Abstract
To assess the impact of organization-directed workplace interventions on physician burnout, including stress or job satisfaction in all settings, we conducted a systematic review of the literature published from January 1, 2007, to October 3, 2018, from multiple databases. Manual searches of grey literature and bibliographies were also performed. Of the 633 identified citations, 50 met inclusion criteria. Four unique categories of organization-directed workplace interventions were identified. Teamwork involved initiatives to incorporate scribes or medical assistants into electronic health record (EHR) processes, expand team responsibilities, and improve communication among physicians. Time studies evaluated the impact of schedule adjustments, duty hour restrictions, and time-banking initiatives. Transitions referred to workflow changes such as process improvement initiatives or policy changes within the organization. Technology related to the implementation or improvement of EHRs. Of the 50 included studies, 35 (70.0%) reported interventions that successfully improved the 3 measures of physician burnout, job satisfaction, and/or stress. The largest benefits resulted from interventions that improved processes, promoted team-based care, and incorporated the use of scribes/medical assistants to complete EHR documentation and tasks. Implementation of EHR interventions to improve clinical workflows worsened burnout, but EHR improvements had positive effects. Time interventions had mixed effects on burnout. The results of our study suggest that organization-directed workplace interventions that improve processes, optimize EHRs, reduce clerical burden by the use of scribes, and implement team-based care can lessen physician burnout. Benefits of process changes can enhance physician resiliency, augment care provided by the team, and optimize the coordination and communication of patient care and health information.
Abbreviations and Acronyms: EHR, electronic health record; MBI, Maslach Burnout Inventory; WTR, Working Time Regulations
Article Highlights.
-
•
There is increasing awareness that physician burnout is a cause of diminished health and retention of physicians and their care teams, quality of patient care, and viability of health care systems. Many causes of burnout derive from organizational- and system-level factors, including electronic health records (EHRs).
-
•
Most studies evaluating the impact of organization-directed interventions on physician burnout are of poor quality. More randomized controlled trials are needed to adequately test the effect of organization-directed interventions on physician burnout.
-
•
There is evidence from a few high-quality studies that (1) the largest benefits result from interventions that improve workplace processes, promote team-based care, and incorporate the use of scribes or medical assistants to complete EHR documentation and tasks; (2) modifications to intensivists’ schedules for shift work or interrupted schedules significantly reduces burnout; and (3) duty hour requirements and protected sleep have no significant effect on reducing burnout among residents.
-
•
Evidence from poor-quality studies suggests that EHR training and technological improvements of EHR reduce burnout; however, evidence from high-quality studies is needed to identify which technological improvements have the greatest impact.
The prevalence of physician burnout is substantial, with more than half of US physicians reporting at least one symptom of burnout, which is significantly higher than that in the general population.1 Burnout is defined as a long-term stress reaction marked by loss of enthusiasm for work (emotional exhaustion), feelings of cynicism (depersonalization), and a lack of sense of personal accomplishment.2 Causes of physician burnout include time pressure, chaotic environments, requirements for electronic health records (EHRs), and responsibilities outside of work.3
Physician burnout can affect physician health and quality of care.4, 5, 6 As a result of stress, physicians may experience depression or anxiety, may engage in alcohol and/or drug abuse,7 and have suicide rates that are 1.2 to 2.4 times higher than that of the general population.8 Work-related stress can also lead to lower patient satisfaction and care quality and increased medical error rates and malpractice risk.9, 10, 11 Burnout also has potentially serious financial implications for the health care system12, 13, 14 by leading to physician shortages and in costs to replace a physician, which can exceed $500,000 to $1,000,000 per physician.5, 15
Interventions to address burnout have been classified as either physician-directed or organization-directed.16 Physician-directed interventions aim to enhance resilience among physicians through activities such as promoting mindfulness or cognitive behavioral techniques to improve an individual’s ability to cope, communicate effectively, and increase competency. However, these supportive physician-directed approaches may be insufficient because they address individual solutions. Burnout more often stems from organizational- or system-level factors,17 and interventions to prevent burnout may be more effective when they focus on changing the system rather than individual physicians.16 Some examples of organization-directed interventions include changing schedules, reducing the intensity of workloads, improving teamwork, and increasing physician participation in decision making.
To date, the effectiveness of organization-directed workplace or workflow interventions has not been fully examined. The objective of this review was to assess the evidence on the effect of organization-directed workplace interventions on physician burnout systematically.
Methods
Search Strategy
MEDLINE, Embase, and the Cochrane Library databases were searched on October 3, 2018, for relevant articles published in English from January 1, 2007, to October 3, 2018, that reported on organization-directed interventions for physician burnout related to work, the workplace, or workflow. Search terms included physician, burnout, stress, workflow, time and motion studies, lean, work engagement, psychosocial factors, work behaviors, health outcomes, job performance, job satisfaction, job-person fit, organizational factors, and quadruple aim. Manual searches of grey literature including key conferences and organization websites and bibliographies were also performed. Search details are available in Supplemental Tables 1 through 7 (available online at http://www.mcpiqojournal.org).
Screening Process
One investigator (K.J.T.C. or A.A.) screened all titles and abstracts for eligibility against a priori established inclusion criteria (Supplemental Table 8, available online at http://www.mcpiqojournal.org). Studies marked for inclusion underwent full-text screening by 2 independent reviewers (K.J.T.C. and A.A.), and discrepancies were resolved by adjudication or, if necessary, by a third reviewer. All results at both title/abstract and full-text review stages were tracked in DistillerSR (Evidence Partners).
Data Extraction and Quality Assessment
Included studies were extracted into structured forms by one reviewer (A.A.) and checked for accuracy and completeness by a second (K.J.T.C). Study quality was assessed using the Oxford Centre for Evidence-based Medicine Levels of Evidence18 (Table 1) by 2 independent reviewers (K.J.T.C. and A.A.), and disagreements were resolved by a third reviewer (T.B.).
Table 1.
Study Characteristics Stratified by Intervention Typea
| Reference, year | Country | Study design | No. of participants | Population and setting | Type of intervention | Outcome | Follow-up | Level of evidenceb |
|---|---|---|---|---|---|---|---|---|
| Teamwork (N=20) | ||||||||
| Chapman & Blash,19 2017 | United States | Cross-sectional | 886 | Primary care practices | Teamwork: Employing medical assistants in an innovative model of care with new roles with a focus on career advancement, training, and enhanced compensation for the new medical assistant roles | Staff satisfaction | 4 y | 4 |
| Contratto et al,20 2016 | United States | Pre-post intervention survey | 9 | Physicians Urban academic general internal medicine primary care practice |
Teamwork: To evaluate the impact of using full-time clerical support to enter tests ordered by physicians, identify incomplete health maintenance measures, and preload new patient information | 14-Item survey | 4 mo | 4 |
| Contratto et al,21 2017 | United States | Quasi-experimental (single-group pre-post intervention) mixed-methods | 7 | Academic general internal medicine practice | Teamwork: Clerical support personnel for physician order entry | Physician satisfaction | 4 mo | 4 |
| Danila et al,22 2018 | United States | Pre-post intervention survey | 6 | Physicians (3 rheumatologists and 3 endocrinologists) Rheumatology and endocrinology clinics |
Teamwork: Use of scribes | JSS | 6 wk | 4 |
| Gidwani et al,23 2017 | United States | RCT | 4 | Physicians Academic family medicine clinic |
Teamwork: Use of scribes to draft all relevant documentation | Physician satisfaction, measured by a 5-item instrument that included physicians’ perceptions of medical record quality and accuracy | 1 y | 1b |
| Heaton et al,24 2016 | Multinational | Systematic review | NA | NA | Teamwork: Use of scribes | Physician satisfaction | NA | 4 |
| Hung et al,25 2018 | United States | Pre-post intervention survey | 680 | Physicians 46 Primary care departments in a large ambulatory care delivery system |
