Abstract
This systematic review answered two questions among adults with chronic conditions: When included in the same statistical model, are Common Sense Model constructs and self-efficacy both associated with (1) self-management behaviors and (2) health outcomes? We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and included 29 articles. When included in the same statistical model, Common Sense Model constructs and self-efficacy were both correlated with outcomes. Self-efficacy was more consistently associated with self-management behaviors, and Common Sense Model constructs were more consistently associated with health outcomes. Findings support the continued inclusion and integration of both frameworks to understand and/or improve chronic illness self-management and outcomes.
Keywords: adults, chronic illness, Common Sense Model, self-efficacy, self-management
As no one theory, framework, or model can explain the complexity of human behavior, there is interest in integrating them to improve our understanding of self-management behaviors (e.g. adherence to medication, exercise, and diet regimens) and health outcomes (e.g. quality of life, pain, and disability). Integrating theoretical frameworks could also improve our understanding of the effectiveness of behavioral interventions by identifying potential treatment targets. However, if frameworks are redundant, integration can unnecessarily complicate our understanding of phenomena and “threaten the scientific principle of parsimony” (Birken et al., 2017: 2).
Over a decade ago, Lau-Walker (2006) proposed the integration of the Common Sense Model of Self-Regulation and the self-efficacy framework, which have separately guided behavioral health research for years (Bandura, 1997; Bandura and Locke, 2003; Leventhal et al., 1980, 2003, 2011). She noted that the Common Sense Model describes the general effects of information gained prior to illnesses on health behaviors, whereas self-efficacy focuses on the effects of specific experiences on enacting specific health behaviors. Lau-Walker also noted several commonalities between the Common Sense Model and self-efficacy, including a focus on the importance of individual experience as opposed to personality. She concluded that through their integration, researchers and clinicians could address patients’ initial conceptions of illness (via the Common Sense Model) as well as patients’ confidence in their ability to adopt and maintain health behaviors (via self-efficacy) resulting in better, more individualized interventions that address the varied needs of patients, including the effects of an illness on a person’s lifestyle, required behavioral changes, and how to sustain those changes.
The Common Sense Model: health beliefs and behaviors in daily life
The Common Sense Model emerged from research examining the effect of fear on health behaviors. Leventhal et al. found that neither a threat message nor an action plan alone were sufficient to lead to health behavior change, but that they did motivate health behavior change when combined (Leventhal, 1971; Leventhal et al., 1965; Leventhal and Trembly, 1968). Subsequent studies found that individuals form cognitive representations, termed illness representations, based on their perceptions and beliefs about health threats (i.e. illnesses). These multi-level illness representations include both concrete “perceptual” experiences (e.g. symptoms and functional changes) and abstract concepts and labels (e.g. hypertension; Baumann and Leventhal, 1985; Meyer et al., 1985). When combined with action plans, illness representations direct decisions and behaviors related to threat management (i.e. self-management).
Most research on the Common Sense Model focuses on these illness representations. Indeed, conceptualizing illness representations as combining perceptions and abstract concepts sets the Common Sense Model apart from other health belief frameworks, which tend to focus only on the abstract (Leventhal et al., 2016). Illness representations are generally classified into five content areas: identity (e.g. symptoms, illness’ name), timeline (e.g. expected and experienced duration, perceived rate of onset), control/cure (e.g. whether the condition can be controlled/cured), cause (e.g. contact with a causal agent), and consequence (e.g. disruption of ongoing activities, prognosis). While not the focus of this review, the Common Sense Model also describes treatment representations, which are formed using the same five content areas. (See Leventhal et al. (2016) for a thorough description of all facets of the Common Sense Model.)
The Common Sense Model proposes a dynamic interplay between illness representations, self-management, and health outcomes. For example, imagine a person with head pain. If they identify that health threat as an acute headache without serious consequences, they are likely to manage the pain with something simple, like ibuprofen. If the ibuprofen reduces the pain, it confirms their illness representation of the headache as an acute, inconsequential problem. As a result, they are likely to repeat the same set of behaviors the next time they identify head pain as an acute headache. However, if the ibuprofen fails to reduce the pain, their model of illness and management becomes incoherent. To regain coherence, their illness representation may change, for example, they may identify the pain as an aneurysm: an acute problem with serious consequences. As a result, they will now manage the health threat with a more serious treatment, such as a visit to the emergency room. The emergency room visit then serves as the opening phase of a series of treatments and experiences that will define the consequences and ultimate control of the condition.
