Short abstract
Objective
To date the application of eHealth strategies among adults and adolescents undergoing metabolic and bariatric surgery (MBS) has not been systematically reviewed. This study comprehensively examines eHealth intervention studies among MBS patients within the RE-AIM framework to assess reach, effectiveness, adoption, implementation and maintenance of these efforts.
Methods
A search was conducted using PubMed, EMBASE, CINAHL, PsycNET and SCOPUS of original research relating to eHealth strategies for MBS patients published in peer-reviewed journals and revealed 38 published articles between 2011 and 2019.
Results
Studies varied widely in terms of design (qualitative to randomized controlled trials) and eHealth delivery method (telemedicine to blog post content) with a balance of pre- or post-MBS use. No studies included adolescents and very few reported (1) a conceptual framework to support study design/outcomes; and (2) race/ethnicity composition.
Conclusions
Although some studies report that eHealth strategies/interventions are effective in producing post-MBS weight loss and other positive health outcomes, most are pilot studies or have study design limitations. There is an opportunity for development of (1) tailored eHealth interventions to support pre- and post-MBS sustained behavior change and improved outcomes; and (2) rigorous studies that employ robust conceptual frameworks so dissemination and implementation efforts can be mapped to construct-driven outcomes.
Keywords: eHealth, mHealth, severe obesity, bariatric surgery, metabolic, outcomes
Introduction
A 130% increase in the prevalence of severe or extreme obesity (body mass index (BMI) ≥40 or ≥35 with ≥1 comorbidity) is estimated over the next two decades.1,2 This is a sobering projection for healthcare systems given the chronic health-related consequences of obesity, including type 2 diabetes, cardiovascular and liver disease, osteoarthritis and some forms of cancer.2 Worldwide studies show that not only is metabolic and bariatric surgery (MBS) the most effective weight loss treatment, but for individuals with a BMI of ≥35 it is the only treatment that is able to provide long-term weight loss (≥50% weight loss maintained for a minimum of five years).2–4 MBS not only improves weight loss outcomes, but also substantially improves type 2 diabetes; recent studies have reported remission rates of 80% for type 2 diabetes in patients 36 months post-MBS.2,4 As such, the UK National Institute of Health and Care Excellence Obesity Guidance and the International Diabetes Federation promote MBS as an effective treatment option for severe obesity.3,4
Despite MBS showing significant post-operative weight loss trajectories for many patients, these findings are not universal primarily due to lack of adherence to post-operative lifestyle modifications. To achieve maximum weight loss and prevent weight regain, patients must increase physical activity, decrease sedentary behaviors, and adhere to dietary recommendations including vitamin/micronutrient intake in particular.5 Unfortunately, these patients often face numerous challenges (e.g. transportation, socioeconomic, geographical, social support issues) that prevent them from seeking further assistance or support to improve and prolong weight loss outcomes.5 Current studies document the promising effects of use of mobile and online technologies (eHealth), including wearable devices for improving health outcomes among those with obesity and diabetes (common precondition for MBS) by eliminating geographic, time and transportation barriers.5 Post-MBS weight loss maintenance interventions that are accessible, cost-effective and scalable are not only desirable, but have the potential for both deep and wide impact on health outcomes. This review explored the use of eHealth interventions among those adults and adolescents who are considering (pre) or those who have undergone (post) MBS. A broad definition of eHealth was applied to include interventions using the internet, social media (Facebook, Twitter, Snapchat, Instagram) internet/WiFi-enabled wearable devices, telemedicine, email, short messaging services (SMS) and e-learning.
eHealth strategies applied to obesity prevention and treatment
In the adult literature, current studies show that the delivery of obesity prevention and treatment eHealth strategies are both cost effective and scalable.6–8 Evidence-based eHealth dissemination strategies include websites, emails, text messages, monitoring devices, mobile applications, computer programs, podcasts and personal digital assistants. Many eHealth systems are used to set and track individual goals, to monitor diet and physical activity and to create tailored responses based on behavior change progress. Specifically, in a meta-analyses of eHealth weight loss or weight maintenance interventions Hutchesson et al.6 reported modest weight loss compared with no behavior treatment (mean difference: –2.70 (–3.33, –2.08), p < 0.001; nine studies pooled) or minimal treatment (mean difference: –1.40 (–1.98, –0.82), p < 0.001; 16 studies pooled). eHealth interventions with features including self-monitoring and personalized feedback or technologies such as text messages and social media were more effective than standard eHealth programs (mean difference: 1.46 (0.80, 2.13), p < 0.001). Reviews in young adults have not reported such strong supportive findings. Willmott et al.9 found a limited evidence base for eHealth weight management interventions targeting young adults but this was largely due to weak study designs.
A recent review and meta-analysis10 of the evidence for BMI/BMI z-score improvements in eHealth randomized controlled trials to prevent (n = 3 studies included) or treat (n = 5 trials included) overweight/obesity in children and adolescents ages 0–18 years focused on parents/caregivers as agents of change. Meta-analysis results showed no significant difference in the effects of parent-focused eHealth obesity interventions on child BMI/BMI z-score compared with a control (standardized mean difference –0.15, 95% confidence interval –0.45 to 0.16, z = 0.94, p = 0.35). The authors concluded that there is a need for more robust, high-quality parent-focused eHealth studies that target families with younger children.
eHealth strategies applied to diabetes management
Numerous studies have reported that eHealth interventions are effective in diabetes self-management programs. In a systematic review conducted by Greenwood et al.,11 the use of multiple modalities, including text messages and email, improved HbA1c levels among participants with type 2 diabetes. Review studies incorporated a variety of features such as communication, education, feedback and patient-generated health data which showed significant improvement in A1c levels when two-way communication between patient and health care provider was utilized, as well as customized education support and real-time feedback.
Joiner et al.12 reported the use of eHealth lifestyle programs based on the Diabetes Prevention Program that resulted in a mean –3.98% weight loss from baseline to 15 month follow-up across all interventions. The subtotal estimate across the stand-alone eHealth interventions (–3.34%) was less than the estimate across interventions with behavioral support given by a counselor remotely (–4.31%) and the estimate across interventions with behavioral support given by a counselor in-person (–4.65%). The majority of the interventions in this study included web-based applications such as video conferencing, SMS and mobile applications, in addition to behavioral support from a counselor via face-to-face communication, online messages, email and telephone.
eHealth strategies in pre–post MBS care management
As shown above, there is increasing evidence to support the use of eHealth strategies in adults with obesity and type 2 diabetes. Given that type 2 diabetes is one of the most prevalent co-morbidities associated with severe obesity, it is logical to think that these same eHealth strategies may be effective in pre- and post-MBS education, knowledge, behavior change and social support delivery. However, it is also important to measure the acceptability of such strategies, and whether they improve MBS outcomes. Indeed, Das et al.13 reported that an eHealth portal tailored to provide post-operative MBS support decreased attrition rates in clinical follow-ups and improved adult patients’ health. Additionally, the eHealth portal became a safe outlet where patients could express their concerns and seek assistance in real-time. It also allowed providers to better tailor their care to meet the patients’ needs.
To date, no systematic reviews are available that focus on the application of eHealth strategies and/or interventions in adults or adolescents who are either making the decision to have MBS or who have already completed the procedure. Moreover, the studies that do exist in the literature do not employ conceptual frameworks to guide dissemination and implementation efforts that can be mapped to construct-driven outcomes.