Teamwork/Transitions: Lean-based workflow redesigns, which included colocating physician and medical assistant dyads, delegating major responsibilities to nonphysician staff, and mandating greater coordination and communication among all care team members | MBI | 3 y | 4 |
| Imdieke & Martel,26 2017 | United States | Quasi-experimental, nonrandomized pre- and post-intervention study | 2 | Internal medicine physicians Hospital-based, outpatient primary care clinic |
Teamwork: Incorporating medical scribes in an ambulatory clinic to support physician documentation in the electronic medical record | Physician satisfaction | 4-6 wk | 4 |
| Koshy et al,27 2010 | United States | Nonrandomized, static-group comparison study | 5 | Urologists, residents Urology clinic within a single academic medical center |
Teamwork: Scribes to record electronic medical information throughout the patient-physician encounter | Physician acceptance and satisfaction | 10 mo | 4 |
| Linzer et al,28 2015 | United States | Cluster RCT | 166 (135 completed the study) | Primary care physicians (family and general internists) 34 Clinics in Upper Midwest and NYC |
Teamwork/Transitions: Projects to improve communication, changes in workflow, and targeted quality improvement projects | Survey tools from MEMO and PWS | 12 mo, 18 mo | 2b |
| Linzer et al,29 2017 | United States | Cluster RCT | 165 | Primary care physicians (family and general internists) 34 Clinics in Upper Midwest and NYC |
Teamwork/Transitions: Quality improvement projects to improve communication between physicians, workflow design, and chronic disease management | OWL | 6 mo, 12 mo | 2b |
| McCormick et al,30 2018 | United States | Pre-post intervention survey | 6 | Urologists Academic urology clinic |
Teamwork: Use of scribes | Work satisfaction | 3 mo | 4 |
| Pierce et al,31 2017 | United States | Pre-post intervention survey | 55 | Physicians and advanced practice clinicians Academic hospital |
Teamwork: 13 Team-based and organizational tactics to improve resilience, including expansion of leadership roles, faculty coaching for new hires, and value-based clinical schedule redesign | NR | 3 y | 4 |
| Pozdnyakova et al,32 2018 | United States | Prospective, pre-post pilot study | 6 | General internal medicine faculty | Teamwork: Use of scribes to complete EHR | Workplace satisfaction; burnout | 1 wk | 4 |
| Quenot et al,33 2012 | France | Longitudinal, monocentric, before-and-after, interventional study | 4 | Physicians ICU |
Teamwork: Intensive communication strategy regarding end-of-life practices in the ICU to alleviate stress for caregivers | MBI | Post-intervention | 4 |
| Shaw et al,34 2017 | United States | Pre-post intervention survey | NR | Medical doctors NR |
Teamwork: Team-based primary care redesign, “Primary Care 2.0”, with the goal of addressing the Quadruple Aim of health care (ie, the Triple Aim plus reducing workforce burnout) with the following components: (1) an expanded “care coordinator” role for medical assistants including scribing, population health management, and between-visit care management, (2) health coaching and motivational interviewing, (3) “lean” quality improvement to support a Learning Health System, (4) telehealth, (5) protected physician time for care coordination, and (6) an onsite extended interdisciplinary care team (ie, mental health, pharmacy, physical therapy) | NR | 5 mo | 4 |
| Shultz & Holmstrom,35 2015 | Multinational | Systematic review | NA | Emergency department, urology, or cardiology clinicians | Teamwork: Use of scribes | Clinician satisfaction | NA | 4 |
| Was & Cornaby,36 2016 | United States | Pre-post intervention survey | 23 | Residents Large academic center |
Teamwork: Common space for residents (ie, “Gas Lounge”) | NR | Post-intervention | 4 |
| West et al,37 2014 | United States | RCT | 74 | Physicians Department of medicine at the Mayo Clinic |
Teamwork: 19 Biweekly facilitated physician discussion groups incorporating elements of mindfulness, reflection, shared experience, and small group learning | JSS, Empowerment at Work Scale, Medical Outcomes Study Short-Form Health Survey, MBI, Perceived Stress Scale, Jefferson Scale of Physician Empathy | 1 y | 1b |
| Willard-Grace et al,38 2017 | United States | Cross-sectional | 236 | Clinicians County-run primary care clinics |
Teamwork: A defined model of team-based care in which the association between enhanced roles for medical assistants, registered nurses, and behavioral health professionals is defined | MBI | NR | 4 |
| Time (N=14) | ||||||||
| Ali et al,39 2011 | United States | Cluster RCT | 45 | Physicians with various specialties ICU |
Time: Two intensivist staffing schedules were compared: continuous and interrupted (rotations every 2 wk) for 14 mo | Scales derived from the National Study of the Changing Workforce | 9 mo | 1b |
| Desai et al,40 2018 | United States | Cluster-randomized trial | 80 | First-year residents 63 Internal medicine residency practices |
Time: Duty hour policies of the 2011 ACGME | Overall well-being, MBI | 7 mo | 1b |
| Fassiotto & Maldonado,41 2016 | United States | Pre-post intervention survey | 60 | Medical school faculty NR |
Time: Time-banking intervention measures unacknowledged teaching, service, and clinical activities and acknowledges them with practical rewards | NR | Post-intervention | 4 |
| Garland et al,42 2012 | Canada | Crossover RCT | 34 | Physicians ICU |
Time: Shift work staffing in which there was 24-7 intensivist presence. The same pool of intensivists supplied day shift and night shift coverage. In any given week, a single intensivist was responsible for all 7-day shifts, whereas 2 different intensivists alternated the 7 night shifts | MBI (emotional exhaustion subscale) | Post-intervention | 1b |
| Kim & Wiedermann,43 2011 | United States | Prospective cohort | 56 | Residents Large pediatric training program |
Time: 2003 ACGME work hour limits | NR | 7 y | 4 |
| Landrigan et al,44 2008 | United States | Prospective cohort | 220 | Residents Pediatric residency programs at hospitals |
Time: 2003 ACGME work hour limits for US resident physicians. Residents can work no more than 30 consecutive hours and no more than 80 to 88 h/wk, averaged over 4 wk | MBI | 1 y | 4 |
| Lucas et al,45 2012 | United States | Cluster randomized crossover noninferiority trial | 62 | Physicians University-affiliated teaching hospital |
Time: Assignment to random sequences of 2- and 4-wk rotations | Questionnaire includes questions from MEMO study, Perceived Stress Scale, MBI, national job burnout survey | 2/4 wk | 1b |
| Moeller & Walker,46 2017 | United States | Pre-post intervention survey | NR | Physicians NR |
Time: Practice Refresh pilot program that initially reduces and then gradually increases the time physicians spend with patients so that physicians can learn and practice skills in efficiency, teamwork, and self-care | NR | NR | 4 |
| Morrow et al,47 2014 | United Kingdom | Cross-sectional | 82 | Junior doctors Deanery |
Time: United Kingdom WTR applied fully to junior doctors since 2009, with a limit of 48 h/wk, averaged across a reference period of 26 wk, alongside specified minimum rest periods | NA | NA | 4 |
| Parshuram et al,48 2015 | Canada | RCT | 47 | Residents University-affiliated ICUs |
Time: In-house overnight schedules of 24, 16, or 12 h | MBI | 2 mo | 2b |
| Ripp et al,49 2015 | United States | Pre-post intervention survey | 128 (2011-2012 cohort); 111 (2008-2009 cohort) | Internal medicine residents Academic medical centers |
Time: 2011 ACGME modified duty hours standards to limit continuous duty of first-year residents to 16 h | MBI, ESS | 1 y | 4 |
| Schuh et al,50 2011 | United States | Prospective, unblinded study | 34 | Neurology residents Neurology residency program |
Time: 2008 Institute of Medicine work duty hour recommendations that limit shifts to 16 or 24 h with a 5-h nap, eliminate averaging of any on-call shifts, increase time off between shifts for night float and overnight call, limit consecutive night float shifts to 4, and provide 1 d off/wk/5 per mo without averaging | MBI | 1 mo | 4 |
| Shea et al,51 2014 | United States | RCT | 106 | Graduate internal medicine interns Internal medicine service hospital |
Time: A 2-h period of protected time in which interns were expected to sleep (12:30 am-5:30 am) for 4 wk | MBI | Post-intervention | 1b |
| Tucker et al,52 2010 | Wales | Cross-sectional | 336 | Residents and interns NR |
Time: Schedule design | Questionnaire developed for study | NA | 4 |
| Transitions (N=9) | ||||||||
| Albadry et al,53 2014 | Egypt | Cross-sectional | 140 | Residents and assistant lecturers Outpatient clinic |
Transitions: Six Sigma methodology as quality improvement intervention | MBI | 6 mo | 4 |
| Amis & Osicki,54 2018 | United Kingdom | Pre-post intervention survey | 13 | First-year residents | Transitions: A checklist aimed to reduce the number of inappropriate prescribing tasks | Job satisfaction | 3 Weekends | 4 |
| Callahan et al,55 2018 | United States | Pre-post intervention survey | 9 | Fellows NR |
Transitions: Bundle of evidence-based interventions to improve burnout and professional satisfaction that were designed to fit the fellowship program | ESS, quality of life | 6 mo | 4 |
| Dunn et al,56 2007 | United States | Noncontrolled prospective intervention study | 22-32 | Physicians Primary care group |
