Abstract
Background
Although knowledge is an important factor that influences decisions regarding deceased organ donation, the associations of knowledge with attitude and behavior regarding organ donation remain uncertain in countries with low organ donation rates like Japan.
Material/Methods
We conducted a cross-sectional survey of hospital medical and non-medical staff in 15 Japanese medical facilities. The questionnaire included items on knowledge, attitude, and behavior toward deceased organ donation and transplantation. Participants were divided into 3 groups according to the tertile of knowledge score. Modified Poisson regression models were used for associations of knowledge score with organ donor registration and willingness to become an organ donor after death.
Results
Of the 1967 staff, 1275 returned the questionnaires (response rate, 64.8%). There were 1190 study subjects with complete data for analysis. For the lowest (n=512), middle (n=428), and highest (n=250) tertile knowledge groups, the proportions of participants who registered and expressed willingness to donate organs were 20.1%, 23.4%, and 28.4% and 31.1%, 38.3%, and 44.0%, respectively. The adjusted proportion ratios for organ donor registration were 0.90 (95% CI, 0.73–1.10) for the middle and 1.00 (0.80–1.26) for the highest tertile of knowledge, compared with the lowest tertile. However, participants with the highest tertile of knowledge score expressed higher willingness for organ donation than the lowest tertile (adjusted proportion ratio, 1.37; 95% CI, 1.13–1.66).
Conclusions
For hospital staff in Japanese medical facilities, high knowledge about organ donation and transplantation was not associated with donor registration, but was associated with willingness to become an organ donor.
MeSH Keywords: Attitude, Behavior, Knowledge, Tissue and Organ Procurement, Transplantation
Background
Tremendous progress has been made in organ transplantation over the past 2 or 3 decades [1]. Not only has it improved the survival and quality of life of patients with end-stage organ failure, but it has also provided economic benefits [2]. However, the shortage of solid organs available for transplantation remains a longstanding and serious global problem [3,4]. The above is true also for Japan. A total of 2207 solid organ transplantations were performed in Japan in 2016 [5]. However, while the graft survival rate in Japan is comparable to those reported by other countries like the USA [6,7], Japan lags behind other countries in terms of deceased donor transplantation. In fact, about 85% of solid organ transplantations in Japan were living donor transplantations [5]; sadly, the number of deceased organ donors in Japan in 2017 was only 0.88 per million population (pmp), which is far lower than, for example, that of Spain (46.90 pmp) and the USA (31.96 pmp) [8]. Even among Asian countries, Japan lags behind Korea (9.95 pmp) and Taiwan (4.50 pmp), for example. Consequently, approximately 14 000 Japanese patients in need of transplantation remain on the waiting list at present and, for example, patients with end-stage kidney disease have to wait for donor organs for 13.3 years on average [9], which is much longer than the waiting period in other countries [7].
The major barriers to deceased organ donation are, in general, lack of knowledge about deceased organ donation and transplantation, religious and cultural perspectives, and mistrust about organ transplantation and the criteria applied for the definition of brain death [10–12]. These barriers could be potentially overcome through identification of potential organ donors and donation requests, family support in the intensive care unit, education, social media, and law enforcement (opt-out system) [13–16]. Among these, education of both the healthcare professionals and the general public is a key factor in enhancing organ donor registration [17–19]. Systematic reviews show that educational programs on deceased organ donation and transplantation effectively influenced participants’ willingness to become organ donors and to register as an organ donor [20,21]. For example, highly educated physicians were reported to be more likely to donate their own organs and feel more comfortable in approaching the family of potential organ donors [22]. However, because such education is not systematically incorporated into the medical and nursing curricula, even medical and nursing students and healthcare professionals do not necessarily have enough information or knowledge in this area [23–27]. Therefore, effective approaches are needed to raise awareness of the organ shortage and to educate not only the general population, but also health professionals, about deceased organ donation.
Previous studies showed the significant impact of knowledge on attitude and behavior regarding deceased organ donation [28]. Most previous studies that assessed the relationships among knowledge, attitude, and behavior regarding organ donation were conducted in countries with moderate or high deceased organ donation rates [22,24,27,29–33], and little information is available on such relationships in countries with low deceased donation rates.
The purpose of the present study was to quantitatively assess the associations of knowledge level with willingness to become an organ donor after death and organ donor registration in Japan, a country with a low deceased organ donation rate.
Material and Methods
Study design, setting, and participants
This was a multicenter cross-sectional study conducted at the Saku Central Hospital Group in Nagano Prefecture, Japan. The group consists of 15 medical facilities: 3 clinical hospitals, 2 geriatric health services facilities, 6 home-visit nursing stations, 2 institutions that provide rural medicine and oriental medicine, 1 clinic, and 1 healthcare center. Although Saku Central Hospital Advanced Care Center, the largest of the 3 clinical hospitals, is a 450-bed tertiary hospital, no full-time transplant surgeons or infectious disease physicians had ever worked in the facility [34]. Therefore, only a few living donor kidney transplantations are performed each year in that Center.
Our study was conducted between November 1 and December 31, 2014. There were 1967 full-time medical and non-medical staff in the hospital group at the start of the study and all the full-time staff were eligible for study participation. Those who did not respond to the survey were excluded. The Institutional Review Boards of Saku Central Hospital Group and Kyoto University approved the study (#E2241). Returning a completed questionnaire was regarded as consent for study participation. Participation was voluntary and uncompensated.
Exposure
The main exposure variable was knowledge regarding deceased organ donation and transplantation. We assessed the participants’ level of knowledge on the basis of responses to the 20 either/or questions listed in Table 1. Since there was no validated questionnaire on knowledge regarding organ donation and transplantation at the time of our study in Japan, we developed a total of 20 items about knowledge based on the Delphi method [35]. The Delphi method is a validated approach for achieving consensus on core outcomes for clinical trials in medical areas, and consists of iterative surveys with responses to reach consensus among a panel of experts [35]. First, 2 transplant nephrologists (MM and MI) identified the potential questionnaire items from previous studies that focused on knowledge [22,24,25,29,31,32]. To account for the particular situation of organ donation in Japan, MM and MI also referred to an information booklet, The Gift of Life, which had been prepared by the Japan Organ Transplant Network for the general population [9]. The booklet contains basic information about deceased organ donation and transplantation, comparison of deceased organ donation rates between countries including Spain and the USA, and sports in transplant recipients. Thus, 24 potential items were extracted for the first round of questionnaires.
Table 1.