Conceptual frameworks to support the dissemination and implementation of eHealth strategies in MBS patients
RE-AIM
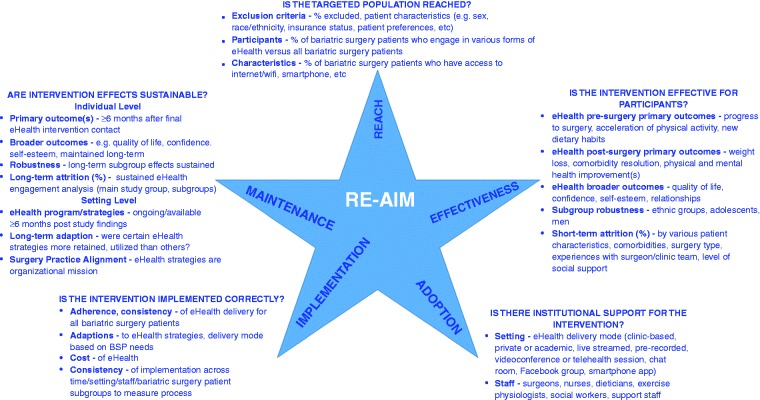
The dissemination and implementation of eHealth strategies has not been consistently guided by conceptual frameworks in clinical settings regardless of the patient population. The RE-AIM (Reach, Effectiveness/Efficacy, Adoption, Implementation, and Maintenance) framework has been highly compatible with community-based public health intervention dissemination and implementation in various fields.14–18 RE-AIM was initially designed to help evaluate interventions and public health programs, to produce a more balanced approach to internal and external validity and to address key issues important for dissemination and generalization.14 RE-AIM has been applied to policies15,16 and community-based multilevel interventions,17 and to studies focused on reducing health disparities.18 The dimensions of the framework are as follows: (1) Reach (the absolute number, proportion and representativeness of individuals who are willing to participate); (2) Effectiveness (impact of an intervention on outcomes, including potential negative effects, quality of life, and economic outcomes); (3) Adoption (absolute number, proportion, representativeness of settings and intervention agents willing to initiate a program); (4) Implementation (intervention agents’ fidelity to various elements of an intervention’s protocol including consistency of delivery as intended, intervention time and cost); and (5) Maintenance (extent to which a program/policy becomes institutionalized or part of the routine organizational practices and policies, but also has individual-level outcomes). While generally the dimensions of ‘Reach’ and ‘Effectiveness’ apply to individuals, and ‘Adoption’, ‘Implementation’ and ‘Maintenance’ to a setting/system, all five of the dimensions have applicability to the dissemination and implementation of eHealth interventions among individuals who are considering MBS or who have already completed the procedure (Figure 1). Within this framework, it has been recommended that obesity interventions use multiple disciplines and perspectives in creating and implementing programs, integrate research and practice partnerships and assess the potential of intervention strategies to reduce health disparities.17,18 This is true particularly in low resource settings and for populations traditionally underrepresented in obesity research, for which dissemination and implementation may not be a simple process, particularly when multiple entities are involved (surgeons, dietitians, primary care physicians, other sub-specialists, family members, other social support members).14 Given that MBS is an elective surgery and patients will most likely return to their pre-operative environments (work, school, family, household, neighborhood, community, rural or urban geographic area), applying eHealth strategies can address barriers to follow-up care experienced by many patients, including geographic distance, transportation and economic limitations. However, further study to determine the breadth of patients who would use it and the support needed from healthcare settings is essential to understand the infrastructure needed for widespread use.
Figure 1.
RE-AIM (Reach, Effectiveness, Adoption, Implementation, Maintenance) dimensions as applied to the use of eHealth strategies among individuals considering bariatric surgery or who have completed the procedure.
To address the abovementioned gaps in the literature, this review summarizes the current state of eHealth strategies as applied to those who are either considering (pre) or have completed (post) MBS. The review was particularly focused on capturing any previous application and integration of a conceptual framework to support the study hypotheses and to map to primary or other outcomes.
Methods
A literature search was conducted in February 2019 using the following electronic databases: Medline, Psych INFO, Social Sciences Citation Index, and Web of Science. Keyword searches were conducted using Boolean operators “AND” and “OR” to specify or broaden the search. The wildcard character “*” was used to truncate words to include all forms of the root word. “bariatric surgery”, “weight loss surgery”, gastric bypass surgery”, “adjustable gastric band”, “sleeve gastrectomy”, “gastroplasty,” “jejunoileal bypass”, “duodenal switch”, “roux en y”, “gastric balloon”, “metabolic surgery”, “metabolic and bariatric surgery”, “obesity”, “surgery”, “morbid”, “telecommunications”, “electronic mail”, “telemedicine”, “remote consultation”, “cell phone”, “videoconferencing”, “smartphone”, “social media”, “internet”, “eHealth” and “mHealth” were included with all keywords. Key words were searched throughout the entire text of identified manuscripts and included all relevant terms to capture the use of eHealth strategies among patients either considering or who had completed MBS.
In summary, the specific inclusion criteria for articles included in this review were (1) published in a peer-reviewed journal (online and/or print format); (2) mentioned or addressed eHealth or mHealth delivery and/or intervention strategies in the MBS patient population; (3) included both adults (≥18 years old) or adolescents (<18 years old) who were either considering or who had completed MBS (see PRISMA flow diagram and checklist in the Supplementary Material online for details). There was no restriction on publication date or language, as the goal of this review was to be as comprehensive as possible. Case studies were not included in this review as none were captured in the overall search. Data were abstracted independently by two of the authors to ensure reliability. Articles were identified by first examining titles and abstracts followed by the full text of relevant articles. Reference lists of selected articles also were examined to further detect other published research.
Search criteria key reported outcomes
This review was specifically focused on each included article’s reported outcomes within the RE-AIM framework using a checklist created by the Implementation Science Team at the National Cancer Institute as a guide to score National Institutes of Health grant proposals but easily adapted for policy/program analysis and journal articles.19 Specifically, the checklist includes the following: (1) Reach – sample characteristics including the number of study participants and demographic characteristics if available; (2) Efficacy/Effectiveness – primary and/or secondary or broader outcomes (cardiometabolic or other physical health outcomes, mental health or psychosocial consequences such as improvement in anxiety, depression, disordered eating, quality of life) and use of qualitative methods/data to interpret outcomes; (3) Adoption (setting and staff, not individual level) – characteristics of settings/staff participating, exclusions, percent of settings/staff approached that participated (e.g. valid denominator) and use of qualitative methods to understand adoption at setting/staff level; (4) Implementation – attention to adherence, fidelity, consistency of delivery, adaptations, cost and use of qualitative methods to understand implementation; and (5) Maintenance – measure of primary outcome at both the individual and setting levels at ≥6 months’ follow-up after final intervention contact, measure of broader outcomes or use of multiple criteria at follow-up, robustness of data, long-term attrition (%) and differential rates by patient characteristics or treatment condition.
Results
Tables 1 and 2 summarize the current state of the literature in terms of published eHealth strategies, programs and interventions specifically targeting individuals who are either undergoing or who have completed MBS by study design (review articles to randomized controlled trials) and several other key characteristics.14–61 Specifically, Tables 1 and 2 are organized by the RE-AIM constructs as follows: (1) the Reach column reports sample characteristics (e.g. unit of analysis, mean age, sex); (2) the Efficacy/Effectiveness column reports the primary focus or premise of the study; (3) the Adoption column summarizes the key reported primary and secondary (where applicable) outcomes; (4) the Implementation column reports the eHealth mechanism (e.g. smartphone app, Facebook content, etc.); and (5) the Maintenance column reports primary outcomes at >6 months’ follow up, if applicable. Studies are organized by design (review, qualitative and mixed methods in Table 1 and observational/cross-sectional, retrospective/prospective cohort, quasi-experimental/case control, and randomized controlled trials in Table 2) and summarized in the following Results section. Overall findings are then synthesized by RE-AIM constructs in the Discussion section.
