Abstract
As part of our continuing investigation for interesting biological activities of native medicinal plants, thirty-nine plants, obtained from diverse areas in Saudi Arabia and Yemen, were screened for insecticidal activity against yellow fever mosquito Aedes aegypti (L.). Out of the 57 organic extracts, Saussurea lappa, Ocimum tenuiflorum, Taraxacum officinale, Nigella sativa, and Hyssopus officinalis exhibited over 80% mortality against adult female Ae. aegypti at 5 μg/mosquito. In the larvicidal bioassay, the petroleum ether extract of Aloe perryi flowers showed 100% mortality at 31.25 ppm against 1st instar Ae. aegypti larvae. The ethanol extract of Saussurea lappa roots was the second most active displaying 100% mortality at 125 and 62.5 ppm. Polar active extracts were processed using LC-MS/MS to identify bioactive compounds. The apolar A. perryi flower extract was analyzed by headspace SPME-GC/MS analysis. Careful examination of the mass spectra and detailed interpretation of the fragmentation pattern allowed the identification of various biologically active secondary metabolites. Some compounds such as caffeic and quinic acid and their glycosides were detected in most of the analyzed fractions. Additionally, luteolin, luteolin glucoside, luteolin glucuronide and diglucuronide were also identified as bioactive compounds in several HPLC fractions. The volatile ketone, 6-methyl-5-hepten-2-one was identified from A. perryi petroleum ether fraction as a major compound.
Keywords: Medicinal plants, Mosquito control, Aedes aegypti, Phenolic acids, Flavonoids, LC-MS/MS, Headspace-SPME, Aloe perryi volatile constituents, 6-Methyl-5-hepten-2-one
1. Introduction
An infected mosquito is the primary vector of numerous mosquito-borne illnesses, caused by bacteria, viruses or parasites. In fact, a mosquito bite can spread dangerous diseases, such as Japanese encephalitis, malaria, West Nile fever, Zika, dengue, yellow fever and chikungunya (Moreno-Madriñán and Turell, 2018). Severe cases of mosquito-borne diseases can lead to death. In 2016, the outbreak of dengue fever, one of the most disparaging diseases, in Jeddah and Jizan cities located in the west of Saudi Arabia, was triggered by the early season heat and humidity which caused mosquitoes to venture inside homes for shade (Alhaeli et al., 2016). The efforts of the Saudi Ministry of Health, which focus on fighting the mosquitoes and control their spread, led to the diminution of mosquito breeding areas and reduction in the number of infected people. However, exposure to conventional synthetic pesticides such as organochlorines, organophosphates and carbamates has raised serious concerns regarding toxic effects on human health, contamination of agricultural products, and the development of resistance to commonly used insecticides (Nicolopoulou-Stamati et al., 2016). On the other hand, plant-based organic pesticides offer an effective, degradable, safe, environmentally friendly and cheaper alternative to conventional synthetic pesticides (Dinesh et al., 2014).
As a result, great efforts have been taken, over the last years, to improve the insecticidal properties of plant extracts and their isolated secondary metabolites. Indeed, a number of insecticidal agents have been reported from herbs including volatiles such as oils of Bifora, Satureja, Coridothymus, Thymbra, Coriandrum and Pimpinella (Sampson et al., 2005, Benelli et al., 2017, Vivekanandhan et al., 2018) and defense proteins such as lectins and proteinase and amylase inhibitors found in a wide variety of plants (Vandenborre et al., 2010). Saudi Arabia and Yemen are both characterized by wide diversity of flora due to climate and height differences among different areas. As part of our continuing investigation of native medicinal plants for interesting biological activities, fifty-seven extracts, prepared from thirty nine plants collected from different areas in Saudi Arabia and Yemen, were screened for larvicidal and insecticidal activities against the mosquito vector Ae. Aegypti (see Fig. 1).
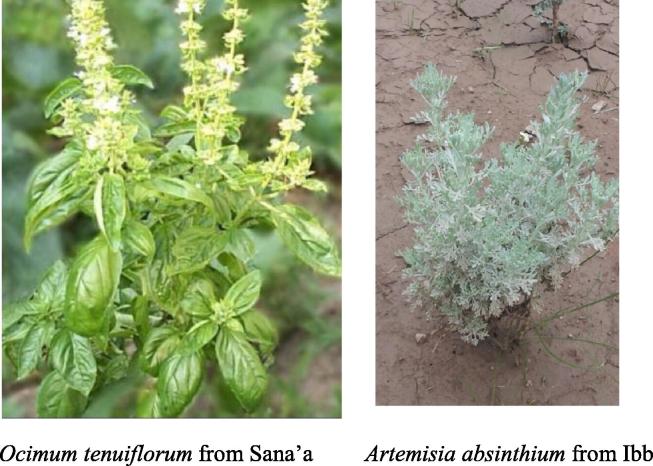
Fig. 1.
Pictures of selected traditional plants analyzed in this study.
2. Materials and methods
2.1. Plant material
Based on local knowledge and use, thirty nine plants were selected from several areas in Saudi Arabia and Yemen during various periods and through several field trips, in the years 2013–2016. Some of the plant samples were purchased from the local market. Taxonomic identification of the plants was made by referring to published references at the Pharmacognosy Departments, Colleges of Pharmacy, King Saud and Sana’a Universities, Saudi Arabia and Yemen (Migahid, 1989, Chaudhary, 2001). Part of the identification was also done by the taxonomist, Dr. Ali Al-Ajami. A voucher specimen of each plant was deposited at the corresponding departments. The botanical and local Arabic names, families, collection places and common traditional uses of the inspected species are presented in Table 1.
Table 1.
List of screened plants against Ae. aegypti and their traditional uses.
