Abstract
Activation of arginine–vasopressin is one of the hormonal responses to face vasodilation-related hypotension. Released from the post-pituitary gland, vasopressin induces vasoconstriction through the activation of V1a receptors located on vascular smooth muscle cells. Due to its non-selective receptor affinity arginine–vasopressin also activates V2 (located on renal tubular cells of collecting ducts) and V1b (located in the anterior pituitary and in the pancreas) receptors, thereby potentially promoting undesired side effects such as anti-diuresis, procoagulant properties due to release of the von Willebrand’s factor and platelet activation. Finally, it also cross-activates oxytocin receptors. During septic shock, vasopressin plasma levels were reported to be lower than expected, and a hypersensitivity to its vasopressor effect is reported in such situation. Terlipressin and selepressin are synthetic vasopressin analogues with a higher affinity for the V1 receptor, and, hence, potentially less side effects. In this narrative review, we present the current knowledge of the rationale, benefits and risks of vasopressin use in the setting of septic shock and vasoplegic shock following cardiac surgery. Clearly, vasopressin administration allows reducing norepinephrine requirements, but so far, no improvement of survival was reported and side effects are frequent, particularly ischaemic events. Finally, we will discuss the current indications for vasopressin and its agonists in the setting of septic shock, and the remaining unresolved questions.
Keywords: Vasopressin, Septic shock, Vasoplegia, Decatecholaminization
Background
Vasopressin (arginine–vasopressin, AVP, also called “antidiuretic hormone” ADH) is a natural hormone with potent vasoconstrictive effects. Its vasoconstrictive property was discovered in the nineteenth century by Oliver et al. after analysis of post-pituitary gland extracts [1]. While its vasoconstrictor effects are due to activation of V1a receptors, vasopressin also activates V2 and V1b as well as oxytocin receptors, thereby promoting anti-diuresis and exerting procoagulant activity. During the last three decades, its vasoconstrictor properties have prompted growing interest for its use in the management of vasodilatory shock.
In this review, we aim at describing the (patho)-physiological rationale for the use of AVP in distributive shock. Thereafter, we will report main results from animal and human studies, and describe benefits and risks associated with administration of vasopressin or its analogues. Finally, we will focus on vasopressin and its agonists use in the setting of septic shock and vasoplegic shock after cardiac surgery.
Physiology of vasopressin and its receptors
Vasopressin is a nine-amino-acid peptide, synthesized in the hypothalamus as a “pre-pro-hormone”. This precursor circulates along axons of magnocellular neurons, through the pituitary stalk, to the post-pituitary gland. Vasopressin is stored in the post-pituitary gland, mostly in the intracellular compartment. After stimulation, only 10–20% of the amount of vasopressin can be immediately released into blood circulation.
Physiologically, plasma osmolality as well as blood volume and pressure are the main regulators of vasopressin secretion. Clearly, the former is the most important one: increased plasma osmolality sensed by hypothalamic osmoreceptors, leads to a pronounced increase in the plasma vasopressin level. A 2% decrease in whole body water leads to a doubling in vasopressin level [2].
The latter, via hypovolemia and hypotension, induces stimulation of atrial volume receptors and carotid baroreceptors, which results in vasopressin secretion. Secretion of vasopressin is more sensitive to small osmolarity variations as compared to hypotension-related vasopressin release that requires large pressure and volume variations [3].
Vasopressin has a short plasma half-life of 5–15 min, its clearance mainly depending on renal and liver vasopressinases [4].
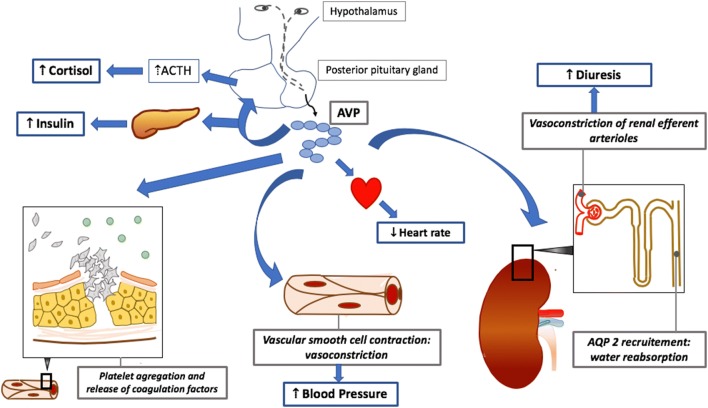
In the periphery, vasopressin binds to 3 receptor subtypes, all belonging to the family of membrane-bound G protein-coupled receptors [5]:
V1a receptors are located on vascular smooth muscle cells, their activation causes vascular smooth cell contraction.