Transitions: Data-guided interventions and systematic improvement processes that included (1) leadership valuing physician well-being equal to quality of care and financial stewardship, (2) physicians identifying factors that influenced well-being, followed by plans for improvement with accountability, and (3) measuring the well-being of physicians regularly using validated instruments | ACP/ASIM survey on physician satisfaction, MBI | 6 y | 4 |
| Giannini et al,57 2013 | Italy | Pre-post intervention survey | 71 | Doctors ICU |
Transitions: Increase in daily visiting time to at least 8 h (policy change) | MBI, STAI | 6 mo, 12 mo | 4 |
| Hung et al,25 2018 | United States | Pre-post intervention survey | 680 | Physicians 46 Primary care departments in a large ambulatory care delivery system |
Teamwork/Transitions: Lean-based workflow redesigns, which included colocating physician and medical assistant dyads, delegating major responsibilities to nonphysician staff, and mandating greater coordination and communication among all care team members | MBI | 3 y | 4 |
| Lee et al,58 2017 | United States | Pre-post intervention survey | Baseline, 18; postin-tervention, 15 | Neuroradiology fellows and neuroradiologists Academic neuroradiology practice, part of a larger health care system with 6 hospitals and 80 outpatient imaging sites |
Transitions: Image interpretive and non–image interpretive reading room workflows | 14-Question survey, Likert scale rating 1-5 | 1 mo | 4 |
| Linzer et al,28 2015 | United States | Cluster RCT | 166 (135 completed the study) | Primary care physicians (family and general internists) 34 Clinics in Upper Midwest and NYC |
Teamwork/Transitions: Projects to improve communication, changes in workflow, and targeted quality improvement projects | Survey tools from MEMO and PWS | 12 mo, 18 mo | 2b |
| Linzer et al,29 2017 | United States | Cluster RCT | 165 | Primary care physicians (family and general internists) 34 Clinics in Upper Midwest and NYC |
Teamwork/Transitions: Quality improvements projects to improve communication between physicians, workflow design, and chronic disease management | OWL | 6 mo, 12 mo | 2b |
| Technology (N=10) | ||||||||
| Agha et al,59 2010 | United States | NR | 9 | Pulmonary, rheumatology, and endocrine physicians NR |
Technology: To measure the impact of EHR use on physician satisfaction | NR | NR | 4 |
| Babbott et al,60 2013 | United States | Prospective | 422 | Internal medicine and family medicine physicians | Technology: Secondary analysis on data from the MEMO study in which physicians and office managers completed questionnaires about their office practice, including specific EHR features the office used | NR | NR | 4 |
| Beam et al,61 2017 | United States | Pre-post intervention survey | 158 | Physicians Neonatal ICU |
Technology: Computerized physician order entry implementation | Job satisfaction | 1 y | 4 |
| Ehrlich et al,62 2016 | United States | Pre-post intervention survey | 25 | Ophthalmologists Large academic ophthalmology department |
Technology: EHR system | 30-Question survey using Likert scale rating, job satisfaction | 24 mo | 4 |
| Heyworth et al,63 2012 | United States | Pre-post intervention survey | 163 | Primary care and specialty NR |
Technology: To measure predictors of physician satisfaction following EHR adoption | Massachusetts eHealth Collaborative survey | Post-intervention | 4 |
| Joseph et al,64 2017 | United States | Pre-post intervention survey | NR | Physicians NR |
Technology: The impact of a brief, intensive technology deployment and training intervention that was aimed at improving individual clinician’s efficiency in using EHR | NR | NR | 4 |
| Lapointe et al,65 2018 | United States | Pre-post intervention survey | 25 | Internal medicine residents 591-Bed urban hospital |
Technology: EHR-based text paging system to communicate with internal medicine residents | Stress | 6 mo | 4 |
| Menachemi et al,66 2009 | United States | Cross-sectional | 4203 | Primary care physicians and clinical specialists Outpatient settings |
Technology: To evaluate the relationship between physician IT adoption and practice satisfaction | Survey using Likert scale questions on job/practice satisfaction | NA | 4 |
| Milenkiewicz,67 2017 | United States | Pre-post intervention survey | NR | Physicians Department of Addiction Medicine at Kaiser Permanente |
Technology: To test the usability of an EHR tool to improve and standardize the documentation process | NR | Post-intervention | 4 |
| Wylie et al,68 2014 | United States | Cross-sectional | 2365 | Primary care physicians Practice with more than 10 physicians |
Technology: To identify how EHR use affected clinical practice | Likert-type scale questions regarding how EHR affected medical practice | NA | 4 |
ACGME = Accreditation Council for Graduate Medical Education; ACP/ASIM = American College of Physicians/American Society of Internal Medicine; her = electronic health record; ESS = Epworth Sleepiness Scale; JSS = Physician Job Satisfaction Scale; ICU = intensive care unit; IT = information technology; MBI = Maslach Burnout Inventory; MEMO = Minimizing Error, Maximizing Outcome; NA = not available; NR = not reported; NYC = New York City; OWL = Office and Work Life measures; PWS = Physician Worklife Study; RCT = randomized controlled trial; STAI = State-Trait Anxiety Inventory; WTR = Working Time Regulations.
Oxford Centre for Evidence-based Medicine Levels of evidence18: 1b = individual RCT (with narrow confidence interval); 2b = individual cohort study (including low-quality RCT; eg, <80% follow-up); 4 = case series (and poor-quality cohort and case control studies).
Results
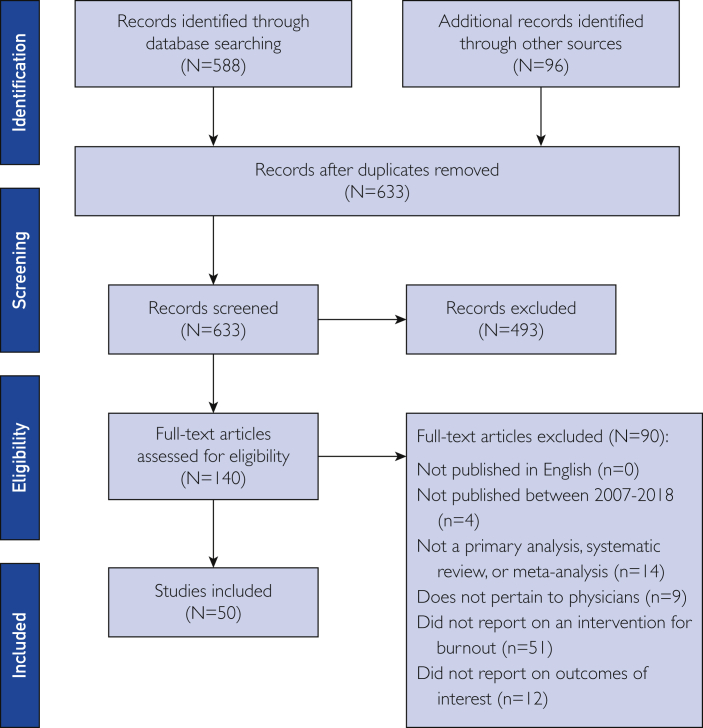
Literature searches yielded 633 unique citations (Figure 1), of which 140 articles were eligible for full-text screening. Following full-text screening, 50 citations were included in the study,19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68 of which 36 (72.0%) were full-length articles19, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 32, 33, 35, 37, 39, 40, 42, 44, 45, 47, 48, 49, 50, 51, 52, 54, 56, 57, 58, 61, 62, 63, 65, 66, 68 and 14 (28.0%) were conference abstracts.20, 31, 34, 36, 38, 41, 43, 46, 53, 55, 59, 60, 64, 67
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram69 of literature search.
Study and Physician Characteristics
Table 1 presents the characteristics of the 50 included studies.19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68 Most (40) studies were from the United States,19, 20, 21, 22, 23, 25, 26, 27, 28, 29, 30, 31, 32, 34, 36, 37, 38, 39, 40, 41, 43, 44, 45, 46, 49, 50, 51, 55, 56, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68 followed by Europe (5),33, 47, 52, 54, 57 Canada (2),42, 48 Egypt (1),53 and multinational (2).24, 35 Study designs included randomized controlled trials (10),23, 28, 29, 37, 39, 40, 42, 45, 48, 51 pre-post intervention surveys (24),20, 21, 22, 25, 26, 30, 31, 32, 33, 34, 36, 41, 46, 49, 54, 55, 57, 58, 61, 62, 63, 64, 65, 67 prospective studies (5),43, 44, 50, 56, 60 cross-sectional studies (7),19, 38, 47, 52, 53, 66, 68 and other designs (4).24, 27, 35, 59 The included studies evaluated interventions among primary care physicians and residents (12),19, 20, 21, 23, 25, 26, 28, 29, 38, 56, 60, 68 inpatient and outpatient secondary care physicians (eg, intensive care, surgery) (15),22, 27, 30, 32, 33, 35, 39, 42, 55, 57, 58, 59, 61, 62, 67 residents (eg, intensive care, internal medicine, neuroradiology, pediatric) (13),36, 40, 43, 44, 47, 48, 49, 50, 51, 52, 53, 54, 65 a mixture of primary and secondary care physicians (3),31, 63, 66 and groups of physicians with specialty unspecified (7).24, 34, 37, 41, 45, 46, 64
Measures of Burnout
The most frequently used measure of burnout (15 studies) was the Maslach Burnout Inventory (MBI), a validated measure considered the criterion standard for identifying burnout.25, 33, 37, 38, 40, 42, 44, 45, 48, 49, 50, 51, 53, 56, 57 Sixteen studies developed their own surveys to measure outcomes related to physician burnout including job satisfaction, burnout, depersonalization, fatigue, and stress.19, 20, 21, 23, 26, 27, 30, 32, 52, 54, 58, 61, 62, 65, 66, 68 Additional measures included the Physician Job Satisfaction Scale,22, 37 Epworth Sleepiness Scale,49, 55 Office and Work Life measures,29 survey tools from the Minimizing Error, Maximizing Outcome study and the Physician Worklife Study,28 scales derived from the National Study of the Changing Workforce,39 Massachusetts eHealth Collaborative survey,63 and American College of Physicians/American Society for Internal Medicine physician satisfaction survey.56 Two studies34, 64 provided qualitative findings, and 10 studies did not report the instrument used to measure burnout.31, 35, 36, 41, 43, 46, 47, 59, 60, 67
Characteristics of Organization-Directed Interventions
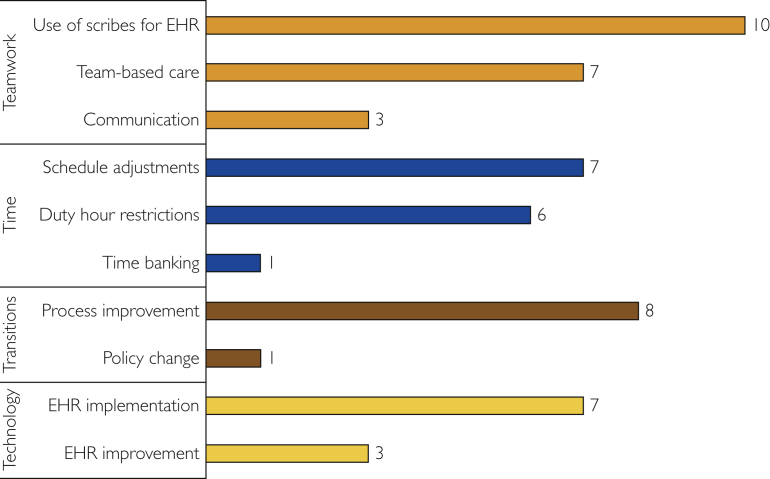
Interventions were categorized into the “4Ts,” a unique categorization created for this study: Teamwork, Time, Transitions, and Technology. Figure 2 provides an overview of the types of interventions and number of studies that fell into each category. Teamwork involved initiatives to incorporate scribes into EHR processes, expand team responsibilities, and improve communication among physicians. Studies about Time evaluated the impact of duty hour limits, schedule changes, and time-banking initiatives. Transitions referred to workflow changes such as process improvement initiatives or policy changes within the organization. Technology related to the implementation or improvement of EHRs.
