Abstract
Objective
To use a mixed methods approach to focus quality improvement efforts to enhance patient experience through human-centered design.
Patients and Methods
A mixed method approach began with returned Press Ganey Medical Practice Surveys from a large, multidisciplinary, outpatient medicine practice from July 1, 2016, through June 30, 2017, using correlation and gap analysis. The second phase deployed human-centered design approaches to process map patient journeys and generate opportunities for care improvement and to generate a theoretical framework for designing optimal care experiences.
Results
Our outpatient medical practices have the greatest ability to improve patient experience scores by focusing on how care teams deliver and educate patients on medications, instructions for follow-up care, and explanations about problems or conditions. By leveraging communication, the expertise of our care team members, and connection between patients and care team members, we can employ a variety of observed opportunities to enhance patient experience. Specific opportunities include leveraging tools in the electronic health record, fostering connection through empathy between patients and members of the care team, and capitalizing on the expertise of nurses on the care team.
Conclusion
A mixed methods approach to the analysis and observation of clinical care and business operations allows for the detection of opportunities with the highest potential impact for improvement when resources are constrained.
Abbreviations and Acronyms: EHR, electronic health record
Patient-centeredness in the provision of health care engages patients in discussions and empowers them with decisions in a manner consistent with their values and preferences.1 Previous investigators have suggested that the 3 main components of patient-centered care are communication, partnership, and health promotion.2 The intent of patient-centered care is to reduce health care costs, improve health outcomes, and enhance patient experience.3 The Institute of Medicine recommends patient-centered care as 1 of the 6 objectives to improve the delivery of health care in the modern era.4
Health care costs, health outcomes, and patient experience are core measures of health care quality. In the outpatient setting, drivers of patient experience include provider communication style and organizational factors. Providers who address patient concerns, actively listen, and engage patients in decision making have higher patient satisfaction scores.2 Organizational factors that improve patient experience include the ratio of support to clinical staff and the proportion of staff who would recommend the clinic as a place to work or receive care.5 Patient satisfaction with health care has been associated with diabetes self-management, treatment plan adherence,6 and surgical complications and readmissions.7 Patient satisfaction has been linked to patient loyalty to an individual provider or organization8 and to job satisfaction among health care providers.9
Measures of patient experience are becoming increasingly requested by both government and nongovernment payers, as well as by public reporting and health care ranking organizations.10 Measurement of patient experience leveraging commercial survey tools has become a standard practice across most large health care organizations. Translation of survey findings to practice improvements has been a challenge to individual providers and group practices,11 where characteristics of individual provider practice styles can be mixed with environmental and organizational factors, such as aspects of the practice setting.12 Furthermore, higher patient satisfaction has been observed to be correlated with nondesirable outcomes, such as greater health care expenditures and patient mortality.13 As such, patient satisfaction measures should not be the sole driver of practice change.
Few published studies have predicated practice change on human-centered approaches.14 To improve experience for both patients and providers, discoveries from human-centered quality improvement initiatives can be integrated into clinical practice through actionable steps in alignment with broader institutional goals.15 Research suggests that there are a variety of interventions that may improve patient care team interactions16; however, tailoring these interventions for each clinical scenario can be challenging because improvement efforts require the coordination of multidisciplinary practices.17
In the present study, we sought to determine which specific aspects of patient experience had the greatest potential for improvement in overall patient experience in a group of large, ambulatory, general and specialty internal medicine practices. We then deployed a human-centered design approach to observe patients and members of the care team to create a patient journey map identifying specific areas for improvement, and we created a theoretical framework to be used in the design of the optimal person-centered care experience. We report on the methods used for this investigation, the improvement opportunities identified, and a 3-part framework for consideration when designing optimal patient experiences.
Patients and Methods
Study Overview, Setting, and Populations
This study was conducted in 2 phases from July 1, 2016, through December 1, 2018, and was approved by the Mayo Clinic Institutional Review Board.