V2 receptors are located on basolateral surface of renal tubular cells, mainly on collecting ducts. Vasopressin binding induces aquaporin 2 recruitment, which allows an increase in permeability of epithelial membrane to water, leading to water re-absorption.
V1b receptors are located in the anterior pituitary and in the pancreas. Vasopressin induces corticotropic axis stimulation (increase in cortisol) and insulin secretion.
Of note, other functions have been described. Vasopressin has procoagulant property: activation of V1a receptors leads to platelet aggregation, and extra-renal V2 receptors activation induces the release of coagulation factors [6, 7]. In addition, oxytocin and vasopressin can cross-activate their respective receptors [8, 9]. Figure 1 summarizes the physiologic effects of vasopressin.
Fig. 1.
Physiological effects of vasopressin. AVP Arginine VasoPressin, AQP2 Aquaporin 2. Vasopressin is synthesized in the hypothalamus and circulates along axons of magnocellular neurons to the post-pituitary gland. After stimulation, vasopressin is released into blood circulation, to 3 receptor subtypes. Binding on V1a receptors induces vascular smooth cell contraction in the periphery and on renal efferent arteriole and platelet aggregation. Vasopressin binding on renal V2 receptors causes aquaporin 2 recruitment, leading to water re-absorption and on extra-renal V2 receptors induces the release of coagulation factors. Binding on V1b receptors induces corticotropic axis stimulation and insulin secretion. During septic shock, vasopressin plasma level is low. Administration of vasopressin or its analogues induces a strong vasoconstriction, leading to an increase in blood pressure, and higher glomerular filtration rate
The ratio of V1/V2 effects reflects vascular selectivity. This ratio is close to 1 for vasopressin, in other words natural AVP has no receptor selectivity. Synthetic analogues, which have been tested in pre-clinical shock models and/or patients with vasodilatory shock of various causes, have higher vascular specificity. For example, terlipressin (Phe(2)-Orn(8)-vasotocin) has a V1/V2 ratio around 2.2 [10].
Physiopathological mechanisms involved in septic shock
Septic shock is characterized by micro- and macrocirculatory disturbances with a decrease in peripheral vascular resistance, maldistribution of cardiac output to organs, and impairment of oxygen extraction. Several mechanisms contribute to sepsis-related vasodilatation, and vasodilatation occurs despite high endogenous catecholamines levels and activation of the renin–angiotensin–aldosterone system [11, 12].
The impact of vasopressin on the vasomotor tone is marginal in healthy subjects. During shock, blood vasopressin concentration is initially high. However, for similar levels of hypotension Landry et al. showed in 19 patients with septic shock that vasopressin plasma level was inappropriately low, as compared to 12 patients with cardiogenic shock [13]. Data regarding the natural course of vasopressin level was reported in a prospective cohort of 182 patients [14]: the more serious the infection (sepsis versus severe sepsis versus septic shock), the lower the vasopressin level was. In septic shock, after an initial and transient increase, plasma levels of vasopressin decreased until day 4 [15], which coincided with a decreased post-pituitary storage [16].
In addition to the deficiency of circulating vasopressin, Landry et al. also highlighted the hypersensitivity of patients with septic shock to exogenous vasopressin administration: while arterial hypotension was corrected [13, 17] in patients with septic shock, similar infusion rates had no effect on blood pressure in healthy subjects. All these observations together with the fact that exogenous vasopressin offers an alternative mechanism of action independent of adrenergic receptor activation prompted the interest for this hormone in the management of patients with septic shock [12].
Haemodynamic effects of V1a agonist administration in septic shock
V1a agonists and cardiovascular system
In the experimental model, vasopressin administration resulted in various effects depending on the shock model and on vasopressin dose. When vasopressin was administered in hypodynamic endotoxin shock model, a decrease in cardiac output and myocardial ischaemia was observed [18–20]. In a hyperdynamic model of shock, the impact of vasopressin was different according to its infusion rate. High dose of vasopressin (greater than 0.15 UI/min) resulted in a decrease in cardiac output, oxygen consumption and in regional organ blood flow [21, 22]. When lower doses of vasopressin were tested (less than 0.1 U/min), mean arterial pressure was increased, without detrimental effect on cardiac output [23]. In another animal model (porcine faecal peritonitis) with infusion of low dose of vasopressin, heart rate and cardiac output were decreased without increase in troponin level nor change in myocardial relaxation, suggesting that vasopressin was safe regarding the theoretical risk of coronary vasoconstriction [24].
