Abstract
Objectives
To evaluate the effect of the sodium-glucose cotransporter 2 inhibitor (SGLT2-I) dapagliflozin on endothelial function in patients with high-risk type 2 diabetes mellitus (T2DM).
Methods
This was a prospective, double-blind, randomized, placebo-controlled, clinical trial of patients with T2DM with underlying ischemic heart disease who were receiving metformin and insulin therapy (n = 81). After 12-weeks of additional therapy with either dapagliflozin (n = 40) or placebo (n = 41), systemic endothelial function was evaluated by change in flow-mediated dilation (ΔFMD), change in nitroglycerin-mediated dilation (ΔNMD) and surrogate markers including intercellular adhesion molecule 1 (ICAM-1), endothelial nitric oxide synthase (eNOS), high-sensitivity C-reactive protein (hs-CRP), and lipoprotein(a) (Lp[a]). Glycemic and lipid profiles were also measured.
Results
The dapagliflozin group demonstrated significant reductions of hemoglobin A1c (HbA1c) and fasting blood glucose (FBG) compared to the placebo group (ΔHbA1c –0.83 ± 1.47% vs –0.16 ± 1.25%, P = 0.042 and ΔFBG vs –0.73 ± 4.55 mmol/L vs –1.90 ± 4.40 mmol/L, P = 0.015, respectively). The placebo group showed worsening of ΔFMD while the dapagliflozin group maintained similar measurements pre- and posttherapy (P = not significant). There was a reduction in ICAM-1 levels in the dapagliflozin group (–83.9 ± 205.9 ng/mL, P < 0.02), which remained unchanged in the placebo group (–11.0 ± 169.1 ng/mL, P = 0.699). Univariate correlation analysis revealed a significant negative correlation between HbA1c and ΔFMD within the active group.
Conclusion
A 12-week therapy with dapagliflozin, in addition to insulin and metformin therapies, in high-risk patients resulted in significant reductions in HbA1c, FBG, and surrogate markers of the endothelial function. Although the dapagliflozin group demonstrated a significant association between reduction in HbA1c and improvement in FMD, there was no significant difference in FMD between the 2 groups.
1. Introduction
Type 2 diabetes mellitus (T2DM) is a major risk factor for accelerated cardiovascular disease (CVD) and atherosclerosis development [1]. The diabetes-associated cardiovascular mortality rate exceeds 70% and is 2- to 4-fold higher in patients with T2DM than those without the disease [2]. The progression of insulin resistance in T2DM accelerates the development of endothelial dysfunction, which has been shown to be associated with increased cardiovascular risk [3].
Flow-mediated dilation (FMD) of the peripheral arteries such as the brachial artery, is one of the most widely used tests of endothelial dysfunction in macrocirculation [4]. FMD measurements of the peripheral vessels correlate well with coronary artery endothelial functions [5]. In addition to detecting subclinical atherosclerosis, the role of FMD in advanced disease had been emerging in recent years. Several studies that cumulatively involved approximately 2000 subjects showed that FMD was able to independently predict and prognosticate cardiac events in patients with moderate to high risk of CVD [6]. FMD also independently predicted restenosis in patients who had received bare-metal or drug-eluting stents [7]. A meta-analysis suggested that for every 1% increase in FMD there was a 13% (95% confidence interval: 9%–17%) decrease in the future risk of cardiovascular events [8].
To differentiate endothelium-dependent from endothelium-independent responses, exogenous nitric oxide donators (eg, glycerol-trinitrate) can be applied, called nitroglycerin-mediated dilation (NMD). The impaired endothelial-independent function is associated with structural vascular alterations and changes in smooth muscle cells rather than in the endothelium [9]. NMD can be a marker of anatomical coronary abnormality; a weaker response of NMD had been observed in patients with CVD and had been associated with the presence and quantity of calcium within the coronary artery in asymptomatic adults [10]. Both brachial FMD as well as NMD is an independent predictor of long-term cardiovascular events [11].
Previous studies have shown that oral hypoglycemic agents may play roles in improving endothelial function beyond their glycemic control. Metformin was the first antidiabetic drug that showed an improvement in FMD following 3 months of therapy compared to placebo [12]. Subsequently, dipeptidyl peptidase-4 inhibitors (DPP4-Is) have been extensively studied. In a single-arm study, sitagliptin showed an improvement in FMD measurements in moderately controlled patients with T2DM, in addition to an improvement of glycated hemoglobin (HbA1c) within 12 weeks of therapy [13].
Sodium-glucose cotransporter 2 inhibitors (SGLT2-I) are a relatively new class of oral antidiabetic agents with promising cardiovascular benefits [14]. Its effects include a reduction in body weight, blood pressure, serum triglyceride levels, visceral fat, and uric acid, as well as arterial stiffness improvement [15]. The cardiovascular safety profile of dapagliflozin had been shown in a meta-analysis and showed no increase in major cardiovascular events [16]. More recently, the DEFENCE study demonstrated significant improvement in endothelial function with dapagliflozin in patients with HbA1c >7% (53 mmol/mol) [17]. However, the study excluded patients with a known history of cardiovascular diseases.
To date, there has been no clear evidence to confirm the protective role of SGLT2-Is on endothelial function or their ability to suppress the progression of atherosclerosis. In view of the plausible effects of SGLT2-Is on vascular function and atherosclerosis, this study was therefore designed to evaluate the effects of dapagliflozin on endothelial function as assessed by FMD and other inflammatory markers in patients with T2DM and established CVD.
2. Materials and Methods
A. Participants
Eighty-one (58 male and 23 female) participants were recruited between May 1, 2016, and March 15, 2017, from outpatient cardiology and endocrine clinics in the Clinical Training Centre, University Technology Mara, Sungai Buloh and Medical Faculty University Technology Mara, Selayang Campus, Malaysia. Eligibility included (1) type 2 diabetes, on stable doses of subcutaneous insulin and/or metformin, for more than 6 months; (2) established ischemic heart disease; (3) HbA1c of ≥7.0% (53 mmol/mol) and <10.5% (91 mmol/mol) and (4) age 30 to 75 years. Exclusion criteria included (1) type 1 or secondary diabetes; (2) prior use of SGLT2-Is or glucagon-like peptide (GLP-1) agonists; (3) occurrence of acute coronary events within the past 3 months; (4) serious liver or renal functional diseases (calculated creatinine clearance of <60 ml/min/1.73 m2); (5) frequent hypoglycemia; (6) recurrent urinary tract or genital infections; (7) moderate or severe cardiac insufficiency, that is, New York Heart Association class III and IV; (8) dehydration; and (9) hypersensitivity to SGLT2-Is and GLP-1 agonists. The Institutional Review Board at the University Technology MARA, Malaysia, approved the study, and all participants gave verbal and written consent. This clinical trial registration number is given 100-IRMI/PRI 16/6/2 (007/2017). This clinical trial study was conducted in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki).
