Good outcomes for breast cancer patients require readily accessible early detection, diagnostic, and treatment services. This study aimed to identify barriers and facilitators to breast cancer care from the perspectives of women with and without a breast cancer diagnosis in Kenya.
Keywords: Breast cancer, Early detection of cancer, Cancer diagnosis and treatment, Focus groups, Hermeneutic phenomenology
Abstract
Background.
Early detection and prompt access to quality treatment and palliative care are critical for good breast cancer outcomes. Interventions require understanding of identified barriers and facilitators to care. A hermeneutic phenomenological approach, whose purpose is to describe feelings and lived experiences of participants, can expand the existing scope of understanding of barriers and facilitators in accessing breast cancer care in Kenya.
Methods.
This is qualitative research applying focus groups and a hermeneutic phenomenological approach to identify barriers and facilitators to breast cancer care from the knowledge, perceptions, and lived experiences of women with and without a diagnosis of breast cancer in Kenya. We conducted four focus group discussions with 6–11 women aged 30–60 years in each. Groups were classified according to breast cancer diagnosis and socioeconomic status. The transcribed discussions were coded independently by two investigators. Together they reviewed the codes and identified themes.
Results.
The key barriers were costs, inadequate knowledge, distance to health facilities, communication with health providers, medicines stockouts, long waiting periods, limited or no counseling at diagnosis, patient vulnerability, and limited access to rehabilitation items. Facilitators were dependable social support, periodical access to subsidized awareness, and early detection services and friendly caregivers. We found no marked differences in perceptions between groups by socioeconomic status.
Conclusion.
There is need for targeted awareness and education for health providers and the public, early detection services with onsite counseling and cost mitigation. Support from the society and religious organizations and persons may be leveraged as adjuncts to conventional management. Further interpretations are encouraged.
Implications for Practice.
Continuing cancer education for health providers in technical skills for early detection, treatment, and survivorship care, as well as nontechnical skills like communication, and an understanding of their patients’ preferences and socioeconomic status may guide individualized management plans and positively affect patient experiences. Patients and the general public also need education on cancer to avoid misconceptions and inaccuracies that perpetuate fear, confusion, delayed presentation for treatment, and stigma. Critical analysis of the cancer care value chain and processes, development, and implementation of interventions to reduce costs while streamlining processes may improve client experiences.
Introduction
The estimated annual number of new cases of breast cancer (BC) in Kenya is about 6,000 with approximately 2,550 deaths. By 2025, a 35% increase is projected [1]. Good population outcomes require readily accessible early detection, diagnostic, and treatment services [2]. Although several studies in sub‐Saharan Africa (SSA), including Kenya, have identified barriers and facilitators to early detection, diagnosis, and treatment, it is not clear if the list is exhaustive. Barriers identified include low or lack of BC awareness, partner consensus, lack of information, distant health facilities, long queues in hospitals, costs, fear, stigma, and inadequate health professionals to perform tests or to provide genetic counseling [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16]. Facilitators are educational messages and social support from religious persons and partners [10], [11]. We aimed to expand the scope of current research and extend multidisciplinary involvement. What are the barriers and facilitators to accessing women breast cancer care (BCC) in Kenya? Is there a difference in knowledge and perception between women with and without a BC diagnosis? Is there a difference by socioeconomic status? And what are the lived experiences of these women when seeking and during care? We used the hermeneutic phenomenological approach to elicit feelings and lived experiences in participants’ own statements that may pave the way for our readers to draw otherwise implicit information based on their own expertise. We leveraged focus groups’ advantage of participant interaction to draw out more and richer information. Bradbury‐Jones et al. suggest that “use of focus groups within a phenomenology framework may provide a greater understanding of phenomenon under study” [17]. To our knowledge, this is the first hermeneutic phenomenological study conducting standardized focus group discussions using similar discussion guides for women with and without a diagnosis of BC in SSA.
Materials and Methods
This was a qualitative study using focus groups and hermeneutic (interpretive) phenomenology. Ethical approvals were obtained from the Kenyatta National Hospital‐University of Nairobi Ethics and Research Committee and Research Triangle Institute.