During phase 1 of the study, we used 17,141 Press Ganey Medical Practice Surveys (Press Ganey Associates Inc) completed by patients after an ambulatory visit in 1 of 10 divisions in the Mayo Clinic Department of Medicine in Rochester, Minnesota, a large, integrated, multispecialty practice of 474 physicians serving more than 200,000 unique patients annually. The Department of Medicine comprises the following clinical divisions: allergic diseases; community internal medicine; endocrinology; gastroenterology and hepatology; general internal medicine; hematology; infectious diseases; preventive, occupational, and aerospace medicine; pulmonology and sleep medicine; and rheumatology. The Department of Medicine covers a broad range of general and subspecialty practices, but most practice areas have a similar staffing composition and workflow structure, with shared reporting through the departmental level. We, therefore, chose to examine the entire Department of Medicine practice for this study. The intent of this analysis phase was to identify 1 to 3 unique areas of care delivery with the largest potential effect on overall patient experience.
Phase 2 of the study used a human-centered design approach to observe and synthesize best practices related to the areas of focus identified in phase 1. Best practices were used to identify areas of opportunity at the department and individual practice area levels to enhance patient experience and to construct concepts that could be used to design an optimal patient experience across the department as a whole.
Phase 1: Using Patient Survey Results to Focus Quality Improvement Efforts
To use patient experience surveys to focus quality improvement efforts, we used 17,141 Press Ganey Medical Practice Surveys completed and returned from July 1, 2016, through June 30, 2017. Press Ganey Medical Practice Surveys display suitable properties for deployment in health care settings18 and are used in routine clinical care and quality monitoring across the Mayo Clinic ambulatory care practice. The survey instrument (Supplemental Appendix 1, available online at http://www.mcpiqojournal.org) is divided into 6 domains, each comprising 2 to 10 individual survey items: access (4 items), moving through your visit (2 items), nurse/assistant (4 items), care provider (10 items), personal issues (6 items), and overall assessment (3 items). Items are assessed on a 5-point Likert scale (very poor, poor, fair, good, and very good). If a patient had completed more than 1 survey during the study period, only the most recent completed survey was included.
The Spearman rank correlation coefficient was calculated to understand correlations between individual survey items and the overall assessment question: “Overall rating of care received during your visit.” The following interpretation was used: 0.00 to 0.19, very weak; 0.20 to 0.39, weak; 0.40 to 0.59, moderate; 0.60 to 0.79, strong; and 0.80 to 1.00, very strong. Individual survey items demonstrating strong or very strong correlations with the score for overall satisfaction in 8 of 10 of the divisions were assessed for areas of opportunity within the department as a whole. To measure the potential impact of each item deemed strongly or very strongly correlated with patient overall satisfaction, we calculated the prevalence of the 4 lowest response options (very poor, poor, fair, good). Prevalence of opportunity to affect overall satisfaction with care, ongoing division and institutional initiatives, and similarity of target areas were taken into consideration by the study team to determine where to focus phase 2 study efforts.
Phase 2: Human-Centered Design Observations and Synthesis
Process mapping of patient journeys through health care experiences has been published elsewhere, and this approach can be viewed as a mechanism to understand the series of steps or events involved in the health care process.17 To focus our observations, the project team created an interview and observation guide to be deployed by all observers (Supplemental Appendix 2, available online at http://www.mcpiqojournal.org). Prompts for observations were grouped by observation location: patient waiting room, rooming, and within the visit/with the provider. Individual observation questions were developed collectively by the study team through several rounds of open discussion and brainstorming. The study team chose individual questions to pay particular attention to during observations, which appear in bold in the observation guide. The specific aims of the observations were as follows:
-
1.
Assessing the full patient journey and not just the appointment. For example, identifying opportunities before patients are evaluated in the clinic, in the waiting area, during rooming, and after the appointment.
-
2.
Understanding how behaviors and needs differ across all people (patients, family members, care teams, staff, etc), affecting the full human experience for all included in the patient journey.
-
3.
Identifying current patient experience strategies and how they are being used in practice.
In addition to the observations, we also developed and deployed interview guides specific to 2 main stakeholder groups: provider/members of the care team and patients. Interview questions were developed collectively by the study team based on input received from the clinical practice chairs of the divisions. Interview guides were included with the observation guides in the research booklets. Observers were asked to document their observations directly in their research booklet or other note-keeping source of their choosing.