Exploratory clinical studies highlighted that vasopressin or terlipressin administration in septic shock patients allowed an increase in blood pressure and a decrease in norepinephrine requirement. The effect of vasopressin on cardiac output is more controversial. On one hand, non-randomized clinical studies reported a decrease in cardiac output [25, 26], on the other hand, a randomized study with small sample size did not confirm this finding. Finally, cardiac output, with similar target of blood pressure, was similar [27] or higher [28] in patients receiving vasopressin in addition to norepinephrine. Of note, vasopressin administration was safe regarding coronary circulation: its administration was not associated with differences between troponin serum levels, electrocardiogram patterns in a secondary analysis of a randomized controlled trial comparing norepinephrine and vasopressin in septic shock patients [29].
V1a agonists and splanchnic circulation
Because of its strong vasoconstrictor effect, concerns have been raised about vasopressin use and its impact on splanchnic circulation with a fear of splanchnic ischaemia [30] and liver dysfunction [31]. These arguments were turned down with experimental studies. It was demonstrated that with adequate fluid resuscitation, mesenteric flow and ileal microcirculation were preserved in a rat model of resuscitated endotoxin shock model with low doses of terlipressin [23]. These findings were in accordance with results of prospective randomized experimental study in a model of hyperdynamic porcine endotoxemia, where terlipressin administration was not associated with detrimental effect on hepatosplanchnic perfusion, oxygen exchange and metabolism [32]. Conversely, in an endotoxic pig model with high doses of vasopressin administration (0.28 UI/min), a decrease in splanchnic blood flow with an increased lactate release was observed [19]. Interestingly regarding safety concerns, clinical trials [28, 33] did not report side effects on splanchnic circulation with vasopressin administration.
V1a agonists and renal circulation
Distribution of V1a receptors in renal circulation is heterogeneous. The vasoconstrictor effect of vasopressin at low dose acts predominantly on renal efferent arterioles and has negligible effect on the afferent arterioles. This mechanism is related to a local phenomenon of nitrogen monoxide release [34, 35].
The efferent vasoconstriction induces a theoretical increase in glomerular renal perfusion pressure that results in higher glomerular filtration. Indeed, the first clinical studies confirmed this finding with increased diuresis and creatinine clearance in patients treated with vasopressin [25, 27].
V1a agonists and skin circulation
Vasopressin induces vasoconstriction of cutaneous vessels, with a dose–effect relationship. In a retrospective study, Dünser et al. reported ischaemic lesions of skin in almost one-third of patients (19/63) exposed to vasopressin [36]. Risk factors associated with the occurrence of ischaemic cutaneous lesions were overweight, high dose of norepinephrine, transfusion of platelets and fresh frozen plasma, history of peripheral arterial occlusive disease and the occurrence of septic shock. Only these last two items remained associated with the occurrence of cutaneous complications after multivariate analysis.
Current knowledge of vasopressin and analogues use in the management of septic shock
Vasopressin
Administration of vasopressin with or without norepinephrine during septic shock has been studied in large-scale studies, which assessed whether vasopressin administration could result in an improvement in survival and renal function.
Russel et al. in the VASST study (VAsopressin in Septic Shock Trial) [37], compared the effect of vasopressin administration (n = 396) versus norepinephrine administration (n = 382) in patients with septic shock, in a randomized, double-blinded placebo-controlled study. The primary endpoint was mortality at day 28. An a priori stratification with respect to severity was integrated into the study design: severity was defined according to the norepinephrine infusion rates required to maintain arterial pressure, i.e. < vs ≥ 15 µg/min. The vasopressin infusion rate was 0.01–0.03 U/min. No differences were observed between groups in survival at day 28 and 90. Furthermore, there was no difference in organ failure occurrence between groups. Of note, safety profile was reassuring with no significant difference between groups in side effects occurrence. In contrast to the authors’ initial hypothesis that the more severe patients would benefit from the vasopressin treatment, outcome did not differ in the stratum of patients with norepinephrine doses ≥ 15 µg/min; in patients with norepinephrine infusion rates < 15 µg/min, vasopressin administration was associated with significantly improved survival at day 28 (26.5% vs 35.7%, p = 0.05) and 90 (35.8% vs 46.1%, p = 0.04). It remains an open question, whether this effect was due to vasopressin per se and/or the fact that in the less severe patients, a higher proportion could be completely weaned from norepinephrine support [38]. A post hoc analysis of VASST study according to the Sepsis-3 definition confirmed this finding [39]: while in patients, who fulfilled the sepsis-3 criteria of septic shock, i.e. arterial hypotension requiring introduction of catecholamine to maintain mean blood pressure > 65 mmHg despite adequate fluid resuscitation and hyperlactatemia > 2 mmol/L, there was no difference in mortality, survival was increased in patients with hypotension requiring vasopressors alone without hyperlactatemia.
