Abstract
Mucinous appendiceal neoplasms are rare and diagnosis is often difficult as patients present with non-specific symptoms often suggestive of appendicitis only and most diagnoses are made following post-surgery histology examination. Here we present a case of a mucinous appendiceal adenocarcinoma with areas of both Low-grade Appendiceal Mucinous Neoplasm and High-grade Appendiceal Mucinous Neoplasm, in a ruptured appendix at a district general hospital. Without early detection and treatment these pathologies can lead to pseudomyxoma peritonei, a syndrome of progressive mucinous ascites. This case highlights the limitations of radiological studies, benefits of diagnostic laparoscopy and provides a rationale for removing the mesoappendix with the appendix during routine appendectomies.
INTRODUCTION
Primary appendiceal neoplasms are found in ~2% of appendicetomies [1]. In particular, appendiceal mucinous adenocarcinomas are remarkably rare with 0.2% of appendicectomies demonstrating mucinous masses [1]. High-grade Appendicial Mucinous Neoplasm (HAMN) is thought to be the intermediate stage between Low-grade Appendiceal Mucinous Neoplasm (LAMN) and mucinous appendiceal adenocarcinomas [2]. More than half of LAMN are asymptomatic however in those who do present with symptoms, right lower quadrant pain and acute appendicitis have been reported [1]. Detection can prove challenging and diagnoses are often made intraoperatively and histologically, or are misdiagnosed as ovarian masses in females [3]. Failure to diagnose and excise mucinous neoplasms before appendiceal rupture can lead to pseudomyxoma peritonei (PMP), a condition with a 5-year disease-free survival rate of 37.4% after treatment and an incidence of ~1/million per annum [4].
CASE REPORT
An 84-year-old gentleman with a background of previous percutaneous coronary intervention and quadruple coronary artery bypass grafting, presented to a colorectal surgery clinic via the 2 week wait pathway complaining of central abdominal pain for 6 months with no other associated symptoms. He had a performance status of 0 and clinical examination identified a10 × 6 cm mobile lump palpable in the central abdomen below the umbilicus. His tumour markers including CEA and CA 19–9 were elevated at 46 and 30, respectively.
Cross sectional computed tomography imaging of the abdomen and pelvis with contrast confirmed a large cystic lesion within the lower abdomen as shown in Fig. 1. This case was discussed in the colorectal multidisciplinary team meeting where the possibility of the mass being an AMN was raised. It was radiologically thought to be unlikely and a provisional diagnosis of a mesenteric cyst was made.
Figure 1.

Cross sectional computed tomography image showing a large cystic, trabeculated lesion with an enhancing wall in the lower abdomen measuring 11.3 × 11.5 × 16 cm.
Following discussion with the patient and his relatives and obtaining informed consent, we proceeded with an elective diagnostic laparoscopy. At laparoscopy a large ruptured cyst possibly arising from the appendix was seen as shown in Fig. 2. There was free mucin in the right paracolic gutter and pelvis. Intraoperatively, the decision was made to proceed to a midline laparotomy for debulking and washout. The cystic mass, appendix and lateral peritoneum were excised and washout cleared all visible mucin deposits.
Figure 2.
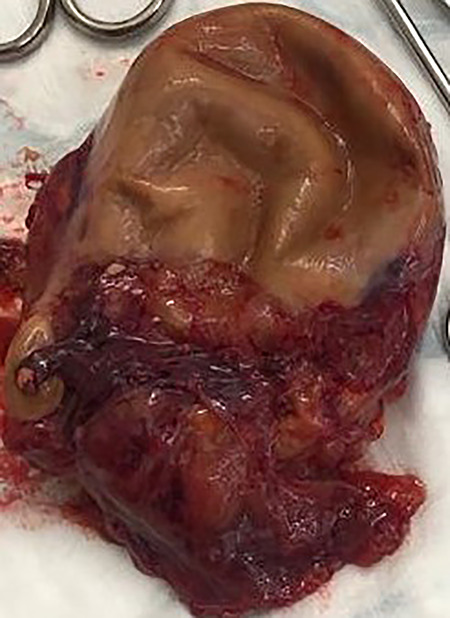
Resected mucinous appendiceal adenocarcinoma with areas of LAMN and HAMN.