The purpose of the observations was to understand the current workflows and how they relate to positive patient experiences in the Department of Medicine outpatient practice. We selected a range of practices and providers who were highest performing on the patient experience surveys, including the community internal medicine division, to observe patients receiving longitudinal care, the general internal medicine practice responsible for intake and coordination of patients with complex illness, and pulmonology/sleep medicine and gastroenterology/hepatology to represent the specialty practices. During the observation period, we observed 16 half-day clinic sessions with 14 unique providers. To understand other areas where patients would be experiencing care and receiving health-related information, we also observed clinic waiting rooms and on-site outpatient pharmacies.
Four members of our team (M.A.D., H.I.S., P.R., L.P.M.) participated in shadowing of patients, caregivers, and care teams. The team met intermittently during the observation period to discuss insights and feedback received from stakeholders, patients, providers, and care teams. With that input, team members conducted additional interviews with patients, medical secretaries, nursing administrators and managers to gain additional perspective into the workflows of each during the patient journey, as well as patient needs commonly reported before and after the clinic visit.
Observations across the 4-member team were compiled into a shared file that became the foundation for analysis to triangulate the data based on observations, interviews, and varying team members. The notes were compiled and reviewed, and insights were grouped under the process step in which the insight was observed. Multiple entries of a similar point gave us confidence that we had achieved saturation in the data collection. Insights were then used to identify challenges across the journey based on a deep contextual knowledge that the team members have of the outpatient practice, with confirmation from practice providers throughout the synthesis process. Opportunities were created using human-centered design principles to identify system solutions for people, and each was assigned to 1 of 3 concepts that could be used to design the optimal patient experience.
Results
Phase 1: Using Patient Survey Results to Focus Quality Improvement Efforts
During the study, 17,141 surveys were completed by patients who had a visit at any of the 10 clinical divisions in the Department of Medicine and provided authorization for participation in research. During the study time frame, the practices had an overall response rate of 14.5% (17,141 of 118,378). Approximately 44% of the surveys were completed online, and 56% were completed on paper. The mean ± SD age of survey respondents was 64.0±14.3 years, and 56% were female. Patient proxies completed 3.6% of returned surveys.
The Department of Medicine had high scores on patient experience surveys, with 95% of patients reporting very good satisfaction with their care. Patients reported very good levels of satisfaction for questions related to the care provider (94.7%), personal issues (94.4%), and the nurse/assistant (92.5%). Patients reported lower satisfaction for questions related to access (89.8%) and moving through the visit (85.5%). Of all 26 individual items, 7 survey questions had either strong (Spearman rank correlation coefficient = 0.60-0.79) or very strong (Spearman rank correlation coefficient = 0.80-1.00) correlation with patient overall rating of care across most individual specialty areas with sufficient sample size and the overall Department of Medicine. One specialty area had too few survey responses owing to low ambulatory clinical practice volumes (infectious diseases).
Gap analysis of received scores for these 7 survey items suggested that focusing on the following 3 survey items could affect up to 1 in 5 surveys completed across the Department of Medicine (Table):
-
1.
Information the care provider gave you about medications (if any).
-
2.
Instructions the care provider gave you about follow-up care (if any).
-
3.
Explanations the care provider gave you about your problem or condition.
Table.