Twenty either/or questions to assess participants’ knowledge about deceased organ donation and transplantation in Japan.
Q: Each statement below concerns deceased organ donation and transplantation in Japan. Please select either “Yes” or “No”
|
Second, 11 experts, consisting of 6 transplant nephrologists, 4 nephrologists, and a single transplant surgeon in 4 academic and 4 community hospitals in Japan, formed the expert panel. We conducted the first round of questionnaire in which we asked 11 expert members to rate each item based on appropriateness (appropriate or inappropriate) by e-mail. A free text box was also included for comments. The percentage of agreement for each questionnaire item was defined based on the proportion of experts who rated the item. Seventeen of 24 potential items with a percentage of agreement of ≥80% were taken through to the second round of questionnaire and the remaining 7 items were allocated for discussion and modification during the subsequent expert panel meeting.
Third, 5 core members of the 11-panel team attended the panel meeting to have a face-to-face discussion about the potential questionnaire items appraised in the first round of questionnaires and to reach a consensus. In this meeting, the experts commented on the potential items and assessed them qualitatively. At the end, 3 potential indicators were deleted and 4 were modified.
After the expert panel meeting, the list of all accepted and modified potential items was converted into the second-round questionnaire and emailed to all panel members again for final appraisal. In this second round, the respondents were asked to rerate the potential items in the same way as the first round. They were shown the results of the first round and comments from experts. Thus, the 19 items with percent agreement of ≥80% were selected as the set of questionnaires. Because a single item was elected by the 5-panel members to be retained, the final set consisted of 20 items. The 20-item questionnaire was pilot-tested in a sample of 20 medical staff at another hospital and 20 individuals from the general public at large [36]. Based on the results of the pilot study, none of the items required modification or deletion from the questionnaire. The total score ranged from 0 to 20, with higher scores indicating better understanding. We divided the participants’ knowledge score into lowest, middle, and highest groups by tertiles.
Outcomes
Our primary outcome of interest was organ donor registration and the secondary outcome was willingness to become an organ donor after brain or circulatory death. At the time of our study, 4 modalities were available for Japanese to declare their consent to deceased organ donation. These included web-based registration and signed consent on either the health insurance card, driver’s license, or donor card. We describe here these 4 modalities as “organ donor registration”, indicating clear consent to donate organs after death [37].
Measurements
We measured outcomes using an anonymous questionnaire developed by our group and validated in our previous studies [25,37]. The questionnaire asked about attitude toward deceased organ donation, with options of “Yes”, “No”, or “Uncertain”. Only “Yes” was regarded as being positive for willingness. When the participant responded “Yes” to the question, we asked about the modality s/he selected to indicate consent for deceased organ donation. In addition to knowledge and the 2 outcomes of interest, data on age, sex, lifestyle, marital status, health status, experience in obtaining information or knowledge regarding transplantation and their sources, occupation, family discussion about organ donation, and work experience in organ transplantation were obtained through the questionnaires.
At the start of the study, each department head at each medical facility explained the present study and distributed the questionnaire to each staff member according to occupation. The collection box was placed in each department, taking account of the response rate. However, due to the large number of nurses in the Saku Central Hospital Group, the above procedure was conducted at each ward of the hospital. Participants placed the questionnaire in sealed opaque envelopes and returned them to the collection box during the study period.
Statistical analysis
Before the main analysis, we tested the reliability and validity of the 20 either/or questions that assessed knowledge among the study population. We evaluated the internal consistency reliability using Cronbach’s alpha. The minimum acceptable value was set at an alpha of ≥0.7 [38]. To test the criterion validity, we categorized the medical staff who have been engaged in organ transplantation as “experienced medical staff” and all other medical staff as “non-experienced medical staff” [39]. Thus, we compared the mean (standard deviation; SD) knowledge score between experienced medical staff, non-experienced medical staff, and non-medical staff group. Trends between the 3 groups were analyzed using the trend test.
We performed a complete case analysis. Summary statistics were presented as median values (interquartile range; IQR) for continuous variables and percentages for categorical variables. We divided participants into tertiles based on the knowledge score: lowest, middle, and highest tertile groups. Data of the subject characteristics of the 3 groups were compared by the Kruskal-Wallis test for continuous variables and chi-squared test for categorical variables.
We used a modified Poisson regression with robust error variance to estimate the proportion ratios and 95% confidence intervals (95% CI) for the associations of knowledge level with the outcomes [40]. Since the odds ratio always overestimates the relative risk ratio when the outcome is not rare [41], Poisson regression is preferred over logistic regression in these situations [42]. The multivariable models were adjusted for age, sex, occupation (medical or non-medical staff), family discussion about deceased organ donation, work experience in organ transplantation, and willingness to become an organ donor [11,29,30,43,44]. The proportions of outcomes were compared using the lowest tertile of knowledge score as the reference.
To test the robustness of our findings, we conducted 2 sensitivity analyses. First, we repeated the analysis using different cut-off values of knowledge score. The cut-off points were selected based on a pilot test. Second, we used multiple imputations by chained equations to handle missing covariates (data on age, sex, occupation, and work experience in organ transplantation were missing in 2.3%, 2.3%, 1.0%, and 0.6% of cases, respectively). In addition, we performed subgroup analysis stratified by occupation (medical vs. non-medical staff) based on a previous study [26]. Statistical tests were two-sided, and P values of less than 0.05 were considered statistically significant. All statistical analyses were performed using STATA statistical software, version 13.0 (STATA Corporation, College Station, TX).
Results
Knowledge
The questions were found to be reliable, with a Cronbach’s alpha coefficients of 0.76. There was a statistically significant difference in knowledge score by occupation and work experience in organ transplantation. The mean (SD) knowledge scores among experienced medical staff, non-experienced medical staff, and non-medical staff group were 14.6 (2.3), 13.9 (2.0), and 11.7 (2.9), respectively (P for trend <0.001).
Participants
Of the 1967 full-time staff from 15 participating medical facilities, 1275 (64.8%) returned completed questionnaires. Eighty-five participants were excluded because of missing information on exposure and covariates. Since there were no missing data on other characteristics, the participants who were included in the main analysis were the same as those with complete data (Figure 1). Among the 1190 participants with complete data, the response rate for each profession was as follows: doctors 22.9%, nurses 72.8%, health nurses 17.9%, obstetric nurses 52.3%, pharmacists 47.6%, clinical laboratory technicians 81.7%, clinical radiologists 40.0%, clinical engineers 63.6%, occupational therapists 59.0%, physical therapists 60.7%, nutritionists 48.5%, care workers 60.2%, other medical staff 61.8%, and non-medical staff 82.0%. The characteristics of the study participants according to tertiles of knowledge score are shown in Table 2. The median age of the entire group was 35 years (IQR 28–45) and 70.8% were females. These characteristics were very similar to those of 1967 eligible staff (median age 35 [IQR 27–44] and females 68.0%).