Table 1.
Summary of current literature reviews, qualitative and mixed methods studies that include eHealth strategies among patientsa undergoing metabolic and bariatric surgery by key outcome and other characteristics within the RE-AIM conceptual frameworkb.
|
Reach |
Efficacy/Effectiveness |
Adoption |
Implementation |
Maintenance |
Conceptual/ theoretical frameworkc |
|
|---|---|---|---|---|---|---|
| Authors (year) | Sample characteristics | Primary focus | Key reported outcomes | eHealth mechanism | Primary outcome at ≥6 month follow-up | |
| Reviews (n = 6) | ||||||
| Coldebella et al. (2018)20 | 10 studies (818 participants) ages 33–54, mostly female | Telemedicine as a potential method for providing healthcare services to MBS patients | 9/10 studies showed positive service delivery outcomes (feasibility, acceptability, quality of life, eating psychopathology) related to telemedicine use | Telemedicine (10 studies included) | N/A | No |
| Groller (2017)21 | 24 studies (2546 subjects) | MBS center written and online pre/post education practices (curriculum, delivery) | Practices varied by curriculum and dose; written or web-based aides supported pre–post MBS learning needs | Web-based mediums | N/A | No |
| Zhang et al. (2016)22 | N/A; app is unit of analysis | Assessed quality of information shared on smartphone apps related to MBS patient care | Average score of 4 (SD: 1.76) on Silberg2 scale (information quality assessment), on a scale of 0–9 | Smartphone apps | N/A | No |
| Bond and Thomas (2015)23 | 24 patients in pilot study; no demographics provided | Physical activity and sedentary behaviors in relation to MBS outcomes (mHealth vs. self-reported outcomes) | mHealth technology can be used to modify Physical activity and sedentary behaviors and provide more accurate measurements versus self-report | mHealth technology; wearables to track post-operative physical and sedentary behavior | N/A | No |
| Stevens et al. (2014)24 | N/A; app is unit of analysis | 28 smartphone apps related to MBS were reviewed | Smartphone apps have potential to provide accurate, reliable information; health professional involvement in only 12/28 apps | Smartphone apps | N/A | No |
| Thomas et al. (2011)25 | Not specified | Accuracy of reporting and a delivery mechanism for innovative interventions | Mixed results in the literature are due to the inaccuracy of self-reporting | Ecological momentary assessment via palmtop computer; accelerometers | N/A | No |
| Qualitative studies (n = 9) | ||||||
| Koball et al. (2018)26 | N/A; qualitative content analysis | Describe content of nutrition-related information sought on MBS Facebook support groups/pages. Secondary aim was to evaluate the accuracy of this content | Over 50% of posts contained inaccurate content; 7% of posts were inconsistent with American Society for Metabolic and Bariatric Surgery nutrition guidelines and expert opinions | Facebook MBS support groups | N/A | No |
| Groller (2018)27 | N/A; comments on previous publication only | Letter to the Editor; commented on Koball et al. (2018), who reported > 50% of Facebook posts were inaccurate | Healthcare professionals need to warn patients and teach how to decipher the credibility of online messages | Facebook support groups | N/A | No |
| Meleo-Erwin (2019)28 | N/A; qualitative thematic analysis | Thematic analysis of 217 blog posts on patient post-operative follow-up care experiences | Patients tell complex stories about their post operative experiences with their MBS home clinic | Blog posts and online forum comments | N/A | No |
| Willmer and Salzmann-Erikson (2018)29 | N/A; qualitative analysis | Purposeful qualitative content approach of shared values, feelings and thoughts among MBS patients | Four themes were constructed during data analysis: (1) a new life; (2) negotiating the system and playing the waiting game; (3) managing the pre-operative diet; and (4) managing others’ attitudes | Online MBS blog | N/A | Epistemology of naturalistic inquiry |
| Koball et al. (2017)30 | N/A; Facebook support group content was unit of analysis | Extraction of data from MBS support groups/pages on Facebook over one month via content analysis | Seeking recommendations (11%), information/recommendations (53%), change since MBS (19%), and lending support (32%) most common post content | MBS support groups and pages on Facebook | N/A | No |
| Zhang et al. (2016)31 | N/A | Illustrate development of an MBS after-care smartphone app; highlight user feature preferences | Users generally receptive toward use; valued information on multidisciplinary team consult meeting content and ability to reschedule appointments | MBS after-care smartphone application | N/A | No |
| Das and Faxvaag (2014)32 | 60 participants; 75% women; mean age 40 | Exploration of forum usage by MBS patients and what influenced their participation in the forum over one year (6800 posts) | Major themes that influenced online discussion forum participation: (1) motivation to seek information, advice and guidance; (2) need for peer social support and networking; and (3) concerns regarding self-disclosure | Online discussion forum | N/A | No |
| Connor et al. (2013)33 | N/A; app is unit of analysis | Letter to the Editor; commented on Stevens et al. (2014) showing 32% medical involvement | Smartphone apps could be valuable for providers for patient performance data; research should include this delivery method | Smartphone apps | N/A | No |
| Cranwell and Seymour-Smith (2012)34 | N/A; support group content was unit of analysis | 284 posts over one year were collected to analyze content on patient’s post operative appetite and weight loss | Online group monitoring, and offering unsolicited advice to peers is highly sensitive but effective | Online MBS support groups | N/A | Discursive Psychology |
| Mixed methods (n = 1) | ||||||
| Atwood et al. (2018)35 | N/A; support group content analysis | 1412 messages in pre- (n = 822) and post-(n = 590) surgery sections of a forum were coded | Most messages provided: (a) procedure and nutrition factual information; (b) advice for coping with MBS preparation process, physical symptoms; and (c) encouragement regarding adherence to surgical guidelines, weight loss progress | Online MBS forum | N/A | Social Support Behavior CodeModeld |
aThere were no adolescent studies identified.
cWas a specific conceptual or theoretical model, framework and/or constructs mentioned in the review that mapped intervention strategies to outcomes.
dCutrona and Suhr.36
MBS: metabolic and bariatric surgery.
Table 2.
Summary of current analytical studies that include eHealth strategies among adultsa who are considering or who have completed metabolic and bariatric surgery by key outcome and other characteristics within the RE-AIM conceptual frameworkb.
