Abstract
This is a case report of a woman in her sixth decade of life diagnosed with primary angiosarcoma of the breast using mammography and ultrasound, confirmed with imaging-guided biopsy, and finally treated with surgery and radiation. Imaging studies obtained and discussed include mammography, ultrasonography, and MRI. Further discussion on the presenting symptoms, useful imaging modalities, and treatment options takes place. It is important to consider primary angiosarcoma of the breast, though rare, in any woman presenting with a palpable breast mass and, if feasible, an MRI will be most helpful in the diagnosis of this rare tumor.
Keywords: Angiosarcoma, Primary angiosarcoma, Breast, Breast imaging
Introduction
Primary angiosarcoma of the breast is a rare, rapidly growing vascular tumor. The primary type of angiosarcoma differs from the secondary type in that it presents in premenopausal women and arises sporadically. The secondary type is usually associated with prior radiation treatment and presents later in life. Initial imaging findings in primary angiosarcoma may be nonspecific, leading to a delay in diagnosis. Our case is a unique primary angiosarcoma in a postmenopausal patient. Her case, as well as the imaging findings, are discussed.
Case report
A 58-year-old woman, with past medical history of hypertension, obstructive sleep apnea and hyperlipidemia, and no history of prior malignancy, presented for screening mammogram which revealed an evolving asymmetry in the central superior aspect of the left breast. The patient was then referred for, and obtained, a diagnostic mammogram of the left breast including digital 2D and tomosynthesis views, along with ultrasonography. All were found to be benign and no further workup was done or recommended regarding this.
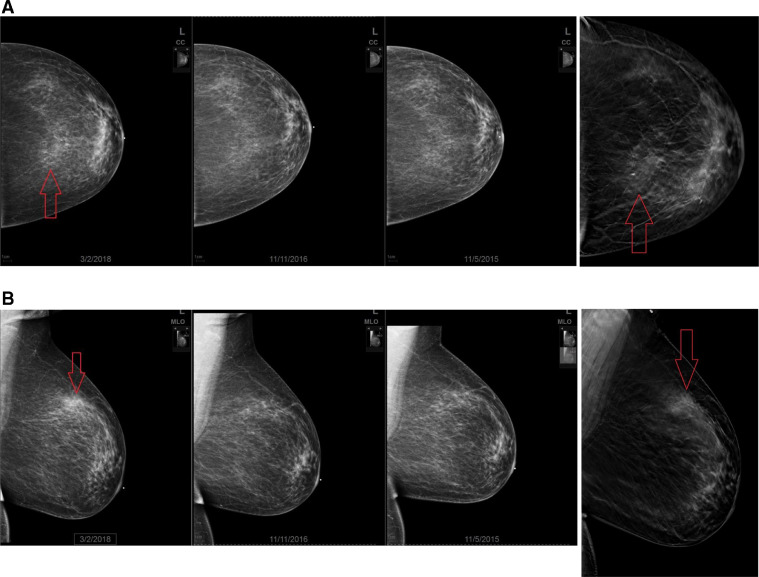
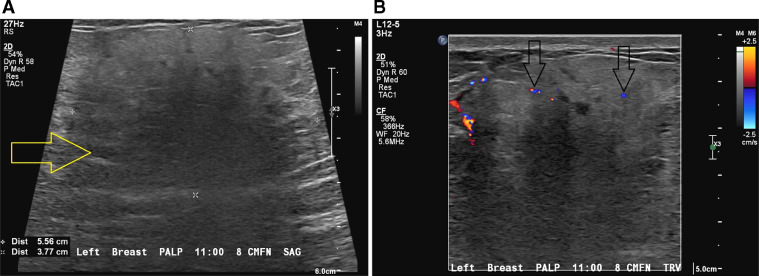
Six months later, the patient felt a lump in the superior aspect of her left breast. She presented to her primary care provider who found it was tender, but not warm, swollen or discolored. The patient was then referred for diagnostic work up including mammogram and ultrasound and given antibiotics in case of infection. The mammogram confirmed presence of a developing asymmetry in the superior slightly medial left breast (Fig. 1) and the ultrasound showed a new area of mixed echogenicity with areas of posterior acoustic shadowing (Fig. 2) and minimal internal vascularity on color Doppler assessment.
