Abstract
Recent decades have seen an increase in survival rates for cancer patients, partially explained by earlier diagnoses and new chemotherapeutic agents. However, chemotherapy may be associated with adverse cardiovascular events, including hypertension and pulmonary hypertension, supraventricular and ventricular arrhythmias, cardiomyopathy, and other forms of cardiovascular disease. For patients, the benefits of chemotherapy may be partially obfuscated by deleterious effects on the cardiovascular system, resulting in a significant increase in morbidity and mortality. In this article, we review strategies for prevention and treatment of chemotherapy-related cardiotoxicity.
Keywords: cancer, cardiotoxicity, prevention, treatment, chemotherapy, heart disease, anthracyclines, cardio-oncology
INTRODUCTION
The overall mortality rate from cancer fell by 27% between 1991 and 2016.1 This improvement in survival can be attributed to several causes, such as early detection, control of risk factors, and new chemotherapy treatments, among others. However, the benefits of chemotherapy may be partially obfuscated by drug-related adverse cardiovascular effects, especially cardiomyopathy.2–4 The most typical presentation of cardiomyopathy secondary to chemotherapy is dilated cardiomyopathy, which manifests in the course of chemotherapy or later.3 Prevention of cardiomyopathy and other types of chemotherapy-related cardiotoxicity involves approaches that minimize exposure of the drug—and therefore its potential cardiotoxic effects—and initiating cardioprotective drugs to decrease cardiovascular injury. Once cardiac damage is established, treatment should be started promptly.
The growing need to manage patients with drug-related adverse cardiovascular effects has led to the rapid creation and adoption of cardio-oncology, a multidisciplinary science aimed at monitoring, treating, and preventing treatment-related cardiotoxicity.5 This article addresses chemotherapeutic treatments that are associated with adverse cardiovascular events and presents strategies to prevent and treat chemotherapy-related cardiotoxicity.
CANCER TREATMENTS ASSOCIATED WITH CARDIOTOXICITY
Anthracyclines
The main class of chemotherapeutic agents related to cardiotoxicity are anthracyclines, which are used extensively to treat solid tumors such as breast cancer, osteosarcoma, and hematological malignancies.6 Anthracyclines are responsible for early and late cardiotoxicity, particularly heart failure (HF), and are related to cumulative dose.7 Since these adverse side effects can impact a patient's quality of life as much as the cancer diagnosis, the best approach to anthracycline-induced cardiotoxicity is to prevent cardiac injury.8 Table 1 summarizes strategies to reduce the cardiotoxic effect of anthracyclines.8,9
Table 1.
Strategies to reduce anthracycline-induced chemotherapy.9
| CARDIOPROTECTIVE STRATEGY |
Limit cumulative dose (mg/m2)
|
| Alter administration (continuous infusion) |
| Use fewer cardiotoxic anthracycline analogues (epirubicin, idarubicin, and mitoxantrone) |
| Choose lipossomal formulations |
| Administer cardioprotective drugs (discussed in “Prevention” section) |
According to the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America, patients who develop left ventricular (LV) dysfunction during anthracycline treatment should be treated as heart failure (HF) patients,10 and the decision of whether or not to continue chemotherapy should be discussed with the cardio-oncology team. An observational study evaluated the efficacy of carvedilol and enalapril in patients with LV ejection fraction (LVEF) < 45% under high anthracyclines doses, and 42% of treated patients experienced full LVEF recovery. In this study, the best predictor for improvement in LVEF was the time that cardiovascular drugs were initiated. None of the patients who started carvedilol and enalapril after 6 months of cardiac injury had recovery of LVEF.11 In another study, this one with longer follow-up, HF treatment was also associated with improvement in LV dysfunction after chemotherapy.12
There is no evidence regarding cardioprotection in patients with signs of subclinical myocardial dysfunction detected through biomarkers or changes in global longitudinal strain (GLS). Based on strain, chemotherapy should not be stopped or changed.13 Closer surveillance for signs and symptoms of cardiac dysfunction is warranted.14 The SUCCOUR (Strain sUrveillance of Chemotherapy for improving Cardiovascular Outcomes) trial will be the first randomized controlled trial to investigate the role of cardioprotective drugs based on changes in GLS.15
Immunotherapy