Responses to the Most Common Items Correlated With “Overall Rating of Care Received During Your Visit” and Calculated Proportion of Surveys With an Opportunity to Advance to "Very Good" Response Option
| Variable | Explanations the care provider gave you about your problem or condition | Care provider efforts to include you in decisions about your treatment | Confidence in this care provider | Response to concerns/complaints made during visit | Concern the care provider showed for questions or worries | Information care provider gave you about medications (if any) | Instructions care provider gave you about follow-up care (if any) |
|---|---|---|---|---|---|---|---|
| Divisions (N=10) for which item was correlated with overall rating of care (No.) | 10 | 9 | 9 | 9 | 8 | 8 | 8 |
| Responses (No.) (N=17,141) | |||||||
| Very poor | 54 | 63 | 88 | 68 | 64 | 51 | 81 |
| Poor | 109 | 99 | 118 | 92 | 113 | 97 | 119 |
| Fair | 369 | 367 | 343 | 322 | 345 | 395 | 472 |
| Good | 2195 | 2231 | 1826 | 2480 | 2217 | 2370 | 2535 |
| Very good | 14,242 | 13,937 | 14,530 | 12,262 | 14,178 | 12,218 | 12,824 |
| Missing | 172 | 444 | 236 | 1917 | 224 | 2010 | 1110 |
| Responses with opportunity for improvement (%) | 15.9 | 16.1 | 13.8 | 17.3 | 15.9 | 17.0 | 18.7 |
Phase 2: Human-Centered Design Observations and Synthesis
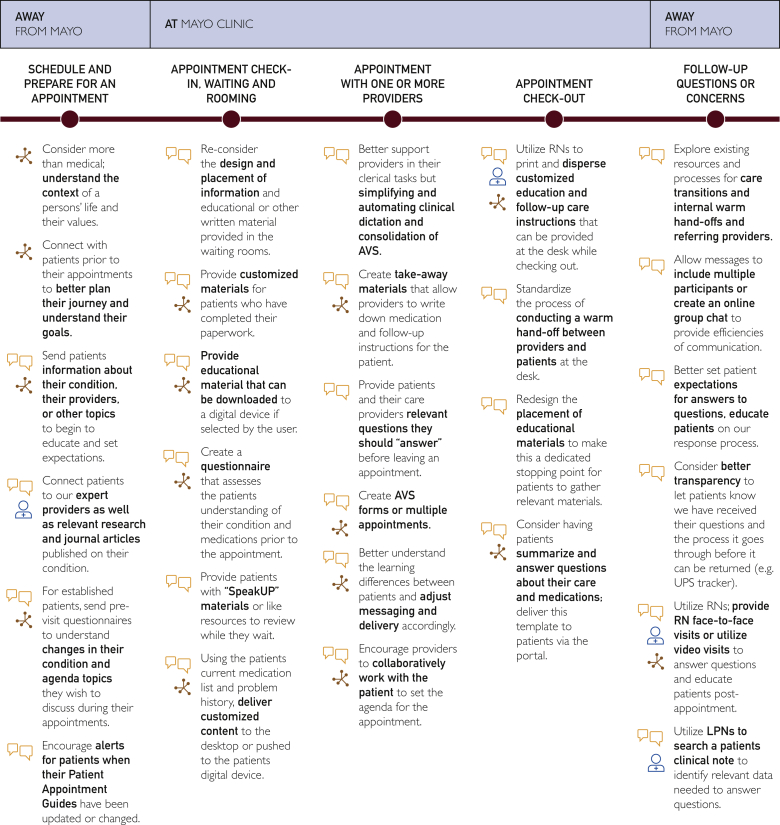
Results of the analytic phase 1 of this study were used to focus observations in phase 2. Through the observational work, we identified a variety of insights and associated challenges across the patient journey, which were used to extrapolate opportunities for care improvement (Figure 1).
Figure 1.
Patient journey map of opportunities to improve information delivered regarding medications, patient condition, and instructions for follow-up care in an ambulatory internal medicine practice. AVS = after-visit summary.
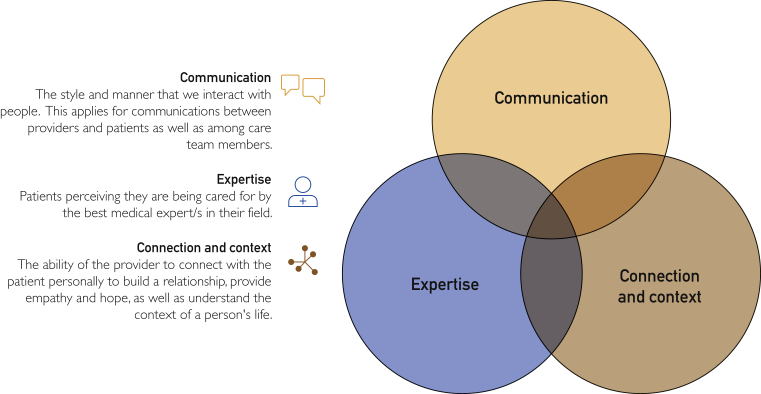
Further synthesis of data collected during the observations generated 3 concepts to be considered when designing an optimal patient experience (Figure 2). Each opportunity identified during the observation and data synthesis mapped to at least 1 of 3 concepts: communication, expertise, and contact and connection. Communication describes the style and manner with which we interact with people. This applies to communication between providers and patients as well as among care team members. Expertise refers to the belief and desire by patients to be receiving medical advice from individuals viewed as skilled in their field. Finally, context and connection refers to the ability of the care team member to connect meaningfully with the patient/caregiver, to provide empathy and hope, and to understand the context of the patient’s life and medical situation.
