Abstract
Objective
Hip fracture surgery in geriatric patients on anticoagulants may increase the risk for blood loss. Anticoagulation reversal may lower these risks; however, data on blood loss and transfusions are limited. The study purpose was to compare outcomes between hip fracture patients 1) not on anticoagulants 2) whose anticoagulants were reversed, and 3) whose anticoagulants were not reversed.
Methods
This four-year retrospective cohort study at six Level 1 Trauma Centers enrolled geriatric patients (≥65) with isolated hip fractures. The primary outcome was total hospital blood loss (ml). Secondary outcomes: hospital length of stay (HLOS) and volume of packed red blood cells (pRBC) transfusions (ml). Statistical analyses included: Fisher’s, chi-squared, Kruskal-Wallis, linear mixed-effect and logistic regression. Bonferroni adjusted alpha = 0.025.
Results
Of the 459 patients, 189 (41%) were not on anticoagulants, 186 (41%) were reversed, and 84 (18%) were not reversed. The LS mean (SE) blood loss was 134 ml (12) for not reversed patients and 159 (17) for reversed patients; no significant difference compared to those not on anticoagulants [138 (12)], p-diff = 0.14 and 0.83, respectively. The LS mean (SE) HLOS was significantly longer for the reversed patients, 7.7 (0.4) days, when compared to those not on anticoagulants, 6.8 (0.4), p = 0.02, and when compared to those not reversed, 6.3 (0.6), p = 0.01. There was no significant difference in pRBC transfusions.
Conclusion
Not reversing anticoagulants for geriatric hip fractures was not associated with increased volume of blood loss or transfusions when compared to those reversed. Delayed surgery for anticoagulant reversal may be unnecessary and contributing to an increased HLOS.
Keywords: Geriatric, Hip fractures, Anticoagulation, Reversal
Abrreviations: DOACs, direct oral anticoagulants; FDA, U.S. Food and Drug Administration; FFP, fresh frozen plasma; PCC, prothrombin complex concentrates; aPCC, activated PCC; ION, Injury Outcomes Network; INR, international normalized ratio
1. Introduction
Approximately 300,000 geriatric people (aged ≥ 65) are hospitalized for hip fractures each year in the United States.1 Fragility hip fractures have an associated one-year mortality rate of 6–30%.2, 3, 4 Many geriatric patients take anticoagulants, requiring reversal in four to six percent of patients often for an urgent invasive procedure, surgery for patients on pre-injury anticoagulants may increase the risk for blood loss and blood transfusions.5, 6, 7, 8, 9, 10, 11, 12 However, anticoagulation reversal may increase the time to surgery. Surgery within 24 h of admission has been associated with reduced morbidity, hospital length of stay (HLOS), and complication rates.14,15 Delaying surgery for more than 24 h has shown to increase the time in rehabilitation, pressure sores, urinary infection, pneumonia, and thromboembolic complications.13,16 The urgency for surgery pressures surgeons to act quickly, determine the patient’s current medications, treatment course, coagulation status, and the best method for anticoagulant reversal.17
Reversal agents can counter anticoagulants faster and prevent surgical delays.16 Vitamin K is used to reverse warfarin, but can cause warfarin resistance.16 A drawback to direct oral anticoagulants (DOACs) is the lack of FDA-approved and available reversal agents.10,18 Still, DOACs (dabigatran, rivaroxaban, apixaban, and edoxaban) are preferred to warfarin because they have fewer interactions, a wider therapeutic window, no need for monitoring, and a lower risk for bleeding.8, 9, 10, 11 “Non-specific” reversal agents: fresh frozen plasma (FFP), prothrombin complex concentrates (PCC), activated PCC (aPCC) and recombinant activated factor VIIa have been used to reverse DOACs or accelerate warfarin reversal.9,10,16 Another option is to “wait and watch” for the anticoagulation effect to dissipate naturally.5,12,19 However, there is no evidence demonstrating that reversal reduces mortality.20
Data on blood loss and transfusions for patients whose anticoagulant was not reversed is limited. The purpose of this study was to compare outcomes among 1) “patients not on anticoagulants” 2) patients whose pre-injury anticoagulants were “reversed”, and 3) patients whose pre-injury anticoagulants were “not reversed”.
2. Methods
This multicenter retrospective observational study was approved by the institutional review boards at all six participating Level 1 Trauma Centers with a waiver of informed consent. The study included geriatric patients (≥65) with an isolated fragility hip fracture requiring surgery from January 2014–January 2018. Poly-trauma patients were excluded, defined as an Abbreviated Injury Scale of ≥2 in any other anatomical body region. ICD 9 and 10 codes for hip fractures were used to identify patients from trauma registries.
It was estimated that at least 195 patients would adequately power this study for comparing blood loss using an ANOVA at a significance level of 0.025; however, to account for potential confounders a sample size of 606, or 202 per study arm, was approved.22,23 All patients identified were screened and categorized into one study arm: 1) “not on anticoagulants”, 2) “reversed”, and 3) “not reversed”. Patients were enrolled in reverse chronological order until the enrollment goal of 202 per group was met. If the following reversal therapies were utilized prior to surgery for patients taking pre-injury anticoagulants, the patient was considered reversed: vitamin K, factor VIIa, PCC, aPCC, FFP, Idarucizumab, and wait and watch. Patients who went to surgery >24 h after the last dose of anticoagulation medication was taken were reversed using the wait and watch method. This cut-off was calculated using anticoagulant half-lives to determine when serum levels are reduced by 94–97%.21 If the timing of the last dose was not recorded, it was estimated using the pharmacological dosing regimen. Patients were considered reversed using the wait and watch method regardless of the reason for surgical delay.