There is strong evidence, from cross-sectional and longitudinal studies, systematic reviews, and meta-analyses, that illness representations are correlated with a variety of physical and mental health outcomes, including physical functioning, emotional well-being, and adherence to self-management behaviors (Baines and Wittkowski, 2013; Broadbent et al., 2011; Hagger et al., 2017; Hagger and Orbell, 2003; Kaptein et al., 2008). At the same time, effect sizes for these associations tend to be small to moderate (Hagger et al., 2017; McAndrew et al., 2018). One reason for the small effect sizes may be that while the Common Sense Model can explain the choice of a self-management behavior, the choice does not always result in actual behavior (Webb and Sheeran, 2006).
Self-efficacy: a general approach to motivated behavior
Self-efficacy (Bandura, 1997), or belief in one’s ability to enact specific behaviors in specific situations, has been suggested as a natural corollary to the Common Sense Model and as a way to explain additional variance in self-management behaviors (Lau-Walker, 2006; Leventhal and Cameron, 1987). Self-efficacy theory was developed as part of Social Cognitive Theory (Bandura, 1997) but is also a framework in its own right (Lau-Walker, 2006). The framework suggests that four types of mastery experiences provide the basis for judgments about self-efficacy (Bandura, 1997). Enactive experiences involve actively participating in a task and are the most influential. Vicarious experiences involve watching and/or comparing one’s performance on a task to another’s performance on a task. Vicarious mastery experiences are particularly powerful in the early phases of learning and/or when one perceives the person performing the task and the situation in which the task is performed as similar to one’s own. The efficacy of the third type of mastery experience, verbal persuasion, depends on the credibility of the source. Finally, physical and emotional states can affect how individuals interpret task performance and therefore affect self-efficacy.
The self-efficacy framework also suggests that perceived self-efficacy affects behavior by influencing cognitive processes (e.g. planning for the future), motivational processes (e.g. improved commitment to goals), and regulating potentially disruptive affective processes (e.g. fear of failure). Given the dynamic nature of self-efficacy, efforts at mastery can increase or decrease self-efficacy. For example, if a person feels confident in their ability to engage in exercise (i.e. they have high self-efficacy), attending an exercise class is an enactive mastery experience that can lead to stable and/or increased self-efficacy if participation was easy or decreased self-efficacy if participation was difficult. Therefore, it is not only the behavior that affects self-efficacy but also the outcome of the behavior.
While the self-efficacy framework was not developed specifically to describe health behaviors, cross-sectional studies, longitudinal studies, and systematic reviews suggest that higher levels of self-efficacy are associated with engaging in health behaviors, such as care after stroke (Jones and Riazi, 2011), smoking cessation (Villanti et al., 2010), physical activity in older adults (Schepens et al., 2012), and adherence to diabetes self-management regimens (Gherman et al., 2011). Furthermore, a review of literature found that increasing self-efficacy can lead to beneficial changes in health behaviors (Sheeran et al., 2016), for example, through cognitive behavioral techniques such as goal setting and self-monitoring (Nezami et al., 2016).
Complementary differences and overlap
As noted by Lau-Walker (2006), the Common Sense Model and self-efficacy have complementary differences that support their integration. The Common Sense Model focuses on how illness beliefs guide the selection of self-management behaviors, particularly via interpretations of illness and health outcomes. That is, how the experience of a set of symptoms coalesces into illness representations and action plans for self-management. The self-efficacy framework emphasizes how beliefs about self-management behaviors guide self-management, which then affect health outcomes. For example, how confidence in being able to adhere to medication affects the likelihood of taking that medication. As suggested by Lau-Walker (2006), understanding these varied inputs could improve our understanding of self-management behaviors and our ability to intervene to affect health outcomes through self-management behaviors.