Figure 2.
Human-centered concepts to consider when designing an optimal patient experience.
Discussion
In the present study, we described a partnering of quantitative and qualitative methods to advance patient experience in a large, ambulatory, internal medicine practice. We reported on how patient survey information routinely collected for clinical operations can be leveraged to focus quality improvement initiatives and how deep understanding through human-centered design approaches can identify insights and challenges in current clinical practice workflows and tools that can be leveraged to generate discrete quality improvement efforts and initiatives. Through these methods we determined that we could focus quality improvement efforts on how care teams deliver information and educate patients on medications, instructions for follow-up care, and explanations about patient problems and conditions. Through these human-centered design observations and synthesis, we found a variety of opportunities we could explore to design an optimum experience for patients, caregivers, and members of the care team, and a theoretical framework for considering communication, expertise, and contact and connection when designing interactions with patients. The main implication of these findings is that patient experience surveys can be leveraged to identify opportunities for practice change.
Patient experience measures via Press Ganey Medical Practice Surveys have been used to understand predictors of satisfaction with care, including patient physical function,19 provider demographic characteristics,20 and care delivery characteristics (communication21). Research shows that providers feel ill-equipped to use patient-reported experience information to improve patient care.22 Garnering an understanding of experience through journey mapping is a more recent development in methodology and application to health care.17 The present study introduces (1) a set of methods to be considered to advance patient experience to help fill the gap between information collected and observed for clinical practice operations and (2) discrete quality improvement initiatives to facilitate high-quality, patient-centered care.
The model using communication and connection between patients and providers is not novel; these are 2 components of the patient-centered care framework recommended by the Institute of Medicine to improve health care.4 The present findings support the literature that information sharing and communication between patients and providers is a key facilitator of patient experience.23 The present work identified the importance of patient understanding of their health condition or diagnosis to be a key driver of overall patient experience, and a study of 500 patient/provider interactions indicated that the greatest discrepancy between patient and provider communication was regarding diagnosis and prognosis.24 When patients and providers were in agreement about these discussions, patient-reported satisfaction with care was significantly higher,24 confirming the importance of patient/provider communication related to health conditions or diagnoses.
Summarizing information for patients to take with them after a health care interaction has been studied in both hospital and ambulatory care settings. After-visit summaries have been extensively studied in the primary care literature. Many electronic health record (EHR) platforms provide out-of-the-box solutions for the summary of information after a patient encounter with a health care provider. Epic (Epic Systems Corp), one of the most widely used EHRs, deploys the after-visit summary for use in ambulatory care settings. Patients perceive the after-visit summary tool to have useful content, but they also note that they may require more explanation of confusing or contradicting information often found in these scripted documents.25 The present thematic analysis showed us that patients have varying needs based on the context of their health and psychosocial condition. Research has found that patient needs vary based on health contexts of chronic illness vs acute medical situations, and longitudinal primary care vs specialty care.26, 27 Current solutions provided by EHR vendors may not meet the needs of patients, caregivers, or providers.26 Health care providers have the opportunity to push the development of health care visit summaries tailored to patient learning styles, incorporating technological solutions such as audio and video to supplement printed materials.