Immunotherapy has improved outcomes of breast cancer when combined with anthracyclines, although it is known to have some cardiotoxic effects. The human epidermal growth factor receptor 2 (HER2) is overexpressed in approximately 20% to 25% of patients with breast cancer and is associated with poor prognosis.16 Monoclonal antibodies (eg, trastuzumab, pertuzumab) can inhibit HER2 and substantially improve the efficacy of cancer therapy. The first study that demonstrated correlation between trastuzumab and cardiotoxicity evaluated the efficacy and safety of trastuzumab in women with metastatic breast cancer that overexpressed HER2. The study concluded that trastuzumab increases the clinical benefit of chemotherapy for metastatic breast cancer with overexpressed HER2; however, there was a 27% incidence of cardiac dysfunction in the group receiving anthracycline, cyclophosphamide, and trastuzumab, although the symptoms generally improved with standard medical management.17 The Herceptin Adjuvant (HERA) trial showed that 1-year treatment with trastuzumab after adjuvant chemotherapy improves disease-free survival. However, trastuzumab was correlated with a major risk of HF and decrease in LVEF.18,19 Other trials demonstrated a higher incidence of cardiotoxicity when trastuzumab was used as adjuvant treatment in breast cancer19 and an increased risk of cardiac dysfunction and heart failure when it was given concomitantly with anthracyclines.20
Trastuzumab cardiotoxicity appears to be highly reversible and not dose related.21 Fei et al. found 68% full or partial reversibility in patients with breast cancer who developed cardiotoxicity after anthracyclines and trastuzumab in a retrospective study.22 Management of trastuzumab cardiotoxicity has two aspects: withdrawal of the medication and treatment of cardiac dysfunction based on heart failure guidelines.10 All patients with LVEF < 40% should be treated with an angiotensin-converting enzyme inhibitor (ACEI) and beta-blocker, the standard treatment for heart failure.23 Median time to LVEF recovery is 1.5 months after withdrawal of the agent.21 If retreatment with trastuzumab is needed after recovery of cardiac function, it is fundamental to maintain the use of ACEIs and beta-blockers.21,23
Inhibition of the Vascular Endothelial Growth Factor Signaling Pathway
Hormone receptor-negative tumors are associated with high concentrations of vascular endothelial growth factor (VEGF). Bevacizumab, a monoclonal antibody, can inhibit VEGF and benefit patients with this kind of solid tumor.24 However, it appears that these agents are associated with severe systemic arterial hypertension, ischemic events, pulmonary hypertension, and heart failure.24,25 The development of cardiotoxicity in these patients may be related to transient impairment of the contractile elements within the cell or to the increased afterload on a compromised ventricle.26 Other tyrosine-kinase inhibitor agents have been associated with congestive heart failure. A meta-analysis including 21 trials analyzed the association of congestive heart failure with VEGF tyrosine-kinase inhibitors—including sorafenib, sunitib, vandetanib, axitinib, and panzopanib—and found congestive heart failure in 138 of 5,752 patients (2.4%).27
There is no specific treatment for cardiac dysfunction caused by VEGF tyrosine-kinase inhibitors. Like the others, management of chemotherapy-related cardiotoxicity is based on standard treatment of HF.10 Since anti-VEGF therapy can worsen hypertension, and uncontrolled pressure can lead to HF, cardioprotective antihypertensive drugs such as ACEIs and beta-blockers should be considered over other agents.28 Discontinuing anti-VEGF therapy and treating the HF can reverse the cardiomyopathy.29
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors (ICIs) are a new category of antitumor agents that interrupt the mechanism used by several tumors cells to evade destruction by the body's activated T lymphocytes and other immune cells, thus unleashing the body's own immune system to destroy cancer cells.30 The most commonly used agents are ipilimumab, nivolumab, and pembrolizumab. The systemic augmentation of immune responses by ICIs, especially when used in combination, leads to a range of immune-related toxicities, including myocarditis, colitis, hepatitis, pneumonitis, thyroiditis, myositis, hypophysitis, and dermatitis.31,32
Myocarditis is the most lethal among these, with an incidence of between 0.27% and 1.14%.33,34 About half of these patients may present with ventricular dysfunction.34 Clinical presentation of myocarditis includes signs of acute heart failure manifesting as dyspnea, pulmonary edema, chest pain, arrhythmias, syncope, and even cardiogenic shock or sudden death.34
Treatment of ICI-related myocarditis includes preventing new episodes of toxicity, immunosuppression to relieve inflammation, and clinical support to avoid cardiac worsening.32 Guidelines from the American Society for Clinical Oncology recommend the use of intravenous prednisone 1 to 2 mg/kg intravenously or methylprednisolone 500 to 1000 mg/kg. Mycophenolate mofetil or infliximab are recommended for those unresponsive to first-line treatment.35 In this scenario, collaboration between the cardiologist, oncologist, and immunologist is crucial to gain a better understanding of the myocarditis and prevent its progression without interrupting treatment.32
PREVENTION
The majority of published research in prevention of chemotherapy-induced cardiotoxicity focuses on anthracyclines and HER2 inhibitors. Prevention of cardiotoxicity should begin before cancer treatment is initiated, with the cardiologist and oncologist evaluating the patient for cardiovascular risk and, based on results, determining the best treatment approach.