Post-operatively the patient was discharged on day 6 and had an uncomplicated recovery. Post-operative pathology examination revealed a foci of appendiceal rupture and confirmed the suspected mesenteric cyst was in fact a moderately differentiated mucinous appendiceal adenocarcinoma arising on a background of LAMN and areas of HAMN. Staging was determined as pT4a NX xM1c R1 following intraoperative findings, imaging and pathology reports.
DISCUSSION
Mucinous appendiceal masses are four times more common in women than men with a peak incidence above 50 years of age [1]. AMNs can be associated with colonic polyps and masses and therefore studies have recommended endoscopic investigations in these patients [1].
This case demonstrates the importance of appreciating the limitations of radiological studies and how it may in some cases prove misleading. It also highlights the diagnostic benefits laparoscopy can provide patients with persistent non-specific symptoms, and raises the case for routinely removing the mesoappendix with the appendix to excise surrounding lymph nodes. A study by Davenport et al discussed that removal of the mesoappendix for appendiceal neuroendocrine neoplasms may have spared a proportion of patients later requiring a right hemicolectomy [5].
Since appendiceal mucinous adenocarcinomas are often diagnosed following histological reports, routine removal of the mesoappendix could prove crucial for patients prognostically, and may reduce the need for further intervention. To enable removal of the mesoappendix, a 10 mm laparoscopic port may routinely be required instead of just 5 mm ports.
Mucinous appendiceal adenocarcinoma is a serious condition with the potential to progress to PMP, which may require extensive surgical intervention and chemotherapy. With a 10 year survival rate <10% for patients with mucinous appendiceal adenocarcinoma, the potential for this condition to be misdiagnosed as benign gynaecological and gastroenterological conditions presents opportunities for sinister and life changing misdiagnoses [1]. This case highlights the potential benefits of diagnostic laparoscopy in patients when imaging does not provide a definite diagnosis. LAMN, HAMN and mucinous appendiceal adenocarcinomas are rare and may continue to be masked by non-specific presentations. However, measures such as diagnostic laparoscopy and removing the mesoappendix along with the appendix may help identify this condition earlier, halt progression to PMP and aid successful and safe treatment.
FUNDING
This study was funded by Imperial College London.
All authors contributed equally to this study.
References
- 1. Tirumani SH, Fraser-Hill M, Auer R, Shabana W, Walsh C, Lee F, et al. Mucinous neoplasms of the appendix: a current comprehensive clinicopathologic and imaging review. Cancer Imaging 2013;13:14–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Legué LM, Creemers G-J, de Hingh IHJT, Lemmens VEPP, Huysentruyt CJ. Review: pathology and its clinical relevance of mucinous appendiceal neoplasms and pseudomyxoma peritonei. Clin Colorectal Cancer 2019;18:1–7. [DOI] [PubMed] [Google Scholar]
- 3. Scaffa C, Di Bella O, Tartaglia E, Rotondi M, Lup F, Messalli EM. Surgical approach to appendiceal mucocele mimicking an adnexal complex mass: case report. Eur J Gynaecol Oncol 2007;28:503–5. [PubMed] [Google Scholar]
- 4. Smeenk RM, Verwaal VJ, Antonini N, Zoetmulder FA. Survival analysis of pseudomyxoma peritonei patients treated by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg 2007;245:104–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Davenport E, Courtney ED, Benson-Cooper S, Bissett IP, et al. Appendiceal neuroendocrine neoplasms in the era of laparoscopic appendicectomy. ANZ J Surg 2014;84:337–40. [DOI] [PubMed] [Google Scholar]


