Abstract
Introduction
Both-bone forearm fractures account for 3.4% of all pediatric fractures and 26% of all pediatric upper extremity fractures. Although non-operative management remains a feasible treatment option for children older than 10 years, they have a higher incidence for malunion due to their limited bone remodelling potential. Therefore, surgical intervention could be advocated for this age group, however the optimal method of surgical fixation in this age group remains controversial.
Authors wanted to evaluate hybrid fixation (plating of ulna & elastic nail for radius) of adolescent both-bone forearm fractures in a large single-institution cohort of patients.
Methods
A single-center, prospective cohort study was conducted at an academic Level 1 Trauma Center from February 2016 to February 2019.
A total of 60 patients (age 10–16 years) with both-bones forearm fracture were enrolled. Patients were assessed radiographically for union as well as clinically using the “Outcome Grading System” developed by Martus et al. for functional assessment of surgical management of pediatric forearm fractures using forearm rotation range of motion & complications rate.
Results
At final follow up for each patient (24 months) Union was achieved in all cases. Delayed union occurred in 4 patients (2 radii & 2 ulnae) with no case of combined radius & ulnar delayed union. At final follow up, the mean supination range was 81.27° ± 4.1°, while the mean pronation range was 68.17° ± 3.03°. The “Outcome Grading System” results were: 48 cases (80%) scored excellent, 10 cases (16.7%) scored good & 2 cases (3.3%) scored fair.
Conclusion
Hybrid fixation method in adolescent both-bones forearm fracture could be a viable option in managing these injuries & may reduce the problem of ulnar non-union encountered when using elastic stable intramedullary nail (ESIN) in that age group.
Level of evidence
Level II, Therapeutic study.
Keywords: Fracture, Fixation, Forearm, Pediatric
1. Introduction
1.1. Background
Both-bone forearm fractures account for 3.4% of all pediatric fractures and 26% of all pediatric upper extremity fractures.1,2 Most forearm fractures in children younger than 10 years can be treated successfully non-operatively, due to their remodelling potential.3,4 Although non-operative management remains a feasible treatment option for children older than 10 years, they have a higher incidence for malunion due to their limited bone remodelling potential.5 Therefore, surgical intervention could be advocated for this age group. Common indications for operative intervention include unacceptable reduction, loss of reduction, open fractures, polytrauma & compartment syndrome.6 Treatment should aim at maintaining length and rotational stability as well as restoring functional pronation & supination range of motion.
The optimal method of surgical fixation in this age group remains controversial.7,8 elastic stable intramedullary nail (ESIN) offers many benefits like small wounds, minimal soft tissue dissection, and spanning the whole length of the bone.9 However, some recent studies have reported high complication rates of ESIN fixation, including delayed union and non-union of the ulna. Moreover, several studies have shown that the complication rate of ESIN fixation is higher in children aged > 10 years than in younger children.10, 11, 12, 13
Hybrid fixation, utilizing an elastic stable intramedullary nail (ESIN) for fixing the radius combined with conventional plating for the ulna, offers an attractive alternative, which would help reduce non-union rate as well as providing forearm rotational control with ulnar plate fixation while reducing the need for soft tissue dissection for radius plating.
The aim of this study was to evaluate hybrid fixation of adolescent both-bone forearm fractures in a large single-institution cohort of patients. The primary outcome was to report the union time & rate for the ulna using this technique. The secondary outcomes were to report, operative time, forearm supination-pronation range of motion & complications.
Since the aim of this study was to establish that hybrid fixation would be associated with less non-union of the ulna compared to ESIN, thus the null hypothesis was that hybrid fixation has the same rate for ulna non-union compared to ESIN.
2. Methods
2.1. Study design
An Institutional Review Board (IRB) approved, single-center, prospective follow-up study including all patients treated with hybrid fixation of both-bones forearm fracture who were eligible for enrollment.
2.2. Setting
An academic Level 1 Trauma Center. The study was conducted from February 2016 to February 2019 (patient enrollment continued for 1 year, then study was terminated when a minim of 2 years follow-up was achieved for all patients).