At the same time, at least some Common Sense Model constructs overlap with the self-efficacy framework. Previous research has found a small to moderate, positive correlation between self-efficacy and the Common Sense Model’s control/cure domain (Bonsaksen et al., 2013; Griva et al., 2000) and a smaller positive correlation between self-efficacy and the timeline domain (Lau-Walker, 2004). There are also conceptual similarities. Both frameworks put a primary focus on an individual’s experiences and perceptions and suggest that personal experiences are unlikely to affect beliefs and behaviors unless understood and framed within cognitive schemas. Therefore, while the conceptual case for combining the Common Sense Model and self-efficacy is undoubtedly strong, given these similarities, one cannot assume that constructs from both frameworks will explain variance in outcomes when included in the same statistical models.
The present review
Given their complementary differences and overlap, recommendations for their integration, and the rapid increase in studies applying both the Common Sense Model and self-efficacy framework (see Supplementary Material 1), our goal was to answer two questions—When included in the same model, are Common Sense Model constructs and self-efficacy both associated with (1) self-management behaviors and (2) health outcomes? To answer these questions, we reviewed studies seeking to understand behaviors and outcomes of patients with chronic health conditions. Assessing the simultaneous contributions of these frameworks is necessary to advance theory, guide integration efforts, provide a broader perspective on how the frameworks can be used to facilitate health behaviors, and to inform the parsimonious design and analysis of behavioral health research.
Methods
We followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for systematic reviews (Moher et al., 2009) to answer two questions among people with chronic conditions—When included in the same model, are Common Sense Model constructs and self-efficacy both associated with (1) self-management behaviors and (2) health outcomes? For this review, the Common Sense Model was represented by measures of illness representations. Self-efficacy measures had to be related to self-management of the specific condition under study (e.g. diabetes self-management self-efficacy) or specific behaviors (e.g. exercise self-efficacy). Studies were eligible if they were published in English in a peer-reviewed journal and included measures of both Common Sense Model constructs and self-efficacy in at least one statistical model related to chronic illness self-management behaviors or health outcomes. Participants had to have a chronic condition. Any study design and length of follow-up was acceptable. Our focus was on studies aiming to understand/predict behavior (there were not enough studies to examine changes in behavior). Given our interest in understanding whether the constructs were statistically significant correlates in the same statistical model (i.e. coefficients in multivariable analyses), our approach prohibited meta-analysis, which relies on coefficients from bivariate correlations and cannot be completed with regression coefficients. Protocol is available at: https://www.mcandrewhealthlab.com/.
To obtain generalizable information, we excluded articles that used general self-efficacy measures, review articles, studies with pediatric populations, studies reporting on qualitative work, studies that were not described as testing Common Sense Model constructs or self-efficacy, studies that did not provide sufficient information on whether the measures of interest were simultaneously included in statistical models, and studies in which statistical models/outcomes were not clearly defined. We also excluded studies that reported on the same outcome at the same timepoint using the same cohort as another study (e.g. longitudinal studies reporting on the same timepoint).
On 23 June 2017, we searched PubMed, MEDLINE, PsycINFO, CINAHL, and Web of Science using the following search terms (based on PubMed search): ((((“social cognitive theory”) OR “self efficacy”) OR “self-efficacy”)) AND (((((“common sense model”) OR “illness perception*”) OR “illness representation*”) OR “illness belief*”) OR “treatment representation*”). We included “treatment representation” to ensure we did not miss relevant articles but did not assess treatment representations in this review. Search entries for each database are available in Supplementary Material 2.
After obtaining records from each database, we combined results in a reference manager (EndNote) to remove duplicates. Next, two authors separately reviewed half of the abstracts to exclude articles based on the criteria listed above. Those authors then downloaded full-text articles for the remaining abstracts and reviewed roughly 30 percent together to refine the exclusion process. Once 80-percent agreement on exclusion was reached, the authors separately reviewed the remaining full-text articles to determine the final list of included papers. A third author offered statistical consultation, and all three authors discussed articles about which any author felt unsure.
