CI/10 CP/2 NA. Peripheral blood samples were collected and frozen at –20oC. At the time of blood sample, all treated patients were under interferon β-1 therapy. PedMS patients were analyzed during the inactive phase of a RR course of the disease (no clinical relapses or steriod assumption within 30 days of study entry, no Gd-enhancing lesions at the concomitant MRI), and were steriod-free (at least 1 mth prior to blood sample). 9 Ped MS patients had taken interferon β-1a for 21–673 days from blood sample. | 20 healthy pediatric controls (PC), 14 M/6 F, 8.8 ± 3.3 yrs, education 3.4 ± 2.6 yrs, cognitive abilities NA. | The PedMS patients and PC controls differed significantly for age at study entry, but there was no significant gender difference between them. The investigation performed using a High-Throughput Next Generation Sequencing approach was followed by an integrated bioinformatics/ biostatistics analysis. This revealed 49 mature miRNAs significantly differentially expressed between PedMS and PC. After further selection, the total was reduced to 27 miRNAs that were subjected to qRT-PCR validation. In the validation study, 12 miRNAs (let-7a-5p, let-7b-5p, miR-25-3p, miR-125a-5p, miR-942-5p, miR-221-3p, miR-652-3p, miR-182-5p, miR-185-5p, miR-181a-5p, miR-320a, miR-99b-5p) were significantly upregulated and 1 miRNA (miR-148b-3p) significantly downregulated in PedMS compared to PC. | The interactions between the validated miRNAs and their targets uncovered predicted genes related to immunological functions (i.e., TNFSF13B, TLR2, BACH2, KLF4), as well as genes involved in autophagy-related processes (i.e., ATG16L1, SORT1, LAMP2) and ATPase activity (i.e., ABCA1, GPX3). No significant molecular profiles were associated with any PedMS demographic/clinical features. Both miRNAs and mRNA expressions predicted the PedMS and PC phenotypes with an accuracy of 92% and 91%, respectively. | 12 miRNAs (let-7a-5p, let-7b-5p, miR-25-3p, miR-125a-5p, miR-942-5p, miR-221-3p, miR-652-3p, miR-182-5p, miR-185-5p, miR-181a-5p, miR-320a, miR-99b-5p) were significantly upregulated and 1 miRNA (miR-148b-3p) significantly downregulated in PedMS compared to PC. | |||||||||
| Peripheral blood leukocytes (PBL) | ||||||||||||||
| Magner et al., 2016; USA | 24 MS patients on no therapy, 2 M/22 F, 22 were Caucasians, 52 ± 11 yrs, disease course 19 RRMS/5 SPMS, disease duration 16.9 ± 11.5 yrs, EDSS 3.5 ± 1.6. All patients were evaluated clinically within 1 month of their study participation and assessed using EDSS scale. MS patient scores 1.0–4.5 and 5.0–6.5 indicate degrees of impaired ambulation. Patients with scores ≥ 7 are not ambulatory. Whole blood samples taken at 0 and 48 hours were separated over Ficoll and recovered leukocytes were lysed for total RNA. | 25 HC, 5 M/20 F, 25 were Caucasians, 50 ± 9 yrs | Untreated MS patient PBL Dicer protein levels were 40% lower than the levels found in age and gender matched HC (P = 0.049). Further analysis suggested that Dicer protein levels decreased with disease progression. Despite the significant changes in Dicer protein levels, there were no statistically significant difference in DICER1 mRNA levels between untreated MS and HC. By next generation sequencing analysis, significant differences in miRNA expression levels were found for untreated RRMS patients compared to HC: miR-484, miR-9-5p, miR-323b-3p, miR-15b-5p, miR-145-5p, miR-337-5p, miR-485-5p, miR-654-3p, miR-377-3p, miR-493-5p, miR-301b, miR-409-3p, miR-494 (all upregulated), miR-451a, miR-144-5p, miR-101-3p (all downregulated) with false discovery rates 0.0019–0.0462. The highest logFC values were for miR-337-5p (logFC = 1.58), miR-144-5p (logFC = –1.98) and miR-451a (logFC = –1.71). In untreated RRMS patients, two miRNAs (miR-146b-5p, miR-874) were negatively correlated with EDSS and two others (miR-107, miR-3614) were positively correlated. MiR-107 has been shown to target Dicer (Asirvatham et al., 2008; Martello et al., 2010). | Potential biomarkers for untreated RRMS were identified. Analysis of PBL miRNA will include miRNA expressed in each circulating cell population as well as miRNA shed from tissues, often in exosomes, that become associated with PBL. | ||||||||||
| Blood serum | ||||||||||||||
| Vistbakka et al., 2018; Finland | 53 RRMS patients, 12 M/41 F, 35.3 ± 7.1 yrs, disease duration 5.4 ± 5.4 yrs, EDSS 1.6 ± 1.7, progression index 0.21 ± 0.50; 20 PPMS patients, 10 M/10 F, 52.7 ± 8.0 yrs, disease duration 7.6 ± 6.5 yrs, EDSS 5.4 ± 1.8, progression index 0.38 ± 0.82. Diagnosis of MS was based on the revised McDonald criteria. Active DMT treatment was ongoing in 37 patients with RRMS. All patients underwent clinical and neurological examination including assessment of neurological disability expressed by EDSS score. Progression index was calculated by dividing EDSS score by disease duration from diagnosis. An average annual relapse rate (ARR) was calculated in RRMS group starting from the time of diagnosis. Prior to sampling, none of the patients had any relapses for at least 8 weeks. The mean ARR was 1.7 ± 3.4, and mean number of relapses during the last 2 yrs was 0.9 ± 1.1. Venous blood was collected and sera separated by centrifugation (1600 × g, 15 minutes, room temperature) and stored at –80oC. | 27 HC, 9 M/18 F, 38.2 ± 11.8 yrs. Healthy controls had no history of any autoimmune disease or use of any immunomodulatory therapy. | By RT-PCR, miR-24-3p and miR-191-5p were expressed in all the samples, while miR-128-3p and miR-376c-3p were expressed in 95% and 87% of the samples, respectively. Overexpression of miR-128-3p, miR-191-5p, and miR-24-3p occurred in sera of patients with MS (RRMS and PPMS) compared to HC, although after the Bonferroni correction (to reduce type-1 errors, false positives) only miR-191-5p and miR-24-3p remained statistically significant. Expression levels of miR-376c-3p did not differ between the groups. Overexpression was found of miR-191-5p (RRMS, P = 0.01, FC = 1.65; PPMS, P < 0.001, FC = 1.75) and miR-24-3p (RRMS, P = 0.01, FC = 2.10; PPMS, P = 0.01, FC = 3.58) in both subtypes and miR-128-3p in PPMS (P = 0.03, FC = 1.72) compared to HC. After the Bonferroni correction, miR-128-3p did not reach statistical significance. No statistically significant differences were found between RRMS and PPMS. Comparison between untreated and treated MS patients did not show any statistical differences in miRNA expression levels. In the male population, miR-128-3p and miR-191-5p were overexpressed in RRMS (P = 0.007, FC = 11.33 and P = 0.009, FC = 4.68), PPMS (P = 0.023, FC = 3.56 and P = 0.022, FC = 4.01) and among all patients with MS (P = 0.003, FC = 7.49 and P = 0.004, FC = 4.40) compared to HC. Also, miR-128-3p was overexpressed in RRMS compared to PPMS (P = 0.038, FC = 3.18). However, the results of PPMS to HC and PPMS to RRMS comparisons did not pass the Bonferroni correction. In the female population, miR-24-3p was overexpressed in RRMS (P = 0.020, FC = 1.78), PPMS (P = 0.011, FC = 6.06) and in all patients with MS (P = 0.007, FC = 2.62) compared to HC. The RRMS to HC comparison did not pass the Bonferroni correction. Overexpression of miR-24-3p was detected in PPMS cohort in male to female comparison (P = 0.038, FC = 8.17) but it did not pass the Bonferroni correction. | In the whole MS group, miR-24-3p showed positive correlation with the progression index, and after adjustment for gender, disease subtype, and age, this correlation was preserved. In the RRMS group, miR-128-3p showed positive correlation with ARR, and this became stronger after adjustment for gender and age. In the PPMS group, miR-376c-3p tended to correlate positively with EDSS, but was not preserved after gender and age adjustment. | In MS, serum miR-24-3p and miR-128-3p showed a tendency of association with disability and disease activity, respectively. | |||||||||
| Regev et al., 2018; USA (CLIMB, EPIC) Lebanon (AMIR) Sweden (STOPMS II) | CLIMB cohort: 24 RRMS patients, 5 M/19 F, 32.4 ± 6.6 yrs, disease duration 3.9 ± 2.4 yrs, EDSS 0.6 ± 0.9; 18 SPMS patients, 3 M/15 F, 56.4 ± 9.3 yrs, disease duration 17.2 ± 5.9 yrs, EDSS 5.5 ± 1.6. AMIR cohort: 31 RRMS patients, 10 M/21 F, 33.5 ± 10.2 yrs, disease duration 4.6 ± 4.7 yrs, EDSS 2.1 ± 1.2; 5 SPMS patients, 3 M/2 F, 40.2 ± 7.8 yrs, disease duration 15.2 ± 11.0 yrs, EDSS 4.5 ± 1.4. EPIC cohort: 27 RRMS patients, 7 M/20 F, 37.6 ± 6.8 yrs, disease duration 3.9 ± 2.4 yrs, EDSS 1.0 ± 0.8; 7 SPMS patients 0 M/7 F, 52.7 ± 5.8 yrs, disease duration 19.0 ± 6.0 yrs, EDSS 5.1 ± 1.3. STOPMS II cohort: 33 RRMS patients, 10 M/23 F, 33.1 ± 9.4 yrs, disease duration 2.2 ± 3.4 yrs, EDSS 1.7 ± 1.7; 21 SPMS patients, 10 M/11 F, 43.2 ± 4.3 yrs, disease duration 19.6 ± 5.2 yrs, EDSS 5.3 ± 1.5. None of the selected patients were receiving DMT at the time of sample collection. Blood samples were collected in tubes without additives and kept at room temperature for 30–60 minutes. Each sample was centrifuged (2000 r/min, 10 minutes) to separate the serum and then stored at –70oC. | CLIMB cohort: 30 healthy controls (HC), 5 M/25 F, 45.4 ± 15.0 yrs; AMIR cohort: 19 HC, 7 M/12 F, 37.6 ± 11.2 yrs; EPIC cohort: 26 HC, 14 M/12 F, 45.5 ± 10.2 yrs; STOPMS II cohort: 13 HC, 7 M/6 F, 30.9 ± 5.6 yrs. | In the reproducibility phase 73 miRNAs showing promise as biomarkers from a larger validation set of participants from CLIMB patients (validation phase) were further analysed by RT-PCR with MS group (24 RRMS, 18 SPMS) and 30 HC from the CLIMB cohort. Five previously validated miRNAs viz. miR-484, miR-320a, miR-320c, miR-486-5p (all increased) and miR-140-5p (decreased) showed a significant difference, and 1 miRNA remained significant after accounting for multiple comparisons to control for false discovery rate (miR-484). In a comparison between RRMS and HC, only miR-484 showed a significant difference after accounting for multiple comparisons. When SPMS and HC were compared, 8 miRNAs were significantly different, and 6 miRNAs (mR-484, miR-140-5p, miR-142-5p, miR-320a, miR-320b, miR-320c) were significantly different after accounting for multiple comparisons. When RRMS and SPMS were compared, no previously validated miRNAs were significantly different between the groups. Four miRNAs, miR-320b, miR-337-3p, miR-199a-5p, and miR-142-5p, were significantly correlated with EDSS in the reproducibility phase cohort. In the transportability phase the 73 miRNAs were further analysed in 3 external cohorts with study participants from 3 MS centers worldwide with 91 RRMS, 33 SPMS and 58 HC. For the comparison of MS and HC, 4 miRNAs were differentially expressed in 2 of the 4 MS cohorts: let-7e-5p, let-7f-5p, miR-486-5p, miR-30e-5p. For the comparison of RRMS and HC, 2 miRNAs were differentially expressed in 2 of the 4 MS cohorts: let-7e-5p and let-7f-5p. For the comparison of SPMS and HC, miR-320a, miR-320b, miR-320c and miR-486-5p were differentially expressed in the CLIMB and STORMS II cohorts. The expression of miR-337-3p negatively correlated with EDSS in the discovery set (n = 85) and validation phase (n = 58). These findings were further tested in samples from the reproducibility phase and transportability phase. Results showed that miR-337-3p was negatively correlated with EDSS in 3 of 4 cohorts. An additional 5 miRNAs (miR-142-5p, miR-199a-5p, miR-330-3p, miR-194-5p, miR-941) showed a significant correlation in 2 of the cohorts. In the CLIMB cohort, SPMS patients have significantly decreased miR-337-3p expression compared to RRMS patients. Comparisons between SPMS and RRMS in the other 3 cohorts showed a similar reduction in miR-337-3p expression in SPMS patients compared to RRMS patients in 3 of the 4 cohorts. | Including let-7c-5p, miR-452-5p and miR-484 in a predictive model for MS vs. HC gave by ROC analysis an AUC value of 0.85 in the validation cohort. | When comparing RRMS with HC, miR-484 was significantly different between the groups after accounting for multiple group comparisons. When SPMS and HC were compared, mR-484, miR-140-5p, miR-142-5p, miR-320a, miR-320b, miR-320c remained significantly different after accounting for multiple group comparisons. In disability correlation analysis, miR-320a, miR-337-3p, miR-199a-5p, and miR-142-5p correlated with the EDSS in the reproducibility phase cohort. SPMS patients had significantly decreased miR-337-3p expression compared to RRMS patients in 3 of the 4 cohorts. | |||||||||