|
Reach |
Efficacy/Effectiveness |
Adoption |
Implementation |
Maintenance |
Conceptual/theoretical frameworkd | |
|---|---|---|---|---|---|---|
| Authors (year) | Sample characteristics (age, ethnicity)c | Primary focus | Reported outcomes (primary and other) | eHealth mechanism | Primary outcome at≥6-month follow-up | |
| Observational/cross-sectional (n = 6) | ||||||
| Ristanto and Caltabiano (2019)37 | 88 patients (92% female, mean age 44 years) | Physical and mental health well being | Patients who attended ≥6 post op counseling sessions had greater physical well-being vs. those who attended <6 sessions | Web-based post-op support groups | N/A | No |
| Elvin-Walsh et al. (2018)38 | 50 dieticians; 49 patients | Attitudes, use of smartphone apps as a tool for maintaining connectivity between dietitians and patients post-op measured by survey; acceptability of eHealth strategies | Clinic practice setting is a barrier for some. Patients prefer email and text messaging follow-up. 68% of patients receptive to two-way communication with dietitians via app | Smartphone apps to decrease loss to follow-up | N/A | No |
| Graham et al. (2017)39 | 95 providers (46 nurses, 32 dietitians, 12 psychologists, one surgeon) | Allied health professionals’ perceptions of role of social media, mobile apps and patient-support technology in the UK; accuracy of information | Technologies (e.g. telehealth and videoconferencing) are not widely used in MBS in the UK | Social media, mobile apps and patient-support technology | N/A | No |
| Zhang et al. (2015)40 | 2408 patient site visits to date; demographics not specified | Access and usage of CBT online portal and program modules | Eight users participated in the pre-assessment questionnaire and attempted individual module use. Four individuals completed at least three modules available on the online portal | Online post-op CBT program and smartphone app | N/A | No |
| Peacock et al. (2016)41 | 440 patient pre-op; 330 post-op responses | Cross-sectional survey on perceived post-op nutritional barriers and helpful dietary services reported by MBS patients | Psychophysiological barriers were most commonly reported (86%); 62% reported receiving helpful services | Online obesity support website | N/A | No |
| Martins et al. (2015)42 | 103 patients (95% female, mean age 35.69 years) | Patterns of post-op internet use; influence of internet health information on post-op meeting/appointment attendance | 51.5% accessed the internet for MBS information every day. Facebook and search tools were the most used sites | Post-op web-based medical information and internet use | N/A | No |
| Retrospective/prospective cohort (n = 9) | ||||||
| Monfared et al. (2018)43 | 1230 patients (mean age 45.8 years) | Retrospective review of attrition to MBS rates among patients who self-selected online vs. in-person educational seminar | No differences in attrition rates by educational seminar delivery method. The online group was younger by average three years | Online pre-op educational seminar | N/A | No |
| Miletics et al. (2018)44 | 3484 patients (78% female; mean age 46.5 years) | Progression to MBS rates for live and online seminar; weight loss outcome comparisons at one year post-op | 2744 attended live seminar, 740 completed the online seminar; live seminar attendees more likely to progress to MBS; no weight loss differences between delivery methods | Online pre-op educational seminar | N/A | No |
| Bradley et al. (2017)45 | Not reported | Post-op weight regain in a newly developed, remote acceptance-based behavioral intervention | Supports feasibility, acceptability, preliminary efficacy of a remotely delivered post-op weight regain behavioral intervention | Online post-op behavioral intervention | N/A | No |
| Tenhagen et al. (2016)46 | 14 patients | Feasibility of obtaining frequent objective weight measurements using an internet-connected home weighing scale | 50% used weekly for one year; potential for timely interventions during follow-up in the case of insufficient weight loss or weight regain | Internet-connected weighing scale | One year follow up; no post-intervention follow-up | No |
| Taylor et al. (2016)47 | 255 patients (mean age 43 years) | Feasibility of tracking physical activity with smartphone app with minimal user interaction | Analyses show pre-MBS patients have an average of 16 min/day and post-MBS patients 21 min/day of exercise | Smartphone app | N/A | No |
| Mundi et al. (2015)48 | 20 patients (mean age 41 years) | Feasibility of using smartphone app with EMA/EMI functionality for MBS preparation | App was well-received based on subject satisfaction scores; positive behavior change and increased weight loss | Smartphone-based education modules | N/A | No |
| Wood et al. (2014)49 | 2608 patients (mean age 46 years ) | Weight loss after gastric bypass surgery tracked, used to develop online tool with age/sex specific weight loss trajectories | Patient-centered electronic tool will assist patients/providers in teaching, informed consent and post-op weight loss | Web-based tool provides weight loss expectations | N/A | No |
| Sudan et al. (2011)50 | 28 patients (older, males) | Exploration of teleconferencing for rural Veteran MBS patients | Cooperative network using teleconference and computerized records facilitated MBS with high patient satisfaction | Teleconferencing network | N/A | No |
| Morrow et al. (2011)51 | Seven patients (89% female, mean age 54 years) | Exploration of videoconferencing as vehicle for the delivery of support to patients residing in remote areas | Videolink session was acceptable and useful to both patients and clinicians and reported to be user-friendly | Videoconferencing for education delivery | N/A | No |
| Quasi-experimental, case–control (n = 5) | ||||||
| Wang et al. (2019)52 | 192 patients | Case–control study to examine rural vs. urban MBS patient use of telehealth | Telemedicine use was significantly higher among rural vs. urban MBS patients | Telehealth | N/A | No |
| Sherf-Dagan et al. (2018)53 | 128 patients (mean age 40 years) | Non-randomized trial to evaluate the effect of an online lecture on nutrition knowledge, weight loss expectations and anxiety among MBS candidates | Education by an online lecture prior to the MBS improved nutrition knowledge, but not anxiety | Online pre-op educational seminar delivery | N/A | No |
| Baillot et al. (2017)54 | 29 females | Feasibility and effect of pre-surgical exercise training delivered in-home via telehealth vs. usual care group | The telehealth group significantly increased their physical fitness compared with the usual care group | Telehealth | N/A | No |
| Vilallonga et al. (2013)55 | 33 patients | Controlled prospective trial of (1) patient WiFi weighing scale with instant WiFi data to the patient and surgeon vs. (2) standard follow-up group at the outpatient clinic | Excess weight loss similar in both groups. Treatment group considered it valuable in saving time. Standard follow-up in outpatient clinic setting with surgeon was preferred | Internet of things, scale internet connectivity | N/A | No |
| Eaton et al. (2012)56 | 338 patients (81% female, mean age 41 years) | Comparison of information retention after online vs. in-person delivery methods | Mean test scores were significantly higher in the on-line vs. the in-person group (86%, 80%, p = 0.003) | Web-delivery of info session | N/A | No |
| Randomized controlled trials (n = 5) | ||||||
| Mangieri et al. (2019)57 | 56 LSG patients | LSG patients randomized to a post-op mHealth program vs. standard care | mHealth patients lost significantly more weight vs. control at 12 and 24 months post-op | iPad© minis with MyFitnessPal© | Two year follow up; mHealthpatients > post-op weight loss | No |
| Versteegden et al. (2018)58 | 200 patients | Randomized to eHealth intervention, eHealth plus monitoring device, or standard care | Primary outcome is BMI loss over two years; secondary outcomes are quality of life, comorbidity resolution, return to work time | Online eHealth; wireless monitoring devices | Two year follow-up planned (trial in progress) | No |
| Conceicao et al. (2016)59 | 180 patients; ages 18–65 years | RCT in two hospital centers; control group (treatment as usual) and intervention group receiving the APOLO-Bari internet based support program plus treatment as usual | N/A; RCT in progress to test: (1) self-help manual; (2) direct contact with a trained psychologist; (3) weekly feedback monitoring and immediate feedback responses | Internet-based bariatric program (APOLO-Bari) | N/A (trial in progress) | No |
| Cassin et al. (2016)60 | 47 patients (mean age 46 years) | RCT of efficacy of pre-op phone-based cognitive behavioral therapy vs. standard pre-op care for improving eating psychopathology, psychosocial functioning | Tele-CBT group reported significant improvements in binge and emotional eating and overall health | Telephone delivery of pre-op cognitive behavioral therapy | Not reported; seven week post-measurement only | No |
| Wild et al. (2015)61 | 117 patients (mean age 41 years, 70% female) | RCT of efficacy of a videoconferencing-based psychoeducational group intervention in patients post-MBS | Did not show efficacy of group program for whole sample; results indicate that the intervention is effective for subgroup of patients with depression | Videoconference delivery of post-op psychoeducational intervention | One year follow up; treatment was effective for patients with depressive symptoms | No |
aThere were no adolescent studies identified.
cWith the exceptions of Wood et al. (2014), who reported 97% non-Hispanic White; 2% non-Hispanic Black, 1% other, and Cassin et al. (2016), who reported 92% non-Hispanic White; no other studies reported ethnicity distributions.
dWas a specific conceptual or theoretical model, framework and/or constructs mentioned in the review that mapped intervention strategies to outcomes.