Non-Pharmacological Prevention
The first step in preventing chemotherapy-related cardiotoxicity is to recommend that patients reduce their cardiovascular risk, ie, control blood pressure, lower cholesterol, maintain a healthy blood glucose level, consume a healthy diet, and stop smoking. Moderate aerobic exercise is a promising nonpharmacological strategy to prevent and/or treat chemotherapy-induced cardiotoxicity.36 A review of 56 studies involving 4,826 participants showed improved quality of life and physical capacity during and after a physical training program.37
Pharmacological Strategies
Dexrazoxane is the only cardioprotective agent approved by the US Food and Drug Administration (FDA) for anthracycline-induced cardiotoxicity. Dexrazoxane changes the configuration of topoisomerase IIb to prevent the binding of doxorubicin.38 There is strong evidence that patients who were treated with dexrazoxane had a lower incidence of HF compared to those who did not receive treatment. However, dexrazoxane is only FDA approved for patients with metastatic breast cancer who have already received > 300 mg/m2 of doxorubicin. This threshold may be due in part to evidence that dexrazoxane can interfere in anthracycline's antitumor efficacy.39
The use of cardiovascular drugs such as beta-blockers, ACEIs, and angiotensin receptor blockers to prevent cardiotoxicity is controversial and based on a limited number of clinical trials. In a randomized clinical trial comparing placebo versus carvedilol in patients treated with high doses of anthracycline chemotherapy, Kalay et al. found a greater reduction in LVEF in the placebo group (69% to 53%) than in the carvedilol group (70% to 69%, P < .001).40 Another randomized study of nebivolol evaluated 45 women with breast cancer who underwent anthracycline treatment and demonstrated that nebivolol was protective against LVEF changes, ventricular diameters, and increased NT-pro-BNP levels compared to placebo.41
The recent PRADA (Prevention of Cardiac Dysfunction During Adjuvant Breast Cancer Therapy) Trial evaluated cardioprotection using metoprolol and candesartan in 130 breast cancer patients undergoing contemporary doses of anthracyclines (240 mg/m2).42 This study demonstrated benefit of candesartan in preventing cardiotoxicity, with a less-pronounced decrease in LVEF compared to the metoprolol group. However, it did not show benefit from metoprolol, with a 1.8% reduction of LVEF in the placebo group versus 1.6% in the metoprolol group.
The CECCY (Carvedilol Effect in Preventing Chemotherapy Induced Cardiotoxicity) trial tested the use of carvedilol versus placebo in 200 patients with breast cancer and normal LVEF receiving anthracycline 240 mg/m2 (Figure 1).43 A small percentage of patients developed cardiotoxicity, characterized by < 10% reduction in LVEF (14.5% in the carvedilol group vs 13.5% in placebo), and there was a modest 1.3% decrease in LVEF in the placebo group versus 0.9% in the carvedilol group. However, carvedilol was associated with attenuated troponin I values, a lower incidence of diastolic dysfunction, and a slight decrease in LV diastolic diameter.
Figure 1.
