Abstract
Background:
The use of medical radiation in diagnosis and procedural and surgical treatment is increasing. Therefore, healthcare personnel should be adequately aware and knowledgeable about radiation hazards to protect themselves and their patients from its adverse effects. The objective of this study was to examine awareness about radiation hazards and knowledge about protection methods among the anesthesia personnel and surgical subspecialists of a quaternary care academic center.
Methods:
A validated questionnaire was completed by anesthetic personnel and surgical subspecialists. It consisted of questions that required demographic information and assessed awareness about radiation hazards. In addition, 15 multiple-choice questions assessed knowledge about radiation across the following domains: the main principle of radiation protection, personal annual radiation dose, personal protection equipment, safe distance from an X-ray machine, and susceptible organs.
Results:
A total of 270 potential participants were emailed and invited to respond to an online questionnaire, and the response rate was 79.3%. Of the 214 participants, 69.2% were women; the mean age of the sample was 34.8 years. Most of the participants (63.1%) considered radiation exposure that occurs as a part of daily work to be very harmful; 86.4% and 78.5% reported that they always wore a lead apron and a thyroid shield when working in an environment that entails radiation exposure, respectively. The mean score for knowledge about radiation hazards and protection was 6.4 ± 2.0 (maximum possible score = 15) Therefore, there is a need to improve anesthetic personnel and surgical subspecialists’ knowledge about radiation protection, especially with regard to the use of lead goggles and harmful doses of radiation.
Conclusion:
The present findings suggest that there is a reasonable level of awareness but a relative lack of knowledge about radiation hazards and protection among anesthesia personnel and surgical subspecialists. Therefore, continuing medical education on radiation hazards and protection must be mandated.
Keywords: Radiology, radiation hazard, awareness, knowledge, anesthetic personnel, surgical subspecialists
Introduction
Both ionizing and nonionizing radiations are commonly used in daily medical practice. It plays important roles in both diagnostic and therapeutic modalities. However, ionizing radiation has hazardous effects on interventionists and anesthesia personnel who are exposed to radiation in their workplaces.
Several studies have demonstrated that exposure to medical radiation increases the risk of bone marrow suppression, cataract, infertility, birth deformities, and several types of cancer, especially thyroid carcinoma.1–3 The threshold dose varies across radiation-related diseases. For example, 100–200 mGy is associated with teratogenic effects and cancer,3 whereas 500 mGy is associated with cataracts.4 Therefore, awareness and knowledge about radiation hazards and protective measures play an important role in reducing radiation exposure among healthcare workers.
A general principle of radiation protection, which has been proposed by the International Commission on Radiological Protection (ICRP), states that radiation protection is based on three principles: justification, optimization (as low as reasonably achievable (ALARA)), and dose limitation.5 This is the foundation of radiation protection strategies. Healthcare personnel’s knowledge about radiation hazards and protection has been extensively studied, but inconsistent observations have been made across different medical subspecialties. Nigerian radiologists, radiotherapists, and dentists have been found to demonstrate satisfactory levels of knowledge about radiation hazards and the use of personal protective devices.6 This can be contrasted against the findings of another study that was conducted among pediatric residents and fellows in Italy. Specifically, only 27% of the participants correctly answered questions that assessed knowledge about radiation protection (ALARA).7 These contrasting findings may be attributable to differences between the two study samples. In other words, most of participants of the Nigerian study had been working in a radiology department, whereas the Italian study had been conducted among pediatric residents and fellows.
Research studies have also examined radiation safety awareness among healthcare professionals in Asia-Pacific countries. For example, in one study, in-depth interviews were conducted among medical and dental practitioners in India, and they demonstrated poor awareness about radiation hazards.8 Another study that was conducted among general practitioners, internists, and radiologists in Hong Kong revealed that knowledge and awareness about radiation protection were significantly poorer among nonradiologists. However, the overall knowledge of radiologists was substantially poorer than what was expected.