The primary aim was to evaluate the efficacy of not reversing anticoagulants prior to hip fracture surgery on outcomes. The primary outcome was the total volume of blood loss during hospitalization. All instances of blood loss recorded in the electronic medical record were included in the total volume of blood loss. Secondary outcomes included: total volume of packed red blood cells (pRBC), cryoprecipitate, FFP, and platelets transfused, thromboembolic complications, HLOS, intensive care unit (ICU) LOS, readmission, and wound hematomas. All blood loss and transfusions were reported in milliliters (ml).
Categorical and dichotomous data were expressed as proportions (counts) and compared using Fisher’s exact or chi-squared, when appropriate. Continuous data were expressed as means (standard deviation, SD) or medians (interquartile range, IQR) and compared using Kruskal-Wallis or ANOVA, when appropriate. Linear mixed-effect and multivariable logistic regression were used to determine if the study arms were independently associated with outcome variables for outcomes with sufficient numbers to adjust. Bonferroni adjusted alpha = 0.025. All hypothesis tests were two-tailed.
3. Results
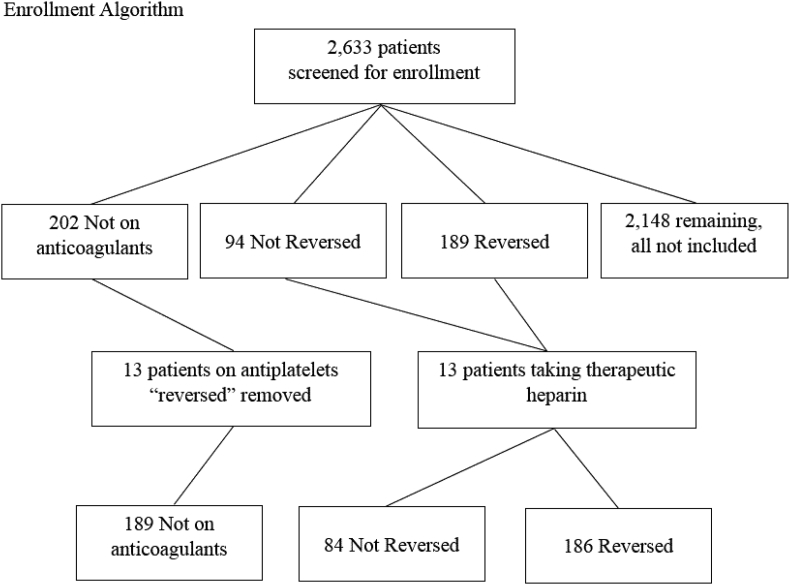
There were 2633 patients screened, all patients who were reversed or not reversed were included in the study and 202 patients not on anticoagulants were included in reverse chronological order. All other patients screened were not on anticoagulants and were not included in the study as the enrollment goal was met. Of the patients not on anticoagulants, 13 who were taking pre-injury anti-platelets but treated as they were on anticoagulants were excluded. An additional 13 patients were excluded who were taking pre-injury therapeutic doses of heparin or enoxaparin. Therefore, 459 patients were included in the final population: 189 (41%) were not on anticoagulants, 186 (41%) underwent anticoagulant reversal, and 84 (18%) were not reversed. See Fig. 1.
Fig: 1.
Enrollment algorithm.
The median [IQR] age was 83 [77–88] years old and 66% of patients were female; age and sex were not statistically different between study arms (Table 1). There were fewer patients not on anticoagulants who walked with an assistive device (27%) than and reversed patients (41%), p = 0.01. Patients not on anticoagulants were taking a median [IQR] of 5 [2, 8] medications, whereas those not reversed were taking 6 [4, 9] and those reversed were taking 7 [5, 10]. There were a higher proportion of reversed patients (23%) who had congestive heart failure (CHF) than patients not on anticoagulants (8%), p < 0.001. Other comorbidities were comparable across study arms.
Table 1.
Patient demographic and clinical characteristics.
| Not on Anticoagulants n = 189 | Not Reversed n = 84 | Reversed n = 186 | p | |
|---|---|---|---|---|
| Age Median (IQR) | 82 (76, 88) | 83.5 (75.5, 88) | 83.5 (78, 88) | 0.39 |
| Sex % Female (n) | 68% (128) | 71% (60) | 62% (116) | 0.29 |
| Pre-ambulatory Status | ||||
| Walks without an assistive device | 68% (128) | 62% (50) | 55% (100) | 0.01a |
| Walks with an assistive device | 27% (50) | 38% (31) | 41% (75) | |
| Cannot walk | 5% (9) | 0 | 3% (6) | |
| Prior Hip Fracture | 9% (16) | 8% (7) | 11% (21) | 0.54 |
| Pre-injury Medications | ||||
| Cholinesterase Inhibitors | 12% (22) | 12% (10) | 10% (19) | 0.88 |
| Analgesic | 15% (28) | 26% (22) | 26% (48) | 0.02b |
| Narcotic | 15% (29) | 31% (26) | 27% (51) | 0.004c |
| Anti-arrhythmia | 1% (2) | 29% (24) | 30% (56) | <0.001d |
| Beta Blocker | 15% (29) | 35% (33) | 28% (54) | <0.001e |
| Calcium Channel Blockers | 22% (42) | 24% (20) | 24% (44) | 0.93 |
| Vitamin D | 21% (40) | 17% (14) | 26% (48) | 0.22 |
| Iron | 6% (11) | 8% (7) | 9% (16) | 0.55 |
| Potassium | 11% (20) | 18% (15) | 19% (36) | 0.05 |
| Statin | 32% (61) | 36% (30) | 50% (93) | 0.001f |
| Medication Count Median (IQR) | 5 (2, 8) | 6 (4, 9) | 7 (5, 10) | <0.001g |
| Comorbidities | ||||
| Diabetes Mellitus | 18% (34) | 14% (12) | 25% (46) | 0.09 |
| Hypertension | 63% (119) | 62% (52) | 65% (120) | 0.91 |
| Congestive Heart Failure | 8% (16) | 14% (12) | 23% (42) | <0.001h |
| Dementia | 24% (46) | 14% (12) | 18% (34) | 0.12 |
| COPD | 15% (29) | 10% (8) | 15% (28) | 0.40 |
| Smoker | 8% (16) | 6% (5) | 6% (11) | 0.58 |
| Cerebrovascular Accident | 5% (10) | 8% (7) | 11% (21) | 0.11 |
| Anemia | 0 | 1% (1) | 1% (1) | 0.18 |
| Cancer | 1% (2) | 0 | 2% (4) | 0.50 |
| Admission Vital Signs | ||||
| SBP Median (IQR) | 144 (129, 166) | 148.5 (129, 168.5) | 144 (127, 161) | 0.53 |
| DBP Median (IQR) | 75 (67, 86) | 81 (70, 94) | 77 (67.5, 89) | 0.41 |