Patient, caregiver, and care team interactions continue to evolve through electronic mediums, altering the way these individuals communicate and connect. Empathy, or the ability to connect with and share the feelings of another, has been correlated with measures of patient experience.28 Characteristics of provider communication and overall provider rating from patient experience surveys are associated with degree of provider empathy, leading to the implementation of empathy training for provider staff at large academic medical centers.28 The relationship between both provider empathy and communication and patient outcomes has shown mixed results in the literature, but links with these components of care and patient satisfaction continue to be reported.23 Information provided about medications, problem or condition, and follow-up care were 3 areas identified in this study where improvements in visit interactions could positively impact patient satisfaction. A study of online medical forum users observed that 40% of patients sought online medical information due to dissatisfaction with their provider.29 In that study, patients reported being less satisfied with the information they received after a visit to a specialist than to primary care. Patient-centered communication approaches and care coordination have been associated with lower rates of patients seeking supplemental electronic medical information, particularly among patients with lower levels of education.30 Frameworks for facilitating empathy and person-centered care emphasize building relationships with patients and caregivers, providing care tailored to the patient, and being respectful of the patient's and caregiver’s time.31
The increasing complexity of patient and caregiver needs compels us to leverage all members of the care team to their highest degree of licensure. The role of the nurse as a member of the care team has grown, in part fueled by the Institute of Medicine’s 2010 release of The Future of Nursing report.32 A wealth of data support the importance of nurses in patient and caregiver education. Research has found that nurse-led education can support overall patient and caregiver well-being,33 activation,34, 35 and knowledge retention.34 Nurses also play a role in coaching patients and caregivers through self-care and instructions on disease management,36, 37 areas that the present study identified as distinct needs of patients to drive patient experience. However, the role of nurses in educational tasks may be limited due to increasing time spent in the non–patient-facing activities, such as EHR interaction.38 Care models could evolve to expand the role of nursing in medication prescribing and education,39 facilitating care redesign to incorporate all 3 components for an optimal care experience: communication, connection and context, and high-quality medical expertise.
The present study has several strengths. First, we used a mixed methods approach to help bridge the gap between findings from a broadly used survey instrument and the characteristics of individual patient situations and clinical practice areas. Second, we used a reliable measure of assessment for the patient experience data. Third, the qualitative component of the study allowed for in-depth assessment of interactions between patients and members of the care team. Fourth, the qualitative component allowed for fluidity in the research framework to adjust the observations and interviews as we gathered new information.
This study also has several limitations. First, the study was limited to 1 department at 1 site in Rochester, Minnesota, which may limit the generalizability of the findings. Second, we were unable to assess for the impact of nonresponse bias for the quantitative analysis due to the operational nature of the survey collection. Although we are unable to assess for nonresponse bias, the survey vendor does perform a simple random sample of patients who had a visit to the outpatient practices, allowing for all patients to have equal opportunity to receive and complete a Press Ganey Medical Practice Survey after their visit. Third, it can be difficult to maintain and demonstrate the rigor in the qualitative portion of the study due to the variability among observers and the fluidity of a qualitative-based approach. We do believe that despite this limitation, the present findings provide key insights into opportunities for quality improvement within a clinical episode of care.
Conclusion
Quality improvement in large medical practices can be difficult to focus and drive forward due to the multidisciplinary practice styles and the number of individuals involved in the experience of health care by the patient.11 In addition, providers struggle with how best to translate patient-reported experiences into meaningful practice change.22 A mixed methods approach to the analysis and observation of clinical care and business operations allows for the detection of areas with the highest potential effect for improvement when resources are constrained.