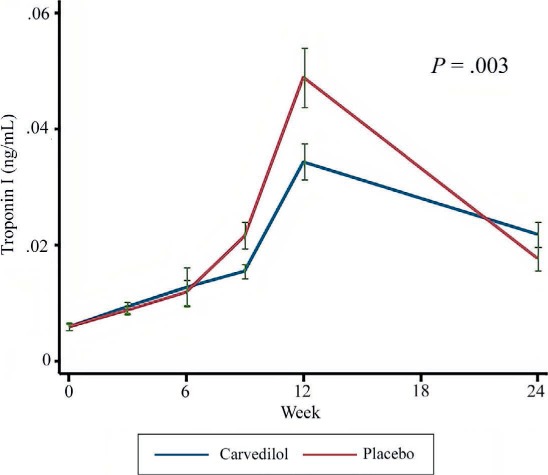
Sequential levels of troponin I during chemotherapy treatment.43
The MANTICORE (Multidisciplinary Approach to Novel Therapies in Cardiology Oncology Research) trial, which evaluated bisoprolol and perindopril in the prevention of cardiotoxicity in patients with breast cancer receiving trastuzumab, demonstrated a decline in LVEF attenuated in the bisoprolol group compared to the perindopril and placebo groups.16 Table 2 sumarizes the most important clinical trials in primary prevention of cardiotoxicity.16,40–47
Table 2.
A summary of the most important clinical trials in primary prevention of cardiotoxicity.16,40–47 LVEF: left ventricular ejection fraction
| STUDY | PATIENTS | CHEMOTHERAPY REGIMEN | CARDIOPROTECTIVE DRUG | PRIMARY OUTCOME | FOLLOW-UP (MONTHS) |
|---|---|---|---|---|---|
| Cardinale44 2006 | 114 | Epirubicin | Enalapril | Cardiotoxicity incidence: | 12 |
| Idarubicin | Control: 43% | ||||
| Daunorubicin | Enalapril: 0% | ||||
| P < .001 | |||||
| Kalay40 2006 | 50 | Doxorubicin | Carvedilol | LVEF change pre/post chemotherapy: | 6 |
| Epirubicin | Placebo: 68.9%/52.3%; P < .001 | ||||
| Carvedilol: 70.5%/69.7%; P = .30 | |||||
| Georgakopoulos45 2010 | 125 | Doxorubicin | Metoprolol | No difference in cardiotoxicity | 12 |
| Enalapril | P = .55 | ||||
| Bosch46 2013 | 201 | Idarubicin | Carvedilol | Mean change in LVEF reduction (%): | 6 |
| Daunorubicin | Enalapril | Control: −3.28 | |||
| Enalapril + Carvedilol: −0.17% | |||||
| P = .04 | |||||
| Kaya41 2013 | 45 | Doxorubicin | Nebivolol | LVEF change pre/post chemotherapy: | 6 |
| Epirubicin | Placebo: 66.6%/57.5%; P = .001 | ||||
| Nebivolol: 65.6%/63.8%; P = .50 | |||||
| Gulati42 2016 | 126 | Epirubicin | Metoprolol | Mean change in LVEF reduction (%): | 6 |
| Candesartan | Placebo: −2.6 | ||||
| Candesartan: 0.8; P = .026 | |||||
| Metoprolol: −1.6%; P = .77 | |||||
| Pituskin16 2017 | 94 | Trastuzumab | Bisoprolol | Mean change in LVEF reduction (%): | 12 |
| Perindopril | Placebo: 5% | ||||
| Perindopril: 3% | |||||
| Bisoprolol: −1 % | |||||
| P = .01 | |||||
| Avila43 2018 | 200 | Doxorubicin | Carvedilol | No change in LVEF | 6 |
| P = .84 | |||||
| Guglin47 2019 | 468 | Trastuzumab | Lisinopril | Cardiotoxicity rate: | 12 |
| Carvedilol | Placebo: 32% × lisinopril 30%, carvedilol 29% | ||||
| P = .27, P = .35 |
It is believed that patients who develop increased troponin during chemotherapy treatment have a higher risk of developing cardiotoxicity. Under this premise, Cardinale et al. tested cardioprotection with enalapril in 114 patients who developed positive troponin during treatment with high doses of anthracyclines. Compared to placebo, patients randomized to enalapril had significantly lower rates of cardiac events, including heart failure and asymptomatic ventricular dysfunction.44 Another study proposed testing enalapril with two strategies—enalapril started in all patients before chemotherapy, and enalapril started only in patients with an increase in troponin during or after chemotherapy—and concluded that enalapril did not impact troponin levels in either strategy.48
Aldosterone antagonists were evaluated in a randomized clinical trial that included 83 women with breast cancer receiving spironolactone or placebo during anthracycline chemotherapy. The trial demonstrated a benefit in both systolic and diastolic function in patients who received spironolactone compared to placebo.49
Statins are thought to have antioxidative and pleiotropic properties in addition to their inflammatory and lipid-lowering effects, which led to testing of its potential role in anthracycline-induced cardiotoxicity. There is some evidence in preclinical and small clinical trials showing a benefit of statins in maintaining LVEF in patients treated with anthracycline.50,51 Recently, a retrospective study evaluated statin exposure during trastuzumab treatment, with or without anthracyclines, in 129 women with HER2+ breast cancer and found a significant change in LVEF in the control group but not in the statin group.52
CONCLUSION
The survival rates of cancer patients have improved substantially with the development of immune checkpoint inhibitors and other therapies with specific molecular targets. However, the potential cardiotoxicity of these treatments requires clinicians to pay special attention to clinical signs and symptoms in order to manage cardiovascular complications. Preventive, diagnostic, and therapeutic algorithms must be continuously re-evaluated in interdisciplinary cardio-oncology boards, and additional studies are needed to develop more specific strategies for preventing and treating chemotherapy-related cardiotoxicity.
