Abstract
Introduction:
Rising costs of post-acute care facilities for both the patient and payers make discharge home after hospital stay, with or without home help, a favorable alternative for all parties. Our objectives were to assess the effect of marital status, a large source of social support for many, on disposition following hospital stay.
Methods:
Patients were prospectively entered into an institutional review board-approved, trauma database at a large, academic medical center. Patients aged 55 years or older with any fracture injury between 2014 and 2017 were included. Retrospectively, their relationship status was recorded through review of patient records. A status of “married” was separated from those with a status self-reported as “single,” “divorced,” or “widowed.” Multinomial logistic regression was used to assess whether discharge location differs by marital status while controlling for demographics and injury characteristics.
Results:
Of 1931 patients, 8.3% were divorced, 29.9% were single, 20.0% were widowed, and 41.8% were married. There was a significant correlation between discharge disposition and marital status. Single patients had 1.71 times, and widowed patients had 1.80 times, the odds of being discharged to a nursing home, long-term care facility, or skilled nursing facility compared to married patients after controlling for age, gender, Score for Trauma Triage in the Geriatric and Middle-Aged score, and insurance type. Additionally, single and widowed patients experienced 1.36 and 1.30 times longer length of hospital stay than their married counterparts, respectively.
Discussion:
Patients who are identified as “single” or “widowed” should have early social work intervention to establish clear discharge expectations. Early intervention in this way would allow time for contact with close, living relatives or friends who may be able to provide sufficient support so that patients can return home. Increasing home discharge rates for these patients would reduce lengths of hospital stay and reduce post-acute care costs for both patient and payers without materially altering unplanned readmission rates.
Keywords: discharge, geriatric trauma, length of stay, marriage status, trauma surgery
Introduction
Rising costs of post-acute care facilities for both the patient and payers make discharge home after hospital stay a favorable alternative for all parties.1 A 2017 report from Genworth Financial indicated that the annual cost to consumers for a private room in a nursing home was an estimated US$97 455, a 50% increase since 2004, while 44 hours per week of home health aide services averaged about half of that total, at US$49 192.1 As the over-65 population in the United States continues to balloon, estimated to nearly double from its current 48 million to over 88 million by 2050, the cost of post-acute and long-term care for these patients will climb steeply.2 With consideration for both rising cost of post-acute and long-term care, as well as the increasing need and demand for these facilities, the way in which physicians and hospital systems prepare for and handle patient disposition must be reexamined. While a variety of factors play into the selection of an appropriate discharge location, there is currently no standardization across hospital systems that determine discharge location nor any clear guide as to which patient demographic factors tend to prompt higher levels of care.3
While there has been some study of physical limitations that encourage selection of disposition to a facility with a higher level of care, there has been little study of the social factors that impact the choice.3,4 The purpose of this study was to elucidate to what extent in-home social support, in the form of a spouse, would directly play on discharge location choice, as well as other less obvious components of a patient’s hospital course including length of hospital stay, unplanned readmission, and in-hospital cost for middle-aged and geriatric trauma patients, while controlling for confounding factors.
Methods
Data Source
Patients were prospectively entered into an institutional review board-approved, middle-aged, and geriatric trauma database at a large, academic medical center. Over a 3-year period from September 2014 to October 2017, a total of 3842 trauma activation patients were collected. Retrospectively, their relationship status was recorded and added to the database through review of patient demographic records.
Patient Selection
The following criteria were required for inclusion in the study: age older than 55 years, diagnosis of at least 1 traumatic orthopedic fracture, available in-hospital cost data, a recorded marital status of “married,” “single,” “divorced,” “legally separated” (later coded as “divorced”), or “widowed”, and a recorded discharge location. Additionally, patients were excluded from the study if their recorded marital status was listed as “other” or “unknown” or if their discharge location was “hospice care,” “death,” “transfer to other hospital,” “transfer to psychiatric facility,” or “transfer to substance abuse treatment facility.” Of the 3842 trauma activation patients collected, only 1931 were left after consideration of inclusion and exclusion criteria.