Figure 1.
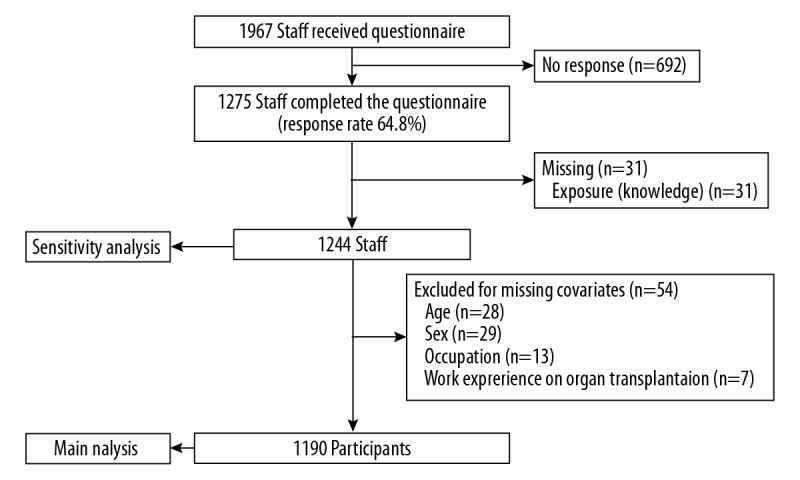
Flow chart of the subject recruitment process.
Table 2.
Characteristics of study participants by knowledge score about deceased organ donation and transplantation.
| Total (n=1190) | Knowledge score | P value | |||
|---|---|---|---|---|---|
| Lowest tertile (n=512) | Middle tertile (n=428) | Highest tertile (n=250) | |||
| Knowledge score, median (IQR), range | 14 (12–15), 5–20 | 12 (11–13), 5–13 | 14 (14–15), 14–15 | 16 (16–17), 16–20 | <0.001 |
| Age, median (IQR), range, years | 35 (28–45), 20–71 | 34 (26–43), 20–61 | 35 (28–46), 21–67 | 39 (29–47), 22–71 | <0.001 |
| Female sex, n (%) | 842 (70.8) | 334 (65.2) | 319 (74.5) | 189 (75.6) | 0.001 |
| Life style, living with family, n (%) | 821 (69.0) | 346 (67.6) | 303 (70.8) | 172 (68.8) | 0.57 |
| Marital status, married, n (%) | 683 (57.4) | 290 (56.6) | 248 (57.9) | 145 (58.0) | 0.90 |
| Current health status, visiting physicians for chronic disease, n (%) | 242 (20.3) | 105 (20.5) | 77 (18.0) | 60 (24.0) | 0.17 |
| History of obtaining information or knowledge about organ transplantation, n (%) | 1033 (86.8) | 427 (83.4) | 377 (88.1) | 229 (91.6) | 0.004 |
| Source of information or knowledge*, n (%) | |||||
| Television | 827 (69.5) | 362 (70.7) | 290 (67.8) | 175 (70.0) | 0.61 |
| Work place (hospital) | 560 (47.1) | 214 (41.8) | 201 (47.0) | 145 (58.0) | <0.001 |
| Newspapers | 535 (45.0) | 227 (44.3) | 196 (45.8) | 112 (44.8) | 0.90 |
| Medical education | 334 (28.1) | 127 (24.8) | 136 (31.8) | 71 (28.4) | 0.06 |
| Internet | 222 (18.7) | 102 (19.9) | 77 (18.0) | 43 (17.2) | 0.60 |
| High school education | 96 (8.1) | 47 (9.2) | 33 (7.7) | 16 (6.4) | 0.39 |
| Social networking service | 19 (1.6) | 9 (1.8) | 7 (1.6) | 3 (1.2) | 0.84 |
| Occupation, n (%) | <0.001 | ||||
| Physicians | 51 (4.3) | 12 (2.3) | 19 (4.4) | 20 (8.0) | |
| Nurses | 602 (50.6) | 229 (44.7) | 231 (54.0) | 142 (56.8) | |
| Health nurses | 26 (2.2) | 9 (1.8) | 10 (2.3) | 7 (2.8) | |
| Obstetric nurses | 23 (1.9) | 10 (2.0) | 6 (1.4) | 7 (2.8) | |
| Pharmacists | 20 (1.7) | 5 (1.0) | 11 (2.6) | 4 (1.6) | |
| Clinical laboratory technicians | 67 (5.6) | 25 (4.9) | 27 (6.3) | 15 (6.0) | |
| Clinical radiologists | 18 (1.5) | 7 (1.4) | 8 (1.9) | 3 (1.2) | |
| Clinical engineers | 21 (1.8) | 7 (1.4) | 7 (1.6) | 7 (2.8) | |
| Occupational therapists | 23 (1.9) | 11 (2.2) | 10 (2.3) | 2 (0.8) | |
| Physical therapists | 37 (3.1) | 12 (2.3) | 21 (4.9) | 4 (1.6) | |
| Nutritionists | 16 (1.3) | 9 (1.8) | 5 (1.2) | 2 (0.8) | |
| Care workers | 62 (5.2) | 31 (6.1) | 19 (4.4) | 12 (4.8) | |
| Other medical staff | 42 (3.5) | 19 (3.7) | 16 (3.7) | 7 (2.8) | |
| Non-medical staff | 182 (15.3) | 126 (24.6) | 38 (8.9) | 18 (7.2) | |
| Work experience in organ transplantation, n (%) | <0.001 | ||||
| Medical staff who has never been engaged in organ transplantation | 768 (64.5) | 310 (60.6) | 300 (70.1) | 158 (63.2) | |
| Medical staff who has been engaged in organ transplantation | 240 (20.2) | 76 (14.8) | 90 (21.0) | 74 (29.6) | |
| Family discussion about deceased organ donation, n (%) | 505 (42.4) | 184 (35.9) | 198 (46.3) | 123 (49.2) | <0.001 |
The sum of the percentages exceeds 100 because selection of more than one source of information or knowledge was permissible.
IQR – interquartile range.