KEY POINTS
Chemotherapeutic agents can be associated with cardiovascular events that can increase morbidity and mortality among cancer patients.
The majority of prevention studies focusing on anthracyclines and HER2 inhibitors demonstrate the importance of minimizing exposure to the chemotherapy and initiating cardioprotective drugs at the right time.
Cardio-oncology is a growing field that is increasing knowledge about chemotherapy-induced cardiotoxicity and enabling more effective monitoring, treatment, and prevention.
Footnotes
Conflict of Interest Disclosure:
The authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
REFERENCES
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019 Jan;69(1):7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Bloom MW, Hamo CE, Cardinale D et al. Cancer Therapy-Related Cardiac Dysfunction and Heart Failure: Part 1: Definitions, Pathophysiology, Risk Factors, and Imaging. Circ Heart Fail. 2016 Jan;9(1) doi: 10.1161/CIRCHEARTFAILURE.115.002661. e002661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henriksen PA. Anthracycline cardiotoxicity: an update on mechanisms, monitoring and prevention. Heart. 2018 Jun;104(12):971–7. doi: 10.1136/heartjnl-2017-312103. [DOI] [PubMed] [Google Scholar]
- 4.Tabár L, Dean PB, Chen TH et al. The incidence of fatal breast cancer measures the increased effectiveness of therapy in women participating in mammography screening. Cancer. 2019 Feb 15;125(4):515–523. doi: 10.1002/cncr.31840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koutsoukis A, Ntalianis A, Repasos E, Kastritis E, Dimopoulos MA, Paraskevaidis I. Cardio-oncology: A Focus on Cardiotoxicity. Eur Cardiol. 2018 Aug;13(1):64–9. doi: 10.15420/ecr.2017:17:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller KD, Siegel RL, Lin CC et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016 Jul;66(4):271–89. doi: 10.3322/caac.21349. [DOI] [PubMed] [Google Scholar]
- 7.Suter TM, Ewer MS. Cancer drugs and the heart: importance and management. Eur Heart J. 2013 Apr;34(15):1102–11. doi: 10.1093/eurheartj/ehs181. [DOI] [PubMed] [Google Scholar]
- 8.Cardinale D, Biasillo G, Cipolla CM. Curing Cancer, Saving the Heart: A Challenge That Cardioncology Should Not Miss. Curr Cardiol Rep. 2016 Jun;18(6):51. doi: 10.1007/s11886-016-0731-z. [DOI] [PubMed] [Google Scholar]
- 9.Zamorano JL, Lancellotti P, Rodriguez Muñoz D et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC) Eur Heart J. 2016 Sep 21;37(36):2768–801. doi: 10.1093/eurheartj/ehw211. [DOI] [PubMed] [Google Scholar]
- 10.Yancy CW, Jessup M, Bozkurt B et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Card Fail. 2017 Aug;23(8):628–51. doi: 10.1016/j.cardfail.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 11.Cardinale D, Colombo A, Lamantia G et al. Anthracycline-induced cardiomyopathy: clinical relevance and response to pharmacologic therapy. J Am Coll Cardiol. 2010 Jan 19;55(3):213–20. doi: 10.1016/j.jacc.2009.03.095. [DOI] [PubMed] [Google Scholar]
- 12.Cardinale D, Colombo A, Bacchiani G et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015 Jun 2;131(22):1981–8. doi: 10.1161/CIRCULATIONAHA.114.013777. [DOI] [PubMed] [Google Scholar]
- 13.Thavendiranathan P, Poulin F, Lim KD, Plana JC, Woo A, Marwick TH. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol. 2014 Jul 1;63(25 Pt A):2751–68. doi: 10.1016/j.jacc.2014.01.073. [DOI] [PubMed] [Google Scholar]
