Abstract
Most children who present with hypertensive crisis have a secondary cause for hypertension. This study describes the epidemiology and management of children with hypertensive crisis. A retrospective cohort study was done in a tertiary pediatric hospital from 2009 to 2015. Thirty-seven patients were treated for hypertensive crisis. Twelve (32.4%) patients were treated for hypertensive emergency. The majority of our patients (33 [89.1%]) had a secondary cause of hypertension. The most common identifiable cause of hypertension was a renal pathology (18/37 [48.6%]). Oral nifedipine (23 [62.1%]) was the most frequently used antihypertensive, followed by intravenous labetalol (8 [21.6%]). There were no mortalities or morbidities. Hypertensive crisis in children is likely secondary in nature. Oral nifedipine and intravenous labetalol are both effective treatments.
Keywords: hypertensive crisis, hypertensive emergency, pediatric
Introduction
Most children who present with hypertensive crisis have secondary hypertension 1 2 and renal pathology is the most common etiology. 2 To date, there remains limited data and consensus for the optimal treatment of hypertension in children. 1 3 Various agents, both oral and intravenous have been used with good results with no major mortality and morbidity. 4 5
Our study aims to describe the epidemiology and management of children treated for hypertensive crisis in our institution. The primary aim of the study was to look at the immediate treatment administered in hypertensive crisis. The secondary aims were to describe outcomes such as length of hospital stay, blood pressure centiles on discharge, need for outpatient antihypertensives, any major adverse events or mortality in children with hypertensive crisis.
We hypothesize that both oral and intravenous antihypertensive medications are efficacious in the management of children with hypertensive crisis and if the cause for hypertension was treated promptly, there would be reduced mortality and morbidity.
Methods
Subjects
We conducted a single-center retrospective observational study of pediatric patients treated for hypertensive crisis in KK Women's and Children's Hospital, Singapore from 2009 to 2015. Our hospital is the largest tertiary care pediatric hospital in Singapore with 365 inpatient beds. Patients were identified based on their admission and discharge diagnosis as well as reviewing the medical records of patients referred to the Nephrology Service for the management of hypertension. Based on the presence of target organ damage, identified patients were further subdivided into two groups: (1) hypertensive emergency and (2) hypertensive urgency.
As there is still a lack of a clear definition of hypertensive crisis in children, we defined hypertensive crisis as hypertensive emergency (severe hypertension with evidence of target organ damage) and hypertensive urgency (severe hypertension with no target organ damage). 6 This definition from the fourth report on diagnosis and treatment of hypertension in children was used instead of that from the 2017 Clinical Practice Guidelines for Hypertension 7 as this research study was conceptualized before the 2017 guidelines were published. We recorded blood pressure at presentation to the children's emergency room or at referral to the nephrology service. Patients were considered to have target organ damage if they had evidence of cardiac failure, renal impairment, hypertensive retinopathy, or neurological involvement.
We included all patients less than or equal to 21 years old admitted to our hospital via the children's emergency room or referred to the nephrology service who fulfilled the clinical criteria for hypertensive crisis. We excluded patients less than 1 month old.
Ethics approval was obtained from the hospital research committee and a waiver of consent was granted for this study.
Study Variables
Patient demographics were collected. Coexisting medical conditions including comorbidities known to be associated with hypertension or increased cardiovascular risk were collected. Records of the highest documented blood pressure, presenting symptoms, and evidence of target organ damage were obtained. Outcome parameters included causes for hypertension, initial drug of choice, number of antihypertensive agents administered to achieve blood pressure control, major adverse events related to the administration of antihypertensive agents, and whether patients required antihypertensive medications on discharge. Data were collected until the time of discharge and follow-up data were not included in this study.
Statistical Analysis
Patients were analyzed in two groups: hypertensive emergency and hypertensive urgency. Continuous variables, presented as medians with interquartile ranges (IQR), were compared using the Wilcoxon rank sum test. Categorical variables, presented as frequencies and percentages, were compared using two-tailed t -test. Statistical analysis was conducted using SPSS 19 (IBM, United States). A p -value of <0.05 was taken as significant for all statistical tests.
Results
Over the study period, we identified a total of 37 patients with hypertensive crisis. Twelve (32.4%) and twenty-five (67.6%) patients had hypertensive emergency and urgency, respectively. There were no statistically significant differences in the demographics of both groups of patients ( Table 1 ). Seven (18.9%) patients were known to be hypertensive prior to the episode of hypertensive crisis. There was no correlation between target organ damage at presentation and preceding history of hypertension ( p = 0.5). Twenty (54.0%) patients were admitted to the intensive care unit and the rest were admitted to the high dependency unit.