LSG: laparoscopic sleeve gastrectomy; CBT: cognitive behavioral therapy; MSB: metabolic and bariatric surgery; EMA/EMI: ecological momentary assessment/ecological momentary intervention; RCT: randomized controlled trial; post-op: post operative; pre-op: pre-operative; BMI: body mass index.
A total of 38 studies were found that met the search criteria, from years 2011 to 2019. There were a total of 16 descriptive/partial analytical studies20–35 that included six reviews, nine qualitative and one mixed methods study (Table 1). There were a total of 22 analytical studies of which six were observational/cross-sectional, nine were prospective cohort designs, four were quasi-experimental and three were randomized controlled trials (Table 2). Overall, if reported (many studies did not report race/ethnic distribution of sample), study patient samples were composed of mainly adult non-Hispanic White females. No studies were found that either included or focused solely on adolescents (<18 years old). Two studies included the ethnic group distribution of the study sample. The majority of the qualitative studies included content or themes as the unit of analysis from sources such as internet blogs and Facebook posts. Only two studies included a theoretical/conceptual framework, Discursive Psychology34 and the Social Support Behavioral Code Model.35
Reviews
A total of six reviews were found in the literature search that discussed various eHealth strategies targeting MBS patients including telemedicine, web-based media, smartphone apps and wearables to track activity levels. In general, most reviews concluded that eHealth strategies can assist patients undergoing MBS in both pre- and post-operative acquisition of health information and knowledge as well as personal feedback to assist them with weight loss and improved lifestyle habits. One review24 of smartphone apps noted that less than half included allied health professional involvement in development, thus had the potential to include and capture inaccurate information. Thomas et al.,25 who assessed the accuracy of reporting via ecological momentary assessment (palmtop computer and accelerometer) concluded that eHealth strategies can potentially have an important role in the delivery of behavioral interventions and suggested that future studies should target MBS patients.
Qualitative studies
The majority of qualitative studies (including one mixed methods analysis) included online content, for example, Facebook MBS support groups, blog post comments, support groups and discussions, as well as MBS aftercare smartphone app acceptance. Most studies reported a general acceptance of eHealth mechanisms for information delivery and sharing. However, Koball et al. (2018)30 noted that over half of posts in a Facebook MBS support group contained inaccurate content, particularly in context to the American Society for Metabolic and Bariatric Surgery nutrition guidelines and expert registered dietitian nutritionist opinions. This prompted a letter to the editor27 that stated that healthcare professionals need to warn patients and teach them how to decipher credible versus false post-operative nutrition information available online. Several studies found that patients were open and forthcoming in sharing their personal experiences and feelings about MBS and post-operative challenges, and often offered peer-support.29,30,32,34,35 All studies were completed with adult samples, none reported ethnic group distribution and none used a conceptual framework to support the study design or outcomes.
Observational studies
Six reports of observational studies were included in the review, with a total sample size greater than 2700 patients or allied health professionals (dietitians, psychologists). eHealth implementation mechanisms included various web-based post-operative support groups, smartphone apps to decrease loss to follow-up, and social media. The majority of the studies primarily examined the use of eHealth tools after MBS to assist with physical and mental health well-being, and the utility of such tools in connecting allied health staff with patients in need of support. In general, studies reported that patients are amenable to eHealth strategies such as email and SMS,38 and many use the internet, and Facebook in particular, to seek out information about MBS. Interestingly, one study39 reported that eHealth strategies such as telehealth and teleconferencing are not widely utilized (adopted) in the UK with this patient population. No studies reported long-term (≥6 months post-study/intervention) follow-up on eHealth usage and outcomes. All studies were in adults, none reported the ethnic group distribution and none used a conceptual framework.
Retrospective/prospective cohort studies
The search revealed nine longitudinal cohort design studies with a total sample size greater than 8000 patients (ranging from seven to 3484 patients) and using a variety of eHealth mechanisms including online/teleconference delivery of pre-operative educational seminars43,44 and post-operative behavioral interventions,45 internet-connected weighing scales,46 smartphone-based education modules,48 web-based weight loss trajectory tools49 and tracking apps.47 Primary outcomes included pre-operative surgical attrition rates in online versus in-person educational seminar delivery,42,43 feasibility and acceptability of online delivery of behavioral/lifestyle interventions,44 education modules,47–49 physical activity tracking46 and weekly usage of an online-connected scale.46 In the two studies that explored patient self-selection of in-person versus online delivery of the mandatory pre-operative educational seminar, one study found no difference in progress to MBS by delivery type43 and the second found that in-person delivery patients were more likely to progress to MBS.44 All other studies reported general acceptance, feasibility and adoption of eHealth tools for MBS patients including rural Veterans50 and those living in remote or rural areas.51 No studies reported (1) maintenance or ≥6 months’ post-delivery outcomes. No studies reported the ethnic group distribution of their samples or applied a conceptual framework to the study design and outcomes.
Quasi-experimental design/case–control studies
A total of five quasi-experimental studies were found in the search. One compared rural versus urban telehealth use rates,52 while others compared eHealth versus standard of care/in-person delivery of nutrition education, weight loss expectations and anxiety management,53 exercise training,54 WiFi scale use55 and educational information.56 Four studies reported positive outcomes for eHealth delivery including improved basic knowledge of MBS55 and nutrition/dietary intake53 and fitness.54 One study reported higher use among rural versus urban MBS patients.52 Excess weight loss was similar in both the group using a WiFi weight scale and the standard outpatient clinic group. The treatment group commented on the benefit of saved (travel) time, but overall, patients preferred the outpatient setting.55 No studies reported long-term outcomes, included adolescent patients, ethnic group distribution or a conceptual framework.
Randomized controlled trials
A total of five randomized-controlled trials were captured in the review. Two are currently reported as in progress;58,59 the first is recruiting a total of 180 patients to receive either an internet/web-based post-MBS program including scheduled online interactive chat sessions with a psychologist, and weekly feedback and monitoring or standard of care.59 The second trial in progress is randomizing 200 MBS patients to one of three arms: an eHealth intervention, an eHealth intervention plus a monitoring device, or standard of care.58 The first completed trial of MBS patients undergoing laparoscopic sleeve gastrectomy procedures found that those randomized to an eHealth intervention that included iPad© minis with MyFitnessPal© installed had significantly more weight loss at 12 and 24 months post-MBS.57 A second completed pilot trial randomized patients to a telephone-delivered cognitive behavioral therapy intervention versus standard of care to assess improvement in pre-operative eating psychopathology and psychosocial functioning.60 The authors reported positive treatment effect outcomes (improving eating psychopathology and depression) at seven weeks post-baseline. A third completed trial assessed the efficacy of a videoconferencing-delivered psychoeducational post-MBS group intervention61 and reported positive outcomes (excess weight loss, health-related quality of life, self-efficacy) in the subgroup of patients with depressive symptoms, but not for the global sample. Cassin et al.60 did report that the majority of the sample was non-Hispanic White and female. None of the trials reported the use of a conceptual framework.
Discussion
Only one study57 reported that a mHealth intervention was effective in post-MBS weight loss maintenance versus standard of care. Most studies had design limitations (e.g. uncontrolled trials, low power). Published studies varied widely in terms of study design (qualitative to randomized controlled trials) and eHealth delivery method (telemedicine to blog post content) with a relatively consistent balance of pre- or post-operative MBS delivery. No studies included adolescents; only two included a conceptual framework to support study design and outcomes; and only two reported race/ethnicity composition of the study sample. Overall reported results were generally positive in terms of feasibility, acceptability and preliminary efficacy of eHealth delivery of pre- and post-operative MBS educational materials, knowledge exchange and social support. There was very little long-term (≥ 6 months) follow-up reported.