A further post hoc analysis of the VASST trial suggested an association between the use of vasopressin and hydrocortisone: vasopressin reduced mortality in patients, who—at the discretion of the attending physician—were treated with hydrocortisone. Conversely, in patients who did not received hydrocortisone, vasopressin administration was associated with higher mortality [40].
Another post hoc analysis of the VASST trial tried to assess the impact of vasopressin on kidney (dys)function: Gordon et al. analysed the 464 patients with acute kidney injury of VASST study cohort [41], categorizing them according to RIFLE classification [42]. Patients at “Risk” stage and treated with vasopressin had significantly less worsening of renal function (progression to “injury/failure” stage) than patients treated with norepinephrine.
The potential impact of hydrocortisone treatment together with a putative beneficial effect of vasopressin on AKI prompted the design of the VANISH study [43], which compared the effects of either vasopressin or norepinephrine as the vasopressor of first choice together with hydrocortisone or vehicle using a two-by-two factorial design. No interaction was identified between vasopressin and hydrocortisone [43]. Furthermore, neither mortality nor AKI were significantly influenced; nevertheless, the authors concluded that “the confidence interval included a potential clinically important benefit for vasopressin”, which should be tested further in larger trials.
Clearly, both the VANISH and VASST trials were “negative” in the sense that no superiority of vasopressin could be demonstrated. Nevertheless, these studies showed that vasopressin is not inferior to norepinephrine either, and, that its administration was not associated with higher rates of adverse effects, especially ischaemic events. Moreover, these studies demonstrated that vasopressin allows at least a reduction of norepinephrine infusion rates and fastened weaning from norepinephrine. In the context of “decatecholaminization”, vasopressin use limits norepinephrine infusion rates and potentially its related side effects [44]. Interestingly, in a retrospective study, patients with septic shock who received fixed-dose of vasopressin in association with norepinephrine had an improve prognosis when vasopressin infusion resulted in an increase in mean arterial pressure [45].
Vasopressin analogues: terlipressin and selepressin
Synthetic analogues of vasopressin with higher vascular selectivity (V1/V2 ratio > 1) were also studied in the setting of septic shock.
In a blinded, randomized study recruiting 32 patients with septic shock, terlipressin administration in combination with norepinephrine was superior to norepinephrine alone (complication and survival at day 7), but results have to be tempered due to the small sample size [46].
In 2018, Liu et al. reported results of a randomized multicentric double-blind study, aimed at comparing terlipressin and norepinephrine as first-line vasopressor agent in septic shock [47]. In this study, 526 patients were analysed: 260 received up to 4 mg terlipressin per day, and 266 received norepinephrine. There was no difference in mortality at day 28 between groups (primary endpoint). Likewise, improvement and variation of SOFA score until day 7 were comparable. Terlipressin administration was associated with an increase in adverse effects (30% vs 12%, p < 0.01). The most common was digital ischaemia (12.6% in terlipressin group versus 0.35% in norepinephrine group, p < 0.001). 76% of adverse effects occured during the first 24 h.
A more recent synthetic V1a agonist, selepressin, was reported, in a sheep model of faecal peritonitis, to be superior to norepinephrine and vasopressin. If, in established septic shock, selepressin maintained mean arterial pressure to a similar extent as did vasopressin and norepinephrine, selepressin administration resulted in reduced lung edema [48]. These results were in accordance with previous study, highlighting the reduced vascular leakage with selepressin administration [49].
Recently, the SEPSISACT study [50] compared with a randomized placebo-controlled trial the addition of selepressin to norepinephrine. This study was divided in two parts: the first was aimed at assessing the best-performing regimen of selepressin (between three dosing regimens of selepressin), and, in the second part, the authors compared this selepressin regimen to placebo. Among the 817 patients who completed the trial, no difference between the two groups on the primary composite endpoint was observed (ventilator and/or vasopressor free days within 30 days). Likewise, no difference in secondary endpoints was observed (mortality, need for renal replacement therapy and length of stay in the intensive care unit). Selepressin administration was not associated with higher rate of side effects.
A meta-analysis of 20 study including patients with septic shock suggested a potential improvement of survival with the use of vasopressin (9 studies) and its analogues (11 studies), when compared with adrenergic vasopressors (mostly norepinephrine). This meta-analysis underlined the additional risk of digital ischaemia [51]. In a recent meta-analysis of individual patients data from randomized studies (1453 septic shock patients) [52], no difference in mortality was found between vasopressin and norepinephrine. Furthermore, vasopressin use was not associated with more undesirable effect, but safety profiles were different: vasopressin led to more digital ischaemia, but fewer arrhythmias. This decrease in the incidence of arrhythmias was also reported in a meta-analysis dedicated to this specific question [53]. In this analysis were included randomized controlled trials aimed at comparing the association of vasopressin with norepinephrine to catecholamines alone for patients with distributive shock.