| RR Median (IQR) | 18 (16, 18.5) | 16 (16, 18) | 18 (16, 18) | 0.58 |
| HR Median (IQR) | 79 (70, 90) | 76 (68, 87.5) | 80 (70, 89.5) | 0.33 |
| O2 Median (IQR) | 95 (93, 98) | 94.5 (92, 97) | 96 (94, 97) | 0.21 |
Bonferroni-adjusted p = 0.025, N/A = not applicable, no values collected for this patient group; therefore, p-value not calculated. a = A higher proportion of reversed patients walked with an assistive device than those not on anticoagulants, no significant difference between those not on anticoagulants and those reversed, p = 0.04, or those not reversed and reversed, p = 0.23. b = A higher proportion of patients on anticoagulants than those not on anticoagulants were taking pre-injury analgesics, no significant difference between those not reversed and reversed, p = 0.95. c = A higher proportion of patients on anticoagulants than patients not on anticoagulants were taking narcotics, no significant difference between those reversed and not reversed, p = 0.55. d = A higher proportion of patients on anticoagulants than patients not on anticoagulants were taking anti-arrhythmia medication, no significant difference between those not reversed and reversed, p = 0.80. e = A higher proportion of reversed patients were than those not on anticoagulants were taking pre-injury beta-blockers, no significant difference between those not on anticoagulants and those not reversed, p = 0.36, or those reversed and not reversed, p = 0.08. f = A higher proportion of reversed patients were taking pre-injury statins than those not on anticoagulants, no significant difference between those not on anticoagulants and those not reversed, p = 0.58, or those reversed and not reversed, p = 0.03. g = Patients on anticoagulants had a higher medication count than those not on anticoagulants, no significant difference between those reversed and not reversed, p = 0.17. h = A higher proportion of reversed patients were than those not on anticoagulants had congestive heart failure, no significant difference between those not on anticoagulants and those not reversed, p = 0.14, or between those not reversed and reversed, p = 0.11.
Pre-injury anticoagulants were DOACs (34%) and warfarin (66%) (Table 2). There were more patients on warfarin in the reversed arm (73%) than in the not reversed arm (52%), and less patients in the reversed arm (27%) who were taking DOACs than in the not reversed arm (48%), p < 0.001. Indications for anticoagulant use were similar among groups. There were more patients in the reversed arm (45%) who received an anticoagulant bridge than in the not reversed arm (18%), p < 0.001. Anticoagulation reversal methods were vitamin K (42%), FFP (22%), factor VIIa (1%), and “wait and watch” (46%) (Table 3). Patients could have had multiple reversal methods. Thirty-eight percent of reversed patients had surgery delayed due to a concern for the anticoagulant effect. Other reasons for surgical delay included family reasons (2%) and medical clearance (17%).
Table 2.
Anticoagulant information.
| Not Reversed n = 84 | Reversed n = 186 | p | |
|---|---|---|---|
| Anticoagulation Medication | |||
| Edoxaban | 0 | 1% (1) | 0.002 |
| Apixaban | 15% (13) | 11% (20) | |
| Dabigatran | 1% (1) | 3% (6) | |
| Warfarin | 52% (44) | 73% (135) | |
| Rivaroxaban | 31% (26) | 13% (24) | |
| Anticoagulation Medication Type | |||
| Warfarin | 52% (44) | 73% (135) | 0.001 |
| DOAC | 48% (40) | 27% (51) | |
| Indication for Anticoagulation1 | |||
| A-fib | 64% (54) | 70% (131) | 0.31 |
| DVT or PE | 12% (10) | 15% (27) | 0.56 |
| Mechanical Valve Replacement | 5% (4) | 4% (8) | >0.99 |
| Stroke or CVA | 10% (8) | 5% (10) | 0.21 |
| CAD | 8% (7) | 9% (16) | 0.94 |
| Other | 1% (1) | 3% (5) | 0.44 |
| Bridge Given % Yes (n) | 17% (14) | 48% (90) | <0.001 |
| Anticoagulant Bridge Medication | |||
| Heparin | 1% (1) | 4% (7) | 0.44 |
| Enoxaparin | 15% (13) | 45% (83) | <0.001 |
| Total Bridge Dose (ml) | |||
| Heparin Median (IQR) | 50002 | 5000 (2500, 13500) | N/A |
| Enoxaparin Median (IQR) | 120 (60, 150) | 60 (30, 140) | 0.12 |
| Bridge Timing | |||
| Pre-Op | 0 | 4% (8) | N/A |
| Post-Op | 17% (14) | 46% (86) | <0.001 |
| Time from last dose to surgery (hours) Median (IQR) | 22 (17, 26) | 48 (29, 62) | <0.001 |
Bonferroni-adjusted p = 0.025, DOAC = direct oral anticoagulant, A-fib = atrial fibrillation, VTE = venous thromboembolism, CVA = cerebrovascular accident, CAD = coronary artery disease, Alpha 1 = Alpha 1 antitrypsin deficiency, PVD = peripheral vascular disease. 1 = Patients can have multiple indications for anticoagulant use, 2 = heparin bridge only provided to one patient in the not reversed group.