B. Protocols
Participants were randomized in a double-blinded, balanced, crossover fashion to oral consumption of either dapagliflozin 10 mg/day (n = 40) (DAPA group) or matching placebo (n = 41) (placebo group) in addition to diet, exercise, insulin, and/or metformin therapies. The randomization was achieved by stratified randomization. Subjects were stratified according to HbA1c < 9% and HbA1c ≥ 9% and genders. Four separate blocks were generated, and all subjects have been identified and assigned to the blocks. Simple randomization was performed within each block to assign subjects to one of the groups. The medication was prepared and packaged by AstraZeneca and disbursed by a dedicated research assistant. All patients were required to maintain the doses of concomitant drugs without any additional drugs during the 12-week study period. Baseline measurements of blood and urine variables and FMD were performed during the 2 to 4 weeks of the screening period. After baseline data collection, the assigned therapies were started. The treatment intervention date was set as the study start date. The assigned treatment was continued for 16 weeks (duration of the study). Background therapy to all study participants in both arms included insulin with metformin accompanied by standard advice for a diabetic diet and physical activities. Insulin therapy included both human and recombinant insulin, ranging between once to 4 times daily, with a total dose of between 0.5 u-2 u/kg/day. All patients were required to perform home blood glucose monitoring at least 3 times per week. Any episode of symptomatic hypoglycemia and asymptomatic hypoglycemia (absence of symptoms but with glucose < 3.9 mmol/L) needed to be recorded by the patient. Patients were instructed to titrate their insulin doses to achieve the glycemic targets based on a titration schedule.
C. Biochemical Analyses
Blood and urine samples were obtained in sterile containers at baseline and at study end. All blood samples were centrifuged at 3500 rpm for 7 minutes to extract serum and plasma samples, which were kept frozen at –20°C until laboratory testing at an ISO 15189:2007 accredited laboratory (SAMM 688) located at Center Of Pathology Diagnostics and Research Laboratories (CPDRL), UiTM Sungai Buloh. Fasting blood glucose (FBG) was analyzed using the hexokinase method, while total cholesterol (TC), triglyceride (TG) and high-density lipoprotein–cholesterol (HDL-C) were measured by enzymatic reference methods. FBG, TC, TG, HDL-C, lipoprotein(a)(Lp[a]), [18] and high-sensitivity C-reactive protein (hs-CRP) [19] were measured on an automated analyzer (Cobas Integra 400 PLUS, Roche Diagnostics, Germany). LDL-C was derived using the Friedewald equation. HbA1c were analyzed using the Biorad D10 machine (Bio-Rad Laboratories, Singapore). Serum intercellular adhesion molecule-1 (ICAM-1) [20] and endothelial nitric oxide synthase (eNOS) [21] concentrations were measured by enzyme-linked immunosorbent assay (eBioscience Bender MedSystems, Vienna Austria). All absorbance was read on a microplate reader (Tecan Sapphire II, Austria). In addition to these parameters, other biochemical safety parameters (eg, red blood cell count and hematocrit) were measured.
D. Measurement of Flow-Mediated Dilation
After an overnight fast of 12 hours, FMD and NMD were measured using an ultrasound machine (Model GE VIVID S5 [SCHMIDT BioMedTech Sdn Bhd, Malaysia] 5-12-MHz linear array transducer) by trained personnel who were blinded to the treatment groups. The brachial artery was scanned in longitudinal sections 2 to 10 cm above the elbow (control scan) after 15 minutes’ rest in the supine position. The depth and gain settings were optimized to identify the anterior and posterior intimal interfaces between the lumen and vessel wall. A view of a 5-cm transverse section of the brachial artery was recorded for periods of 30 seconds at baseline and during peak reactive hyperemia (after deflation of the blood pressure cuff previously inflated at 50 mmHg above the systolic blood pressure around the forearm). The vasodilator response to hyperemia was recorded for 5 minutes after deflation. Following 10 minutes of rest, a further control scan was performed and recorded. A single 500-μg dose of glyceryl trinitrate (GTN) was administered sublingually. Thereafter, the vasodilator response to GTN was recorded for 15 minutes. Mean diameter measurements were calculated from 3 different cardiac cycles. FMD and NMD were expressed as a percentage change relative to the diameter before cuff inflation and before drug administration, respectively. Maximal diameter responded to hyperemia and GTN was used to calculate FMD and NMD. The variability for repeated measurements of resting arterial diameter was 0.32±0.72 mm.
For the reference of a normal FMD value, according to a study in Finland, the mean [SD] FMD was 7.0% [4.0%] for men and 8.8% [4.6%] for women based on 2109 healthy Finnish adults aged 24 to 39 years [22]. A small population study (160 subjects) showed FMD [SD] of patients with non-CVD, cardiovascular risk factors, and acute myocardial infarction of 7.8% [3.1%], 5% [2.6%], and 3.3% [3%], respectively [23]. Some previous papers have defined endothelial dysfunction as FMD less than 3% [24, 25].
Average glyceryl trinitrate-induced dilatation (NMD) [SD] in the normal healthy population was 19.2% [6.6%] (range 8.5–38.7) and was also inversely related to vessel size. A study examining 181 Japanese patients with T2DM showed the NMD level in patients with T2DM with microangiopathy was significantly lower than that in patients without microangiopathy (12.1 ± 6.3% vs 15.7 ± 6.4%; P = 0.001) [8].
E. Study Outcomes
The primary study outcome was a change in FMD (ΔFMD [ = value FMD at week 12 − value FMD at baseline]) and change in NMD (ΔNMD [ = value NMD at week 12 − value NMD at baseline]). Secondary endpoints included changes in the values of the following items at the end of the 12-week treatment, relative to the baseline: (1) ICAM-1, eNOS, Lp(a), and hs-CRP; (2) indexes of glycemic control: HbA1c and FBG levels; (3) indexes of lipid metabolism: total cholesterol, HDL-cholesterol, LDL-cholesterol, and triglyceride (TG); (4) indexes of hemodynamic and metabolic changes: weight, body mass index (BMI), waist circumference, and blood pressure.
F. Safety and Evaluation of Adverse Events
During the course of the study, symptoms and signs and all other adverse events (AEs) were constantly monitored. When AEs occurred, details were reported immediately. All related AEs, not only side effects to the drug but also abnormal values from the clinical tests, were reported and documented.
G. Statistical Analysis
Sample size calculation was based on a previous study, which showed an attenuation of FMD [SD] with sitagliptin 4.13% [1.59%] vs 5.12% [1.55%]; P < 0.001 and an attenuation of 7.2% to 4.3% P < 0.001 with an average of 1.5% attenuation [27]. Based on the assumption that dapagliflozin would be able to produce an effect of 1%, the number of cases required to detect a significant difference in ∆FMD between the 2 groups under the conditions of a two-sided P value of 5% and power of 85% was 36 patients per group with a total sample size of 72. Assuming a dropout rate of 10%, the target number of patients was therefore set to 40 cases per group, with a total of 80 cases.
Statistical package for the social sciences (SPSS) for Windows Version 24.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analysis. Continuous data that were normally distributed were presented as mean and SD (mean ± SD), while not normally distributed data were described as median interquartile range. Categorical data were presented as numbers of patients and percentages (n, %). Within-group comparisons were performed using a paired samples t test or Wilcoxon signed-rank test for normally and non-normally distributed data, respectively. Between-group comparisons were performed using an independent samples t test or Mann-Whitney U test for normally and non-normally distributed data, respectively. Chi-square test or Fisher exact tests were performed for categorical variables.