Outcome Measures
The outcome measures in this study were discharge location, length of hospital stay, unplanned readmission, readmission within 90 days, and total in-hospital cost. Discharge location was split into 4 separate categories: home (home/left the hospital against medical advice), home with health-care services, rehabilitation facility (subacute rehabilitation, acute rehabilitation), and skilled nursing facility (nursing home, skilled nursing facility, long-term care, or transitional nursing care).
Independent Variables
The primary independent variable was patient marital status. Each discharge record included in our analysis contained self-reported marital status and was stratified into one of 4 groups: married, single, divorced, or widowed. To account for confounding variables, relevant patient demographics (age, sex, and primary payer) and medical characteristics (Score for Trauma Triage in the Geriatric and Middle-Aged [STTGMA] and injury category) were also included.
The STTGMA score is a validated inpatient mortality risk stratification tool designed to efficiently triage middle-aged and geriatric patients presenting to the emergency department (ED) with trauma-related injuries.5 At our academic medical center, patients aged 55 years or older with fracture injuries generating an orthopedic consult for nonpenetrating trauma are assigned an STTGMA score upon initial ED evaluation. The STTGMA scores take into account the following variables: patient age, Charlson comorbidity index, Glasgow Coma Scale on the initial evaluation, mechanism of injury, and Abbreviated Injury Severity subscores for the head and neck, chest, and extremities and pelvis. Mechanisms of injury are categorized as low- and high-energy mechanisms. Low-energy mechanisms of injury include all falls from standing height or ≤2 stairs, while high-energy mechanisms of injury include all falls from >2 stairs, motor vehicle or motorcycle accidents, and pedestrians struck by vehicles. The STTGMA scores are calculated on a scale of 0% to 100%, with higher scores denoting greater risk of inpatient mortality.6 Orthopedic surgical residents are formally educated on how to compute the STTGMA score using an online education module and an Internet-based STTGMA score calculator (https://sttgma.wordpress.com/about/). In addition, the STTMGA tool has been proven to risk stratify functional outcomes in middle-aged and geriatric patients up to 1 year following their hospitalization, making it an important reference source for evaluating expected long-term recovery.7
Statistical Analyses
Analyses were performed using SPSS version 25 (IBM Corporation, Armonk, New York) and GraphPad Prism version 8 (GraphPad Software, La Jolla, California). Total in-hospital cost displayed a bimodal distribution and was classified as a categorical variable consisting of 3 groups (US$0- US$1999, US$2000- US$9999, and US$10 000+) based on optimal cut points. Length of stay was analyzed as a count variable and was not log-transformed. Descriptive statistics were generated and stratified by demographic and medical characteristics. Bivariate analyses between patient characteristics, hospital outcomes, and marital status utilized χ2 and analysis of variance tests. To account for potential confounding variables, multiple logistic regression was utilized to model binary outcomes (unplanned readmission and readmission within 90 days). Multivariable analysis for the length of stay utilized negative binomial regression and multivariable analysis for other categorical variables (discharge location and total in-hospital cost) utilized multinomial logistic regression. Output ratios represent odds ratios (ORs) for categorical variables (discharge location, unplanned readmission, readmission within 90 days, complications, and total cost) and risk ratios (RRs) for length of stay. Collinearity was assessed using variable tolerance and no concerning values were noted. Statistical significance was defined as P < .05.
Results
Descriptive Statistics
In total, 1931 middle-aged and geriatric trauma patients were analyzed. Overall, 41.79% (n = 807) of patients were married, 29.88% (n = 577) were single, 8.29% (n = 160) were divorced, and 20.04% (n = 387) were widowed. Females were prominently represented (66.5%, n = 1284), as were patients aged 65 to 79 years (37.0%, n = 715). The majority of patients either had Medicare/Medicaid or Medicare/Medicaid with supplement for their primary payer (35.5%, n = 685; 33.6%, n = 649, respectively). The vast majority of fractures involved the extremities (82.1%, n = 1586), followed by fractures of the torso (sternum/ribs) or pelvis (8.5%, n = 164; Table 1).