Table 3.
Methods for anticoagulation reversal.
| Reversed n = 186 | |
|---|---|
| Reversal Agents Useda | |
| FFP | 22% (40) |
| Factor VIIa | 1% (2) |
| Vitamin K | 42% (79) |
| Watch and Wait | 46% (86) |
| Total Dose of Reversal Agent | |
| FFP (ml) Median (IQR) | 516 (387, 622) |
| Factor VIIa (mcg) Mean (SD) | 10026 (14106) |
| Vitamin K (mg) Median (IQR) | 5 (4, 10) |
| Surgical Delay Reasona | |
| Concern for anticoagulation effect | 38% (71) |
| Family reasoning | 2% (3) |
| Medical clearance | 17% (32) |
| No dedicated operating room available | 2% (4) |
| No dedicated surgeon available | 1% (1) |
| No reason for delay dictated | 41% (77) |
Multiple anticoagulation reversal strategies or reasons for surgical delays for some patients.
The types of hip fracture were similar across study arms (Table 4). Clinical labs collected before, during and after surgery were comparable, except for pre-operative hemoglobin and pre-operative international normalized ratio (INR). The mean (SD) pre-operative hemoglobin was higher for patients not reversed 13.0 (2.1), when compared to patients not on anticoagulants 11.7 (2.1) and reversed patients 11.2 (2.2), p < 0.001. The median [IQR] pre-operative INR was lower for patients not on anticoagulants, 1.1 [1.0, 1.2] when compared to patients not reversed 1.4[1.2, 2.0] and reversed patients 1.6 [1.3, 1.8], p < 0.001. The median [IQR] time to surgery was significantly longer for the reversed group, being 33 h [24, 44]; when compared to those not on anticoagulants, 20 h [15, 28] and those not reversed being 17 h [12, 23], p < 0.001. There was a higher proportion of not reversed patients (15%) and reversed patients (10%) who had a bipolar hemiarthroplasty than patients not on anticoagulants (4%), p = 0.006. There were fewer not reversed patients (6%) than patients not on anticoagulants (20%), who had a hemiarthroplasty, p = 0.02. There were more reversed patients (22%) who had internal fixation than patients not on anticoagulants (10%), p = 0.004. All other procedures were comparable across study arms.
Table 4.
Hip fracture and procedure details.
| Not on Anticoagulants n = 189 | Not Reversed n = 84 | Reversed n = 186 | p | |
|---|---|---|---|---|
| Fracture Type | ||||
| Intertrochanteric | 50% (93) | 48% (45) | 46% (87) | 0.68 |
| Femoral Neck | 47% (87) | 49% (46) | 50% (95) | 0.84 |
| Peritrochanteric | 2% (3) | 2% (2) | 1% (1) | 0.38 |
| Subtrochanteric | 8% (15) | 6% (6) | 8% (16) | 0.83 |
| Clinical Labs | ||||
| Pre-Op Hemoglobin Mean (SD) | 11.7 (2.1) | 13.0 (2.1) | 11.2 (2.2) | <0.001a |
| Op. Hemoglobin Median (IQR) | 11.61 | 121 | 8 (7.6, 7.9) | N/A |
| Post-Op Hemoglobin Median (IQR) | 10.6 (9.2, 12.5) | 10.4 (9.9, 11.7) | 9.8 (8.9, 12.2) | 0.92 |
| Hemoglobin Drop Median (IQR) | −0.6 (−2.1, 0.1) | −1.2 (−1.8, −0.5) | −0.1, (−0.8, 0.2) | 0.43 |
| Pre-Op INR Median (IQR) | 1.1 (1.0, 1.2) | 1.4 (1.2, 2.0) | 1.6 (1.3, 1.8) | <0.001b |
| Post-Op INR Median (IQR) | 6.4 (1.1, 11.6) | 3.3 | 1.3 (1.2, 1.5) | N/A |
| ALT Median (IQR) | 21 (17, 27) | 21 (17, 28) | 22 (19, 28) | 0.52 |
| Cr Median (IQR) | 1.0 (0.8, 1.2) | 0.9 (0.7, 1.2) | 1.0 (0.8, 1.3) | 0.16 |
| Lactate Median (IQR) | 1.4 (1.1, 1.9) | 1.2 (1.0, 2.4) | 1.5 (1.2, 1.9) | 0.75 |
| K Median (IQR) | 4 (3.7, 4.2) | 4 (3.8, 4.3) | 4.1 (3.8, 4.3) | 0.12 |
| CrCl Abnormal (<60) % (n) | 90% (171) | 86% (72) | 92% (172) | 0.22 |
| Time to Surgery Median (IQR) | 20 (15, 28) | 17 (12, 23) | 33 (24, 44) | <0.001c |
| Procedures | ||||
| Bipolar Hemiarthroplasty | 4% (8) | 15% (13) | 10% (19) | 0.006d |
| Individual Screw Placement | 3% (5) | 5% (4) | 3% (5) | 0.60 |
| Total Hip Arthroplasty | 10% (19) | 14% (12) | 7% (13) | 0.16 |
| Locking Plate | 3% (5) | 2% (2) | 5% (9) | 0.42 |
| Dynamic Hip Screw Placement | 7% (14) | 2% (2) | 7% (13) | 0.26 |
| Hemiarthroplasty | 20% (37) | 6% (5) | 16% (29) | 0.02e |
| Intramedullary Fixation | 55% (104) | 55% (46) | 53% (98) | 0.89 |
| Internal Fixation | 10% (19) | 12% (10) | 22% (41) | 0.004f |
Bonferroni-adjusted p = 0.025, N = number of patients, p = p-value, pre-op = pre-operative, SD = standard deviation, op. = operative, IQR = interquartile range, post-op = post-operative, ALT = Alanine Aminotransferase, Cr = creatinine, K = potassium, CrCl = creatinine clearance. 1 = Only one patient with operative hemoglobin collected. a = Patients reversed and not on anticoagulants had a significantly lower pre-op hemoglobin than those not reversed, no significant differences observed between those reversed and not on anticoagulants, p = 0.11. b = The pre-op INR for patients on anticoagulants was significantly higher than those not on anticoagulants, no significant differences between those reversed and not reversed, p = 0.68. c = Reversed patients had a significantly longer time to surgery than those not on anticoagulants and those not reversed, no significant differences observed between those not reversed and those not on anticoagulants, p = 0.04. d = Patients on anticoagulants had significantly more bipolar hemiarthroplasties than those not on anticoagulants, no statistical difference observed for patients reversed and not reversed, p = 0.22. e = Patients not on anticoagulants had a higher proportion of hemiarthroplasties than those not reversed, no significant difference between those not on anticoagulants and those reversed, p = 0.31, or between those not reversed and reversed, p = 0.03. f = Reversed patients had significantly more internal fixation devices placed than those not on anticoagulants, no significant difference between those not reversed and not on anticoagulants, p = 0.65, or not reversed and reversed, p = 0.05.