3. Results
A. Baseline Characteristics
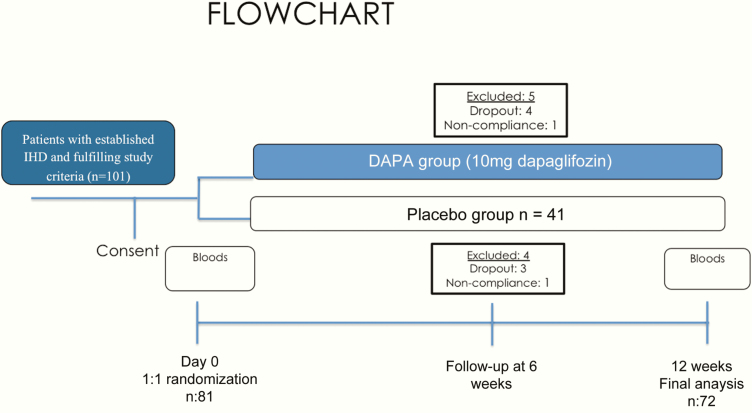
A total of 81 patients were enrolled in this study between May 1, 2016, until March 15, 2017. Nine patients were excluded due to noncompliance to study medication and were lost to follow-up (Fig. 1). Baseline demographics are demonstrated in Table 1 which showed no significant difference between the 2 groups apart from BMI. Most patients were obese with higher mean BMI in the placebo group (29.85 ± 4.23 kg/m2 vs 27.49 ± 4.10 kg/m2; P = 0.021). Notably, the mean duration of T2DM was approximately 9.5 years, and the mean HbA1c was approximately 9% (75 mmol/mol) in both groups. Both groups demonstrated well-controlled systolic and diastolic blood pressures and normal estimated glomerular filtration rates. Most patients had more than 2 diseased vessels, which suggested advanced atherosclerosis. A majority of patients were on metformin therapy, with similar mean daily insulin doses in both groups (Table 1).
Figure 1.
Study Protocol. Abbreviations: DAPA, dapagliflozin; IHD, ischaemic heart disease.
Table 1.
Baseline Demographic and Clinical Characteristics of Patients
| Characteristic | DAPA (n = 36) | Placebo (n = 36) | P |
|---|---|---|---|
| Age, mean (years) | 57.25 ± 8.49 | 58.00 ± 7.32 | 0.689 |
| Sex(male/female) | 28 (77.8)/8 (22.2) | 27 (75)/9 (25) | 0.5 |
| Race | |||
| Malayasian | 24 (66.7) | 17 (47.2) | 0.12 |
| Chinese | 5 (13.9) | 4 (8.3) | |
| Indian | 7 (19.4) | 15 (41.7) | |
| Duration of DM, years | 8.94 ± 6.62 | 10.72 ± 6.58 | 0.26 |
| Current smokers | 6 (16.7) | 3 (8.4) | 0.288 |
| On metformin | 33 (91.7) | 32 (88.9) | 0.689 |
| IHD >2VD | 22 (61.1) | 24 (66.7) | 0.49 |
| Treatment IHD | |||
| CABG | 7 (19.4) | 13 (36.1) | |
| Stent | 14 (38.9) | 19 (52.7) | |
| Medical therapy | 15 (41.7) | 4 (11.1) | |
| BMI, kg/m2 | 27.49 ± 4.10 | 29.85 ± 4.23 | 0.021 |
| Weight, kg | 76.18 ± 9.08 | 79.4 ± 14.60 | 0.352 |
| Waist circumference, cm | 96.10 ± 8.28 | 97.59 ± 8.56 | 0.455 |
| SBP, mmHg | 140.92 ± 22.07 | 141.06 ± 21.61 | 0.978 |
| DBP, mmHg | 78.31 ± 11.17 | 77.86 ± 12.78 | 0.875 |
| HbA1c, % | 9.66 ± 1.86 | 9.31 ± 1.58 | 0.397 |
| Fasting plasma glucose, mmol/L | 10.69 ± 4.551 | 9.58 ± 4.024 | 0.275 |
| eGFR, mL/min/1.73 m2 | 85.24 ± 18.69 | 82.31 ± 15.66 | 0.474 |
| Diabetic nephropathy, n | 22 (61.1) | 18 (50) | 0.341 |
| UACR 30–299 mg/g | 17 (48.6) | 14 (38.9) | 0.477 |
| UACR ≥ 300 mg/g | 5 (13.9) | 3 (8.3) | 0.478 |
| Total cholesterol, mmol/L | 4.23 ± 1.10 | 4.30 ± 1.22 | 0.779 |
| LDL-C, mmol/L | 2.28 ± 1.09 | 2.38 ± 1.07 | 0.695 |
| HDL-C, mmol/L | 1.13 ± 0.29 | 1.13 ± 0.25 | 0.991 |
| Triglycerides, mmol/L | 2.04 ± 1.09 | 1.98 ± 0.87 | 0.811 |
| Total unit of insulin, IU | 50.17 ± 31.63 | 64.92 ± 45.65 | 0.166 |
| History of dyslipidemia | 6 (16.7) | 4 (11.1) | 0.734 |
| History of hypertension | 15 (41.7) | 11 (30.6) | 0.462 |
Data are expressed as numbers (%), mean ± standard deviation. P values are results of t test for continuous data, and Fisher’s exact test for categorical data.
Abbreviations: BMI, body mass index; C, cholesterol; CABG, coronary artery bypass graft; DAPA, dapagliflozin; DBP, diastolic blood pressure; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; HbA1c, hemoglobin A1c; IHD, Ischaemic heart disease; SBP, systolic blood pressure, UACR, urinary albumin-to-creatinine ratio. HDL; high-density lipoprotein, LDL, low-density lipoprotein; VD, vessel disease.
B. Changes in Hemodynamic and Metabolic Parameters
There were no significant reductions in body weight, BMI, waist circumference, estimated glomerular filtration rate, and systolic and diastolic blood pressures in both groups. The DAPA group had a significantly lower BMI at baseline compared to the placebo group (27.49 ± 4.17 kg/m2 vs. 29.81 ± 4.10kg/m2; P = 0.021), which persisted at the 12-week follow-up (27.42 ± 4.92 kg/m2 vs 30.89 ± 6.45 kg/m2; P = 0.015) (Table 2). HbA1c and fasting plasma glucose improved significantly from baseline to 12 weeks in the DAPA group. After 12 weeks of therapy, the DAPA group demonstrated significantly greater reductions in HbA1c compared with the placebo group (HbA1c –0.83 ± 1.47% vs –0.16 ± 1.25%; P = 0.043). This was accompanied by a greater reduction in FBG within the DAPA group compared with the placebo group (FBG –1.90 ± 4.40 mmol/mol vs 0.73 ± 4.55 mmol/mol; P = 0.015) (Table 3).
Table 2.
