Abstract
Background
Early recognition of sepsis is critical for timely initiation of treatment. The first objective of this study was to assess the timeliness of diagnostic procedures for recognizing sepsis in emergency departments. We define diagnostic procedures as tests used to help diagnose the condition of patients. The second objective was to estimate associations between diagnostic procedures and time to antibiotic treatment, and to estimate associations between time to antibiotic treatment and mortality.
Methods
This observational study from 24 emergency departments in Norway included 1559 patients with infection and at least two systemic inflammatory response syndrome criteria. We estimated associations using linear and logistic regression analyses.
Results
Of the study patients, 72.9% (CI 70.7–75.1) had documented triage within 15 minutes of presentation to the emergency departments, 44.9% (42.4–47.4) were examined by a physician in accordance with the triage priority, 44.4% (41.4–46.9) were adequately observed through continual monitoring of signs while in the emergency department, and 25.4% (23.2–27.7) received antibiotics within 1 hour. Delay or non-completion of these key diagnostic procedures predicted a delay of more than 2.5 hours to antibiotic treatment. Patients who received antibiotics within 1 hour had an observed 30-day all-cause mortality of 13.6% (10.1–17.1), in the timespan 2 to 3 hours after admission 5.9% (2.8–9.1), and 4 hours or later after admission 10.5% (5.7–15.3).
Conclusions
Key procedures for recognizing sepsis were delayed or not completed in a substantial proportion of patients admitted to the emergency department with sepsis. Delay or non-completion of key diagnostic procedures was associated with prolonged time to treatment with antibiotics. This suggests a need for systematic improvement in the initial management of patients admitted to emergency departments with sepsis.
Introduction
Sepsis is a major challenge, being present in a large proportion of hospitalizations that culminate in death [1–3]. Most sepsis cases seem to arise outside hospital settings [4], and these patients present to emergency departments with heterogeneous signs and symptoms, making detection and diagnosis challenging [5]. New sepsis criteria and early antibiotic treatment has been a major focus of research and debate over the last years [6] but factors associated with delayed treatment in the emergency departments have received less attention.
Previous research, mostly based on single case studies and smaller patient cohorts, suggests that systematic screening and diagnostic procedures for recognizing sepsis are not consistently carried out according to current guidelines [5, 7] and that sepsis is not recognized early enough [7]. Early recognition of sepsis is of critical importance for timely treatment [8–10], and compliance with sepsis guidelines is associated with improved outcomes [11–13]. However, no studies have assessed the association between timeliness of diagnostic procedures and time to treatment [11]. More knowledge about such associations can prove useful in improving initial care of the many patients admitted to emergency departments with sepsis. Moreover, there is a need for robust data documenting the extent to which diagnostic procedures are delayed or not carried out for patients with sepsis presenting to the emergency room.
The objectives of the study were to assess the timeliness of diagnostic procedures for recognizing sepsis in emergency departments and to evaluate associations between timeliness of procedures and time to initial administration of antibiotics and association between time to antibiotic administration and 30-day all-cause mortality.
Methods
Setting and participants
We conducted a multicenter, observational study based on data in electronic health records of 24 Norwegian hospitals.
The Norwegian health care system is publicly funded, and it scores relatively high on the Organisation for Economic Co-operation and Development’s quality indicators [14]. In Norway, primary care physicians decide whether to refer patients with suspected sepsis to an emergency department for further assessment and treatment.
This study is a part of a 4-year longitudinal research project to assess the effects and outcomes of inspections on early detection of sepsis and time to treatment in emergency departments. The project was initiated in 2015 by the Norwegian Board of Health Supervision, which is the body delegated with the overall responsibility for external inspections of health care in Norway. The protocol for this project has been published previously [15]. In the present article, we report the results of the first part of the study, establishing baseline levels of compliance with sepsis guidelines, and assessing the associations between delayed diagnostic procedures and time to treatment and between time to treatment and mortality.
Measures of care delivery and outcome
The Norwegian Board of Health Supervision identified key clinical practices involved in recognition of sepsis by examining international guidelines [16, 17] and receiving advice from experts on sepsis. The choice of which care processes to include was based on key elements of the guideline: screening for sepsis and diagnosing sepsis, source control, and treatment. Operationalizing these elements into process measures of care delivery was a pragmatic decision based on what data that could be expected to be available in the electronic health records. The data were collected by inspection teams, who evaluated the practices at each hospital. We operationalized these practices into process measures of care delivery, which we used as the study variables (see Box 1). We defined mortality as all-cause mortality within 30 days from hospital admission.
Box 1. Clinical processes of delivery of sepsis care.
Proportion of patients triaged within 15 minutes of arrival at an emergency department.*
Proportion of patients assessed by a physician in accordance with the urgency specified in the initial triage.
Proportion of patients whose vital signs were measured within 1 hour of arrival at an emergency department.
Proportion of patients whose blood lactate was measured within 1 hour of arrival at an emergency department.
Proportion of patients from whom blood samples† were taken within 1 hour of arrival at an emergency department.
Proportion of patients from whom blood cultures were taken before administration of antibiotics.
Proportion of patients with adequate supplementary investigations to detect the focus of infection.
Proportion of patients adequately observed‡ while in an emergency department.
Proportion of patients who had received antibiotics within 1, 2, 4, and more than 4 hours.