Figure 2.
Number of studies by intervention type. EHR = electronic health record.
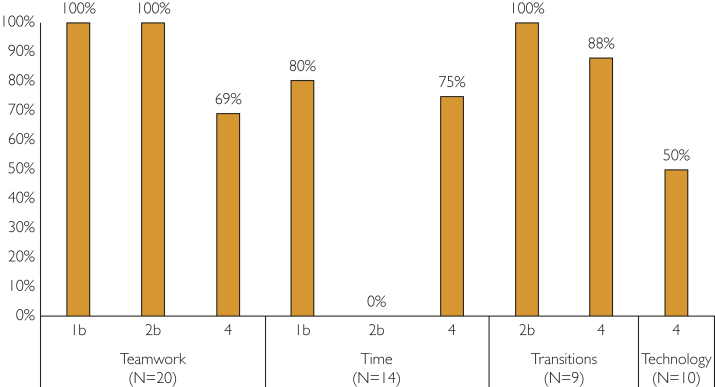
Thirty-eight of the 50 studies were designed to measure the effect of an organization-directed workplace intervention on physician burnout, job satisfaction, or stress. Eleven of the remaining 12 studies (22.0%) employed a workplace modification not specifically designed to address burnout but included outcomes related to it (the 12th study was a systematic review of several interventions that are included in the 50 studies we assessed). Thirty-five of the 50 workplace interventions (70.0%) successfully decreased physician burnout or stress and/or improved job satisfaction (Figure 3). A large proportion of interventions pertaining to Teamwork and Transitions had a positive impact on burnout, whereas, interventions categorized as Time and Technology had a less consistent overall impact on burnout.
Figure 3.
Proportion of interventions with a positive impact on burnout, stratified by intervention type and quality of evidence. The x-axis represents the category of intervention and the study quality; the y-axis represents the proportion of articles with a positive impact on reducing physician burnout or related measures. Each bar describes the proportion of studies with a positive impact on physician burnout that fell into the indicated level of quality and type of intervention. Levels of evidence: 1b = individual randomized controlled trial (with narrow confidence interval); 2b = individual cohort study (including low-quality randomized controlled trials; eg, less than 80% follow-up); 4 = case series (and poor-quality cohort and case-control studies).
Study Quality
The evaluation of study quality using the Oxford Centre for Evidence-based Medicine Levels of Evidence18 is shown in Table 1. The majority of the studies (40 [80.0%]) were categorized as level 4 studies, which includes case series, pretest and posttest single-arm, cross-sectional, and poor-quality cohort studies.19, 20, 21, 22, 24, 25, 26, 27, 30, 31, 32, 33, 34, 35, 36, 38, 41, 43, 44, 46, 47, 49, 50, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68 High-quality studies were limited to Teamwork, Time, and Transitions interventions (Figure 3).
Teamwork
Twenty of the 50 included studies focused on improving teamwork through team-based care models, use of scribes to enter EHR data, and encouraging communication between physicians.19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38 All of these subcategories of teamwork generally improved burnout, satisfaction, and stress (Table 2). A cross-sectional survey associated greater perceived capabilities of the care team with lower prevalence of exhaustion and cynicism, a higher likelihood to recommend the clinic as a place to work, and greater feasibility of providing primary care.38 Expanding the duties of medical assistants to add EHR documentation, health coaching, or navigation and/or management of population health and between-visit care improved survey scores of professional fulfillment34 and practice satisfaction.19, 23, 24, 26, 27, 30, 35 Notably, 9 of the 20 studies examined the impact of scribes, and 7 of the 9 studies examining the use of scribes successfully improved clinic workflow efficiencies.20, 21, 23, 24, 26, 27, 30 Finally, providing full-time clerical support for physician order entry in primary care (n=16) also decreased weekly self-reported burnout (baseline, 43%; 4-month follow-up, 14%; P=not reported).20
Table 2.
Study Results Stratified by Outcomea
| Intervention category | Reference, yearb | Burnoutc | Satisfactiond | Stresse |
|---|---|---|---|---|
| Teamwork | ||||
| Team-based care | Chapman & Blash,19 2017 | - | ↑* | - |
| Hung et al,25 2018 | ↑+++ | ↑+ | ↑+++ | |
| Linzer et al,28 2015 | ↓+ | NS | NS | |
| Linzer et al,29 2017 | - | ↑+++ | ↓+++ | |
| Pierce et al,31 2017 | ↓* | - | - | |
| Shaw et al,34 2017 | - | NS | - | |
| Willard-Grace et al,38 2017 | ↓++ | - | - | |
| Use of scribes for EHR | Contratto et al,20 2016 | ↓* | - | - |
| Contratto et al,21 2017 | ↓* | - | - | |
| Danila et al,22 2018 | - | NS | - | |
| Gidwani et al,23 2017 | - | ↑+++ | - | |
| Heaton et al,24 2016 | - | ↑* | - | |
| Imdieke & Martel,26 2017 | - | ↑+++ | - | |
| Koshy et al,27 2010 | - | ↑+++ | - | |
| McCormick et al,30 2018 | - | ↑+ | - | |
| Pozdnyakova et al,32 2018 | NS | - | - | |
| Communication | Linzer et al,28 2015 | NS | ↑+ | NS |
| Quenot et al,33 2012 | NS | - | - | |
| Was & Cornaby,36 2016 | - | ↑* | - | |
| West et al,37 2014 | ↓+ | - | NS | |
| Time | ||||
| Schedule adjustments | Ali et al,39 2011 | ↓++ | - | - |
| Garland et al,42 2012 | ↓+ | - | - | |
| Lucas et al,45 2012 | ↓+++ | - | - | |
| Moeller & Walker,46 2017 | - | ↑* | - | |
| Parshuram et al,48 2015 | NS | - | - | |
| Shea et al,51 2014 | NS | - | - | |
| Tucker et al,52 2010 | - | - | ↓++ | |
| Duty hour restrictions | Desai et al,40 2018 | ↓ + to ↓ +++ | ↓ + to +++ | - |
| Kim & Wiedermann,43 2011 | ↓+ | NS | - | |
| Landrigan et al,44 2008 | ↓ ++ | NS | - | |
| Morrow et al,47 2014 | - | - | ↑* | |
| Ripp et al,49 2015 | NS | - | - | |
| Schuh et al,50 2011 | ↑+ | ↓ + | - | |
| Time banking | Fassiotto & Maldonado,41 2016 | - | ↑+ | - |
| Transitions | ||||
| Process improvement | Albadry et al,53 2014 | ↓* | - | - |
| Amis & Osicki,54 2018 | - | ↑* | - | |
| Callahan et al,55 2018 | - | ↑++ | ||
| Dunn et al,56 2007 | ↓++ | NS | - | |
| Giannini et al,57 2013 | ↑++ | - | - | |
| Hung et al,25 2018 | ↑+++ | ↑+ | ↑+++ | |
| Lee et al,58 2017 | - | ↑+++ | ↓+++ | |
| Linzer et al,28 2015 | ↓+ | NS | NS | |
| Linzer et al,29 2017 | - | ↑+++ | ↓+++ | |
| Technology | ||||
| EHR implementation | Agha et al,59 2010 | - | ↓* | - |
| Babbott et al,60 2013 | NS | NS | ↑+ | |
| Beam et al,61 2017 | - | ↑* | - | |
| Ehrlich et al,62 2016 | - | NS | - | |
| Heyworth et al,63 2012 | - | - | ↑+ | |
| Menachemi et al,66 2009 | - | ↑++ | - | |
| Wylie et al,68 2014 | - | ↓+ | - | |
| EHR improvement | Joseph et al,64 2017 | - | ↑* | - |
| Lapointe et al,65 2018 | - | ↑* | ↓* | |
| Milenkiewicz,67 2017 | - | ↑* | - |
The arrows indicate the directionality of the intervention on the effect of burnout, satisfaction, and stress. Improvements are denoted by green color where the associations of the intervention on burnout or proxy measures were statistically significant. Red color indicates the intervention did not improve the burnout or proxy measure (by a nonsignificant result) or resulted in detractions whereby the outcome measure worsened with the intervention. White content with dashes indicates no data were reported. EHR = electronic health record; NS = not significant; + = P<.05; ++ = P<.01; +++ = P<.001; * = no P value reported.