Changes in Metabolic and Hemodynamic Parameter
| DAPA (n = 36) | Placebo (n = 36) | P | |
|---|---|---|---|
| Weight, kg | |||
| Baseline | 76.18 ± 14.10 | 79.40 ± 14.59 | 0.352 |
| Week 12 | 75.21 ± 11.89 | 80.96 ± 15.72 | 0.092 |
| Change | –1.05 ± 15.71 | 1.76 ± 18.55 | 0.503 |
| P value within group | 0.699 | 0.584 | |
| BMI, kg/m2 | |||
| Baseline | 27.49 ± 4.13 | 29.85 ± 4.23 | 0.021 |
| Week 12 | 27. 42 ± 4.92 | 30.89 ± 6.45 | 0.015 |
| Change | –0.11 ± 5.83 | 0.956 ± 7.44 | 0.509 |
| P value within group | 0.906 | 0.459 | |
| SBP, mmHg | |||
| Baseline | 140.92 ± 22.08 | 141.06 ± 21.61 | 0.979 |
| Week 12 | 136.08 ± 21.75 | 143.33 ± 18.98 | 0.136 |
| Change | –4.83 ± 17.73 | 2.28 ± 18.17 | 0.097 |
| P value within group | 0.11 | 0.457 | |
| DBP, mmHg | |||
| Baseline | 78.31 ± 11.18 | 77.86 ± 12.78 | 0.876 |
| Week 12 | 80.39 ± 10.88 | 80.17 ± 11.92 | 0.934 |
| Change | 2.08 ± 11.17 | 2.31 ± 13.78 | 0.940 |
| P value within group | 0.271 | 0.322 | |
| Waist circumference, cm | |||
| Baseline | 96.03 ± 8.66 | 97.63 ± 8.81 | 0.455 |
| Week 12 | 95.81 ± 8.32 | 98.25 ± 7.54 | 0.209 |
| Change | 0.68 ± 4.35 | 0.51 ± 5.58 | 0.504 |
| P value within group | 0.381 | 0.606 | |
| eGFR, mL/min/1.73m2 | |||
| Baseline | 85.98 ± 18.42 | 82.20 ± 15.87 | 0.463 |
| Week 12 | 85.105 ± 19.87 | 81.90 ± 18.07 | 0.549 |
| Change | –0.88 ± 12.0 | –0.30 ± 10.34 | 0.92 |
| P value within group | 0.699 | 0.865 |
Data are mean ± standard deviation (n). P values within groups are results of paired t test or Wilcoxon signed-rank test. P values among groups are results of independent sample t test.
Abbreviations: BMI, body mass index; DAPA, dapagliflozin; DBP: diastolic blood pressure, eGFR; estimated glomerular filtration rate SBP; systolic blood pressure.
Table 3.
Changes in Parameters of Glycemic Control
| DAPA (n = 36) | Placebo (n = 36) | P | |
|---|---|---|---|
| HbA1c, % | |||
| Baseline | 9.66 ± 1.86 | 9.31 ± 1.58 | 0.397 |
| Week 12 | 8.83 ± 1.50 | 9.15 ± 1.94 | 0.438 |
| Change | –0.83 ± 1.47 | –0.16 ± 1.26 | 0.043 |
| P value within group | 0.02 | 0.448 | |
| Fasting plasma glucose, mmol/L | |||
| Baseline | 10.69 ± 4.55 | 9.57 ± 4.02 | 0.275 |
| Week 12 | 8.78 ± 2.98 | 10.30 ± 4.19 | 0.080 |
| Change | –1.91 ± 4.40 | 0.73 ± 4.55 | 0.015 |
| P value within group | 0.013 | 0.963 |
P values within groups are results of paired t test or Wilcoxon signed-rank test. P values among groups are results of independent sample t test.
Abbreviations: DAPA, dapagliflozin; HbA1c, hemoglobin A1c.
C. Endothelial Function After 12 Weeks of Treatment
After a 12-week therapy, there were no significant differences in ΔFMD between both groups and within each group. However, the placebo group demonstrated a trend toward worsening of ΔFMD while the DAPA group had almost similar mean values throughout the same duration. The placebo group showed a nonsignificant worsening of NMD measurements, but it was significantly lower compared with the DAPA group (19.64 ± 9.71% vs 15.11 ± 8.44 %; P = 0.038).
As a surrogate marker for endothelial functions, the ΔICAM-1 level showed significant improvement in the DAPA group but not in the placebo group (ΔICAM-1, DAPA group vs placebo group, –83.9 ± 205.9 ng/mL; P < 0.02 vs –11.0 ± 169.1 ng/mL; P = 0.699). However, there were no significant changes in both groups for eNOS. Notably, there was a slight increase in Lp(a) level in the DAPA group, though it was not statistically significant.
The DAPA group showed significant increase in hs-CRP, with a median of 1.93 (5.29) to 6.03 (9.36) mg/L, P = 0.009. The DAPA group also demonstrated a significantly greater rise in hs-CRP in comparison with the placebo group (DAPA 2.9 [6.97] mg/L vs placebo 0.12 [1.97] mg/L; P = 0.043) (Table 4). According to the American Heart Association/Centers for Disease Control classification, the majority of patients in both arms are high-risk patients at baseline. Within the DAPA group, there are increased numbers of patients under the high-risk category: from 13 to 22 patients by week 12 (Table 5). All randomized patients had no history of acute illness throughout the study, minimizing confounding factors that affect the hs-CRP level, which represents generalized ongoing inflammation.
Table 4.
Changes in Endothelial Function and Surrogate Markers
| DAPA (n = 36) | Placebo (n = 36) | P | |
|---|---|---|---|
| FMD, % | |||
| Baseline | 11.22 ± 8.34 | 11.49 ± 5.84 | 0.792 |
| Week 12 | 11.41 ± 6.87 | 9.84 ± 5.25 | 0.281 |
| Change | 0.19 ± 10.38 | -1.36 ± 7.76 | 0.400 |
| P value within group | 0.91 | 0.21 | |
| NMD, % | |||
| Baseline | 19.62 ± 11.27 | 16.83 ± 8.39 | 0.238 |
| Week 12 | 19.64 ± 9.71 | 15.11 ± 8.44 | 0.038 |
| Change | 0.018 ± 12.20 | -1.73 ± 8.81 | 0.489 |
| P value within group | 0.99 | 0.248 | |
| ICAM-1, ng/ml | |||
| Baseline | 381.1 ± 144.3 | 335.4 ± 98.6 | 0.123 |
| Week 12 | 297.2 ± 17.17 | 324.4 ± 166.5 | 0.558 |
| Change | -83.9 ± 205.9 | -11.0 ± 169.1 | 0.107 |
| P value within group | 0.021 | 0.699 | |
| eNOS, pg/ml | |||
| Baseline | 1.26 ± 0.37 | 1.22 ± 0.39 | 0.651 |
| Week 12 | 1.29 ± 0.26 | 1.32 ± 0.18 | 0.683 |
| Change | 0.02 ± 0.51 | 0.13 ± 0.45 | 0.309 |
| P value within group | 0.685 | 0.258 | |
| Lp(a), g/L | |||
| Baseline | 27.6 (62.5) | 21.6 (33.8) | 0.451 |
| Week 12 | 33.5(114.15) | 13.7 (72) | 0.08 |
| Change | 1.15 (100.2) | 0.1 (61.6) | 0.851 |
| P value within group | 0.382 | 0.71 | |
| hs-CRP, mg/L | |||
| Baseline | 1.93 (5.29) | 2.7 (2.74) | 0.503 |
| Week 12 | 6.03 (9.36) | 2.96 (4.47) | 0.237 |
| Change | 2.9 (6.97) | 0.12(1.97) | 0.043 |
| P value within group | 0.009 | 0.221 |
Data are mean ± standard deviation (n) and median (IQR). P values within groups are results of a paired t test or Wilcoxon signed-rank test. P values among groups are results of independent sample t test.