| Wang et al., 2017; China | 30 RRMS patients at relapse, 10 M/20 F, 31.1 ± 13.4 yrs, smoking status 6 Ever/current/24 Never, alcohol consumption 6 Ever/current/24 Never, EDSS 2.8 ± 1.6. Regarding inclusion criteria: clinical diagnoses were confirmed using the 2010 revisions to McDonald diagnostic criteria, all participants were on periods of relapse and Epstein-Barr virus (EBV)-immnoglobulin (Ig)G-positive but EBV-IgM-negative. Regarding exclusion criteria, PPMS and PedMS cases were excluded, patients who met the diagnostic criteria of other systemic autoimmune diseases involving CNS demyelination were excluded, patients who received treatment within the previous 60 days were excluded. Venous blood was collected with no anti-coagulant prior to therapy, allowed to stand for 20 min, centrifuged (1500 × g, 10 minutes, 20oC). Sera was collected and stored at –80oC for analysis. | 30 HC, 10 M/20 F, 34.4 ± 9.4 yrs, smoking status 8 Ever/current/ 22 Never, alcohol consumption 4Ever/current/26Never, EDSS NA. | By qRT-PCR assay, 20 EBV miRNAs were expressed robustly and detectable in all samples. Expression of ebv-miR-BHRF1-2-5p and ebv-miR-BHRF1-3 was significantly increased in RRMS patients compared to HC (FC = 1.48 and 1.33, respectively), while the other 18 miRNAs showed no significant difference. The upregulated expression of ebv-miR-BHRF1-2-5p and ebv-miR-BHRF1-3 was associated positively with EDSS scores of RRMS patients | By ROC analysis, the AUC values for ebv-miR-BHRF1-2-5p and ebv-miR-BHRF1-3 used independently were 0.74 and 0.72, respectively. With a combination of the two miRNAs, the AUC value was 0.76. Among the candidate target genes of ebv-miR-BHRF1-2-5p and ebv-miR-BHRF1-3, mucosa-associated lymphoid tissue lymphoma transport protein 1 (MALT1) was predicted to have two potential binding sites for ebv-miR-BHRF1-2-5p on the 3′-UTR. MALT1 is involved in immune homeostasis (Gewies et al., 2014; Jaworski et al., 2014). Also a binding site for ebv-miR-BHRF1-3 was found within the mRNA of phosphatase and tensin homologue (PTEN), which had been confirmed previously as a target of ebv-miR-BHRF1-3 (Bernhardt et al., 2016). | Mature EBV miRNAs are transported by exosomes, which protect them from degradation by RNases. Thus, EBV-encoded miRNAs are stable in the serum so that they can be used as a diagnostic marker and monitor of EBV-associated disorders, including MS. Large-scale studies have confirmed that EBV is the only viral agent that is associated positively with MS (Pender et al., 2014; Belbasis et al., 2015). | |||||||||
| Vistbakka et al., 2017; Finland | Screening phase: 18 PPMS patients, 8 M/10 F, 53.5 ± 8.5 yrs, disease duration from first symptoms 15.6 ± 10.0 yrs, disease duration from diagnosis 11.0 ± 7.7 yrs, EDSS 5.9 ± 1.3, progression index 0.8 ± 1.0. Validation phase: 31 PPMS patients, 13 M/18 F, 56.3 ± 9.7 yrs, disease duration from first symptoms 16.8 ± 10.9 yrs, disease duration from diagnosis 10.9 ± 8.4 yrs, EDSS 5.3 ± 1.8, progression index 0.7 ± 0.8; 31 SPMS patients, 7 M/24 F, 48.8 ± 9.5 yrs, disease duration from first symptoms 23.4 ± 8.3 yrs, disease duration from diagnosis 16.6 ± 8.3 yrs, EDSS 5.7 ± 1.4, progression index 0.45 ± 0.3. Blood was collected and allowed to clot for 30 min before centrifugation (1500 × g, 15 minutes). Serum was separated and stored at –80oC. | Screening phase: 10 HC, 4 M/6 F, 51.8 ± 8.2 yrs. Validation phase: 21 HC, 9 M/12 F, 52.7 ± 8.1 yrs. | Expression of miRNAs was measured using RT-PCR. Of the 84 miRNAs analysed in the screening phase, 4 were significantly downregulated (miR-375, miR-130b-3p, miR-141-3p, miR-124-3p) and 5 were upregulated (miR-128-3p, miR-376c-3p, miR-191-5p, miR-26a-5p, miR-24-3p) in PPMS compared to HC. In the validation phase, when the group including all MS patients was compared to HC, 5 miRNAs (miR-128-3p, miR-376c-3p, miR-26a-5p, miR-191-5p, miR-24-3p) were upregulated (FC > 1.5, P < 0.05), but after the Bonferoni correction (to reduce the chances of obtaining false-positive results) only the differences for 4 miRNAs (miR-128-3p, miR-376c-3p, miR-26a-5p, miR-191-5p) reached statistical significance. Of these, miR-191-5p had the strongest upregulation in PPMS (FC = 1.9). Analysis between the groups revealed significant upregulation of 5 miRNAs (miR-128-3p, miR-376c-3p, miR-26a-5p, miR-191-5p, miR-24-3p) in PPMS compared to HC. After the Bonferroni correction, 4 of them (miR-128-3p, miR-376c-3p, MIR-191-5p, miR-24-3p) remained statistically significant. miR-191-5p showed the greatest upregulation (FC = 2.3). In SPMS, 3 miRNAs (miR-376c-3p, miR-26a-5p, miR-191-5p) were upregulated (FC > 1.5, P < 0.05), but only miR-191-5p remained statistically significant after the Bonferroni correction (FC = 1.6). Comparison between PPMS and SPMS showed that 2 miRNAs (miR-128-3p, miR-24-3p) were significantly upregulated in PPMS after the Bonferroni correction (miR-128-3p, FC = 1.5; miR-24-3p, FC = 1.5). In the screening and validation phases, 18 MS and 9 HC samples were the same. To confirm that the results could be replicated in an independent cohort, additional logistic regression model analyses were performed excluding all the overlapping samples. Analysis showed that 3 miRNAs (miR-128-3p, miR-26a-5p, miR-191-5p) were significantly expressed in progressive MS patients (PPMS and SPMS) compared to HC as was detected in the whole validation cohort. The expression of miR-376c-3p did not differ statistically between MS and HC. Comparison between the groups showed that 3 miRNAs (miR-128-3p, miR-26a-5p, miR-191-5p) were significantly expressed in PPMS and 2 miRNAs (miR-26a-5p, miR-191-5p) in SPMS compared to HC. No differences in the expression levels were detected between PPMS and SPMS. However, the independent cohort was of very small size (n = 13) for PPMS vs. HC and for PPMS vs. SPMS. In PPMS vs. HC, expression of miR-376-3p was on border of statistical significance (P = 0.07) and for PPMS vs. SPMS, expression of miR-128-3p was on border of statistical significance (P = 0.07). In the whole MS group, expression of miR-124-3p correlated positively with time from first symptoms. The SPMS group had a positive correlation between expression of miR-128-3p and progression index. In the PPMS group, miR-124-3p correlated with time from first symptoms and miR-375 with age. When patients with EDSS > 6 were excluded from the analysis, a negative correlation was found between miR-375 and progression index in PPMS. | By ROC analysis, high values for AUC, sensitivity and specificity were obtained for miR-128-3p (AUC 0.727, sensitivity 0.645, specificity 0.714) and miR-191-5p (AUC 0.808, sensitivity 0.742, specificity 0.810) in PPMS, suggesting them as potential predictors of PPMS. | Increased expression of miR-191-5p was associated with PPMS and SPMS, while that of miR-128-3p was mostly associated with PPMS. | |||||||||
| Sharaf-Eldin et al., 2017; Egypt | 18 RRMS patients, 4 M/14 F, 29.1 ± 7.2 yrs, disease duration 5.5 yrs, EDSS 2.8, MSSS 4.6; 19 SPMS patients, 5 M/14 F, 37.7 ± 8.0 yrs, disease duration 8.0 yrs, EDSS 6.6, MSSS 8.4. Diagnoses of MS were based on the revised McDonald criteria (Polman et al., 2011). Disability and MS severity were evaluated according to EDSS and multiple sclerosis severity score (MSSS) (Roxburgh et al., 2005). None of the patients had received glucocorticosteroids, immunomodulators, immunosuppressants or other DMT for at least 3 weeks prior to study entry. Venous blood samples were collected, centrifuged (4500 r/min, 30 minutes) and sera stored at –80oC. | 23 HC, 6 M/17 F, 35.8 ± 9.8 yrs. They had no sign or history of autoimmune, inflammatory or neurological diseases. | By RT-qPCR, miR-145 and miR-223 (FC = 2.0 and FC = 2.2, respectively) were significantly upregulated in MS patients (n = 37) compared to HC, whereas miR-326 expression (FC = 1.8) did not differ significantly between MS patients and HC. For RRMS patients, FC values for miR-145, miR-223 and miR-326 were 2.6, 2.7 and 3.1, respectively, while for SPMS patients FC values for miR-145, miR-223 and miR-326 were 1.4, 2.2 and 1.2, respectively. FC value for miR-326 was significantly different between RRMS and SPMS. Expression of target genes SP1 (specificity protein 1) was significantly downregulated in MS patients compared to HC, whereas that of SMAD3 (signaling mother against decapentaplegic peptide 3) was not significantly downreguated in MS patients compared to HC. EDSS or MSSS did not correlate significantly with the expression levels of any of the miRNAs or mRNAs investigated. Regarding treatments, there were no significant differences in expression levels of miR-145, miR-223, miR-326, SP1, and SMAD3. | By ROC analysis, MS patients could be distinguished from HC by expression of miR-145 with AUC value 0.670 (sensitivity 0.730, specificity 0.609), expression of miR-223 with AUC value 0.702 (sensitivity 0.730, specificity 0.609. Combining miR-145 and miR-223 gave AUC value 0.713 (sensitivity 0.892, specificity 0.478). Also combining miR-145, miR-223 and miR-326 gave AUC value 0.725 (sensitivity 0.892, specificity 0.478). | Expression of miR-145 and miR-223 can distinguish MS patients from HC. | |||||||||
| Regev et al., 2017; USA | Cohort 1: 41 MS patients 29 RRMS/7 SPMS/5 PPMS, 7 M/34 F, 47.7 ± 9.5 yrs, disease duration from first symptoms 8.5 ± 7.6 yrs, EDSS 2.2 ± 2.5, DMT at MRI Untreated28/Glatiramer acetate4/beta interferons9. Cohort 2: 79 MS patients 66 RRMS/10 SPMS/3 PPMS, 26 M/53 F, 43.0 ± 7.5 yrs, disease duration from first symptoms 11.7 ± 6.8 yrs, EDSS 2.0 ± 1.9, DMT at MRI Untreated6/ Glatiramer acetate30/beta interferons 25/other 18. Serum samples were collected in tubes without additives, centrifuged (2000 × g, 10 minutes) to separate serum, and stored at –70oC. MRI scans were performed to identify brain lesions, brain atrophy, and cervical spinal cord lesions and atrophy. | MiRNAs were measured by RT-qPCR. In cohort 1, the miRNAs that demonstrated strong correlations with MRI were similar for brain parenchymal fraction and global cerebral GM fraction. However, the miRNAs associated with lesions were mostly different from those associated with atrophy, suggesting different pathogenic processes underlying focal lesions (inflammatory demyelination) vs. neurodegeneration (axonal and neuronal loss). In cohort 2, miRNAs that showed a strong correlation with whole-brain atrophy also indicated a strong correlation with cerebral GM atrophy. However, a different set of miRNAs correlated with spinal cord vs. brain atrophy. Although several mRNAs were associated with MRI outcome, none of these associations remained significant when correcting for multiple comparisons using false discovery rate. Several miRNAs showed significant associations with EDSS score in both cohorts. These associations for seven miRNAs miR-19a-3p, miR-101-3p, miR-30e-3p, miR-19b-3p, miR-29c-3p, miR-32-5p, miR-195-5p remained significant after correcting for multiple comparisons using false discovery rate. All of these miRNAs except for miR-195-5p had a protective relationship shown by a higher miRNA expression being associated with lower severity of MRI-indicated involvement. MiR-195-5p had a pathogenic relationship shown by a higher miRNA expression being associated with greater severity of MRI-indicated involvement. | Significant correlations were found between miRNAs and disability for miR-19a-3p, miR-101-3p, miR-30e-3p, miR-19b-3p, miR-29c-3p, miR-32-5p, miR-195-5p. Although several miRNAs were associated with MRI outcomes, none of these associations remained significant when correcting for multiple comparisons, suggesting that further validation of the findings is needed. | |||||||||||