| Plant speciesl/local name | VN | Family | Collection sites & time | Traditional uses & Ailments treated |
|---|---|---|---|---|
|
Acacia nilotica Linn. ”Arabic Sant’’ |
Sana-30 | Fabaceae | Hajjah/Yemen August 2014 |
Gastrointestinal disorders (Ali et al., 2012) |
|
Acalypha fruticosa Forssk ”Anshat” |
Sana-56 | Euphorbiaceae | Mahwit/Yemen August 2013 |
Malaria, bacterial infections, nasal bleeding, stomachache and skin diseases (Duraipandiyan et al., 2006, Mothana et al., 2010) |
| Albizia lebbeck L. Benth ”Labak” |
KSU-15101 | Leguminosae | Riyadh/SA June 2014 |
Asthma, arthritis, epilepsy, diabetes and burns (Migahid 1989) |
|
Aloe perryi Baker ”Teif” |
Sana-4469 | Xanthorrhoeaceae Asphodelaceae |
Socotra/Yemen June 2014 | Eye infections, hemorrhoids, wound healing, burns and skin diseases (Al-Fatimi et al., 2005) |
| Anagallis arvensis L. = Scarlet pimpernel ”Ein alkot” |
KSU-15866 | Myrsinaceae | Wadi Al-Ghaat/SA February 2013 |
Fungal infections, skin diseases, leprosy, epilepsy (Lopez et al., 2011) |
|
Artemisia absinthium L. ”Shoukr or Sheeh” |
Sana-34 | Asteraceae | Sana’a/Yemen June 2014 |
Fever, urinary tract diseases, fragmentation of kidney stones, expulsion of worms and snakes (Jaradat, 2005, Lachenmeier, 2010) |
| Caralluma quadrangula Forssk ”Ghalf” | KSU-15450 | Asclepiadaceae | Jizan/SA March/2013 | Diabetes, general tonic (Adnan et al., 2014) |
| Caralluma wissmanii Schwartz = Angolluma wissmanii Plowes ” Atba’a alkalbah” | KSU-16009 | Asclepiadaceae | Agabat Alabna/SA March 2013 |
Stomachache, diabetes (Adnan et al., 2014) |
| Citrullus colocynthis L. Schrad. ”Hanzal” | Sana-32 | Cucurbitaceae | Sabwa/Yemen January 2014 |
Diabetes, constipation, hair-growth-promoting (Rahimi et al., 2012) |
| Commiphora gileadensis L. = C. opobalsamum L. Engl. ”Basham” | Sana-29 | Burseraceae | Hadramout/Yemen August 2014 |
Headache, urinary retention (Abbas et al., 2007) |
|
Costus spicatus Jacq. ‘’Qist’’ |
Sana-5 | Costaceae | Taiz /Yemen March 2013 |
Complaints of the bladder and urethra, expel kidney stones (Quintans Júnior et al., 2010) |
|
Cyperus rotundus Linn. “Alsaad” |
KSU-15182 | Cyperaceae | Najd area/ SA March 2016 | Wounds, bruises, carbuncles, uterine disorders (Al-Massarani et al., 2016) |
|
Dracaena cinnabari Balf.f. ”Dam alakhwain” |
Sana-9 SP-D225 |
Asparagaceae | Socotra/Yemen March 2014 | Dysentery, diarrhea, hemorrhage (Al-Fatimi et al., 2005) |
|
Eucalyptus tereticornis Sm. ”Kafoor” |
Sana-41 | Myrtaceae | Ibb/Yemen July 2014 |
Insecticidal, anesthetic, antiseptic (Maurya et al., 2016) |
|
Foeniculum vulgare Mill. ”Shomar” |
Sana-19 | Apiaceae | Ibb/Yemen July 2014 |
Abdominal pain (Oktay et al., 2003) |
| Hibiscus sabdariffa L. ”Karkadeh” |
Sana-18 | Malvaceae. | Ibb/Yemen May 2014 |
Hypertension (Wahabi et al., 2010) |
|
Hyssopus officinalis L. “Zofa” |
Sana-4 | Lamiaceae | Dhale/Yemen April 2013 |
Coughing and sore throat (Ortiz de Elguea-Culebras et al., 2018) |
| Indigofera spinosa Forssk. ”Shabrak” |
KSU-15794 | Fabaceae | Jabal Shatha/SA February 2013 | Kidney stones, cough, cold (Al-Fatimi et al., 2007) |
|
Jasminum grandiflorum L. ”Alganah” |
Sana-45 | Oleaceae | Taiz/Yemen June 2014 |
Toothache, ulcers (Arun et al., 2016) |
|
Jasminum sambac L. ”Fol or Yasmeen Arabi” |
Sana-6 | Oleaceae | Taiz/Yemen June 2014 |
Fragrance (Sengar et al., 2015) |
| Lavandula angustifolia Miller ”Dharm” | Sana-13 | Lamiaceae | Aden/Yemen June 2014 |
Diuretic (Cavanagh and Wilkinson 2002) |
|
Nigella sativa L. ”Habba soda” |
KSU-15132 | Ranunculaceae | LM/Riyadh/SA June 2014 |
Asthma, cough, bronchitis, rheumatoid arthritis (Al-Fatimi et al., 2005) |
| Ocimum tenuiflorum L. ”Reehan” |
Sana-48 | Lamiaceae | Dalih/Yemen March 2014 | Gastroenteritis, dysentery, diarrhea, wound healing, acne, vitiligo (Chhetri et al., 2015) |
| Pandanus odoratissimus Linn. ”Kadi” | Sana-111 | Pandanaceae | Hodeida/Yemen June 2014 |
Headache, rheumatism, epilepsy, urinary complains, enuresis (El-Shaibany et al., 2016). |
| Phoenix dactylifera L. ”Ajwa seed” |
Sana-11 | Arecaceae | Hadramout/Yemen July 2013 |
Diabetes, febrile fever (Al-daihan and Bhat, 2012) |
|
Propolis (bee glue) ”Okbor” |
Sana-28 | Apidae | Mahwit/Yemen July 2013 |
Gastroenteritis, infectious diseases (Fernandes et al., 2005) |
|
Psidium guajava Linn. ”Guava” |
Sana-20 | Myrtaceae | Lahj/Yemen June 2013 |
Cough, inflammation, diabetes, hypertension, diarrhea (Gutierrez et al., 2008) |
|
Punica granatum L. ”Romman” |
KSU-15156 | Punicaceae | Ibb/Yemen May 2014 |
Diabetes, gum bleeding (Jurenka 2008) |
|
Rosmarinus officinalis L. ”Ekleel aljabal” |
Sana-23 | Lamiaceae | Taiz/Yemen May 2014 |
Renal colic, dysmenorrhea (al-Sereiti et al., 1999) |
|
Ruta chalepensis L. ”Shathab” |
Sana-30 | Rutaceae | Sana’a/Yemen May 2014 |
Pain, fever, rheumatism, epilepsy (Al-Said et al., 1990) |
|
Salvia spinosa L. ”Lesan Althor” |
Sana-52 | Labiatae | Dhamar/Yemen August 2014 | Diarrhea, urinary disorders, piles, chest and stomach pains (Bahadori et al., 2015) |
|
Saussurea lappa C.B. Clarke ‘’Qist Hindi’’ |
KSU-16323 | Asteraceae | LM/Riyadh/SA March 2014 |
Asthma, gastric ulcer, inflammation and liver diseases (Zahara et al., 2014) |
| Sisymbrium irio L. “Howerna” |
KSU-14380 | Brassicaceae | Najd area/ SA February 2015 | Cough, chest congestion, clean wounds (Al-Massarani et al., 2017) |
| Sisymbrium officinale L. ”Samara” |
Sana-17 | Brassicaceae | Dhamar/Yemen April 2013 |
Sore throat, bronchitis, poison and venom antidote (Blazević et al. 2010) |
|
Taraxacum officinale L. “Tarkhashkon” |
Sana- 8 | Asteraceae | Ibb/Yemen May 2013 |
Digestive disorders, bile and liver problems, diuretic (Bhatia et al., 2014) |
|
Teucrium polium L. ”Ja’adah” |
KSU-15788 | Lamiaceae | Akabat Alabna/SA April 2013 | Diabetes, hypertension, inflammation, rheumatism (Tariq et al., 1989) |
| Tribulus terrestris L. “Qutiba” |
Sana-17 | Zygophyllaceae | Taiz/Yemen August 2013 |
Kidney stone, infertility, erectile dysfunction (El-Shaibany et al., 2015) |
| Vitis vinifera L. “Karm” |
Sana-9 | Vitaceae | Saada/Yemen June 2013 |
Diabetes, anti-cholesterol, and anti-platelet functions (Feei Ma and Zhang 2017) |
| Zea mays L. (silk corn fiber) ”Zorah” | Sana-7 | Poaceae | Sana/Yemen August 2014 |
Urinary tract disorders, kidney stones, asthma, hypertension (Žilić et al., 2016) |
VN: Voucher No. of the Plant, Ht: height.
SA: Saudi Arabia, LM: local market.
2.2. Extraction of plant material
The air-dried and powdered plant materials (10 g of each) were extracted with different organic solvents (300 mL × 2) at room temperature by cold maceration. The combined extracts were filtered and concentrated under reduced pressure using a rotary evaporator (Buchi, Flawil, Switzerland) to obtain the crude dried residues; stored at −10 °C until use.
2.3. Mosquitoes
Aedes aegypti L. (Orlando 1952 strain) used in larvicidal bioassays were supplied from a laboratory colony maintained at the Mosquito and Fly Research Unit at the USDA-ARS, Center for Medical, Agricultural, and Veterinary Entomology (CMAVE), Gainesville, FL. The detailed mosquito rearing was previously reported (Pridgeon et al., 2008).
2.4. Adulticidal activity
The toxicity of each plant sample, against adult female Ae. aegypti, was measured using the procedure described by Chang et al. (2014). Initial adult screening was performed at 5 μg/mosq on three to six-day post-emergence females. Stock permethrin (0.1 μg/μL in DMSO) was a technical grade mixture of 46.1% cis and 53.2 trans isomers (Chemservice, West Chester, PA) and used to prepare controls of 0.38 and 1.72 ng/μL. These dilutions, along with acetone were included as positive and negative controls, respectively for each assay. Acetone was used to dilute the stock solutions and produce a 200 mM DMSO/acetone treatment solution that was used to prepare three serial dilutions (1:1) in acetone. Mortality was scored at 24 h and assays were repeated at least three times.