Shultz and Holmstrom35 was not included in this table because it is a systematic review of several interventions. The relevant interventions are already included in the table under the original author names.
Burnout includes overall burnout, emotional exhaustion, depersonalization, personal accomplishment, and cynicism.
Satisfaction includes outcomes reported as satisfaction, professional fulfillment, well-being, and joy of practice.
Stress includes outcomes reported as stress, psychological strain, and job distress.
The benefits of increasing physician-to-physician communication by providing social support through the availability of physical spaces or allowing for more opportunities to connect with their peers was evaluated in 2 trials.36, 37 One of them, which randomized participants by sex and specialty, compared informal vs formal group curriculum to enhance communication.37 The curriculum allowed physicians to share personal and professional experiences, promote wellness and mental health, and improve their understanding of clinician-patient relationships. Depersonalization, emotional exhaustion, and overall burnout decreased substantially over 1 year in the group given the formal curriculum and increased in the informal group (P=.03 and P=.002, respectively).37
Time
Fourteen studies evaluated the effect of interventions limiting working hours, modifying work schedules, or promoting time banking to relieve physician burnout or stress or improve job satisfaction.39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52 Of these, 8 (57.1%) reported a positive impact (Figure 3, Table 2).39, 41, 42, 43, 44, 45, 46, 52 The effect on burnout of restricting the number of hours physicians are allowed to work, primarily residents or interns, was examined in 6 studies.40, 43, 44, 47, 49, 50 Only 2 of these studies found that limiting work hours alleviated burnout.43, 44 Both studies evaluated outcomes of the 2003 Accreditation Council for Graduate Medical Education duty hour restrictions. Additional studies that examined duty hour restrictions using 2008 Institute of Medicine and 2011 Accreditation Council for Graduate Medical Education guidelines noted a higher prevalence of burnout49 and depersonalization.50 Similarly, according to a qualitative evaluation of the 2009 UK Working Time Regulations (WTR), the WTR “actually increased fatigue and stress” due to the pressure to get the same amount of work done in a limited time frame.47 On the other hand, interns randomized to receive 5 hours of protected time to sleep while on call reported significantly lower levels of MBI-assessed emotional exhaustion and MBI-assessed depersonalization over 6 consecutive 4-week periods.51 Similarly, surveys of junior doctors found that after 6 months of WTR compliance, those working schedules that required 7 consecutive nights experienced a greater accumulation of fatigue when compared with those limited to working just 3 or 4 nights in row.52
A time-banking intervention for medical school faculty found that institutional recognition of time spent on additional activities, such as teaching, clinical service, and mentorship, improved job satisfaction (P=.02).41
Transitions
Nine of the 50 identified studies (18.0%) evaluated the effect of workflow changes in the workplace.25, 28, 29, 53, 54, 55, 56, 57, 58 Eight of these studies reported that changes to workflow redesign, including targeted quality improvement projects and separating workflows, had a substantial and positive impact on physician burnout, job satisfaction, and/or stress (Figure 3, Table 2).25, 28, 29, 53, 54, 55, 56, 58 Quality improvement interventions that improved processes ranged from streamlining prescribing tasks, establishing quality metrics, and changing workflows. Interventions were often described as evidence-based or utilized a specific methodology such as Six Sigma. The highest-quality study from this category observed a significant improvement in physician burnout following the implementation of quality improvement initiatives in areas that are most taxing for physicians, including improved routine screening processes and medication reconciliation (P=.02).28 Additionally, high-quality evidence revealed that physician satisfaction increased (P<.001) and stress decreased (P<.001) with quality improvement interventions.29
Technology
Ten studies focused on technological interventions to improve efficiencies in the workplace, and all were centered around EHR health information technology.59, 60, 61, 62, 63, 64, 65, 66, 67, 68 Five (50%) of the 10 studies reported interventions that successfully improved burnout, satisfaction, and/or stress (Figure 3, Table 2).64, 65, 66, 67, 68 All 3 studies with interventions evaluating EHR improvements significantly improved satisfaction and decreased stress (Table 2).64, 65, 67 With the exception of Menachemi et al,66 interventions of EHR implementation in a workflow generally worsened or had no effect on burnout or its indicators.59, 60, 63, 66, 68 Trends identified within these studies included perceived insufficient training contributed to EHR ineffectiveness; EHR use by the physician within clinic visits negatively impacted patient-centered communication; and physician characteristics associated with less satisfaction included older age (>55 years), male sex, and surgical specialties. Two studies concluded that EHR adoption63 and EHR systems with more features have been associated with greater physician stress.60 Similarly, higher keyboard use was associated with poor physician satisfaction regarding EHR use (P=.04).59
Some features of EHRs and their use were assessed to provide insights. The authors noted that physicians who were satisfied with various applications of information technology, including EHR usage, personal device assistant usage, use of email with patients, and use of disease management software, were 4 times more likely to be satisfied with their medical practice (odds ratio, 3.97; 95% CI, 3.29-4.81).66 A 4-year longitudinal study correlated the following with greater satisfaction with EHR adoption by physicians (n=119): affordability of incorporating EHRs into the practice, greater preintervention satisfaction with their practice, and finding that the EHR was easy to use.63 More personal or professional stress before EHR implementation was correlated with greater EHR adoption satisfaction.63 Physicians who reported that they use EHRs in more sophisticated ways (eg, for more aspects of their practice, documentation, and prescription writing) were more likely to view EHR adoption as improving all aspects of clinical practice in a cross-sectional study.68
Discussion
This systematic review identified 50 studies evaluating the effect of organization-directed workplace interventions on physician burnout, of which 38 were designed specifically to alleviate burnout or improve its associated indicators, such as job satisfaction, stress, emotional exhaustion, or fatigue. The remaining interventions were not designed to reduce burnout but captured outcomes related to burnout. Interventions were stratified into 4 unique categories created for this study: Teamwork, Time, Transitions, and Technology. Workplace changes promoting Teamwork including the use of scribes or medical assistants to reduce the clerical burden of EHR use were the most frequent and successful organization-driven interventions to decrease burnout and improve job satisfaction. Other successful interventions included process improvement for workplace Transitions, schedule adjustments and time banking (Time), and improvements to Technology regarding the EHR.
Physician burnout is compounded by recent changes to clinical practice. These modifications include an increase in clerical duties, accountability for varied quality metrics, and organizational changes to health care delivery including new payment and delivery approaches, EHRs, and new EHR-generated tasks like managing patient portal communications.70, 71 Studies have documented that for every clinical hour spent with patients, physicians spend nearly 2 additional hours completing administrative tasks and data entry in the EHR72 with up to another 2 hours of personal time at night.72 Although the integration of EHRs was meant to enhance the coordination and quality of care, it generated unintended consequences that appear to raise the risk of burnout.17
Our review results suggest that relatively few high-quality studies have evaluated the potential benefits of Transitions to workflow in relieving and preventing physician burnout. One highly beneficial intervention was a change in workflow that reassigned tasks from the physician to medical assistants, nurses, and physician assistants.28 This modification to the workflow supports the team-based care approach to reduce burnout. Quality improvement (lean) interventions identified in this study to improve unit workflow were not designed to improve burnout per se but were particularly successful at improving measures related to physician burnout. These successful interventions acknowledged that leadership support was required to redesign workflow with the goal of increasing staff productivity and efficiency.