Table 1. Demographics of children with hypertensive emergency and urgency ( n = 37) .
| Demographics | Hypertensive emergency ( n = 12) | Hypertensive urgency ( n = 25) | p -Value |
|---|---|---|---|
| Age (y) a | 12.4 (9.6–14.0) | 9.9 (3.8–15.0) | 0.1 |
| Male, n (%) | 8 (66.7) | 14 (56.0) | 0.5 |
| Ethnicity, n (%) | |||
| Chinese | 7 (58.3) | 14 (56.0) | 0.9 |
| Malay | 3 (25.0) | 5 (20.0) | 0.7 |
| Indian | 2 (16.7) | 4 (12.0) | 0.9 |
| Others | 0 (0.0) | 2 (8.0) | 0.3 |
| History of hypertension, n (%) | 3 (25.0) | 4 (16.0) | 0.5 |
| Comorbidities, n (%) b | |||
| Oncological | 1 (8.3) | 3 (12.0) | 0.9 |
| Chronic renal disease | 2 (16.7) | 2 (8.0) | 0.3 |
| Prematurity | 0 (0.0) | 0 (0.0) | NA |
| Endocrine | 0 (0.0) | 0 (0.0) | NA |
| Cardiac | 0 (0.0) | 1 (4.0) | 0.5 |
| Obesity | 2 (16.7) | 2 (8.0) | 0.4 |
| OSA | 0 (0.0) | 3 (12.0) | 0.2 |
| Symptoms at Presentation, n (%) | 10 (83.3) | 9 (36.0) | <0.01 |
| Headache | 7 (58.3) | 9 (36.0) | 0.2 |
| Shortness of breath | 2 (16.7) | 0 (0.0) | <0.01 |
| Blurring of vision | 1 (8.3) | 0 (0.0) | 0.1 |
| BP at presentation, mm Hg above 95th centile for age/gender/height, n (%) | |||
| < 20 mm Hg | 3 (35.0) | 11 (44.0) | 0.3 |
| > 20 mm Hg | 9 (75.0) | 14 (56.0) | 0.3 |
Abbreviations: BP, blood pressure; NA, not applicable; OSA, obstructive sleep apnea.
In median (interquartile range).
Condition that is associated with hypertension and carries the potential to increase the risk for cardiovascular disease and can have an adverse effect on health outcome.
A renal pathology (18/37 [48.6%]) was the most common cause of hypertension in our cohort ( Fig. 1 ). Amongst patients with a renal pathology, renal artery stenosis was the most common etiology (7/18 [38.9%]). Other renal pathology included poststreptococcal glomerulonephritis (5/18 [27.8%]), lupus nephritis (3/18 [16.7%]), reflux nephropathy (2/18 [11.1%]), and hemolytic uremic syndrome (1/18 [5.6%]). One (2.7%) patient had an endocrine pathology, pheochromocytoma. Two (5.4%) cardiac cases identified had coarctation of the aorta. Drug-induced hypertension was found in two (5.4%) patients. This was secondary to the steroid use and ciclosporin. Oncological causes were found in five (13.5%) patients. These included acute lymphoblastic leukemia with kidney infiltration, paraganglioma, and Wilm's tumor. Other causes were found in five (13.5%) patients. These included two patients with Takayasu arteritis and three patients with autonomic instability following neurological insult. There was no statistically significant difference in the presence of comorbidities amongst both groups of patients.
Fig. 1.
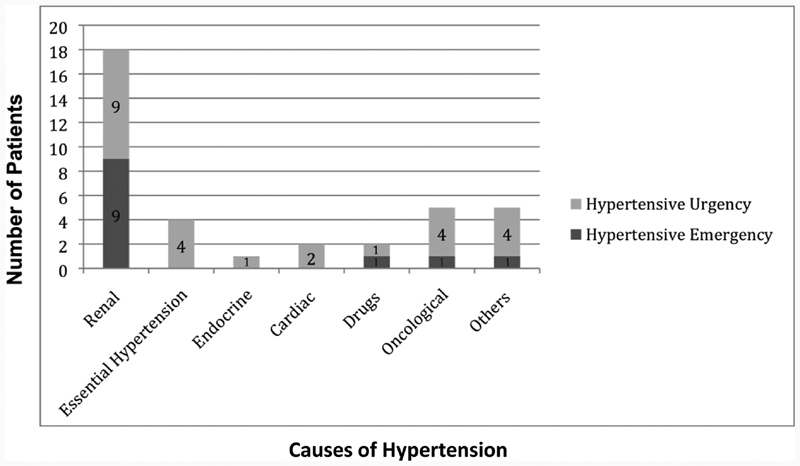
Causes of hypertension.