After compiling a final list of included articles, two authors entered the following information into an excel spreadsheet: first author, date, location, setting, sample size, gender distribution, race/ethnicity distribution, study design, setting, patient population, type of analysis, Common Sense Model measure, self-efficacy measure, self-management behavior(s), health outcome(s), variables included in final analyses, and a qualitative description of findings. In addition, the authors determined the primary summary measure, that is, whether self-management behaviors and/or health outcomes were associated with (1) both Common Sense Model constructs and self-efficacy; (2) Common Sense Model constructs, but not self-efficacy; (3) Self-efficacy, but not Common Sense Model constructs; or (4) neither Common Sense Model constructs nor self-efficacy. We then separated findings based on outcome (i.e. self-management behaviors and health outcomes) and study design. We included results from any statistical model that provided the simultaneous direct effects of at least one Common Sense Model construct and self-efficacy.
During data abstraction, each of the two authors did primary data extraction for half the articles and then validated extraction for the other half of the articles. Finally, all three authors reviewed summary tables separately and together to narratively describe and synthesize results. We collected information on the effects of Common Sense Model constructs and self-efficacy when they were included in the same model and most models included many other factors (e.g. demographic characteristics, other psychological constructs). Therefore, we do not report effect sizes as they would be difficult to compare across models with different covariates and outcomes. Consistent with other work, effect sizes were generally small to moderate (Hagger et al., 2017; McAndrew et al., 2018). We used the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (National Institutes of Health, 2014) to assess study quality as “good,” “fair,” or “poor.” We updated this search on 10 April 2019, using the same methods, but limiting the search to our prior search date (Supplementary Material 2).
Results
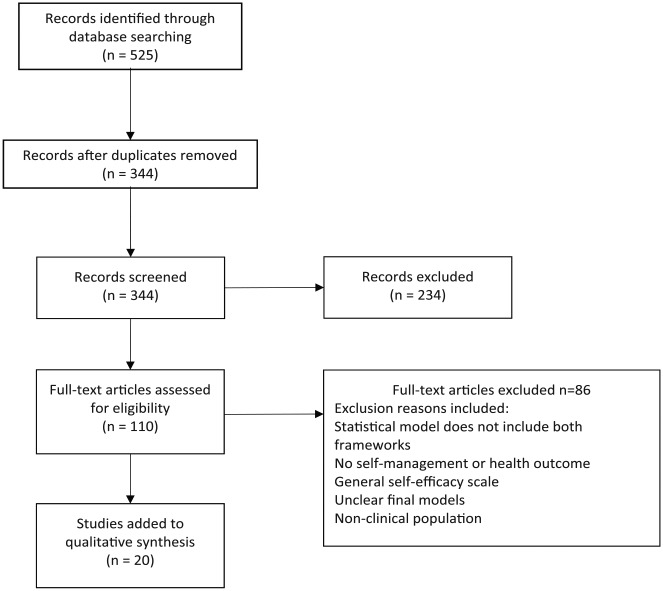
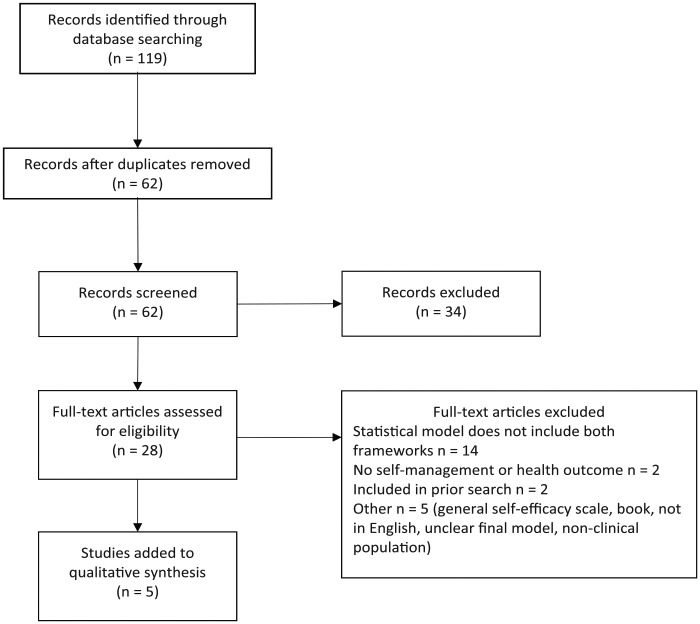
The initial search resulted in 525 abstracts (Figure 1). We excluded 181 duplicates and reviewed the remaining 344 abstracts, excluding an additional 234 because they did not meet inclusion criteria. Next, we reviewed 110 full-text articles, which resulted in 24 articles meeting inclusion criteria. The updated search resulted in five additional articles (after reviewing 119 abstracts, excluding 57 duplicates, and reviewing 28 full-text articles (Figure 2)). The final 29 articles (Supplementary Material 1) reported results of 55 statistical models that included both a measure of the Common Sense Model and self-efficacy (i.e. many articles reported multiple models). Also of note, the 29 included articles represented 25 studies as the following groups of articles reported on different outcomes among the same participant cohorts: (1) Foster et al. (2010) and Campbell et al. (2013); (2) Gandy et al. (2013, 2015); and (3) Steca et al. (2013: a), Greco et al. (2014, 2015).