A majority of past studies have focused on various subspecialties, especially radiology. However, only a few studies have been conducted among anesthesia personnel and surgical subspecialists, even though they are frequently exposed to radiation. Therefore, the primary objective of this study was to examine knowledge and awareness about radiation hazards and knowledge about radiation protection among anesthesia providers and surgical subspecialists.
Methods
This questionnaire-based cross-sectional study was conducted among the anesthesia personnel and surgical subspecialists of a quaternary care academic center in Bangkok, Thailand. This study was approved by the institutional review board (approval no. Si150/2018) and registered at ClinicalTrials.gov (ID: NCT03475927).
A questionnaire was developed by the two authors of this article and validated by six experts: three radiologists, two neurosurgeons who worked in neuroradiology suites, and one anesthesiologist who was also a medical educator. The validity of the questionnaire was examined by computing the index of item-objective congruence (IOC);9,10 an IOC score > 0.6 is considered to be indicative of adequate content validity. The IOC scores of all the items of this questionnaire were >0.6. The questionnaire consisted of three sections: demographic information, awareness about radiation protection practices, and knowledge about radiation hazard (see Appendix 1).
The first section required participants to provide the following demographic information: age, gender, occupational position (staff, resident, fellow, or nurse), work experience (years), department, percentage of total working hours which the respondent was exposed to radiation across the past 12 months, and prior participation in a radiation hazards and protection class.
The second section, which consisted of questions on awareness about radiation hazards and protection practices, assessed awareness about radiation hazards and the habitual use of personal protection, namely, a lead apron, eye goggles, and a thyroid shield, when working in an environment that entails radiation exposure.
The third section, which assessed knowledge about radiation hazards and protection, focused on the following:
The principle of radiation protection (ALARA);11
Maximum permissible dose of radiation per year for workers in general and pregnant women in specific;1
Primary sources of radiation exposure in intervention rooms;1
Organs that are susceptible to radiation-related diseases;1,4
Lead aprons and the standard thickness of lead in a lead apron;1,11
The inverse relationship between the distance between the self and radiation machine and radiation dose;1
The radiation dose of fluoroscopes that are used in medical procedures.1
This section consisted of 15 multiple-choice questions. Each question had four response options, one of which was the correct answer. One point was assigned to each correct answer, and zero points were assigned to each wrong or missing answer.
An online version of the questionnaire was created using Google Forms because this method allows participants to conveniently complete the questionnaire and researchers to immediately and automatically collect data without biasing the data collection process. Potential participants were emailed the link that they had to access to complete the questionnaire between 1 April and 30 June 2018. The participants of this study included the following:
Anesthesiologists and nurse anesthetists (both staff and trainees);
Surgeons and trainees of the following units: cardiothoracic surgery, neurosurgery, orthopedic surgery, urology, and general surgery.
Participants were clearly instructed to complete the questionnaire within 30 min.
At 2 weeks after the first email had been sent to the participants, another email was sent to encourage more participants to respond to the survey. To prevent duplications, the participants were firmly instructed to not respond to the questionnaire again, if they had previously completed it. The participants were informed that their participation in this study was entirely on a voluntary basis before they responded to the questionnaires.
Statistical analysis
In a past study,7 27% of the participants were able to correctly identify what the ALARA principle of radiation protection refers to. Accordingly, the required sample size was found to be 210 participants for the following specifications: 95% confidence interval (CI) for 27 ± 6%. The demographic characteristics of the participants were examined by computing descriptive statistics. Since the total scores were normally distributed, parametric tests were conducted. The mean scores of the different subgroups of the sample (e.g. groups differing in gender, position, and working unit) were compared using independent-samples t-test and one-way analysis of variance (ANOVA). Pearson’s correlation analysis was conducted to examine the relationship between total scores and continuous variables (e.g. age, percentage of radiation exposure during the past 12 months). Data analysis was conducted using Predictive Analytics Software Statistics 18.0.0 (SPSS Inc., Chicago, IL). A p-value < 0.05 was considered to be indicative of statistical significance.