The median [IQR] hospital LOS was shorter for not reversed patients, 4 days [4,5], than patients not on anticoagulants, 5 days [4, 7], and reversed patients, 6 days [4, 9], p < 0.001 (Table 5). More patients not on anticoagulants (6%) returned to the ICU than reversed patients (1%), p = 0.007. There were no other significant differences observed for in-hospital complications or ICU LOS. The median volume of blood loss was similar across groups. Patients not on anticoagulants lost a median [IQR] of 100 [50, 150] ml of blood, compared to 100 [50, 150] for not reversed patients, and 100 [50, 200] for reversed patients; this was not significant. The median [IQR] volume of pRBC transfused approached statistical significance, with the highest median volume of transfusions for the reversed patients 660 [359, 761], not reversed patients had a median volume of 570 [310, 660], whereas patients not on anticoagulants had a median volume of 498 [350, 700] pRBC transfusion, p = 0.03. There were few platelet transfusions, none of the reversed patients received a platelet transfusion, only one not reversed patient and one patient not on anticoagulants had a platelet transfusion. FFP transfusions were similar across study arms and there were no cryoprecipitate transfusions for any patient in this study. There were no deaths in the not reversed group, two deaths (1%) in the reversed group, and one death (1%) in the not on anticoagulants group, however there was no statistically significance in mortality.
Table 5.
Outcomes and complications by study arm.
| Not on Anticoagulants n = 189 | Not Reversed n = 84 | Reversed n = 186 | p | |
|---|---|---|---|---|
| ICU LOS Median (IQR) | 3 (3, 5) | 4 (3, 7) | 4 (3, 9) | 0.50 |
| Hospital LOS Median (IQR) | 5 (4, 7) | 4 (4, 5) | 6 (4, 9) | <0.001a |
| Complications | ||||
| PE | 2% (3) | 0 | 0 | 0.22 |
| Return to ICU | 6% (11) | 2% (2) | 1% (1) | 0.007b |
| Pneumonia | 2% (3) | 0 | 4% (7) | 0.12 |
| DVT | 4% (7) | 1% (1) | 2% (4) | 0.59 |
| Stroke or CVA | 2% (3) | 0 | 1% (1) | 0.53 |
| MI | 1% (2) | 0 | 0 | 0.67 |
| Wound Hematoma | 1% (2) | 1% (1) | 2% (4) | 0.78 |
| Mortality % (n) | 1% (1) | 0 | 1% (2) | >0.99 |
| Odds Ratio (CI) | 0.3 (0.1, 1.3) | 0.3 (0, 2.5) | Reference | 0.20 |
| Blood transfusions (ml) | ||||
| FFP Median (IQR) | 6231 | 513 (316, 661) | 443 (299, 620) | N/A |
| pRBC Median (IQR) | 498 (350, 700) | 570 (310, 660) | 660 (359, 761) | 0.03 |
| Platelets Median (IQR) | 456 (284) | 2631 | N/A | N/A |
| Blood Loss Median (IQR) | 100 (50, 150) | 100 (50, 150) | 100 (50, 200) | 0.70 |
Bonferroni-adjusted p = 0.025, N = number of patients, p = p-value, ICU = intensive care unit, LOS = length of stay, PE = pulmonary embolus, DVT = deep vein thrombosis, CVA = cerebrovascular accident, MI = myocardial infarction, FFP = fresh frozen plasma, RBC = packed red blood cells. 1 = Value only collected for one patient. a = All differences observed were significantly different. b = Patients not on anticoagulants were more likely than those reversed to return to ICU, no statistically significant differences observed for patients not on anticoagulants and not reversed patients, p = 0.36, or for patients not reversed and reversed, p = 0.23.
After adjusting for the enrolling facility, the average difference (CI) in the total volume of pRBCs transfused was a decrease of 232 ml (−470, 6) for the not reversed group when compared to those reversed, (Table 6). The mean (SE) volume of blood loss was 138 ml (12) in patients not on anticoagulants and was 134 ml (17) for not reversed patients; whereas blood loss for reversed patients was 159 (12), after adjustment; but these differences were not significant. The ICU LOS was a mean difference (CI) of 1.9 days shorter (−7.5, 3.6) for patients not reversed when compared to those reversed, p-diff = 0.49. Whereas, the hospital LOS was an average of 1.4 days significantly shorter (−2.4, −0.3) for not reversed patients when compared to those reversed, p-diff = 0.01.