Table 1.
Patient Characteristics (Demographic and Medical).a
| Variables | n | % |
|---|---|---|
| Overall | 1931 | – |
| Marital status | ||
| Married | 807 | 41.8 |
| Single | 577 | 29.9 |
| Divorced | 160 | 8.3 |
| Widowed | 387 | 20.0 |
| Sex | ||
| Male | 647 | 33.5 |
| Female | 1284 | 66.5 |
| Age (years) | ||
| 55-64 | 570 | 29.5 |
| 65-79 | 715 | 37.0 |
| 80+ | 646 | 33.5 |
| Primary payer | ||
| Medicare/Medicaid/NYSHIP | 685 | 35.5 |
| Medicare/Medicaid with supplement | 649 | 33.6 |
| Private | 337 | 17.5 |
| Self-pay/no insurance | 81 | 4.2 |
| Workers’ compensation | 178 | 9.2 |
| STTGMA score (%) | ||
| 0-0.5 | 512 | 26.5 |
| 0.51-0.9 | 447 | 23.2 |
| 0.91-1.7 | 493 | 25.5 |
| 1.71+ | 478 | 24.8 |
| Fracture category | ||
| Head | 57 | 3.0 |
| Spine | 58 | 3.0 |
| Torso/pelvis | 164 | 8.5 |
| Extremities | 1586 | 82.1 |
| Polytrauma | 66 | 3.4 |
Abbreviation: STTGMA, Score for Trauma Triage in the Geriatric and Middle-Aged; NYSHIP, New York State Health Insurance Program.
Bivariate Analyses
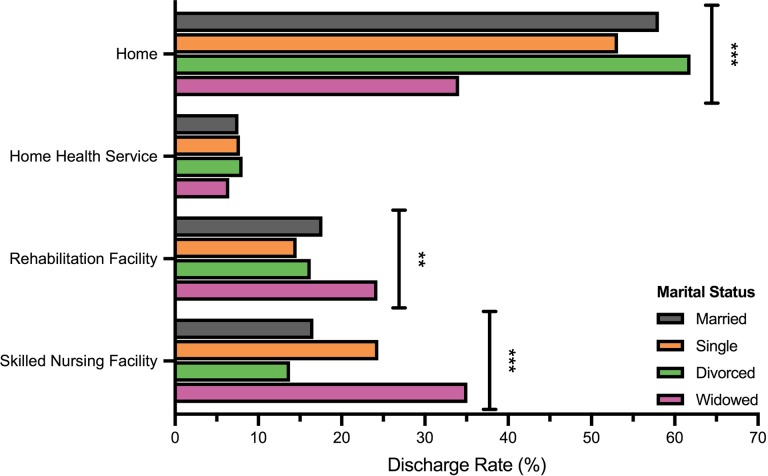
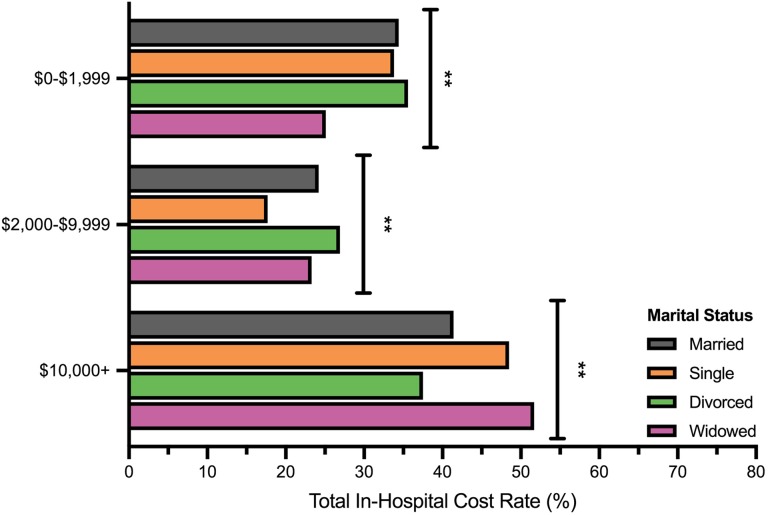
Using unadjusted bivariate analyses, patients stratified by marital status displayed significant differences in discharge disposition, length of hospital stay, unplanned readmission, and total in-hospital cost (Table 2). Divergence in the distributions of discharge location and total in-hospital cost was further assessed between groups. Analyses revealed significant differences in home, rehabilitation facility, and skilled nursing facility discharge, as well as low and high total in-hospital cost (Table 2, Figures 1 and 2).