2.5. Larvicidal activity
Bioassays were conducted using the system described by Ali et al. (2013) to determine the larvicidal activity of the selected plants against 1st instar Ae. aegypti. This method uses 1st instar larvae, rather than the 3rd instars of the WHO larval bioassay, to take advantage of small quantities of isolated extracts which are often not available in amounts adequate for the WHO assay. Permethrin and acetone were used as positive and negative controls, respectively for each assay. Permethrin at 0.025 ppm gave 100% mortality and acetone had 0% mortality in the screening bioassays. Larval mortality was recorded 24 h post treatment.
2.6. LC-MS/MS analysis
LC-MS/MS analysis was carried out using an AB Sciex 3200 Q TRAP MS/MS detector. Experiments were performed with a Shimadzu 20A HPLC system coupled to an Applied Biosystems 3200 Q-Trap LC- MS/MS instrument equipped with an ESI source operating in negative ion mode. For the chromatographic separation, a GL Science Intersil ODS 250 × 4.6 mm, i.d., 5 µm particle size, octadecyl silica gel analytical column operating at 40 °C has been used. The solvent flow rate was maintained at 0.7 mL/min (0.5 mL/min for O.tenuiflorum and N. sativa extracts). Detection was carried out with PDA detector. The elution gradient consisted of mobile phases (A) acetonitrile: water: formic acid (10:89:1, v/v/v) and (B) acetonitrile: water: formic acid (89:10:1, v/v/v). The composition of B was increased from 10% to 100% in 40 min. LC-ESI-MS/MS data were collected and processed by Analyst 1.6 software.
2.7. Headspace-SPME
The manual SPME device (Supelco, Bellafonte, PA, USA) with a fiber-precoated 65 μm thick layer of polydimethylsiloxane/divinylbenzene (PDMS/DVB-blue) was used for extraction of Aloe perryi volatiles. The vial containing the petroleum ether extract was sealed with parafilm. The fiber was pushed through the film layer for exposure to the headspace of the extract for 15 min at 40 °C. The fiber was then inserted immediately into the injection port of the GC-MS for desorption of the adsorbed volatile compounds for analysis.
2.8. GC-MS analysis
The GC-MS analysis was carried out with an Agilent 5975 GC-MSD system. Innowax FSC column (60 m × 0.25 mm, 0.25 μm film thickness) was used with helium as carrier gas (0.8 mL/min). GC oven temperature was kept at 60 °C for 10 min and programmed to 220 °C at a rate of 4 °C/min, and kept constant at 220 °C for 10 min and then programmed to 240 °C at a rate of 1 °C/min. The injector temperature was set at 250 °C. Mass spectra were recorded at 70 eV. Mass range was from m/z 35 to 450. Relative percentage amounts of the separated compounds were calculated from TIC chromatograms.
The identification of the essential oil components was carried out by comparison of their relative retention times with those of authentic samples or by comparison of their relative retention index (RRI) to series of n-alkanes. Computer matching against commercial (Wiley GC/MS Library, MassFinder Software 4.0) (McLafferty and Stauffer, 1989, Hochmuth, 2008) and in-house “Başer Library of Essential Oil Constituents” built up by genuine compounds and components of known oils.
3. Results
3.1. Adulticidal and larvicidal activities against Ae. aegypti
The Saudi and Yemeni medicinal plants were evaluated in adulticidal and larvicidal bioassays against the yellow fever and dengue mosquitoes. In adult bioassays, extracts were tested at the screening dose of 5 μg/mosquito against female Ae. aegypti. Out of the 57 screened extracts, the EtOH extract of H. officinalis aerial parts (#29), the MeOH extract of N. sativa seeds (#34), the MeOH extract of O. tenuiflorum aerial parts (#36), the EtOH extract of S. lappa roots (#50) and the EtOH extract of T. officinale aerial parts (#53) produced over 80% mortality at the tested concentration of 5 μg/mosquito (Table 2). Among which, S. lappa possessed the greatest mortality in the adulticidal activity. Average mortality in the lower dose permethrin control (0.19 ng/mosquito) was 60 ± 10% and at the higher dose of 0.86 ng/mosquito was 100%. The acetone had an average mortality of 6.7 ± 5.8% and untreated controls showed 0% mortality. Screening for larvicidal activity indicated 100% mortality at the dose of 31.25 ppm for petroleum ether extract of A. perryi flowers whereas methanol extract of P. dactylifera showed 100% mortality at 125 ppm and the mortality of methanol extract of O. tenuifolium was 70% against 1st instar Ae. aegypti larvae. Ethanol extract of S. lappa roots gave 100% mortality at 125 and 62.5 ppm whereas larval mortality at 31.25 ppm was 40%. Control mortality in these experiments was 0 for solvent only wells and 100% in permethrin treated wells (0.025 ppm).
Table 2.
Adulticidal activities of tested plant extracts against Ae. aegypti.
| # | Plant species | Plant part screened | Extraction solvent | % mortality ± SE 5 μg/mosquito |
|---|---|---|---|---|
| 1 | Acacia nilotica | F | EtOH | 63.3 ± 15.3 |
| 2 | Acalypha fruticosa | L, S | MeOH | 30 ± 20 |
| 3 | Acalypha fruticosa | L, S | n-Hexane | 30 ± 17.3 |
| 4 | Acalypha fruticosa | L, S | CHCl3 | 23.3 ± 5.8 |
| 5 | Acalypha fruticosa | L, S | EtOAc | 6.7 ± 11.5 |
| 6 | Acalypha fruticosa | L, S | n-BuOH | 3.3 ± 5.8 |
| 7 | Acalypha fruticosa | L, S | Water | 6.7 ± 5.8 |
| 8 | Albizia lebbeck | Fr | EtOH | 3.3 ± 5.8 |
| 9 | Albizia lebbeck | Se | EtOH | 10 ± 10 |
| 10 | Aloe perryi | F | MeOH | 53.3 ± 30.6 |
| 11 | Aloe perryi | F | Pet. ether | 60 ± 17.3 |
| 12 | Aloe perryi | F | Water | 50 ± 10 |
| 13 | Anagallis arvensis | L, S | MeOH | 10 ± 10 |
| 14 | Anagallis arvensis | L, S | EtOH | 6.7 ± 5.8 |
| 15 | Artemisia absinthium | L, S | MeOH | 10 |
| 16 | Artemisia absinthium | L, S | n-Hexane | 6.7 ± 5.8 |
| 17 | Artemisia absinthium | L, S | Water | 3.3 ± 5.8 |
| 18 | Caralluma quadrangula | L, S | EtOH | 13.3 ± 5.8 |
| 19 | Caralluma wissmannii | L, S | EtOH | 3.3 ± 5.8 |
| 20 | Citrullus colocynthis | L, S | MeOH | 3.3 ± 5.8 |
| 21 | Commiphora gileadensis | B | MeOH | 56.7 ± 15.3 |