Footnotes
Grant Support: This study was funded by the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery and Mayo Clinic College of Medicine and Science.
Potential Competing Interests: The authors report no competing interests.
Supplemental Online Material
Supplemental material can be found online at http://www.mcpiqojournal.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
References
- 1.Mead N., Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51(7):1087–1110. doi: 10.1016/s0277-9536(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 2.Little P., Everitt H., Williamson I., et al. Preferences of patients for patient centred approach to consultation in primary care: observational study. BMJ. 2001;322(7284):468–472. doi: 10.1136/bmj.322.7284.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Constand M.K., MacDermid J.C., Dal Bello-Haas V., Law M. Scoping review of patient-centered care approaches in healthcare. BMC Health Serv Res. 2014;14:271. doi: 10.1186/1472-6963-14-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Institute of Medicine . The National Academies Press; Washington, DC: 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. [PubMed] [Google Scholar]
- 5.Flott K., Darzi A., Mayer E. Care pathway and organisational features driving patient experience: statistical analysis of large NHS datasets. BMJ Open. 2018;8(7):e020411. doi: 10.1136/bmjopen-2017-020411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zolnierek K.B.H., DiMatteo M.R. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lobo Prabhu K., Cleghorn M.C., Elnahas A., et al. Is quality important to our patients? the relationship between surgical outcomes and patient satisfaction. BMJ Qual Saf. 2018;27(1):48–52. doi: 10.1136/bmjqs-2017-007071. [DOI] [PubMed] [Google Scholar]
- 8.Safran D.G., Montgomery J.E., Chang H., Murphy J., Rogers W.H. Switching doctors: predictors of voluntary disenrollment from a primary physician's practice. J Fam Pract. 2001;50(2):130–136. [PubMed] [Google Scholar]
- 9.Perzynski A.T., Caron A., Margolius D., Sudano J.J. Primary care practice workplace social capital: a potential secret sauce for improved staff well-being and patient experience. J Patient Exp. 2019;6(1):72–80. doi: 10.1177/2374373518777742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Urden L.D. Patient satisfaction measurement: current issues and implications. Lippincotts Case Manag. 2002;7(5):194–200. doi: 10.1097/00129234-200209000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Coulter A., Locock L., Ziebland S., Calabrese J. Collecting data on patient experience is not enough: they must be used to improve care. BMJ. 2014;348:g2225. doi: 10.1136/bmj.g2225. [DOI] [PubMed] [Google Scholar]
- 12.Berkowitz B. The patient experience and patient satisfaction: measurement of a complex dynamic. Online J Issues Nurs. 2016;21(1):1. doi: 10.3912/OJIN.Vol21No01Man01. [DOI] [PubMed] [Google Scholar]
- 13.Fenton J.J., Jerant A.F., Bertakis K.D., Franks P. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med. 2012;172(5):405–411. doi: 10.1001/archinternmed.2011.1662. [DOI] [PubMed] [Google Scholar]
- 14.Flott K.M., Graham C., Darzi A., Mayer E. Can we use patient-reported feedback to drive change? the challenges of using patient-reported feedback and how they might be addressed. BMJ Qual Saf. 2017;26(6):502–507. doi: 10.1136/bmjqs-2016-005223. [DOI] [PubMed] [Google Scholar]
- 15.Fustino N.J., Kochanski J.J. Improving patient satisfaction in a midsize pediatric hematology-oncology outpatient clinic. J Oncol Pract. 2015;11(5):416–420. doi: 10.1200/JOP.2015.004911. [DOI] [PubMed] [Google Scholar]
- 16.Griffin S.J., Kinmonth A.L., Veltman M.W.M., Gillard S., Grant J., Stewart M. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trials. Ann Fam Med. 2004;2(6):595–608. doi: 10.1370/afm.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trebble T.M., Hansi N., Hydes T., Smith M.A., Baker M. Process mapping the patient journey: an introduction. BMJ. 2010;341:c4078. doi: 10.1136/bmj.c4078. [DOI] [PubMed] [Google Scholar]
- 18.Presson A.P., Zhang C., Abtahi A.M., Kean J., Hung M., Tyser A.R. Psychometric properties of the Press Ganey(R) Outpatient Medical Practice Survey. Health Qual Life Outcomes. 2017;15(1):32. doi: 10.1186/s12955-017-0610-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kohring J.M., Pelt C.E., Anderson M.B., Peters C.L., Gililland J.M. Press Ganey Outpatient Medical Practice Survey scores do not correlate with patient-reported outcomes after primary joint arthroplasty. J Arthroplasty. 2018;33(8):2417–2422. doi: 10.1016/j.arth.2018.03.044. [DOI] [PubMed] [Google Scholar]