Obesity continues to be a major public health crisis in this country and severe obesity continues to increase most rapidly.62–64 Over the past 15 years, the number of Americans with a BMI of ≥40 kg/m2 increased by 50% and those with a BMI ≥50 kg/m2 increased by 75%, a rate two and three times faster, respectively, than the rest of the obese population.61 Similar trends are shown in adolescents; almost 10% of non-Hispanic Black and 7.6% of Hispanic American youth ages 2–19 years are affected by severe obesity, defined as ≥ 120% of the 95th percentile of BMI adjusted for age and sex.63 MBS continues to remain a common elective procedure in the USA with about a quarter of a million adults and adolescents undergoing the procedure annually.64 In parallel, the world is experiencing exponential technological growth with the youngest generations becoming increasingly comfortable with eHealth strategies and content as their initial resource to gather information on a variety of topics. Yet there is very limited rigorous research available that examines the use of eHealth strategies and delivery methods for both pre- and post-operative MBS education delivery, social support and weight loss resolution, as well as monitoring of dietary intake and physical activity, and among adolescents in particular. We found only two studies34,35 that reported a conceptual framework to support the study and intervention design and to map major constructs to patient outcomes. Below we summarize these findings by the RE-AIM constructs.
Reach
Across all articles contained in this review, there was reach to several thousand individual patients either in person or via online content posted in social media, support groups or chat rooms. In terms of the RE-AIM framework, most studies did not report inclusion/exclusion criteria, the percent of participants based on a valid denominator, and characteristics of participants versus non-participants. Ethnicity was rarely reported (in only two studies), challenging generalizability of findings. However, this may be one of the inherent challenges of online data capture; it is often collected anonymously so researchers can use only the content of the post or comment for analysis. Regardless, there is enormous potential via telehealth capabilities to reach MBS patients who need to travel several hours to see their surgeon or support team. In addition to increased reach via telehealth, extended ability to collect additional monitoring can be achieved by including some of the strategies highlighted in this review such as Wi-Fi-enabled weighing scales and exercise/physical activity trackers and monitors, as well as online dietary intake diaries.
Efficacy/Effectiveness
RE-AIM’s Efficacy/Effectiveness dimension focuses on (1) primary outcome with or without comparison with a public health goal; (2) broader outcomes (e.g. other outcomes, measure of quality of life or potential negative outcome) or use of multiple criteria; (3) robustness across subgroups (e.g. moderation analyses); (4) short-term attrition (%) and (5) differential rates by patient characteristics or treatment condition. All of these criteria were rarely reported in studies included in this review. This may be due to the facts that the majority of the studies included were not randomized controlled trials and the application of eHealth strategies with MBS patients is still an underdeveloped field. Some studies did report mental health or psychological outcomes beyond weight loss and cardiometabolic resolution. Many of the studies’ primary outcomes were more focused on feasibility and acceptance of eHealth strategies in general, which are critical dimensions to show proof of concept and lay the foundation for future, more rigorous interventions and study designs.
Adoption (setting and staff level)
In general, studies in this review did not report (1) setting or staff/allied health professional exclusions or participation refusal; (2) percent of settings/staff approached that participate (valid denominator); and (3) characteristics of settings and staff participating (both comparison and intervention) compared with either non-participants or some relevant resource data. Several studies did include allied health professionals’ opinions and patients’ opinions about motivation to access via eHealth mechanisms. However, no studies examined clinic or patient home setting facilitators and/or barriers to both short- and long-term adoption, which is critical in the post-operative phase in particular when patients need the most support for consistent weight loss.
Implementation
The RE-AIM framework’s Implementation outcomes focus on (1) percent of perfect delivery or calls completed, et cetera (e.g. adherence or consistency); (2) adaptations made to intervention during study; (3) cost of intervention (time or money); and (4) consistency of implementation across staff/time/settings/subgroups (looking for consistent process, distinct from outcome comparison). Little reporting of these outcomes was found in this review. However, as stated previously this may be due to lack of maturity in this field as applied to this patient population in general. Certainly, details of eHealth strategy adaptations for MBS patients would be informative due to the varying levels, or need of weight loss and comorbidity resolution support. Virtually nothing is known about how eHealth strategies can be effectively implemented among adolescents considering MBS, or who have already completed the procedure, yet, for most, technology is intricately woven into their daily lives. Another critical gap in the literature is the finding that virtually nothing is known about culturally-competent eHealth strategies targeting ethnic minority patients, and how the acceptance of delivery of eHealth strategies varies by various racial or ethnic subgroups. Furthermore, very little information is available on how various sociodemographic groups access, utilize and interact with technology and their general comfort level with various eHealth strategies. This is essential information to inform the development of effective interventions that could be driven by robust qualitative methodologies.
Maintenance (individual and setting level)
Finally, the RE-AIM framework’s Maintenance dimension measures the following outcomes for both individual and setting level outcomes: (1) measure of primary outcome (with or without comparison with a public health goal) at ≥ 6 months’ follow-up after final intervention contact; (2) measure of broader outcomes or use of multiple criteria at follow-up (e.g. measure of quality of life or potential negative outcome) at follow-up; (3) robustness data – subgroup effects over the long term; (4) measure of long-term attrition (%) and differential rates by patient characteristics or treatment condition. This review had no studies that reported outcomes greater than six months after the intervention study was completed, leaving another critical gap in the field in terms of sustainability and scalability of eHealth strategies targeting MBS patients, as well as the institution/systems where they receive their clinical care.
All five RE-AIM dimensions necessitate qualitative research methods to explore deeper the specific barriers and facilitators to primary and secondary outcomes. These include: (1) acceptability (the perception among implementation stakeholders that a given treatment, service, practice or innovation is agreeable, palatable or satisfactory); (2) appropriateness (the perceived fit, relevance or compatibility of the innovation/evidence based practice for a given practice setting, provider, or consumer; and/or perceived fit of the innovation to address a particular issue or problem); and (3) feasibility (the extent to which a new treatment, or an innovation, can be successfully used or carried out within a given agency or setting). Thus, a mixed-methods research design and approach would be logical as the field develops and includes more diverse MBS patients in terms of race, ethnicity, age, sex and geographic residency. It is not until the patients themselves tell us what they feel is appropriate, acceptable, relevant and compatible with their lifestyle in terms of eHealth dissemination and implementation strategies that we can expect uptake of and engagement with eHealth interventions, leading to improved and sustained health outcomes.
Summary and conclusions
Very few studies to date have specifically reported outcomes or effect sizes for the combination of replicable eHealth interventions targeting MBS patients both pre- and post-operatively despite the significant increase in adult and adolescent severe obesity. As such, there is an opportunity to perform more rigorous studies that employ robust conceptual frameworks so that dissemination and implementation efforts can be mapped to construct-driven outcomes. There is additional opportunity to develop engaging and effective eHealth strategies and products targeting both adult and adolescent MBS patients. None of the studies included a conceptual framework with key, testable constructs to support the combination of eHealth and MBS interventions. Both approaches need to take into account key constructs from the socioecological framework including not only intra/interpersonal and developmental factors, but also those of the system or setting that provides the eHealth strategy.
Supplemental Material
Supplemental material, DHJ898987 Supplemental Material1 for Application and effectiveness of eHealth strategies for metabolic and bariatric surgery patients: A systematic review by Sarah E Messiah, Paul M Sacher, Joshua Yudkin, Ashley Ofori, Faisal G Qureshi, Benjamin Schneider, Deanna M Hoelscher, Nestor de la Cruz-Muñoz and Sarah E Barlow in Digital Health
Supplemental material, DHJ898987 Supplemental Material2 for Application and effectiveness of eHealth strategies for metabolic and bariatric surgery patients: A systematic review by Sarah E Messiah, Paul M Sacher, Joshua Yudkin, Ashley Ofori, Faisal G Qureshi, Benjamin Schneider, Deanna M Hoelscher, Nestor de la Cruz-Muñoz and Sarah E Barlow in Digital Health
Conflict of interest
The authors have no conflicts of interest to declare.