| 22 | Commiphora gileadensis | Gum | – | 70 ± 26.5 |
| 23 | Costus spicatus | R | EtOH | 56.7 ± 28.9 |
| 24 | Cyperus rotundus | R | EtOH | 63.3 ± 20.8 |
| 25 | Dracaena cinnabari | Re | MeOH | 20 ± 10 |
| 26 | Eucalyptus tereticornis | L | MeOH | 23.3 ± 15.3 |
| 27 | Foeniculum vulgare | L | MeOH | 6.7 ± 5.8 |
| 28 | Hibiscus sabdariffa | L | MeOH | 16.7 ± 20.8 |
| 29 | Hyssopus officinalis | L, S | EtOH | 86.7 ± 15.3 |
| 30 | Indigofera spinose | L, S | EtOH | 23.3 ± 15.3 |
| 31 | Jasminum grandiflorum | L, S | EtOH | 3.3 ± 5.8 |
| 32 | Jasminum sambac | L | MeOH | 3.3 ± 5.8 |
| 33 | Lavandula angustifolia | F | MeOH | 10 ± 10 |
| 34 | Nigella sativa | Se | MeOH | 93.3 ± 11.5 |
| 35 | Nigella sativa | Se | Water | 50 ± 17.3 |
| 36 | Ocimum tenuiflorum | L, S | MeOH | 96.7 ± 5.8 |
| 37 | Pandanus odoratissimus | L | MeOH | 46.7 ± 15.3 |
| 38 | Pandanus odoratissimus | Peduncle | MeOH | 23.1 ± 32.1 |
| 39 | Pandanus odoratissimus | F | MeOH | 3.3 ± 5.8 |
| 40 | Pandanus odoratissimus | F | Pet. ether | 50 ± 20 |
| 41 | Pandanus odoratissimus | F | Water | 63.3 ± 15.3 |
| 42 | Phoenix dactylifera | Se | MeOH | 10 ± 10 |
| 43 | Phoenix dactylifera | Se | Pet. ether | 10 ± 10 |
| 44 | Propolis (bee glue) | Re | MeOH | 13.3 ± 5.8 |
| 45 | Psidium guajava | L | MeOH | 23.1 ± 23.1 |
| 46 | Punica granatum | F | MeOH | 73.3 ± 15.3 |
| 47 | Rosmarinis officinalis | L, S | MeOH | 6.7 ± 11.5 |
| 48 | Ruta chalepensis | L, S | MeOH | 16.7 ± 28.9 |
| 49 | Salvia spinosa | L, S | MeOH | 13.3 ± 5.8 |
| 50 | Saussurea lappa | R | EtOH | 100 |
| 51 | Sisymbrium irio | L, S | Water | 73.3 ± 5.8 |
| 52 | Sisymbrium officinale | L, S | MeOH | 10 ± 17.3 |
| 53 | Taraxacum officinale | L, S | EtOH | 93.3 ± 5.8 |
| 54 | Teucrium polium | L | EtOH | 16.7 ± 15.3 |
| 55 | Tribulus terrestis | L, S | MeOH | 36.7 ± 5.8 |
| 56 | Vitis vinifera (Red grape) | Se | MeOH | 23.3 ± 15.3 |
| 57 | Zea mays (silk corn fiber) | Fiber | MeOH | 3.3 ± 5.8 |
| Acetone | 6.7 ± 5.8 | |||
| Untreated | 0 | |||
| Permethrin (0.86 ng/mosquito) | 100 | |||
| Permethrin (0.19 ng/mosquito) | 60.0 ± 10.0 | |||
B: Bark; L: Leaves; F: Flowers; R: Roots or rhizomes; Re: resin; S: Stems; Se: Seeds; Fr: Fruits.
3.2. LC-MS/MS analysis
Based on results, the active alcoholic extracts were processed for LC MS/MS analysis to identify the bioactive compounds. The results of the analyzed fractions (the MeOH extracts of H. officinalis and O. tenuiflorum and the EtOH extracts S. lappa, H. officinalis and T. officinale) are presented in Table 3.
Table 3.
Identified compounds by LC-MS/MS analysis of the active plant extracts.
| RT | [M-H]−m/z | Fragments | Identified compounds | |
|---|---|---|---|---|
| H. officinalis leaves & stems EtOH extract # 29 | ||||
| 8.0 | 353 | 191, 179 | 3-caffeoylquinic acid | |
| 9.7 | 637 | 351, 285 | luteolin diglucuronide | |
| 9.9 | 447 | 285 | luteolin glucoside | |
| 9.9 | 609 | 301, 271, 255, 179 | quercetin 7-rutinoside | |
| 10.5 | 637 | 461, 285 | leukoseptoside A | |
| 11.1 | 621 | 487, 351, 269 | apigenin derivative | |
| 11.4 | 461 | 285 | luteolin glucuronide | |
| 12.6 | 445 | 269, 175, 113 | apigenin glucuronide | |
| 13.1 | 359 | 197, 179, 161 | rosmarinic acid | |
| 16.3 | 285 | 175, 133 | luteolin | |
| N. sativa seeds MeOH extract # 34 | ||||
| 3.5 | 286 | 162 | unknown | |
| 4.9 | 267 | 249 | unknown | |
| 5.3 | 289 | 199, 169, 127 | unknown | |
| 6.8 | 401 | 283, 269 | apigenin pentoside | |
| 7.7 | 353 | 191, 179, 161 | 5-caffeoylquinic acid | |
| 7.9 | 771 | 609, 429, 284 | luteolin / Kaempferol-sophoroside-glucoside | |
| O. tenuiflorum leaves & stems MeOH extract # 36 | ||||
| 7.7 | 341 | 179 | caffeoyl glucoside | |
| 9.4 | 609 | 300, 271, 179, 151 | rutin | |
| 10.4 | 463 | 300, 271, 179, 151 | quercetin glucuronide | |
| 13.2 | 539 | 471, 377, 307, 275 | unknown | |
| 13.9 | 359 | 197, 179, 161 | rosmarinic acid | |
| 18.0 | 581 | 461, 436 | unknown | |
| 27.5 | 343 | 328, 313, 241 | nevadensin | |
| 27.8 | 283 | 240, 215 | acacetin/ wogonin | |
| 30.6 | 555 | 487, 469, 425 | unknown | |
| 33.6 | 293 | 275, 235, 231, 171 | unknown | |
| S. lappa root EtOH extract # 50 | ||||
| 9.2 | 353 | 191, 173 | 5-caffeoylquinic acid | |
| 12.3 | 515 | 352, 191, 179, 161 | 1,5-dicaffeoylquinic acid | |
| 12.4 | 515 | 353, 299, 203, 191, 179 | 4,5-dicaffeoylquinic acid | |
| 13.2 | 561 | 369, 351, 215, 191 | feruloyl quinic acid derivative | |
| 14.3 | 313 | 298, 283, 265 | dihydroxy-dimethoxyflavone similar to cirsimaritin | |
| 15.1 | 431 | 268 | apigenin glucoside | |
| T. officinale leaves & stems EtOH extract # 53 | ||||
| 6.0 | 341 | 179, 161 | caffeoyl glucoside | |
| 9.1 | 191 | 173, 127 | quinic acid | |
| 9.9 | 447 | 357, 327 | luteolin-6-C-glucoside | |
| 10.0 | 179 | 135 | caffeic acid | |
| 11.1 | 477 | 301, 179, 151 | quercetin glucuronide | |
| 11.3 | 198 | 163 | unknown | |
| 12.1 | 461 | 285 | luteolin glucuronide | |
| 14.5 | 473 | 293, 219, 179, 161 | cichoric acid | |
| 15.9 | 285 | 199, 151, 133 | luteolin | |
| 17.9 | 269 | 201, 151, 117 | apigenin | |
3.2.1. Identification of caffeic and quinic acids derivatives
The EtOH extract of T. officinale revealed caffeoyl and hexose esterification of caffeic acid, indicated by a molecular ion peak at m/z 341 [M-H]− then fragmented ion at m/z 179 [M-H]− and a base peak ion at m/z 135 [M-H]−, characteristic for caffeic acid, in addition to another peak at 161. Loss of a −162 amu hexose unit allowed the determination of this compound as caffeoyl glucoside. Cichoric acid which contains two caffeic acid and tartaric acid units was also identified in the T. officinale extract (Table 3). Cichoric acid presented a pseudo molecular ion peak at m/z 473 and caffeic acid fragments at m/z 179 and 161 (Table 3). The EtOH extract H. officinalis showed a molecular ion peak at m/z 359 [M-H]− and product ions at m/z 197 [M-H]− and 161 [M-H]− which presents characteristic fragmentation behavior of rosmarinic acid (caffeic acid dimer). Rosmarinic acid was also the most abundant compound in O. tenuiflorum extract (Table 3).