Table 2.
Bivariate Analyses of Marital Status and Hospital Outcomes.
| Variables | Married (n = 807) | Single (n = 577) | Divorced (n = 160) | Widowed (n = 387) | P Value |
|---|---|---|---|---|---|
| Discharge location | <.001 | ||||
| Home | 469 (58.1) | 307 (53.2) | 99 (61.9) | 132 (34.1) | <.001 |
| Home health services | 61 (7.6) | 45 (7.8) | 13 (8.1) | 25 (6.5) | .856 |
| Rehabilitation facility | 143 (17.7) | 84 (14.6) | 26 (16.3) | 94 (24.3) | .002 |
| Skilled nursing facility | 134 (16.6) | 141 (24.4) | 22 (13.8) | 136 (35.1) | <.001 |
| Length of stay (days) | 4.3 (5.4)b | 5.5 (7.5)b | 4.3 (6.1)b | 5.6 (6.0)b | <.001 |
| Unplanned readmission | 60 (7.4) | 46 (8.0) | 19 (11.9) | 37 (9.6) | .224 |
| 90-Day readmission | 94 (11.7) | 74 (12.8) | 23 (14.4) | 47 (12.1) | .756 |
| Total in-hospital cost (US$) | <.001 | ||||
| 0-1999 | 278 (34.4) | 195 (33.8) | 57 (35.6) | 97 (25.1) | .006 |
| 2000-9999 | 195 (24.2) | 102 (17.7) | 43 (26.9) | 90 (23.3) | .012 |
| 10 000 | 334 (41.4) | 280 (48.5) | 60 (37.5) | 200 (51.7) | .001 |
a Numbers in parentheses represent percentage value within category.
b Values represent standard deviation.
Figure 1.
Discharge frequency by marital status. *P < .05, **P < .01, ***P < .001.
Figure 2.
Cumulative in-patient cost by marital status. *P < .05, **P < .01, ***P < .001.
Multivariate Analyses
After adjustment for available demographic and medical characteristics, patients with a status of “single” (never been married) had significantly greater odds of being discharged to a skilled nursing facility versus home (OR: 1.71, confidence interval [CI]: 1.25-2.34, P = .001) and risk of prolonged length of hospital stay (RR: 1.36, CI: 1.20-1.54, P < .001) compared to married patients. In addition, a status of “widowed” was significantly associated with greater odds of skilled nursing facility versus home discharge (1.80, CI: 1.25-2.58, P = .001) and risk of longer length of stay (RR: 1.30, CI: 1.12-1.52, P = .001; Table 3). Other outcomes were statistically similar between groups.
Table 3.