Fig. 1.
A and B. Craniocaudal (A) and mediolateral oblique (B) conventional and tomosynthesis mammography images demonstrate a developing focal asymmetry in the upper inner left breast at mid depth (red arrow). There are no associated calcifications, skin thickening, nipple retraction or lymphadenopathy. (Color version of figure is available online.)
Fig. 2.
A and B. Targeted sonogram of the left breast demonstrates an ill-defined heterogeneous predominantly hypoechoic mass (yellow arrow) with associated posterior acoustic shadowing at the 11:00 axis 8.0 cm from the nipple. Color Doppler image demonstrates foci of vascular flow within the mass (black arrows). (Color version of figure is available online.)
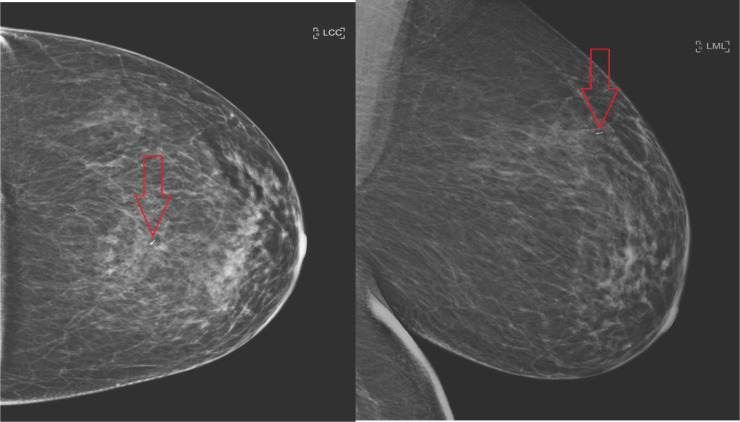
Ultrasound guided biopsy followed (Fig. 3). Pathology showed high grade malignant vascular proliferation, with cytologic atypia and increased mitotic activity, infiltrating benign breast tissue. The greatest dimension of the tumor found on histology was 1.9 cm and positive tumor markers included CD31, CD34, and smooth muscle actin. The tumor was labeled as unifocal, 5.0 cm high grade angiosarcoma of the left breast, stage II (T1, N0, M0). The patient then elected to undergo a bilateral total mastectomy with left sentinel node mapping and biopsy without reconstruction. Before the procedure, the patient obtained an MRI of the breast and a PET/CT.
Fig. 3.
Craniocaudal and mediolateral oblique conventional mammography images demonstrate a biopsy clip in the corresponding location of focal asymmetry in the upper inner left breast at mid depth (red arrows). (Color version of figure is available online.)
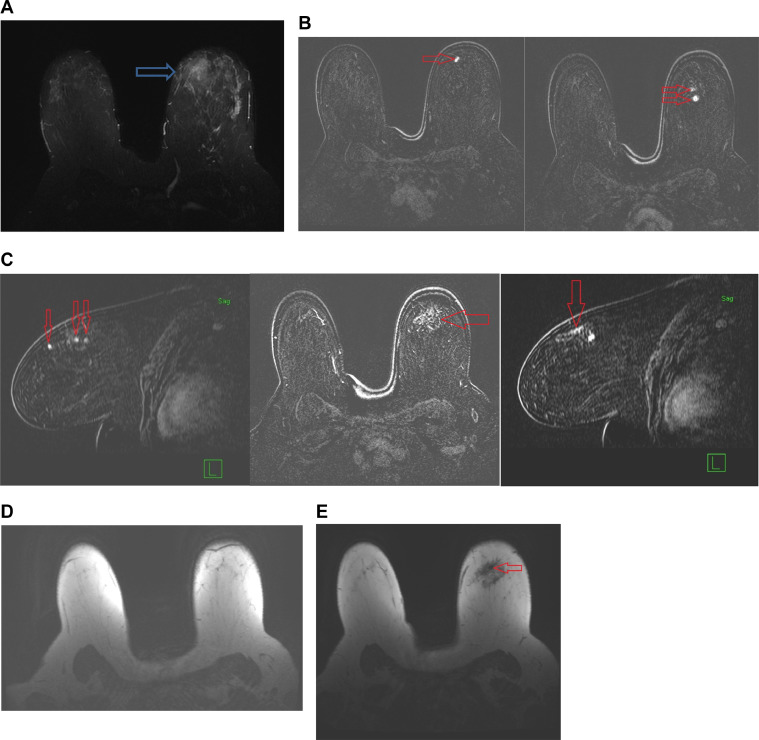
MRI of the left breast identified 3 early and avidly enhancing irregular masses in the upper outer quadrant at mid-depth arranged in a linear fashion starting at the 11:00 axis anteriorly and extending to the 12:00 axis posteriorly which span approximately 5 cm in AP dimension (Fig. 4). In addition, there was also a nonmass-like enhancement in the upper inner quadrant (containing the biopsy clip) which begins to cross midline across the 12:00 axis and extends for approximately 5 × 5 × 3.2 cm transverse by AP by craniocaudad. There was also marked surrounding T2 signal hyperintensity on STIR sequence, likely representing edema and/or nonenhancing tumor. Asymmetric patchy T2 signal hyperintensity also infiltrated the subareolar and upper outer quadrant parenchyma. No lymphadenopathy was found on MRI. The PET/CT showed a hypermetabolic ill-defined tissue in the left upper breast with SUV max 2.8.
Fig. 4.