* Norwegian hospitals are required to establish a system for prioritizing patients admitted to emergency departments. The scales that are in use are based on the South African Triage Scale (SATS) and the Rapid Emergency Triage and Treatment System (RETTS).
† Leukocyte count, hemoglobin, C-reactive protein, creatinine, electrolytes, platelet count, glucose, bilirubin, blood lactate
‡ ‘Adequate’ is defined as continual observation and measurement and documentation of vital signs at least every 15 minutes in critically ill patients with sepsis and organ failure, measurement and documentation of vital signs every 15 minutes if a physician has not examined a patient with sepsis but no documented organ failure, and every 30 minutes after first examination in such patients unless the physician decides otherwise.
Study cohort
We sampled data from electronic health records of patients admitted to 24 Norwegian hospitals from May 2015 through February 2017. Hospital size and geographic location were the main inclusion criteria. The 24 hospitals were representative of Norwegian hospitals with emergency departments and included all university and regional hospitals in Norway and a geographically based selection of local hospitals, together serving 75% of the total Norwegian population of 5 million. The hospitals ranged in size from 58 to 1640 beds and had emergency departments that served their local or regional communities.
We defined sepsis as the suspicion of infection together with two systemic inflammatory response syndrome signs, in accordance with internationally established and widely adopted definitions of sepsis at the time the protocol was developed [16]. The inclusion criteria were clinically suspected infection on presentation to an emergency department and at least two systemic inflammatory response syndrome signs, not including high leukocyte counts. We excluded high leukocyte counts as a criterion because the result of the blood sample in many cases would not be available for the clinicians when they do their initial judgment of severity of the patient’s condition.
Organ failure was defined as fulfilling one of the following criteria at arrival to the emergency department: oxygen saturation <90% or PaO2/FiO2 <40 kPa, altered mental status, urine output <0.5 mL/kg/hour or increase in serum creatinine >50 micro mol/L, international normalized ratio >1.5 or activated partial thromboplastin time > 60 seconds, platelet count < 100 or 50% reduction in previous three days, serum bilirubin >70 mmol/L, serum lactate >4 mmol/L, blood pressure <90 systolic, mean arterial pressure <60, or fall in mean arterial pressure >40 mm Hg. We did not use a Sequential Organ Failure Assessment (SOFA) score for inclusion, as this was not in use at the emergency departments, and it was not possible to collect data retrospectively in order to evaluate the patients’ SOFA score.
Data collection
We used a two-step case ascertainment approach to identify eligible patients. First, we searched the Norwegian Patient Registry using a predefined list of the ICD-10 diagnostic codes that are most commonly used in Norway to classify sepsis and infections [18] (see S1 File). The patient registry contains diagnostic and therapeutic codes for all hospital admissions. The search produced a list of patients who had been discharged from the participating hospitals with a sepsis and/or infection code, together with an identification number that enabled access to the corresponding health records. Second, information about the patients’ clinical status upon presentation to the emergency department from the individual patient records was assessed on-site at the hospitals to determine eligibility. Out of 5188 patients initially screened for eligibility, 1559 patients were included in the study (see S1 Fig). The sample size was arrived at through power calculations to detect changes between the baseline measurements (which is the study sample used for this study) and post-inspection measurements. The power calculations are explained in detail in the study protocol [15].
Six regional inspection teams from the County Governors, who carry out inspections on behalf of the Norwegian Board of Health Supervision, were tasked with assessing eligibility and collecting data. The inspections were headed by experienced team leaders with particular training in performing similar inspections. The teams consisted of a minimum of four inspectors with medical and legal expertise, including an independent senior consultant physician in internal medicine or critical care medicine.
Each team performed four inspections within a time frame of about seven weeks in four geographically proximate hospitals. The inspections were rolled out sequentially from March 2016 to February 2017, averaging two per month. The sequence of inspections was randomized to facilitate comparison of outcomes before and after the inspections. The details of and rationale for the study design are described in the published study protocol [15].
The teams collected the data retrospectively during their inspection site visits. To allow for possible changes in clinical performance over time, they sampled data from two different time intervals for each hospital. For each time interval, we aimed to include the last 33 consecutive patients with sepsis who fulfilled the inclusion criteria on presentation to the emergency departments. The first sample included the last 33 patients admitted at each hospital before 1 October 2015, which was immediately before the Norwegian Board of Health Supervision announced the inspection campaign. The second sample included the last 33 patients before inspection of each hospital.
Data were recorded manually on case record forms, and subsequently digitized and saved to a single database containing information from all 24 participating hospitals. Upon completion of the database, we obtained information from the National Patient Registry on 30 day all-cause mortality and Charlson Comorbidity Index [19] for all patients, based on their national identity number and date of hospital admittance.
Data analyses
To assess the timeliness of diagnostic procedures, we calculated the percentages and 95% confidence intervals of patients with sepsis who had been documented as undergoing diagnostic procedures and receiving antibiotics within specified time limits (see Box 1). We did the analysis with all patients included and for the subgroup of patients with organ failure. Because several patient records lacked data on one or more measures of care delivery, we have also provided the number of records with missing documentation.
To estimate mean difference in time to first dose of antibiotics between categories of clinical procedure variables, we performed linear regression analyses using minutes to first dose of antibiotics as the outcome variable. Following previous research [16] and knowledge of the clinical care process in emergency departments, we focused on the following clinical procedures as exposure variables: triage within 15 minutes, examination by a physician in accordance with priority ascertained by triage, blood lactate measurements within one hour, and evidence of an adequate observation regimen within the emergency department. We performed univariate analyses for each procedure and then included all factors in a multivariable analysis.