Teamwork interventions consistently improved physician burnout, satisfaction, and stress. High-quality evidence provided the value of Teamwork to improve clinic workflow efficiency, such as timely and accurate medical record completion. Our included studies did not generally measure the effect of teamwork on an intermediate outcome, such as out-of-clinic time to complete clerical work. However, 2 low-quality studies noted that productivity increases led to fewer hours spent on EHR documentation outside of work.30, 52 In-room clinical and clerical support provided by medical assistants or scribes particularly for EHR completion have reduced burnout, reallocated time for clinical care, and improved face-to-face patient interactions.23, 24, 26, 27, 30, 35 In support of these findings, a recent Veterans Health Administration study determined that physician burnout was more prevalent when tasks and responsibilities were not shared with other team members.73 Better communication among staff is part of optimizing workflow, with results from a prospective study revealing that communication improvement among staff and physicians was especially effective at reducing burnout.28, 29 Other successful Teamwork interventions supported peer-to-peer communication. Providing physicians with a sense of community bolstered by a culture of appreciation, support, and engagement can help reduce burnout.37 Executive leadership can encourage this type of professional environment by providing protected time that allows physicians to enhance their professional development and engage with colleagues. This review identified a limited number of studies evaluating organization-directed interventions aimed at promoting professional training and support at work. Results from a randomized controlled trial suggest that providing physicians with employer-allocated support (time and sponsorship) for small-group discussions focused on mindfulness, reflections, shared experience, and small-group learning improved empowerment and engagement and reduced depersonalization.37 Despite the paucity of robust studies evaluating the benefits of leadership-driven physician support programs, available evidence suggests that fostering professional development through discussion groups and training can alleviate burnout and enhance the quality of care.
Time interventions had mixed results on physician burnout. One frequently mentioned organization-directed intervention is the impact of nationally imposed physician and resident work hour restrictions on burnout. In the United States, the Accreditation Council for Graduate Medical Education has recommended that residents work a maximum of 80 hours per week, with the goal of supporting resident well-being, furthering their education, and improving patient safety. However, while addressing exhaustion and burnout of residents remains essential, the reported benefits of working hour limits varied. Only 2 of the 6 studies that evaluated work hour limits for residents reported a lower rate of burnout.43, 44 Residents or interns reported that while working time decreased, workload did not, which ultimately worsened stress and fatigue.47 Therefore, interventions focused on restricting working hours may not be effective in reducing burnout if they only alter this one factor and fail to address the other organizational factors contributing to burnout.
Successful Technology interventions were limited to the improvement of EHR-related health information technology use. Even though health information technology is significantly contributing to burnout, there is hope that Technology may be a remedy. The role of clinicians has continuously evolved over the past 2 decades from writing notes on paper to transcribing notes. Future studies may examine the value of leveraging voice recognition systems to add notes to a patient’s medical record or using digital health technology components like clinical decision support tools or machine learning for the augmentation of patient care.
Strengths and Limitations
To our knowledge, this is the first systematic review focused exclusively on the effect of organization-directed workplace interventions on physician burnout. Unlike previous reviews,16, 74 our review included 11 interventions (22.0%) not designed to decrease burnout but that measured burnout indicators as an indirect outcome of system changes. As a result, this systematic review has included more workplace intervention studies compared with earlier reviews and taken a more explorative evaluation of these organization-directed interventions that could affect physician burnout. Our comprehensive evaluation established the “4Ts” framework (Teamwork, Transitions, Time, and Technology) to address physician burnout interventions in the workplace, which may clarify the approach and emphases of future research.
The findings from the systematic review are limited primarily by differences among the included studies. Given the range of study designs, study settings, interventions, and outcomes measured, it is not possible to compare the effectiveness of individual workplace changes. Follow-up times were of generally of short duration (range, 1 week to 7 years). Furthermore, the study results are restricted by the limited quality of the included studies, with 40 of the articles (80.0%) ranked as level 4 according to the Oxford Centre for Evidence-based Medicine Levels of Evidence18 (Table 1). All Technology studies were of poor quality. Limited studies identified in our review had both a robust design and used validated instruments to measure burnout, such as the MBI. Additionally, few studies employed bivariate or multivariate analyses to group individuals by study variables. Lastly, because 14 (28.0%) of the included studies are conference abstracts, there is incomplete information on the study population, interventions, and methodology, which made it difficult to fully evaluate the study results and quality.
Future Directions
The future of high-quality affordable care in the United States depends on a large and dedicated supply of physicians. This supply is potentially threatened by the growing prevalence of physician burnout, which has significant consequences for the health of both physicians and patients, as well as the sustainability of the health care system. Physician burnout has expanded the health system performance triple aim (improved population health and patient care with lower costs)75 to the quadruple aim (triple aim plus improving the work life of health care professionals).76 As an example, comprehensive care can support both the triple and quadruple aims in primary care; comprehensiveness of practice among family physicians was associated with improved outcomes77 and lower costs, and a causal link between scope of practice and physician wellness was identified.70 In regard to the workplace, practice redesigns that extend the scope of practice or encourage physicians to spend more than 20% of their time on a meaningful activity78 may help to achieve the quadruple aim.
The most efficacious strategy to alleviate physician burnout will target organization-directed changes rather than the level of the individual. Given the negative consequences of burnout, it is imperative that executive leadership within health care organizations support the implementation of evidence-based interventions79 that encourage Teamwork, manage working Time requirements, Transition workflows, and improve Technology. However, there may be additional information required to understand how the workplace environment contributes to physician burnout. The National Academy of Medicine outlines potential organizational, practice, financial, and regulatory environment considerations to identify increased risk of burnout.80
Recently, a collaborative report of distinguished Massachusetts institutions issued a call to action to fight physician burnout.81 It was recommended that every major health care organization appoint an executive-level chief wellness officer to champion burnout reduction and its etiology. And echoing our findings, it was recommended that EHR standards be improved with strong focus on usability and open health care application programming interfaces to better customize system workflows and interfaces to allow agility. Moreover, the American College of Physicians has put forth 7 recommendations to mitigate the adverse effects of excessive administrative tasks on physicians, patients, and the health care system.82 The recommendations are aligned with the findings from this study, including a focus on streamlining administrative tasks and reducing high volumes of clerical work.
Conclusion
Over the past decade, most workplace intervention research studied attempts to alleviate burnout by streamlining workflow via team-based interventions, promoting teamwork to provide patient care and offering professional growth and support opportunities, being mindful of physician schedules and reducing their workload, and improving use of the EHR. Differences among studies make it difficult to directly compare the effectiveness of each type of intervention. However, evidence from high-quality studies suggests that streamlining workflows, providing leadership-driven professional support opportunities, and reducing the administrative burden of EHRs through team-based care by the use of scribes and medical assistants generally improve physician burnout.
Acknowledgments
We thank Dr Charles Turkelson and Dr Nicole Fusco for careful review of the submitted manuscript.
Footnotes
Grant Support: This study was funded by IBM Watson Health.
Potential Competing Interests: The authors report no competing interests.
Supplemental Online Material
Supplemental material can be found online at http://www.mcpiqojournal.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
References
- 1.Shanafelt T.D., Hasan O., Dyrbye L.N., et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613. doi: 10.1016/j.mayocp.2015.08.023. [published correction appears in Mayo Clin Proc. 2016;91(2):276] [DOI] [PubMed] [Google Scholar]
- 2.Maslach C., Schaufeli W.B., Leiter M.P. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 3.Linzer M., Manwell L.B., Williams E.S., et al. Working conditions in primary care: physician reactions and care quality. Ann Intern Med. 2009;151(1):28–36. doi: 10.7326/0003-4819-151-1-200907070-00006. W6-W9. [DOI] [PubMed] [Google Scholar]
- 4.Agency for Healthcare Research and Quality . Agency for Healthcare Research and Quality; Rockville, MD: 2017. Physician Burnout. AHRQ Publication No. 17-M018-1-EF. [Google Scholar]
- 5.Shanafelt T., Goh J., Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826–1832. doi: 10.1001/jamainternmed.2017.4340. [DOI] [PubMed] [Google Scholar]
- 6.Sinsky C.A., Dyrbye L.N., West C.P., Satele D., Tutty M., Shanafelt T.D. Professional satisfaction and the career plans of US physicians. Mayo Clin Proc. 2017;92(11):1625–1635. doi: 10.1016/j.mayocp.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 7.Montgomery A.J., Bradley C., Rochfort A., Panagopoulou E. A review of self-medication in physicians and medical students. Occup Med (Lond) 2011;61(7):490–497. doi: 10.1093/occmed/kqr098. [DOI] [PubMed] [Google Scholar]
- 8.Schernhammer E.S., Colditz G.A. Suicide rates among physicians: a quantitative and gender assessment (meta-analysis) Am J Psychiatry. 2004;161(12):2295–2302. doi: 10.1176/appi.ajp.161.12.2295. [DOI] [PubMed] [Google Scholar]
- 9.Shanafelt T.D., Noseworthy J.H. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129–146. doi: 10.1016/j.mayocp.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 10.Balch C.M., Oreskovich M.R., Dyrbye L.N., et al. Personal consequences of malpractice lawsuits on American surgeons. J Am Coll Surg. 2011;213(5):657–667. doi: 10.1016/j.jamcollsurg.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 11.Shanafelt T.D., Balch C.M., Bechamps G., et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(6):995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Y., Feng X. The relationship between job satisfaction, burnout, and turnover intention among physicians from urban state-owned medical institutions in Hubei, China: a cross-sectional study. BMC Health Serv Res. 2011;11:235. doi: 10.1186/1472-6963-11-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Landon B.E., Reschovsky J.D., Pham H.H., Blumenthal D. Leaving medicine: the consequences of physician dissatisfaction. Med Care. 2006;44(3):234–242. doi: 10.1097/01.mlr.0000199848.17133.9b. [DOI] [PubMed] [Google Scholar]
- 14.Sibbald B., Bojke C., Gravelle H. National survey of job satisfaction and retirement intentions among general practitioners in England. BMJ. 2003;326(7379):22. doi: 10.1136/bmj.326.7379.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buchbinder S.B., Wilson M., Melick C.F., Powe N.R. Estimates of costs of primary care physician turnover. Am J Manag Care. 1999;5(11):1431–1438. [PubMed] [Google Scholar]
- 16.Panagioti M., Panagopoulou E., Bower P., et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. 2017;177(2):195–205. doi: 10.1001/jamainternmed.2016.7674. [DOI] [PubMed] [Google Scholar]
- 17.Friedberg M.W., Chen P.G., Van Busum K.R., et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Rand Health Q. 2014;3(4):1. [PMC free article] [PubMed] [Google Scholar]
- 18.Oxford Centre for Evidence-based Medicine – Levels of Evidence (March 2009). Centre for Evidence-Based Medicine website. https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/ Accessed June 20, 2019.