Data Collection
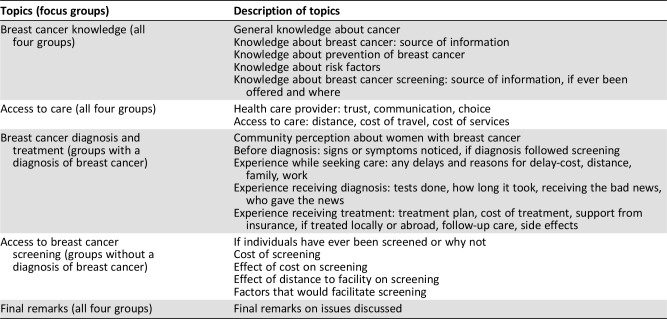
We created a focus group discussion guide based on key concepts of access to BC care in Kenya (Table 1). We recruited women diagnosed with BC (for groups designated BCa) through membership lists of our partner organizations, Kenya Cancer Association and Kenya Hospices and Palliative Care Association, and their affiliates. The group of women without a BC diagnosis were recruited through general outreach. Each group was further separated into two cohorts based on socioeconomic status: high socioeconomic status (HSES) and low socioeconomic status (LSES). The resulting four groups (BCa‐HSES, BCa‐LSES, HSES, and LSES) were homogenous by BC diagnosis and socioeconomic status. After eligibility assessment, women were approached by trained research assistants for consent to participate. Participants were drawn from Nairobi county, an urban setting and its environs. Table 2 details the characteristics of the four focus groups. Those who had had a diagnosis of BC were within 3 years postdiagnosis to minimize recall bias. Each individual provided written consent after being informed that the purpose of the discussion was for us to understand the issues related to the use of health care services and specifically their knowledge about cancer and use of BC services and that the findings would help us identify optimal client‐centered approaches for scaling up services. Four focus group discussions, with 6–11 women aged between 30 and 60 years in each, were conducted in Nairobi, Kenya, between February and June 2018.
Table 1. Focus group discussion topics on women breast cancer (women only).
Table 2. Description of participants of four focus groups drawn from Nairobi, Kiambu, and Machakos Counties of Kenya.
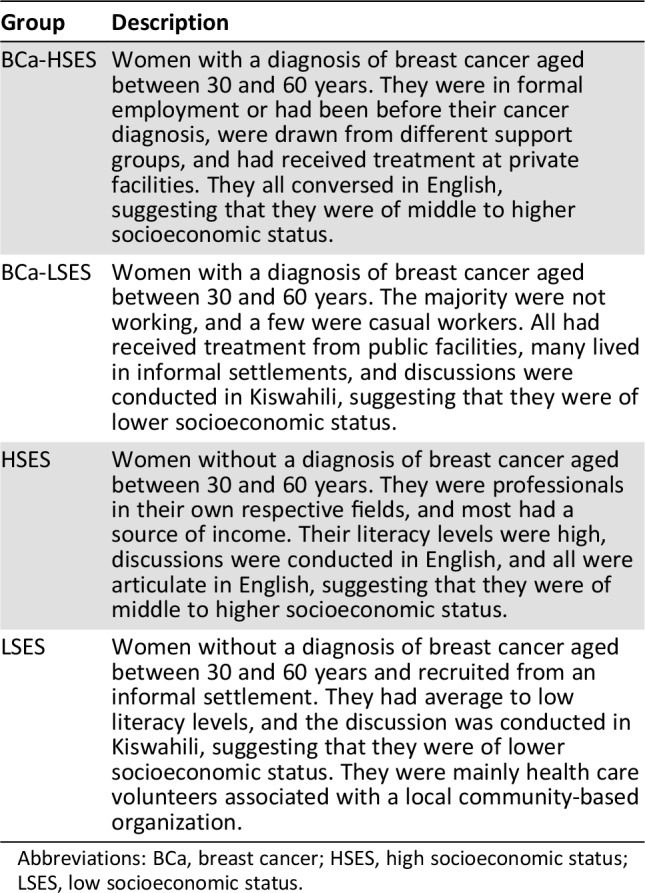
Abbreviations: BCa, breast cancer; HSES, high socioeconomic status; LSES, low socioeconomic status.
Trained and experienced interviewers facilitated the discussions with at least three note takers per discussion. Participants were individually asked to share their knowledge, perceptions, and lived experiences on the key concepts under study leading to discussions within the groups. We sought to exhaust information on concepts by providing adequate time for responses. Discussions were held in English and Kiswahili as appropriate, in quiet secluded rooms that were free from interruptions. Participation was voluntary, each participant was offered $5.00 as travel compensation, and refreshments were provided.