2.3. Participants
Patients 10–16 years of age who presented to our service and suffered simple, closed, diaphyseal both-bones forearm fracture (Type 22-A3 fractures according to AO/Müller Classification)15] & who were indicated for surgical management were eligible for enrollment in the study, while those with open or pathologic or Monteggia or Galeazzi or bilateral fractures or those with compartment syndrome were excluded. Those with fractures older than 14 days were also excluded. Indications for surgery were polytrauma, unacceptable reduction & loss of reduction, our institution uses the parameters of acceptable reduction that are widely accepted in the existing literature16,17]. The decision of operative management was taken by the senior investigator (SG).
Data on age, gender, fracture level, fracture pattern, operative time and complications (e.g. loss of reduction, malunion, infection) were registered
2.4. Intervention
The radius was fixed using one ESIN (with a nail diameter of 40% of the medullary canal diameter) inserted through a styloid process entry point. Closed reduction was achieved under C-arm guidance for all radius fractures. The ulna was fixed using a 3.5 mm dynamic compression plate (DCP) with 3 screws on each side of the fracture. All surgeries were performed by the same surgeon (AH). Surgeries were performed under general anesthesia in the supine position with hand to be operated over side arm support, a tourniquet was used. Postoperatively patients were put in a splint for comfort. No formal physical therapy was recommended post-operatively.
All patients were systematically examined at the outpatient clinic after 2, 6 weeks, 3, 6 months and 2 years. Clinical data (forearm supination-pronation range) were obtained during follow up visits. Radiographic data (antero-posterior & lateral radiographs of the forearm to assess bony union) were obtained until either union was achieved or a diagnosis of non-union was established.
Delayed union was defined as incomplete consolidation at 90 days as described by Schmittenbecher et al.18 Incomplete healing by 6 months was considered a nonunion.19
The outcomes were assessed by 2 of the authors (AA & AA) blinded to each other's assessment, if not in agreement a 3rd assessment was done by the senior investigator (SG).
The “Outcome Grading System” (Table 1) developed by Martus et al.14 was used for functional assessment. This outcome grading system for surgical management of pediatric forearm fractures incorporates a modification of the validated Clavien-Dindo classification of surgical complications (Table 2) and the minimum forearm rotation required for activities of daily living (ADL) in normal subjects.20,21 Normal range of forearm rotation was considered to be 70° of pronation and 85° of supination.22 An outcome was judged excellent if the range of motion was full and no complications greater than grade 1 occurred. A good outcome was reported upon mild loss of motion (<10°) with complications up to grade 2. A fair outcome was reported if loss of motion was more significant (10°–30°) and complications were grade 3 or less in severity. A poor outcome was reported if there was a significant loss of motion (>30°) and/or there were complications of grade 4 or 5 in severity.
Table 1.
Outcome grading system.
| Outcome Grade | Range of Motion | Complication Grade |
|---|---|---|
| Excellent | Full | Grade 1 or none |
| Good | Loss of <10° pronation and/or supination | Grade 2 or less |
| Fair | Loss of 10–30° pronation and/or supination | Grade 3 or less |
| Poor | Loss of >30° pronation and/or supination | Up to grade 5 |
Table 2.
Modification of the clavien-dindo classification of surgical complications.
| Complication Grade | Definition | Examples |
|---|---|---|
| 1 | Deviation from a routine postoperative course without the need for intervention. |
|
| 2 | Resolution after outpatient management, pharmacologic therapy, or close observation |
|
| 3 | Requiring inpatient management or reoperation |
|
| 4 | Complication that is limb threatening, life threatening, or resulting in a permanent deficit |
|
| 5 | Death of patient |
|
2.5. Statistics
The statistical analysis was performed using the statistical package SPSS (Statistical Package for the Social Sciences) version 25.
Mean and standard deviation (SD) were used to express continuous data while frequency (count) and relative frequency (percentage) was used to express categorical data.
Continuous variables were age, operative time, length of follow-up period, bone union time and range of motion. Categorical variables were sex, side of injury, fracture pattern, fracture level, functional outcome and complication.