Results
A total of 270 potential participants were emailed and invited to respond to the questionnaire, and the response rate was 79.3% (N = 214). The average age of the participants was 34.8 ± 8.6 years (25–66 years). Most of the participants were women (69.2%) and worked in the Department of Anesthesiology (77.6%). With regard to occupational positions, staff members (34.1%) and residents (33.2%) were overrepresented in the study sample. Their work experience ranged from 6 months to 40 years (Table 1). The mean estimated percentage of time for which the participants had worked in an environment that entailed radiation exposure during normal working hours in the past 12 months was 30.5% ± 21.8% (0%–100%). Most of the participants (65%) had never received any training about radiation hazards.
Table 1.
Demographic data.
| Variable | (N = 214) |
|---|---|
| Age (years) | 34.75 ± 8.56 (25–66) |
| Gender | |
| Male: female | 66 (30.8):148 (69.2) |
| Position | |
| Staff | 73 (34.1) |
| Resident | 71 (33.2) |
| Fellow | 12 (5.6) |
| Nurse anesthetist | 24 (11.2) |
| Nurse anesthetist student | 34 (15.9) |
| Units | |
| Anesthesiology | 166 (77.6) |
| Orthopedics | 19 (8.9) |
| Neurosurgeon | 12 (5.6) |
| Cardiothoracic | 11 (5.1) |
| Urology | 4 (1.9) |
| Vascular | 2 (0.9) |
| Work experience (years) | 7.1 ± 8.1 (0.5–40) |
| Percentage of radiation exposure in the past 12 months | 30.5 ± 21.8 (0–100) |
| Ever attended lesson about radiation hazard | 75 (35) |
Data are presented as mean ± standard deviation (min–max) or n (%).
Awareness about radiation hazards
A majority of the participants (63.1%) considered medical radiation to be very hazardous to human beings. However, one-third of them believed that it was not very hazardous, and a small percentage of them considered it to be nonhazardous (Table 2). Furthermore, 86.4% and 78.5% of them reported that they always wore a lead apron and a thyroid shield when working in environments that entailed radiation exposure, respectively. However, only 31.3% of them reported that they wore lead goggles in such work environments (Figure 1).
Table 2.
Awareness of radiation hazard.
| Variable | n (%) |
|---|---|
| Willing to join the training about radiation hazard | |
| Yes | 139 (64.9) |
| Not sure | 68 (31.8) |
| No | 7 (3.3) |
| Medical radiation hazard | |
| Very hazardous | 135 (63.1) |
| Not much hazard | 72 (33.6) |
| No hazard | 7 (3.3) |
Figure 1.
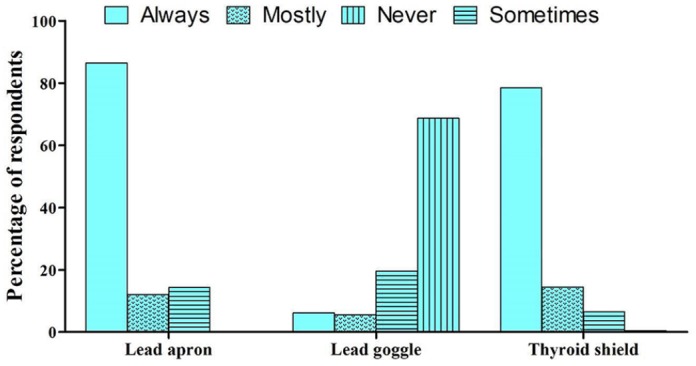
Distribution of participants according to habitual personal protection with lead apron, eye goggles, and thyroid shield while working in an environment with radiation.