- 14.Liu J, Banchs J, Mousavi N et al. Contemporary Role of Echocardiography for Clinical Decision Making in Patients During and After Cancer Therapy. JACC Cardiovasc Imaging. 2018 Aug;11(8):1122–31. doi: 10.1016/j.jcmg.2018.03.025. [DOI] [PubMed] [Google Scholar]
- 15.Negishi T, Thavendiranathan P, Negishi K, Marwick TH, SUCCOUR investigators Rationale and Design of the Strain Surveillance of Chemotherapy for Improving Cardiovascular Outcomes: The SUCCOUR Trial. JACC Cardiovasc Imaging. 2018 Aug;11(8):1098–1105. doi: 10.1016/j.jcmg.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 16.Pituskin E, Mackey J, Koshman S et al. Multidisciplinary Approach to Novel Therapies in Cardio-Oncology Research (MANTICORE 101-Breast): a Randomized Trial for the Prevention of Trastuzumab-Associated Cardiotoxicity. J Clin Oncol. 2017 Mar 10;35(8):870–7. doi: 10.1200/JCO.2016.68.7830. [DOI] [PubMed] [Google Scholar]
- 17.Slamon DJ, Leyland-Jones B, Shak S et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overex-presses HER2. N Engl J Med. 2001 Mar 15;344(11):783–92. doi: 10.1056/NEJM200103153441101. [DOI] [PubMed] [Google Scholar]
- 18.Cameron D, Piccart-Gebhart MJ, Gelber RD et al. 11 years' follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the HERceptin Adjuvant (HERA) trial. Lancet. 2017 Mar 25;389(10075):1195–205. doi: 10.1016/S0140-6736(16)32616-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldhirsch A, Gelber RD, Piccart-Gebhart MJ et al. 2 years versus 1 year of adjuvant trastuzumab for HER2-positive breast cancer (HERA): an open-label, randomised controlled trial. Lancet. 2013 Sep 21;382(9897):1021–8. doi: 10.1016/S0140-6736(13)61094-6. Herceptin Adjuvant (HERA) Trial Study Team. [DOI] [PubMed] [Google Scholar]
- 20.Moja L, Tagliabue L, Balduzzi S et al. Trastuzumab containing regimens for early breast cancer. Cochrane Database Syst Rev. 2012 Apr 18;(4) doi: 10.1002/14651858.CD006243.pub2. CD006243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ewer MS, Vooletich MT, Durand JB et al. Reversibility of trastuzumab-related cardiotoxicity: new insights based on clinical course and response to medical treatment. J Clin Oncol. 2005 Nov 1;23(31):7820–6. doi: 10.1200/JCO.2005.13.300. [DOI] [PubMed] [Google Scholar]
- 22.Fei HW, Ali MT, Tan TC et al. Left Ventricular Global Longitudinal Strain in HER-2 + Breast Cancer Patients Treated with Anthracyclines and Trastuzumab Who Develop Cardiotoxicity Is Associated with Subsequent Recovery of Left Ventricular Ejection Fraction. Echocardiography. 2016 Apr;33(4):519–26. doi: 10.1111/echo.13168. [DOI] [PubMed] [Google Scholar]
- 23.Ohtani K, Ide T, Hiasa KI et al. Cardioprotective effect of renin-angiotensin inhibitors and β-blockers in trastuzumab-related cardiotoxicity. Clin Res Cardiol. 2019 Oct;108(10):1128–1139. doi: 10.1007/s00392-019-01448-4. [DOI] [PubMed] [Google Scholar]
- 24.Cameron D, Brown J, Dent R et al. Adjuvant bevacizumab-containing therapy in triple-negative breast cancer (BEATRICE): primary results of a randomised, phase 3 trial. Lancet Oncol. 2013 Sep;14(10):933–42. doi: 10.1016/S1470-2045(13)70335-8. [DOI] [PubMed] [Google Scholar]