Table 6.
Adjusted models for outcomes and complications by study arm.
| Not on Anticoagulants n = 189 | Not Reversed n = 84 | Reversed n = 186 | Model p-value | |
|---|---|---|---|---|
| Total Volume of pRBC Transfused n = 115 | ||||
| LS Mean (SE)a | 581 (58) | 511 (106) | 743 (54) | 0.008 |
| LS Mean (CI) Differencea | −161 (−317, −5) | −232 (−470, 6) | Reference | |
| p-difference | 0.04 | 0.06 | Reference | |
| Total Volume of Blood Loss n = 443 | ||||
| LS Mean (SE)b | 138 (12) | 134 (17) | 159 (12) | 0.001 |
| LS Mean (CI) Differenceb | −21 (−48, 7) | −25 (−62, 12) | Reference | |
| p-difference | 0.14 | 0.18 | Reference | |
| Hospital LOS n = 448 | ||||
| LS Mean (SE)c | 6.8 (0.4) | 6.3 (0.6) | 7.7 (0.4) | <0.001 |
| LS Mean (CI) Differencec | −0.9 (−1.6, −0.1) | −1.4 (−2.4, −0.3) | Reference | |
| p-difference | 0.02 | 0.01 | Reference | |
| ICU LOS n = 57 | ||||
| LS Mean (SE)d | 7.3 (1.8) | 6.6 (2.7) | 8.5 (1.8) | 0.005 |
| LS Mean (CI) Differenced | −1.2 (−5.2, 2.9) | −1.9 (−7.5, 3.6) | Reference | |
| p-difference | 0.56 | 0.49 | Reference | |
Bonferroni-adjusted p = 0.025, LS = least-squared mean, SE = standard error, CI = confidence internal, p-difference = p-value for the difference in LS Means, a = adjusted for enrolling facility, b = adjusted for hemiarthroplasty and enrolling facility, c = adjusted for pre-ambulatory status and enrolling facility, d = adjusted for total hip arthroplasty and enrolling facility. Variables available to adjusted models: pre-ambulatory status, pre-operative hemoglobin, pre-operative INR, enrolling facility, pre-injury potassium, pre-injury statins, preinjury analgesics, bipolar hemiarthroplasty, hemiarthroplasty, total hip arthroplasty, internal fixation, and congestive heart failure.
4. Discussion
This study evaluated the outcomes for geriatric patients with hip fractures requiring surgery who were not taking pre-injury anticoagulants, whose pre-injury anticoagulant was reversed, and whose pre-injury anticoagulant was not reversed. The results showed that patients who were not reversed did not experience statistically significant increase in the total volume of blood transfusions, total volume of blood loss, mortality, or ICU LOS when compared to those reversed. Though, there a significant decrease in the HLOS for patients not reversed when compared to those reversed.
Although statistically non-significant, there was an increase of the blood transfusions and blood loss for patients in the reversed arm when compared to patients not reversed; it is possible that this may be in part due to the differences in anticoagulant bridging. Almost half of the reversed patients were given an anticoagulation bridge prior to surgery. However, limited data exists to demonstrate a benefit of bridging, and more recently studies have shown an increase of bleeding and transfusions for patients who had their anticoagulant bridged after interruption when compared to patients who did not have their anticoagulant bridged.25,26 The American Academy of Neurology guideline states there is insufficient evidence to support or refute bridging, but also states that most studies have found that bridging is probably associated with increased bleeding.27 The American College of Cardiology recommends selective bridging for patients with a history of bleeding complications and not to bridge for patients who are at a lower risk for bleeding complications.24 Additionally the rapid onset and offset of DOACs is thought to obviate the need for bridging.17
It is no surprise that there was a higher proportion of patients who were taking pre-injury warfarin who were reversed than not reversed, given that there are only two FDA approved reversal agent for DOACs, Idarucizumab for dabigatran and Andexanet for rivaroxaban and apixaban.10,18,20,28 However, Idarucizumab can lead to thrombotic events.20 The lack of approved reversal agents for DOACs may contribute to the decision not to reverse. Despite the approval of Idarucizumab in 2015, there were no patients in this study reversed using Idarucizumab.28 Andexanet was not approved during enrollment in this study. Antiocoagulation reversal for patients on DOACs was attained using non-specific reversal agents or the wait and watch method. Thromboembolism is a complication of non-specific reversal agents, occurring in 1.6% of PCC treated patients and 4.5% of FFP treated patients; though there was no significant difference in the rate of thromboembolic complications among groups in this study.7 It is possible these patients went to surgery without complete or with inadequate reversal of the anticoagulant. Therefore, some of the reversed and not reversed patients may be in a similar coagulant status, evidenced by the lack of statistical difference in the pre-operative INR for patients reversed and not reversed, p = 0.68. The American Society for Regional Anesthesia and Pain Medicine recommends an INR of less than 1.5 before surgery because of hematoma and bleeding risks.12 Further research is needed to determine if outcomes are improved for patients considered adequately reversed when compared to patients considered partially reversed.
Given that anticoagulation reversal is thought to lower the risk for blood loss and transfusions, it was unexpected that there were no significant differences in blood loss or transfusions between groups.16,19,29 This may be due to the mean pre-operative hemoglobin being significantly lower for the reversed group than the not reversed group, p < 0.001. The unadjusted volume of pRBC transfusions approached statistical significance and was higher for those reversed than those not reversed, p = 0.03. After adjustment there were no significant differences in blood loss or transfusion, though all volumes were highest for the reversed patients. Additionally, the reversed patients had a significantly longer time to surgery when compared to those not on anticoagulants and those not reversed, p < 0.001. Grimes et al. found that 11% of patients who went to surgery ≥24 h of admission were provided a blood transfusion; whereas only 3% of those who went to surgery <24 h required a blood transfusion, however no p-value was provided for the difference in these proportions.30 Delaying surgery for anticoagulant reversal may be associated with bleeding or need for transfusions.