| Regev et al., 2016; USA | Discovery phase: 7 RRMS patients, 2 M/5 F, 50 ± 6.4 yrs, disease duration 8.7± 1.5 yrs, EDSS 0.5 ± 0.8; 9 SPMS patients, 3 M/6 F, 50 ± 6.4 yrs, disease duration 17.0 ± 7.7 yrs, EDSS 5.8 ± 1.4; 10 PPMS patients, 5 M/5 F, 57 ± 7.5 yrs, disease duration 16.6 ± 5.2 yrs, EDSS 5.1 ± 2.3. Validation phase: 29 RRMS patients, 10 M/19 F, 36 ± 7.6 yrs, disease duration 3.4 ± 3.0 yrs, EDSS 1.1 ± 0.9; 19 SPMS patients, 6 M/13 F, 46 ± 6.9 yrs, disease duration 15.2 ± 4.8 yrs, EDSS 6.1 ± 1.2; 10 PPMS patients, 5 M/5 F, 47 ± 5.5 yrs, disease duration 10.9 ± 5.9 yrs, EDSS 5.3 ± 2.1. Samples from patients with MS were obtained from the CLIMB study. Those patients selected for this study had not received treatment with steroids in the past month; glatiramer acetate, interferon beta, fingolimod, dimethyl fumarate., or teriflunomide in the past 3 months; or other DMT in the past 6 months including cyclophosphamide, rituximab, daclizumab, methotretate, and natalizumab. Blood samples were collected in tubes without additives, and kept at room temperature for 30–60 minutes. Samples were centrifuged (2000 r/min, 10 minutes) to separate serum and then stored at –70oC. | Discovery phase: 20 HC, 6 M/14 F, 33 ± 9.2 yrs. Validation phase: 30 HC, 9 M/21 F, 43 ± 1.2 yrs. HCs were obtained from the Brigham PhenoGenetic Cohort study and from healthy participants enrolled in the CLIMB study. | By RT-PCR, in the discovery phase 167 miRNAs were identified that were differentially expressed between patients with MS and HC. After filtering using the selection criteria, 40 miRNAs were chosen for further validation. In the validation phase, 7 miRNAs were significantly differentially expressed in MS compared to HC. Of these 7 miRNAs, 6 were significantly different after correcting for multiple comparisons using false discovery rate: miR-320a, miR-486-5p, miR-320b, miR-25-3p, miR-140-3p (all upregulated) and let-7c-5p (downregulated). The findings remained unchanged after adjustment for age and gender. | By ROC analysis, the highest AUC value was for miR-320a (0.707) and discriminated MS patients from HC. When all 6 miRNAs that were significant after correcting for multiple comparisons were combined (miR-320a + miR-486-5p + miR-320b + miR-25-3p + miR-140-3p + let-7c-5p) the AUC value was 0.795. To identify disease category biomarkers, in the discovery phase 21 miRNAs were identified that were differentially expressed between the groups. In the validation phase, miR-27a-3p and miR-376-3p were significantly differentially expressed in RRMS compared to SPMS in the same direction in the discovery and validation phases. MiR-27a-3p had the highest AUC value (0.78) and only this miRNA remained significant after correcting for multiple comparisons. The results were the same after adjustment for age and gender. In the comparison of RRMS to PPMS, none of the miRNAs selected from the discovery phase were validated in the validation phase. To investigate the association between miRNAs and disability, in the discovery phase using all untreated patients with MS (plus 59 additional patients with RRMS), 103 miRNAs were significantly associated with EDSS score, and 40 were selected for further validation. In the validation phase, 10 miRNAs were significantly associated with EDSS score, and 9 remained significantly correlated to EDSS after adjusting for age. Two of these miRNAs miR-199a-5p, and miR-142-5p remained significantly correlated to EDSS after correcting for multiple comparisons. The highest correlation with EDSS was with miR-199a-5p. | Serum miR-320a, miR-486-5p, miR-320b, miR-25-3p, miR-140-3p, let-7c-5p discriminated MS from HC. MiR-27a-3p distinguished RRMS from SPMS. Also miR-199a-5p, and miR-142-5p were significantly correlated to EDSS score. | |||||||||
| Exosomes isolated from serum | ||||||||||||||
| Selmaj et al., 2017; Poland | Discovery set: 9 RRMS relapse patients, 1 M/8 F, 39 ± 11 yrs, disease duration 6.8 ± 7.8 yrs, EDSS 2.6 ± 1.9; 10 RRMS remission patients, 2 M/8 F, 37 ± 10 yrs, disease duration 6.4 ± 5.5 yrs, EDSS 2.3 ± 1.2. Validation set: 33 RRMS relapse, 8 M/25 F, 36 ± 11 yrs, disease duration 6.9 ± 8.2 yrs, EDSS 2.6 ± 1.1; 30 RRMS remission, 9M/21F, 37 ± 9 yrs, disease duration 7.5 ± 8.8 yrs, EDSS 2.2 ± 1.3. MS patients were classified as RRMS according to the revised McDonald criteria. Relapse was defined as the appearance of new neurological signs or worsening of pre-existing signs after a minimum of 30 days of clinical stability. All patients were sampled before methylprednisolone administration. Patients in remission did not receive DMT for at least 6 months. Venous blood was collected, allowed to coagulate, centrifuged, and serum removed and stored at –80oC. All patients were assessed for EDSS and examined by MRI. Exosomes were isolated from serum samples by the polymer formulation method (Peterson M et al., 2015). The vesicles isolated from sera were confirmed to be exosomes based on size (30–100 nm) as determined by nanoparticle tracking analysis (NTA) and expression of exosomal protein markers CD9 and Alix. There were no significant differences in total number of exosomes in sera of RRMS patients in relapse and in remission or HC. There were no significant differences in total amount of exosome RNA in sera of RRMS patients in relapse or remission and HC | Discovery set: 10 HC, 1 M/9 F, 34 ± 10 yrs. Validation set: 32 HC, 8 M/24 F, 38 ± 10 yrs. | MiRNA profiling of exosomes by next generation sequencing (NGS) in 29 samples of the discovery set identified 4 miRNAs that were significantly differentially expressed in RRMS patients in remission and relapse and HC (miR-122-5p, miR-196b-5p, miR-301a-3p, miR-532-5p). The specificity of these 4 serum exosomal miRNAs for RRMS patients was validated in a separate cohort of 95 subjects by qPCR. All 4 miRNAs were significantly differentially expressed between RRMS in remission and relapse and HC. In agreement with the NGS data, miR-122-5p, miR-196b-5p, miR-532-5p were significantly downregulated in RRMS relapse patients when compared to RRMS remission patients. All 4 miRNAs were significantly downregulated in RRMS relapse compared to HC, and miR-122-5p was significantly downregulated in RRMS remission compared to HC. | By ROC analysis, these 4 miRNAs gave high AUC values for discriminating between RRMS patients in relapse and HC (for miR-122-5p, miR-196b-5p, miR-301a-3p, miR-532-5p the values were 0.878, 0.866, 0.681, 0.800, respectively). Combining the levels of miR-122-5p and miR-196b-5p provided the highest AUC value for discriminating RRMS relapse from HC (0.904) and for RRMS relapse from RRMS remission (0.866). A combined measurement of miR-122-5p and miR-196b-5p improved diagnosis of RRMS relapse vs. remission with sensitivity > 0.89 and specificity > 0.75. No correlation was found between the clinical parameters (disease duration and disability assessed by EDSS) and the levels of the 4 miRNAs tested. To determine whether the levels of the 4 miRNAs correlated with MRI evidence of disease activity, the RRMS samples were divided into 2 categories: patients with Gd-enhancing lesions on brain MRI (Gd- positive) and patients with no signs of Gd enhancement (Gd- negative). The Gd- positive patients had significantly lower serum concentrations of all these miRNAs. Thus, lower levels of circulating exosomal miR-122-5p, miR-196b-5p, miR-301a-3p, miR-532-5p were related to disease activity. | Exosomal miRNAs might be a useful biomarker to distinguish MS relapse. PBMC secretion of all 4 miRNAs was significantly downregulated in RRMS patients compared to HC. PBMCs might represent a potent source of the exosomes containing miR-122-5p, miR-196b-5p, miR-301a-3p, and miR-532-5p, the secretion of which are decreased in RRMS patients. | |||||||||
| Niwald et al., 2017; Poland | 23 stable RRMS patients, 8 M/15 F, 48.8 ± 11.2, disease duration 13.2 ± 7.2 yrs, EDSS 5.5 ± 2.1, MoCA (Montreal cognitive assessment index) 25.9 ± 2.7, BDI (Beck Depression Index) 9.5 ± 5.3; 13 postacute RRMS patients, 3 M/10 F, 41.8 ± 10.2, disease duration 9.8 ± 9.6 yrs, EDSS 6.3 ± 2.8, MoCA 25.2 ± 4.1, BDI 11.7 ± 3.3. The stable RRMS patients were in the remission phase, without treatment, for over 2 yrs without attacks or steroid treatment (late phase). The postacute RRMS patients were in the early phase of remission, 1 to 2 mths free of i.v. 5-day methyl-prednisolone (1000 mg/d) due to severe exacerbation in Neurological units. All the patients underwent complete medical examinations. Venous blood was collected into tubes containing an anticoagulant (EDTA) and left at room temperature until clot formation (30–60 minutes). Blood samples were centrifuged (1200 × g, 10 minutes, 23oC) and the serum carefully removed and stored at –80oC. Exosome isolation from frozen human serum was performed. Serum samples were thawed, and centrifuged (2000 × g, 30 minutes) to remove the cells and residues from the serum. Then, 500 µL of the supernatant was treated with 0.2 volumes of the Total Exosome Isolation reagent and after mixing well were incubated 2–8oC for 30 minutes. After incubation, samples were centrifuged (10,000 × g, 10 minutes, room temperature). The supernatant was removed and the pellet containing the exosomes was suspended in 200 µL PBS and stored at 2–8oC for 1 week or at –20oC until RNA isolation. | 10 HC, 3 M/7 F, 50.7 ± 8.1 yrs. | RNA isolation from the exosomes was performed. Analysis by qPCR showed a decreased expression of miR-155 and miR-301a (in 94% and 51% samples, respectively) and an increased expression of miR-326 (in 72% samples) in RRMS patients (n = 36). The difference in relative expression of miR-155 for RRMS patients compared to HC was statistically significant. No correlation was found between expression levels of miR-155, miR-326 and miR-301a and age. A positive correlation was found between relative expression of miR-326 and miR-301a and BDI. A positive correlation was found between RQ (relative quantification) miR-301a and MoCA. Expression levels of miR-301a and miR-155 were higher in RRMS patients in postacute vs. stable phase of remission. Statistically significant differences in RQ values between early vs. late phase of remission were found for miR-301a and miR-155. There was no significant difference in the case of miR-326. Statistical analysis between two groups of RRMS patients with BDI ≤ 11 vs. BDI > 11 revealed lower miR-326 and miR-301a expression levels in patients with BDI ≤ 11, while miR-155 expression was increased in BDI ≤ 11. A statistically significant difference was found for miR-326, but not for miR-301a and miR-155. Statistical analysis between HC, RRMS BDI > 11 and RRMS BDI ≤ 11 showed significant differences only for miR-326, with a significantly higher expression in RRMS BDI > 11 vs. HC. On dividing RRMS patients into two subgroups based on their disability EDSS ≤ 5 and EDSS > 5, no significant differences were found in expression level of miR-155, miR-326 and miR-301a. | The expression levels of miR-301a and miR-155 were significantly higher in the postacute vs. stable phase of remission, where neuroinflammatory processes are more severe. Expression changes of serum miRNAs could be used as a biomarker of relapse activity. | ||||||||||
| Ebrahimkhani et al., 2017; Australia | 14 RRMS patients, 4 M/10 F, age of onset 35.6 ± 7.3 yrs, disease duration 6.9 ± 7.1 yrs, treatment Y 6/N 8, EDSS 1.5 ± 1.0. Discovery: 11 SPMS7/PPMS4 patients, 6M/5F, 38.4 ± 8.5 yrs, disease duration 15 ± 9.4 yrs, treatment Y 4/N 7, EDSS 5.3± 1.6. Validation: 11 SPMS/PPMS patients, 1 M/10 F, 32.3 ± 8.2 yrs, disease duration 20.4 ± 4.8 yrs, treatment Y 7/N 4, EDSS 6.0 ± 1.1. MS was diagnosed according to the revised McDonald criteria. Venous blood was collected at the time of clinical consultation, left at room temperature for 30 min for coagulation, and then centrifuged (1800 × g, 10 minutes). The resulting serum was centrifuged (3000 × g, 20 minutes) to remove any cellular debris, and stored at –80oC. Serum samples were treated with RNaseA to remove any unprotected circulating RNA. Exosomes were isolated from 1 ml of serum by size exclusion chromatography. Nanoparticle tracking analysis and transmission electron microscopy revealed a population of nanovesicles with a predominant size of 95 nm and cup-shaped morphology typical of exosomes. Western blotting of protein extracts for CD61, CD83 and Alix confirmed that the particles isolated expressed all three characteristic exosome markers. | 11 HC, 2 M/9 F, 40.3 ± 13.3 yrs, treatment Y 0/N 11. | Using NGS and three statistical approaches, 4 significantly upregulated miRNAs were identified for RRMS patients compared to HC (miR-15b-5p, miR-30b-5p, miR-342-3p, miR-451a), and 4 significantly upregulated miRNAs for SPMS/PPMS patients compared to HC (miR-127-3p, miR-370-3p, miR-409-3p, miR-432-5p). There were 3 significantly upregulated miRNAs for RRMS compared to SPMS/PPMS patients. MiRNAs were identified as differentially expressed if they met a fold-change ≥ 2 and P ≤ 0.05 in at least two of the three statistical tests. In the validation study, 6 miRNAs were significantly upregulated in SPMS/PPMS patients compared to HC (miR-370-3p, miR-409-3p, miR-432-5p, miR-15b-5p, miR-223-3p, miR-23a-3p). In addition, 9 miRNAs were dysregulated in RRMS compared to SPMS/PPMS patients (miR-15b-5p, miR-23a-3p, miR-223-3p, miR-30b-5p, miR-342-3p, miR-374a-5p all upregulated, and miR-432-5p, miR-433-3p, miR-485-3p all downregulated (P < 0.05 in at least two tests and FC ≥ 1.7 in either direction)). | By ROC analysis, miR-451a had the highest AUC value (0.83) for distinguishing RRMS patients from HC, while miR-127-3p, miR-409-3p, miR-370-3p, miR-432-5p had AUC values 0.90, 0.91, 0.86, 0.90, respectively, for distinguishing SPMS/PPMS patients from HC. For distinguishing RRMS from SPMS/PPMS patients, miR-433-3p, miR-432-5p, miR-485-5p had AUC values 0.93, 0.86, 0.87, respectively. Using the original 9 miRNAs identified for RRMS vs. SPMS/PPMS it was possible to predict 11/11 PPMS samples in the validation set. | Differentially expressed exosomal miRNAs were identified in both RRMS (miR-15b-5p, miR-451a, miR-30b-5p, miR-342-3p) and progressive MS patient sera (miR-127-3p, miR-370-3p, miR-409-3p, miR-432-5p) compared to HC controls. A group of nine miRNAs (miR- 15b-5p, miR-23a-3p, miR-223-3p, miR-374a-5p, miR-30b-5p, miR-433-3p, miR-485-3p, miR-342-3p, miR-432-5p) were found that distinguished RRMS from progressive disease. | |||||||||
AUC: Area under curve; CI: cognitively impaired; CP: cognitively preserved; DMT: disease-modifying treatment; EDSS: expanded disability status scale; F: females; FC: fold change; M: male(s); MS: multiple sclerosis; N: no; NA: not available; PPMS: primary-progressive MS; ROC: receiver operating characteristics; RRMS: relapsing-remitting MS; SPMS: secondary-progressive MS; Y: yes.