Analyzing the association between time to diagnostic procedures and time to treatment, we needed to address the question of whether all kinds of delays were the results of clinical decisions to prioritize care for the patients who had the most serious clinical condition, thus making any association between delays to diagnostic procedures and delays to treatment a spurious one. We controlled for such confounding by indication by including age, organ failure, and comorbidity as covariates in adjusted analyses. The results were then checked against a subgroup analysis of patients who had a serious medical condition at arrival identified by a red or orange triage color (see S2 File). We made additional adjustment for elapsed time since commencement of the study. Elapsed time was measured using calendar days, and was added as a cubic term.
We used a logistic regression model to estimate the 30-day all-cause mortality rate in relation to time to antibiotic administration. In this analysis, we used all-cause mortality as the binary outcome variable and time to first dose of antibiotics as a cubic exposure term, allowing for a non-linear relationship. We also made adjustment for age, year of admission (entered as categorical variables), Charlson comorbidity index, and organ failure as adjustment variables. We present the model-predicted mortality rates by time to antibiotic administration in a graphical format.
Patients who either had no antibiotic indication or had received antibiotic treatment before admittance in the emergency department were excluded from the regression analyses. So were patients for whom we lacked information on time to antibiotic treatment.
For some patients, data were missing for one or several of the variables included as covariates in the analyses. The results from blood samples are imported to the electronic health record; we therefore coded blood lactate as not taken within one hour when it was not documented in the patient record. Similarly, we coded patients who lacked documentation on adequate observation regimen within the emergency department as not having been observed adequately. We imputed data for four variables in our data set: time to antibiotics in minutes, time to examination by a physician, time to triage, and organ failure. Missing values were imputed using fully conditional specification [20]. See S2 File for more information about the treatment of missing data and the regression models.
The regression analyses were first performed including the whole study sample, and then for the sub-group of patients with organ failure (see supplemental S3 File).
We performed the statistical analyses with Stata versions SE 15.1 and IC 16.0 (StataCorp LP, College Station, TX, USA). For all regression models, we obtained cluster-robust standard errors of model parameters to account for intra-cluster correlations.
Results
The study included 1559 patients from 24 Norwegian hospitals from all the 19 Norwegian counties. Table 1 shows characteristics of the study cohort.
Table 1. Selected characteristics of the study cohort.
| Male | Female | All | |
|---|---|---|---|
| N | 800 (51.3%) | 759 (48.7%) | 1559 |
| Mean (standard deviation) age | 69.3 (16.5) | 64.6 (20.9) | 67.0 (18.9) |
| Median (min—max) age | 72 (18–98) | 69 (18–99) | 71 (18–99) |
| Mean (standard deviation) CCI* | 3.0 (2.5) | 2.2 (2.2) | 2.6 (2.4) |
| Organ failure | 313 (39.5%) | 244 (32.8%) | 557 (36.3%) |
* Charlson Comorbidity Index
The percentages of patients who received care in line with the pre-defined standards are shown in Table 2.
Table 2. Proportion of patients who underwent clinical procedures and received treatment in line with pre-defined standards.
| Number of patient records | Percent of patients documented receiving recommended care (95% confidence interval) | |||||
|---|---|---|---|---|---|---|
| Measure | Records with documentataion* | Records lacking documentation | All study patients† | Patients with organ dysfunction | ||
| Diagnostics | ||||||
| Complete assessment of vital signs within 1 hour | 1360 | 199 | 83.6 (81.8 to 85.5) | 81.0 (77.7 to 84.2) | ||
| Pulse rate measured within 1 hour | 1496 | 63 | 93.3 (92.9 to 94.6) | 94.1 (92.1 to 96.0) | ||
| Temperature measured within 1 hour | 1492 | 67 | 93.1 (91.9 to 94.4) | 94.3 (92.3 to 96.2) | ||
| Blood pressure measured within 1 hour | 1493 | 66 | 92.7 (91.9 to 94.0) | 93.9 (91.9 to 95.9) | ||
| Respiration rate measured within 1 hour | 1476 | 83 | 91.5 (90.9 to 92.9) | 93.4 (91.3 to 95.4) | ||
| Mental status assessed within 1 hour | 1390 | 169 | 86.0 (84.8 to 87.7) | 83.1 (80.0 to 86.2) | ||