A molecular ion peak at m/z 191 with fragmented ions at m/z 173 and 127 indicated the presence of quinic acid in T. officinale extract (Table 3). Caffeic acid and quinic acid esters were distinguished as caffeoylquinic acid. Identification of these compounds was done according to the identification key previously published by Clifford and collogues (Clifford et al., 2003, Clifford et al., 2005, Clifford et al., 2008).
The 3-caffeoylquinic acid, presented by a pseudo molecular ion peak at m/z 353 and a base peak ion at m/z 191 was determined in the EtOH extract of H. officinalis. The high abundance ion at m/z 179 allowed the identification of this compound as 3-caffeoylquinic acid (Table 3).
3.2.2. Identification of luteolin and apigenin derivatives
The luteolin was determined in T. officinale and H. officinalis with its molecular ion peak at m/z 285 [M-H]− and product ions at m/z 151 and 133 amu. Luteolin glucuronide, determined in T. officinale and H. officinalis extracts, showed a pseudo molecular ion peak at m/z 461 and a base peak ion at m/z 285 (luteolin aglycon) due to the loss of a 176 amu glucouronide moiety (Kapp et al., 2013). The diglucuronide of luteolin was also suggested in H. officinalis extract at m/z 637 amu. Luteolin glucoside presenting a molecular ion peak at m/z 447 and an aglycon at m/z 285 (loss of a glucose moiety) was detected in O. tenuiflorum and H. officinalis extracts. T. officinale extract had also showed the same molecular ion peak but with different product ions at m/z 357 and 327. 90. The 30 amu difference from the molecular ion peak indicated that the compound is a C-glucoside (Taamalli et al., 2015). Subsequently, it was determined as luteolin-6-C-glucoside (isoorientin). Apigenin and its derivative were determined in the same way described above. As an aglycon, apigenin was only determined in T. officinale, its glucoside derivative was found in S. lappa, whereas glucuronide derivative was found in H. officinalis (Table 3).
3.3. HS-SPME-GC/MS analysis
In order to identify the volatile constituents of the petroleum ether extract of Aloe perryi, HS-SPME-GC/MS analysis was conducted. Thirty-three compounds were identified which represented 70.6% of A. perryi constitution. The ketone, 6-methyl-5-hepten-2-one (22.4%), menthol (8.9%) and the sesquiterpine 1,4-bis (1,1-dimethylethyl)-benzene (4.5%) were the main constituents (Table 4).
Table 4.
The volatile composition of the petroleum ether extract of Aloe perryi flowers.
| RRI | Constituents | Conc.% | IM |
|---|---|---|---|
| 1348 | 6-Methyl-5-hepten-2-one | 22.4 | MS |
| 1399 | Methyl octanoate | 1.2 | MS |
| 1400 | Tetradecane | 1.7 | RRI, MS |
| 1440 | 1,4-Bis (1,1-dimethylethyl)-benzene* | 4.5 | MS |
| 1443 | Ethyl octanoate | 1.7 | MS |
| 1452 | 1-Octen-3-ol | 3.5 | MS |
| 1475 | Acetic acid | 1.2 | RRI, MS |
| 1479 | Furfural | 1.3 | RRI, MS |
| 1496 | 2-Ethyl hexanol | 0.5 | MS |
| 1500 | Methyl nonanoate | 0.8 | MS |
| 1516 | 2-Acetyl furan | 0.4 | MS |
| 1521 | 2-Nonanol | 0.5 | MS |
| 1541 | Neomenthyl acetate | 0.7 | MS |
| 1541 | Benzaldehyde | 1.3 | RRI, MS |
| 1544 | Ethyl nonanoate | 0.8 | MS |
| 1589 | Ethyl malonate | 0.5 | MS |
| 1590 | 5-Methyl-2-furfural | 1.1 | MS |
| 1591 | 2-Methyl propanoic acid | 0.7 | MS |
| 1602 | 6-Methyl-3,5-heptadien-2-one | 1.7 | MS |
| 1625 | 4,4-Dimethyl but-2-enolide | 0.6 | MS |
| 1638 | Menthol | 8.9 | RRI, MS |
| 1647 | Butanedioic acid diethylester* | 0.4 | MS |
| 1684 | Isovaleric acid | 2.9 | RRI, MS |
| 1703 | 6-Oxo-Isophorone | 6.5 | MS |
| 1747 | 3,4-Dimethyl-2,5-furandione | 0.8 | MS |
| 1762 | Pentanoic acid | 0.4 | RRI, MS |
| 1800 | Ethyl phenylacetate | 0.6 | MS |
| 1815 | Methyl dodecanoate | 0.3 | MS |
| 1870 | Hexanoic acid | 0.7 | RRI, MS |
| 1853 | Ethyl dodecanoate | 0.2 | MS |
| 1868 | (E)-Geranyl acetone | 0.2 | MS |
| 1882 | 1-Isobutyl-4-isopropyl-3-isopropyl-2,2-Dimethyl succinate | 1.1 | MS |
| 1965 | 2-Ethyl hexanoic acid | 0.5 | MS |
| Total | 70.6 |
RRI: Relative retention indices calculated against n-alkanes; %: calculated from TIC data; *: Tentative identification from Wiley; IM: Identification method based on the relative retention indices (RRI) of authentic compounds on the HP Innowax column; MS, identified on the basis of computer matching of the mass spectra with those of the Wiley and MassFinder libraries and comparison with literature data.
4. Discussion
In our continuous search to find novel bioactive compounds from plants, 39 plant were evaluated for their insecticidal potential activities. Our findings are in agreement with reports for folkloric use, in some communities, for several of the currently screened plants or related species, as insecticides (Tomczyk and Szymanska, 1995, Singh et al., 2014, Benchouikh et al., 2015, Ortiz de Elguea-Culebras et al., 2018). The roots of S. lappa showing 100% mortality at 5 μg/mosquito are traditionally used in the Himalaya region. In a previous study, a moderate larvicidal activity was observed for the essential oil of S. lappa against Ae. aegypti with LC50 value 141.43 (Manzoor et al., 2013). The sesquiterpene costunolide in S. lappa demonstrated significant insecticidal activity against Papilio demoleus butterflies (Vattikonda et al., 2015). The 20% alcohol solution of Nigella sativa showed a 100% mortality against the cattle tick, Rhipicephalus annulatus (Aboelhadid, et al., 2016). T. officinale was also effective against the insect, B. cockerelli, commonly found on potato and tomato crops. The ethanol extract of the plant dried leaves killed more than 50% of 5th and 3rd instars with concentration of 0.01 and 0.1 g/ml, respectively (Granados-Echegoyen et al., 2015). The leaf extract of Ocimum gratissimum had a potent larvicidal activity with an LC50 19.50 mg/ml against Ae. aegypti, while in the present study, the tested species, O. tenuiflorum, was inactive against the larvae and demonstrated remarkable potency as adulticidal agent (Ghosh et al., 2012). Results of a previous study, on the mosquito larvicidal activity of petroleum ether extract of A. vera leaf, showed 34% mortality against Ae. aegypti 1st instar larvae at 80 ppm, increased to 89% at 400 ppm of A. vera leaf extract treatment (Subramaniam et al., 2012). The results clearly reveals that the currently investigated species, A. perryi, exhibits a higher potency (100% mortality for petroleum ether extract at 31.25 ppm). This could be due to higher concentration of active larvicidal compounds in the flowers.