Contributorship
SM and PS conceived the study. JY and AO researched literature with guidance from SM. SM wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Ethical approval
Not applicable; no human subjects involvement.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health, National Institute on Minority Health and Health Disparities (grant #R01MD011686).
Guarantor
SM.
Peer review
Dr. Emily E Johnson, Med Univ S Carolina and Dr. Carrie S Sheets, InSight Counseling LLC have reviewed the manuscript.
ORCID iD
Sarah E Messiah https://orcid.org/0000-0001-6685-2175
Supplemental material
Supplementary material for this article is available online.
References
- 1.Finkelstein EA, Khavjou OA, Thompson Het al. Obesity and severe obesity forecasts through 2030. Am J Prev Med 2012; 42: 563–570. [DOI] [PubMed] [Google Scholar]
- 2.NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017; 390: 2627–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Welbourn R, Dixon J, Barth JHet al. NICE-accredited commissioning guidance for weight assessment and management clinics: A model for a specialist multidisciplinary team approach for people with severe obesity. Obes Surg 2016; 26: 649–659. [DOI] [PubMed] [Google Scholar]
- 4.Dixon JB, Zimmet P, Alberti KG. Bariatric surgery: An IDF statement for obese Type 2 diabetes. Diabet Med 2011; 28: 628–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ju T, Rivas L, Arnott Set al. Barriers to bariatric surgery: Factors influencing progression to bariatric surgery in a U.S. metropolitan area. Surg Obes Relat Dis Epub ahead of print 6 December 2018. DOI: 10.1016/j.soard.2018.12.004. [DOI] [PubMed]
- 6.Hutchesson MJ, Rollo ME, Krukowski Ret al. eHealth interventions for the prevention and treatment of overweight and obesity in adults: A systematic review with meta-analysis. Obes Rev 2015; 16: 376–392. [DOI] [PubMed] [Google Scholar]
- 7.Arem H, Irwin M. A review of web-based weight loss interventions in adults. Obes Rev 2011; 12: e236–e243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryan K, Dockray S, Linehan C. A systematic review of tailored eHealth interventions for weight loss. Digit Health 2019; 5: 1--23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Willmott TJ, Pang B, Rundle-Thiele Set al. Weight management in young adults: Systematic review of electronic health intervention components and outcomes. J Med Internet Res 2019; 21: e10265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hammersley ML, Jones RA, Okely AD. Parent-focused childhood and adolescent overweight and obesity eHealth interventions: A systematic review and meta-analysis. J Med Internet Res 2016; 18: e203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greenwood DA, Gee PM, Fatkin KJet al. A systematic review of reviews evaluating technology- enabled diabetes self-management education and support. J Diabetes Sci Technol 2017; 11: 1015–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Joiner KL, Nam S, Whitemore R. Lifestyle interventions based on the diabetes prevention program delivered via eHealth: A systematic review and meta-analysis. Prev Med 2017; 100: 194–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Das A, Faxvaag A, Svanaes D. The impact of an eHealth portal on health care professionals’ interaction with patients: Qualitative study. J Med Internet Res 2015; 17: e267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaglio B, Shoup JA, Glasgow RE. The RE-AIM framework: A systematic review of use over time. Am J Public Health 2013; 103: e38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. Am J Public Health 1999; 89: 1322–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jilcott S, Ammerman A, Sommers Jet al. Applying the RE-AIM framework to assess the public health impact of policy change. Ann Behav Med 2007; 34: 105–114. [DOI] [PubMed] [Google Scholar]
- 17.Glasgow RE, Dickinson P, Fisher Let al. Use of RE-AIM to develop a multi-media facilitation tool for the patient-centered medical home. Implement Sci 2011; 6: 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glasgow RE, Askew S, Purcell Pet al. Use of RE-AIM to address health inequities: Application in a low-income community health center based weight loss and hypertension self-management program. Transl Behav Med 2013; 3: 200–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Cancer Institute. Measuring the use of the RE-AIM model dimensions items checklist, https://cancercontrol.cancer.gov/IS/ (2019, accessed 18 March 2019).
- 20.Coldebella B, Armfield NR, Bambling Met al. The use of telemedicine for delivering healthcare to bariatric surgery patients: A literature review. J Telemed Telecare 2018; 24: 651–660. [DOI] [PubMed] [Google Scholar]
- 21.Groller KD. Systematic review of patient education practices in weight loss surgery. Surg Obes Relat Dis 2017; 13: 1072–1085. [DOI] [PubMed] [Google Scholar]
- 22.Zhang MW, Ho RC, Hawa Ret al. Analysis of the information quality of bariatric surgery smartphone applications using the Silberg scale. Obes Surg 2016; 26: 163–168. [DOI] [PubMed] [Google Scholar]
- 23.Bond DS, Thomas JG. Measurement and intervention on physical activity and sedentary behaviours in bariatric surgery patients: Emphasis on mobile technology. Eur Eat Disord Rev 2015; 23: 470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stevens DJ, Jackson JA, Howes N, Morgan J. Obesity surgery smartphone apps: A review. Obes Surg 2014; 24: 32–36. [DOI] [PubMed] [Google Scholar]
- 25.Thomas JG, Bond DS, Sarwer DBet al. Technology for behavioral assessment and intervention in bariatric surgery. Surg Obes Relat Dis 2011; 7: 548–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koball AM, Jester DJ, Pruitt MAet al. Content and accuracy of nutrition-related posts in bariatric surgery Facebook support groups. Surg Obes Relat Dis 2018; 14: 1897–1902. [DOI] [PubMed] [Google Scholar]
- 27.Groller KD. Comment on: Content and accuracy of nutrition-related posts in bariatric surgery Facebook support groups. Surg Obes Relat Dis Epub ahead of print 9 November 2018. DOI: 10.1016/j.soard.2018.10.031. [DOI] [PubMed]
- 28.Meleo-Erwin ZC. ‘No one is as invested in your continued good health as you should be:’ An exploration of the post-surgical relationships between weight-loss surgery patients and their home bariatric clinics. Sociol Health Illn 2019; 41: 285–302. [DOI] [PubMed] [Google Scholar]
- 29.Willmer M, Salzmann-Erikson M. ‘The only chance of a normal weight life’: A qualitative analysis of online forum discussions about bariatric surgery. PLoS One 2018; 13: e0206066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koball AM, Jester DJ, Domoff SEet al. Examination of bariatric surgery Facebook support groups: A content analysis. Surg Obes Relat Dis 2017; 13: 1369–1375. [DOI] [PubMed] [Google Scholar]
- 31.Zhang MW, Ho RC, Hawa Ret al. Analysis of the information quality of bariatric surgery smartphone applications using the Silberg scale. Obes Surg 2016; 26: 163–168. [DOI] [PubMed] [Google Scholar]
- 32.Das A, Faxvaag A. What influences patient participation in an online forum for weight loss surgery? A qualitative case study. Interact J Med Res 2014; 3: e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Connor K, Brady RR, Tulloh Bet al. Smartphone applications (apps) for bariatric surgery. Obes Surg 2013; 23: 1669–1672. [DOI] [PubMed] [Google Scholar]