Knowledge about radiation hazards and protection
Most of the respondents (85.5%) correctly identified ALARA as the general principle of radiation protection that has been proposed by the ICRP. The percentage of correct answers that were provided to this question did not vary across groups that differed in gender, occupational position, department, or work experience.
The mean and median for the maximum possible score of 15 were 6.4 ± 2.0 and 7, respectively (Figure 2). Men obtained a higher mean than women (p = 0.004; Table 3). Furthermore, senior professionals (e.g. staff) obtained a statistically significant higher mean than the others (Table 3). However, age, department, and work experience did not have a significant effect on knowledge. Only 25.7% of the participants had provided correct responses to the questions that assessed the use of lead aprons, and 24.3% of them correctly specified the safe distance that must be maintained between a worker and a radiation machine. Moreover, 5.1% and 1.9% of the participants provided correct answer to all the questions that pertained to the use of lead goggles and harmful doses of radiation, respectively.
Figure 2.
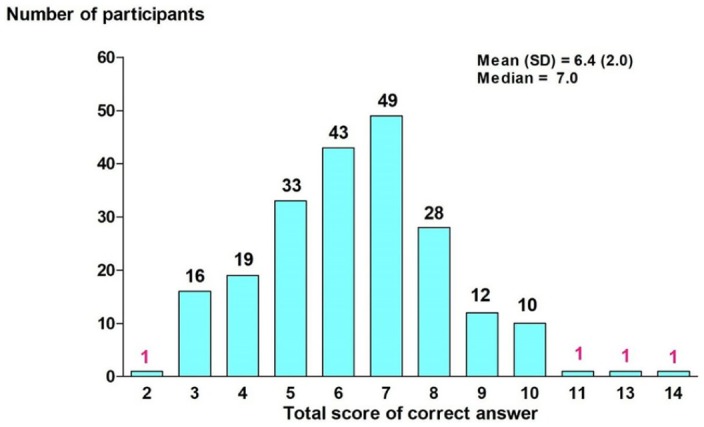
Distribution of participants according to score.
Table 3.
Factors associated with the score of correct answer (0–15) in 214 subjects.
| Variable | n (%) | Total score: mean ± SD | p-value |
|---|---|---|---|
| Age | r = 0.63 | 0.361 | |
| Gender | |||
| Male | 66 (30.8) | 7.0 ± 2.3 | 0.004 |
| Female | 148 (69.2) | 6.1 ± 1.7 | |
| Position | |||
| Staff | 73 (34.1) | 6.9 ± 2.1 | 0.012 |
| Fellow | 12 (5.6) | 6.8 ± 2.1 | |
| Resident | 71 (33.2) | 6.1 ± 1.7 | |
| Anesthetic nurse | 24 (11.2) | 6.3 ± 2.0 | |
| Anesthetic nurse student | 34 (15.9) | 5.7 ± 1.6 | |
| Working unit | |||
| Anesthesiology | 166 (77.6) | 6.4 ± 2.0 | 0.586 |
| Surgerya | 48 (22.4) | 6.2 ± 1.9 | |
| Working experience (years) | |||
| ⩽10 | 166 (77.6) | 6.3 ± 1.9 | 0.238 |
| >10 | 48 (22.4) | 6.7 ± 2.2 | |
| Training of radiation hazard | |||
| Train | 75 (35) | 6.5 ± 2.0 | 0.086 |
| Not train | 139 (65) | 6.1 ± 1.9 | |
| Percentage of radiation exposure in the past 12 months | r = –0.027 | 0.693 | |
SD: standard deviation.
Surgery includes cardiothoracic, neurosurgery, orthopedics, urosurgery, and vascular surgery.
Discussion
To the best of our knowledge, this study was the first attempt to examine knowledge and awareness about radiation hazards among anesthetic personnel and surgical subspecialists in Thailand. The main findings of this study are that most participants considered radiation exposure that occurs as a part of daily work to be very hazardous. Furthermore, most of the participants reported that they always wore a lead apron and a thyroid shield when working in an environment that entailed radiation exposure, respectively. The mean score for knowledge about radiation hazards was 6.4 ± 2.0.