Table 2.
MicroRNAs in CSF of human patients with MS
| Authors, country | Number of patients, gender, ages | Comparison | Changes in miRNAs in DR patients | Functional outcomes | Conclusion |
|---|---|---|---|---|---|
| Quintana et al., 2017; Spain | Discovery study: RRMS patients, 0 M/9 F, 4 LS_OCMB-/ 5 LS_OCMB+, median age 37 yrs. Validation study: 47 MS patients LS_OCMB-, 17 M/30 F, median age 32 yrs, presentation monofocal42/polyfocal2; 39 MS patients LS_OCMB+, 13 M/26 F, median age 34 yrs, presentation monofocal 35/polyfocal 4. All MS patients presented McDonald 2010 RRMS form and none was being treated with corticosteroids, immunosuppressants or immunomodulators. CSF was collected and centrifuged (400 × g, 15 minutes, 19oC) and then stored at –80oC until analysis. All MS patients were recruited at the beginning of the disease (most during the first year). Gadolinium-positive lesions were present in 57% of the patients. | Discovery study: 5 other neurological diseases (OND) controls, 0 M/5 F, median age 38 yrs. Validation study: 55 OND controls, 21 M/34 F, median age 36 yrs. | In the comparison of MS patients and OND controls, no differences were found for gender distribution or age in discovery cohort or in validation cohort. Similarly when separated into MS LS_OCMB-, MS LS_OCMB+, OND, no differences were found for gender distribution or age. Clinical and radiological data collected for MS patients from MRI performed within a mean of 3 months did not show any differences between LS_OCMB- and LS_OCMB+, except for onset symptoms where 50% of LS_OCMB+ patients presented medullar symptoms. In the discoverv study using RT-PCR, 62 miRNAs were detected in at least 75% of individuals. Of these miRNAs, 12 had significantly different expression for MS vs. controls: miR-203, miR-365, miR-21, miR-520c-3p, miR-191, miR-328, miR-30a-5p (upregulated in MS) and miR-140, miR-126, miR-199a-3p, miR-143, miR-19a (downregulated in MS). Greatest fold change values for upregulated miRNAs were for miR-30a-5p FC = 8.0 and miR-520c-3p FC = 6.4, while for downregulated miRNAs were for miR-140 FC = –3.8 and miR-19a FC = –3.4. In the validation study using RT-PCR, statistically significant differences in expression for MS vs. OND control were found for miR-328, miR-30a-5p, miR-150, miR-645 (upregulated in MS) and miR-365, miR-21, miR-191, miR-199a-3p, miR-106a, miR-146a (downregulated in MS). Four miRNAs showed significantly different expression in LS_OCMB+ vs. OND controls: miR-30a-5p, miR-150, miR-645 (upregulated in LS_OCMB+) and miR-191 (downregulated in LS_OCMB+). Two miRNAs had significantly different expression in LS_OCMB- vs. OND controls: miR-199a-3p and miR-106a (downregulated in LS_OCMB-). No significant differences were found for any miRNA between LS_OCMB+ and LS_OCMB-. | By ROC analysis, miR-150 had the greatest AUC value (0.684) for distinguishing MS patients from OND. | Upregulated expression of miR-150 was found for MS patients compared to OND controls and also for LS_OCMB+ compared to LS_OCMB-. |
| Bergman et al., 2016; Sweden | Validation cohort 1: 34 CIS patients, 10 M/24 F, median age 36 yrs, median disease duration from onset 1 yr, EDSS 2, percent sampled during relapse 20, percentage oligoclonal bands (OCB) positive 45, median CSF mononuclear cells 2.5; 43 MS patients, 17 M/26 F, median age 37 yrs, median disease duration from onset 7 yrs, EDSS 2.5, percent sampled during relapse 26, percentage OCB positive 88, median CSF mononuclear cells 6. Validation cohort 2: 96 CIS patients, 25 M/71 F, median age 32 yrs, median disease duration from onset 0 yr, EDSS 1, percent sampled during relapse 26, percentage OCB positive 71, median CSF mononuclear cells 4, percent converted CIS 63; 120 MS patients, 38 M/82 F, median age 37 yrs, median disease duration from onset 6 yrs, EDSS 2, percent sampled during relapse 31, percentage OCB positive 82, median CSF mononuclear cells 4. CSF samples were collected by lumbar puncture, centrifuged (440 × g, 10 minutes, room temperature) to separate cells and large particles from the CSF supernatant. | Validation cohort 1: 34 NINDC (noninflammatory neurologic disease controls) 10 M/24 F, median age 35 yrs, percentage OCB positive 0, median CSF mononuclear cells 2; 31 I inflammatory neurologic disease controls (INDC), 10 M/21 F, median age 45 yrs, percentage OCB positive 9, median CSF mononuclear cells 2. Validation cohort 2: 119 NINDC, 37M/82F, median age 38 yrs, median disease duration from onset 2 yrs, EDSS 1, percentage OCB positive 0, median CSF mononuclear cells 1; 95 INDC, 30 M/65 F, median age 40, median disease duration from onset 2 yrs, EDSS 1, percentage OCB positive 13, median CSF mononuclear cells 2. | By qRT-PCR, 15 miRNAs were selected from the analysis of pooled CIS, MS, NINDC and INDC cell-free CSF samples for examination in validation cohort 1. Of the tested miRNAs, only miR-145 and miR-150 were significantly different for MS compared to NINDC control. In the larger validation cohort 2, it was possible to replicate significantly higher levels of miR-150 in MS compared to both NINDC and INDC controls as well as being significantly higher between CIS and NINDC. Also a significantly higher level of miR-145 in MS compared to NINDC was found. Significantly higher miR-150 levels were found in CSF from patients with CIS who subsequently converted to MS compared to those who did not convert during follow-up (median period of 52 months). High levels of miR-150 correlated with higher CSF cell numbers and higher IgG index, indicating that miR-150 associated with active inflammation. In contrast, miR-150 levels did not correlate with the number of MRI T2 lesions and EDSS score, and there was only a tendency for higher miR-150 levels in relapse. | By ROC analysis, miR-150 level in CSF distinguished MS patients in relapse/remission from controls with AUC value 0.744 (sensitivity 0.890, specificity 0.500). In validation cohort 1, the ratio of miR-150 to miR-204 gave the largest difference between MS and NINDC. Also the ratio of miR-150 to miR-204 was significantly higher in MS compared to NINDC and INDC in validation cohort 2, as well as in patients with CIS who subsequently converted to MS compared to those who did not convert. By ROC analysis, the ratio of miR-150 to miR-204 had an AUC value of 0.811 (sensitivity 0.710, specificity 0.790) for differentiating MS from NINDC. In this respect, miR-150/miR-204 ratio performed as well as the best protein biomarker CXCL13. The miR-150/miR-204 ratio also differentiated patients with CIS who converted to MS compared to those who did not convert with an AUC value of 0.775. | CSF miR-150 is a biomarker for MS patients and for CIS patients who subsequently convert to MS. |
| Ahlbrecht et al., 2016; Germany | 28 CIS-CIS patients, 7 M/21 F, 37.6 ± 11.5 yrs, EDSS 2.0 ± 1.1, onset of DMT after CIS diagnosis 35.7%, Qalb 5.2 ± 2.1, dysfunction of blood/CSF barrier 32.1%; 30 CIS-RRMS patients, 7 M/23 F, 31.1 ± 9.7 yrs, median time to RRMS 156 days, EDSS 2.4 ± 1.1, onset of DMT after CIS diagnosis 36.7%, Qalb 5.0 ± 1.7, dysfunction of blood/CSF barrier 23.3%. Inclusion criteria included CIS patients who underwent lumbar puncture and brain MRI scan at the time of CIS diagnosis whose residual CSF and serum samples were stored at –80oC and who had a documented CIS disease status 1 yr after CIS diagnosis or converted to RRMS within 1 yr. CSF and serum samples were collected simultaneously. CSF samples were centrifuged (170 × g, 10 minutes). Serum samples were centrifuged (1500 × g, 10 minutes). The cell-free supernatants of CSF and serum were stored frozen until the measurement of miRNAs. A dysfunction of the blood-CSF barrier was defined by CSF/serum albumin quotient (Qalb) higher than age-adjusted upper reference limit calculated as 4 + (age in years)/15 (Reiber, 1998). | By qRT-PCR, levels of miR-922 in CSF and serum were significantly higher in CIS-RRMS than CIS-CIS patients. While miR-181c levels in CSF were significantly higher in CIS-RRMS than CIS-CIS patients, there was no difference in serum levels of miR-181c between the two groups. No differences were found between CIS-CIS RRMS and CIS-CIS patients for miR-633 in both CSF and serum. Levels of the investigated miRNAs did not significantly correlate with age, EDSS, CSF cell count, total protein levels in CSF and Qalb. In univariate Cox regression analyses, lower levels of CSF miR-181c and serum miR-922 were significantly associated with a lower risk of conversion from CIS to RRMS. None of the other miRNAs were significantly associated with conversion to RRMS. Of the other baseline factors, younger age, and > 9 lesions on MRI, were significantly associated with conversion to RRMS. In the multivariate Cox regression analyses, CSF miR-181c, age, and MRI were significantly associated with conversion from CIS to RRMS, while serum miR-922 was not significantly associated with conversion to RRMS. | By ROC analysis, for CSF miR-181c the AUC value was 0.67. Combining MRI, age and CSF miR-181c resulted in an increased AUC value of 0.83 and improved values of specificity and positive predicted value for conversion to RRMS compared to CSF miR-181c alone or the combination of age and MRI (96% and 94%, respectively) | CSF miR-181c might serve as a biomarker for early conversion to RRMS. |
AUC: Area under curve; CIS: clinically isolated syndrome; CSF: cerebrospinal fluid; F: females; FC: fold change; LS_OCMB: lipid-specific oligoclonal IgM bands; M: male(s); MS: Multiple sclerosis; ROC: receiver operating characteristics; RRMS: relapsing-remitting MS.
The important findings from the research articles in the PubMed searches are summarized as follows:
-
1)
Peripheral blood: A large-scale study by Nuzziello et al. (2018) that included 58 MS patients, comprising 54 RRMS (93%) and 4 SPMS (7%), and 20 HC showed using PCR that miR-320a (fold change, FC = 1.79), miR-125a-5p (FC = 1.89), miR-652-3p (FC = 1.51), miR-185-5p (FC = 1.5), miR-942-5p (FC = 1.67), and miR-25-3p (FC = 1.49) were significantly upregulated in MS compared to HC. The AUC values for the validated miRNAs ranged from 0.701 to 0.735 for miR-320a, miR-185-5p, miR-125a-5p and miR-652-3p, and are fair tests for discriminating MS patients from HC, with miR-320a having the highest AUC value (0.735). In a study by Liguori et al. (2018) involving 19 pediatric MS (PedMS) patients and 20 healthy pediatric controls (PC) and with RT-PCR validation, 12 miRNAs (let-7a-5p, let-7b-5p, miR-25-3p, miR-125a-5p, miR-942-5p, miR-221-3p, miR-652-3p, miR-182-5p, miR-185-5p, miR-181a-5p, miR-320a, miR-99b-5p) were significantly upregulated and 1 miRNA (miR-148b-3p) significantly downregulated in PedMS compared to PC. PedMS patients were analyzed during the inactive phase of RRMS disease course, and at the time of blood sample all treated patients were receiving interferon β-1 therapy.
-
2)
Peripheral blood leukocytes: Magner et al. (2016) recovered leukocytes from whole blood samples of 24 MS patients, comprising 19 RRMS (79%) and 5 SPMS (21%), and 20 HC, and by next generation sequencing analysis 13 miRNAs (miR-484, miR-9-5p, miR-323b-3p, miR-15b-5p, miR-145-5p, miR-337-5p, miR-485-5p, miR-654-3p, miR-377-3p, miR-493-5p, miR-301b, miR-409-3p, miR-494) were significantly upregulated and 3 miRNAs (miR-451a, miR-144-5p, miR-101-3p) significantly downregulated in untreated RRMS patients compared to HC. The highest logFC values were for miR-337-5p (logFC = 1.58), miR-144-5p (logFC = –1.98) and miR-451a (logFC = –1.71). Two miRNAs (miR-146b-5p, miR-874) were negatively correlated with EDSS, and two others (miR-107, miR-3614) were positively correlated, in untreated RRMS patients.