However, there was a significant decrease in the HLOS for not reversed patients when compared to those reversed which could be in part because of the wait and watch method for anticoagulation reversal. This is similar to another prior study by Buecking et al. which found reversed patients had a significantly longer HLOS, however they compared to patients not on anticoagulants, p = 005.31 To the best of our knowledge, no other studies compared the HLOS amongst patients who were reversed to patients who were not reversed.
There were limitations to this study. The anticoagulant status or timing of the last dose may not have been known before surgery. It is also possible patients in the reversed group did not have their anticoagulant effect completely reversed; consequently, some reversed patients may have been in a similar anticoagulant status as those not reversed. The decision to reverse the anticoagulant was not standardized across participating centers. There is a potential that selection bias was introduced by selecting not to reverse patients who were in better condition for immediate surgery, when sicker patients may have been reversed using the “wait and watch” method if deemed not safe for immediate surgery. Investigation of patient demographic and clinical characteristics to adjust for were methods to reduce the effect of this bias. Future randomized trials are needed to confirm the results of this study.
Geriatric patients with an isolated hip fractures on pre-injury anticoagulant who did not have their anticoagulant reversed prior to hip fracture surgery did not experience any significant increases in blood loss, blood transfusions, in-hospital complications, mortality, or ICU LOS. However, the patients not reversed did have a significantly shorter LOS when compared to those reversed. Our data also suggests that geriatric patients with an isolated hip fracture taking pre-injury anticoagulants, with or without reversal prior to surgery, seem to have a similar risk of blood loss compared to patients not on anticoagulants. Given the extra cost, delays in surgery, increased HLOS, and potential side effects of reversal strategies, we recommend against routinely reversing anticoagulation in patients with hip fractures.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributions
RM, SJ, AO, NN, RB, PM, MK, and DBO contributed to study conceptualization. SJ and MN contributed to data curation. SJ, AO and NN contributed to formal analysis and visualization. RM, SJ, AO, NN, RB, PM, BW, PH, MN, MK, WS, BDO contributed to investigation, validation, methodology, and writing. SJ, AO and DBO contributed to project administration and supervision.
Declaration of competing interest
The authors declare there are no financial conflicts of interest to disclose.
Acknowledgements
We would like to thank all of the clinical research coordinators for their work on this study: Diane Redmond, Kathy Rodkey, Jennifer Pekarek, Brenda Kuipoff, Carolyn Blue, Kimberly Aumann, Shenequa Deas, and Jamie Shaddix.
Contributor Information
Rick Meinig, Email: rickmeinig@gmail.com.
Stephanie Jarvis, Email: sjarvis.traumaresearch@gmail.com.
Alessandro Orlando, Email: alessandro.orlando@me.com.
Nnamdi Nwafo, Email: nnamdinwafo@gmail.com.
Rahul Banerjee, Email: rahulbanerjee7@hotmail.com.
Patrick McNair, Email: pmcnairmobile@panoramaortho.com.
Bradley Woods, Email: bradleykw@hotmail.com.
Paul Harrison, Email: paulh49@cox.net.
Michelle Nentwig, Email: mnentwig@kumc.edu.
Michael Kelly, Email: michaelkelly@centura.org.
Wade Smith, Email: WadeSmith2@gmail.com.
David Bar-Or, Email: davidbme49@gmail.com.
References
- 1.Lee D.J., Elfar J.C. Timing of hip fracture surgery in the elderly. Geriatr Orthop Surg Rehabil. 2014;5(3):138–140. doi: 10.1177/2151458514537273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leung F., Blauth M., Bavonratanavech S. Surgery for fragility hip fracture-streamlining the process. Osteoporos Int. 2010;21(SUPPL. 4):519–521. doi: 10.1007/s00198-010-1402-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marufu T.C., Mannings A., Moppett I.K. Risk scoring models for predicting peri-operative morbidity and mortality in people with fragility hip fractures: qualitative systematic review. Injury. 2015;46(12):2325–2334. doi: 10.1016/j.injury.2015.10.025. [DOI] [PubMed] [Google Scholar]
- 4.Pinto I.P., Felipe L., Ferres B., Puertas E.B., Boni G. 2019. Does Early Surgical Fixation of Proximal Femoral Fractures in Elderly Patients Affect Mortality Rates ? Ã A cirurgia precoce nas fraturas do fêmur proximal em idosos reduz a taxa de mortalidade ? pp. 2017–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Al-rashid M., Parker M.J. 2005. Anticoagulation Management in Hip Fracture Patients on Warfarin; pp. 1311–1315. [DOI] [PubMed] [Google Scholar]
- 6.Sridharan M., Wysokinski W.E., Pruthi R. Periprocedural warfarin reversal with prothrombin complex concentrate. Thromb Res. 2016;139(2016):160–165. doi: 10.1016/j.thromres.2015.11.024. [DOI] [PubMed] [Google Scholar]
- 7.Tornkvist M., Smith J.G., Labaf A. Current evidence of oral anticoagulant reversal: a systematic review. Thromb Res. 2018;162(August 2017):22–31. doi: 10.1016/j.thromres.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 8.Barnes Goeffrey D., Luxas Eleanor, Alexander G Caleb, ZDG National trends in ambulatory oral anticoagulant use. Am J Med. 2016;128(12):1300–1305. doi: 10.1016/j.amjmed.2015.05.044. (National) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aronis K.N., Hylek E.M. Who, when, and how to reverse non-vitamin K oral anticoagulants. J Thromb Thrombolysis. 2016;41(2):253–272. doi: 10.1007/s11239-015-1297-0. [DOI] [PubMed] [Google Scholar]