- 19.Chapman S.A., Blash L.K. New roles for medical assistants in innovative primary care practices. Health Serv Res. 2017;52(suppl 1):383–406. doi: 10.1111/1475-6773.12602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Contratto E.C., Estrada C., Romp K.G., Agne A., Willett L.L. The impact of physician order entry clerical support on physician satisfaction and productivity. J Gen Intern Med. 2016;31(2, suppl):S912–S913. doi: 10.14423/SMJ.0000000000000645. [abstract] [DOI] [PubMed] [Google Scholar]
- 21.Contratto E., Romp K., Estrada C.A., Agne A., Willett L.L. Physician order entry clerical support improves physician satisfaction and productivity. South Med J. 2017;110(5):363–368. doi: 10.14423/SMJ.0000000000000645. [DOI] [PubMed] [Google Scholar]
- 22.Danila M.I., Melnick J.A., Curtis J.R., Menachemi N., Saag K.G. Use of scribes for documentation assistance in rheumatology and endocrinology clinics: impact on clinic workflow and patient and physician satisfaction. J Clin Rheumatol. 2018;24(3):116–121. doi: 10.1097/RHU.0000000000000620. [DOI] [PubMed] [Google Scholar]
- 23.Gidwani R., Nguyen C., Kofoed A., et al. Impact of scribes on physician satisfaction, patient satisfaction, and charting efficiency: a randomized controlled trial. Ann Fam Med. 2017;15(5):427–433. doi: 10.1370/afm.2122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heaton H.A., Castaneda-Guarderas A., Trotter E.R., Erwin P.J., Bellolio M.F. Effect of scribes on patient throughput, revenue, and patient and provider satisfaction: a systematic review and meta-analysis. Am J Emerg Med. 2016;34(10):2018–2028. doi: 10.1016/j.ajem.2016.07.056. [DOI] [PubMed] [Google Scholar]
- 25.Hung D.Y., Harrison M.I., Truong Q., Du X. Experiences of primary care physicians and staff following lean workflow redesign. BMC Health Serv Res. 2018;18(1):274. doi: 10.1186/s12913-018-3062-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Imdieke B.H., Martel M.L. Integration of medical scribes in the primary care setting: improving satisfaction. J Ambul Care Manage. 2017;40(1):17–25. doi: 10.1097/JAC.0000000000000168. [DOI] [PubMed] [Google Scholar]
- 27.Koshy S., Feustel P.J., Hong M., Kogan B.A. Scribes in an ambulatory urology practice: patient and physician satisfaction. J Urol. 2010;184(1):258–262. doi: 10.1016/j.juro.2010.03.040. [DOI] [PubMed] [Google Scholar]
- 28.Linzer M., Poplau S., Grossman E., et al. A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the Healthy Work Place (HWP) Study. J Gen Intern Med. 2015;30(8):1105–1111. doi: 10.1007/s11606-015-3235-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Linzer M., Poplau S., Brown R., et al. Do work condition interventions affect quality and errors in primary care? results from the Healthy Work Place Study. J Gen Intern Med. 2017;32(1):56–61. doi: 10.1007/s11606-016-3856-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCormick B.J., Deal A., Borawski K.M., et al. Implementation of medical scribes in an academic urology practice: an analysis of productivity, revenue, and satisfaction. World J Urol. 2018;36(10):1691–1697. doi: 10.1007/s00345-018-2293-8. [DOI] [PubMed] [Google Scholar]
- 31.Pierce R.G., Anoff D., Cumbler E., et al. A team-based and organizational framework for fostering resilience and well-being in academic hospital medicine. Paper presented at: American Conference on Physician Health; October 12-13, 2017; San Francisco, CA. Abstract book, pp 1-2. https://med.stanford.edu/content/dam/sm/CME/documents/brochures/2017/ACPH-Abstract-Book-FULL.pdf Stanford Medicine website.
- 32.Pozdnyakova A., Laiteerapong N., Volerman A., et al. Impact of medical scribes on physician and patient satisfaction in primary care. J Gen Intern Med. 2018;33(7):1109–1115. doi: 10.1007/s11606-018-4434-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Quenot J.P., Rigaud J.P., Prin S., et al. Suffering among carers working in critical care can be reduced by an intensive communication strategy on end-of-life practices. Intensive Care Med. 2012;38(1):55–61. doi: 10.1007/s00134-011-2413-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shaw J.G., Brown-Johnson C., Chan G., Mahoney M., Winget M. Physician burnout and joy of practice: early mixed-methods findings from the implementation of Stanford Primary Care 2.0. J Gen Intern Med. 2017;32(suppl 2):S272. [abstract] [Google Scholar]
- 35.Shultz C.G., Holmstrom H.L. The use of medical scribes in health care settings: a systematic review and future directions. J Am Board Fam Med. 2015;28(3):371–381. doi: 10.3122/jabfm.2015.03.140224. [DOI] [PubMed] [Google Scholar]
- 36.Was A., Cornaby T. September 18-20, 2016. The ideal gas lounge: boosting resident happiness with empowerment and common space improvements. Paper presented at: International Conference on Physician Health. Boston, MA. [Google Scholar]
- 37.West C.P., Dyrbye L.N., Rabatin J.T., et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174(4):527–533. doi: 10.1001/jamainternmed.2013.14387. [DOI] [PubMed] [Google Scholar]
- 38.Willard-Grace R., Knox M., Huang B., Bodenheimer T., Grumbach K. Clinician perception of team support, burnout and “doability” of primary care. Paper presented at: American Conference on Physician Health; October 12-13, 2017; San Francisco, CA. Abstract book, p 20. https://med.stanford.edu/content/dam/sm/CME/documents/brochures/2017/ACPH-Abstract-Book-FULL.pdf Stanford Medicine website.
- 39.Ali N.A., Wolf K.M., Hammersley J., et al. Midwest Critical Care Consortium Continuity of care in intensive care units: a cluster-randomized trial of intensivist staffing. Am J Respir Crit Care Med. 2011;184(7):803–808. doi: 10.1164/rccm.201103-0555OC. [DOI] [PubMed] [Google Scholar]
- 40.Desai S.V., Asch D.A., Bellini L.M., et al. iCOMPARE Research Group Education outcomes in a duty-hour flexibility trial in internal medicine. N Engl J Med. 2018;378(16):1494–1508. doi: 10.1056/NEJMoa1800965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fassiotto M.A., Maldonado Y.A. September 18-20, 2016. A time banking system to support workplace flexibility. Paper presented at: International Conference on Physician Health. Boston, MA. [Google Scholar]
- 42.Garland A., Roberts D., Graff L. Twenty-four-hour intensivist presence: a pilot study of effects on intensive care unit patients, families, doctors, and nurses. Am J Respir Crit Care Med. 2012;185(7):738–743. doi: 10.1164/rccm.201109-1734OC. [DOI] [PubMed] [Google Scholar]
- 43.Kim H., Wiedermann B. Have Accreditation Council for Graduate Medical Education duty hour limits made a difference? a re-examination of resident sleep, mental health, education, and safety seven years later [abstract] J Investig Med. 2011;59:630–631. [Google Scholar]
- 44.Landrigan C.P., Fahrenkopf A.M., Lewin D., et al. Effects of the Accreditation Council for Graduate Medical Education duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122(2):250–258. doi: 10.1542/peds.2007-2306. [DOI] [PubMed] [Google Scholar]
- 45.Lucas B.P., Trick W.E., Evans A.T., et al. Effects of 2- vs 4-week attending physician inpatient rotations on unplanned patient revisits, evaluations by trainees, and attending physician burnout: a randomized trial. JAMA. 2012;308(21):2199–2207. doi: 10.1001/jama.2012.36522. [DOI] [PubMed] [Google Scholar]
- 46.Moeller M.F., Walker C. Practice refresh: A 1-month intervention to rebuild physician efficiency and wellness. Paper presented at: American Conference on Physician Health; October 12-13, 2017; San Francisco, CA. Abstract book, pp 27-28. https://med.stanford.edu/content/dam/sm/CME/documents/brochures/2017/ACPH-Abstract-Book-FULL.pdf Stanford Medicine website.