Careful interpretation of the LC-MS/MS data of the five active extracts allowed the identification of 28 compounds. Luteolin was detected in three of the analyzed extracts (H. officinalis, T. officinale and N. sativa). Caffeic acid and its caffeoylquinic acid derivatives were also common constituents among the five analyzed fractions. The significant activities of some of the extracts can be substantially justified by their rich contents of phenolic acids and phenolic compounds in general. Previous studies demonstrated that phenolics may reduce insect herbivory in several ways such as discouraging feeding and oviposition, reducing fertility and shortening the insects life span (Dawkar et al., 2013, Czerniewicz et al., 2016). A study conducted by Mitchell and his coworkers, found that many plant flavonoids such as quercetin, chrysin, apigenin, kaempferol and morin, can inhibit, in a dose-dependent manner, the cytochrome P-450 dependent ecdysone 20-monooxygenase activity associated with adult female Ae. aegypti which results in direct cellular toxicity (Mitchell et al., 1993).
The ketone 6-methyl-5-hepten-2-one, identified as the major volatile constituent in the pet. ether extract of A. perryi, is also a volatile oil component of lemon-grass oil (Cympopogon citratus), and a known alarm pheromone constituent in many species of ants and other insects. Additionally, this compound is an acetylcholinesterase (AChE) and esterase enzyme inhibitor (Ganjewala, 2009). A former study indicated that AChE inhibitors decreases, in a dose-dependent way, the hatching of treated eggs, delay the development of larvae and deleteriously affect the behavior of insects (Emara, 2004). These results provide a rational explanation for the remarkable currently observed larvicidal activity of A. perryi. It is worth mentioning, that to the best of our knowledge, this is the first study assessing the mosquitocidal effects of most of the tested plants. Moreover, this is the first report investigating the volatile constituents of A. perryi collected in Yemen or elsewhere.
5. Conclusion
The present study rationalizes the use of some of the explored plants in ethno-agricultural practices. The results suggest that A. perryi, H. officinalis, N. sativa, O. tenuiflorum, S. lappa and T. officinale could be promising sources of new potential eco-friendly mosquitocidal agents. Based on the data, treatments with phenolic acids and flavonoids-rich plant extracts caused a significant insecticidal activity and decreased the number of Ae. aegypti adults. However, bio-guided fractionation must be carried out in order to isolate and identify the compounds that are responsible for these insecticidal activities.
Declaration of Competing Interest
All the authors declare that they have no conflict of interest.
Acknowledgments
This research project was supported by a grant from the “Research Centre of the Female Scientific and Medical Colleges”, Deanship of Scientific Research, King Saud University. This study was in part funded by the Deployed War-Fighter Protection Research Programme via grants from the U.S. Department of Defense through the Armed Forces Pest Management Board. We thank Miss Jessica Louton, (USDA-ARS, CMAVE, Gainesville FL) for mosquito bioassays.
Footnotes
Peer review under responsibility of King Saud University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jsps.2019.07.001.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- Abbas F.A., Al-Massarany S.M., Khan S., Al-Howiriny T.A., Mossa J.S., Abourashed E.A. Phytochemical and biological studies on Saudi Commiphora opobalsamum L. Nat. Prod. Res. 2007;21:383–391. doi: 10.1080/14786410600942025. [DOI] [PubMed] [Google Scholar]
- Adnan M., Jan S., Mussarat S., Tariq A., Begum S., Afroz A., Shinwari Z.K. A review on ethnobotany, phytochemistry and pharmacology of plant genus Caralluma R. Br. J. Pharm. Pharmacol. 2014;66:1351–1368. doi: 10.1111/jphp.12265. [DOI] [PubMed] [Google Scholar]
- Al-daihan S., Bhat R.S. Antibacterial activities of extracts of leaf, fruit, seed and bark of Phoenix dactylifera. AJOL. 2012;11:10021–10025. [Google Scholar]
- Al-Fatimi M., Friedrich U., Jenett-Siems K. Cytotoxicity of plants used in traditional medicine in Yemen. Fitoterapia. 2005;76:355–358. doi: 10.1016/j.fitote.2005.02.009. [DOI] [PubMed] [Google Scholar]
- Al-Fatimi M., Wurster M., Schroder G., Lindequist U. Antioxidant, antimicrobial and cytotoxic activities of selected medicinal plants from Yemen. J. Ethnopharmacol. 2007;111:657–666. doi: 10.1016/j.jep.2007.01.018. [DOI] [PubMed] [Google Scholar]
- Al-Massarani S., Al-Enzi F., Al-Tamimi M., Al-Jomaiah N., Al-amri R., Başer K., Demirci B. Composition & biological activity of Cyperus rotundus L. tuber volatiles from Saudi Arabia. Nat. Volatiles Essent. Oils. 2016;3:26–34. [Google Scholar]
- Al-Massarani S.M., El Gamal A.A., Alam P., Al-Sheddi E.S., Al-Oqail M.M., Farshori N.N. Isolation, biological evaluation and validated HPTLC-quantification of the marker constituent of the edible Saudi plant Sisymbrium irio L. Saudi Pharmaceut. J. 2017;25:750–759. doi: 10.1016/j.jsps.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Said M.S., Tariq M., Al-Yahya M.A., Rafatullah S., Ginnawi O.T., Ageel A.M. Studies on Ruta chalepensis, an ancient medicinal herb still used in traditional medicine. J. Ethnopharmacol. 1990;28:305–312. doi: 10.1016/0378-8741(90)90081-4. [DOI] [PubMed] [Google Scholar]
- Al-Sereiti M.R., Abu-Amer K.M., Sen P. Pharmacology of rosemary (Rosmarinus officinalis Linn.) and its therapeutic potentials. Indian J. Exp. Biol. 1999;37:124–130. [PubMed] [Google Scholar]
- Alhaeli A., Bahkali S., Ali A., Househ M.S., El-Metwally A.A. The epidemiology of Dengue fever in Saudi Arabia: a systematic review. J. Infect. Public Health. 2016;9:117–124. doi: 10.1016/j.jiph.2015.05.006. [DOI] [PubMed] [Google Scholar]
- Ali A., Akhtar N., Khan B., Khan M., Rasul A., Khalid N., Waseem K., Mahmood T., Ali L. Acacia nilotica: A plant of multipurpose medicinal uses. J. Med. Plants Res. 2012;6:1492–1496. [Google Scholar]
- Ali A., Demirci B., Kiyan H., Bernier U., Tsikolia M., Wedge D., Khan I., Baser K., Tabanca N. Biting deterrence, repellency, and larvicidal activity of Ruta chalepensis (Sapindales: Rutaceae) essential oil and its major individual constituents against mosquitoes. J. Med. Entomol. 2013;50:1267–1274. doi: 10.1603/me12177. [DOI] [PubMed] [Google Scholar]
- Aboelhadid S.M., Mahran H.A., El-Hariri H.M., Shokier K.M. Rhipicephalus annulatus (Acari: Ixodidae) control by Nigella sativa, thyme and spinosad preparations. J. Arthropod. Borne. Dis. 2016;10(2):148–158. [PMC free article] [PubMed] [Google Scholar]
- Arun M., Satish S., Anima P. Phytopharmacological profile of Jasminum grandiflorum Linn. (Oleaceae) Chin. J. Integr. Med. 2016;22:311–320. doi: 10.1007/s11655-015-2051-3. [DOI] [PubMed] [Google Scholar]
- Bahadori M.B., Valizadeh H., Asghari B., Dinparast L., Farimani M.M., Bahadori S. Chemical composition and antimicrobial, cytotoxicity, antioxidant and enzyme inhibitory activities of Salvia spinosa L. J. Funct. Foods. 2015;18:727–736. [Google Scholar]
- Benchouikh A., Allam T., Kribii A., Khadija O. The study of the insecticidal effect of Nigella sativa essential oil against Tuta absoluta larvae. IJSTR. 2015;4:88–90. [Google Scholar]
- Benelli G., Pavela R., Canale A., Cianfaglione K., Ciaschetti G., Conti F., Nicoletti M., Senthil-Nathan S., Mehlhorn H., Maggi F. Acute larvicidal toxicity of five essential oils (Pinus nigra, Hyssopus officinalis, Satureja montana, Aloysia citrodora and Pelargonium graveolens) against the filariasis vector Culex quinquefasciatus: synergistic and antagonistic effects. Parasitol. Int. 2017;66:166–171. doi: 10.1016/j.parint.2017.01.012. [DOI] [PubMed] [Google Scholar]
- Bhatia H., Sharma Y.P., Manhas R.K., Kumar K. Ethnomedicinal plants used by the villagers of district Udhampur, J&K, India. J. Ethnopharmacol. 2014;151:1005–1018. doi: 10.1016/j.jep.2013.12.017. [DOI] [PubMed] [Google Scholar]
- Blazević I., Radonić A., Mastelić J., Zekić M., Skocibusić M., Maravić A. Hedge mustard (Sisymbrium officinale): chemical diversity of volatiles and their antimicrobial activity. Chem. Biodivers. 2010;7:2023–2034. doi: 10.1002/cbdv.200900234. [DOI] [PubMed] [Google Scholar]
- Cavanagh H.M., Wilkinson J.M. Biological activities of lavender essential oil. Phytother. Res. 2002;16:301–308. doi: 10.1002/ptr.1103. [DOI] [PubMed] [Google Scholar]
- Chang F., Dutta S., Becnel J., Estep A., Mascal M. Synthesis of the insecticide prothrin and its analogues from biomass-derived 5 (chloromethyl) furfural. J. Agric. Food Chem. 2014;62:476–480. doi: 10.1021/jf4045843. [DOI] [PubMed] [Google Scholar]
- Chaudhary, S., 2001. Flora of the Kingdom of Saudi Arabia: Ministry of Agriculture and Water, Riyadh.