Data Analysis
Note takers’ transcripts were merged manually soon after each discussion by investigator R.G. who then returned them to the note takers for verification. The four transcripts were read many times by investigators R.G. and S.S. to internalize the discussions. The data in the transcripts were coded line by line by R.G. and S.S. independently. R.G. and S.S. met, discussed the codes for consensus, and categorized the codes. They developed a two‐by‐two matrix with the columns representing BC diagnosis status and the rows representing socioeconomic status. This was to better visualize the coded data by the originating focus group and to identify codes that were common across focus groups. We used the categories (themes) to structure our report.
R.G. and S.S. returned to the transcripts and color‐coded statements that were important and held meaning to support answers to our research questions according to the source focus group. These color‐coded excerpts were transferred appropriately into our report narrative, and the colors helped identify the source focus group.
Results
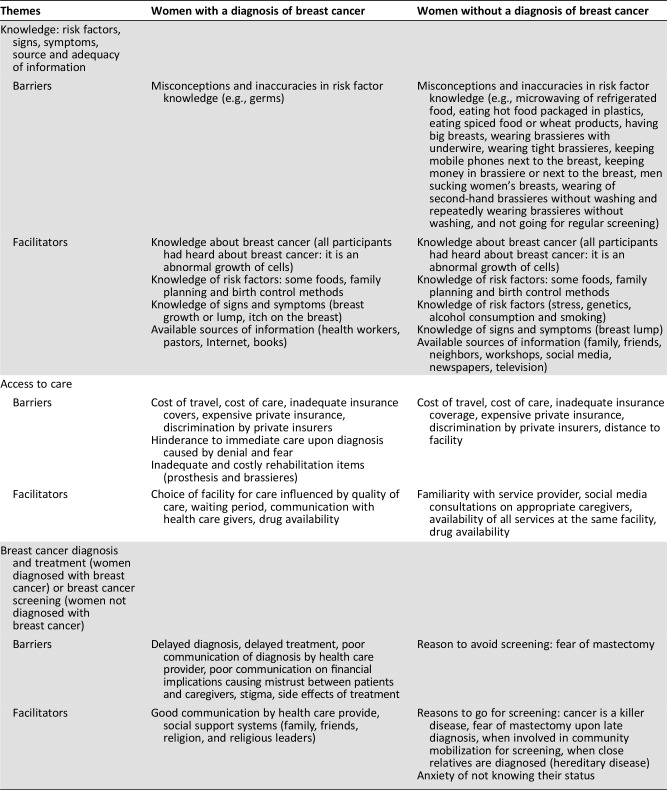
Table 3 displays the emerging themes identified by investigators, and the narrative includes verbatim data organized as barriers and facilitators, both focusing on diagnostic and treatment delays and experiences. Although women with a BC diagnosis were led to discuss diagnosis and treatment, whereas those without a cancer diagnosis were led to discuss screening, these discussions often crossed over because the concepts seemed interrelated. Some barriers and facilitators were common between women with and without a BC diagnosis, whereas others were specific to groups. Those without a BC diagnosis seemed to have more misconceptions and inaccuracies than those who had had a BC diagnosis, and there were no marked differences in knowledge and perceptions by socioeconomic status.
Table 3. Emerging themes identified as possible barriers and facilitators to breast cancer early detection and subsequent treatment among women in Kenya.
Key Barriers
Barrier 1: Inadequate Breast Cancer Knowledge.
General Knowledge and Perceptions About Cancer.
Participants described cancer as “a growth,” “it is about cells that grow abnormally” (BCa‐LSES), a “bad disease that has no cure,” it “does not discriminate and any one can get it” (LSES). From a nonlayman perspective, some of their statements were inaccurate: “an early diagnosis of cancer leads to healing” (LSES) and that “breast cancer is a growth that can make the hair to fall off” (LSES). The women expressed themselves with some undertones of fear that cancer is a death sentence: “When I hear the word cancer, I see death, I see a growth that leads to death” (BCa‐LSES).
Knowledge on Risk Factors of Breast Cancer.
Although all participants had heard about BC, their knowledge of risk factors was at times incorrect. We describe this in Table 3. Genetics was highlighted by a woman (BCa‐LSES) whose mother and grandmother had been diagnosed with BC, so she believed that genes had a role to play in her own diagnosis. Another woman said that “Probably chances are higher compared to those [families] without” (HSES).
Knowledge on Early Detection of Breast Cancer.