For the lowest (n=512), middle (n=428), and highest (n=250) tertile groups, the median (IQR) knowledge scores were 12 (11–13), 14 (14–15), and 16 (16–17), respectively. Participants with the highest tertile of knowledge were more likely to be older female medical staff. They were more likely to have sought information or gained knowledge about organ transplantation, engaged in organ transplantation, and/or discussed organ donation with their families.
Outcome
Table 3 shows attitude and behavior regarding organ donation, according to tertiles of knowledge score. For the lowest, middle, and highest groups, the proportions of participants who registered as organ donors and expressed willingness to become organ donors after death were 20.1%, 23.4%, and 28.4% and 31.1%, 38.3%, and 44.0%, respectively.
Table 3.
Attitude and behavior towards deceased organ donation according to tertiles of knowledge score.
| Outcome | Total (n=1190) | Knowledge score | ||
|---|---|---|---|---|
| Lowest tertile (n=512) | Middle tertile (n=428) | Highest tertile (n=250) | ||
| Organ donor registration, n (%) | 274 (23.0) | 103 (20.1) | 100 (23.4) | 71 (28.4) |
| Driver’s license card | 147 (12.4) | 56 (10.9) | 58 (13.6) | 33 (13.2) |
| Donor card | 138 (11.6) | 46 (9.0) | 48 (11.2) | 44 (17.6) |
| Health insurance card | 108 (9.1) | 43 (8.4) | 38 (8.9) | 27 (10.8) |
| Online registration | 1 (0.1) | 0 (0) | 0 (0) | 1 (0.4) |
| Willingness to donate organs after death, n (%) | 433 (36.4) | 159 (31.1) | 164 (38.3) | 110 (44.0) |
| Willingness to donate organs after brain death | 361 (30.3) | 130 (25.4) | 133 (31.1) | 98 (39.2) |
| Willingness to donate organs after circulatory death | 401 (33.7) | 155 (30.3) | 149 (34.8) | 97 (38.8) |
The associations of knowledge with attitude and behavior regarding organ donation are shown in Table 4. In the modified Poisson regression models adjusted for age, sex, occupation, family discussion, work experience in organ transplantation, and willingness to become an organ donor, the adjusted proportion ratio for organ donor registration was 0.90 (95% CI, 0.73–1.10) for the middle tertile and 1.00 (95% CI, 0.80–1.26) for the highest tertile of knowledge, compared with the lowest tertile. However, subjects in the highest tertile of knowledge had greater willingness to donate organs than those of the lowest tertile (adjusted proportion ratio, 1.37; 95% CI, 1.13–1.66). Supplementary Table 1 shows the adjusted proportion ratios for each characteristic in the multivariable models.
Table 4.
Association (proportion ratio and 95% CI) of knowledge score with attitude and behavior toward deceased organ donation.
| Outcome | knowledge score | ||
|---|---|---|---|
| Lowest tertile (n=512) | Middle tertile (n=428) | Highest tertile (n=250) | |
| Organ donor registration | |||
| Unadjusted | 1 [reference] | 1.16 (0.91–1.48) | 1.41 (1.09–1.83) |
| Adjusted* | 1 [reference] | 0.90 (0.73–1.10) | 1.00 (0.80–1.26) |
| Willingness to donate organs after death | |||
| Unadjusted | 1 [reference] | 1.23 (1.03–1.47) | 1.42 (1.17–1.71) |
| Adjusted** | 1 [reference] | 1.16 (0.98–1.38) | 1.37 (1.13–1.66) |
Modified Poisson regression analysis adjusted for age, sex, occupation (medical or non-medical staff), work experience in organ transplantation, family discussion about deceased organ donation, and willingness to donate organs after death;
Modified Poisson regression analysis adjusted for age, sex, occupation (medical or non-medical staff), work experience in organ transplantation, and family discussion about deceased organ donation.
CI – confidence interval.
The 2 sensitivity analyses showed no association between knowledge and donor registration. However, participants of the middle and highest tertiles had greater willingness to donate organs after death than the lowest tertile in both sensitivity analyses, respectively (Supplementary Tables 2, 3). The results of subgroup analyses also indicated no association between knowledge and donor registration among the medical staff (Table 5). However, although the sample size was small, higher level of knowledge was associated with a higher but insignificant increase in donor registration among the non-medical staff (Table 5).
Table 5.
Subgroup analysis of association (adjusted proportion ratio and 95% CI) between knowledge score and attitude and behavior toward deceased organ donation stratified by occupation.
| Outcome | knowledge score | ||
|---|---|---|---|
| Lowest tertile | Middle tertile | Highest tertile | |
| Organ donor registration | |||
| Medical staff* (n=1008) | 1 [reference] | 0.90 (0.73–1.10) | 0.97 (0.77–1.22) |
| Non-medical staff** (n=182) | 1 [reference] | 0.68 (0.15–3.00) | 1.73 (0.65–4.59) |
| Willingness to donate organs after death | |||
| Medical staff* (n=1008) | 1 [reference] | 1.19 (1.00–1.43) | 1.31 (1.07–1.61) |
| Non-medical staff** (n=182) | 1 [reference] | 0.82 (0.43–1.53) | 2.04 (1.28–3.24) |
Modified Poisson regression analysis adjusted for age, sex, work experience in organ transplantation, family discussion about deceased organ donation, and willingness to donate organs after death;
Modified Poisson regression analysis adjusted for age, sex, work experience in organ transplantation, and family discussion about deceased organ donation.
CI – confidence interval.
Discussion
The present study found no association between high level of knowledge about deceased organ donation/transplantation and being a registered organ donor. However, the results showed that high knowledge level was associated with willingness to become an organ donor after death. These associations were observed within subgroups of participants stratified by occupation. The results suggest that increasing knowledge is essential, but not necessarily sufficient to narrow the gap between positive attitude and actual behavior among the hospital staff in Japan.
Although previous studies assessed the association between knowledge and attitude/behavior toward organ donation, their results varied widely and the issue remains controversial. For example, educational programs that provided knowledge were significantly associated with organ donor registration [20,21]. Especially, knowledge about the concept of brain death, the transplant allocation system and experiential knowledge of recipients were considered more influential than others in the donation decision-making process [28,45]. Several cross-sectional studies concluded that knowledge was associated with willingness to become an organ donor [27,29,31] and organ donor registration [22,32] after multivariate adjustment. Conversely, other studies showed no such association [24,30,33,46]. These discrepancies are related not only to the measurement of “knowledge”, which ranged from 1 to 32 questions, but also to different backgrounds and locations (countries), suggesting that the decision to become a donor may come into conflict with the prevailing knowledge.