Multivariate Analyses of Hospital Outcomes Predicted by Marital Status (Ref = Married).
| Variables | Single | Divorced | Widowed |
|---|---|---|---|
| Ratio (95% CI) | Ratio (95% CI) | Ratio (95% CI) | |
| Discharge location (Ref = Home) | |||
| Home health services | 1.00 (0.65-1.53) | 0.85 (0.44-1.64) | 1.02 (0.59-1.76) |
| Rehabilitation facility | 0.88 (0.63-1.23) | 0.68 (0.41-1.14) | 1.18 (0.81-1.72) |
| Skilled nursing facility | 1.71 (1.25-2.34)a | 0.69 (0.40-1.18) | 1.80 (1.25-2.58)a |
| Length of stay | 1.36 (1.20-1.54)b | 1.06 (0.87-1.30) | 1.30 (1.12-1.52)a |
| Unplanned readmission | 1.10 (0.73-1.66) | 1.64 (0.93-2.88) | 1.03 (0.64-1.65) |
| 90-Day readmission | 1.10 (0.79-1.53) | 1.19 (0.72-1.96) | 0.92 (0.61-1.38) |
| Total in-hospital cost ($) (Ref = 0-1999) | |||
| 2000-9999 | 0.74 (0.54-1.03) | 1.10 (0.69-1.77) | 0.97 (0.66-1.45) |
| 10 000 | 1.25 (0.96-1.63) | 0.90 (0.59-1.38) | 1.28 (0.92-1.79) |
Abbreviation: CI, confidence interval.
Ratio column represents odds ratios for binary (unplanned and 90-day readmission) and categorical variables (discharge location and total cost), while indicating relative risk in arithmetic means for length of stay.
a P < .01.
b P < .001.
Discussion
This study examined the role a spouse plays in the hospital course and eventual discharge decision made for middle-aged and elderly orthopedic trauma patients. We utilized the spouse as a surrogate for home social support network. Controlling for confounders, we found that unmarried (never been and widowed) patients are more likely to be discharged to a nursing home, long-term care facility, or skilled nursing facility than married patients. Married patients also had significantly shorter hospital stays than their unmarried counterparts. Readmissions, both unplanned and planned, within 30 and 90 days, as well as in-hospital cost were not shown to be significantly different across marital status type. However, in-hospital cost does not take into account the post-hospital costs associated with post-acute and long-term care, which increase sharply as the level of care increases. This reduction in post-hospital care costs, along with a reduction in length of hospital stay, reflects reduced cost to married patients overall. Interestingly, divorced patients did not show significantly longer lengths of hospital stay, nor did they have a higher likelihood of being discharged to a skilled nursing facility. This may be due to the relatively smaller size of this group compared to the others, which may not have permitted statistical significance. It is also possible that this group may be more likely than the “single” and “widowed” groups to have nonspousal partners that may, in part or whole, fill the role of in-home caregiver.
While no other study to our knowledge has attempted to identify social demographic factors that may impact patients’ discharge location and hospital length of stay, general outcomes of the hospitalization of elderly patients were studied by several groups in the mid-1980s as the US population began to age in an accelerated manner. A study by Lamont et al in 1983 found that important predictors of decline in function post-hospital stay included patient’s age greater than 85 years as well as abnormal mental status.8 Our data support the finding that older age was a predictor of the need for higher level of care, and thus, we accordingly controlled for this in our analysis. In a 1988 study by Narain et al that included all geriatric hospitalized patients, not just orthopedic patients, researchers found that factors that predicted nursing home admission were functional status, living location, and decreased mental status.9 Living location likely relates to marital status in that patients with decreased function are able to continue living at home provided that they have support within the home. While the above studies focused on important demographic factors that can help alert those caring for a patient that they may require higher levels of care at the time of discharge, these studies focused on nonmodifiable factors that cannot be altered to promote home discharge. Our study identifies a factor that can signal caregivers and social workers to aid the patient in finding other members of their family, friends, or community who can support them in the immediate post-acute period, as a stand in to the care of a spouse, to avoid more costly nursing care. Home discharge, in addition to being the least costly option to patients and payers, also increases patient and family satisfaction with their overall health-care experience.10
Our study had several limitations. Firstly, data on discharge locations were limited to “social work notes.” Any last minute divergence from the plan would not be captured in our database. Secondly, while spousal support represents much of in-home care for some middle-aged and elderly patients, the status of “unmarried” does not account for patients who, while not ever or presently married, have children or other nonspousal partners who help them in their home. This is an important form of in-home social support that was not accounted for and is difficult to collect data on retrospectively, as these data are often not reported in the medical record. Also, the status of “married” does not denote the quality of the marriage nor the extent of support received from the patient’s spouse. “Married” status also does not denote the functional level of the “well” spouse, who may themselves need caretaking, a potential motivating factor for the “injured” spouse to return home. Finally, although we controlled for fracture category (ie, upper, lower, axial, polytrauma, etc) in our investigation, future studies will need to address the specific intersection between injury type, prefunctional status, and their effects on discharge disposition, which have not been addressed here.