-
3)
Blood serum: In a large-scale study by Vistbakka et al. (2018) with 53 RRMS patients, 20 PPMS patients and 27 HC, it was found by RT-PCR that 2 miRNAs were significantly upregulated in both RRMS and PPMS, miR-191-5p (RRMS, FC = 1.65; PPMS, FC = 1.75) and miR-24-3p (RRMS, FC = 2.10; PPMS, FC = 3.58), compared to HC. There were no statistically significant differences between RRMS and PPMS. Active DMT treatment was ongoing in 37 patients with RRMS, (70%) and no significant differences in miRNA expression levels were found between untreated and treated MS patients. Regev et al. (2018) studied miRNA expression in four cohorts of patients: CLIMB cohort comprising 24 RRMS, 18 SPMS, 30 HC; AMIR cohort 31 RRMS, 5 SPMS, 19 HC; EPIC cohort 27 RRMS, 7 SPMS, 26 HC; STORM II cohort 33 RRMS, 21 SPMS, 13 HC. None of the selected patients were receiving DMT at the time of sample collection. By RT-PCR, only the upregulated expression of miR-484 was significantly different when comparing RRMS with HC after accounting for multiple comparisons to control for false discovery rate. Using a combination of miR-15b-5p, miR-451a and miR-584-5p in the reproducibility phase gave AUC 0.676 for discriminating between RRMS and HC. When SPMS and HC were compared, miR-484, miR-320a, miR-320b, miR-320c (all upregulated), miR-140-5p, miR-142-5p (both downregulated) remained significantly different after accounting for multiple group comparisons. A combination of let-7c-5p, miR-320a and miR-424-5p in the reproducibility phase resulted in AUC 0.706 for discriminating SPMS from HC. SPMS patients had significantly decreased miR-337-3p expression compared to RRMS patients in 3 of the 4 cohorts. A combination of miR-134-5p, miR-337-3p and miR-532-3p in the reproducibility phase yielded AUC 0.630 in discriminating RRMS vs. SPMS. In the disability correlation analysis, miR-320a, miR-337-3p, miR-199a-5p, and miR-142-5p correlated with the EDSS in the reproducibility phase cohort. In a previous study Vistbakka et al. (2017) studied miRNA expression in a validation phase with 31 PPMS patients, 31 SPMS patients, 21 HC and found using RT-PCR when the group including all MS patients was compared to HC, 5 miRNAs (miR-128-3p, miR-376c-3p, miR-26a-5p, miR-191-5p, miR-24-3p) were significantly upregulated (FC > 1.5), but after the Bonferroni correction (to reduce the chances of obtaining false-positive results) only the differences for 4 miRNAs (miR-128-3p, miR-376c-3p, miR-26a-5p, miR-191-5p) reached statistical significance. 5 miRNAs were significantly upregulated (miR-128-3p, miR-376c-3p, miR-26a-5p, miR-191-5p, miR-24-3p) in PPMS compared to HC, and after the Bonferroni correction, 4 of them (miR-128-3p, miR-376c-3p, miR-191-5p, miR-24-3p) remained statistically significant, with miR-191-5p showing the greatest upregulation (FC = 2.3). In SPMS, 3 miRNAs (miR-376c-3p, miR-26a-5p, miR-191-5p) were upregulated (FC > 1.5) compared to HC, but only miR-191-5p (FC = 1.6) remained statistically significant after the Bonferroni correction. Comparison between PPMS and SPMS showed that 2 miRNAs (miR-128-3p, miR-24-3p) were significantly upregulated in PPMS after the Bonferroni correction (miR-128-3p, FC = 1.5; miR-24-3p, FC = 1.5). By ROC analysis, miR-128-3p and miR-191-5p had high AUC values (0.727, sensitivity 0.645, specificity 0.714; and 0.808, sensitivity 0.742, specificity 0.810, respectively) indicating these two miRNAs to be fair tests for distinguishing PPMS from HC. Sharaf-Eldin et al. (2017) recruited 18 RRMS, 19 SPMS, 23 HC with none of the patients having received DMT for at least 3 weeks prior to study entry and found by RT-PCR that miR-145 and miR-223 were significantly upregulated in MS patients, but miR-326 did not differ, compared to HC. For RRMS patients, FC values for miR-145, miR-223 and miR-326 were 2.6, 2.7 and 3.1, respectively, while for SPMS patients FC values for miR-145, miR-223 and miR-326 were 1.4, 2.2 and 1.2, respectively. The FC value for miR-326 was significantly different between RRMS and SPMS. MS patients could be distinguished from HC by expression of miR-145 with AUC value 0.670 (sensitivity 0.730, specificity 0.609), and by expression of miR-223 with AUC value 0.702 (sensitivity 0.730, specificity 0.609). Combining miR-145 and miR-223 gave AUC value 0.713 (sensitivity 0.892, specificity 0.478). The EDSS or MSSS did not correlate significantly with the expression levels of any of the miRNAs or mRNAs investigated. Regarding treatments, there were no significant differences in expression levels of miR-145, miR-223, miR-326, SP1, and SMAD3. Regev et al. (2017) studied two cohorts of patients: cohort 1 comprised 29 RRMS, 7 SPMS, 5 PPMS, while cohort 2 comprised 66 RRMS, 10 SPMS, 3 PPMS, with levels of miRNAs measured by RT-PCR being examined in relation to findings of MRI scans to identify brain lesions, brain atrophy, and cervical spinal cord lesions and atrophy. Many of the patients received DMT at MRI especially in cohort 2. Although several miRNAs were associated with MRI outcome, none of these associations remained significant when correcting for multiple comparisons using false discovery rate. Several miRNAs showed significant associations with EDSS score in both cohorts. These associations for 7 miRNAs (miR-19a-3p, miR-101-3p, miR-30e-3p, miR-19b-3p, miR-29c-3p, miR-32-5p, miR-195-5p) remained significant after correcting for multiple comparisons using false discovery rate. All of these miRNAs except for miR-195-5p had a protective relationship shown by a higher miRNA expression being associated with lower severity of MRI-indicated involvement. MiR-195-5p had a pathogenic relationship shown by a higher miRNA expression being associated with greater severity of MRI-indicated involvement. In addition, Regev et al. (2016) studied 29 RRMS, 19 SPMS, 10 PPMS, 30 HC in a validation phase and by RT-PCR identified 6 miRNAs differentially expressed in MS compared to HC after correcting for multiple comparisons using false discovery rate: miR-320a, miR-486-5p, miR-320b, miR-25-3p, miR-140-3p (all upregulated) and let-7c-5p (downregulated). The findings remained unchanged after adjustment for age and gender. By ROC analysis, miR-320a had the highest AUC 0.707 for discriminating MS from HC. When all 6 miRNAs that were significant after correcting for multiple comparisons were combined, the AUC value increased to 0.795 for MS vs. HC. MiR-27a-3p and miR-376-3p were significantly upregulated in RRMS compared to SPMS. MiR-27a-3p had the highest AUC value (0.78) and only this miRNA remained significant after correcting for multiple comparisons. The results were the same after adjusting for age and gender. Also miR-199a-5p, and miR-142-5p were significantly correlated to EDSS score after correcting for multiple comparisons. The highest correlation to EDSS was with miR-199a-5p. In this study, patients had not received treatment in the past 1 month, 3 months or 6 months depending on the treatment. In a study of Epstein-Barr virus (EBV) associated with MS, Wang et al. (2017) examined the expression of EBV miRNAs using RT-PCR in 30 RRMS patients at relapse and 30 HC who had not received treatment within the previous 2 months. 20 EBV miRNAs were expressed in all samples, and expression of ebv-miR-BHRF1-2-5p and ebv-miR-BHRF1-3 was significantly increased in RRMS patients compared to HC (FC = 1.48 and 1.33, respectively), while the other 18 miRNAs showed no significant difference. The upregulated expression of ebv-miR-BHRF1-2-5p and ebv-miR-BHRF1-3 was associated positively with EDSS scores of RRMS patients. By ROC analysis, the AUC values for ebv-miR-BHRF1-2-5p and ebv-miR-BHRF1-3 for discriminating RRMS from HC were 0.74 and 0.72, respectively, while with a combination of the two miRNAs, the AUC value was 0.76.
-
4)
Exosomes isolated from serum: Selmaj et al. (2017) recruited 33 RRMS relapse, 30 RRMS remission and 32 HC in a validation set. All patients were sampled before methylprednisolone administration, and those in remission did not receive DMT for at least 6 months. By PCR, miR-122-5p, miR-196b-5p, miR-301a-3p, miR-532-5p were significantly downregulated in RRMS relapse patients compared to HC, while miR-122-5p was significantly downregulated in RRMS remission patients compared to HC. Furthermore, miR-122-5p, miR-196b-5p, miR-532-5p were significantly downregulated in RRMS relapse patients compared to RRMS remission patients. By ROC analysis, for miR-122-5p, miR-196b-5p, miR-301a-3p, miR-532-5p, AUC values were 0.878, 0.866, 0.681, 0.800, respectively, for discriminating between RRMS patients in relapse and HC. A combination of miR-122-5p and miR-196b-5p gave AUC 0.904 for discriminating RRMS relapse from HC and AUC 0.866 for distinguishing RRMS relapse from RRMS remission. Lower levels of miR-122-5p, miR-196b-5p, miR-301a-3p, miR-532-5p were related to disease activity. Niwald et al. (2017) studied 23 stable RRMS, 13 post-acute RRMS patients and 10 HC. The stable RRMS patients were in the remission phase, without treatment, for over 2 years without attacks or steroid treatment (late phase of remission). The post-acute RRMS patients were in the early phase of remission, 1 to 2 months free of intravenous injection of 5-day methyl-prednisolone (1000 mg/d). Using PCR, expression of miR-155 and miR-301a was decreased (in 94% and 51% samples, respectively) whereas expression of miR-326 was increased (in 72% samples) in RRMS patients. The difference in relative expression of miR-155 for RRMS patients compared to HC was statistically significant. Expression levels of miR-301a and miR-155 were higher in RRMS patients in post-acute vs. stable phase of remission. Significant differences in relative quantitation values between early vs. late phase of remission were found for miR-301a and miR-155. There was no significant difference in the expression level of miR-326. A positive correlation was found between relative expression of miR-326 and miR-301a and Beck Depression Index. On dividing RRMS patients into two subgroups based on their disability EDSS ≤ 5 and EDSS > 5, no significant differences were found in miR-155, miR-326 and miR-301a level of expression. Ebrahimkhani et al. (2017) using next generation sequencing in a validation study with 14 RRMS, 11 SPMS7/PPMS4 and 11 HC identified 4 significantly upregulated miRNAs for RRMS patients compared to HC (miR-15b-5p, miR-30b-5p, miR-342-3p, miR-451a). Also, 6 miRNAs were significantly upregulated in SPMS/PPMS patients compared to HC (miR-370-3p, miR-409-3p, miR-432-5p, miR-15b-5p, miR-223-3p, miR-23a-3p). Furthermore, 9 miRNAs were dysregulated in RRMS compared to SPMS/PPMS patients (miR-15b-5p, miR-23a-3p, miR-223-3p, miR-30b-5p, miR-342-3p, miR-374a-5p all upregulated, and miR-432-5p, miR-433-3p, miR-485-5p all downregulated). By ROC analysis, miR-451a had the highest AUC value (0.83) for distinguishing RRMS patients from HC, while miR-127-3p, miR-409-3p, miR-370-3p, miR-432-5p had AUC values 0.90, 0.91, 0.86, 0.90, respectively, for distinguishing SPMS/PPMS patients from HC. For distinguishing RRMS from SPMS/PPMS patients, miR-433-3p, miR-432-5p, miR-485-5p had AUC values 0.93, 0.86, 0.87, respectively.
-
5)
CSF: A validation study was performed by Quintana et al. (2017) involving 47 MS patients lipid-specific oligoclonal IgM bands negative (LS_OCMB-), 39 MS patients LS_OCMB+, and 55 other neurological diseases (OND) controls. All MS patients had McDonald 2010 RRMS form and none were receiving DMT. All MS patients were recruited at the beginning of the disease (most during the first year). Using RT-PCR, statistically significant differences in expression for MS vs. OND control were found for miR-328, miR-30a-5p, miR-150, miR-645 (all upregulated in MS) and miR-365, miR-21, miR-191, miR-199a-3p, miR-106a, miR-146a (all downregulated in MS). Four miRNAs showed significantly different expression in LS_OCMB+ vs. OND: miR-30a-5p, miR-150, miR-645 (upregulated in LS_OCMB+) and miR-191 (downregulated in LS_OCMB+). Two miRNAs had significantly different expression in LS_OCMB– vs. OND: miR-199a-3p and miR-106a (downregulated in LS_OCMB–). There were no significant differences for any miRNA between LS_OCMB+ and LS_OCMB–. By ROC analysis, miR-150 had the highest AUC value (0.684) for distinguishing MS patients from OND. Bergman et al. (2016) recruited two validation cohorts of patients: cohort 1 comprised 34 CIS, 43 MS, 34 noninflammatory neurologic disease controls (NINDC), 31 inflammatory neurologic disease controls (INDC), while cohort 2 constituted 96 CIS, 120 MS, 119 NINDC, 95 INDC. By RT-PCR, only miR-145 and miR-150 of the tested miRNAs were significantly different for MS compared to NINDC control in cohort 1. In the larger validation cohort 2, significantly higher levels of miR-150 in MS compared to both NINDC and INDC controls were replicated, as well as being significantly higher between CIS and NINDC. In addition, a significantly higher level of miR-145 for MS compared to NINDC was observed. Significantly higher miR-150 levels were found in CSF from CIS patients who subsequently converted to MS compared to those who did not convert during follow-up (median period of 52 months). By ROC analysis, miR-150 level discriminated MS patients in relapse/remission from NINDC controls with AUC value 0.744 (sensitivity 0.890, specificity 0.500). The ratio of miR-150 to miR-204 was significantly higher in MS compared to NINDC and INDC in cohort 2, as well as in patients with CIS who subsequently converted to MS compared to those who did not convert. The ratio of miR-150 to miR-204 had an AUC value of 0.811 (sensitivity 0.710, specificity 0.790) for differentiating MS from NINDC, and also an AUC value of 0.775 for differentiating patients with CIS who converted to MS from those who did not convert. Similar to the pair miR-150/miR-204, the pair miR-145/miR-204 also distinguished MS from NINDC. Ahlbrecht et al. (2016) recruited 28 CIS-CIS and 30 CIS-RRMS patients. CIS patients had a CIS disease status 1 year after CIS diagnosis or converted to RRMS within 1 year. A considerable proportion of CIS-CIS (36%) and CIS-RRMS (37%) patients received DMT. By RT-PCR, levels of miR-922 in CSF and serum were significantly higher in CIS-RRMS than CIS-CIS patients. While miR-181c levels in CSF were significantly higher in CIS-RRMS than CIS-CIS patients, there was no difference in serum levels of miR-181c between the two groups. No differences were found between CIS-CIS RRMS and CIS-CIS patients for miR-633 in both CSF and serum. In univariate Cox regression analyses, lower levels of CSF miR-181c and serum miR-922 were significantly associated with a lower risk of conversion from CIS to RRMS; none of the other miRNAs were significantly associated with conversion to RRMS. By ROC analysis, the AUC value of CSF miR-181c for distinguishing between CIS-CIS and CIS-RRMS patients was 0.67.
Those miRNAs that can be considered as biomarkers of MS and its subtypes in peripheral blood, blood serum, exosomes isolated from serum, and CSF are summarized (Table 3).
Table 3.