| Blood culture taken prior to administration of antibiotics | 1350 | 95 | 85.3 (83.8 to 87.1) | 84.6 (81.6 to 87.6) | ||
| Adequate supplementary examinations to identify source of infection | 1548 | 11 | 93.7 (92.9 to 94.9) | 93.7 (91.7 to 95.7) | ||
| Time to triage (≤ 15 min) | 1375 | 184 | 72.9 (70.7 to 75.1) | 77.0 (73.5 to 80.5) | ||
| Adequate observation regimen in ED | 1524 | 35 | 44.4 (41.4 to 46.9) | 47.4 (43.2 to 51.6) | ||
| Examination by physician in accordance with triage urgency | 1105 | 454 | 44.9 (42.4 to 47.4) | 47.6 (43.4 to 51.7) | ||
| Leukocytes count | Blood samples taken within 1 hour | 1534 | 25 | 87.1 (85.8 to 88.8) | 88.5 (85.9 to 91.2) | |
| Hemoglobin | 1533 | 26 | 87.2 (85.8 to 88.8) | 88.2 (85.5 to 90.8) | ||
| C-reactive protein | 1534 | 25 | 87.0 (85.8 to 88.7) | 88.5 (85.9 to 91.2) | ||
| Creatinine | 1525 | 34 | 86.7 (85.8 to 88.3) | 88.3 (85.7 to 91.0) | ||
| Electrolytes | 1524 | 35 | 86.8 (85.8 to 88.5) | 88.3 (85.7 to 91.0) | ||
| Platelet count | 1510 | 49 | 85.8 (84.8 to 87.5) | 87.4 (84.7 to 90.2) | ||
| Glucose | 1492 | 67 | 85.1 (83.8 to 86.9) | 87.6 (84.9 to 90.4) | ||
| Bilirubin | 963 | 482 | 62.0 (59.6 to 64.4) | 66.2 (62.3 to 70.2) | ||
| Blood lactate | 955 | 604 | 48.6 (46.4 to 51.1) | 58.5 (54.4 to 62.6) | ||
| Treatment | ||||||
| Antibiotics within 1 hour‡ | 1313 | 132 | 25.5 (23.2 to 27.7) | 30.4 (26.4 to 34.3) | ||
| Antibiotics within 2 hours‡ | 1313 | 132 | 55.5 (52.9 to 58.1) | 59.4 (55.2 to 63.6) | ||
| Antibiotics within 4 hours‡ | 1313 | 132 | 79.7 (77.6 to 81.7) | 82.5 (79.2 to 85.7) | ||
* Total number of records: 1559
† Patients with suspected infection together with two systemic inflammatory response syndrome signs
‡ n = 1438 (patients registered as needing antibiotic treatment and not having received antibiotics prior to admission)
Of the patients in our sample, 72.9% (95% confidence interval 70.7 to 75.1), had documented triage within 15 minutes of presentation to the emergency department, 44.9% (42.4 to 47.4) were examined by a physician in accordance with the priority specified during triage, and 83.6% (81.8 to 85.5) had a complete set of vital signs recorded within one hour of presentation. Blood samples were obtained within one hour from more than 80% of the patients for all specified tests except for bilirubin and lactate, 62.0% (59.6 to 64.4) and 48.6% (46.4 to 51.1), respectively; 44.4% (42.4 to 47.4) were adequately observed while in the emergency department according to the degree of priority assigned during triage; and 25.4% (23.2 to 27.7) and 55.5% (52.5 to 58.0) of the patients received antibiotics within one and two hours, respectively.
We found an association between non-completed or delayed diagnostic procedures and prolonged time to administration of antibiotics. In adjusted analyses (Model 1 in Table 3), patients who had not been triaged within 15 minutes had in average an extra delay of 54.7 minutes (95% confidence interval 33.2 to 76.2) to administration of antibiotics. We found a similar pattern of prolonged time to administration of antibiotics of cases where patients were not examined by a physician within the time limits set in triage, 61.2 minutes (40.8 to 81.6), not having blood lactate measured within one hour, 86.2 minutes (71.5 to 100.8), and not having an adequate observation regimen, 39.3 minutes (21.8 to 56.8). When we included all four procedures in one regression analysis (Model 2 in Table 3), they together predicted a delay of 159 minutes to first dose of antibiotics.
Table 3. Linear regression for factors associated with delay in antibiotic treatment.
| Unadjusted | Model 1* | Model 2† | |
|---|---|---|---|
| b (95% CI) | b (95% CI) | b (95% CI) | |
| Not triaged within 15 minutes | 54.4 (32.9 to 75.9) | 54.7 (33.2 to 76.2) | 25.8 (3.8 to 47.8) |
| Examination by physician not in accordance with priority | 60.0 (39.2 to 80.9) | 61.2 (40.8 to 81.6) | 38.0 (16.1 to 59.8) |
| Lactate not measured within 1 hour | 81.6 (65.9 to 97.2) | 86.2 (71.5 to 100.8) | 71.4 (56.0 to 86.8) |
| Inadequate observation regimen | 41.3 (22.3 to 60.4) | 39.3 (21.8 to 56.8) | 23.9 (10.5 to 37.3) |
Outcome variable: Time to antibiotics measured in minutes. n = 1307
* Adjusted for organ failure, patient age, comorbidity, and time to admission
† Adjusted for the other variables in this table, and organ failure, age, comorbidity, and time to admission
Replicating the regression analyses for the sub-group of patients with organ failure yielded similar results, with the model including all four factors also predicting an extra delay of 159 minutes for patients with organ failure (see S3 File).