In the present study, knowledge was not associated with organ donor registration. Moreover, the proportion of hospital staff who registered as organ donors was only 23%. Several factors are cited as the main barriers to donation of organs after death worldwide [47]. Although there is no qualitative study that investigated the barriers in detail in Japan, these can be explained in part by religious and cultural perspectives and mistrust about deceased organ transplantation [11,43,48,49]. First, it has been reported that Southeast Asians, including Japanese, are more reluctant to provide consent for organ donation than are white people [23,50]. Because the tradition of maintaining physical integrity of the body after death is prevalent, the majority of such subjects are less likely to register as an organ donor compared to those without such background [51–53]. This tradition is also maintained in Shinto, the most widespread religion in Japan [10,54]. A recent national survey in Japan reported that only 41.9% of the general population had a favorable view on deceased organ donation [55]. Second, there remains a tradition of not talking about death and dying because of death anxiety [12]. In the same national survey, only 35.4% of Japanese were reported to have discussed deceased organ donation with their families [55]. Third, there is a gap between attitude and behavior regarding deceased organ donation. The same survey also reported that only 12.7% had already registered as organ donors [55]. In this regard, the first heart transplantation performed in Japan in 1968 left a negative impact among the general public, a response markedly different from other Asian countries with high deceased organ donation rates. Because the operator was accused of using invalid criteria for the diagnosis of brain death of the donor and need for surgery of the recipient, that transplantation caused longstanding mistrust about deceased organ transplantation in Japan [56]. To narrow the gap between positive attitude and actual behavior, it is necessary that intensive care and emergency care professionals and donor coordinators receive standardized training and have discussions with the families of potential donors about cultural, religious, and historical backgrounds, in addition to public education [18,57].
Our study has several important strengths. First, to the best of our knowledge, it is the first to quantitatively assess the association between knowledge and attitude/behavior regarding deceased organ donation in a country with a low deceased organ donation rate. Second, all previous studies that identified knowledge as a significant predictor of attitude and behavior toward organ donation were exploratory in nature [22,27,29,31,32] and were designed to estimate the odds ratio, which always overestimates the relative risk ratio when the outcome is not rare [41]. Third, most previous studies examined the association of partial knowledge, such as the concept of brain death, and attitude/behavior regarding organ donation [27,29,31,32]. Fourth, we developed a new questionnaire on comprehensive knowledge about deceased organ donation and transplantation following the Delphi method and verified the internal consistency reliability and criterion validity among this population. Finally, we applied tertile analysis of knowledge scores. The reason for implementing this approach was based on previous studies, which commonly grouped participants based on predefined cut-off values of knowledge score into “+knowledge” and “−knowledge” [22,27,29–32]; such a methodology may not fully reflect the differences in the knowledge level.
Apart from the above strengths, our study has the following limitations. First, due to the cross-sectional design, we could not determine a temporal association or causal relationship. Second, the response rate remains a major concern for non-response bias, although approximately two-thirds of the staff responded to the survey. Third, we could not collect detailed information on the non-responders, although the age and sex of the entire group were similar to those of the eligible staff. Fourth, the outcome may not accurately reflect the actual behavior because of social desirability response bias among participants. Since all data were collected using the self-reported questionnaire, we could not directly confirm whether or not they actually registered as an organ donor [37]. However, the subjects were asked to select the modality that indicates consent for deceased organ donation when they responded by “Yes” to those questions. We also measured outcomes anonymously to alleviate this bias in any way possible. Fifth, we could not assess the test-retest reliability [58] or other validities, such as known-groups validity and predictive validity of the 20 questions. Sixth, we excluded subjects with missing data in the main analysis. Although this could potentially have resulted in selection bias [59], such individuals formed less than 7% of the total number of participants in this study. In addition, the results did not change, even after a sensitivity analysis with multiple imputation methods for missing values of adjustment covariates. Seventh, the non-medical staff constituted only 15.3% of the participants in our study. Although not statistically significant, the adjusted proportion ratio for organ donor registration was higher in the highest tertile of knowledge score compared with the lowest tertile among the non-medical staff. Further investigation with larger sample size is needed to clarify this relationship. Eighth, despite our attempts to reduce the impact of confounding in our results, there is likely residual bias. For example, we could not ask the participants about religious beliefs because the Ethics Review Committee of Saku Central Hospital Group did not approve this item. The final limitation is related to external validity. Because we recruited participants mainly among medical staff in a rural area in Japan to increase the response rate, one cannot generalize the findings to other hospital staff in other areas, or to other occupational groups or populations with different demographics. Although we need to confirm the generalizability of our study among these other populations in Japan in the next step of our investigation, medical staff plays an important role in the organ procurement process, and those who are more comfortable answering questions about organ donation from patients’ families will be more successful in obtaining consent [60].
Conclusions
The results of this cross-sectional study showed no association between high knowledge level about deceased organ donation and transplantation and organ donor registration among hospital staff in Japanese clinical facilities. However, the study identified significant association between knowledge and willingness to donate organs after death. These findings suggest that providing knowledge is essential, but not necessarily enough to narrow the gap between positive attitude and actual behavior in deceased organ donation. Effective strategies based on the prevailing religious, cultural, and historical backgrounds may be helpful in closing this gap in Japan.
Supplementary Data
Supplementary Table 1.
Association (adjusted proportion ratio and 95% CI) of characteristics of study participants with attitude and behavior toward deceased organ donation.
| Characteristics | Organ donor registration* | Willingness to donate organs after death* |
|---|---|---|
| Age per 1 year | 1.00 (0.99–1.00) | 0.99 (0.98–0.99) |
| Female sex (vs. Male sex) | 1.03 (0.84–1.27) | 0.85 (0.72–0.99) |
| Occupation | ||
| Experienced medical staff (vs. non-medical staff) | 2.27 (1.47–3.51) | 1.00 (0.76–1.31) |
| Non-experienced medical staff (vs. non-medical staff) | 1.99 (1.31–3.02) | 1.11 (0.88–1.39) |
| Family discussion about deceased organ donation | 1.92 (1.53–2.40) | 2.14 (1.83–2.50) |
| Willingness to donate organs after death | 5.97 (4.47–7.97) | – |
Modified Poisson regression analysis adjusted for the above participants’ characteristics.
Supplementary Table 2.