(A) Axial STIR image demonstrates mild T2 hyperintensity in the area of developing mammographic asymmetry and sonographic mass. (B) and (C) Axial and sagittal post contrast Subtraction MRI images demonstrate three early and avidly enhancing masses at the 11:00-12:00 axis of the right breast (red arrow). There is associated interspersed nonmass enhancement in the surrounding tissue. In total the abnormal enhancement spans approximately 5.0 cm. (D) T1 axial nonfat saturation image demonstrates no axillary lymphadenopathy on either side. (E) T1 axial nonfat saturation image demonstrates susceptibility artifact from biopsy clip (red arrow). (Color version of figure is available online.)
The mastectomy was performed, and the surgical specimen evaluation confirmed 5.0 cm angiosarcoma in the left breast. Resection margins were found to be negative and 2 sentinel lymph nodes showed no evidence of metastatic tumor. After the surgery, the patient met with a medical oncologist who found no role for chemotherapy. However, adjuvant radiation therapy was recommended to 60 Gy for local control. She is 6 months postmastectomy and is recurrence-free. She will continue to obtain chest CTs every 3-4 months to monitor for recurrence.
Discussion
Angiosarcomas of the breast are rare tumors. Two types exist, primary and secondary, with the former being much rarer, accounting for only 20% of angiosarcomas [1] and less than 0.4% of all malignant neoplasms [2]. These primary angiosarcomas of the breast usually occur sporadically in young women during the third and fourth decades of life. Secondary angiosarcomas, the more common type, are associated with external beam radiation in patients undergoing treatment for adenocarcinoma of the breast. They usually occur several years after primary treatment with breast conservation therapy with an average latency period of 5-6 years [3]. Furthermore, they usually present late in the seventh decade of life, much later than primary angiosarcoma of the breast. Our patient, who presented in her late 50s is unique, in that her disease was primary and presented at an age typical of secondary angiosarcoma.
Prognosis for patients with primary angiosarcoma is dependent on grade. For grade 1 tumors patients have a 76% probability of disease-free survival 5 years after the initial treatment, whereas for grade 3 tumors the probability drops to 15% [4]. Metastases for primary angiosarcoma are usually hematogenous rather than through lymphatics, and have been known to most frequently metastasize to the lungs, bones, and liver [3].
Patients with angiosarcoma often present with a palpable mass in the breast [1]. This is a nonspecific finding and can lead to a delay in diagnosis and treatment. Primary angiosarcoma masses have been reported to be rapidly growing with a mean tumor size around 6 cm. In addition, they are associated with a bluish discoloration of the skin [5], unlike the patient described in our case who presented with a palpable mass which was tender but not discolored.