Abbreviations: DAPA, dapagliflozin; eNOS, endothelial nitric oxide synthase; FMD, flow‐mediated vasodilatation; HbA1c, hemoglobin A1c; hs-CRP, high-sensitivity C-reactive protein; ICAM-1, intercellular adhesion molecule 1; Lp(a), lipoprotein(a); NMD, nitroglycerin‐mediated vasodilatation = endothelial independent dilation.
Table 5.
CVD Risk Based on AHA/CDC Risk Category for hs-CRP
| DAPA (n = 35) | Placebo (n = 36) | P | |
|---|---|---|---|
| Low risk | |||
| Baseline | 10 (27) | 6 (17) | 0.779 |
| Week 12 | 8 (22) | 6 (17) | 0.319 |
| Intermediate risk | |||
| Baseline | 12 (35) | 10 (27) | 0.998 |
| Week 12 | 6 (17) | 10 (27) | 0.984 |
| High risk | |||
| Baseline | 13 (36) | 19 (53) | 0.696 |
| Week 12 | 22 (61) | 19 (53) | 0.71 |
The classification is based on data obtained from population-based studies, the AHA/CDC (American Heart Association/Centers for Disease Control) have classified serum hs-CRP levels < 1, 1 to 3 and >3 mg/L as low, intermediate, and high-risk groups for global CVD, respectively. Data are expressed as numbers (%). Abbreviations: CVD, cardiovascular disease; DAPA, dapagliflozin; hs-CRP, high-sensitivity C-reactive protein.
D. Changes in Lipid Parameters
With regard to lipid metabolism, there was a significant rise in total cholesterol [SD] within the placebo group, +0.42 [0.92] mg/dL; P = 0.012, although it was not statistically significant when compared with the DAPA group. In contrast, LDL cholesterol [SD] was significantly increased within the DAPA group after 12 weeks of therapy, +0.30 [0.83] mg/dL; P = 0.049. There was no change in the triglyceride and HDL-C levels in both groups (Table 6).
Table 6.
Changes in Lipid Parameters
| DAPA (n = 36) | Placebo (n = 36) | P | |
|---|---|---|---|
| Total cholesterol, mg/dL | |||
| Baseline | 4.22 ± 1.15 | 4.31 ± 1.24 | 0.779 |
| Week 12 | 4.42 ± 1.15 | 4.72 ± 1.34 | 0.319 |
| Change | 0.24 ± 0.94 | 0.42 ± 0.92 | 0.445 |
| P value within group | 0.149 | 0.012 | |
| HDL-C, mg/dL | |||
| Baseline | 1.13 ± 0.29 | 1.14 ± 0.25 | 0.998 |
| Week 12 | 1.15 ± 0.28 | 1.14 ± 0.25 | 0.984 |
| Change | 0.02 ± 0.19 | 0.01 ± 0.16 | 0.965 |
| P value within group | 0.529 | 0.603 | |
| LDL-C, mg/dL | |||
| Baseline | 2.28 ± 1.12 | 2.39 ± 1.10 | 0.696 |
| Week 12 | 2.5 ± 1.19 | 2.61 ± 1.18 | 0.71 |
| Change | 0.30 ± 0.83 | 0.24 ± 1.01 | 0.992 |
| P value within group | 0.049 | 0.167 | |
| Triglyceride, mg/dL | |||
| Baseline | 2.04 ± 1.10 | 1.98 ± 0.90 | 0.813 |
| Week 12 | 1.90 ± 0.87 | 1.93 ± 0.97 | 0.900 |
| Change | –0.16 ± 0.87 | –0.02 ± 0.95 | 0.693 |
| P value within group | 0.300 | 0.88 |
Data are mean ± standard deviation (n). P values within groups are results of paired t test or Wilcoxon signed-rank test. P values among groups are results of independent sample t test or Mann Whitney U test.
Abbreviations: DAPA, dapagliflozin; HDL-C, high-density lipoprotein–cholesterol; LDL-C, low-density lipoprotein–cholesterol.
E. Univariate Analysis
We performed univariate analysis to identify the associations between the different variables. Within the overall study cohort there was a significant negative correlation between ΔHbA1c and ΔFMD (r = –0.290; P = 0.013) and between ΔHbA1c and ΔNMD (r = –0.277; P = 0.019). Moreover, there was a significant positive correlation between Δhs-CRP and ΔFMD (r = 0.286; P = 0.026) as well as a negative correlation between ΔWC and ΔFMD (r = –0.248; P = 0.035) (Table 7).
Table 7.
Correlations Between ΔFMD and ΔNMD with Other Variables in Overall Cohort
| ΔFMD | ΔNMD | |||
|---|---|---|---|---|
| r | P | r | P | |
| ΔHbA1c | –0.290 | 0.013 | –0.277 | 0.019 |
| ΔFBS | –0.15 | 0.21 | –0.168 | 0.159 |
| ΔICAM-1 | –0.115 | 0.341 | 0.89 | 0.46 |
| ΔeNOS | 0.088 | 0.473 | –0.047 | 0.703 |
| ΔLp(a) | –0.058 | 0.659 | –0.038 | 0.773 |
| Δhs-CRP | 0.286 | 0.026 | –0.009 | 0.947 |
| ΔWeight | –0.08 | 0.506 | –0.05 | 0.678 |
| ΔBMI | –0.026 | 0.834 | –0.033 | 0.786 |
| ΔWC | –0.248 | 0.035 | 0.092 | 0.441 |
| ΔTotal cholesterol | –0.104 | 0.402 | –0.32 | 0.008 |
| ΔLDL | –0.121 | 0.31 | –0.088 | 0.462 |
| ΔHDL | –0.006 | 0.958 | –0.076 | 0.525 |
| ΔTriglycerides | –0.048 | 0.687 | –0.157 | 0.188 |
*P value < 0.05. Data are correlation (r) and P values (p). Pearson correlations are used in this comparisons. Abbreviations: BMI, body mass index; eNOS, endothelial nitric oxide synthase; FBS, fasting blood glucose; FMD, flow-mediated dilation; HbA1c, hemoglobin A1c; HDL, high-density lipoprotein; hs-CRP, high-sensitivity C-reactive protein; ICAM-1, intercellular adhesion molecule 1; LDL, low-density lipoprotein; Lp(a), lipoprotein(a); NMD, nitroglycerin-mediated dilation; WC, waist circumference.
Within each group there was a significant negative correlation between ΔHbA1c and ΔFMD (r = –0.395; P = 0.017) in the DAPA group, which was not seen within the placebo group (Table 8). We also did not find any association between ΔICAM-1 and other Δ endothelial function biomarkers.
Table 8.
Correlations Between ΔFMD and ΔNMD with Other Variables in the DAPA Group
| ΔFMD | ΔNMD | |||
|---|---|---|---|---|
| r | P | r | P | |
| ΔHbA1c | -0.395 | 0.017 | -0.315 | 0.061 |
| ΔFBS | -0.173 | 0.312 | -0.178 | 0.159 |
| ΔICAM-1 | 0.075 | 0.668 | 0.192 | 0.27 |
| ΔeNOS | -0.146 | 0.409 | -0.222 | 0.206 |
| ΔLp (a) | 0.019 | 0.92 | 0.128 | 0.501 |
| Δhs-CRP | 0.342 | 0.065 | 0.039 | 0.84 |
| ΔWeight | 0.057 | 0.74 | -0.072 | 0.678 |
| Δ BMI | -0.09 | 0.961 | -0.033 | 0.786 |
| ΔWC | -0.067 | 0.698 | 0.148 | 0.388 |
| ΔTotal cholesterol | -0.237 | 0.184 | -0.142 | 0.43 |
| ΔLDL | -.046 | 0.789 | 0.091 | 0.598 |
| ΔHDL | -0.037 | 0.831 | -0.131 | 0.477 |
| ΔTriglycerides | 0.038 | 0.824 | -0.125 | 0.468 |
*P value < 0.05. Data are correlation (r) and P values (p). Pearson correlations are used in this comparisons.