Current knowledge of vasopressin and analogues use in the management of vasoplegic shock after cardiac surgery
Furthermore, vasopressin was evaluated in the setting of vasoplegic shock after cardiac surgery. In 2003, among 48 patients with vasoplegic shock following cardiac surgery, a combination of vasopressin and norepinephrine versus norepinephrine alone showed an improvement of haemodynamic parameters, and fewer new-onset tachyarrhythmias when vasopressin was associated [28].
In VANCS trial [54], a randomized controlled monocentric study, patients in post-operative of cardiac surgery with refractory hypotension after fluid resuscitation, without cardiac output impairment (> 2.2 L/min/m2), received vasopressin (0.01 at 0.06 U/min) or norepinephrine (10 at 60 µg/min). The primary composite endpoint (death or major complication in the 30 post-operative days) occurred more frequently in norepinephrine group than in the vasopressin group. Interestingly, patients treated with vasopressin presented less new-onset tachyarrhythmias. There were no harm effects (digital, myocardial, mesenteric ischaemia nor hyponatremia) in the vasopressin group.
Conclusion: what is the current place for vasopressin and its analogues in the management of vasoplegic shock states?
Recommendations of Surviving Sepsis Campaign suggest administration of vasopressin in second-line after norepinephrine, to maintain mean blood pressure goal or to decrease norepinephrine dosage [55].
Use of vasopressin or analogue in first line is marginal [56], and its use has never been associated with improved prognosis of patient in septic shock.
After this review of current knowledge, we might suggest that vasopressin and analogues could be considered:
Early, in patient with sepsis with low blood pressure, without hyperlactatemia, alone or in association with norepinephrine.
In association with norepinephrine, to decrease norepinephrine infusion rate in order to limit the undesirable effects, according to the concept of “decatecholaminization” [57].
Acknowledgements
Not applicable.
Authors’ contributions
JD, NF, PR and PA wrote the manuscript. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Oliver G, Schäfer EA. On the physiological action of extracts of pituitary body and certain other glandular organs: preliminary communication. J Physiol (Lond). 1895;18(3):277–279. doi: 10.1113/jphysiol.1895.sp000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robertson GL, Shelton RL, Athar S. The osmoregulation of vasopressin. Kidney Int. 1976;10(1):25–37. doi: 10.1038/ki.1976.76. [DOI] [PubMed] [Google Scholar]
- 3.Dunn FL, Brennan TJ, Nelson AE, Robertson GL. The role of blood osmolality and volume in regulating vasopressin secretion in the rat. J Clin Invest. 1973;52(12):3212–3219. doi: 10.1172/JCI107521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sklar AH, Schrier RW. Central nervous system mediators of vasopressin release. Physiol Rev. 1983;63(4):1243–1280. doi: 10.1152/physrev.1983.63.4.1243. [DOI] [PubMed] [Google Scholar]
- 5.Birnbaumer M. Vasopressin receptors. Trends Endocrinol Metab. 2000;11(10):406–410. doi: 10.1016/S1043-2760(00)00304-0. [DOI] [PubMed] [Google Scholar]
- 6.Mannucci PM, Aberg M, Nilsson IM, Robertson B. Mechanism of plasminogen activator and factor VIII increase after vasoactive drugs. Br J Haematol. 1975;30(1):81–93. doi: 10.1111/j.1365-2141.1975.tb00521.x. [DOI] [PubMed] [Google Scholar]
- 7.Haslam RJ, Rosson GM. Aggregation of human blood platelets by vasopressin. Am J Physiol. 1972;223(4):958–967. doi: 10.1152/ajplegacy.1972.223.4.958. [DOI] [PubMed] [Google Scholar]
- 8.Song Z, Albers HE. Cross-talk among oxytocin and arginine-vasopressin receptors: relevance for basic and clinical studies of the brain and periphery. Front Neuroendocrinol. 2018;51:14–24. doi: 10.1016/j.yfrne.2017.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zingg HH. Vasopressin and oxytocin receptors. Baillieres Clin Endocrinol Metab. 1996;10(1):75–96. doi: 10.1016/S0950-351X(96)80314-4. [DOI] [PubMed] [Google Scholar]