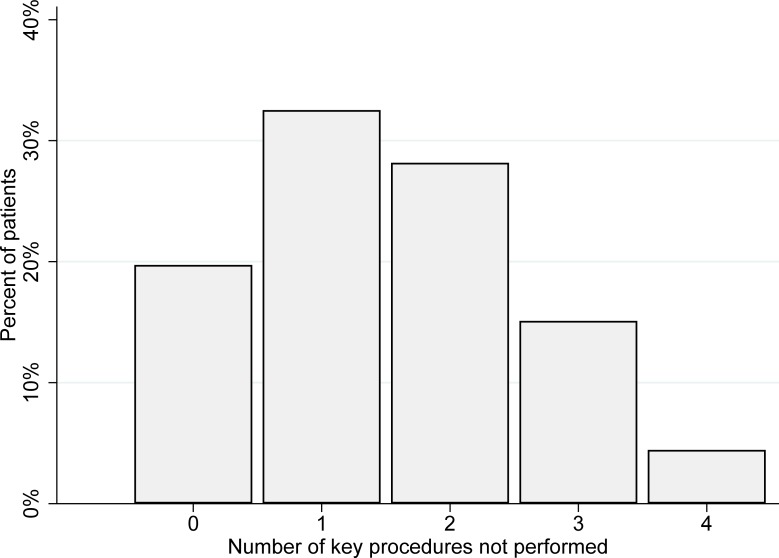
Fig 1 shows the distribution of patients according to the number of the four specified procedures that were not performed within the recommended time limits.
Fig 1. Distribution of patients according to number of non-completed or delayed key diagnostic procedures.
Key procedures: triage within 15 minutes, examination by physician in accordance with urgency specified during triage, blood lactate measured within 1 hour, adequate observation regimen. N = 1559.
The 30-day all-cause mortality was 9.9% (8.4 to 11.4) for the entire study sample and 17.4% (14.2 to 20.5) for patients with documented organ failure.
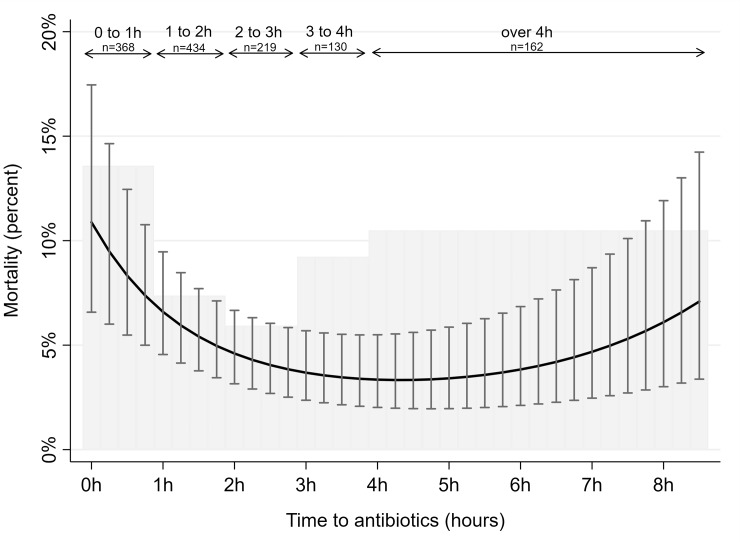
Fig 2 displays the observed 30-day all-cause mortality in hourly intervals for time from admission to administration of antibiotics (bars). Patients receiving antibiotics within 1 hour had an observed mortality of 13.6% (10.1 to 17.1), whereas those receiving antibiotics in the timespan 2 to 3 hours after admission had an observed mortality of 5.9% (2.8 to 9.1) and those receiving antibiotics 4 hours or later after admission had an observed mortality of 10.5% (5.7 to 15.3).
Fig 2. All-cause 30-day mortality by time to antibiotic treatment.
Gray shaded histogram represents mortality rates according to time to antibiotic treatment in hours. Solid black curve with bars represents model-predicted mortality rates with 95% confidence intervals according to time to antibiotic treatment in minutes using logistic regression models, adjusted for patient’s age, date of admission, comorbidity, and presence of organ failure. Date of admission was measured using calendar days since study start, entered as a polynomial function with first (b -0.011 p<0.001), second (b 2.5e-5 p<0.001) and third degree (b -1.2e-8 p<0.01) variables. The model prediction uses average values for adjustment values.
Fig 2 also shows the model-predicted 30-day all-cause mortality according to time to antibiotic treatment in minutes, adjusted for patient’s age, date of admission and presence of organ failure (shown by the solid black curve).
Replicating the analysis of the association between time to antibiotic treatment and 30-day mortality for the sub-group of patients with organ failure, we found a similar curvilinear trend where predicted mortality was highest for patients who received antibiotics within one hour (see S3 File).
Discussion
Principal findings
In this study of 24 emergency departments, we found that they frequently failed to perform important diagnostic procedures in time, and that delays in or non-completion of diagnostic procedures were associated with prolonged time to administration of antibiotics. In 46% of the study patients, two or more of the following four key procedures had not been carried out in a timely manner: triage within 15 minutes, examination by physician in accordance with priority as set in triage, measuring blood lactate within one hour, and adequate observation. Non-completion or delay of these procedures together predicted a delay of 159 minutes to administration of antibiotics. We also found a substantial variation in mortality according to time to antibiotics. Patients who started antibiotic treatment between 2 and 3 hours after admission had lower mortality than those who started antibiotics earlier or later.
Strengths and limitations
The main strengths of our study are the combination of inclusion procedures and the size of the patient cohort from 24 different study sites. The hospitals that the study patients attended can be considered representative of Norwegian hospitals because they included all university and regional hospitals and a geographically based selection of local hospitals, serving 75% of the total Norwegian population. Moreover, we included consecutive patients admitted to the emergency departments during two different time periods by using a cluster randomized sampling approach. Therefore, our study cohort is representative of patients admitted to Norwegian emergency departments with infection and meeting two or more systemic inflammatory response syndrome criteria.