Alterations of miRNA expression in MS and its subtypes in peripheral blood, blood serum, exosomes isolated from serum, and CSF
| Author | Sample | Comparison | Altered miRNA expression |
|---|---|---|---|
| Nuzziello et al. (2018) | Peripheral blood | MS vs. HC | Upregulated: miR-320a (FC = 1.79), miR-125a-5p (FC = 1.89), miR-652-3p (FC = 1.51), miR-185-5p (FC = 1.5), miR-942-5p (FC = 1.67), miR-25-3p (FC = 1.49) |
| Vistbakka et al. (2017) | Blood serum | MS vs. HC | Upregulated: miR-128-3p, miR-376c-3p, miR-26a-5p, miR-191-5p |
| Sharaf-Eldin et al. (2017) | Blood serum | MS vs. HC | Upregulated: miR-145, miR-223 |
| Regev et al. (2016) | Blood serum | MS vs. HC | Upregulated: miR-320a, miR-486-5p, miR-320b, miR-25-3p, miR-140-3p Downregulated: let-7c-5p |
| Vistbakka et al. (2018) | Blood serum | RRMS vs. HC | Upregulated: miR-191-5p (FC = 1.65), miR-24-3p (FC = 2.10) |
| Regev et al. (2018) | Blood serum | RRMS vs. HC | Upregulated: miR-484 |
| Sharaf-Eldin et al. (2017) | Blood serum | RRMS vs. HC | Upregulated: miR-145 (FC = 2.6), miR-223 (FC = 2.7), miR-326 (FC = 3.1) |
| Wang et al. (2017) | Blood serum | RRMS vs. HC | Upregulated: ebv-miR-BHRF1-2-5p (FC = 1.48), ebv-miR-BHRF1-3 (FC = 1.33) |
| Regev et al. (2018) | Blood serum | SPMS vs. HC | Upregulated: miR-484, miR-320a, miR-320b, miR-320c Downregulated: miR-140-5p, miR-142-5p |
| Vistbakka et al. (2017) | Blood serum | SPMS vs. HC | Upregulated: miR-191-5p (FC = 1.6) |
| Sharaf-Eldin et al. (2017) | Blood serum | SPMS vs. HC | Upregulated: miR-145 (FC = 1.4), miR-223 (FC = 2.2), miR-326 (FC = 1.2) |
| Vistbakka et al. (2018) | Blood serum | PPMS vs. HC | Upregulated: miR-191-5p (FC = 1.75), miR-24-3p (FC = 3.58) |
| Vistbakka et al. (2017) | Blood serum | PPMS vs. HC | Upregulated: miR-128-3p, miR-376c-3p, miR-24-3p, miR-191-5p (FC = 2.3) |
| Sharaf-Eldin et al. (2017) | Blood serum | RRMS vs. SPMS | Upregulated: miR-326 |
| Regev et al. (2016) | Blood serum | RRMS vs. SPMS | Upregulated: miR-27a-3p |
| Vistbakka et al. (2017) | Blood serum | PPMS vs. SPMS | Upregulated: miR-128-3p (FC = 1.5), miR-24-3p (FC = 1.5) |
| Ebrahimkhani et al. (2017) | Exosomes of blood serum | RRMS vs. HC | Upregulated: miR-15b-5p, miR-30b-5p, miR-342-3p, miR-451a |
| Niwald et al. (2017) | Exosomes of blood serum | RRMS vs. HC | Downregulated: miR-155 |
| Ebrahimkhani et al. (2017) | Exosomes of blood serum | SPMS/PPMS vs. HC | Upregulated: miR-370-3p, miR-409-3p, miR-432-5p, miR-15b-5p, miR-223-3p, miR-23a-3p |
| Ebrahimkhani et al. (2017) | Exosomes of blood serum | RRMS vs. SPMS/PPPMS | Upregulated: miR-15b-5p, miR-23a-3p, miR-223-3p, miR-30b-5p, miR-342-3p, miR-374a-5p Downregulated: miR-432-5p, miR-433-3p, miR-485 |
| Selmaj et al. (2017) | Exosomes of blood serum | RRMS relapse vs. HC | Downregulated: miR-122-5p, miR-196b-5p, miR-301a-3p, miR-532-5p |
| Selmaj et al. (2017) | Exosomes of blood serum | RRMS remission vs. HC | Downregulated: miR-122-5p |
| Selmaj et al. (2017) | Exosomes of blood serum | RRMS relapse vs. RRMS remission | Downregulated: miR-122-5p, miR-196b-5p, miR-532-5p |
| Quintana et al. (2017) | CSF | MS vs. OND | Upregulated: miR-328, miR-30a-5p, miR-150, miR-645 Downregulated: miR-365, miR-21, miR-191, miR-199a-3p, miR-106a, miR-146a |
| Bergman et al. (2016) | CSF | MS vs. NINDC | Upregulated: miR-150, miR-145 |
| Bergman et al. (2016) | CSF | CIS vs. INDC | Upregulated: miR-150 |
| Bergman et al. (2016) | CSF | CIS-MS vs. CIS-CIS | Upregulated: miR-150 |
| Ahlbrecht et al. (2016) | CSF | CIS-RRMS vs. CIS-CIS | Upregulated: miR-922, miR-181c |
CIS: Clinically isolated syndrome; CSF: cerebrospinal fluid; FC: fold change; HC: healthy controls; INDC: inflammatory neurologic disease controls; MS: multiple sclerosis; NINDC: noninflammatory neurologic disease controls; OND: other neurological diseases; PPMS: primary-progressive MS; RRMS: relapsing-remitting MS; SPMS: secondary-progressive MS.
Discussion
MS is a chronic inflammatory demyelinating and neurodegenerative disease of the CNS. Genetic, epigenetic, and environmental factors are likely involved in its susceptibility and/or outcomes (Oksenberg and Baranzini, 2010). The disease onset typically occurs in young adults, especially females, although diagnosis during childhood and adolescence has been increasingly reported worldwide. In RRMS, inflammation together with blood-brain barrier damage is the key mechanism in the initiation of the disease process. In SPMS and PPMS, inflammation-promoting effects become decreased over time while neurodegenerative events are increased by mechanisms such as oxidative stress and mitochondrial damage, followed by intracellular influx of Na+ and Ca2+ leading to cell death. Widespread diffuse inflammation with slowly expanding lesions and abundant cortical lesions, as well as lymphocyte infiltration and microglia activation in the normal-appearing white matter, is characteristic of the pathology of progressive phenotypes (Vistbakka et al., 2017).
MiRNAs are involved in neurogenesis, oligodendrocyte differentiation, neurite outgrowth, and myelin formation (Dugas et al., 2010; de Faria et al., 2012; Zhao et al., 2010). Alterations in miRNA expression have been reported in various pathologies (Esteller, 2011), particularly those associated with inflammation and immune function (O’Connell et al., 2012; Singh et al., 2013). In addition, abnormal expression of several components of the miRNA production pathway has been found in various diseases (Divekar et al., 2011; Gascon and Gao, 2012). Overexpression of Dicer mRNA in peripheral blood leukocytes was shown in MS (Jafari et al., 2015). Also decreased Dicer protein in B cells from MS patients has been observed (Aung and Balashov, 2015). Dicer expression is required for normal development of oligodendrocytes (Shin et al., 2009). Protecting oligodendrocytes from further injury and promoting remyelination may be a feasible way of improving clinical outcome in MS patients in the near future (Rodgers et al., 2013; Dulamea, 2017).
Previous studies had constructed molecular networks by integrating dysregulated miRNAs and miRNA targets from target gene prediction databases (Angerstein et al., 2012; Hecker et al., 2013; Jernås et al., 2013). Most were performed using small patient cohort sizes without technical replicates and independent validation (Kemppinen et al., 2011). Thus, it is possible that some of the findings are false positives. In addition, these studies were conducted using different samples or tissues (e.g., peripheral blood or isolated cells), different technological microarray platforms, and different statistical methods to analyze the data. Consequently, little overlap in expression of dysregulated miRNAs was observed between the various studies (Kemppinen et al., 2011).
The recent studies reviewed here have shown that miRNAs in blood, especially in blood serum and exosomes isolated from serum (Table 1) and in CSF (Table 2) can serve to distinguish MS patients from controls. In addition, miRNAs in CSF are altered in CIS patients compared to controls and distinguish CIS patients who subsequently convert to MS from those that do not convert (Table 2). The expression levels of a large number of miRNAs have been found to be altered in MS and its subtypes (RRMS, SPMS, PPMS) compared to HC and other neurologic diseases and also in CIS compared to controls (Table 3), and by ROC AUC analysis have been shown to distinguish the disease subtypes from HC and each other. Thus, these miRNAs have the potential to serve as diagnostic markers for the disease and to distinguish between its subtypes. Apart from two studies that had employed next generation sequencing, all of the studies reviewed had used PCR to validate the findings from discovery or screening sets. In addition, there were indications of overlap in the results from the different research groups and this included miRNAs such as miR-320a and miR-25-3p (upregulated in peripheral blood and blood serum of MS patients vs. HC), miR-191-5p and miR-145 (upregulated in blood serum and CSF of MS patients vs. controls), miR-223 (upregulated in blood serum and exosomes of SPMS patients vs. controls). While MS patients in several studies had received DMT therapy, no statistically significant differences in miRNA expression levels were found between untreated and treated patients in two of the studies (Sharaf-Eldin et al. 2017; Vistbakka et al. 2018). Clearly the use of similar analytical procedures by the various research groups for detecting and quantifying miRNAs levels has assisted in increasing the levels of similarity between findings. However, while there was agreement with some findings on miRNA expression in previous studies including upregulation of miR-145 in plasma of MS patients (Søndergaard et al., 2013) and serum of MS patients (Sharaf-Eldin et al., 2017), there were also some differences. For example, a downregulation of miR-15b, miR-23a and miR-223 in serum of both RRMS and PPMS was reported in a previous study (Fenoglio et al., 2013), whereas an upregulation of miR-15b-5p was found in exosomes from serum for RRMS and SPMS/PPMS and of miR-23a-3p in exosomes from serum for SPMS/PPMS (Ebrahimkhani et al., 2017) and an upregulation of miR-223 in serum of RRMS and SPMS was observed (Sharaf-Eldin et al., 2017). This lack of agreement could possibly be due to differences in selection/recruitment of patients and possibly being at different stages of MS (relapse vs. remission, early vs. late phase of remission), technologies, analytical procedures, and/or statistical methods, of which the latter in the recent studies were very rigorous and often involved several statistical tests and Bonferroni corrections for false positives. Exosomal miRNA analysis has been considered to provide a more robust and different data set than an analysis of serum miRNAs (Backes et al., 2016; Selmaj et al., 2017). Gallo et al. (2012) reported that the majority of miRNAs detectable in serum were concentrated in exosomes, and with the concentration of miRNA in whole, unfractionated serum being between that of the exosomal pellet and the exosome-depleted serum supernatant.
Several of the serum miRNAs had high FC values, for example miR-24-3p (FC = 3.58, 2.10), miR-326 (FC = 3.1), miR-191-5p (FC = 2.3). These help to indicate those miRNAs that can serve as markers and provide a quantitative aspect to the results that are more often expressed only qualitatively as increased or decreased expression. Regarding the functionality of these miRNAs, miR-24 appears to promote pro-apoptotic effects (Zhou and Zhang, 2014) and inhibits interferon-γ (Fayyad-Kazan et al., 2014) and interleukin (IL)-4 expressions (Pua et al., 2016) suggesting a role in the regulation of Th1/Th2 cell balance, thereby regulating inflammatory responses. MiR-326 promotes the differentiation of Th17 cells, which are IL-17 producing T helper CD4+ cells, by targeting Ets-1, a negative regulator of Th17 differentiation. In MS patients, miR-326 was positively correlated with IL-17 production, and this might be associated with chronic autoimmune diseases (Tzartos et al., 2008; Du et al., 2009). During the course of MS, miR-326-mediated downregulation of CD47 mRNA results in reduced interaction of CD47 with the signal regulatory protein alpha, thus promoting phagocytosis of myelin by macrophages (Koning et al., 2007; Junker et al., 2009). MiR-191 regulates cytokine-dependent naïve, memory, and regulatory T cell survival and thereby maintains immune homeostasis by controlling levels of insulin receptor substrate 1 (Lykken and Li, 2016). Interestingly, miR-326 had increased expression in exosomes isolated from serum of RRMS patients, and was reported to be increased in MS brains (Junker et al., 2009). A reduction of symptoms occurred in experimental autoimmune encephalomyelitis, a model system for MS, in mice lacking miR-326 by in vivo silencing (Junker, 2011). Also downregulation of miR-326 by its specific inhibitor (lentivirus-sponge) led to an improved experimental autoimmune encephalomyelitis score through inhibition of Th17 differentiation (Du et al., 2009).
Expression of miRNAs is controlled by genetic and epigenetic mechanisms. MiRNAs can be epigenetically regulated by DNA methylation and/or specific histone modifications (Moutinho and Esteller, 2017). Moreover, epigentic mechanisms regulate the human leukocyte antigen-DRB1*15 allele, which is linked to MS disease and possibly one of the reasons why MS is more often transmitted to offspring by mothers than fathers (Küçükali et al., 2015). Vitamin D deficiency, smoking and EBV are major environmental factors for MS and are all known to exert epigenetic changes. Epigenetic mechanisms could regulate axonal loss, apoptosis, and mitochondrial dysfunction in MS (Küçükali et al., 2015).
Further studies are warranted by other research groups to independently validate the findings in this review so that single miRNAs or pairs of miRNAs in blood serum and CSF can be used as diagnostic markers for adult onset and PedMS and for monitoring disease progression and response to therapy. Also the functionality of those miRNAs that best discriminate MS and its subtypes from controls needs to be investigated.
Footnotes
Conflicts of interest: There are no conflicts of interest.
Financial support: None.