Abbreviations: BMI, body mass index; eNOS, endothelial nitric oxide synthase; FBS, fasting blood glucose; FMD, flow-mediated dilation; HbA1c, hemoglobin A1c; HDL, high-density lipoprotein; hs-CRP, high-sensitivity C-reactive protein; ICAM-1, intercellular adhesion molecule 1; LDL, low-density lipoprotein; Lp(a), lipoprotein(a); NMD, nitroglycerin-mediated dilation; WC, waist circumference.
F. Adverse Events
The recorded AEs were 6 for the DAPA group and 8 for the placebo group. Interestingly, the placebo group reported more hypoglycemic episodes than the DAPA group (placebo group 9 [21.9] vs DAPA group 1 [2.5]; P = 0.015). However, these were documented as minor events and did not require assistance.
4. Discussion
The primary outcome of our study was the improvement in FMD following a 12-week therapy with dapagliflozin. Although our study was unable to demonstrate any significant change, there seemed to be a signal of worsening of FMD within the placebo group, while the DAPA group remained unchanged. This was in contrast to the only other study of SGLT2-Is on FMD (ie, DEFENCE), which looked at the effect of dapagliflozin versus metformin on endothelial function and showed significant improvement in ΔFMD in the DAPA group [17]. However, the study was conducted among patients with an early stage of the disease without CVD. Furthermore, the results were only significant in patients with a baseline of HbA1c of greater than 7% (53 mmol/mol). Of note, our study is the first to investigate the effects of SGLT2-Is toward endothelial dysfunctions in patients with T2DM and underlying CVD.
Based on currently available data, the effectiveness of DPP4-Is in improving endothelial dysfunction has yet to be ascertained. A recent study showed improvement in FMD by linagliptin accompanied by a modest improvement in glycemic control after 16 weeks of treatment [18]. However, large-scale outcome trials with DPP4-Is failed to demonstrate superior cardiovascular safety compared with a placebo. In the SAVOR Timi-53 study, saxagliptin treatment was associated with an increased risk for hospitalization for heart failure [26]. However, sitagliptin did not appear to increase the risk of major adverse cardiovascular events, hospitalization for heart failure, or other AEs [27].
The evidence of short- and long-term effects of GLP-1 agonists on FMD had been discouraging. The SAIS-2 study demonstrated no improvement of FMD in liraglutide when compared with the glargine group despite reductions of HbA1c in both groups [35]. Hopkins et al studied the effect of GLP-1 in an obese patient (BMI > 40) with T2DM without underlying ischemic heart disease, and the result demonstrated no improvement in FMD and NMD despite reductions in BMI and HbA1c [21]. However, both studies were relatively small.
Due to the encouraging positive cardiovascular effects demonstrated by the SGLT2- s in contrast to the DPP4-Is and GLP-1, there is a continuous need to further understand the underlying mechanism of this particular class.
In our study, we compared the effects of add-on dapagliflozin to insulin +/- metformin on FMD and other surrogate markers for endothelial dysfunction. This included patients with HbA1c of more than 7% (53 mmol/mol) and less than 10.5% (89 mmol/mol) with underlying CVDs. To our knowledge, there has been no published clinical trial that compared the effects of dapagliflozin as an add-on therapy to the effects on insulin in patients with T2DM with a history of CVD. This was particularly important as our cohort represented a particularly high-risk population.
Our study subsequently showed significantly lower ΔNMD within the placebo group after 12 weeks of therapy, which further supported the worsening of endothelial dysfunction. NMD is affected by vascular smooth muscle cell dysfunction and surrounding extracellular matrix in the medial layer of the arterial wall. The accelerating risk factors for atherosclerosis such as hyperglycemia, dyslipidemia, hypertension, and uremia may exert long-term cumulative effects on vascular smooth muscle cell and the surrounding matrix in the medial layer rather than on the endothelium [8]. Patients with high plaque burden translated by high total cholesterol were found to have reduced vasodilator response to nitroglycerine [28]. The worsening NMD in the placebo group within our study cohort may, therefore, possibly be explained by the significant worsening of total cholesterol within the placebo group, which was not seen within the DAPA group. This is further supported by the significant negative correlations between the ΔTC and ΔNMD.
In our study, a surrogate marker of endothelial function, ICAM-1, showed significant improvements in the DAPA group, with a reduction [SD] of –8.39 [20.59] ng/mL; P < 0.02. Despite the absence of any correlations within the DAPA groups, there was a significant negative correlation between ΔICAM-1 and ΔFMD within the placebo group, (r = –0.377; P = 0.023). ICAM-1 is a cellular adhesion molecule that is poorly expressed by the resting endothelium but is upregulated during inflammatory atherogenesis and may be an index of endothelial activation or even a molecular marker of early atherosclerosis [29]. These results indicate that dapagliflozin as an add-on therapy provided better glycemic control and improved oxidative stress, which could attenuate the progression of atherosclerosis in high-risk T2DM. However, there was a nonsignificant correlation between ΔICAM-1 with other endothelial biomarkers such as Δhs-CRP, ΔeNOS, ΔFMD, and ΔNMD.
Interestingly, our result showed a significant increase in LDL-C within the DAPA group. Similar findings were also seen in other studies, which demonstrated high, large, buoyant LDL-C and an increase in HDL-C after 12 weeks of therapy of dapagliflozin [30]. In one meta-analysis, canagliflozin also showed higher LDL-C, compared with empagliflozin and dapagliflozin after 24 weeks of treatment [31]. Although LDL-C is a strong risk factor for CVD and atherosclerosis, prior studies have shown no independent association for LDL-C with diabetes [32].
Lp(a), which is a biomarker for a CVD risk factor showed a nonsignificant increase in the DAPA group. A previous study showed that Lp(a) has an inverse correlation with the incidence of T2DM in contrast to positive correlations of Lp(a) with cardiovascular risk [33]. Nonetheless, patients with insulin-dependent DM tend to have higher Lp(a) at baseline, when compared with the patients without diabetes [34]. In addition, Lp(a) is significantly higher in patients with diabetes with ischemic heart disease compared with patients without manifestation of vascular disease and Lp(a) levels ≥30 mg/dl have been shown as being independently associated with the presence of CVD [29]. This, therefore, could possibly explain the relatively high baseline Lp(a) within our study cohort, which subsequently remained unchanged throughout the study duration.