Sensitivity analysis of association (adjusted proportion ratio and 95% CI) between knowledge score and attitude and behavior toward deceased organ donation based on cutoff points of knowledge score.
| Outcomes | Knowledge score | ||
|---|---|---|---|
| ≤12 (n=304) | 13–16 (n=771) | 17–20 (n=115) | |
| Organ donor registration* | 1 [reference] | 0.92 (0.73–1.17) | 0.94 (0.69–1.28) |
| Willingness to donate organs after death** | 1 [reference] | 1.26 (1.04–1.53) | 1.59 (1.22–2.08) |
Modified Poisson regression analysis adjusted for age, sex, occupation (medical or non-medical staff), work experience in organ transplantation, family discussion about deceased organ donation, and willingness to donate organs after death;
Modified Poisson regression analysis adjusted for age, sex, occupation (medical or non-medical staff), work experience in organ transplantation, and family discussion about deceased organ donation.
CI – confidence interval.
Supplementary Table 3.
Sensitivity analysis of association (adjusted proportion ratio and 95% CI) between knowledge score and attitude and behavior toward deceased organ donation after multiple imputation.
| Outcomes | Knowledge score | ||
|---|---|---|---|
| Lowest tertile (n=534) | Middle tertile (n=446) | Highest tertile (n=264) | |
| Organ donor registration* | 1 [reference] | 0.92 (0.75–1.13) | 0.99 (0.79–1.23) |
| Willingness to donate organs after death** | 1 [reference] | 1.19 (1.01–1.41) | 1.39 (1.15–1.67) |
Multiple imputation for missing covariate variables was used.
Modified Poisson regression analysis adjusted for age, sex, occupation (medical or non-medical staff), work experience in organ transplantation, family discussion about deceased organ donation, and willingness to donate organs after death;
Modified Poisson regression analysis adjusted for age, sex, occupation (medical or non-medical staff), work experience in organ transplantation, and family discussion about deceased organ donation.
CI – confidence interval.
Acknowledgments
We thank all staff of Saku Central Hospital Group.
Footnotes
Source of support: This study was supported by the internal budget of the Saku Central Hospital Group
References
- 1.Rana A, Gruessner A, Agopian VG, et al. Survival benefit of solid-organ transplant in the United States. JAMA Surg. 2015;150:252–59. doi: 10.1001/jamasurg.2014.2038. [DOI] [PubMed] [Google Scholar]
- 2.Haller M, Gutjahr G, Kramar R, et al. Cost-effectiveness analysis of renal replacement therapy in Austria. Nephrol Dial Transplant. 2011;26:2988–95. doi: 10.1093/ndt/gfq780. [DOI] [PubMed] [Google Scholar]
- 3.Wolfe RA, Roys EC, Merion RM. Trends in organ donation and transplantation in the United States, 1999–2008. Am J Transplant. 2010;10:961–72. doi: 10.1111/j.1600-6143.2010.03021.x. [DOI] [PubMed] [Google Scholar]
- 4.Wynn JJ, Alexander CE. Increasing organ donation and transplantation: The U.S. experience over the past decade. Transpl Int. 2011;24:324–32. doi: 10.1111/j.1432-2277.2010.01201.x. [DOI] [PubMed] [Google Scholar]
- 5.The World Health Organization and the Spanish Transplant Organization. Global Observatory on Organ Donation and Transplantation. Available from: URL: http://www.transplant-observatory.org/
- 6.The Japan Society for Transplantation. Fact book 2018 of organ transplantation in Japan. Available from: URL: http://www.asas.or.jp/jst/pdf/factbook/factbook2018.pdf.
- 7.Hart A, Smith JM, Skeans MA, et al. OPTN/SRTR 2017 annual data report: Kidney. Am J Transplant. 2019;19(Suppl 2):19–123. doi: 10.1111/ajt.15274. [DOI] [PubMed] [Google Scholar]
- 8.Donation & Transplantation Institute. International Registry in Organ Donation and Transplantation. Available from: URL: http://www.irodat.org/?p=database.
- 9.Japan Organ Transplant Network. Available from: URL: https://www.jotnw.or.jp/
- 10.Da Silva IR, Frontera JA. Worldwide barriers to organ donation. JAMA Neurol. 2015;72:112–18. doi: 10.1001/jamaneurol.2014.3083. [DOI] [PubMed] [Google Scholar]
- 11.Webb G, Phillips N, Reddiford S, Neuberger J. Factors affecting the decision to grant consent for organ donation: a survey of adults in England. Transplantation. 2015;99:1396–402. doi: 10.1097/TP.0000000000000504. [DOI] [PubMed] [Google Scholar]
- 12.Li MT, Hillyer GC, Husain SA, Mohan S. Cultural barriers to organ donation among Chinese and Korean individuals in the United States: A systematic review. Transplant Int. 2019;32:1001–18. doi: 10.1111/tri.13439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cameron AM, Massie AB, Alexander CE, et al. Social media and organ donor registration: The Facebook effect. Am J Transplant. 2013;13:2059–65. doi: 10.1111/ajt.12312. [DOI] [PubMed] [Google Scholar]
- 14.Sandroni C, D’Arrigo S, Callaway CW, et al. The rate of brain death and organ donation in patients resuscitated from cardiac arrest: A systematic review and meta-analysis. Intensive Care Med. 2016;42:1661–71. doi: 10.1007/s00134-016-4549-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmad MU, Hanna A, Mohamed AZ, et al. A Systematic review of opt-out versus opt-in consent on deceased organ donation and transplantation (2006–2016) World J Surg. 2019;43:3161–71. doi: 10.1007/s00268-019-05118-4. [DOI] [PubMed] [Google Scholar]
- 16.Witjes M, Jansen NE, van der Hoeven JG, Abdo WF. Interventions aimed at healthcare professionals to increase the number of organ donors: A systematic review. Crit Care. 2019;23:227. doi: 10.1186/s13054-019-2509-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abidin ZL, Ming WT, Loch A, et al. Are health professionals responsible for the shortage of organs from deceased donors in Malaysia? Transpl Int. 2013;26:187–94. doi: 10.1111/tri.12019. [DOI] [PubMed] [Google Scholar]
- 18.Matesanz R, Dominguez-Gil B, Coll E, et al. How spain reached 40 deceased organ donors per million population. Am J Transplant. 2017;17:1447–54. doi: 10.1111/ajt.14104. [DOI] [PubMed] [Google Scholar]