Copyright license agreement: The Copyright License Agreement has been signed by both authors before publication.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
C-Editors: Zhao M, Li JY; T-Editor: Jia Y
References
- 1.Ahlbrecht J, Martino F, Pul R, Skripuletz T, Sühs KW, Schauerte C, Yildiz Ö, Trebst C, Tasto L, Thum S, Pfanne A, Roesler R, Lauda F, Hecker M, Zettl UK, Tumani H, Thum T, Stangel M. Deregulation of microRNA-181c in cerebrospinal fluid of patients with clinically isolated syndrome is associated with early conversion to relapsing-remitting multiple sclerosis. Mult Scler. 2016;22:1202–1214. doi: 10.1177/1352458515613641. [DOI] [PubMed] [Google Scholar]
- 2.Alroughani R, Boyko A. Pediatric multiple sclerosis: a review. BMC Neurol. 2018;18:27. doi: 10.1186/s12883-018-1026-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Angerstein C, Hecker M, Paap BK, Koczan D, Thamilarasan M, Thiesen HJ, Zettl UK. Integration of microRNA databases to study microRNAs associated with multiple sclerosis. Mol Neurobiol. 2012;45:520–535. doi: 10.1007/s12035-012-8270-0. [DOI] [PubMed] [Google Scholar]
- 4.Asirvatham AJ, Gregorie CJ, Hu Z, Magner WJ, Tomasi TB. MicroRNA targets in immune genes and the Dicer/Argonaute and ARE machinery components. Mol Immunol. 2008;45:1995–2006. doi: 10.1016/j.molimm.2007.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aung LL, Balashov KE. Decreased Dicer expression is linked to increased expression of co-stimulatory molecule CD80 on B cells in multiple sclerosis. Mult Scler. 2015;21:1131–1138. doi: 10.1177/1352458514560923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Backes C, Meese E, Keller A. Specific miRNA disease biomarkers in blood, serum and plasma: challenges and prospects. Mol Diagn Ther. 2016;20:509–518. doi: 10.1007/s40291-016-0221-4. [DOI] [PubMed] [Google Scholar]
- 7.Bayer US. Multiple Sclerosis MS. 2018. [accessed 1 March 2019]. https://www.multiplesclerosiscom/us/treatment .
- 8.Belbasis L, Bellou V, Evangelou E, Ioannidis JP, Tzoulaki I. Environmental risk factors and multiple sclerosis: an umbrella review of systematic reviews and meta-analyses. Lancet Neurol. 2015;14:263–273. doi: 10.1016/S1474-4422(14)70267-4. [DOI] [PubMed] [Google Scholar]
- 9.Benson LA, Healy BC, Gorman MP, Baruch NF, Gholipour T, Musallam A, Chitnis T. Elevated relapse rates in pediatric compared to adult MS persist for at least 6 years. Mult Scler Relat Dis. 2014;3:186–193. doi: 10.1016/j.msard.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 10.Bergman P, Piket E, Khademi M, James T, Brundin L, Olsson T, Piehl F, Jagodic M. Circulating miR-150 in CSF is a novel candidate biomarker for multiple sclerosis. Neurol Neuroimmunol Neuroinflamm. 2016;3:e219. doi: 10.1212/NXI.0000000000000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernhardt K, Haar J, Tsai MH, Poirey R, Feederle R, Delecluse HJ. A viral microRNA cluster regulates the expression of PTEN, p27 and of a bcl-2 homolog. PLoS Pathog. 2016;12:e1005405. doi: 10.1371/journal.ppat.1005405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boiko A, Vorobeychik G, Paty D, Devonshire V, Sadovnick D. Early onset multiple sclerosis: a longitudinal study. Neurology. 2002;59:1006–1010. doi: 10.1212/wnl.59.7.1006. [DOI] [PubMed] [Google Scholar]
- 13.Catalanotto C, Cogoni C, Zardo G. MicroRNA in control of gene expression: An overview of nuclear functions. Int J Mol Sci. 2016;17:1712. doi: 10.3390/ijms17101712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Faria O, Jr, Moore CS, Kennedy TE, Antel JP, Bar-Or A, Dhaunchak AS. MicroRNA dysregulation in multiple sclerosis. Front Genet. 2012;3:311. doi: 10.3389/fgene.2012.00311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Divekar AA, Dubey S, Gangalum PR, Singh RR. Dicer insufficiency and microRNA-155 overexpression in lupus regulatory T cells: an apparent paradox in the setting of an inflammatory milieu. J Immunol. 2011;186:924–930. doi: 10.4049/jimmunol.1002218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Du C, Liu C, Kang J, Zhao G, Ye Z, Huang S, Li Z, Wu Z, Pei G. MicroRNA miR-326 regulates TH-17 differentiation and is associated with the pathogenesis of multiple sclerosis. Nat Immunol. 2009;10:1252–1259. doi: 10.1038/ni.1798. [DOI] [PubMed] [Google Scholar]
- 17.Dugas JC, Cuellar TL, Scholze A, Ason B, Ibrahim A, Emery B, Zamanian JL, Foo LC, McManus MT, Barres BA. Dicer1 and miR-219 are required for normal oligodendrocyte differentiation and myelination. Neuron. 2010;65:597–611. doi: 10.1016/j.neuron.2010.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dulamea AO. The contribution of oligodendrocytes and oligodendrocyte progenitor cells to central nervous system repair in multiple sclerosis: perspectives for remyelination therapeutic strategies. Neural Regen Res. 2017;12:1939–1944. doi: 10.4103/1673-5374.221146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ebrahimkhani S, Vafaee F, Young PE, Hur SSJ, Hawke S, Devenney E, Beadnall H, Barnett MH, Suter CM, Buckland ME. Exosomal microRNA signatures in multiple sclerosis reflect disease status. Sci Rep. 2017;7:14293. doi: 10.1038/s41598-017-14301-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Esteller M. Non-coding RNAs in human disease. Nat Rev Genet. 2011;12:861–874. doi: 10.1038/nrg3074. [DOI] [PubMed] [Google Scholar]
- 21.Fawaz CN, Makki IS, Kazan JM, Gebara NY, Andary FS, Itani MM, El-Sayyed M, Zeidan A, Quartarone A, Darwish H, Mondello S. Neuroproteomics and microRNAs studies in multiple sclerosis: transforming research and clinical knowledge in biomarker research. Expert Rev Proteomics. 2015;12:637–650. doi: 10.1586/14789450.2015.1099435. [DOI] [PubMed] [Google Scholar]
- 22.Fayyad-Kazan H, Hamade E, Rouas R, Najar M, Fayyad-Kazan M, El Zein N, ElDirani R, Hussein N, Fakhry M, Al-Akoum C, Burny A, Martiat P, Badran B. Downregulation of microRNA-24 and -181 parallels the upregulation of IFN-γ secreted by activated human CD4 lymphocytes. Hum Immunol. 2014;75:677–685. doi: 10.1016/j.humimm.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 23.Fenoglio C, Ridolfi E, Cantoni C, De Riz M, Bonsi R, Serpente M, Villa C, Pietroboni AM, Naismith RT, Alvarez E, Parks BJ, Bresolin N, Cross AH, Piccio LM, Galimberti D, Scarpini E. Decreased circulating miRNA levels in patients with primary progressive multiple sclerosis. Mult Scler. 2013;19:1938–1942. doi: 10.1177/1352458513485654. [DOI] [PubMed] [Google Scholar]
- 24.Gallo A, Tandon M, Alevizos I, Illei GG. The majority of microRNAs detectable in serum and saliva is concentrated in exosomes. PLoS One. 2012;7:e30679. doi: 10.1371/journal.pone.0030679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gandhi R, Healy B, Gholipour T, Egorova S, Musallam A, Hussain MS, Nejad P, Patel B, Hei H, Khoury S, Quintana F, Kivisakk P, Chitnis T, Weiner HL. Circulating microRNAs as biomarkers for disease staging in multiple sclerosis. Ann Neurol. 2013;73:729–740. doi: 10.1002/ana.23880. [DOI] [PubMed] [Google Scholar]
- 26.Gascon E, Gao FB. Cause or effect: misregulation of microRNA pathways in neurodegeneration. Front Neurosci. 2012;6:48. doi: 10.3389/fnins.2012.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Geurts JJ, Calabrese M, Fisher E, Rudick RA. Measurement and clinical effect of grey matter pathology in multiple sclerosis. Lancet Neurol. 2012;11:1082–1092. doi: 10.1016/S1474-4422(12)70230-2. [DOI] [PubMed] [Google Scholar]
- 28.Gewies A, Gorka O, Bergmann H, Pechloff K, Petermann F, Jeltsch KM, Rudelius M, Kriegsmann M, Weichert W, Horsch M, Beckers J, Wurst W, Heikenwalder M, Korn T, Heissmeyer V, Ruland J. Uncoupling Malt1 threshold function from paracaspase activity results in destructive autoimmune inflammation. Cell Rep. 2014;9:1292–1305. doi: 10.1016/j.celrep.2014.10.044. [DOI] [PubMed] [Google Scholar]
- 29.Haghikia A, Haghikia A, Hellwig K, Baraniskin A, Holzmann A, Décard BF, Thum T, Gold R. Regulated microRNAs in the CSF of patients with multiple sclerosis: a case-control study. Neurology. 2012;79:2166–2170. doi: 10.1212/WNL.0b013e3182759621. [DOI] [PubMed] [Google Scholar]
- 30.Harris VK, Tuddenham JF, Sadiq SA. Biomarkers of multiple sclerosis: current findings. Degener Neurol Neuromuscul Dis. 2017;7:19–29. doi: 10.2147/DNND.S98936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hecker M, Thamilarasan M, Koczan D, Schröder I, Flechtner K, Freiesleben S, Füllen G, Thiesen HJ, Zettl UK. MicroRNA expression changes during interferon-beta treatment in the peripheral blood of multiple sclerosis patients. Int J Mol Sci. 2013;14:16087–16110. doi: 10.3390/ijms140816087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Housley WJ, Pitt D, Hafler DA. Biomarkers in multiple sclerosis. Clin Immunol. 2015;161:51–58. doi: 10.1016/j.clim.2015.06.015. [DOI] [PubMed] [Google Scholar]
- 33.Huang Q, Xiao B, Ma X, Qu M, Li Y, Nagarkatti P, Nagarkatti M, Zhou J. MicroRNAs associated with the pathogenesis of multiple sclerosis. J Neuroimmunol. 2016;295-296:148–161. doi: 10.1016/j.jneuroim.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 34.Jafari N, Shaghaghi H, Mahmoodi D, Shirzad Z, Alibeiki F, Bohlooli S, Dogaheh HP. Overexpression of microRNA biogenesis machinery: Drosha, DGCR8 and Dicer in multiple sclerosis patients. J Clin Neurosci. 2015;22:200–203. doi: 10.1016/j.jocn.2014.06.106. [DOI] [PubMed] [Google Scholar]
- 35.Jaworski M, Marsland BJ, Gehrig J, Held W, Favre S, Luther SA, Perroud M, Golshayan D, Gaide O, Thome M. Malt1 protease inactivation efficiently dampens immune responses but causes spontaneous autoimmunity. EMBO J. 2014;33:2765–2781. doi: 10.15252/embj.201488987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jernås M, Malmeström C, Axelsson M, Nookaew I, Wadenvik H, Lycke J, Olsson B. MicroRNA regulate immune pathways in T-cells in multiple sclerosis (MS) BMC Immunol. 2013;14:32. doi: 10.1186/1471-2172-14-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Junker A. Pathophysiology of translational regulation by microRNAs in multiple sclerosis. FEBS Lett. 2011;585:3738–3746. doi: 10.1016/j.febslet.2011.03.052. [DOI] [PubMed] [Google Scholar]
- 38.Junker A, Krumbholz M, Eisele S, Mohan H, Augstein F, Bittner R, Lassmann H, Wekerle H, Hohlfeld R, Meinl E. MicroRNA profiling of multiple sclerosis lesions identifies modulators of the regulatory protein CD47. Brain. 2009;132:3342–3352. doi: 10.1093/brain/awp300. [DOI] [PubMed] [Google Scholar]
- 39.Kacperska MJ, Jastrzebski K, Tomasik B, Walenczak J, Konarska-Krol M, Glabinski A. Selected extracellular microRNAs as potential biomarkers of multiple sclerosis activity -preliminary study. J Mol Neurosci. 2015;56:154–163. doi: 10.1007/s12031-014-0476-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kappos L, Polman CH, Freedman MS, Edan G, Hartung HP, Miller DH, Montalban X, Barkhof F, Bauer L, Jakobs P, Pohl C, Sandbrink R. Treatment with interferon beta-1b delays conversion to clinically definite and McDonald MS in patients with clinically isolated syndromes. Neurology. 2006;67:1242–1249. doi: 10.1212/01.wnl.0000237641.33768.8d. [DOI] [PubMed] [Google Scholar]
- 41.Katz Sand I. Classification, diagnosis, and differential diagnosis of multiple sclerosis. Curr Opin Neurol. 2015;28:193–205. doi: 10.1097/WCO.0000000000000206. [DOI] [PubMed] [Google Scholar]
- 42.Kemppinen AK, Kaprio J, Palotie A, Saarela J. Systematic review of genome-wide expression studies in multiple sclerosis. BMJ Open. 2011;1:e000053. doi: 10.1136/bmjopen-2011-000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Koning N, Bö L, Hoek RM, Huitinga I. Downregulation of macrophage inhibitory molecules in multiple sclerosis lesions. Ann Neurol. 2007;62:504–514. doi: 10.1002/ana.21220. [DOI] [PubMed] [Google Scholar]
- 44.Küçükali Cİ, Kürtüncü M, Çoban A, Çebi M, Tüzün E. Epigenetics of multiple sclerosis: an updated review. Neuromolecular Med. 2015;17:83–96. doi: 10.1007/s12017-014-8298-6. [DOI] [PubMed] [Google Scholar]
- 45.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33:1444–1452. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 46.Kurtzke JF. On the origin of EDSS. Mult Scler Relat Disord. 2015;4:95–103. doi: 10.1016/j.msard.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 47.Kutzelnigg A, Lassmann H. Pathology of multiple sclerosis and related inflammatory demyelinating diseases. Handb Clin Neurol. 2014;122:15–58. doi: 10.1016/B978-0-444-52001-2.00002-9. [DOI] [PubMed] [Google Scholar]
- 48.Lee JY, Park JK, Lee EY, Lee EB, Song YW. Circulating exosomes from patients with systemic lupus erythematosus induce a proinflammatory immune response. Arthritis Res Ther. 2016;18:264. doi: 10.1186/s13075-016-1159-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liguori M, Nuzziello N, Licciulli F, Consiglio A, Simone M, Viterbo RG, Creanza TM, Ancona N, Tortorella C, Margari L, Grillo G, Giordano P, Liuni S, Trojano M. Combined microRNA and mRNA expression analysis in pediatric multiple sclerosis: an integrated approach to uncover novel pathogenic mechanisms of the disease. Hum Mol Genet. 2018;27:66–79. doi: 10.1093/hmg/ddx385. [DOI] [PubMed] [Google Scholar]
- 50.Long H, Wang X, Chen Y, Wang L, Zhao M, Lu Q. Dysregulation of microRNAs in autoimmune diseases: Pathogenesis, biomarkers and potential therapeutic targets. Cancer Lett. 2018;428:90–103. doi: 10.1016/j.canlet.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 51.Lublin FD, Reingold SC Defining the clinical course of multiple sclerosis: results of an international survey. National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in Multiple Sclerosis. Neurology. 1996;46:907–911. doi: 10.1212/wnl.46.4.907. [DOI] [PubMed] [Google Scholar]
- 52.Lykken EA, Li QJ. The microRNA miR-191 supports T cell survival following common γ chain signaling. J Biol Chem. 2016;291:23532–23544. doi: 10.1074/jbc.M116.741264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lytle JR, Yario TA, Steitz JA. Target mRNAs are repressed as efficiently by microRNA-binding sites in the 5’ UTR as in the 3’ UTR. Proc Natl Acad Sci U S A. 2007;104:9667–9672. doi: 10.1073/pnas.0703820104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Magner WJ, Weinstock-Guttman B, Rho M, Hojnacki D, Ghazi R, Ramanathan M, Tomasi TB. Dicer and microRNA expression in multiple sclerosis and response to interferon therapy. J Neuroimmunol. 2016;292:68–78. doi: 10.1016/j.jneuroim.2016.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Martello G, Rosato A, Ferrari F, Manfrin A, Cordenonsi M, Dupont S, Enzo E, Guzzardo V, Rondina M, Spruce T, Parenti AR, Daidone MG, Bicciato S, Piccolo S. A MicroRNA targeting dicer for metastasis control. Cell. 2010;141:1195–1207. doi: 10.1016/j.cell.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 56.Momen-Heravi F, Saha B, Kodys K, Catalano D, Satishchandran A, Szabo G. Increased number of circulating exosomes and their microRNA cargos are potential novel biomarkers in alcoholic hepatitis. J Transl Med. 2015;13:261. doi: 10.1186/s12967-015-0623-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Moutinho C, Esteller M. MicroRNAs and epigenetics. Adv Cancer Res. 2017;135:189–220. doi: 10.1016/bs.acr.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 58.Multiple Sclerosis Trust. Prevalence and incidence of multiple sclerosis. 2018. [accessed 1 March 2019]. https://www.mstrust.org.uk/a-z/prevalence-and-incidence-multiple-sclerosis .