Hs-CRP is a recognized biomarker of inflammation and an independent predictor for CVD [35]. On the basis of data obtained from population-based studies, the American Heart Association/Centers for Disease Control have classified serum hs-CRP levels <1, 1 to 3, and >3 mg/L as low, intermediate, and high-risk groups for global CVD, respectively [36]. In addition to the endothelial dysfunction studies, our study demonstrated a significant increase of hs-CRP within the DAPA, group which was not seen within the placebo group. This could suggest an ongoing inflammatory process that had been exaggerated by a rapid decline in glycemia within the DAPA group. This was supported by previous data that showed higher hs-CRP levels in patients who experienced higher glycemic excursions compared with those with smaller glucose changes [31]. Nonetheless, the majority of the patients in both arms are high-risk patients from baseline. Therefore, it is very likely that the rapid changes in HbA1c and FBG within the DAPA group could contribute to the significant transient rise in hs-CRP.
Despite the absence of significant improvements in ΔFMD, our study showed significant reductions in HbA1c and FBG within the DAPA group from baseline. The reduction of HbA1c in the DAPA group was approximately 0.8%. This is in concordance to previous studies that when compared to placebo, SGLT2-Is reduce HbA1c levels by an average of 0.5% to 0.8% when used as monotherapy or add-on therapy [37]. Nonetheless, dapagliflozin is also expected to produce a modest weight loss of approximately 2 kg and decrease systolic and diastolic blood pressures by approximately 4 mmHg and 2 mmHg, respectively [33]. We were not able to demonstrate any significant weight or blood pressure reductions. These results could be mainly due to the use of insulin in both groups, which could possibly offset the expected weight loss in the DAPA group. Our study populations showed significantly high baseline BMI. The differences in BMI are identified as the cofounding factor of this study.
FMD has been reported to be affected by many confounding factors including gender, age, obesity, heart rate, and smoking [38]. However, the prevalence of these potential confounders was not significantly different between the 2 groups. More importantly, the univariate analysis also showed significant negative correlations between HbA1c and ΔFMD. These correlations have not been seen in previous studies.
Finally, there was a significant number of patients within the placebo group who experienced hypoglycemia episodes throughout the study. A plausible explanation is their propensity toward higher doses of insulin intake. In conclusion, the use of dapagliflozin in addition to insulin might subsequently reduce hypoglycemic events caused by higher doses of insulin injections.
This study highlighted several important points. To the best of our knowledge, this is the first study to determine the effects of dapagliflozin on endothelial function in patients with T2DM with underlying IHD. Secondly, our study showed improvement in some aspects of endothelial dysfunctions in both radiological and surrogate markers. Finally, our study populations had well-controlled blood pressure and lipids throughout the study to minimize the effect of cofounders.
Our study limitations include a relatively small number of patients and a short study duration. However, this was a calculated sample size based on a previous similar study and thus should provide a statistically valid result on the primary outcome. Nevertheless, longer trials with larger sample size would be desirable to yield more favorable results and subsequently confirm our findings. Secondly, although the FMD test is non-invasive and easy to perform, it is, however, operator dependent subject to operator bias and easily affected by variations in intravascular volumes. To overcome this, one single technician, who was well trained and experienced in the examination technique, conducted the examinations. Finally, due to the limitations above, we acknowledge that ideally, larger and longer trials would be able to provide a deeper understanding of the effects of SGLT2-I on endothelial dysfunction. However, we hope that this study has provided some preliminary insights that could promote further interests in the subject.
In conclusion, this study showed that dapagliflozin in addition to insulin and metformin therapies in high-risk patients resulted in significant reductions in HbA1c, FBG, and the surrogate marker of the endothelial function represented by ICAM-1. Although the DAPA group demonstrated a significant association between reductions in HbA1c and improvement in FMD, there was no significant difference in FMD between the 2 groups.
Glossary
Abbreviations
- AEs
adverse events
- BMI
body mass index
- CVD
cardiovascular disease
- eNOS
endothelial nitric oxide synthase
- FBG
fasting blood glucose
- FMD
flow-mediated dilation
- GTN
glyceryl trinitrate
- HbA1c
hemoglobin A1c
- HDL-C
high-density lipoprotein–cholesterol
- hs-CRP
high-sensitivity C-reactive protein
- ICAM-1
intracellular adhesion molecule
- Lp(a)
lipoprotein(a)
- NMD
nitroglycerin-mediated dilation
- SD
standard deviation
- SGLT2-I
sodium-glucose cotransporter 2 inhibitor
- TC
total cholesterol
- TG
triglyceride
- T2DM
type 2 diabetes mellitus
Acknowledgments
Financial Support: This study was supported by an Investigator‐Initiated Trial Grant from Astra Zeneca. Astra Zeneca played no role in the study design, conduct, analysis, preparation, or final approval of the manuscript.
Clinical Trial Information : Effects of dapagliflozin on endothelial dysfunction in Type 2 Diabetes with established ischemic heart disease (EDIFIED). Registration no. 100-IRMI/PRI16/6/2 (007/2017). This clinical trial study was conducted in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Author Contributions: N.A.Z was involved in the project conception, literature review and synthesis, data acquisition, detailed data analysis, statistical analysis, critical discussion, and drafting of the manuscript. R.A.G. was involved in the project conception, experimental design, critical discussion, and supervision of the project. S.F.W. was involved in literature review and data. N.H and Z.I were involved in the statistical analysis and critical discussion. F.Z.H. was involved in the data analysis and critical discussion. T.I. contributed to the experimental design and assisted with the laboratory equipment. N.A.D. was involved in data acquisition. J.D.Z. was involved in the supervision of the project. All authors contributed to the revision of the manuscript and reviewed the final version of the manuscript. R.A.G. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Additional Information
Disclosure Summary: The authors have nothing to disclose. No potential conflicts of interest relevant to this article were reported.