Another important strength of our study is that we manually reviewed all patient records and established eligibility on the basis of recorded clinical data rather than on diagnostic codes alone. The latter approach can cause ascertainment bias and misleading inferences because coding practices for sepsis can vary over time and between hospitals [21].
A limitation of our study is the use of systematic inflammatory response syndrome (SIRS) as an inclusion criterion, in line with the Sepsis-2 definition. Since the protocol was initially drafted and the project started, a Sepsis-3 definition as a life-threatening organ dysfunction caused by a dysregulated host response to infection was proposed [6]. As compared to Sepsis-2, Sepsis-3 represents only a minority of patients with infection [22]. Thus, our findings cannot be directly generalized to patient groups that have sepsis according to the Sepsis-3 definition. We have performed sub analyses of patients with organ failure, which is a group of patients that more closely overlaps with the Sepsis-3 definition, to make it easier to compare our findings to those of studies relying on the Sepsis-3 definition. These analyses show similar results for the sub-group of patients with organ failure as those of the whole study sample.
Another limitation of our study is that we did not have data on severity of sepsis in the form of commonly used severity scores like SAPS 2 (simplified acute physiology score) or APACHE II (acute physiology and chronic health evaluation), or a detailed organ failure assessment score like SOFA (sequential organ failure assessment). We did control for age, presence of organ failure, and comorbidity, which are three important variables associated with severity of sepsis [23]; however, even when controlling for these variables, the associations we found between time to antibiotics and mortality were probably subject to confounding by unmeasured variations in severity of illness and patient characteristics. As such, the study design does not allow for unbiased estimation of treatment effects.
Comparison with other studies
The delays we identified in diagnostic procedures are consistent with previous research findings of delay in time to triage [24], recording of vital signs [5, 7], measurement of blood lactate [25, 26], and delays in recognition of sepsis in general [7]. The processes we found to be lacking are essential for reaching an accurate diagnosis and institution of treatment in a timely manner [27].
We found that 25.5% and 55.5% of patients received antibiotics within one and two hours, respectively. This is in line with or slightly faster than the timing reported in previous studies with comparable patient cohorts in emergency department settings, which found that 28% of patients received antibiotics within 1 hour [7] and that median times to commencing antibiotics were 2.1 hours [28] and 182 minutes [29].
No previous studies have demonstrated the extent of delay or non-completion of diagnostic procedures for patients with sepsis in a large, representative cohort of patients admitted to emergency departments, or assessed the association between non-completed or delayed procedures and prolonged time to antibiotic administration.
The mortality rate in our study was in line with mortality rates reported in previous research in an emergency department setting [11]. However, we found a curvilinear association, where patients receiving early treatment and treatment later than four hours after admission had higher mortality rates than those receiving treatment between two and four hours after admission. This parabolic trend conflicts with a previous report of a linear increase in mortality with increasing time to antibiotics [13].
Interpretation of findings and implications
There is an ongoing debate concerning how timing of antibiotics for patients with sepsis should be operationalized in guidelines. The guidelines have come under criticism for not being adequately based in empirical evidence and being overly reliant on treatment protocols mandating antibiotic initiation within one hour of triage [30] and early administration of broad-spectrum antibiotics to all patients with sepsis [31]. Commenting on the sepsis guidelines, the Infectious Disease Society of America recommends administration of antibiotics as soon as possible to patients with severe infections. However, they warn that rigid guideline recommendations with fixed time frames might increase the likelihood of broad-spectrum antibiotics will be given to uninfected patients [32]. In line with this argument, we maintain that the timing of antibiotic treatment should be an informed clinical decision rather than a consequence of unintended delays in diagnostic procedures. Our study indicates that the latter might often be the case: Delays in diagnostic procedures are common and they might lead to delayed treatment.
Emergency departments must therefore attend to optimizing diagnostic screening to improve time to treatment and overall management of sepsis. The Surviving Sepsis Campaign recommends a performance improvement program that includes screening for sepsis [33]; however, it is still necessary to define more precisely what screening measures should be implemented and how they should be monitored as part of the improvement program. We argue that our findings can inform this work.
We assert that the non-linear association we found between antibiotic treatment and mortality reflects the fact that many patients with sepsis are already critically ill when they present to an emergency department and that these patients are more easily recognized and given aggressive treatment earlier. This is an observation study, and the associations we found between time to antibiotics and mortality were probably subject to confounding by unmeasured variations in severity of illness and patient characteristics. Thus, one should not draw conclusions regarding the efficiency of antibiotic treatment at specific time intervals based on these analyses.
To our knowledge, this is the first multicenter study that assesses the association between a wide array of diagnostic procedures and antibiotic treatment. Previous research, mostly based on single case studies and smaller patient cohorts, has found delays in time to treatment comparable to those we found, suggesting that emergency departments elsewhere in Europe and the USA face challenges regarding variability of performance of initial screening procedures to detect sepsis. We therefore argue that our findings might have relevance for emergency departments outside of Norway.