Figure 1.
Flowchart for search completed on 23 June 2017.
Figure 2.
Flowchart for search completed on 10 April 2019.
The 25 studies included participants with a range of conditions, including cardiovascular diseases, diabetes, cancer, arthritis, and low back pain (Table 1). Most articles had cross-sectional designs (n = 17), 10 were longitudinal, and 2 used data from randomized controlled trials. Few articles reported race/ethnicity. Roughly 79 percent of the articles were published within 7 years of the search. The quality of most studies was rated “good” or “fair” due to their cross-sectional or observational nature. Only five articles reported power calculations, with just one of those reporting standardized point estimates, and there was often an absence of information on participation rates among eligible persons.
Table 1.
Characteristics of included articles.
| First author (year) | Country | Study design | Disease population | N | Percent women | Race/ethnicity | Recruitment setting |
|---|---|---|---|---|---|---|---|
| Al-Noumani (2017) | Oman | Cross-sectional | Hypertension | 45 | 64% | NR | Primary care |
| #Bishop (2015) | UK | Prospective longitudinal observational cohort | Low back pain | BL: 485 1+ FU: 420 |
69% | NR | Acupuncture clinic |
| * Campbell (2013) | England | Prospective cohort | Low back pain | BL: 1591 6M FU: 810 5Y FU: 488 |
62% | NR | Primary care |
| Chou (2019) | China | Cross-sectional | Breast & colon cancer | Breast cancer: 105 Colon cancer: 54 |
83% | 100% Chinese | Infusion unit and inpatient cancer unit |
| #Ford (2012) | UK | Cross-sectional | Celiac disease | 284 | 80% | 95% White British | Celiac UK |
| * Foster (2010) | England | Prospective cohort | Low back pain | BL: 1591 6M FU: 810 |
59% | NR | Primary care |
| * Gandy (2015) | Australia | Cross-sectional | Epilepsy | 122 | NR | NR | Tertiary epilepsy center |
| * Gandy (2013) | Australia | Cross-sectional | Epilepsy | 123 | 60% | NR | Tertiary epilepsy center |
| #Glattacker (2018) | Germany | Prospective | Chronic low back pain | BL: 214 End of rehab: 203 6M: 152 |
53% | NR | Rehab for musculoskeletal disease |
| * Greco (2014, 2015) | Italy | Prospective | Cardiovascular disease | 75 | 20% | NR | Cardiovascular rehab unit |
| #Green (2014) | Australia | Cross-sectional | Prostate or breast cancer | Breast cancer: 145 Prostate cancer: 92 |
Breast cancer: 100% Prostate cancer: 0% |
NR | NR |
| #Houle (2016) | Canada | Cross-sectional | Type 2 diabetes | 284 | 49% | NR | Diabetes education course at hospital or social service center |
| #Johansson (2018) | Sweden | Prospective observational | Colorectal cancer | 39 | 41% | NR | Surgical unit at county hospital |
| #Knowles (2017) | Australia | Cross-sectional | Fecal ostomy | 150 | 64% | 60% European background | Online links on ostomy-related websites |
| #Knowles (2016) | Australia | Cross-sectional | End-stage osteoarthritis | 120 | 72% | 74% Caucasian | Orthopedic clinic |
| #La (2016) | South Korea | Cross-sectional | Multiple myeloma | 102 dyads | 46% | NR | Outpatient cancer center |
| #Mann (2009) | USA | Cross-sectional | Type 2 diabetes | 151 | 68% | 58% Latino 34% Black |
Outpatient general internal medicine clinic |
| #Massey (2015) | The Netherlands | Prospective | Kidney transplant patients | BL: 113 6M FU: 106 18M FU: 84 |
35% | 84% Dutch 16% non-Dutch |
Kidney transplant clinic |
| #Meinema (2015) | The Netherlands | Secondary analysis of cluster RCT | Hypertension | 139 | 52% | Surinamese & Ghanaian | Primary healthcare centers |