- 10.Bernadich C, Bandi JC, Melin P, Bosch J. Effects of F-180, a new selective vasoconstrictor peptide, compared with terlipressin and vasopressin on systemic and splanchnic hemodynamics in a rat model of portal hypertension. Hepatology. 1998;27(2):351–356. doi: 10.1002/hep.510270206. [DOI] [PubMed] [Google Scholar]
- 11.Chernow B, Roth BL. Pharmacologic manipulation of the peripheral vasculature in shock: clinical and experimental approaches. Circ Shock. 1986;18(2):141–155. [PubMed] [Google Scholar]
- 12.Levy B, Fritz C, Tahon E, Jacquot A, Auchet T, Kimmoun A. Vasoplegia treatments: the past, the present, and the future. Crit Care. 2018;22(1):52. doi: 10.1186/s13054-018-1967-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Landry DW, Levin HR, Gallant EM, Ashton RC, Seo S, D’Alessandro D, et al. Vasopressin deficiency contributes to the vasodilation of septic shock. Circulation. 1997;95(5):1122–1125. doi: 10.1161/01.CIR.95.5.1122. [DOI] [PubMed] [Google Scholar]
- 14.Lin IY, Ma HP, Lin ACM, Chong CF, Lin CM, Wang TL. Low plasma vasopressin/norepinephrine ratio predicts septic shock. Am J Emerg Med. 2005;23(6):718–724. doi: 10.1016/j.ajem.2005.02.055. [DOI] [PubMed] [Google Scholar]
- 15.Sharshar T, Blanchard A, Paillard M, Raphael JC, Gajdos P, Annane D. Circulating vasopressin levels in septic shock. Crit Care Med. 2003;31(6):1752–1758. doi: 10.1097/01.CCM.0000063046.82359.4A. [DOI] [PubMed] [Google Scholar]
- 16.Sharshar T, Carlier R, Blanchard A, Feydy A, Gray F, Paillard M, et al. Depletion of neurohypophyseal content of vasopressin in septic shock. Crit Care Med. 2002;30(3):497–500. doi: 10.1097/00003246-200203000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Landry DW, Levin HR, Gallant EM, Seo S, D’Alessandro D, Oz MC, et al. Vasopressin pressor hypersensitivity in vasodilatory septic shock. Crit Care Med. 1997;25(8):1279–1282. doi: 10.1097/00003246-199708000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Wilson MF, Brackett DJ, Archer LT, Hinshaw LB. Mechanisms of impaired cardiac function by vasopressin. Ann Surg. 1980;191(4):494–500. doi: 10.1097/00000658-198004000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martikainen TJ, Tenhunen JJ, Uusaro A, Ruokonen E. The effects of vasopressin on systemic and splanchnic hemodynamics and metabolism in endotoxin shock. Anesth Analg. 2003;97(6):1756–1763. doi: 10.1213/01.ANE.0000087039.60041.2E. [DOI] [PubMed] [Google Scholar]
- 20.Avontuur JA, Bruining HA, Ince C. Inhibition of nitric oxide synthesis causes myocardial ischemia in endotoxemic rats. Circ Res. 1995;76(3):418–425. doi: 10.1161/01.RES.76.3.418. [DOI] [PubMed] [Google Scholar]
- 21.Westphal M, Stubbe H, Sielenkämper AW, Borgulya R, Van Aken H, Ball C, et al. Terlipressin dose response in healthy and endotoxemic sheep: impact on cardiopulmonary performance and global oxygen transport. Intensive Care Med. 2003;29(2):301–308. doi: 10.1007/s00134-002-1546-5. [DOI] [PubMed] [Google Scholar]
- 22.Malay M-B, Ashton JL, Dahl K, Savage EB, Burchell SA, Ashton RC, et al. Heterogeneity of the vasoconstrictor effect of vasopressin in septic shock. Crit Care Med. 2004;32(6):1327–1331. doi: 10.1097/01.CCM.0000128578.37822.F1. [DOI] [PubMed] [Google Scholar]
- 23.Asfar P, Pierrot M, Veal N, Moal F, Oberti F, Croquet V, et al. Low-dose terlipressin improves systemic and splanchnic hemodynamics in fluid-challenged endotoxic rats. Crit Care Med. 2003;31(1):215–220. doi: 10.1097/00003246-200301000-00033. [DOI] [PubMed] [Google Scholar]
- 24.Simon F, Giudici R, Scheuerle A, Gröger M, Asfar P, Vogt JA, et al. Comparison of cardiac, hepatic, and renal effects of arginine vasopressin and noradrenaline during porcine fecal peritonitis: a randomized controlled trial. Crit Care. 2009;13(4):R113. doi: 10.1186/cc7959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morelli A, Rocco M, Conti G, Orecchioni A, De Gaetano A, Cortese G, et al. Effects of terlipressin on systemic and regional haemodynamics in catecholamine-treated hyperkinetic septic shock. Intensive Care Med. 2004;30(4):597–604. doi: 10.1007/s00134-003-2094-3. [DOI] [PubMed] [Google Scholar]