The statistical difference was calculated using the Student's t–test for continuous variables which followed a normal distribution and Mann-Whitney U–test for those not following a normal distribution. For comparing categorical data, the Chi-squared (χ2) test was performed.
4. Results
A total of 127 patients were assessed for eligibility, 52 patients were excluded as they didn't meet the inclusion criteria, 15 patients refused to participate in the study, so a final number of 60 patients were enrolled. No patients were lost to follow up at time of final data analysis.
The study included 54 males (90%) and 6 females (10%), the mean age at time of enrolment was 11.83 ± 1.72 years. The mode of injury was falling to the ground (FTG) in 54 patients, road traffic accident (RTA) in 4 patients and direct trauma in 2 patients. The Right side was affected in 44 patients (73.3%) and the left side was affected in 16 patients (26.7%), 56 patients were right-handed, and 4 patients were left handed.
The fracture level was mid-shaft in 48 patients, proximal-shaft in 8 patients & distal-shaft in 4 patients. Fracture pattern was transverse in 38 & short oblique in 22 patients. The mean operative time was 48.5 ± 10.8 min.
Union was achieved in all cases. The mean time to union was 6.7 ± 1.5 weeks. Delayed union occurred in 4 patients (2 radii & 2 ulnae) with no case of combined radius & ulnar delayed union. The 2 radii finally united at 14 weeks while the 2 ulnae finally united at 15 weeks. No surgical intervention was needed to achieved union in these cases.
At final follow up, the mean supination range was 81.27° ± 4.1°, while the mean pronation range was 68.17° ± 3.03°. The “Outcome Grading System” results were: 48 cases (80.0%) scored excellent, 10 cases (16.7%) scored good & 2 cases (3.3%) scored fair (one had limited pronation range and the other had deep wound infection that required debridement & implant removal).
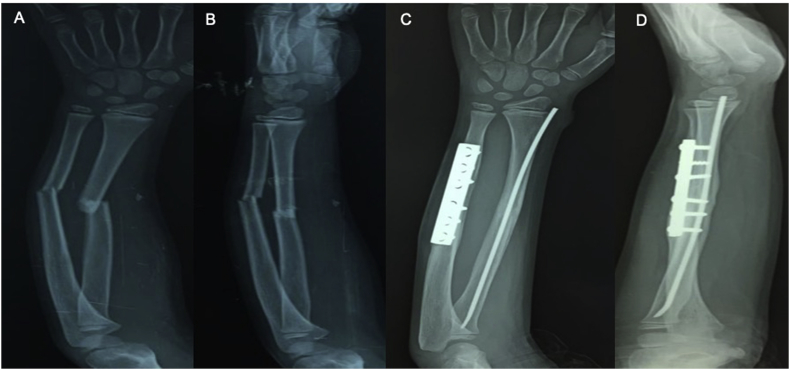
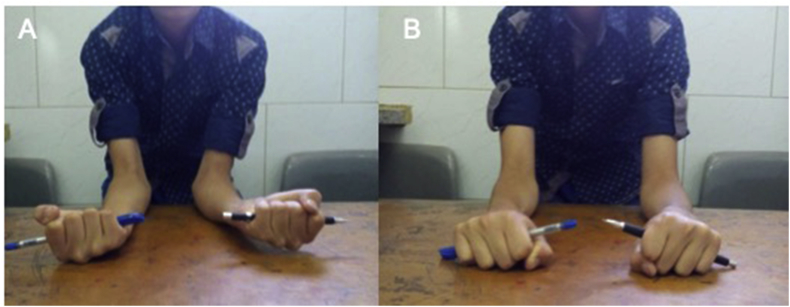
Fig. 1 shows radiograph of one case & Fig. 2 shows a clinical picture for the same patient.
Fig. 1.
Radiograph representing one case A: pre-operative AP, B: pre-operative lateral, C: Final (3 months) AP, D: final (3 months) lateral view.
Fig. 2.
Clinical Picture showing forearm supination-pronation forearm range in patient whose radiographs are shown in Fig. 1. A: maximum supination, B: maximum pronation.