Awareness about radiation hazards
In contradistinction to the present findings, a survey that was conducted among 92 Turkish health personnel including doctors, nurses, and technicians found that 42.4% and 21.7% of them were unaware about radiation hazards and considered common radiologic studies to be moderately safe, respectively.12 On the other hand, 77.3% of the radiology, radiotherapy, and dental staff of a teaching hospital in Nigeria6 were found to be aware about radiation hazards. Similarly, 82% of anesthesia residents in the United States were found to have very high or high levels of concerns about radiation hazards.13 With regard to the Asia-Pacific region, Fan et al.14 found that 78.2% of orthopedic surgeons in China considered radiation exposure to be an issue of great concern.
In order to protect themselves against radiation exposure, 78.5% of the participants of this study wore a thyroid shield, but only 31.3% of them wore lead goggles. Another study14 that was conducted among orthopedic surgeons found that 35%, 3%, and 6% of them preferred to use a mobile lead shield than wear protective apparel, wore lead glasses, and worked without a personal protective device, respectively. Similarly, another survey that was conducted in Nigeria in 201315 found that only 12%, 5%, and 3% of radiographers consistently wore a lead apron, lead goggles, and a thyroid shield in their work environments, respectively.
Almost all the participants (96.7%) of this study considered radiation to be very harmful or harmful. However, only 86.4% and 78.5% of them always wore a lead apron and thyroid shield in their work environments, respectively. These low rates of compliance may be attributable to some participants’ preference for the use of mobile lead shields as an alternative means of radiation protection. Unfortunately, the questionnaire did not include any question that assessed the use of mobile lead shields.
A low rate of compliance with regard to the wearing of lead goggles was found. The medical community has been aware of the issue of radiation-induced germ cell mutations for many decades. On the other hand, radiation-induced thyroid cancer and cataracts have emerged as issues of concern only during the past decade, and relatively less importance has been ascribed to radiation-induced cataracts than to radiation-induced thyroid cancer. Another reason for the low rates of compliance is the limited availability of lead goggles in work environments, when compared to other protective equipment. Therefore, staff should be encouraged to routinely wear lead goggles by making them aware of the adverse consequences of not wearing lead goggles and increasing the availability of lead goggles in workplaces. Their awareness can be enhanced by integrating training that is offered by the staff of radiology departments into undergraduate education and providing annual radiation protection courses to postgraduate students. Furthermore, the routine practice of radiation protection should be encouraged in daily practice.
Knowledge about radiation hazards
ALARA is the fundamental principle that underlies radiation protection, and it enhances knowledge about radiation protection. Most of the participants (85.5%) of this study provided the correct answer to the question on the ALARA principle. However, each person who works in environments that entail radiation exposure should know this principle. Moreover, the overall mean knowledge score was only 6.4 ± 2.0 (maximum possible score = 15), and most of the participants obtained scores that lay below the median (i.e. 7). Our findings suggest that healthcare personnel’s knowledge about radiation hazards and protection requires further improvement. Most of the surgical and anesthetic staffs who participated in the study had never received any formal training on radiation protection, and this may be an important reason that accounts for their inadequate knowledge in this domain.