- 47.Morrow G., Burford B., Carter M., Illing J. Have restricted working hours reduced junior doctors' experience of fatigue? a focus group and telephone interview study. BMJ Open. 2014;4(3):e004222. doi: 10.1136/bmjopen-2013-004222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Parshuram C.S., Amaral A.C., Ferguson N.D., et al. Canadian Critical Care Trials Group Patient safety, resident well-being and continuity of care with different resident duty schedules in the intensive care unit: a randomized trial. CMAJ. 2015;187(5):321–329. doi: 10.1503/cmaj.140752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ripp J.A., Bellini L., Fallar R., Bazari H., Katz J.T., Korenstein D. The impact of duty hours restrictions on job burnout in internal medicine residents: a three-institution comparison study. Acad Med. 2015;90(4):494–499. doi: 10.1097/ACM.0000000000000641. [DOI] [PubMed] [Google Scholar]
- 50.Schuh L.A., Khan M.A., Harle H., et al. Pilot trial of IOM duty hour recommendations in neurology residency programs: unintended consequences. Neurology. 2011;77(9):883–887. doi: 10.1212/WNL.0b013e31822c61c3. [published correction appears in Neurology. 2011;77(18):1712] [DOI] [PubMed] [Google Scholar]
- 51.Shea J.A., Bellini L.M., Dinges D.F., et al. Impact of protected sleep period for internal medicine interns on overnight call on depression, burnout, and empathy. J Grad Med Educ. 2014;6(2):256–263. doi: 10.4300/JGME-D-13-00241.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tucker P., Brown M., Dahlgren A., et al. The impact of junior doctors' worktime arrangements on their fatigue and well-being. Scand J Work Environ Health. 2010;36(6):458–465. doi: 10.5271/sjweh.2985. [DOI] [PubMed] [Google Scholar]
- 53.Albadry A.A., Sleem A.N., Montasser N.A., Naggar E.-S.A.E. May 28-June 1, 2014. Effect of quality improvement intervention on occupational burnout in Mansoura University Hospitals, Egypt. Paper presented at: WELL-Med Conference. Alexandroupolis, Greece. [Google Scholar]
- 54.Amis S.M., Osicki T.H.E. Can patient safety be improved by reducing the volume of "inappropriate prescribing tasks" handed over to out-of-hours junior doctors? Int J Gen Med. 2018;11:105–112. doi: 10.2147/IJGM.S153227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Callahan S., Enfield K.B., Sturek J., et al. An innovative, evidence-based, fellow-driven bundle to improve professional satisfaction and wellness [abstract] Am J Resp Crit Care Med. 2018;197:A4498. [Google Scholar]
- 56.Dunn P.M., Arnetz B.B., Christensen J.F., Homer L. Meeting the imperative to improve physician well-being: assessment of an innovative program. J Gen Intern Med. 2007;22(11):1544–1552. doi: 10.1007/s11606-007-0363-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Giannini A., Miccinesi G., Prandi E., Buzzoni C., Borreani C., ODIN Study Group Partial liberalization of visiting policies and ICU staff: a before-and-after study. Intensive Care Med. 2013;39(12):2180–2187. doi: 10.1007/s00134-013-3087-5. [DOI] [PubMed] [Google Scholar]
- 58.Lee M.H., Schemmel A.J., Pooler B.D., et al. Radiology workflow dynamics: how workflow patterns impact radiologist perceptions of workplace satisfaction. Acad Radiol. 2017;24(4):483–487. doi: 10.1016/j.acra.2016.08.027. [DOI] [PubMed] [Google Scholar]
- 59.Agha Z., Roter D., Laud P., et al. Patient-centered communication and physicians use of electronic medical records. J Gen Intern Med. 2010;25(suppl 3):S344. [Google Scholar]
- 60.Babbott S., Manwell L., Brown R., et al. Electronic health records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc. 2014;21:e100–e106. doi: 10.1136/amiajnl-2013-001875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Beam K.S., Cardoso M., Sweeney M., Binney G., Weingart S.N. Examining perceptions of computerized physician order entry in a neonatal intensive care unit. Appl Clin Inform. 2017;8(2):337–347. doi: 10.4338/ACI-2016-09-RA-0153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ehrlich J.R., Michelotti M., Blachley T.S., et al. A two-year longitudinal assessment of ophthalmologists' perceptions after implementing an electronic health record system. Appl Clin Inform. 2016;7(4):930–945. doi: 10.4338/ACI-2016-05-RA-0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Heyworth L., Zhang F., Jenter C.A., et al. Physician satisfaction following electronic health record adoption in three Massachusetts communities. Interact J Med Res. 2012;1(2):e12. doi: 10.2196/ijmr.2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Joseph C., Ross E., Tuyen L. Rebooting the joy of practice = clinical/operational leadership + workflow standardization + technology. Paper presented at: American Conference on Physician Health; October 12-13, 2017; San Francisco, CA. Abstract book, pp 29-30. https://med.stanford.edu/content/dam/sm/CME/documents/brochures/2017/ACPH-Abstract-Book-FULL.pdf Standord Medicine website.
- 65.Lapointe R., Bhesania S., Tanner T., Peruri A., Mehta P. An innovative approach to improve communication and reduce physician stress and burnout in a university affiliated residency program. J Med Syst. 2018;42(7):117. doi: 10.1007/s10916-018-0956-z. [DOI] [PubMed] [Google Scholar]
- 66.Menachemi N., Powers T.L., Brooks R.G. The role of information technology usage in physician practice satisfaction. Health Care Manage Rev. 2009;34(4):364–371. doi: 10.1097/HMR.0b013e3181a90d53. [DOI] [PubMed] [Google Scholar]
- 67.Milenkiewicz R.V. The less clicks the better: improving the documentation workflow process for physicians. Paper presented at: American Conference on Physician Health; October 12-13, 2017; San Francisco, CA. Abstract book, pp 97-98. https://med.stanford.edu/content/dam/sm/CME/documents/brochures/2017/ACPH-Abstract-Book-FULL.pdf Stanford Medicine website.
- 68.Wylie M.C., Baier R.R., Gardner R.L. Perceptions of electronic health record implementation: a statewide survey of physicians in Rhode Island. Am J Med. 2014;127(10) doi: 10.1016/j.amjmed.2014.06.011. 1010.e21-e27. [DOI] [PubMed] [Google Scholar]
- 69.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 70.Dyrbye L.N., Shanafelt T.D., Sinsky C.A., et al. Burnout among health care professionals: a call to explore and address this underrecognized threat to safe, high-quality care. NAM Perspectives. 2017 https://doi.org/10.31478/201707b [Google Scholar]
- 71.Bohman B., Dyrbye L., Sinsky C.A., et al. Physician well-being: the reciprocity of practice efficiency, culture of wellness, and personal resilience. https://catalyst.nejm.org/physician-well-being-efficiency-wellness-resilience/ NEJM Catalyst website. Published April 26, 2017. Accessed February 9, 2018.
- 72.Sinsky C., Colligan L., Li L., et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165(11):753–760. doi: 10.7326/M16-0961. [DOI] [PubMed] [Google Scholar]
- 73.Kim L.Y., Rose D.E., Soban L.M., et al. Primary care tasks associated with provider burnout: findings from a Veterans Health Administration survey. J Gen Intern Med. 2018;33(1):50–56. doi: 10.1007/s11606-017-4188-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.West C.P., Dyrbye L.N., Erwin P.J., Shanafelt T.D. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 75.Bazemore A., Petterson S., Peterson L.E., Phillips R.L., Jr. More comprehensive care among family physicians is associated with lower costs and fewer hospitalizations. Ann Fam Med. 2015;13(3):206–213. doi: 10.1370/afm.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Berwick D.M., Nolan T.W., Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood) 2008;27(3):759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 77.Bodenheimer T., Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–576. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shanafelt T.D., West C.P., Sloan J.A., et al. Career fit and burnout among academic faculty. Arch Intern Med. 2009;169(10):990–995. doi: 10.1001/archinternmed.2009.70. [DOI] [PubMed] [Google Scholar]
- 79.Suchman A.L. The influence of health care organizations on well-being. West J Med. 2001;174(1):43–47. doi: 10.1136/ewjm.174.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Weidner A.K.H., Phillips R.L., Jr., Fang B., Peterson L.E. Burnout and scope of practice in new family physicians. Ann Fam Med. 2018;16(3):200–205. doi: 10.1370/afm.2221. [published correction appears in Ann Fam Med. 2018;16(4):289] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jha A.K., Iliff A.R., Chaoui A.A., Defossez S., Bombaugh M.C., Miller Y.A. Massachusetts Medical Society, Massachusetts Health and Hospital Association, Harvard T.H. Chan School of Public Health, and Harvard Global Health Institute; Waltham, MA: 2019. A Crisis in Health Care: A Call to Action on Physician Burnout. [Google Scholar]
- 82.Erickson S.M., Rockwern B., Koltov M., McLean R.M., Medical Practice and Quality Committee of the American College of Physicians Putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann intern Med. 2017;166(9):659–661. doi: 10.7326/M16-2697. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.