- 19.Jawoniyi O, Gormley K, McGleenan E, Noble HR. Organ donation and transplantation: Awareness and roles of healthcare professionals-A systematic literature review. J Clin Nurs. 2018;27:e726–38. doi: 10.1111/jocn.14154. [DOI] [PubMed] [Google Scholar]
- 20.Li AH, Rosenblum AM, Nevis IF, Garg AX. Adolescent classroom education on knowledge and attitudes about deceased organ donation: A systematic review. Pediatr Transplant. 2013;17:119–28. doi: 10.1111/petr.12045. [DOI] [PubMed] [Google Scholar]
- 21.Deedat S, Kenten C, Morgan M. What are effective approaches to increasing rates of organ donor registration among ethnic minority populations: A systematic review. BMJ Open. 2013;3:e003453. doi: 10.1136/bmjopen-2013-003453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schaeffner ES, Windisch W, Freidel K, et al. Knowledge and attitude regarding organ donation among medical students and physicians. Transplantation. 2004;77:1714–18. doi: 10.1097/00007890-200406150-00015. [DOI] [PubMed] [Google Scholar]
- 23.Roels L, Spaight C, Smits J, Cohen B. Critical Care staffs’ attitudes, confidence levels and educational needs correlate with countries’ donation rates: Data from the Donor Action database. Transpl Int. 2010;23:842–50. doi: 10.1111/j.1432-2277.2010.01065.x. [DOI] [PubMed] [Google Scholar]
- 24.Marck CH, Weiland TJ, Neate SL, et al. Australian emergency doctors’ and nurses’ acceptance and knowledge regarding brain death: A national survey. Clin Transplant. 2012;26:E254–60. doi: 10.1111/j.1399-0012.2012.01659.x. [DOI] [PubMed] [Google Scholar]
- 25.Murakami M, Fukuma S, Ikezoe M, et al. Effect of an educational program on attitudes towards deceased organ donation. Ann Transplant. 2015;20:269–78. doi: 10.12659/AOT.893325. [DOI] [PubMed] [Google Scholar]
- 26.Hu D, Huang H. Knowledge, attitudes, and willingness toward organ donation among health professionals in China. Transplantation. 2015;99:1379–85. doi: 10.1097/TP.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 27.Fontana F, Massari M, Giovannini L, et al. Knowledge and attitudes toward organ donation in health care undergraduate students in Italy. Transplant Proc. 2017;49:1982–87. doi: 10.1016/j.transproceed.2017.09.029. [DOI] [PubMed] [Google Scholar]
- 28.Rasiah R, Manikam R, Chandrasekaran SK, et al. Deceased donor organs: What can be done to raise donation rates using evidence from Malaysia? Am J Transplant. 2016;16:1540–47. doi: 10.1111/ajt.13603. [DOI] [PubMed] [Google Scholar]
- 29.Rios A, Cascales P, Martinez L, et al. Emigration from the British Isles to Southeastern Spain: A study of attitudes toward organ donation. Am J Transplant. 2007;7:2020–30. doi: 10.1111/j.1600-6143.2007.01879.x. [DOI] [PubMed] [Google Scholar]
- 30.Chung J, Choi D, Park Y. Knowledge and opinions of deceased organ donation among middle and high school students in Korea. Transplant Proc. 2015;47:2805–9. doi: 10.1016/j.transproceed.2015.09.057. [DOI] [PubMed] [Google Scholar]
- 31.Conesa C, Rios Zambudio A, Ramirez P, et al. Socio-personal profile of teenagers opposed to organ donation. Nephrol Dial Transplant. 2004;19:1269–75. doi: 10.1093/ndt/gfh075. [DOI] [PubMed] [Google Scholar]
- 32.Figueroa CA, Mesfum ET, Acton NT, Kunst AE. Medical students’ knowledge and attitudes toward organ donation: Results of a Dutch survey. Transplant Proc. 2013;45:2093–97. doi: 10.1016/j.transproceed.2013.02.135. [DOI] [PubMed] [Google Scholar]
- 33.Rios A, Lopez-Navas AI, Navalon JC, et al. The Latin American population in Spain and organ donation. Attitude toward deceased organ donation and organ donation rates. Transpl Int. 2015;28:437–47. doi: 10.1111/tri.12511. [DOI] [PubMed] [Google Scholar]
- 34.Murakami M, Komatsu H, Sugiyama M, et al. Antimicrobial stewardship without infectious disease physician for patients with candidemia: A before and after study. J Gen Fam Med. 2018;19:82–89. doi: 10.1002/jgf2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones J, Hunter D. Qualitative research: Consensus methods for medical and health services research. BMJ. 1995;311:376–80. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosaasen N, Taylor J, Blackburn D, et al. Development and validation of the kidney transplant understanding tool (K-TUT) Transplant Direct. 2017;3:e132. doi: 10.1097/TXD.0000000000000647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murakami M, Fukuma S, Ikezoe M, et al. Effects of structured education program on organ donor designation of nursing students and their families: A randomized controlled trial. Clin Transplant. 2016;30:1513–19. doi: 10.1111/ctr.12845. [DOI] [PubMed] [Google Scholar]
- 38.Bland JM, Altman DG. Cronbach’s alpha. BMJ. 1997;314:572. doi: 10.1136/bmj.314.7080.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hays R, Anderson R, Revicki DA. Assessing reliability and validity of measurement in clinical trials. In: Staquet MJ, Hays RD, Fayers PM, editors. Quality of life assessment in clinical trials. New York: Oxford Medical Publications; 1998. [Google Scholar]
- 40.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 41.Norton EC, Dowd BE, Maciejewski ML. Odds ratios-current best practice and use. JAMA. 2018;320:84–85. doi: 10.1001/jama.2018.6971. [DOI] [PubMed] [Google Scholar]
- 42.McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–43. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 43.Wakefield CE, Watts KJ, Homewood J, et al. Attitudes toward organ donation and donor behavior: A review of the international literature. Prog Transplant. 2010;20:380–91. doi: 10.1177/152692481002000412. [DOI] [PubMed] [Google Scholar]
- 44.Li AH, Dixon S, Prakash V, et al. Physician registration for deceased organ donation. JAMA. 2014;312:291–93. doi: 10.1001/jama.2014.2934. [DOI] [PubMed] [Google Scholar]
- 45.Jacob Arriola KR, Robinson DH, et al. Understanding the relationship between knowledge and African Americans’ donation decision-making. Patient Educ Couns. 2008;70:242–50. doi: 10.1016/j.pec.2007.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ibrahim M, Randhawa G. Knowledge, attitudes, and behavior of Nigerian students toward organ donation. Transplant Proc. 2017;49:1691–97. doi: 10.1016/j.transproceed.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 47.Bendorf A, Pussell BA, Kelly PJ, Kerridge IH. Socioeconomic, demographic and policy comparisons of living and deceased kidney transplantation rates across 53 countries. Nephrology (Carlton) 2013;18:633–40. doi: 10.1111/nep.12101. [DOI] [PubMed] [Google Scholar]