Only a few of the participants had ever been screened for BC. There was good knowledge that “early screening would lead to early diagnosis and better management of the disease” (BCa‐LSES) and “screening can prevent cancer” (BCa‐LSES). In the HSES group, most women said they knew about breast self‐examination (BSE) and clinical breast examination (CBE). Some could perform BSE confidently, and some could not perform it. Those who had heard about CBE did not know how it was done or thought that they could do it on themselves. Few had heard about mammograms, and only one participant had had mammography.
Several women in the HSES group were somewhat convinced that the lump was the only sign or symptom of BC: “lump—the only one known—there could be other signs but lump is all that is known,” “breast self‐exam … if no lump … good to go,” and “we don't know about any other information.” We probed if they knew about discharge from the nipple. One participant said that people would think that a discharge from the nipple was an infection, and the others agreed. Another woman said that pain in the breast was an unclear sign of cancer. Reddening of the breast was mentioned in the LSES group: “If one notices certain symptoms like reddening of the breast, they need to be checked immediately.”
Barrier 2: Health System Delays.
A participant from the BCa‐HSES group whose late mother had BC grew up with a lot of fear and used to go for screening whenever there was a free offer. Lumps were found in her breasts but “the nurses kept saying it was milk”—diagnosis was delayed to stage 3B. Another participant from the same group who knew about BC as a teenager when her mother was diagnosed said that it took 2 years for her own diagnosis to be made. It was a painless lump. Her doctor noticed masses in her breast upon a mammogram and asked her not to panic—“it was scar tissue.” Later on, she felt “not very fine” and decided to seek another opinion. She had magnetic resonance imaging, then fine needle aspiration followed by a biopsy. “I was given my results in an unsealed envelope and when I checked on my way out of the doctor's clinic, my diagnosis was CA Breast.” In the same group, a participant went to a gynecologist because in her opinion, “breast issues are a gynecology issue.” She was given vitamin A. She later visited a private hospital because the public hospital had long queues, and her diagnosis was made.
Barrier 3: Inadequate Sources of and Information on Cancer.
Even with the sources of information listed in Table 3, participants expressed general inadequacy of the information: “is breast cancer communicable?” (LSES), “does oral sex cause cancer?” (LSES), “what is the Kenyan government doing to reduce the prevalence and delay of treatment of cancer in the country?” (LSES), “the government should enlighten people in the rural areas about cancer; it bothers me that these people are ignorant” (BCa‐LSES), “most people think treatment is only chemotherapy and don't know about the complementary” (HSES), “doctors need to advise on diet and nutrition … not just medication and surgeries,” “people do not know about palliative care” (HSES). “The process from screening to treatment should be clear to the patient, explanation of risks of treatment especially on fertility to be done” (BCa‐HSES), “patients need to have information, what is the road map, i.e., possible outcomes; risks; childbirth” (BCa‐HSES), “who should do it (give information)? at what point? should it be a counselor, oncologist? this should be clear … before chemo, [the patient] should be called together with her husband to be explained to that sex life suffers” (BCa‐HSES), and “fertility risks to be explained to young women” (BCa‐HSES).
There were suggestions from the HSES group to “package the information (on cancer) in a way that is understandable …. languages … for different audiences.” Current “information is not adequate … should go on public campaigns/national announcements … (like) polio, HIV/AIDS … package [information] appropriately … cancer affects everyone … have mass campaigns, not to wait for October … once a year is not enough.”
Barrier 4: Experience with Treatment.
Communication of Diagnosis and Treatment Plan.
Participants had varied reactions to the communication about their diagnosis by health providers: “I was traumatized by the way the diagnosis was presented to me. I changed the doctor” and “I was handed my diagnosis without any counseling” (BCa‐HSES). A participant from the BCa‐HSES group was told by her oncologist that “your cancer is a very bad cancer. It does not respond to chemo, it is really bad.” She was devastated. However, the same oncologist explained the treatment plan well and she also “googled” (searched the Internet). Another participant was not counseled on how long the treatment was going to take and later realized that it was a long process (BCa‐LSES).
A participant said, “I had a wonderful experience with the doctor, oncologist and surgeon.” This participant was an employee of the hospital where her treatment was given. She understood the reason why she had to lose a breast. Her surgeon encouraged her by assuring her that “people have lived for over 20 years” (BCa‐HSES) after surgery.
Delays in Treatment.