The level of knowledge about radiation hazards and protection did not differ significantly between surgical subspecialists and anesthesia personnel and between groups that differed in age, prior participation in a radiation hazards and protection course, or exposure to radiation. On the other hand, a small albeit significant difference in knowledge emerged between groups that differed in gender and professional level. Men and senior professionals obtained slightly higher scores than women and nurse anesthesia students, respectively. Since senior professionals had greater experience in working in environments that entail radiation exposure and in radiation suites, they may have been required to update their knowledge about radiation protection. A higher percentage of men (57.6%) than women (23.6%) were senior professionals, and this may explain the slightly higher scores that were obtained by men. However, the anesthesia and surgical personnel who participated in this study demonstrated inadequate knowledge about radiation protection. Therefore, training about radiation protection is urgently needed. This result is similar to many past findings. Studies that have been conducted among radiology personnel16,17 have shown that they possess inadequate knowledge about radiation protection. Hobbs et al.18 conducted studies among healthcare providers who belong to multiple departments and found that their knowledge about radiation exposure and risk was poor at baseline but had significantly improved after participation in a brief educational presentation. Another study that was conducted among the physicians, interns, and radiologists of a hospital in Hong Kong19 found that all three groups demonstrated very poor levels of knowledge about radiation protection. Furthermore, although radiologists demonstrated inadequate levels of knowledge, they were more knowledgeable than the other two groups.
The other findings of this study, which pertain to participant responses to questions about radiation doses, the use of lead goggles and aprons, and safe distances that must be maintained between personnel and radiation machines, are interesting and merit further discussion. Although it is important for anesthesia and surgical personnel to know the answers to all these questions, very few participants provided correct answers. This was especially evident for questions that pertained to radiation dose (i.e. maximum radiation dose and radiation levels of each procedure) and the use of lead goggles. The number of participants who had correctly answered these questions was only 1.9% and 5.1%, respectively. This finding suggests that there is an urgent need to educate anesthesia personnel and surgical subspecialists about many topics that pertain to radiation protection (including radiation usage and protective equipment) to reduce their exposure to occupational hazards.
Ideally, all healthcare personnel should be mindful of the fact that medical radiation is hazardous and protect both themselves and patients from radiation exposure.
Limitations of this study
The items of the questionnaires that were used in past studies and this research may have been different. Therefore, direct comparisons between the present and past findings must be made with caution.
Conclusion
Awareness and knowledge about radiation hazards may differ based on the occupational roles, level of training, and even nationality of healthcare professionals. The present findings revealed that, in general, there was a high level of awareness about radiation hazards among the present sample. Most of the participants reported that they use protective equipment (except lead goggles) when they work in environments that entail radiation exposure. However, an extremely high number of anesthetic personnel and surgical subspecialists demonstrated inadequate knowledge about radiation hazards. These findings underscore the need to enhance awareness and knowledge about radiation hazards among anesthesia personnel and surgical subspecialists.
Acknowledgments
The authors would like to thank Dr Chulalux Komoltri for her contribution toward data interpretation and statistical analysis and Ms Nichapat Sooksri for her assistance in data collection.
Appendix 1
The awareness of radiation hazard and knowledge of radiation protection questionnaire
Part 1: General information
Gender
□ Male □ Female
Age ………….. years
Position
□ Staff □ Resident □ Fellow □ Nurse anesthetist □ Nurse anesthetist student
Department
□ Anesthesiology □ Cardiothoracic surgery □ General surgery □ Neurosurgery □ Orthopedic surgery □ Urology
How many years have you been practicing in your spe-cialty? …………………… years
In the past 12 months, how much percentage did you work in an environment that exposed to radiation, please esti-mate? ……………………. %
Have you ever participated in any radiation protection training course?
□ Yes □ No
Part 2: Awareness of radiation hazard
-
If there is radiation protection training course in our institute, do you want to join?
□ Yes □ Not sure □ Not join
-
In your opinion, how hazardous is radiation to your body?
□ Very hazardous □ Not much hazardous □ Nonhazardous
-
Have you ever worn lead apron when you work with radiation?
□ Yes, every time □ Yes, mostly □ Yes, sometimes □ No, never
-
Have you ever worn lead goggle when you work with radiation?
□ Yes, every time □ Yes, mostly □ Yes, sometimes □ No, never
-
Have you ever worn thyroid shield when you work with radiation?
□ Yes, every time □ Yes, mostly □ Yes, sometimes □ No, never
Part 3: Knowledge about radiation hazard and protec-tion
Choose the best answer in each of the following questions
- From International Commission on Radiological Protection (ICRP), which of the following is the principle of radiation protection?