- 48.Irving MJ, Tong A, Jan S, et al. Factors that influence the decision to be an organ donor: A systematic review of the qualitative literature. Nephrol Dial Transplant. 2012;27:2526–33. doi: 10.1093/ndt/gfr683. [DOI] [PubMed] [Google Scholar]
- 49.Irving MJ, Jan S, Tong A, et al. What factors influence people’s decisions to register for organ donation? The results of a nominal group study. Transpl Int. 2014;27:617–24. doi: 10.1111/tri.12307. [DOI] [PubMed] [Google Scholar]
- 50.Thornton JD, Wong KA, Cardenas V, et al. Ethnic and gender differences in willingness among high school students to donate organs. J Adolesc Health. 2006;39:266–74. doi: 10.1016/j.jadohealth.2005.12.028. [DOI] [PubMed] [Google Scholar]
- 51.Davison SN, Jhangri GS. Knowledge and attitudes of Canadian first nations people toward organ donation and transplantation: A quantitative and qualitative analysis. Am J Kidney Dis. 2014;64:781–89. doi: 10.1053/j.ajkd.2014.06.029. [DOI] [PubMed] [Google Scholar]
- 52.Marvan ML, Alvarez Del Rio A, Jasso K, Santillan-Doherty P. Psychosocial barriers associated with organ donation in Mexico. Clin Transplant. 2017;31:e13112. doi: 10.1111/ctr.13112. [DOI] [PubMed] [Google Scholar]
- 53.Rios A, Lopez-Navas AI, Garcia JA, et al. The attitude of Latin American immigrants in Florida (USA) towards deceased organ donation – a cross section cohort study. Transpl Int. 2017;30:1020–31. doi: 10.1111/tri.12997. [DOI] [PubMed] [Google Scholar]
- 54.Oliver M, Woywodt A, Ahmed A, Saif I. Organ donation, transplantation and religion. Nephrol Dial Transplant. 2011;26:437–44. doi: 10.1093/ndt/gfq628. [DOI] [PubMed] [Google Scholar]
- 55.Cabinet Office, Government of Japan. Opinion poll on organ transplantation. Available from: URL: https://survey.gov-online.go.jp/h29/h29-ishoku/index.html.
- 56.The Japanese Circulation Society. Statement for heart transplantation. 2016. Available from: URL: http://www.j-circ.or.jp/guideline/pdf/JCS2016_isobe_h.pdf.
- 57.Traino HM, Molisani AJ, Siminoff LA. Regional differences in communication process and outcomes of requests for solid organ donation. Am J Transplant. 2017;17:1620–27. doi: 10.1111/ajt.14165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19:231–40. doi: 10.1519/15184.1. [DOI] [PubMed] [Google Scholar]
- 59.van der Heijden GJ, Donders AR, Stijnen T, Moons KG. Imputation of missing values is superior to complete case analysis and the missing-indicator method in multivariable diagnostic research: A clinical example. J Clin Epidemiol. 2006;59:1102–9. doi: 10.1016/j.jclinepi.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 60.Siminoff LA, Gordon N, Hewlett J, Arnold RM. Factors influencing families’ consent for donation of solid organs for transplantation. JAMA. 2001;286:71–77. doi: 10.1001/jama.286.1.71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1.
Association (adjusted proportion ratio and 95% CI) of characteristics of study participants with attitude and behavior toward deceased organ donation.
| Characteristics | Organ donor registration* | Willingness to donate organs after death* |
|---|---|---|
| Age per 1 year | 1.00 (0.99–1.00) | 0.99 (0.98–0.99) |
| Female sex (vs. Male sex) | 1.03 (0.84–1.27) | 0.85 (0.72–0.99) |
| Occupation | ||
| Experienced medical staff (vs. non-medical staff) | 2.27 (1.47–3.51) | 1.00 (0.76–1.31) |
| Non-experienced medical staff (vs. non-medical staff) | 1.99 (1.31–3.02) | 1.11 (0.88–1.39) |
| Family discussion about deceased organ donation | 1.92 (1.53–2.40) | 2.14 (1.83–2.50) |
| Willingness to donate organs after death | 5.97 (4.47–7.97) | – |
Modified Poisson regression analysis adjusted for the above participants’ characteristics.
Supplementary Table 2.
Sensitivity analysis of association (adjusted proportion ratio and 95% CI) between knowledge score and attitude and behavior toward deceased organ donation based on cutoff points of knowledge score.
| Outcomes | Knowledge score | ||
|---|---|---|---|
| ≤12 (n=304) | 13–16 (n=771) | 17–20 (n=115) | |
| Organ donor registration* | 1 [reference] | 0.92 (0.73–1.17) | 0.94 (0.69–1.28) |
| Willingness to donate organs after death** | 1 [reference] | 1.26 (1.04–1.53) | 1.59 (1.22–2.08) |
Modified Poisson regression analysis adjusted for age, sex, occupation (medical or non-medical staff), work experience in organ transplantation, family discussion about deceased organ donation, and willingness to donate organs after death;
Modified Poisson regression analysis adjusted for age, sex, occupation (medical or non-medical staff), work experience in organ transplantation, and family discussion about deceased organ donation.
CI – confidence interval.
Supplementary Table 3.
Sensitivity analysis of association (adjusted proportion ratio and 95% CI) between knowledge score and attitude and behavior toward deceased organ donation after multiple imputation.
| Outcomes | Knowledge score | ||
|---|---|---|---|
| Lowest tertile (n=534) | Middle tertile (n=446) | Highest tertile (n=264) | |
| Organ donor registration* | 1 [reference] | 0.92 (0.75–1.13) | 0.99 (0.79–1.23) |
| Willingness to donate organs after death** | 1 [reference] | 1.19 (1.01–1.41) | 1.39 (1.15–1.67) |
Multiple imputation for missing covariate variables was used.
Modified Poisson regression analysis adjusted for age, sex, occupation (medical or non-medical staff), work experience in organ transplantation, family discussion about deceased organ donation, and willingness to donate organs after death;
Modified Poisson regression analysis adjusted for age, sex, occupation (medical or non-medical staff), work experience in organ transplantation, and family discussion about deceased organ donation.
CI – confidence interval.