The immediate reaction upon diagnosis for one participant from the BCa‐HSES group was that “If I go to hospital, I'm so dead.” She tried to negotiate within herself and was in denial for 6 months. Another participant said that “I googled what malignancy means and I knew I was dying soon.” It took her 1 week of searching for information to understand the surgery process before a nurse advised her to see an oncologist before surgery. A third participant took 2 weeks, within which she did not believe that the results were hers. She had the tests repeated, then she was “ready for anything” (acceptance). Other periods of delay reported were 2 days in complete denial then 2 months before seeking treatment, 3 months, and 5–6 months, respectively. There were some participants from the BCa‐LSES group who sought treatment immediately.
Side Effects of Treatment.
Treatment side effects were described as a problem with the second chemotherapy cycle, which almost made one participant give up on treatment. Participants experienced lowered immunity and hemoglobin levels, swollen arm, pain in the bones on the side with cancer, numbness in the hands, heat flashes in the head, problems in the bones, issues with blood flow, a weak hand, pain in the joints, menopause or “disappeared monthly periods,” and memory lapses.
Barrier 5: Access and Cost of Care.
The average travel time to health facilities for cancer care was 1 hour with a mean transport cost of about U.S. $2.00 for a return trip by public transport. It was at times difficult to reach the health facility if the respondents had no money (BCa‐LSES).
To choose a health facility, the LSES group considered proximity to their residences, quality of care provided, service provider's attitude, a facility with “all services under one roof,” familiarity with facility health workers, medicine availability, short waiting time, and affordability. Most of the participants in the HSES group did not have a personal doctor, and if they needed a check‐up, they would look for recommendations from social media groups. They would not just walk into any clinic. For the BCa‐LSES participants, choice of service provider varied for various reasons: “though [X] hospital is expensive, I went there because the doctors in public health facilities were on strike,” “the need for immediate treatment made me go to a private hospital,” “one may find treatment machines at [X] hospital faulty and because there is need for consistency in treatment, one opts to go to a private health facility,” “[X] facility staff listen to patients,” “some doctors in public facilities just write and they do not talk to patients; they do not allow conversations between themselves and patients saying that the patients are too many and there is therefore no time, so you find that one does not have the time to express themselves,” “doctors in public facilities are not bad but one may need an interpreter,” and “nurses at [X] hospital sometimes cause delays.” Medicine availability also influenced choice of health care facility.
All participants agreed that services were expensive. Coping financially included going for subsidized screening, buying chemotherapy medicines from the chemist and taking them to the oncologist, fundraising, employers’ contributions, out of pocket expenditures even if one had insurance, enrolling on the National Hospital Insurance Fund (NHIF), and using private insurance, although a participant was told to her face that she was a high risk and should not have been covered by insurance. She said, “discrimination by insurance companies is real … individual cover is quite difficult especially if one has cancer but group cover happens” (BCa‐HSES). Participants also indicated that “NHIF needs to streamline the cancer funding because even if they say they fund chemo, having cancer you can't be sure, cancer is like a Damocles’ sword—it can come back again and you need to keep checking (regular testing), NHIF should re‐look into the coverage. I was lucky my employer covered everything” and asked, “why can't they treat cancer patients for free like HIV patients?” (BCa‐HSES).
Mistrust exists between patients and the health providers concerning financial issues. A participant said that she had realized that doctors “are not treating in the interest of the patient. Every doctor will tell you what is good for them in order to make money.” The general observation was that doctors based their treatment on perceived financial ability of the patient and that hospitals, especially private ones, aimed to benefit financially by misadvising patients on tests or treatments to take. For example, one may not have needed surgery but was still made to go through it, and could even have died from the operation.
Barrier 6: Stigma.
A woman was exposed to public stigma when, because of financial constraints, she organized a fundraising: “due to fundraising women got curious and would stare at me and I had to change my residence” (BCa‐HSES). Another woman said that “only the immediate family was informed. I had to lie due to stigma. Those in rural areas think that breast cancer is a death sentence” (BCa‐HSES). At one participant's workplace, cancer was associated with death because an employee had died of liver cancer. Colleagues perceived people with a diagnosis of cancer as very sick people who were expected to die. She said, “I had to keep it a secret at the workplace. I had to lie that it was the lump that was removed and I would sometimes find people staring directly at my breast” (BCa‐HSES). “Some people discriminate against those who are sick and think that one can infect them and you will even find that some of the friends will step aside or avoid the sick person” (BCa‐LSES).
Facilitators
Psychosocial Support.