- 10.Riley T.R., Gauthier-Lewis M.L., Sanchez C.K., Douglas J.S. Role of agents for reversing the effects of target-specific oral anticoagulants. Am J Health Pharm. 2017;74(2):54–61. doi: 10.2146/ajhp150810. [DOI] [PubMed] [Google Scholar]
- 11.Brown K.S., Zahir H., Grosso M.A., Lanz H.J., Mercuri M.F., Levy J.H. Nonvitamin K antagonist oral anticoagulant activity: challenges in measurement and reversal. Crit Care. 2016;20(1):1–10. doi: 10.1186/s13054-016-1422-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vitale M.A., VanBeek C., Spivack J.H., Cheng B., Geller J.A. Pharmacologic reversal of warfarin-associated coagulopathy in geriatric patients with hip fractures. Geriatr Orthop Surg Rehabil. 2011;2(4):128–134. doi: 10.1177/2151458511417434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khan S.K., Kalra S., Khanna A., Thiruvengada M.M., Parker M.J. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury. 2009;40(7):692–697. doi: 10.1016/j.injury.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 14.Uzoigwe C.E., Burnand H.G.F., Cheesman C.L., Aghedo D.O., Faizi M., Middleton R.G. Early and ultra-early surgery in hip fracture patients improves survival. Injury. 2013;44(6):726–729. doi: 10.1016/j.injury.2012.08.025. [DOI] [PubMed] [Google Scholar]
- 15.Panesar S.S., Simunovic N., Bhandari M. When should we operate on elderly patients with a hip fracture? It’s about time! The Surgeon. 2012;10(4):185–188. doi: 10.1016/j.surge.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Ashouri F., Al-Jundi W., Patel A., Mangwani J. Management of warfarin anticoagulation in patients with fractured neck of femur. ISRN Hematol. 2011;2011:1–5. doi: 10.5402/2011/294628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Douketis J.D., Lip G. Perioperative management of patients receiving anticoagulants. UpToDate. 2019:1–28. [Google Scholar]
- 18.Almegren M. Reversal of direct oral anticoagulants. Vasc Health Risk Manag. 2017;13:287–292. doi: 10.2147/VHRM.S138890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhatia M., Talawadekar G., Parihar S., Smith A. An audit of the role of vitamin K in the reversal of international normalised ratio (INR) in patients undergoing surgery for hip fracture. Ann R Coll Surg Engl. 2010;92(6):473–476. doi: 10.1308/003588410X12664192075774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peacock W.F., Rafique Z., Singer A.J. Direct-Acting oral anticoagulants: practical considerations for emergency medicine physicians. Emerg Med Int. 2016;2016:1–13. doi: 10.1155/2016/1781684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ito S. Pharmacokinetics 101. Paediatr Child Health. 2011;16(9):535–536. doi: 10.1093/pch/16.9.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohn M.R., Levack A.E., Trivedi N.N. The hip fracture patient on warfarin: evaluating blood loss and time to surgery. J Orthop Trauma. 2017;31(8):407–413. doi: 10.1097/BOT.0000000000000857. [DOI] [PubMed] [Google Scholar]
- 23.Foss N.B. Hidden blood loss after surgery for hip fracture. J Bone Jt Surg Br. 2006;88-B(8):1053–1059. doi: 10.1302/0301-620X.88B8.17534. [DOI] [PubMed] [Google Scholar]
- 24.Doherty J.U., Gluckman T.J., Hucker W.J. ACC expert consensus decision pathway for periprocedural management of anticoagulation in patients with nonvalvular atrial fibrillation: a report of the American College of Cardiology clinical expert consensus document task force. J Am Coll Cardiol. 2017. 2017;69(7):871–898. doi: 10.1016/j.jacc.2016.11.024. [DOI] [PubMed] [Google Scholar]
- 25.Rose A.J., Allen A.L., Minichello T. A call to reduce the use of bridging anticoagulation. Circ Cardiovasc Qual Outcomes. 2016;9(1):64–67. doi: 10.1161/CIRCOUTCOMES.115.002430. [DOI] [PubMed] [Google Scholar]
- 26.Levy J.H. Discontinuation and management of direct-acting anticoagulants for emergency procedures. Am J Emerg Med. 2016;34(11):14–18. doi: 10.1016/j.ajem.2016.09.048. [DOI] [PubMed] [Google Scholar]
- 27.Khoo K.F., Lepas B., Armstrong M.J. Summary of evidence-based guideline: periprocedural management of antithrombotic medications in patients with ischemic cerebrovascular disease: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;82(1) doi: 10.1212/WNL.0b013e318294b32d. 95-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dzeshka M.S., Pastori D., Lip G.Y.H. Direct oral anticoagulant reversal: how, when and issues faced. Expert Rev Hematol. 2017;10(11) doi: 10.1080/17474086.2017.1379896. 17474086.2017.1379896. [DOI] [PubMed] [Google Scholar]
- 29.Curtis R., Schweitzer A., van Vlymen J. Reversal of warfarin anticoagulation for urgent surgical procedures. Can J Anesth. 2015;62(6):634–649. doi: 10.1007/s12630-015-0366-3. [DOI] [PubMed] [Google Scholar]
- 30.Grimes J.P., Gregory P.M., Noveck H., Butler M.S., Carson J.L. The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002;112(9):702–709. doi: 10.1016/s0002-9343(02)01119-1. [DOI] [PubMed] [Google Scholar]
- 31.Buecking B., Eschbach D., Bliemel C. Effectiveness of vitamin K in anticoagulation reversal for hip fracture surgery - a prospective observational study. Thromb Res. 2014;133(1):42–47. doi: 10.1016/j.thromres.2013.10.031. [DOI] [PubMed] [Google Scholar]