Nineteen (51.4%) patients with hypertensive crisis were symptomatic at presentation. Headaches were the most common symptom at presentation (16 [43.2%]), followed by the shortness of breath (2 [5.4%]) and only one of our patients (2.7%) had blurred vision. Patients with hypertensive emergency were more likely to be symptomatic and this was statistically significant, p < 0.01.
Amongst those presenting with hypertensive emergency, two (16.7%) had evidence of cardiac failure, four (33.3%) had renal impairment, four (33.3%) had evidence of hypertensive retinopathy, and one (8.3%) had neurological involvement. No patients presented with seizures. However, one patient with a background of acute lymphoblastic leukemia who presented with hypertension subsequently developed seizures in the ward and was diagnosed with posterior reversible encephalopathy syndrome.
Oral nifedipine was the most commonly used antihypertensive medication for the initial management of our patients with hypertensive crisis (59.5%; Table 2 ). Intravenous furosemide was the initial drug of choice for all patients with hypertensive crisis secondary to poststreptococcal glomerulonephritis. There was no statistically significant difference in the initial therapy received amongst both groups of patients.
Table 2. Initial therapy of choice amongst patients with hypertensive crisis.
| Medications | Hypertensive emergency ( n = 12) | Hypertensive urgency ( n = 25) | p -Value |
|---|---|---|---|
| Oral nifedipine, n (%) | 6 (50.0) | 16 (68.0) | 0.3 |
| Oral propranolol, n (%) | 0 (0.0) | 1 (4.0) | 0.5 |
| Oral enalapril, n (%) | 0 (0.0) | 2 (8.0) | 0.3 |
| Intravenous labetalol, n (%) | 4 (33.3) | 4 (16.0) | 0.2 |
| Intravenous furosemide, n (%) | 2 (16.7) | 2 (5.7) | 0.3 |
There was a significant difference in the length of hospital stay amongst patients admitted for hypertensive emergency versus patients admitted for hypertensive urgency (9.0 [IQR 6, 16] vs. 4.0 [IQR 2,15] days, p < 0.01). However, blood pressure of ≤95th centile upon discharge and the need for antihypertensive treatment after discharge from hospital were not statistically different ( Table 3 ). There were no adverse events from the treatment of hypertension and no mortalities in our cohort of patients.
Table 3. Secondary outcomes.
| Secondary outcomes | Hypertensive emergency ( n = 12) | Hypertensive urgency ( n = 25) | p -Value |
|---|---|---|---|
| Length of hospital stay (d) | 9.0 (6.0–16.0) | 4.0 (2.0–15.0) | <0.01 |
| BP ≤ 95th centile on discharge, n (%) | 9 (75.0) | 22 (88.0) | 0.30 |
| Need for outpatient antihypertensives, n (%) | 7 (58.3) | 15 (60.0) | 0.90 |
| Major adverse events, n (%) | 0 (0.0) | 0 (0.0) | NA |
| Mortality, n (%) | 0 (0.0) | 0(0.0) | NA |
Abbreviations: BP, blood pressure; NA, not applicable.
Note: Continuous variables summarized in median (interquartile ranges) and categorical summarized in numbers and percentages.
Discussion
Consistent with what is already known, our study demonstrated that hypertensive crisis in pediatric patients was mostly secondary hypertension 1 2 with a renal pathology being the most common cause. The majority of our patients received oral nifedipine for immediate treatment of severe hypertension and none of our patients had any significant mortality or morbidity from the treatment of hypertensive crisis.
In contrast to adults, where acute hypertension is mostly due to uncontrolled primary hypertension, in children, hypertension is likely caused by an underlying secondary pathology. 8 The most common causes of hypertension in children are renal vascular disease including renal artery stenosis or renal vein thrombosis and renal parenchymal disease. 9 10
Essential hypertension is identifiable in children and adolescents and there is a strong association with obesity. 6 It is often associated with a positive family history of hypertension or cardiovascular disease. Amongst our cohort, all four patients with essential hypertension had a family history of hypertension and two were noted to be obese with none having any evidence of end organ damage. In the recently published clinical practice guidelines for screening and management of high blood pressure in children and adolescents, 7 it is recommended that hypertensive patients more than 6 years old who are overweight or obese and have a positive family history of hypertension and/or do not have history or physical examination findings suggestive of a secondary cause of hypertension do not require extensive evaluation for secondary causes of hypertension. It is also recommended that all children at or more than 3 years old have their blood pressure checked annually and those with obesity, renal disease, hypertension, history of obstruction or co-arctation of the aortic arch, diabetes are taking medications known to cause high blood pressure should have their blood pressure checked at every health care visit. In our institution, it is not a standard practice to monitor blood pressure regularly in well patients above 3 years old and thus, we would recommend blood pressure screening at every health care visit of children at risk of hypertension, regardless of age. All patients presenting with hypertensive crisis do warrant a thorough evaluation to look for an underlying secondary cause for hypertension as directed by their clinical symptoms, presentation, and examination findings.