All the participants who had been diagnosed with BC agreed that they needed social support—friends, family, church, employers, and support groups. A participant from the BCa‐HSES group belonged to a support group where they had activities like “dancing in our night gowns,” and this made her very happy. Individual coping was enhanced by keeping “a strong faith” (religion), avoiding negative people and toxic friends, positive thinking, and reading positive books. Health providers also encouraged patients: “I was diagnosed at stage 3 and the nurse attending to me told me that, ‘you are not God; cancer has no medication; you are the medicine and so you need to take it positively; everyone has their day and it's not only cancer that kills,’” “Dr. [X] is good and has taken care of me since I got sick and it's now 8 years” (BCa‐LSES—this participant had had two primary breast cancer diagnoses), and “I had been told that if one is touched with a knife, meaning if one is operated on, there are negative consequences and so I decided to go to a traditional healer but then I was advised in good time” (BCa‐LSES). It was mentioned that private sector employers “usually sack people when they get sick due to absenteeism” (BCa‐HSES). On the home front, it was reported that a husband got advice to re‐marry prior to his wife's death and that another husband said, “I don't want to sleep with a dead body” (BCa‐LSES).
Discussion
We sought to identify barriers and facilitators to breast cancer early detection and subsequent treatment by combining focus group discussions and a hermeneutic phenomenology approach among women with and without a diagnosis of breast cancer in Kenya. The focus groups were further categorized by socioeconomic status. Using standardized discussion guides, we found that those without a BC diagnosis seemed to have more misconceptions and inaccuracies in their knowledge about cancer than those who had had a BC diagnosis. This could be because those with a diagnosis have generally had more interaction with information as they sought help. Studies in SSA show that general knowledge and awareness about cancer is good but inadequate [4], [11], [14]. Inadequate knowledge is associated with late presentation, late detection, and poor outcomes [16]. In our study, a lump in the breast seemed to be the main known symptom of BC. Knowledge of symptoms and signs based on recall methods, like in our case, is generally lower than in studies that use recognition methods [18]. Studies in Kenya using recognition methods have revealed good knowledge of other symptoms [7], [19].
Social support from family, friends, and religious persons and organizations is a facilitator to BCC [10], [11]. Our findings support this conclusion, but we also report situations similar to those in Uganda in which husbands’ support was lacking [10]. Religious persons were a dependable coping support. Some women in SSA make their first stop at their churches before seeking treatment [20]. This support could be leveraged from the time of diagnosis as an adjunct to conventional care.
Insensitive disclosure of BC diagnoses by health providers to patients has been reported [10], and our findings concur. This may result from time constraints and heavy workload for health providers and lack of knowledge of how to communicate bad news. Inadequate or lack of counseling at the time of diagnosis contributed to devastation and delay in seeking treatment for many women.
Fear affected women both with and without a BC diagnosis. Fear of mastectomy and fear of dying from cancer are common barriers to BCC in SSA [4], [11], [12], [13]. There is also fear of exposure to public stigma upon disclosure of one's diagnosis [10]. This may hinder patients and their families from accessing social and financial support.
Known barriers to care such as cost, distance to equipped health facilities [4], [11], [14], and strikes by hospital staff [11] were discussed. Health system barriers have extensively featured in Kenyan government documents [21], [22], [23]. Kenya has adopted universal health coverage aiming to improve health systems and eliminate catastrophic health expenditures. NHIF has substantially eased affordability by covering some diagnostics and treatment costs. However, recommendations were that NHIF needs to cover all costs—screening, diagnosis, treatment, and palliative care.
Tailored educative messages may reach those of the LSES through face‐to‐face gatherings, whereas social media, Internet, and television may work for those of HSES. Studies in Kenya have shown that younger women prefer education through electronic media and community health workers (CHWs), rural women prefer information through CHWs, and urban women are inclined to media and mother‐child clinics [4]. Sixty‐six percent of women prefer their health providers to be sources of educative messages [24]. Educative messages sent to women, men, and children may eliminate fear and misconceptions, enhance self‐awareness, and reduce stigma. Health providers need education to avoid missed opportunities for early detection and to avoid wrong diagnosis and delayed diagnosis [11]. Educating health providers on soft skills of communicating diagnoses, treatment plans and prognosis, and money matters may cultivate mutual trust and is consistent with other study recommendations that physicians provide sensitive disclosure through explanation of the disease, treatment, and prognosis [10].