In sum, patients who are identified as “unmarried” should have early social work intervention to establish discharge goals and expectations early. Early intervention in this way would allow time for contact with close, living relatives or friends who may be able to provide in-home care for the patient or, minimally, sufficient support so that the patient can return home. Increasing home discharge rates by promoting social support for these middle-aged and geriatric fracture patients would reduce lengths of hospital stay and reduce post-acute and long-term care costs for both patient and payers.
Acknowledgments
The authors extend thanks to Kari Broder for her help in the development of this manuscript.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Kenneth A. Egol, MD  https://orcid.org/0000-0002-8125-7451
https://orcid.org/0000-0002-8125-7451
References
- 1. Gurnon E. The staggering prices of long-term care 2017. Forbes, Next Avenue. September 26, 2017. www.forbes.com/sites/nextavenue/2017/09/26/the-staggering-prices-of-long-term-care-2017/#15f755142ee2. Accessed November 2018.
- 2. US Census Bureau. Population Aging Slower than Other Countries, Census Bureau Reports The United States Census Bureau. 2017. www.census.gov/newsroom/press-releases/2016/cb16-54.html. Accessed November 2018.
- 3. De Pablo P, Losina E, Phillips CB, et al. Determinants of discharge destination following elective total hip replacement. Arthritis Rheum. 2004;51(6):1009–1017. [DOI] [PubMed] [Google Scholar]
- 4. Aharonoff GB, Barsky A, Hiebert R, Zuckerman JD, Koval KJ. Predictors of discharge to a skilled nursing facility following hip fracture surgery in New York State. Gerontology 2004;50(5):298–302. [DOI] [PubMed] [Google Scholar]
- 5. Konda SR, Seymour R, Manoli A, Gales J, Karunakar MA; Carolinas Trauma Network Research Group. Development of a middle-aged and geriatric trauma mortality risk score: a tool to guide palliative care consultations. Bull Hosp Jt Dis (2013). 2016;74(4):298–305. [PubMed] [Google Scholar]
- 6. Konda SR, Lott A, Selah H, Schubl S, Chan J, Egol KA. How does frailty factor into mortality risk-assessment of a middle-aged and geriatric trauma population? Geriatr Orthop Surg Rehabil. 2017. ;8(4):225–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Konda SR, Lott A, Saleh H, Gales J, Egol KA. Use of the STTGMA tool to risk stratify 1-year functional outcomes and mortality in geriatric trauma patients. J Orthop Trauma. 2018;32(9):461–466. [DOI] [PubMed] [Google Scholar]
- 8. Lamont CT, Sampson S, Matthias R, Kane R. The outcome of hospitalization for acute illness in the elderly. J Am Geriatr Soc. 1983;31(5):282–288. [DOI] [PubMed] [Google Scholar]
- 9. Narain P, Rubenstein LZ, Wieland GD, et al. Predictors of immediate and 6-month outcomes in hospitalized elderly patients. J Am Geriatr Soc 1988;36(9):775–783. [DOI] [PubMed] [Google Scholar]
- 10. Karlsson S, Edberg AK, Jakobsson U, Hallberg IR. Care satisfaction among older people receiving public care and service at home or in special accommodation. J Clin Nurs. 2013;22(3-4):318–330. [DOI] [PubMed] [Google Scholar]