Abstract
Purpose
To report an extremely rare case involving a 41-year-old man with nine intraocular cilia embedded in the retina after a perforating ocular injury caused by a metal wire. This case is particularly rare because of the number and location of the cilia.
Observations
The patient underwent an uneventful corneal suturing and extracapsular extraction of the damaged lens of his right eye. Intraocular foreign bodies were discovered following surgery and were removed at a later date. Following lens extraction and ocular repair, the patient's best-corrected visual acuity (BCVA) was counting fingers. Fundus examination during follow-up revealed several eyelashes embedded in the retina. Thirty-two days after the injury, the patient showed signs of ocular inflammation. Therefore, the patient underwent vitrectomy and intraocular foreign body removal. Nine cilia were embedded in the retina at the posterior perforation site. At the final follow-up visit, his BCVA was 20/25.
Conclusion and importance
This report describes an unusual case where intraocular cilia were embedded in the retina after a perforating ocular injury. The eyelashes caused an intraocular inflammatory reaction that subsided after their removal.
Keywords: Cilia, Ocular foreign body, Retina, Vitrectomy
1. Introduction
Cases with presence of intraocular cilia is extremely rare [0.4% of all cases of intraocular foreign bodies (IOFBs) 1] and was first reported by Lerche in 1835. Most cilia enter the eye during penetrating ocular injury or during intraocular surgery 1, but Oh et al. 2 found the presence of a cilium in the vitreous cavity without any apparent etiology. Interestingly, the retained eyelashes were found entrapped in the cornea, anterior and posterior chambers, iris, lens, vitreous cavity, and retina. 1,3 Intraocular cilia are most commonly found in the anterior segment, but it is extremely rare for cilia to be present in the posterior portion of the eye. 4
The largest study on retained eyelashes found that injury caused by a metal wire accounted for 54% of the cases. 1 The presence of intraocular cilia are more frequently associated with slow-moving objects penetrating the eye (e.g., a wire) because their low speed allows sufficient time for the eyelids to close before ocular penetration. 1,5
Intraocular reactions to cilia are variable and unpredictable. Some patients exhibit absolutely no reaction (Yalniz-Akkaya 6 reported the presence of intraocular cilia for as long as 50 years), while some patients develop severe intraocular inflammation. Complications caused by penetrating injury with retained cilia can include corneal edema, bullous keratopathy, granulomatous, non-granulomatous iridocyclitis, cyst formation, lens abscess, vitreous traction, retinal detachment, endophthalmitis, and sympathetic ophthalmia. 1 Therefore, some surgeons prefer to monitor the asymptomatic patients with intraocular cilia, while some prefer to surgically remove the cilia before the onset of potentially devastating complications. 1,6 Here, we report a rare case involving a 41-year-old man with nine intraocular cilia embedded in the retina after a perforating ocular injury caused by a metal wire.
2. Case report
A 41-year-old caucasian male, primary school teacher presented at our ophthalmic emergency room (ER) 1 h after incurring a perforating ocular injury in his right eye caused by a metal wire. He stated that during a school activity, he had to manipulate a 1.2-mm metal wire, which he was holding at the level of his eyes, when it suddenly stretched and pierced his right eye. His chief complaints were pain and decreased vision in the injured eye. His medical and ophthalmic histories were unremarkable. At the time of presentation, his visual acuity was hand motion in the right eye and 20/20 in the left eye. Slit-lamp examination of the patient's right eye revealed a 4-mm corneal laceration, positive Seidel test, athalamia, traumatic cataract, and anterior capsular rupture. The intraocular pressure in the injured eye was below normal, and therefore, fundus examination was not possible. Ultrasound was not performed because the trauma had resulted in an open-globe injury. The patient underwent an uneventful corneal suturing and extracapsular extraction of the damaged lens. Intraoperatively, posterior capsular rupture was observed and an anterior vitrectomy was subsequently performed.
Ultrasound examination performed 3 days after the surgery revealed a thickened posterior ocular wall, indicating that the wire could have penetrated the posterior segment. Moreover, linear, highly reflective echoes were present in the vitreous cavity (Fig. 1). Twenty-three days after the surgery, fundus examination of the right eye revealed the presence of several eyelashes embedded in the retina. The intraocular cilia were surrounded by a thickened posterior hyaloid membrane along the 4 o'clock meridian, approximately 3 disc diameters from the optic disc (Fig. 2), and his visual acuity then was counting fingers. Three days later (at postoperative day 26), a green laser was applied around IOFBs (Fig. 3) to prevent rhegmatogenous retinal detachment.
Fig. 1.