- 59.National MS Society, Just the facts. [accessed 1 March 2019]. https://www.nationalmssociety.org/nationalmssociety/media/msnationalfiles/brochures/brochure-just-the-facts.pdf .
- 60.National MS Society, Who gets MS? Epidemiology. [accessed March 1 March 2019]. https://www.nationalmssociety.org/What-is-MS/Who-Gets-MS .
- 61.Niwald M, Migdalska-Sęk M, Brzeziańska-Lasota E, Miller E. Evaluation of selected microRNAs expression in remission phase of multiple sclerosis and their potential link to cognition, depression, and disability. J Mol Neurosci. 2017;63:275–282. doi: 10.1007/s12031-017-0977-y. [DOI] [PubMed] [Google Scholar]
- 62.Nuzziello N, Vilardo L, Pelucchi P, Consiglio A, Liuni S, Trojano M, Liguori M. Investigating the role of microRNA and transcription factor co-regulatory networks in multiple sclerosis pathogenesis. Int J Mol Sci. 2018;19:3652. doi: 10.3390/ijms19113652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.O’Connell RM, Rao DS, Baltimore D. microRNA regulation of inflammatory responses. Annu Rev Immunol. 2012;30:295–312. doi: 10.1146/annurev-immunol-020711-075013. [DOI] [PubMed] [Google Scholar]
- 64.Oksenberg JR, Baranzini SE. Multiple sclerosis genetics- is the glass half full, or half empty? Nat Rev Neurol. 2010;6:429–437. doi: 10.1038/nrneurol.2010.91. [DOI] [PubMed] [Google Scholar]
- 65.Olsson T, Barcellos LF, Alfredsson L. Interactions between genetic, lifestyle and environmental risk factors for multiple sclerosis. Nat Rev Neurol. 2017;13:25–36. doi: 10.1038/nrneurol.2016.187. [DOI] [PubMed] [Google Scholar]
- 66.Paul A, Comabella M, Gandhi R. Biomarkers in multiple sclerosis. Cold Spring Harb Perspect Med. 2019 doi: 10.1101/cshperspect.a029058. doi: 101101/cshperspecta029058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pender MP, Burrows SR. Epstein-Barr virus and multiple sclerosis: potential opportunities for immunotherapy. Clin Transl Immunology. 2014;3:e27. doi: 10.1038/cti.2014.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Peplow PV, Martinez B, Calin GA, Esquela-Kerscher A. MicroRNAs in Diseases and Disorders: Emerging Therapeutic Targets. London, UK: Royal Society of Chemistry Publishing; 2019. [Google Scholar]
- 69.Peterson MF, Otoc N, Sethi JK, Gupta A, Antes TJ. Integrated systems for exosome investigation. Methods. 2015;87:31–45. doi: 10.1016/j.ymeth.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 70.Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, Fujihara K, Havrdova E, Hutchinson M, Kappos L, Lublin FD, Montalban X, O’Connor P, Sandberg-Wollheim M, Thompson AJ, Waubant E, Weinshenker B, Wolinsky JS. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011;69:292–302. doi: 10.1002/ana.22366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pua HH, Steiner DF, Patel S, Gonzalez JR, Ortiz-Carpena JF, Kageyama R, Chiou NT, Gallman A, de Kouchkovsky D, Jeker LT, McManus MT, Erle DJ, Ansel KM. MicroRNAs 24 and 27 suppress allergic inflammation and target a network of regulators of T helper 2 cell-associated cytokine production. Immunity. 2016;44:821–832. doi: 10.1016/j.immuni.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pusic AD, Pusic KM, Kraig RP. What are exosomes and how can they be used in multiple sclerosis therapy. Expert Rev Neurother. 2014;14:353–355. doi: 10.1586/14737175.2014.890893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Quintana E, Ortega FJ, Robles-Cedeño R, Villar ML, Buxó M, Mercader JM, Alvarez-Cermeño JC, Pueyo N, Perkal H, Fernández-Real JM, Ramió-Torrentà L. miRNAs in cerebrospinal fluid identify patients with MS and specifically those with lipid-specific oligoclonal IgM bands. Mult Scler. 2017;23:1716–1726. doi: 10.1177/1352458516684213. [DOI] [PubMed] [Google Scholar]
- 74.Regev K, Healy BC, Khalid F, Paul A, Chu R, Tauhid S, Tummala S, Diaz-Cruz C, Raheja R, Mazzola MA, von Glehn F, Kivisakk P, Dupuy SL, Kim G, Chitnis T, Weiner HL, Gandhi R, Bakshi R. Association between serum microRNAs and magnetic resonance imaging measures of multiple sclerosis severity. JAMA Neurol. 2017;74:275–285. doi: 10.1001/jamaneurol.2016.5197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Regev K, Healy BC, Paul A, Diaz-Cruz C, Mazzola A, Raheja R, Glanz BI, Kivisakk P, Chitnis T, Jagodic M, Piehl F, Olsson T, Khademi M, Hauser S, Oksenberg J, Khoury SJ, Weiner HL, Gandhi R. Identification of MS-specific serum miRNAs in an international multicenter study. Neurol Neuroimmunol Neuroinflamm. 2018;5:e491. doi: 10.1212/NXI.0000000000000491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Regev K, Paul A, Healy B, von Glenn F, Diaz-Cruz C, Gholipour T, Mazzola MA, Raheja R, Nejad P, Glanz BI, Kivisakk P, Chitnis T, Weiner HL, Gandhi R. Comprehensive evaluation of serum microRNAs as biomarkers in multiple sclerosis. Neurol Neuroimmunol Neuroinflamm. 2016;3:e267. doi: 10.1212/NXI.0000000000000267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Reiber H. Cerebrospinal fluid – physiology, analysis and interpretation of protein patterns for diagnosis of neurological diseases. Mult Scler. 1998;4:99–107. doi: 10.1177/135245859800400302. [DOI] [PubMed] [Google Scholar]
- 78.Renoux C, Vukusic S, Mikaeloff Y, Edan G, Clanet M, Dubois B, Debouverie M, Brochet B, Lebrun-Frenay C, Pelletier J, Moreau T, Lubetzki C, Vermersch P, Roullet E, Magy L, Tardieu M, Suissa S, Confavreux C. Natural history of multiple sclerosis with childhood onset. N Eng J Med. 2007;356:2603–2613. doi: 10.1056/NEJMoa067597. [DOI] [PubMed] [Google Scholar]
- 79.Rodgers JM, Robinson AP, Miller SD. Strategies for protecting oligodendrocytes and enhancing remyelination in multiple sclerosis. Discov Med. 2013;16:53–63. [PMC free article] [PubMed] [Google Scholar]
- 80.Roxburgh RH, Seaman SR, Masterman T, Hensiek AE, Sawcer SJ, Vukusic S, Achiti I, Confavreux C, Coustans M, le Page E, Edan G, McDonnell GV, Hawkins S, Trojano M, Liguori M, Cocco E, Marrosu MG, Tesser F, Leone MA, Weber A, et al. Multiple Sclerosis Severity Score: using disability and disease duration to rate disease severity. Neurology. 2005;64:1144–1151. doi: 10.1212/01.WNL.0000156155.19270.F8. [DOI] [PubMed] [Google Scholar]
- 81.Selmaj I, Cichalewska M, Namiecinska M, Galazka G, Horzelski W, Selmaj KW, Mycko MP. Global exosome transcriptome profiling reveals biomarkers for multiple sclerosis. Ann Neurol. 2017;81:703–717. doi: 10.1002/ana.24931. [DOI] [PubMed] [Google Scholar]
- 82.Sharaf-Eldin WE, Kishk NA, Gad YZ, Hassan H, Ali MAM, Zaki MS, Mohamed MR, Essawi ML. Extracellular miR-145, miR-223 and miR-326 expression signature allow for differential diagnosis of immune-mediated neuroinflammatory diseases. J Neurol Sci. 2017;383:188–198. doi: 10.1016/j.jns.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 83.Sheinerman KS, Umansky SR. Circulating cell-free microRNA as biomarkers for screening, diagnosis, and monitoring of neurodegenerative diseases and other neurologic pathologies. Front Cell Neurosci. 2013;7:150. doi: 10.3389/fncel.2013.00150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shin D, Shin JY, McManus MT, Ptácek LJ, Fu YH. Dicer ablation in oligodendrocytes provokes neural impairment in mice. Ann Neurol. 2009;66:843–857. doi: 10.1002/ana.21927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Singh RP, Massachi I, Manickavel S, Singh S, Rao NP, Hasan S, Mc Curdy DK, Sharma S, Wong D, Hahn BH, Rehimi H. The role of miRNA in inflammation and autoimmunity. Autoimmun Rev. 2013;12:1160–1165. doi: 10.1016/j.autrev.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 86.Søndergaard HB, Hesse D, Krakauer M, Sørensen PS, Sellebjerg F. Differential microRNA expression in blood in multiple sclerosis. Mult Scler. 2013;19:1849–1857. doi: 10.1177/1352458513490542. [DOI] [PubMed] [Google Scholar]
- 87.Tzartos JS, Friese MA, Craner MJ, Palace J, Newcombe J, Esiri MM, Fugger L. Interleukin-17 production in central nervous system-infiltrating T cells and glial cells is associated with active disease in multiple sclerosis. Am J Pathol. 2008;172:146–155. doi: 10.2353/ajpath.2008.070690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Vistbakka J, Elovaara I, Lehtimäki T, Hagman S. Circulating microRNAs as biomarkers in progressive multiple sclerosis. Mult Scler. 2017;23:403–412. doi: 10.1177/1352458516651141. [DOI] [PubMed] [Google Scholar]
- 89.Vistbakka J, Sumelahti ML, Lehtimäki T, Elovaara I, Hagman S. Evaluation of serum miR-191-5p, miR-24-3p, miR-128-3p, and miR-376c-3 in multiple sclerosis patients. Acta Neurol Scand. 2018;138:130–136. doi: 10.1111/ane.12921. [DOI] [PubMed] [Google Scholar]
- 90.Wang YF, He DD, Liang HW, Yang D, Yue H, Zhang XM, Wang R, Li B, Yang HX, Liu Y, Chen Y, Duan YX, Zhang CY, Chen X, Fu J. The identification of up-regulated ebv-miR-BHRF1-2-5p targeting MALT1 and ebv-miR-BHRF1-3 in the circulation of patients with multiple sclerosis. Clin Exp Immunol. 2017;189:120–126. doi: 10.1111/cei.12954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhao X, He X, Han X, Yu Y, Ye F, Chen Y, Hoang T, Xu X, Mi QS, Xin M, Wang F, Appel B, Lu QR. MicroRNA-mediated control of oligodendrocyte differentiation. Neuron. 2010;65:612–626. doi: 10.1016/j.neuron.2010.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhou J, Zhang J. Identification of miRNA-21 and miRNA-24 in plasma as potential early stage markers of acute cerebral infarction. Mol Med Rep. 2014;10:971–976. doi: 10.3892/mmr.2014.2245. [DOI] [PubMed] [Google Scholar]