A retrospective cohort study, looking at the etiology, treatment, and outcomes of the pediatric hypertensive crisis amongst pediatric patients presenting to Yonsei University Severance Hospital, South Korea, was performed by Lee et al. 1 In this study, all 51 patients received treatment with either labetalol, hydralazine, nicardipine or nitroprusside. In contrast, only 34 (72.3%) of our patients received antihypertensive medications. The rest of the patients were not treated with antihypertensive medication as their hypertension resolved after receiving targeted treatment for the underlying cause of hypertension. This included surgical intervention for renal, vascular, or cardiac causes and oncological causes or with prompt withdrawal of the offending agents. A possible reason for this could be the majority of the patients in the prior study had oncological causes for hypertension and thus, the difference in etiology of the hypertension could have resulted in higher treatment rates.
Available guidelines have recommended intravenous antihypertensive medication for severe hypertension with acute end organ damage. 6 In our institution, for patients with hypertensive crisis requiring prompt blood pressure control, intravenous labetalol was the drug of choice except in patients with hypertensive crisis secondary to poststreptococcal glomerulonephritis who were treated with intravenous furosemide. Most of our patients who were treated with intravenous labetalol required doses in the range of 0.25 to 2.5 mg/kg/h.
A retrospective study performed in Texas, United States, 11 reported the safe use of intravenous labetalol in 21 infants and small children less than 2 years old with hypertensive crisis. All patients who had received intravenous labetalol had significant reduction of blood pressure within 6 hours and the time taken to reduce blood pressure by 20%. Labetalol was found to be safe with reported hypoglycemia and hypotension in two patients. The efficacy and good safety profile of labetalol are the reasons it is favored as our first line intravenous antihypertensive in our institution. Other intravenous antihypertensives internationally used include enalaprilat, hydralazine, nicardipine, and esmolol. 11 12 However, nicardipine and enalaprilat are not available in our local formulary and thus, local availability may drive the choice of antihypertensive agents.
In adults, the use of short acting nifedipine has been associated with an increased risk of renal, cerebral, or coronary ischemia and is no longer considered acceptable for the initial treatment of hypertensive crisis. 13 Oral nifedipine is not on the recommended list of the oral medication that may be used in the treatment of acute severe hypertension in the latest clinical practice guidelines on the management of hypertension in children and adolescents. 7 However, it has been and is still widely prescribed by pediatricians in the treatment of acute hypertension in children due to the efficacy in blood pressure control and its safety profile. 13 Egger et al and Blaszak et al 14 15 reported that nifedipine is effective and safe in the treatment of acute hypertension in children in the hospital setting. In a retrospective study in Canada, 198 children received short acting nifedipine for hypertension over 3 years at five pediatric hospitals. Eighty-five percent of hypertensive episodes resolved and 5.1% had minor adverse events with only two patients experiencing serious adverse events which involved reduction of blood pressure of more than 40% but both were asymptomatic and recovered with restoration of normal blood pressure within 2 hours. 13 In our study, nifedipine was commonly used as initial treatment for patients who presented with hypertensive crisis. There were no known significant adverse events related to the use of nifedipine in our patients from this study. The pediatric population may be better able to tolerate nifedipine as children typically do not have significant vascular and cardiovascular risk factors, unlike the adult population, which result in significant mortality and morbidity from large changes in end organ perfusion.
There are limitations in our study. First, as hypertensive crisis is not common in children, the number of subjects in our study were small. Second, our methodology could have limited the search subjects with discharge diagnosis coded under the primary diagnosis instead of “hypertension.” As most of the cases of hypertension were referred to our nephrology unit, we attempted to broaden our search by going through the records of all the referrals made to the Nephrology Service during the study period. Nevertheless, in our knowledge, this is the first study looking at the epidemiology and treatment of hypertensive crisis in Singapore. We also used the initial blood pressure on arrival to the children's emergency to classify these patients and thus, as blood pressure is variable, especially when a child is sick or stressed about being brought into the emergency department, it could have been falsely elevated. Looking at the blood pressure trend over the course of the hospital stay could have been more accurate. We also recruited patients who were referred to the nephrology service and thus, this could have led to an over representation of renal pathology amongst subjects.