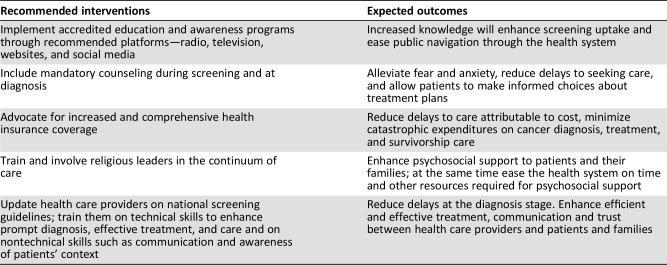
This study was carried out in Nairobi and its environs where most of the cancer care services in Kenya are found and may therefore not be generalizable. However, we were able to gather information on BCC that is similar to other studies carried out in Kenya and other SSA countries [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16]. Women's views on aspects of BCC and their recommendations are considered and presented in Table 4 with expected outcomes. Each of our four groups was unique by BC diagnosis and socioeconomic status. Using standardized discussion guides, we found some similarities and differences in perceptions while noting that even CHWs in the LSES group had limited knowledge on BC. We provided adequate time to exhaust discussion on each concept and have reported many participants’ statements verbatim. We encourage further research to ascertain saturation of themes.
Table 4. Recommended interventions and expected outcomes for breast cancer early detection and subsequent treatment in Kenya.
Conclusion
Inadequate knowledge among both health providers and the public, inadequate awareness and screening services, cost of services, and communication between patients and their health providers were key barriers. Social and spiritual support by religious persons was accessible. In using hermeneutic phenomenology, we hope that every reader will individually identify phenomena from the participants’ verbatim expressions and explore interventions in their own spheres of expertise. For example, researchers may develop studies from as many deductions as they can make from the verbatim writings, policy makers may include mandatory counseling during screenings and at diagnosis, educationists may include soft skills of communication in teaching curricula, managers in industry may examine value chains to identify processes and inputs that can be modified to reduce costs, and financial counseling could help patients make informed choices on treatment and survivorship plans with understanding of cost implications.
Acknowledgments
The authors thank all participants; RTI International for funding the study; Kenya Hospices and Palliative Care Association (KEHPCA) and Kenya Cancer Association (KENCANSA) for selecting participants and organizing focus groups; and Kenyatta National Hospital (KNH), Nairobi Radiotherapy & Cancer Centre, and Kibera Community Self Help Project (KICOSHEP) for identifying participants.
Author Contributions
Conception/design: Robai Gakunga, Zipporah Ali, Anne Korir, Sujha Subramanian
Provision of study material or patients: Asaph Kinyanjui, Zipporah Ali, Emily Ochieng’, Nancy Gikaara, Florence Maluni, Anne Korir
Collection and/or assembly of data: Robai Gakunga, Emily Ochieng’, Nancy Gikaara, Florence Maluni, Anne Korir, Sujha Subramanian
Data analysis and interpretation: Robai Gakunga, Asaph Kinyanjui, Zipporah Ali, Emily Ochieng’, Nancy Gikaara, Florence Maluni, David Wata, Mercy Kyeng’, Anne Korir, Sujha Subramanian
Manuscript writing: Robai Gakunga, Asaph Kinyanjui, Sujha Subramanian
Final approval of manuscript: Robai Gakunga, Asaph Kinyanjui, Zipporah Ali, Emily Ochieng’, Nancy Gikaara, Florence Maluni, David Wata, Mercy Kyeng’, Anne Korir, Sujha Subramanian
Disclosures
The authors indicated no financial relationships.