References and Notes
- 1. Fox CS, Coady S, Sorlie PD, et al. Trends in cardiovascular complications of diabetes. Jama. 2004;292(20):2495–2499. [DOI] [PubMed] [Google Scholar]
- 2. Ross R. Atherosclerosis–an inflammatory disease. N Engl J Med. 1999;340(2):115–126. [DOI] [PubMed] [Google Scholar]
- 3. Tabit CE, Chung WB, Hamburg NM, Vita JA. Endothelial dysfunction in diabetes mellitus: molecular mechanisms and clinical implications. Rev Endocr Metab Disord. 2010;11(1):61–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ghiadoni L, Versari D, Giannarelli C, Faita F, Taddei S. Non-invasive diagnostic tools for investigating endothelial dysfunction. Curr Pharm Des. 2008;14(35):3715–3722. [DOI] [PubMed] [Google Scholar]
- 5. Flammer AJ, Anderson T, Celermajer DS, et al. The assessment of endothelial function: from research into clinical practice. Circulation. 2012;126(6):753–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Green DJ, Jones H, Thijssen D, Cable NT, Atkinson G. Flow-mediated dilation and cardiovascular event prediction: Does nitric oxide matter? Hypertension. 2011;57(3):363–369. [DOI] [PubMed] [Google Scholar]
- 7. Patti G, Pasceri V, Melfi R, et al. Impaired flow-mediated dilation and risk of restenosis in patients undergoing coronary stent implantation. Circulation. 2005;111(1):70–75. [DOI] [PubMed] [Google Scholar]
- 8. Kawano N, Emoto M, Mori K, et al. Association of endothelial and vascular smooth muscle dysfunction with cardiovascular risk factors, vascular complications, and subclinical carotid atherosclerosis in type 2 diabetic patients. J Atheroscler Thromb. 2012;19(3):276–284. [DOI] [PubMed] [Google Scholar]
- 9. Akamatsu D, Sato A, Goto H, et al. Nitroglycerin-mediated vasodilatation of the brachial artery may predict long-term cardiovascular events irrespective of the presence of atherosclerotic disease. J Atheroscler Thromb. 2010;17(12):1266–1274. [DOI] [PubMed] [Google Scholar]
- 10. Kullo IJ, Malik AR, Bielak LF, Sheedy PF 2nd, Turner ST, Peyser PA. Brachial artery diameter and vasodilator response to nitroglycerine, but not flow-mediated dilatation, are associated with the presence and quantity of coronary artery calcium in asymptomatic adults. Clin Sci (Lond). 2007;112(3):175–182. [DOI] [PubMed] [Google Scholar]
- 11. Chan SY, Mancini GB, Kuramoto L, Schulzer M, Frohlich J, Ignaszewski A. The prognostic importance of endothelial dysfunction and carotid atheroma burden in patients with coronary artery disease. J Am Coll Cardiol. 2003;42(6):1037–1043. [DOI] [PubMed] [Google Scholar]
- 12. Vitale C, Mercuro G, Cornoldi A, Fini M, Volterrani M, Rosano GM. Metformin improves endothelial function in patients with metabolic syndrome. J Intern Med. 2005;258(3):250–256. [DOI] [PubMed] [Google Scholar]
- 13. Kubota Y, Miyamoto M, Takagi G, et al. The dipeptidyl peptidase-4 inhibitor sitagliptin improves vascular endothelial function in type 2 diabetes. J Korean Med Sci. 2012;27(11):1364–1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zinman B, Wanner C, Lachin JM, et al. ; EMPA-REG OUTCOME Investigators . Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–2128. [DOI] [PubMed] [Google Scholar]
- 15. Inzucchi SE, Zinman B, Wanner C, et al. SGLT-2 inhibitors and cardiovascular risk: proposed pathways and review of ongoing outcome trials. Diab Vasc Dis Res. 2015;12(2):90–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sonesson C, Johansson PA, Johnsson E, Gause-Nilsson I. Cardiovascular effects of dapagliflozin in patients with type 2 diabetes and different risk categories: a meta-analysis. Cardiovasc Diabetol. 2016;15:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Shigiyama F, Kumashiro N, Miyagi M, et al. Effectiveness of dapagliflozin on vascular endothelial function and glycemic control in patients with early-stage type 2 diabetes mellitus: DEFENCE study. Cardiovasc Diabetol. 2017;16(1):84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.RRID: AB_2249850, https://scicrunch.org/resolver/AB_2249850
- 19.RRID:AB_1614450, https://scicrunch.org/resolver/AB_1614450.
- 20.RRID: AB_64051, https://scicrunch.org/resolver/AB_64051.
- 21.RRID:AB_2153005, https://scicrunch.org/resolver/AB_2153005.
- 22. Juonala M, Magnussen CG, Venn A, et al. Influence of age on associations between childhood risk factors and carotid intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study, the Childhood Determinants of Adult Health Study, the Bogalusa Heart Study, and the Muscatine Study for the International Childhood Cardiovascular Cohort (i3C) Consortium. Circulation. 2010;122(24):2514–2520. [DOI] [PubMed] [Google Scholar]
- 23. Dalli E, Segarra L, Ruvira J, et al. [Brachial artery flow-mediated dilation in healthy men, men with risk factors, and men with acute myocardial infarction. Importance of occlusion-cuff position]. Rev Esp Cardiol. 2002;55(9):928–935. [DOI] [PubMed] [Google Scholar]
- 24. Adams MR RJ, McCredie R, et al. Normal ranges for brachial artery flow-mediated dilatation: a non-invasive ultrasound test of arterial endothelial function. J Vasc Invest 1996;2:146–50. [Google Scholar]
- 25. Järvisalo MJ, Raitakari M, Toikka JO, et al. Endothelial dysfunction and increased arterial intima-media thickness in children with type 1 diabetes. Circulation. 2004;109(14):1750–1755. [DOI] [PubMed] [Google Scholar]
- 26. Scirica BM, Braunwald E, Raz I, et al. ; SAVOR-TIMI 53 Steering Committee and Investigators* Heart failure, saxagliptin, and diabetes mellitus: observations from the SAVOR-TIMI 53 randomized trial. Circulation. 2014;130(18):1579–1588. [DOI] [PubMed] [Google Scholar]
- 27. Green JB, Bethel MA, Armstrong PW, et al. ; TECOS Study Group Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;373(3):232–242. [DOI] [PubMed] [Google Scholar]
- 28. Adams MR, Robinson J, McCredie R, et al. Smooth muscle dysfunction occurs independently of impaired endothelium-dependent dilation in adults at risk of atherosclerosis. J Am Coll Cardiol. 1998;32(1):123–127. [DOI] [PubMed] [Google Scholar]
- 29. Meydani M. Soluble adhesion molecules: surrogate markers of cardiovascular disease? Nutr Rev. 2003;61(2):63–68. [DOI] [PubMed] [Google Scholar]
- 30. Hayashi T, Fukui T, Nakanishi N, et al. Dapagliflozin decreases small dense low-density lipoprotein-cholesterol and increases high-density lipoprotein 2-cholesterol in patients with type 2 diabetes: comparison with sitagliptin. Cardiovasc Diabetol. 2017;16(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zaccardi F, Webb DR, Htike ZZ, Youssef D, Khunti K, Davies MJ. Efficacy and safety of sodium-glucose co-transporter-2 inhibitors in type 2 diabetes mellitus: systematic review and network meta-analysis. Diabetes Obes Metab. 2016;18(8):783–794. [DOI] [PubMed] [Google Scholar]
- 32. Wilson PWF, Meigs JB. Risk of type 2 diabetes mellitus and coronary heart disease: a pivotal role for metabolic factors. Eur Heart J Suppl. 2008;10(suppl_B):B11–B5. [Google Scholar]
- 33. Mora S, Kamstrup PR, Rifai N, Nordestgaard BG, Buring JE, Ridker PM. Lipoprotein(a) and risk of type 2 diabetes. Clin Chem. 2010;56(8):1252–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kahri J, Groop PH, Viberti G, Elliott T, Taskinen MR. Regulation of apolipoprotein A-I-containing lipoproteins in IDDM. Diabetes. 1993;42(9):1281–1288. [DOI] [PubMed] [Google Scholar]
- 35. Danesh J, Collins R, Peto R. Lipoprotein(a) and coronary heart disease. Meta-analysis of prospective studies. Circulation. 2000;102(10):1082–1085. [DOI] [PubMed] [Google Scholar]
- 36. Roberts WL; CDC; AHA CDC/AHA Workshop on markers of inflammation and cardiovascular disease: application to clinical and public health practice: laboratory tests available to assess inflammation–performance and standardization: a background paper. Circulation. 2004;110(25):e572–e576. [DOI] [PubMed] [Google Scholar]
- 37. Mikhail N. Place of sodium-glucose co-transporter type 2 inhibitors for treatment of type 2 diabetes. World J Diabetes. 2014;5(6):854–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Benjamin EJ, Larson MG, Keyes MJ, et al. Clinical correlates and heritability of flow-mediated dilation in the community: the Framingham Heart Study. Circulation. 2004;109(5):613–619. [DOI] [PubMed] [Google Scholar]