- as low as reasonably achievable (ALARA)
- as big as reasonably achievable (ABARA)
- as fast as reasonably achievable (AFARA)
- as slow as reasonably achievable (ASARA)
- From International Commission on Radiological Protection (ICRP) recommendation, how much is 1-year maximum permissible dose limit for adult radiation workers?
- 0.5 mSv
- 5 mSv
- 50 mSv
- 500 mSv
- From International Commission on Radiological Protection (ICRP) recommendation, how much is 1-month maximum permissible dose limit for pregnancy radiation workers?
- 0.01 mSv
- 0.05 mSv
- 0.1 mSv
- 0.5 mSv
- In the intervention room, which of the following is the major source of radiation affect to healthcare workers?
- Direct from primary beam itself
- Reflection from patient
- Other part of X-ray machine (not primary beam)
- Reflection from wall of room
- To which organ, radiation can be hazardous?
- Ovary and testis
- Thyroid gland
- The eyes
- All of the above
- From International Commission on Radiological Protection (ICRP) recommendation, how much thickness of lead should be inserted in the lead apron?
- 0.05 mm
- 0.1 mm
- 0.3 mm
- 0.5 mm
- Which of the following is TRUE about lead apron?
- After use, lead apron should be folded before collection
- Barium, tungsten, tin, and antimony can be inserted in the lead apron instead of lead to reduce the weight
- Lead apron can reduce the radiation dose to personnel by 70%
- Worker should wear as thick lead apron as possible to reduce the radiation dose maximally
- By how much percent, prescribed plastic lens can reduce radiation dose?
- 80
- 60
- 30
- 5
- By how much percent, prescribed glass lens can reduce radiation dose?
- 80
- 60
- 30
- 5
- Which of the following is true about lead goggle?
- Lead goggle can reduce radiation dose to personnel by 80%
- Only the primary operator should wear lead goggle because he/she is closest to the primary X-ray beam
- From International Commission on Radiological Protection (ICRP) recommendation, 0.5–0.75 mm of lead thickness should be inserted in the lead goggle
- Prescribe glass lens can be used as radiation protection glass
- Radiation dose decreases with distance. What is the formula of radiation decrease by distance? (d = distance between the worker and the primary beam)
- From International atomic energy agency (IAEA) recommendation, what is the safe distance between the worker and the X-ray machine?
- 0.2–0.5 m
- 0.5–0.75 m
- 0.75–1 m
- 1–2 m
- Which of the following is TRUE about dosimeters?
- Dosimeters can be switched between personnel
- Dosimeters must be placed outside of the lead apron
- Dosimeters should be collected for measuring the radiation amount every 6 months
- There is only one type of dosimeter, which is film-badge dosimeter
- What is the radiation amount of chest X-ray?
- 0.02 mSv
- 0.05 mSv
- 0.5 mSv
- 1 mSv
- During intervention using fluoroscope, how much radiation amount compared to chest X-ray (CXR) does the patient have to receive?
- 1–10 times more than CXR
- 10–20 times more than CXR
- 20–50 times more than CXR
- 100–1000 times more than CXR
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from Siriraj Institutional Review Board (approval no. Si 150/2018).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: In the questionnaire, the participants were informed that their participation in this study was entirely on a voluntary basis before they responded to the questionnaires. The formal informed consent was waived by the Institutional Review Board/Ethics Committee.
Trial registration: This study was registered at ClinicalTrials.gov (ID: NCT03475927).