The difficulty in the diagnosis of angiosarcoma is associated with the nonspecific findings found on initial imaging. The most common mammographic finding is an ill-defined noncalcified mass or focal asymmetry [5]. Despite mammography being of little help in the diagnosis of angiosarcoma, sonography is more useful. Yang et al., in a case study, found the typical sonographic findings of angiosarcoma to be abnormal, diffuse, mixed hyperechogenic, and hypoechogenic regions without a discrete mass in 38% of patients, as well as hypervascularity on color Doppler. This is consistent with the ultrasound of our patient, which showed a vague area of mixed echogenicity.
Arguably the most useful radiographic test in identifying angiosarcoma of the breast is an MRI. T1-weighted MRI will show a heterogenous mass with low signal intensity, whereas a T2-weighted MRI will show high signal intensity. Tumor grade is correlated with the enhancement on MRI, with high-grade angiosarcomas showing rapid enhancement with washout, and low-grade angiosarcomas showing progressive enhancement [3]. T2-weighted MRI may also show hemorrhage or blood lakes in high grade tumors [3]. Our patient, who obtained an MRI after diagnosis was confirmed with US-guided biopsy, showed 3 early, avidly enhancing irregular masses with surrounding T2 signal hyperintensity.
The general treatment for either form of angiosarcoma of the breast is surgical resection. Although our patient received a sentinel node biopsy in addition to her mastectomy, which was found to be benign, this is generally not required as the tumor does not usually spread through lymphatics, as mentioned above, but instead spreads hematogenously. Furthermore, chemotherapy has been shown to reduce the rate of local recurrence in patients with angiosarcoma [6], despite our patient not receiving chemotherapy. Adjuvant radiation, similar to our patient's postoperative plan, has been shown to reduce cell population in secondary angiosarcoma tumors which are rapidly growing [7], however, not much data exists on adjuvant radiation for primary tumors.
When a patient presents with a palpable breast mass and benign findings on mammogram, it is important to have breast angiosarcoma on the differential. Referral for an ultrasound or, if possible, MRI will be of significant help in identifying this rapidly growing tumor.
References
- 1.Desbiens, C, J-C Hogue, and Y Lévesque. “Primary breast angiosarcoma: avoiding a common trap.” Research article. Case Rep Oncol Med, 2011. doi: 10.1155/2011/517047. [DOI] [PMC free article] [PubMed]
- 2.Kaklamanos I G, Birbas K, Syrigos KN, Vlachodimitropoulos D, Goutas N, Bonatsos G. Breast angiosarcoma that is not related to radiation exposure: a comprehensive review of the literature. Surg Today. 2011;41(February (2)):163–168. doi: 10.1007/s00595-010-4341-x. [DOI] [PubMed] [Google Scholar]
- 3.Glazebrook KN, Magut MJ, Reynolds C. Angiosarcoma of the breast. Am J Roentgenol. 2008;190(February (2)):533–538. doi: 10.2214/AJR.07.2909. [DOI] [PubMed] [Google Scholar]
- 4.Rosen PP, Kimmel M, Ernsberger D. Mammary angiosarcoma: the prognostic significance of tumor differentiation. Cancer. 1988;62(November (10)):2145–2151. doi: 10.1002/1097-0142(19881115)62:10%3C2145::AID-CNCR2820621014%3E3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 5.Yang WT, Bryan T, Hennessy J, Dryden MJ, Valero V, Hunt KK, Krishnamurthy S. Mammary angiosarcomas: imaging findings in 24 patients. Radiology. 2007;242(March (3)):725–734. doi: 10.1148/radiol.2423060163. [DOI] [PubMed] [Google Scholar]
- 6.Cohen-Hallaleh RB, Smith HG, Smith RC, Stamp GF, Al-Muderis O, Thway K. Radiation induced angiosarcoma of the breast: outcomes from a retrospective case series. Clin Sarcoma Res. 2017;7(August) doi: 10.1186/s13569-017-0081-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feigenberg SJ, Mendenhall NP, Reith JD, Ward JR, Copeland EM. Angiosarcoma after breast-conserving therapy: experience with hyperfractionated radiotherapy. Int J Radiat Oncol Biol Phys. 2002;52(March (3)):620–626. doi: 10.1016/s0360-3016(01)02669-4. [DOI] [PubMed] [Google Scholar]