References
- 1.Ferlay J, Ervik M, Lam F et al. Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer; 2018. https://gco.iarc.fr/today. Accessed October 15, 2018. [Google Scholar]
- 2.Pace LE, Shulman LN. Breast cancer in sub‐Saharan Africa: Challenges and opportunities to reduce mortality. The Oncologist 2016;21:739–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Busakhala NW, Chite FA, Wachira J et al. Screening by clinical breast examination in Western Kenya: Who comes? J Glob Oncol 2016;2:114–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kisiangani J, Baliddawa J, Marinda P et al. Determinants of breast cancer early detection for cues to expanded control and care: The lived experiences among women from Western Kenya. BMC Womens Health 2018;18:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee S, Gedleh A, Hill JA et al. In their own words: A qualitative study of Kenyan breast cancer survivors’ knowledge, experiences, and attitudes regarding breast cancer genetics. J Glob Oncol 2017;4:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sherman S, Okungu V. Access to breast cancer treatment services in Mombasa County, Kenya: A quality of care analysis of patient and survivor experiences. Am J Publ Health Res 2018;6:189–194. [Google Scholar]
- 7.Naanyu V, Asirwa CF, Wachira J et al. Lay perceptions of breast cancer in Western Kenya. World J Clin Oncol 2015;6:147–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wachira J, Chite AF, Naanyu V et al. Barriers to uptake of breast cancer screening in Kenya. East Afr Med J 2014;91:391–397. [PubMed] [Google Scholar]
- 9.Makau‐Barasa LK, Greene SB, Othieno‐Abinya NA et al. Improving access to cancer testing and treatment in Kenya. J Global Oncol 2018;4:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meacham E, Orem J, Nakigudde G et al. Exploring stigma as a barrier to cancer service engagement with breast cancer survivors in Kampala, Uganda. Psychooncology 2016;25:1206–1211. [DOI] [PubMed] [Google Scholar]
- 11.Pruitt L, Mumuni T, Raikhel E et al. Social barriers to diagnosis and treatment of breast cancer in patients presenting at a teaching hospital in Ibadan, Nigeria. Glob Public Health 2015;10:331–344. [DOI] [PubMed] [Google Scholar]
- 12.Moodley J, Cairncross L, Naiker T et al. Understanding pathways to breast cancer diagnosis among women in the Western Cape Province, South Africa: A qualitative study. BMJ Open 2016;6:e009905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martei YM, Vanderpuye V, Jones BA. Fear of mastectomy associated with delayed breast cancer presentation among Ghanaian women. The Oncologist 2018;23:1446–1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jedy‐Agba E, McCormack V, Olaomi O et al. Determinants of stage at diagnosis of breast cancer in Nigerian women: Sociodemographic, breast cancer awareness, health care access and clinical factors. Cancer Causes Control 2017;28:685–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonsu AB, Ncama BP. Recognizing and appraising symptoms of breast cancer as a reason for delayed presentation in Ghanaian women: A qualitative study. PLoS One 2019;14:e0208773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akuoko CP, Armah E, Sarpong T et al. Barriers to early presentation and diagnosis of breast cancer among African women living in sub‐Saharan Africa. PLoS One. 2017;12:e0171024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bradbury‐Jones C, Sambrook S, Irvine F. The phenomenological focus group: An oxymoron? J Adv Nurs 2009;65:663–671. [DOI] [PubMed] [Google Scholar]
- 18.McCutchan GM, Wood F, Edwards A et al. Influences of cancer symptom knowledge, beliefs and barriers on cancer symptom presentation in relation to socioeconomic deprivation: A systematic review. BMC Cancer 2015;15:1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Subramanian S, Gakunga R, Jones MD et al. Establishing cohorts to generate the evidence base to reduce the burden of breast cancer in sub‐Saharan Africa: Results from a feasibility study in Kenya. J Glob Oncol 2019;5:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ndejjo R, Mukama T, Kiguli J et al. Knowledge, facilitators and barriers to cervical cancer screening among women in Uganda: A qualitative study. BMJ Open 2017;7:e016282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ministry of Health, Kenya . National Cancer Control Strategy 2017‐2022. Nairobi, Kenya: Ministry of Health; June 2017. http://kehpca.org/wp‐content/uploads/KENYA‐NATIONAL‐CANCER‐CONTROL‐STRATEGY‐2017‐2022.pdf. Accessed October 24, 2018.
- 22.Ministry of Health, Kenya . Kenya Health Policy 2014‐2030. Nairobi, Kenya: Ministry of Health; July 2014. http://publications.universalhealth2030.org/uploads/kenya_health_policy_2014_to_2030.pdf. Accessed October 24, 2018.
- 23.Ministry of Health, Kenya . Kenya National Strategy for the Prevention and Control of Non‐Communicable Diseases 2015‐2020. Nairobi, Kenya: Ministry of Health; 2015. http://ilakenya.org/wp‐content/uploads/2015/08/Kenya‐national‐strategy‐for‐NCDs‐2015‐2020.pdf. Accessed October 24, 2018.
- 24.Scheel JR, Molina Y, Patrick DL et al. Breast cancer downstaging practices and breast health messaging preferences among a community sample of urban and rural Ugandan women. J Glob Oncol 2016;3:105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]