Conclusion
Majority of children with hypertensive crisis have secondary hypertension. Thorough evaluation for an underlying cause of secondary hypertension could result in prompt and appropriate treatment for the underlying cause and result in complete resolution of hypertension. This is evidenced by the majority of our patients not requiring antihypertensive treatment on discharge. Choice of antihypertensive medication is largely based on the underlying cause for hypertension, the presence of acute end organ damage and the urgency for rapid blood pressure control. More studies are needed to evaluate the optimal medical treatment of pediatric hypertensive crisis and its outcomes.
Key Findings
Renal pathology is the most common cause of secondary hypertension.
In our experience, oral nifedipine was the most commonly used antihypertensive and appeared safe in children with hypertensive crisis.
Footnotes
Conflict of Interest None declared.
References
- 1.Lee G H, Lee I R, Park S J, Kim J H, Oh J Y, Shin J I. Hypertensive crisis in children: an experience in a single tertiary care center in Korea. Clin Hypertens. 2016;22:10. doi: 10.1186/s40885-016-0040-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta-Malhotra M, Banker A, Shete S et al. Essential hypertension vs. secondary hypertension among children. Am J Hypertens. 2015;28(01):73–80. doi: 10.1093/ajh/hpu083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lurbe E, Agabiti-Rosei E, Cruickshank J K et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34(10):1887–1920. doi: 10.1097/HJH.0000000000001039. [DOI] [PubMed] [Google Scholar]
- 4.Miyashita Y, Peterson D, Rees J M, Flynn J T. Isradipine for treatment of acute hypertension in hospitalized children and adolescents. J Clin Hypertens (Greenwich) 2010;12(11):850–855. doi: 10.1111/j.1751-7176.2010.00347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flynn J T. Hypertension in the young: epidemiology, sequelae and therapy. Nephrol Dial Transplant. 2009;24(02):370–375. doi: 10.1093/ndt/gfn597. [DOI] [PubMed] [Google Scholar]
- 6.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents.The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents Pediatrics 2004114(2 Suppl 4th Report):555–576. [PubMed] [Google Scholar]
- 7.Flynn J T, Kaelber D C, Baker-Smith C M et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(03):e20171904. doi: 10.1542/peds.2017-1904. [DOI] [PubMed] [Google Scholar]
- 8.Singh D, Akingbola O, Yosypiv I, El-Dahr S. Emergency management of hypertension in children. Int J Nephrol. 2012;2012:420247. doi: 10.1155/2012/420247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang W C, Lin M J, Chen C Y, Wu H P. Clinical overview of hypertensive crisis in children. World J Clin Cases. 2015;3(06):510–513. doi: 10.12998/wjcc.v3.i6.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stein D R, Ferguson M A. Evaluation and treatment of hypertensive crises in children. Integr Blood Press Control. 2016;9:49–58. doi: 10.2147/IBPC.S50640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas C A, Moffett B S, Wagner J L, Mott A R, Feig D I. Safety and efficacy of intravenous labetalol for hypertensive crisis in infants and small children. Pediatr Crit Care Med. 2011;12(01):28–32. doi: 10.1097/PCC.0b013e3181e328d8. [DOI] [PubMed] [Google Scholar]
- 12.Webb T N, Shatat I F, Miyashita Y. Therapy of acute hypertension in hospitalized children and adolescents. Curr Hypertens Rep. 2014;16(04):425. doi: 10.1007/s11906-014-0425-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yiu V, Orrbine E, Rosychuk R J et al. The safety and use of short-acting nifedipine in hospitalized hypertensive children. Pediatr Nephrol. 2004;19(06):644–650. doi: 10.1007/s00467-004-1444-x. [DOI] [PubMed] [Google Scholar]
- 14.Egger D W, Deming D D, Hamada N, Perkin R M, Sahney S. Evaluation of the safety of short-acting nifedipine in children with hypertension. Pediatr Nephrol. 2002;17(01):35–40. doi: 10.1007/s004670200006. [DOI] [PubMed] [Google Scholar]
- 15.Blaszak R T, Savage J A, Ellis E N. The use of short-acting nifedipine in pediatric patients with hypertension. J Pediatr. 2001;139(01):34–37. doi: 10.1067/mpd.2001.114699. [DOI] [PubMed] [Google Scholar]