- 34.Cranwell J, Seymour-Smith S. Monitoring and normalising a lack of appetite and weight loss. A discursive analysis of an online support group for bariatric surgery. Appetite 2012; 58: 873–881. [DOI] [PubMed] [Google Scholar]
- 35.Atwood ME, Friedman A, Meisner BAet al. The exchange of social support on online bariatric surgery discussion forums: A mixed-methods content analysis. Health Commun 2018; 33: 628–635. [DOI] [PubMed] [Google Scholar]
- 36.Cutrona CE, Suhr JA. Controllability of stressful events and satisfaction with spouse support behaviors. Commun Res 1992; 19: 154–174. [Google Scholar]
- 37.Ristanto A, Caltabiano ML. Psychological support and well-being in post-bariatric surgery patients. Obes Surg 2019; 29: 739–743. [DOI] [PubMed] [Google Scholar]
- 38.Elvin-Walsh L, Ferguson M, Collins PF. Nutritional monitoring of patients post-bariatric surgery: Implications for smartphone applications. J Hum Nutr Diet 2018; 31: 141–148. [DOI] [PubMed] [Google Scholar]
- 39.Graham YNH, Hayes C, Mahawar KKet al. Ascertaining the place of social media and technology for bariatric patient support: What do allied health practitioners think? Obes Surg 2017; 27: 1691–1696. [DOI] [PubMed] [Google Scholar]
- 40.Zhang MW, Ho RC, Cassin SEet al. Online and smartphone based cognitive behavioral therapy for bariatric surgery patients: Initial pilot study. Technol Health Care 2015; 23: 737–744. [DOI] [PubMed] [Google Scholar]
- 41.Peacock JC, Schmidt CE, Barry K. A qualitative analysis of post-operative nutritional barriers and useful dietary services reported by bariatric surgical patients. Obes Surg 2016; 26: 2331–2339. [DOI] [PubMed] [Google Scholar]
- 42.Martins MP, Abreu-Rodrigues M, Souza JR. The use of the internet by the patient after bariatric surgery: Contributions and obstacles for the follow-up of multidisciplinary monitoring. Arq Bras Cir Dig 2015; 28: 46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Monfared S, Martin A, Gupta Ket al. Web-based educational seminars compare favorably with in-house seminars for bariatric surgery patients. Obes Surg. Epub ahead of print 7 November 2018. DOI: 10.1007/s11695-018-3590-4. [DOI] [PubMed]
- 44.Miletics M, Claros L, Stoltzfus Jet al. Progression to surgery: Online versus live seminar. Surg Obes Relat Dis 2018; 14: 382–385. [DOI] [PubMed] [Google Scholar]
- 45.Bradley LE, Forman EM, Kerrigan SGet al. Project HELP: A remotely delivered behavioral intervention for weight regain after bariatric surgery. Obes Surg 2017; 27: 586–598. [DOI] [PubMed] [Google Scholar]
- 46.Tenhagen M, van Ramshorst GH, Demirkiran Aet al. Perioperative online weight monitoring in bariatric surgery with a digital internet-connected scale. Obes Surg 2016; 26: 1120–1126. [DOI] [PubMed] [Google Scholar]
- 47.Taylor D, Murphy J, Ahmad Met al. Quantified-self for obesity: Physical activity behaviour sensing to improve health outcomes. Stud Health Technol Inform 2016; 220: 414–416. [PubMed] [Google Scholar]
- 48.Mundi MS, Lorentz PA, Grothe Ket al. Feasibility of smartphone-based education modules and ecological momenta assessment/intervention in pre-bariatric surgery patients. Obes Surg 2015; 25: 1875–1881. [DOI] [PubMed] [Google Scholar]
- 49.Wood GC, Benotti P, Gerhard GSet al. A patient-centered electronic tool for weight loss outcomes after Roux-en-Y gastric bypass. J Obes 2014; 2014: 364941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sudan R, Salter M, Lynch Tet al. Bariatric surgery using a network and teleconferencing to serve remote patients in the Veterans Administration Health Care System: feasibility and results. Am J Surg 2011; 202: 71–76. [DOI] [PubMed] [Google Scholar]
- 51.Morrow E, Bruce DM, Bruce Eet al. Post surgical review of bariatric surgery patients: A feasibility study of multidisciplinary follow up using videoconferencing. Clin Pract Epidemiol Ment Health 2011; 7: 84–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang CD, Rajaratnam T, Stall Bet al. Exploring the effects of telemedicine on bariatric surgery follow-up: A matched case control study. Obes Surg 2019; 29: 2704–2706. [DOI] [PubMed] [Google Scholar]
- 53.Sherf-Dagan S, Hod K, Mardy-Tilbor Let al. The effect of pre-surgery information online lecture on nutrition knowledge and anxiety among bariatric surgery candidates. Obes Surg 2018; 28: 1876–1885. [DOI] [PubMed] [Google Scholar]
- 54.Baillot A, Boissy P, Tousignant Met al. Feasibility and effect of in-home physical exercise training delivered via telehealth before bariatric surgery. J Telemed Telecare 2017; 23: 529–535. [DOI] [PubMed] [Google Scholar]
- 55.Vilallonga R, Lecube A, Fort JMet al. Internet of things and bariatric surgery follow-up: Comparative study of standard and IoT follow-up. Minim Invasive Ther Allied Technol 2013; 22: 304–311. [DOI] [PubMed] [Google Scholar]
- 56.Eaton L, Walsh C, Magnuson Tet al. On-line bariatric surgery information session as effective as in-person information session. Surg Obes Relat Dis 2012; 8: 225–229. [DOI] [PubMed] [Google Scholar]
- 57.Mangieri CW, Johnson RJ, Sweeney LBet al. Mobile health applications enhance weight loss efficacy following bariatric surgery. Obes Res Clin Pract 2019; 13: 176–179. [DOI] [PubMed] [Google Scholar]
- 58.Versteegden DPA, van Himbeeck MJJ, Nienhuijs SW. Assessing the value of eHealth for bariatric surgery (BePatient trial): Study protocol for a randomized controlled trial. Trials 2018; 19: 625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Conceicao EM, Machado PP, Vaz ARet al. APOLO-Bari, an internet-based program for longitudinal support of bariatric surgery patients: Study protocol for a randomized controlled trial. Trials 2016; 17: 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cassin SE, Sockalingam S, Du Cet al. A pilot randomized controlled trial of telephone-based cognitive behavioural therapy for preoperative bariatric surgery patients. Behav Res Ther 2016; 80: 17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wild B, Hunnemeyer K, Sauer Het al. A 1-year videoconferencing-based psychoeducational group intervention following bariatric surgery: Results of a randomized controlled study. Surg Obes Relat Dis 2015; 11: 1349–1360. [DOI] [PubMed] [Google Scholar]
- 62.Flegal KM, Kruszon-Moran D, Carroll MDet al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016; 315: 2284–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hales CM, Fryar CD, Carroll MDet al. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA 2018; 319: 1723–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Aminian A, Daigle CR, Brethauer SAet al. Citation classics: Top 50 cited articles in bariatric and metabolic surgery. Surg Obes Relat Dis 2014; 10: 898–905. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DHJ898987 Supplemental Material1 for Application and effectiveness of eHealth strategies for metabolic and bariatric surgery patients: A systematic review by Sarah E Messiah, Paul M Sacher, Joshua Yudkin, Ashley Ofori, Faisal G Qureshi, Benjamin Schneider, Deanna M Hoelscher, Nestor de la Cruz-Muñoz and Sarah E Barlow in Digital Health
Supplemental material, DHJ898987 Supplemental Material2 for Application and effectiveness of eHealth strategies for metabolic and bariatric surgery patients: A systematic review by Sarah E Messiah, Paul M Sacher, Joshua Yudkin, Ashley Ofori, Faisal G Qureshi, Benjamin Schneider, Deanna M Hoelscher, Nestor de la Cruz-Muñoz and Sarah E Barlow in Digital Health