- 20.Rogo-Gupta L.J., Haunschild C., Altamirano J., Maldonado Y.A., Fassiotto M. Physician gender is associated with Press Ganey patient satisfaction scores in outpatient gynecology. Womens Health Issues. 2018;28(3):281–285. doi: 10.1016/j.whi.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 21.Griffiths B. Enhanced communication performance improvement and patient satisfaction in an endoscopy/ambulatory surgery unit. Gastroenterol Nurs. 2015;38(3):194–200. doi: 10.1097/SGA.0000000000000116. [DOI] [PubMed] [Google Scholar]
- 22.Rozenblum R., Lisby M., Hockey P.M., et al. The patient satisfaction chasm: the gap between hospital management and frontline clinicians. BMJ Qual Saf. 2013;22(3):242–250. doi: 10.1136/bmjqs-2012-001045. [DOI] [PubMed] [Google Scholar]
- 23.Rathert C., Wyrwich M.D., Boren S.A. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2013;70(4):351–379. doi: 10.1177/1077558712465774. [DOI] [PubMed] [Google Scholar]
- 24.Jackson J.L. Communication about symptoms in primary care: impact on patient outcomes. J Altern Complement Med. 2005;11(suppl 1):S51–S56. doi: 10.1089/acm.2005.11.s-51. [DOI] [PubMed] [Google Scholar]
- 25.Belyeu B.M., Klein J.W., Reisch L.M., et al. Patients' perceptions of their doctors' notes and after-visit summaries: a mixed methods study of patients at safety-net clinics. Health Expect. 2018;21(2):485–493. doi: 10.1111/hex.12641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Federman A., Sarzynski E., Brach C., et al. Challenges optimizing the after visit summary. Int J Med Inform. 2018;120:14–19. doi: 10.1016/j.ijmedinf.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clarke M.A., Moore J.L., Steege L.M., et al. Toward a patient-centered ambulatory after-visit summary: identifying primary care patients' information needs. Inform Health Soc Care. 2018;43(3):248–263. doi: 10.1080/17538157.2017.1297305. [DOI] [PubMed] [Google Scholar]
- 28.Chaitoff A., Sun B., Windover A., et al. Associations between physician empathy, physician characteristics, and standardized measures of patient experience. Acad Med. 2017;92(10):1464–1471. doi: 10.1097/ACM.0000000000001671. [DOI] [PubMed] [Google Scholar]
- 29.Li N., Orrange S., Kravitz R.L., Bell R.A. Reasons for and predictors of patients' online health information seeking following a medical appointment. Fam Pract. 2014;31(5):550–556. doi: 10.1093/fampra/cmu034. [DOI] [PubMed] [Google Scholar]
- 30.Senft N., Everson J. eHealth engagement as a response to negative healthcare experiences: cross-sectional survey analysis. J Med Internet Res. 2018;20(12):e11034. doi: 10.2196/11034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hsu C., Gray M.F., Murray L., et al. Actions and processes that patients, family members, and physicians associate with patient- and family-centered care. BMC Fam Pract. 2019;20(1):35. doi: 10.1186/s12875-019-0918-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Institute of Medicine . The National Academies Press; Washington, DC: 2010. The Future of Nursing: Leading Change, Advancing Health. [PubMed] [Google Scholar]
- 33.Gronning K., Rannestad T., Skomsvoll J.F., Rygg L.O., Steinsbekk A. Long-term effects of a nurse-led group and individual patient education programme for patients with chronic inflammatory polyarthritis - a randomised controlled trial. J Clin Nurs. 2014;23(7-8):1005–1017. doi: 10.1111/jocn.12353. [DOI] [PubMed] [Google Scholar]
- 34.Ghisi G.L., Abdallah F., Grace S.L., Thomas S., Oh P. A systematic review of patient education in cardiac patients: do they increase knowledge and promote health behavior change? Patient Educ Couns. 2014;95(2):160–174. doi: 10.1016/j.pec.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 35.Whitehead L.C., Crowe M.T., Carter J.D., et al. A nurse-led education and cognitive behaviour therapy-based intervention among adults with uncontrolled type 2 diabetes: a randomised controlled trial. J Eval Clin Pract. 2017;23(4):821–829. doi: 10.1111/jep.12725. [DOI] [PubMed] [Google Scholar]
- 36.Baptiste D.L., Davidson P., Groff Paris L., Becker K., Magloire T., Taylor L.A. Feasibility study of a nurse-led heart failure education program. Contemp Nurse. 2016;52(4):499–510. doi: 10.1080/10376178.2016.1229577. [DOI] [PubMed] [Google Scholar]
- 37.Shim J.L., Hwang S.Y. Long-term effects of nurse-led individualized education on middle-aged patients with acute coronary synrome: a quasi-experimental study. BMC Nurs. 2017;16:59. doi: 10.1186/s12912-017-0254-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Higgins L.W., Shovel J.A., Bilderback A.L., et al. Hospital nurses' work activity in a technology-rich environment: a triangulated quality improvement assessment. J Nurs Care Qual. 2017;32(3):208–217. doi: 10.1097/NCQ.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 39.Kooienga S., Wilkinson J. RN prescribing: an expanded role for nursing. Nurs Forum. 2017;52(1):3–11. doi: 10.1111/nuf.12159. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.