5. Discussion
Surgical management for adolescent both-bones forearm fracture is becoming more popular, however the optimal method of surgical fixation in this age group remains controversial.7,8
Given the relative success of closed reduction and casting in children, it is critical that operative techniques demonstrate low complication rates.23
Several advantages of ESIN have been reported in the literature, including decreased operative time, minimal soft tissue dissection, improved cosmesis, ease of implant removal, and early return to activity after implant removal.12,24
Delayed union and nonunion of the ulna after ESIN fixation of pediatric forearm fractures has been recently reported to be common.8,10, 11, 12,18,25 Ogonda et al.10 attributed that to fracture distraction by the curved nail tip as its introduced in an antegrade fashion from the olecranon. He also attributed the lower incidence of delayed or no-union of the radius to the upward directed force when the nail is inserted in a retrograde fashion.
Salvi26 described that the ulna plays a greater role in maintaining the stability of the forearm than the radius, especially during buckling and torsional stress. Therefore, restoring the original function of the ulna is necessary to rebuild forearm stability, and ulnar plate fixation theoretically provides better stability than ESIN fixation.
Advocates of both-bones forearm fractures plating suggest that it allows for anatomic restoration of the radial bow. Several studies in the adult population showed that a change in either the magnitude or location of radial bow has been associated with the decrease of forearm rotation range.27,28 Although the use of plate fixation has been shown to lower the risk of forearm loss of rotation rang, it has not eliminated that risk, as factors other than the method of fracture fixation come to play in determining the forearm rotation range. Schemitsch et al. showed in their cadaveric study that re-establishing the magnitude and location of radial bow is more difficult to achieve with ESIN.28 Although nail contouring helps re-establish the radial bow, in our experience, planned nail contouring is frequently compromised during nail insertion. In the study conducted by Shah et al.23 they showed that the magnitude of radial bow was nearly completely restored with use of ESIN, but the location of the maximal radial bow was translated distally, despite that they found no difference between plating and ESIN groups in regaining forearm rotation at their final follow up. Many comparison studies in children report no difference in functional outcome between ESIN and plating.12,24,29, 30, 31
Colaris et al. in their study32 cautions against single-bone fixation in both-bones forearm fractures in children.
In light of the previously mentioned literature, the authors wanted to evaluate the hybrid fixation technique in adolescent both-bones forearm fractures, which would provide maximal ulnar stability (thought to yield a better supination-pronation range outcome & a lower non-union rate) as well as fixing the radius with a minimally invasive technique thus achieving dual bone fixation while minimizing the need for extensive soft tissue dissection & improving cosmesis.
In this study, the authors observed high union rate of the ulna compared to rates reported in the literature when using ESIN as well as achieving favorable functional outcome.
To the best of the authors knowledge this is the first prospective pilot study to present results for hybrid fixation of adolescent both-bones forearm fractures, paving the way to further studies that would include more patients and perhaps parallel groups study design. The authors think that among the strengths of this study is the fact that all surgeries were performed by one surgeon to help eliminate surgeon's training & skills as a confounding factor.
The authors think the limitations to this study is that in order to generalize their results, further research would be needed that involve multiple centers with multiple surgeons performing this technique.
In conclusion, the authors believe that hybrid fixation method in adolescent both-bones forearm fracture could be a viable option in managing these injuries & may reduce the problem of ulnar non-union encountered when using ESIN in that age group.
Disclosure
No form of financial support was received during this study. None of the authors is associated with any commercial entities at time of manuscript submission.
Compliance with ethical standards
Funding
No funding was received for this study.
Conflict of interest
Authors declare that they have no conflict of interest
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from parents or legal guardians of children who participated in the study.
Contributor Information
Ahmed S. Elhalawany, Email: ahmedsamir.ash198@gmail.com.
Ahmed Afifi, Email: ahmedafifi@kasralainy.edu.eg.
Ashraf Anbar, Email: ashraf.anbar@gmail.com.
Sherif Galal, Email: Sherif.Galal@kasralainy.edu.eg.