- 26.Holmes CL, Walley KR, Chittock DR, Lehman T, Russell JA. The effects of vasopressin on hemodynamics and renal function in severe septic shock: a case series. Intensive Care Med. 2001;27(8):1416–1421. doi: 10.1007/s001340101014. [DOI] [PubMed] [Google Scholar]
- 27.Patel BM, Chittock DR, Russell JA, Walley KR. Beneficial effects of short-term vasopressin infusion during severe septic shock. Anesthesiology. 2002;96(3):576–582. doi: 10.1097/00000542-200203000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Dünser MW, Mayr AJ, Ulmer H, Knotzer H, Sumann G, Pajk W, et al. Arginine vasopressin in advanced vasodilatory shock: a prospective, randomized, controlled study. Circulation. 2003;107(18):2313–2319. doi: 10.1161/01.CIR.0000066692.71008.BB. [DOI] [PubMed] [Google Scholar]
- 29.Mehta S, Granton J, Gordon AC, Cook DJ, Lapinsky S, Newton G, et al. Cardiac ischemia in patients with septic shock randomized to vasopressin or norepinephrine. Crit Care. 2013;17(3):R117. doi: 10.1186/cc12789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Asfar P, Bracht H, Radermacher P. Impact of vasopressin analogues on the gut mucosal microcirculation. Best Pract Res Clin Anaesthesiol. 2008;22(2):351–358. doi: 10.1016/j.bpa.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 31.Asfar P, Radermacher P, Calès P, Oberti F. The effects of vasopressin and its analogues on the liver and its disorders in the critically ill. Curr Opin Crit Care. 2010;16(2):148–152. doi: 10.1097/MCC.0b013e328335a35b. [DOI] [PubMed] [Google Scholar]
- 32.Asfar P, Hauser B, Iványi Z, Ehrmann U, Kick J, Albicini M, et al. Low-dose terlipressin during long-term hyperdynamic porcine endotoxemia: effects on hepatosplanchnic perfusion, oxygen exchange, and metabolism. Crit Care Med. 2005;33(2):373–380. doi: 10.1097/01.CCM.0000152253.45901.FB. [DOI] [PubMed] [Google Scholar]
- 33.Klinzing S, Simon M, Reinhart K, Bredle DL, Meier-Hellmann A. High-dose vasopressin is not superior to norepinephrine in septic shock. Crit Care Med. 2003;31(11):2646–2650. doi: 10.1097/01.CCM.0000094260.05266.F4. [DOI] [PubMed] [Google Scholar]
- 34.Edwards RM, Trizna W, Kinter LB. Renal microvascular effects of vasopressin and vasopressin antagonists. Am J Physiol. 1989;256(2 Pt 2):F274–F278. doi: 10.1152/ajprenal.1989.256.2.F274. [DOI] [PubMed] [Google Scholar]
- 35.Rudichenko VM, Beierwaltes WH. Arginine vasopressin-induced renal vasodilation mediated by nitric oxide. J Vasc Res. 1995;32(2):100–105. doi: 10.1159/000159082. [DOI] [PubMed] [Google Scholar]
- 36.Dünser MW, Mayr AJ, Tür A, Pajk W, Barbara F, Knotzer H, et al. Ischemic skin lesions as a complication of continuous vasopressin infusion in catecholamine-resistant vasodilatory shock: incidence and risk factors. Crit Care Med. 2003;31(5):1394–1398. doi: 10.1097/01.CCM.0000059722.94182.79. [DOI] [PubMed] [Google Scholar]
- 37.Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877–887. doi: 10.1056/NEJMoa067373. [DOI] [PubMed] [Google Scholar]
- 38.Bracht H, Calzia E, Georgieff M, Singer J, Radermacher P, Russell JA. Inotropes and vasopressors: more than haemodynamics! Br J Pharmacol. 2012;165(7):2009–2011. doi: 10.1111/j.1476-5381.2011.01776.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Russell JA, Lee T, Singer J, Boyd JH, Walley KR. The septic shock 3.0 definition and trials: a vasopressin and septic shock trial experience*. Critical Care Med. 2017;45(6):940–948. doi: 10.1097/CCM.0000000000002323. [DOI] [PubMed] [Google Scholar]
- 40.Russell JA, Walley KR, Gordon AC, Cooper DJ, Hébert PC, Singer J, et al. Interaction of vasopressin infusion, corticosteroid treatment, and mortality of septic shock. Crit Care Med. 2009;37(3):811–818. doi: 10.1097/CCM.0b013e3181961ace. [DOI] [PubMed] [Google Scholar]
- 41.Gordon AC, Russell JA, Walley KR, Singer J, Ayers D, Storms MM, et al. The effects of vasopressin on acute kidney injury in septic shock. Intensive Care Med. 2010;36(1):83–91. doi: 10.1007/s00134-009-1687-x. [DOI] [PubMed] [Google Scholar]