- 25.Chaar M, Kamta J, Ait-Oudhia S. Mechanisms, monitoring, and management of tyrosine kinase inhibitors-associated cardiovascular toxicities. Onco Targets Ther. 2018 Sep 25;11:6227–37. doi: 10.2147/OTT.S170138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Plana JC, Galderisi M, Barac A et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2014 Oct;15(10):1063–93. doi: 10.1093/ehjci/jeu192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ghatalia P, Morgan CJ, Je Y et al. Congestive heart failure with vascular endothelial growth factor receptor tyrosine kinase inhibitors. Crit Rev Oncol Hematol. 2015 May;94(2):228–37. doi: 10.1016/j.critrevonc.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 28.Sundararajan S, Kumar A, Poongkunran M, Kannan A, Vogelzang NJ. Cardiovascular adverse effects of targeted antiangiogenic drugs: mechanisms and management. Future Oncol. 2016;12(8):1067–80. doi: 10.2217/fon.16.4. [DOI] [PubMed] [Google Scholar]
- 29.Uraizee I, Cheng S, Moslehi J. Reversible cardiomyopathy associated with sunitinib and sorafenib. N Engl J Med. 2011 Oct 27;365(17):1649–50. doi: 10.1056/NEJMc1108849. [DOI] [PubMed] [Google Scholar]
- 30.Jain D, Aronow W. Cardiotoxicity of cancer chemotherapy in clinical practice. Hosp Pract (1995) 2019 Feb;47(1):6–15. doi: 10.1080/21548331.2018.1530831. [DOI] [PubMed] [Google Scholar]
- 31.Johnson DB, Chandra S, Sosman JA. Immune Checkpoint Inhibitor Toxicity in 2018. JAMA. 2018 Oct 23;320(16):1702–3. doi: 10.1001/jama.2018.13995. [DOI] [PubMed] [Google Scholar]
- 32.Hu JR, Florido R, Lipson EJ et al. Cardiovascular toxicities associated with immune checkpoint inhibitors. Cardiovasc Res. 2019 Apr 15;115(5):854–68. doi: 10.1093/cvr/cvz026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson DB, Balko JM, Compton ML et al. Fulminant Myocarditis with Combination Immune Checkpoint Blockade. N Engl J Med. 2016 Nov 3;375(18):1749–55. doi: 10.1056/NEJMoa1609214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mahmood SS, Fradley MG, Cohen JV et al. Myocarditis in Patients Treated With Immune Checkpoint Inhibitors. J Am Coll Cardiol. 2018 Apr 24;71(16):1755–64. doi: 10.1016/j.jacc.2018.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lyon AR, Yousaf N, Battisti NML, Moslehi J, Larkin J. Immune checkpoint inhibitors and cardiovascular toxicity. Lancet Oncol. 2018 Sep;19(9):e447–e458. doi: 10.1016/S1470-2045(18)30457-1. [DOI] [PubMed] [Google Scholar]
- 36.Jones LW, Liu Q, Armstrong GT et al. Exercise and risk of major cardiovascular events in adult survivors of childhood hodgkin lymphoma: a report from the childhood cancer survivor study. J Clin Oncol. 2014 Nov 10;32(32):3643–50. doi: 10.1200/JCO.2014.56.7511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mishra SI, Scherer RW, Geigle PM et al. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst Rev. 2012 Aug 15;(8) doi: 10.1002/14651858.CD007566.pub2. CD007566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lyu YL, Kerrigan JE, Lin CP et al. Topoisomerase IIbeta mediated DNA double-strand breaks: implications in doxorubicin cardiotoxicity and prevention by dexrazoxane. Cancer Res. 2007 Sep 15;67(18):8839–46. doi: 10.1158/0008-5472.CAN-07-1649. [DOI] [PubMed] [Google Scholar]
- 39.Swain SM, Whaley FS, Gerber MC et al. Cardioprotection with dexrazoxane for doxorubicin-containing therapy in advanced breast cancer. J Clin Oncol. 1997 Apr;15(4):1318–32. doi: 10.1200/JCO.1997.15.4.1318. [DOI] [PubMed] [Google Scholar]
- 40.Kalay N, Basar E, Ozdogru I et al. Protective effects of carvedilol against anthracycline-induced cardiomyopathy. J Am Coll Cardiol. 2006 Dec 5;48(11):2258–62. doi: 10.1016/j.jacc.2006.07.052. [DOI] [PubMed] [Google Scholar]