Conclusions
We found that key procedures for recognizing sepsis and organ failure in the emergency department were delayed or not carried out in a substantial proportion of patients with sepsis. Delay or non-completion of key diagnostic procedures together predicted a delay of 2.5 hours to the first dose of antibiotics. Initiation of antibiotic treatment should be an informed clinical decision. Delays in antibiotic treatment could potentially have a negative effect on patient outcomes. These findings have important implications for managers and health professionals. The extent of delay and non-completion of important diagnostic procedures suggests that there is a need for systematic improvement efforts in the initial management of patients with sepsis presenting to emergency departments.
Supporting information
List of ICD 10 codes used to search the National Patient Register.
(PDF)
Description of how missing data are treated and of how we fitted the regression models.
(PDF)
Sub-analyses of association between diagnostic measures and time to treatment and between time to treatment and mortality for the sub-group of patients with organ failure.
(PDF)
Description Patient flow diagram showing the number of patients included and excluded.
(TIF)
Acknowledgments
We thank Paul Barach for reading a draft of the manuscript and providing valuable input. We also thank the inspection teams from the County Governors and the clinical experts for participating in data collection, and the staff at the Norwegian Board of Health Supervision who developed the sepsis inspection. An earlier draft of the manuscript was reviewed by Trish Reynolds and edited by Karyn Heavner, both from Edanz Group.
Disclaimer: Data from the Norwegian Patient Registry has been used in this publication. The interpretation and reporting of these data are the sole responsibility of the authors. No endorsement by the Norwegian Patient Registry is intended nor should be inferred.
Data Availability
As this study used data from the Norwegian Patient Registry, there are legal restrictions on sharing the data set. The registry is regulated according to the Act relating to Personal Health Data Registries (2014) and specific regulation for the registry under the provision of this act. These laws do not permit us to share these data for secondary use. Third parties can apply to obtain data from the Norwegian Directorate of Health, which is the body granting access to the registry. The Directorate responds to inquiries regarding the Norwegian Patient Registry via email helseregistre@helsedir.no. Data obtained from the Norwegian Patient Registry can be used to identify electronic health records at the hospitals, pending approval from ethics committee and hospitals.
Funding Statement
The Norwegian Board of Health Supervision funded the expenses incurred by the clinical experts on the inspection teams and part of the costs related to data collection. Erik Solligård was one of the clinical experts. Members of the inspection teams are employed by the County Governors in Norway. Western Norway University of Applied Sciences funds the PhD scholarship for Gunnar Husabø. Einar Hovlid, Gunnar Husabø and Geir Sverre Braut are part-time employees at the Norwegian Board of Health Supervision. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Rhee C, Dantes R, Epstein L, Murphy DJ, Seymour CW, Iwashyna TJ, et al. Incidence and Trends of Sepsis in US Hospitals Using Clinical vs Claims Data, 2009–2014. JAMA. 2017;318(13):1241–9. 10.1001/jama.2017.13836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prescott HC, Osterholzer JJ, Langa KM, Angus DC, Iwashyna TJ. Late mortality after sepsis: propensity matched cohort study. BMJ. 2016;353:i2375 10.1136/bmj.i2375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reinhart K, Daniels R, Kissoon N, Machado FR, Schachter RD, Finfer S. Recognizing Sepsis as a Global Health Priority—A WHO Resolution. N Engl J Med. 2017;377(5):414–7. 10.1056/NEJMp1707170 [DOI] [PubMed] [Google Scholar]
- 4.Page DB, Donnelly JP, Wang HE. Community-, Healthcare-, and Hospital-Acquired Severe Sepsis Hospitalizations in the University HealthSystem Consortium. Crit Care Med. 2015;43(9):1945–51. 10.1097/CCM.0000000000001164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morr M, Lukasz A, Rübig E, Pavenstädt H, Kümpers P. Sepsis recognition in the emergency department–impact on quality of care and outcome? BMC Emerg Med. 2017;17(1):11 10.1186/s12873-017-0122-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singer M, Deutschman CS, Seymour C, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–10. 10.1001/jama.2016.0287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goodwin A, Srivastava V, Shotton H, Protopapa K, Butt A, Mason M. Just say sepsis. A review of the process of care received by patients with sepsis London: National Confidential Enquiry into Patient Outcome and Death. 2015. [Google Scholar]
- 8.Gatewood MOK, Wemple M, Greco S, Kritek PA, Durvasula R. A quality improvement project to improve early sepsis care in the emergency department. BMJ Qual Saf. 2015;24(12):787–95. 10.1136/bmjqs-2014-003552 [DOI] [PubMed] [Google Scholar]
- 9.Pruinelli L, Westra BL, Yadav P, Hoff A, Steinbach M, Kumar V, et al. Delay Within the 3-Hour Surviving Sepsis Campaign Guideline on Mortality for Patients With Severe Sepsis and Septic Shock. Crit Care Med. 2018;46(4):500–5. 10.1097/CCM.0000000000002949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Torsvik M, Gustad LT, Mehl A, Bangstad IL, Vinje LJ, Damås JK, et al. Early identification of sepsis in hospital inpatients by ward nurses increases 30-day survival. Critical Care. 2016;20(1):244 10.1186/s13054-016-1423-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Damiani E, Donati A, Serafini G, Rinaldi L, Adrario E, Pelaia P, et al. Effect of performance improvement programs on compliance with sepsis bundles and mortality: a systematic review and meta-analysis of observational studies. PLoS One. 2015;10(5):e0125827 10.1371/journal.pone.0125827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levy MM, Rhodes A, Phillips GS, Townsend SR, Schorr CA, Beale R, et al. Surviving Sepsis Campaign: association between performance metrics and outcomes in a 7.5-year study. Crit Care Med. 2015;43(1):3–12. 10.1097/CCM.0000000000000723 [DOI] [PubMed] [Google Scholar]