- Chhetri B.K., Ali N.A., Setzer W.N. A Survey of chemical compositions and biological activities of Yemeni aromatic medicinal plants. Medicines. 2015;2:67–92. doi: 10.3390/medicines2020067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifford M.N., Johnston K.L., Knight S., Kuhnert N. Hierarchical scheme for LC-MSn identification of chlorogenic acids. J. Agric. Food Chem. 2003;51:2900–2911. doi: 10.1021/jf026187q. [DOI] [PubMed] [Google Scholar]
- Clifford M.N., Kirkpatrick J., Kuhnert N., Roozendaal H., Salgado P.R. LC–MSn analysis of the Cis isomers of chlorogenic acids. Food Chem. 2008;106:379–385. [Google Scholar]
- Clifford M.N., Knight S., Kuhnert N. Discriminating between the six isomers of dicaffeoylquinic acid by LC-MS n. J. Agric. Food Chem. 2005;53:3821–3832. doi: 10.1021/jf050046h. [DOI] [PubMed] [Google Scholar]
- Czerniewicz P., Chrzanowski G., Sytykiewicz H., Sprawka I., Leszczynski B. Aphidicidal and deterrent activity of phenolic acid extracts from some herbal plants towards Myzus persicae Sulz. and Rhopalosiphum padi L. Fresen. Environ. Bull. 2016;25:5714–5721. [Google Scholar]
- Dawkar V., Chikate Y., Lomate P., Dholakia B., Gupta V., Giri A. Molecular insights into resistance mechanisms of Lepidopteran insect pests against toxicants. J. Proteome Res. 2013;12:4727–4737. doi: 10.1021/pr400642p. [DOI] [PubMed] [Google Scholar]
- Dinesh D.S., Kumari S., Kumar V., Das P. The potentiality of botanicals and their products as an alternative to chemical insecticides to sandflies (Diptera: Psychodidae): a review. J. Vector Borne Dis. 2014;51:1–7. [PubMed] [Google Scholar]
- Duraipandiyan V., Ayyanar M., Ignacimuthu S. Antimicrobial activity of some ethnomedicinal plants used by Paliyar tribe from Tamil Nadu, India. BMC Compl. Altern. Med. 2006;6:35. doi: 10.1186/1472-6882-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Shaibany A., AL-Habori M., Al-Massarani S., El-Gamal A., Al-Ajami A., Al-Adhl A. Hepatoprotective effect of Pandanus odoratissimus check for this species in other resources L Inflorescence extracts in acetaminophen-treated guinea pigs. Trop. J. Pharm. Res. 2016;15:259–266. [Google Scholar]
- El-Shaibany A., AL-Habori M., Al-Tahami B., Al-Massarani S. Anti-hyperglycaemic activity of Tribulus terrestris L aerial part extract in glucose-loaded normal rabbits. Trop. J. Pharm. Res. 2015;14:2263–2268. [Google Scholar]
- Emara T. Effect of 6-methyl-5-hepten-2-one on acetylcholinesterase activity, growth and development of Spodoptera littoralis. Egypt. J. Biol. 2004;6:136–146. [Google Scholar]
- Feei Ma Z., Zhang H. Phytochemical constituents, health benefits, and industrial applications of grape seeds: a mini-review. Antioxidants (Basel) 2017;6:71. doi: 10.3390/antiox6030071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes J.A., Balestrin E.C., Betoni J.E., Orsi Rde O., da Cunha M.L., Montelli A.C. Propolis: anti-Staphylococcus aureus activity and synergism with antimicrobial drugs. Mem. Inst. Oswaldo. Cruz. 2005;100:563–566. doi: 10.1590/s0074-02762005000500018. [DOI] [PubMed] [Google Scholar]
- Ganjewala D. Cymbopogon essential oils: hemical compositions and bioactivities. Int. J. Essen. Oil Ther. 2009;3:56–65. [Google Scholar]
- Ghosh A., Chowdhury N., Chandra G. Plant extracts as potential mosquito larvicides. Indian J. Med. Res. 2012;135(5):581–598. [PMC free article] [PubMed] [Google Scholar]
- Granados-Echegoyen C., Pérez-Pacheco R., Bautista-Martínez N., Alonso-Hernández N., Sánchez-García J.A., Martinez-Tomas S.H., Sánchez-Mendoza S. Insecticidal effect of botanical extracts on developmental stages of Bactericera cockerelli (Sulc) (Hemiptera: Triozidae) Southwest Entomol. 2015;40(1):97–110. [Google Scholar]
- Gutierrez R.M., Mitchell S., Solis R.V. Psidium guajava: A review of its traditional uses, phytochemistry and pharmacology. J. Ethnopharmacol. 2008;117:1–27. doi: 10.1016/j.jep.2008.01.025. [DOI] [PubMed] [Google Scholar]
- Hochmuth, D.H., 2008. MassFinder 4.0, Hochmuth Scientific Consulting, Hamburg, Germany.