References
- 1.Landin L.A. Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950–1979. Acta Orthop Scand Suppl. 1983;202:1–109. [PubMed] [Google Scholar]
- 2.Mann D.C., Rajmaira S. Distribution of physeal and nonphyseal fractures in 2,650 longebone fractures in children aged 0–16 years. J Pediatr Orthop. 1990;10(6):713–716. doi: 10.1097/01241398-199011000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Larsen E., Vittas D., Torp-Pedersen S. Remodeling of angulated distal forearm fractures in children. Clin Orthop Relat Res. 1988;237:190–195. [PubMed] [Google Scholar]
- 4.Vittas D., Larsen E., Torp-Pedersen S. Angular remodeling of midshaft forearm fractures in children. Clin Orthop Relat Res. 1991;265:261–264. [PubMed] [Google Scholar]
- 5.Kay S., Smith C., Oppenheim W.L. Both–bone midshaft forearm fractures in children. J Pediatr Orthop. 1986;6:306–310. doi: 10.1097/01241398-198605000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Sun Y.Q., Penna J., Haralabatos S.S. Intramedullary fixation of pediatric forearm diaphyseal fractures. Am J Orthoped. 2001;30:67–70. [PubMed] [Google Scholar]
- 7.Jubel A., Andermahr J., Isenberg J., Issavand A., Prokop A., Rehm K.E. Outcomes and complications of elastic stable intramedullary nailing for forearm fractures in children. J Pediatr Orthop B. 2005;14:375–380. doi: 10.1097/01202412-200509000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Ho C.A., Jarvis D.L., Phelps J.R., Wilson P.L. Delayed union in internal fixation of pediatric both-bone forearm fractures. J Pediatr Orthop B. 2013;22:383–387. doi: 10.1097/BPB.0b013e328361c7ea. [DOI] [PubMed] [Google Scholar]
- 9.Du S.H., Feng Y.Z., Huang Y.X. Comparison of pediatric forearm fracture fixation between single- and double-elastic stable intramedullary nailing. Am J Therapeut. 2014;23(3):e730–e736. doi: 10.1097/MJT.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 10.Ogonda L., Wong-Chung J., Wray R., Canavan B. Delayed union and non-union of the ulna following intramedullary nailing in children. J Pediatr Orthop B. 2004;13(5):330–333. doi: 10.1097/01202412-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Adamczyk M.J., Riley P.M. Delayed union and nonunion following closed treatment of diaphyseal pediatric forearm fractures. J Pediatr Orthop. 2005;25(1):51–55. doi: 10.1097/00004694-200501000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Fernandez F.F., Eberhardt O., Langendorfer M., Wirth T. Nonunion of forearm shaft fractures in children after intramedullary nailing. J Pediatr Orthop B. 2009;18(6):289–295. doi: 10.1097/BPB.0b013e32832f5b20. [DOI] [PubMed] [Google Scholar]
- 13.Flynn J.M., Jones K.J., Garner M.R., Goebel J. Eleven years' experience in the operative management of pediatric forearm fractures. J Pediatr Orthop. 2010;30(4):313–319. doi: 10.1097/BPO.0b013e3181d98f2c. [DOI] [PubMed] [Google Scholar]
- 14.Martus J.E., Preston R.K., Schoenecker J.G., Lovejoy S.A., Green N.E., Mencio G.A. Complications and outcomes of diaphyseal forearm fracture intramedullary nailing. J Pediatr Orthop. 2013;33(6):598–607. doi: 10.1097/BPO.0b013e3182a11d3b. [DOI] [PubMed] [Google Scholar]
- 15.Müller M.E., Nazarian S., Koch P. Springer-Verlag; Berlin Heidelberg New York: 1987. Classification AO des fractures: les os longs. [Google Scholar]
- 16.Flynn J., Sarwark J.F., Waters P.M. The surgical management of pediatric fractures of the upper extremity. Instr Course Lect. 2003;52:635–645. [PubMed] [Google Scholar]