- 13.Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, et al. Time to Treatment and Mortality during Mandated Emergency Care for Sepsis. N Engl J Med. 2017;376(23):2235–44. 10.1056/NEJMoa1703058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.OECD. Health at a Glance 2017: OECD Indicators. Paris: OECD Publishing; 2017. [Google Scholar]
- 15.Hovlid E, Frich JC, Walshe K, Nilsen RM, Flaatten HK, Braut GS, et al. Effects of external inspection on sepsis detection and treatment: a study protocol for a quasiexperimental study with a stepped-wedge design. BMJ Open. 2017;7(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39(2):165–228. 10.1007/s00134-012-2769-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Institute for Health and Care Excellence. Sepsis: recognition, diagnosis and early management (NICE guideline 51). 2016. [PubMed] [Google Scholar]
- 18.Knoop ST, Skrede S, Langeland N, Flaatten HK. Epidemiology and impact on all-cause mortality of sepsis in Norwegian hospitals: A national retrospective study. PLoS One. 2017;12(11):e0187990 10.1371/journal.pone.0187990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987;40(5):373–83. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 20.Van Buuren S. Flexible imputation of missing data: Chapman and Hall/CRC; 2018. [Google Scholar]
- 21.Gohil SK, Cao C, Phelan M, Tjoa T, Rhee C, Platt R, et al. Impact of policies on the rise in sepsis incidence, 2000–2010. Clin Infect Dis. 2016;62(6):695–703. 10.1093/cid/civ1019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vincent J-L, Martin GS, Levy MM. qSOFA does not replace SIRS in the definition of sepsis. Crit Care. 2016;20(1):210–. 10.1186/s13054-016-1389-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nasa P, Juneja D, Singh O. Severe sepsis and septic shock in the elderly: An overview. World J Crit Care Med. 2012;1(1):23–30. 10.5492/wjccm.v1.i1.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Houston C, Sanchez LD, Fischer C, Volz K, Wolfe R. Waiting for Triage: Unmeasured Time in Patient Flow. West J Emerg Med. 2015;16(1):39–42. 10.5811/westjem.2014.11.22824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The Royal College of Emergency Medicine. Severe Sepsis and Septic Shock, Clinical Audit 2016/17. National Report.; 2017.
- 26.Hayden GE, Tuuri RE, Scott R, Losek JD, Blackshaw AM, Schoenling AJ, et al. Triage sepsis alert and sepsis protocol lower times to fluids and antibiotics in the ED. Am J Emerg Med. 2016;34(1):1–9. 10.1016/j.ajem.2015.08.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Institute for Health and Care Excellence. Sepsis. Quality standard QS1612017.
- 28.Liu VX, Fielding-Singh V, Greene JD, Baker JM, Iwashyna TJ, Bhattacharya J, et al. The Timing of Early Antibiotics and Hospital Mortality in Sepsis. Am J Respir Crit Care Med. 2017;196(7):856–63. 10.1164/rccm.201609-1848OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stoneking LR, Winkler JP, DeLuca LA, Stolz U, Stutz A, Luman JC, et al. Physician documentation of sepsis syndrome is associated with more aggressive treatment. West J Emerg Med. 2015;16(3):401–7. 10.5811/westjem.2015.3.25529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marik PE, Farkas JD, Spiegel R, Weingart S. POINT: Should the Surviving Sepsis Campaign Guidelines Be Retired? Yes. Chest. 2019;155(1):12–4. 10.1016/j.chest.2018.10.008 [DOI] [PubMed] [Google Scholar]
- 31.Patel JJ, Bergl PA. COUNTERPOINT: Should Broad-Spectrum Antibiotics Be Routinely Administered to All Patients With Sepsis as Soon as Possible? No. Chest. 2019;156(4):647–9. 10.1016/j.chest.2019.05.031 [DOI] [PubMed] [Google Scholar]
- 32.IDSA Sepsis Task Force. Infectious Diseases Society of America (IDSA) POSITION STATEMENT: Why IDSA Did Not Endorse the Surviving Sepsis Campaign Guidelines. Clin Infect Dis. 2017;66(10):1631–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43(3):304–77. 10.1007/s00134-017-4683-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
List of ICD 10 codes used to search the National Patient Register.
(PDF)
Description of how missing data are treated and of how we fitted the regression models.
(PDF)
Sub-analyses of association between diagnostic measures and time to treatment and between time to treatment and mortality for the sub-group of patients with organ failure.
(PDF)
Description Patient flow diagram showing the number of patients included and excluded.
(TIF)
Data Availability Statement
As this study used data from the Norwegian Patient Registry, there are legal restrictions on sharing the data set. The registry is regulated according to the Act relating to Personal Health Data Registries (2014) and specific regulation for the registry under the provision of this act. These laws do not permit us to share these data for secondary use. Third parties can apply to obtain data from the Norwegian Directorate of Health, which is the body granting access to the registry. The Directorate responds to inquiries regarding the Norwegian Patient Registry via email helseregistre@helsedir.no. Data obtained from the Norwegian Patient Registry can be used to identify electronic health records at the hospitals, pending approval from ethics committee and hospitals.