- 42.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative workgroup Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8(4):R204–R212. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gordon AC, Mason AJ, Thirunavukkarasu N, Perkins GD, Cecconi M, Cepkova M, et al. Effect of early vasopressin vs norepinephrine on kidney failure in patients with septic shock: the VANISH randomized clinical trial. JAMA. 2016;316(5):509–518. doi: 10.1001/jama.2016.10485. [DOI] [PubMed] [Google Scholar]
- 44.Lesur O, Delile E, Asfar P, Radermacher P. Hemodynamic support in the early phase of septic shock: a review of challenges and unanswered questions. Ann Intensive Care. 2018;8(1):102. doi: 10.1186/s13613-018-0449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sacha GL, Lam SW, Duggal A, Torbic H, Bass SN, Welch SC, et al. Predictors of response to fixed-dose vasopressin in adult patients with septic shock. Ann Intensive Care. 2018;8(1):35. doi: 10.1186/s13613-018-0379-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xiao X, Zhang J, Wang Y, Zhou J, Zhu Y, Jiang D, et al. Effects of terlipressin on patients with sepsis via improving tissue blood flow. J Surg Res. 2016;200(1):274–282. doi: 10.1016/j.jss.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 47.Study Group of investigators. Liu Z-M, Chen J, Kou Q, Lin Q, Huang X, et al. Terlipressin versus norepinephrine as infusion in patients with septic shock: a multicentre, randomised, double-blinded trial. Intensive Care Med. 2018;44(11):1816–1825. doi: 10.1007/s00134-018-5267-9. [DOI] [PubMed] [Google Scholar]
- 48.He X, Su F, Taccone FS, Laporte R, Kjølbye AL, Zhang J, et al. A selective V1A receptor agonist, selepressin, is superior to arginine vasopressin and to norepinephrine in ovine septic shock*. Critical Care Med. 2016;44(1):23–31. doi: 10.1097/CCM.0000000000001380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Maybauer MO, Maybauer DM, Enkhbaatar P, Laporte R, Wiśniewska H, Traber LD, et al. The selective vasopressin type 1a receptor agonist selepressin (FE 202158) blocks vascular leak in ovine severe sepsis*. Crit Care Med. 2014;42(7):e525–e533. doi: 10.1097/CCM.0000000000000300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Laterre P-F, Berry SM, Blemings A, Carlsen JE, François B, Graves T, et al. Effect of selepressin vs placebo on ventilator- and vasopressor-free days in patients with septic shock: the SEPSIS-ACT randomized clinical trial. JAMA. 2019 doi: 10.1001/jama.2019.14607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jiang L, Sheng Y, Feng X, Wu J. The effects and safety of vasopressin receptor agonists in patients with septic shock: a meta-analysis and trial sequential analysis. Crit Care. 2019;23(1):91. doi: 10.1186/s13054-019-2362-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nagendran M, Russell JA, Walley KR, Brett SJ, Perkins GD, Hajjar L, et al. Vasopressin in septic shock: an individual patient data meta-analysis of randomised controlled trials. Intensive Care Med. 2019;45(6):844–855. doi: 10.1007/s00134-019-05620-2. [DOI] [PubMed] [Google Scholar]
- 53.McIntyre WF, Um KJ, Alhazzani W, Lengyel AP, Hajjar L, Gordon AC, et al. Association of vasopressin plus catecholamine vasopressors vs catecholamines alone with atrial fibrillation in patients with distributive shock: a systematic review and meta-analysis. JAMA. 2018;319(18):1889. doi: 10.1001/jama.2018.4528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hajjar LA, Vincent JL, Barbosa Gomes Galas FR, Rhodes A, Landoni G, Osawa EA, et al. Vasopressin versus norepinephrine in patients with vasoplegic shock after cardiac surgery: the VANCS randomized controlled trial. Anesthesiology. 2017;126(1):85–93. doi: 10.1097/ALN.0000000000001434. [DOI] [PubMed] [Google Scholar]
- 55.Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–377. doi: 10.1007/s00134-017-4683-6. [DOI] [PubMed] [Google Scholar]
- 56.Scheeren TWL, Bakker J, De Backer D, Annane D, Asfar P, Boerma EC, et al. Current use of vasopressors in septic shock. Anna Intensive Care. 2019;9(1):20. doi: 10.1186/s13613-019-0498-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Asfar P, Russell JA, Tuckermann J, Radermacher P. Selepressin in septic shock: a step toward decatecholaminization? Crit Care Med. 2016;44(1):234–236. doi: 10.1097/CCM.0000000000001441. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.