- Jaradat N. Medical plants utilized in Palestinian folk medicine for treatment of diabetes mellitus and cardiac diseases. J. Al-Aqsa. Univ. 2005;9:1–29. [Google Scholar]
- Jurenka J.S. Therapeutic applications of pomegranate (Punica granatum L.): a review. Altern. Med. Rev. 2008;13:128–144. [PubMed] [Google Scholar]
- Kapp K., Hakala E., Orav A., Pohjala L., Vuorela P., Püssa T., Vuorela H., Raal A. Commercial peppermint (Mentha piperita L.) teas: antichlamydial effect and polyphenolic composition. Food Res. Int. 2013;53:758–766. [Google Scholar]
- Lachenmeier D.W. Wormwood (Artemisia absinthium L.) a curious plant with both neurotoxic and neuroprotective properties. J. Ethnopharmacol. 2010;131:224–227. doi: 10.1016/j.jep.2010.05.062. [DOI] [PubMed] [Google Scholar]
- Lopez V., Jager A.K., Akerreta S., Cavero R.Y., Calvo M.I. Pharmacological properties of Anagallis arvensis L. (“scarlet pimpernel”) and Anagallis foemina Mill. (“blue pimpernel”) traditionally used as wound healing remedies in Navarra (Spain) J. Ethnopharmacol. 2011;134:1014–1017. doi: 10.1016/j.jep.2010.12.036. [DOI] [PubMed] [Google Scholar]
- Manzoor F., Samreen K.B., Parveen Z. Larvicidal activity of essential oils against Aedes aegypti and Culex quinquefasciatus larvae (Diptera: Culicidae) J. Anim. Plant Sci. 2013;23(2):420–424. [Google Scholar]
- Maurya A., Verma S., Jayanthy A., Shankar M., Sharma R. Concise review on phytochemistry and pharmacological properties of Eucalyptus tereticornis Smith. AJRC. 2016;9:457–461. [Google Scholar]
- McLafferty F.W., Stauffer D.B. J Wiley and Sons; New York, USA: 1989. The Wiley/NBS Registry of Mass Spectral Data. [Google Scholar]
- Migahid A.M. third ed. University Libraries, King Saud University; Riyadh: 1989. Flora of Saudi Arabia. [Google Scholar]
- Mitchell M., Keogh D., Crooks J., Smith S. Effects of plant flavonoids and other allelochemicals on insect cytochrome P-450 dependent steroid hydroxylase activity. Insect Biochem. Mol. Biol. 1993;23:65–71. doi: 10.1016/0965-1748(93)90083-5. [DOI] [PubMed] [Google Scholar]
- Moreno-Madriñán M., Turell M. History of mosquitoborne diseases in the United States and implications for new pathogens. Emerg. Infect. Dis. 2018;24:821–826. doi: 10.3201/eid2405.171609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mothana R.A., Abdo S.A., Hasson S., Althawab F.M., Alaghbari S.A., Lindequist U. Antimicrobial, antioxidant and cytotoxic activities and phytochemical screening of some Yemeni medicinal plants. Evid. Based Compl. Alternat. Med. 2010;7:323–330. doi: 10.1093/ecam/nen004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolopoulou-Stamati P., Maipas S., Kotampasi C., Stamatis P., Hens L. Chemical pesticides and human health: the urgent need for a new concept in agriculture. Front. Public Health. 2016;4:148. doi: 10.3389/fpubh.2016.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oktay M., Gülçin İ., Küfrevioğlu Ö.İ. Determination of in vitro antioxidant activity of fennel (Foeniculum vulgare) seed extracts. LWT - Food Sci. Technol. 2003;36:263–271. [Google Scholar]
- Ortiz de Elguea-Culebras G., Sánchez-Vioque R., Berruga M., Herraiz-Peñalver D., González-Coloma A., Andrés M., Santana-Méridas O. Biocidal potential and chemical composition of industrial essential oils from Hyssopus officinalis, Lavandula intermedia var. Super, and Santolina chamaecyparissus. Chem. Biodivers. 2018;15(1):e1700313. doi: 10.1002/cbdv.201700313. [DOI] [PubMed] [Google Scholar]
- Pridgeon J.W., Pereira R.M., Becnel J.J., Allan S.A., Clark G.G., Linthicum K.J. Susceptibility of Aedes aegypti, Culex quinquefasciatus Say, and Anopheles quadrimaculatus Say to 19 pesticides with different modes of action. J. Med. Entomol. 2008;45:82–87. doi: 10.1603/0022-2585(2008)45[82:soaacq]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Quintans Júnior L., Santana M., Melo M., de Sousa D., Santos I., Siqueira R., Lima T., Silveira G., Antoniolli A., Ribeiro L., Santos M. Antinociceptive and anti-inflammatory effects of Costus spicatus in experimental animals. Pharm. Biol. 2010;48:1097–1102. doi: 10.3109/13880200903501822. [DOI] [PubMed] [Google Scholar]
- Rahimi R., Amin G., Ardekani M.R. A review on Citrullus colocynthis Schrad. from traditional Iranian medicine to modern phytotherapy. J. Altern. Compl. Med. 2012;18:551–554. doi: 10.1089/acm.2011.0297. [DOI] [PubMed] [Google Scholar]
- Sampson B., Tabanca N., Kirimer N., Demirci B., Baser K., Khan I., Spiers J., Wedge D. Insecticidal activity of 23 essential oils and their major compounds against adult Lipaphis pseudobrassicae (Davis) (Aphididae: Homoptera) Pest. Manage. Sci. 2005;61:1122–1128. doi: 10.1002/ps.1100. [DOI] [PubMed] [Google Scholar]
- Sengar N., Joshi A., Prasad S.K., Hemalatha S. Anti-inflammatory, analgesic and anti-pyretic activities of standardized root extract of Jasminum sambac. J. Ethnopharmacol. 2015;160:140–148. doi: 10.1016/j.jep.2014.11.039. [DOI] [PubMed] [Google Scholar]
- Singh R., Jayaramaiah R., Sarate P., Thulasiram H., Kulkarni M., Giri A. Insecticidal potential of defense metabolites from Ocimum kilimandscharicum against Helicoverpa armigera. PLoS One. 2014;9:e104377. doi: 10.1371/journal.pone.0104377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramaniam J., Kovendan K., Kumar P.M., Murugan K., Walton W. Mosquito larvicidal activity of Aloe vera (Family: Liliaceae) leaf extract and Bacillus sphaericus, against Chikungunya vector, Aedes aegypti. Saudi J. Biol. Sci. 2012;19:503–509. doi: 10.1016/j.sjbs.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taamalli A., Arráez-Román D., Abaza L., Iswaldi I., Fernández-Gutiérrez A., Zarrouk M., Segura-Carretero A. LC-MS-based metabolite profiling of methanolic extracts from the medicinal and aromatic species Mentha pulegium and Origanum majorana. Phytochem. Anal. 2015;26:320–330. doi: 10.1002/pca.2566. [DOI] [PubMed] [Google Scholar]
- Tariq M., Ageel A.M., al-Yahya M.A., Mossa J.S., al-Said M.S. Anti-inflammatory activity of Teucrium polium. Int. J. Tissue React. 1989;11:185–188. [PubMed] [Google Scholar]
- Tomczyk, A., Szymanska, M., 1995. Possibility of reducing spider mite populations by spraying with selected plant extracts. In: Proceedings of the 35th Scientific Session IOR, Part II, vol. 35, pp. 125–128.
- Vandenborre G., Groten K., Smagghe G., Lannoo N., Baldwin I., Van Damme E. Nicotiana tabacum agglutinin is active against Lepidopteran pest insects. J. Exp. Bot. 2010;61:1003–1014. doi: 10.1093/jxb/erp365. [DOI] [PubMed] [Google Scholar]
- Vattikonda S., Amanchi N., Sangam S. Effect of costunolide a plant product of Saussurea lappa on feeding behaviour of Papilio demoleus L. (Lepidoptera: Papilionidae) Larvae. Res. J. Recent Sci. 2015;4:55–58. [Google Scholar]
- Vivekanandhan P., Venkatesan R., Ramkumar G., Karthi S., Senthil-Nathan S., Shivakumar M.S. Comparative analysis of major mosquito vectors response to seed-derived essential oil and seed pod-derived extract from Acacia nilotica. Int. J. En. Res. Pub. Heal. 2018;15:388. doi: 10.3390/ijerph15020388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahabi H.A., Alansary L.A., Al-Sabban A.H., Glasziuo P. The effectiveness of Hibiscus sabdariffa in the treatment of hypertension: a systematic review. Phytomedicine. 2010;17:83–86. doi: 10.1016/j.phymed.2009.09.002. [DOI] [PubMed] [Google Scholar]
- Zahara K., Tabassum S., Sabir S., Arshad M., Qureshi R., Amjad M., Chaudhari S. A review of therapeutic potential of Saussurea lappa: An endangered plant from Himalaya. Asian Pac. J. Trop. Med. 2014;7S1:S60–9. doi: 10.1016/S1995-7645(14)60204-2. [DOI] [PubMed] [Google Scholar]
- Žilić S., Janković M., Basić Z., Vančetović J., Maksimović V. Antioxidant activity, phenolic profile, chlorophyll and mineral matter content of corn silk (Zea mays L): comparison with medicinal herbs. J. Cereal Sci. 2016;69:363–370. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.