- 17.Noonan K.J., Price C.T. Forearm and distal radius fractures in children. J Am Acad Orthop Surg. 1998;6:146–156. doi: 10.5435/00124635-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Schmittenbecher P., Fitze G., GoÅN deke J. Delayed healing of forearm shaft fractures in children after intramedullary nailing. J Pediatr Orthop. 2008;28:303–306. doi: 10.1097/BPO.0b013e3181684cd6. [DOI] [PubMed] [Google Scholar]
- 19.Martus J.E., Preston R.K., Schoenecker J.G., Lovejoy S.A., Green N.E., Mencio G.A. Complications and outcomes of diaphyseal forearm fracture intramedullary nailing: a comparison of pediatric and adolescent age groups. J Pediatr Orthop. 2013;33(6):598–607. doi: 10.1097/BPO.0b013e3182a11d3b. [DOI] [PubMed] [Google Scholar]
- 20.Clavien P.A., Barkun J., de Oliveira M.L. The clavien-dindo classification of surgical complications. Ann Surg. 2009;250(2):187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 21.Dindo D., Demartines N., Clavien P.-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Youm Y., Dryer R.F., Thambyrajah K. Biomechanical analyses of forearm pronation-supination and elbow flexion-extension. J Biomech. 1979;12:245–255. doi: 10.1016/0021-9290(79)90067-8. [DOI] [PubMed] [Google Scholar]
- 23.Shah A.S., Lesniak B.P., Wolter T.D., Caird M.S., Farley F.A., Vander Have K.L. Stabilization of adolescent both-bone forearm fractures: a comparison of intramedullary nailing versus open reduction and internal fixation. J Orthop Trauma. 2010;24(7):440–447. doi: 10.1097/BOT.0b013e3181ca343b. [DOI] [PubMed] [Google Scholar]
- 24.Van der Reis W.L., Otsuka N.Y., Moroz P. Intramedullary nailing versus plate fixation for unstable forearm fractures in children. J Pediatr Orthop. 1998;18:9–13. [PubMed] [Google Scholar]
- 25.Ballal M.S., Garg N.K., Bruce C.E., Bass A. Nonunion of the ulna after elastic stable intramedullary nailing for unstable forearm fractures: a case series. J Pediatr Orthop B. 2009;18(5):261–264. doi: 10.1097/BPB.0b013e32832f0648. [DOI] [PubMed] [Google Scholar]
- 26.Salvi A.E. Forearm diaphyseal fracture: which bone to synthesize first? Orthopedics. 2006;29(8):669–671. doi: 10.3928/01477447-20060801-19. [DOI] [PubMed] [Google Scholar]
- 27.Schemitsch E.H., Richards R.R. The effect of malunion on functional outcome after plate fixation of fractures of both bones of the forearm in adults. J Bone Joint Surg Am. 1992;74:1068–1078. [PubMed] [Google Scholar]
- 28.Schemitsch E.H., Jones D., Henley M.B. A comparison of malreduction after plate and intramedullary nail fixation of forearm fractures. J Orthop Trauma. 1995;9:8–16. doi: 10.1097/00005131-199502000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Smith V.A., Goodman H.J., Strongwater A. Treatment of pediatric both-bone forearm fractures: a comparison of operative techniques. J Pediatr Orthop. 2005;25:309–313. doi: 10.1097/01.bpo.0000153943.45396.22. [DOI] [PubMed] [Google Scholar]
- 30.Carmichael K.D., English C. Outcomes assessment of pediatric bot bone forearm fractures treated operatively. Orthopedics. 2007;30:379–383. doi: 10.3928/01477447-20070501-08. [DOI] [PubMed] [Google Scholar]
- 31.Reinhardt K.R., Feldman D.S., Green D.W. Comparison of intramedullary nailing to plating for both–bone forearm fractures in older children. J Pediatr Orthop. 2008;28:403–409. doi: 10.1097/BPO.0b013e31816d71f2. [DOI] [PubMed] [Google Scholar]
- 32.Colaris J., Rdijman M., Allema J.H. Single-bone intramedullary fixation of unstable both-bone diaphyseal forearm fractures in children leads to increased re-displacement: a multicenter randomized controlled trial. Arch Orthop Trauma Surg. 2013;133:1079–1087. doi: 10.1007/s00402-013-1763-0. [DOI] [PubMed] [Google Scholar]