Ultrasound findings for a 41-year old man who presented with a penetrating ocular injury caused by a metal wire An ultrasound image acquired 3 days after injury shows highly reflective, linear echoes in the vitreous cavity, indicating the presence of cilia, and a thickened posterior wall. An eyelash (large arrow), its follicle (thin arrow), and its entrapment at the posterior perforation site (dotted line arrow) can be observed visible.
Fig. 2.
A retinography image obtained 23 days after a penetrating ocular injury caused by a metal wire in a 41-year old man. Cilia and their follicles are embedded in the retina.
Fig. 3.
A retinography image obtained 26 days after a penetrating ocular injury caused by a metal wire in a 41-year old man Cilia embedded in the retina can be observed after green laser photocoagulation was applied around them. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
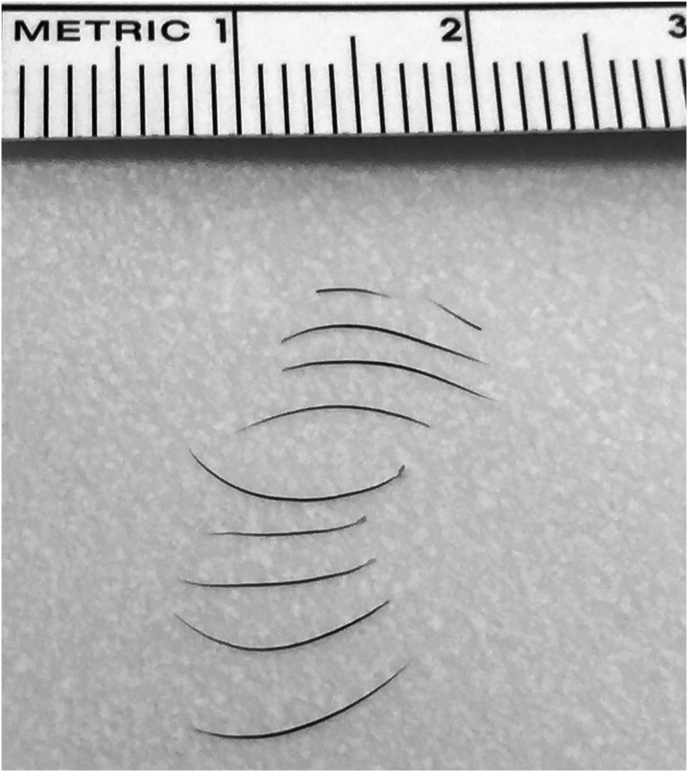
Six days later (at postoperative day 32), the patient returned to our ER with complaints of pain and hyperemia in the right eye. The patient's visual acuity at presentation was counting fingers. Ophthalmological examination showed 2+/4 + cells in the anterior chamber and presence of vitritis, despite treatment with prednisolone acetate eyedrops. Three days later (at postoperative day 35), an uncomplicated 3-port 23-gauge pars plana vitrectomy and IOFB removal were performed (Fig. 4) (See Video, Supplemental Digital Content 1 which demonstrates part of the surgery). Nine cilia were found embedded in the retina at the site of the suspected posterior perforation. After clearance of the vitreous, all cilia were removed by pars plana sclerotomy using IOFB forceps. Interestingly, most of the eyelashes included the follicle (Fig. 5).
Fig. 4.
An intraoperative photograph obtained during the surgical removal of intraocular cilia 35 days after a penetrating ocular injury caused by a metal wire in a 41-year old man.
Fig. 5.
Removal of nine cilia with follicles from the eye of a 41-year old man who incurred a penetrating ocular injury caused by a metal wire 35 days back. The image was obtained immediately after pars plana vitrectomy.
Follow-up examination after vitrectomy/IOFB removal surgery revealed no sign of inflammation. The patient's last follow-up visit was 6 months after the initial presentation during which fundus examination showed an attached retina and a clear vitreous cavity. However, the posterior perforation site was surrounded by laser marks and the posterior hyaloid membrane remained thickened (Fig. 6). The patient's best-corrected visual acuity (BCVA; with a contact lens) was 20/25.
Fig. 6.
A fundus photograph obtained 6 months after a penetrating ocular injury caused by a metal wire in a 41-year-old man. Pars plana vitrectomy and intraocular foreign body removal were performed 5 months back. The posterior perforation site is surrounded by laser marks. A thickened posterior hyaloid membrane can be seen.