- 41.Kaya MG, Ozkan M, Gunebakmaz O et al. Protective effects of nebivolol against anthracycline-induced cardiomyopathy: a randomized control study. Int J Cardiol. 2013 Sep 1;167(5):2306–10. doi: 10.1016/j.ijcard.2012.06.023. [DOI] [PubMed] [Google Scholar]
- 42.Gulati G, Heck SL, Ree AH et al. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): a 2 × 2 factorial, randomized, placebo-controlled, double-blind clinical trial of candesartan and metoprolol. Eur Heart J. 2016 Jun 1;37(21):1671–80. doi: 10.1093/eurheartj/ehw022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Avila MS, Ayub-Ferreira SM, de Barros Wanderley MR, Jr et al. Carvedilol for Prevention of Chemotherapy-Related Cardiotoxicity: The CECCY Trial. J Am Coll Cardiol. 2018 May 22;71(20):2281–90. doi: 10.1016/j.jacc.2018.02.049. [DOI] [PubMed] [Google Scholar]
- 44.Cardinale D, Colombo A, Sandri M et al. Prevention of high-dose chemotherapy-induced cardiotoxicity in high-risk patients by angiotensin-converting enzyme inhibition. Circulation. 2006 Dec 5;114(23):2474–8. doi: 10.1161/CIRCULATIONAHA.106.635144. [DOI] [PubMed] [Google Scholar]
- 45.Georgakopoulos P, Roussou P, Matsakas E et al. Cardioprotective effect of metoprolol and enalapril in doxorubicin-treated lymphoma patients: a prospective, parallel-group, randomized, controlled study with 36-month follow-up. Am J Hematol. 2010 Nov;85(11):894–6. doi: 10.1002/ajh.21840. [DOI] [PubMed] [Google Scholar]
- 46.Bosch X, Rovira M, Sitges M et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: the OVERCOME trial (preventiOn of left Ventricular dysfunction with Enalapril and caRvedilol in patients submitted to intensive ChemOtherapy for the treatment of Malignant hEmopathies) J Am Coll Cardiol. 2013 Jun 11;61(23):2355–62. doi: 10.1016/j.jacc.2013.02.072. [DOI] [PubMed] [Google Scholar]
- 47.Guglin M, Krischer J, Tamura R et al. Randomized Trial of Lisinopril Versus Carvedilol to Prevent Trastuzumab Cardiotoxicity in Patients With Breast Cancer. J Am Coll Cardiol. 2019 Jun 11;73(22):2859–68. doi: 10.1016/j.jacc.2019.03.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cardinale D, Ciceri F, Latini R et al. Anthracycline-induced cardiotoxicity: A multicenter randomised trial comparing two strategies for guiding prevention with enalapril: The International CardioOncology Society-one trial. Eur J Cancer. 2018 May;94:126–37. doi: 10.1016/j.ejca.2018.02.005. ICOS-ONE Study Investigators. [DOI] [PubMed] [Google Scholar]
- 49.Akpek M, Ozdogru I, Sahin O et al. Protective effects of spironolactone against anthracycline-induced cardiomyopathy. Eur J Heart Fail. 2015 Jan;17(1):81–9. doi: 10.1002/ejhf.196. [DOI] [PubMed] [Google Scholar]
- 50.Acar Z, Kale A, Turgut M et al. Efficiency of atorvastatin in the protection of anthracycline-induced cardiomyopathy. J Am Coll Cardiol. 2011 Aug 23;58(9):988–9. doi: 10.1016/j.jacc.2011.05.025. [DOI] [PubMed] [Google Scholar]
- 51.Seicean S, Seicean A, Plana JC, Budd GT, Marwick TH. Effect of statin therapy on the risk for incident heart failure in patients with breast cancer receiving anthracycline chemotherapy: an observational clinical cohort study. J Am Coll Cardiol. 2012 Dec 11;60(23):2384–90. doi: 10.1016/j.jacc.2012.07.067. [DOI] [PubMed] [Google Scholar]
- 52.Calvillo-Argüelles O, Abdel-Qadir H, Michalowska M et al. Cardioprotective Effect of Statins in Patients With HER2-Positive Breast Cancer Receiving Trastuzumab Therapy. Can J Cardiol. 2019 Feb;35(2):153–159. doi: 10.1016/j.cjca.2018.11.028. [DOI] [PubMed] [Google Scholar]