ORCID iD: Chaowanan Khamtuikrua  https://orcid.org/0000-0001-5021-4566
https://orcid.org/0000-0001-5021-4566
References
- 1. Dagal A. Radiation safety for anesthesiologists. Curr Opin Anaesthesiol 2011; 24: 445–450. [DOI] [PubMed] [Google Scholar]
- 2. Iglesias ML, Schmidt A, Ghuzlan AA, et al. Radiation exposure and thyroid cancer: a review. Arch Endocrinol Metab 2017; 61(2): 180–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sont WN, Zielinski JM, Ashmore JP, et al. First analysis of cancer incidence and occupational radiation exposure based on the National Dose Registry of Canada. Am J Epidemiol 2001; 153(4): 309–318. [DOI] [PubMed] [Google Scholar]
- 4. Chodick G, Bekiroglu N, Hauptmann M, et al. Risk of cataract after exposure to low doses of ionizing radiation: a 20-year prospective cohort study among US radiologic technologists. Am J Epidemiol 2008; 168(6): 620–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Park JY, Park SJ, Choi SU, et al. Target-controlled propofol infusion for sedation in patients undergoing transrectal ultrasound-guided prostate biopsy. J Int Med Res 2007; 35(6): 773–780. [DOI] [PubMed] [Google Scholar]
- 6. Awosan KJ, Ibrahim M, Saidu SA, et al. Knowledge of radiation hazards, radiation protection practices and clinical profile of health workers in a teaching hospital in Northern Nigeria. J Clin Diagn Res 2016; 10(8): LC07–LC12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Salerno S, Marchese P, Magistrelli A, et al. Radiation risks knowledge in resident and fellow in paediatrics: a questionnaire survey. Ital J Pediatr 2015; 41: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sukumar S, Rajagopal K, Sabu K. Perception of radiation awareness among medical doctors in India. Int J Pharm Biol Sci 2013; 3: 371–376. [Google Scholar]
- 9. Turner RC, Carlson L. Indexes of item-objective congruence for multidimensional items. Int J Test 2003; 3: 163–171. [Google Scholar]
- 10. Rovinelli RJ, Hambleton RK. On the use of content specialists in the assessment of criterion-referenced test item validity. Dutch J Educ Res 1976; 2: 49–60. [Google Scholar]
- 11. The 2007 recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP 2007; 37: 1–332. [DOI] [PubMed] [Google Scholar]
- 12. Yurt A, Cavusoglu B, Gunay T. Evaluation of awareness on radiation protection and knowledge about radiological examinations in healthcare professionals who use ionized radiation at work. Mol Imaging Radionucl Ther 2014; 23(2): 48–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wang RR, Kumar AH, Tanaka P, et al. Occupational radiation exposure of anesthesia providers: a summary of key learning points and resident-led radiation safety projects. Semin Cardiothorac Vasc Anesth 2017; 21(2): 165–171. [DOI] [PubMed] [Google Scholar]
- 14. Fan G, Wang Y, Guo C, et al. Knowledge deficiency of work-related radiation hazards associated with psychological distress among orthopedic surgeons: a cross-sectional study. Medicine 2017; 96(21): e6682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Eze CU, Abonyi LC, Njoku J, et al. Assessment of radiation protection practices among radiographers in Lagos, Nigeria. Niger Med J 2013; 54(6): 386–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ramanathan S, Ryan J. Radiation awareness among radiology residents, technologists, fellows and staff: where do we stand? Insights Imaging 2015; 6(1): 133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Paolicchi F, Miniati F, Bastiani L, et al. Assessment of radiation protection awareness and knowledge about radiological examination doses among Italian radiographers. Insights Imaging 2016; 7: 233–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hobbs JB, Goldstein N, Lind KE, et al. Physician knowledge of radiation exposure and risk in medical imaging. J Am Coll Radiol 2018; 15: 34–43. [DOI] [PubMed] [Google Scholar]
- 19. Wong CS, Huang B, Sin HK, et al. A questionnaire study assessing local physicians, radiologists and interns’ knowledge and practice pertaining to radiation exposure related to radiological imaging. Eur J Radiol 2012; 81(3): e264–e268. [DOI] [PubMed] [Google Scholar]