3. Discussion
We report a case of a 41-year-old man with nine intraocular cilia embedded in his retina after a perforating ocular injury caused by a metal wire. The present case can be classified as type D ocular trauma as per the Ocular Trauma Classification Group guidelines which has the following categories 7: perforation, grade 4, pupil negative, and zone III. Twenty-three days after the trauma, ophthalmological examination revealed the presence of eyelashes embedded in the retina at the posterior perforation site. Cases of intraocular cilia are very rare, and their occurrence in the posterior segment, particularly in the retina, is even rarer. 4 Till date, only seven cases of retina-embedded eyelashes have been reported in the literature. 1, 8 Duke-Elder 9 offered an explanation for this rarity. Penetrating ocular injuries caused by fast-moving objects (e.g., metal chips) result in reflexive closure of the eyelids only after the foreign body has contacted the conjunctiva or cornea. Therefore, the eyelashes have not entered into the path of the foreign body. In contrast, eyelids reflexively close before a slow-moving object (e.g., a wire) comes in contact with the ocular surface, and this allows them to enter the path of the foreign body. The current case involved ophthalmic trauma caused by a metal wire, which often is the cause of injury in majority of patients with intraocular cilia. 1
The vast majority (91%) of the cases with intraocular cilia have exhibited the present of only one or two fragments of eyelash 1, although cases with five intraocular cilia in the posterior segment 1 and eight intraocular cilia in the anterior chamber 5 have also been reported. To our best knowledge, the present case exhibited the highest number of intraocular eyelashes documented till date.
The reaction of the eyes to intraocular eyelashes is unpredictable. 4 In some cases, the presence of IOFB is tolerated with little or no physiological reaction for up to 50 years. Some eyelashes are considered relatively inert because of their organic nature, but tolerance exhibited is higher when the case does not involve retention of the eyelash follicle. 6 The present case showed no immediate reaction to the intraocular presence of cilia. However, 32 days after the injury, the patient became symptomatic. The location and number of cilia and the retention of follicles likely contributed to the inflammatory reaction. Unfortunately, the presence of intraocular cilia are difficult to detect with ultrasound because of their small diameter. However, once the cilia is surrounded by a fibrous capsule, their size enlarges and they appear as objects with highly reflective echoes. 1 In the present case, ultrasound did not reveal the presence of any IOFBs, although it indicated its presence because of the presence of linear, highly reflective echoes.
4. Conclusion
In conclusion, we have described an unusual case of nine intraocular cilia embedded in the retina after a perforating ocular injury caused by a metal wire. The IOFBs caused an inflammatory reaction that was satisfactorily managed by vitrectomy and IOFB removal surgery. The patient's postoperative visual outcome was excellent, and his BCVA at last follow-up visit was 20/25. The findings from our case suggest that patients with penetrating ocular injuries, caused by slow-moving objects (e.g., wire), should be inspected for the presence of intraocular cilia.
Funding
No funding or grant support was provided to the present study.
Authorship
All authors attest that they meet current ICMJE criteria for Authorship.
Patient consent
The patient signed a written consent to publish his case details.
Declaration of competing interest
The authors have no conflicts of interest to declare.
Acknowledgments
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajoc.2020.100587.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Gopal L., Banker A.S., Sharma T. Intraocular cilia associated with perforating injury. Indian J Ophthalmol. 2000;48:33–36. [PubMed] [Google Scholar]
- 2.Oh K.T., Oh K.T., Singerman L.J. An eyelash in the vitreous cavity without apparent etiology. Ophthal Surg Lasers Imag Retin. 1996;27:243–245. [PubMed] [Google Scholar]
- 3.Dettoraki M., Andreanos K., Davou S. Intravitreal cilium associated with retinal detachment 40 years following penetrating eye injury: a case report. BMC Ophthalmol. 2015;15:25. doi: 10.1186/s12886-015-0010-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta V., Rao A., Sinha A. Post-traumatic inclusion cysts of the iris: a long term prospective case series. Acta Ophthalmol. 2007;85:893–896. doi: 10.1111/j.1600-0420.2007.00975.x. [DOI] [PubMed] [Google Scholar]
- 5.Metrikin D.C., Fante R.G., Hodes B.L., Tueson Intraocular cilia after penetrating eye injury. Arch Ophthalmol. 1992;110:921. doi: 10.1001/archopht.1992.01080190027011. [DOI] [PubMed] [Google Scholar]
- 6.Yalniz-Akkaya Z. Post-traumatic cilia remaining inert in the anterior chamber for 50 years: a case report. J Med Case Rep. 2011;5:527. doi: 10.1186/1752-1947-5-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pieramici D.J., Sternberg P., Jr., Aaberg T.M., Sr. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol. 1997;123:820–831. doi: 10.1016/s0002-9394(14)71132-8. [DOI] [PubMed] [Google Scholar]
- 8.Gupta A.K., Ghosh B., Mazumdar S., Gupta A. An unusual intraocular foreign body. Acta Ophthalmol. 1996;74:200–201. doi: 10.1111/j.1600-0420.1996.tb00072.x. [DOI] [PubMed] [Google Scholar]
- 9.Duke Elder S. CV Mosby Co.; St. Louis, MO: 1972. System of Ophthalmology; pp. 553–561. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.