| #Platt (2014) | Australia | Cross-sectional | Coronary heart disease | 142 | 30% | NR | Outpatient clinic |
| #*Steca (2013a) | Italy | Cross-sectional | Cardiovascular disease | 116 | 21% | NR | Hospital |
| Steca (2013) | Italy | Cross-sectional | Cardiovascular disease | 172 | 24% | NR | Hospital |
| #Tahmasebi (2015) | Iran | Cross-sectional | Diabetes | 396 | 74% | NR | Outpatient endocrinology unit |
| #Theunissen (2003) | The Netherlands | RCT | Hypertension | 108 | 59% | NR | Primary care |
| #Treharne (2008) | UK | Longitudinal | Rheumatoid arthritis | BL: 154 FU: 114 |
74% | 100% White | Outpatient clinic |
| #Treharne (2007) | UK | Longitudinal | Rheumatoid arthritis | 129 | 75% | 100% White | Outpatient and inpatient clinics |
| #Unni (2011) | USA | Cross-sectional | High cholesterol and/or asthma | Total: 840 Cholesterol rx: 240 Asthma rx: 399 |
Cholesterol rx: 46% Asthma rx: 61% |
Cholesterol: 86% White Asthma: 81% White | Internet survey panel |
| #Zelber-Sagi (2017) | Israel | Cross-sectional | Non-alcoholic fatty liver disease | 146 | 53% | NR | Fatty liver clinic |
NR: not reported; UK: United Kingdom; BL: baseline; FU: follow-up; Y: year; M: month; rehab: rehabilitation; USA: United States of America; RCT: randomized controlled trial; rx: medication.
Race/ethnicity and setting reported as described in article. Articles marked with * are groups of articles reporting on different outcomes among the same studies: (1) Foster et al. (2010) and Campbell et al. (2013); (2) Gandy et al. (2013, 2015); and (3) Greco et al. (2014, 2015) and Steca et al. (2013). #All references are provided in Supplement 1.
Models of self-management behaviors, such as medication adherence, exercise, and diet, were tested in 15 studies. Correlates of health outcomes, such as quality of life, disability, and pain, were tested in 17 studies. Almost all studies of self-management behaviors were based in primary care, and most studies of health outcomes were based in specialty settings (Tables 2 and 3). In many cases, Common Sense Model constructs and self-efficacy were significant and simultaneous correlates of self-management behaviors and health outcomes. However, as can be seen in Tables 2 and 4, self-efficacy was a more consistent correlate of self-management behaviors. Alternatively, as can be seen in Tables 3 and 4, the Common Sense Model emerged as a more consistent correlate of health outcomes.
Table 2.
Correlations among Common Sense Model constructs, self-efficacy, and self-management behaviors.
| First author (year) | Self-management behavior | CSM as correlate | Self-efficacy as correlate | Study design | Analysis | Setting |
|---|---|---|---|---|---|---|
| Exercise-related | ||||||
| #Green (2014) | Adherence | ° | • | Cross-sectional | Multiple regression | NR |
| Exercise change after cancer diagnosis | • | ° | Cross-sectional | Multiple regression | NR | |
| #Platt (2014) | Adherence | ° | ° | Cross-sectional | Hierarchical multiple regression | Primary care |
| Diet-related | ||||||
| #Green (2014) | Adherence | ° | • | Cross-sectional | Multiple regression | NR |
| Diet change after cancer diagnosis | • | ° | Cross-sectional | Multiple regression | NR | |
| #Ford (2012) | Adherence to a gluten-free diet | • | ° | Cross-sectional | Logistic regression | Other |
| #Platt (2014) | Adherence | • | • | Cross-sectional | Hierarchical multiple regression | Primary care |
| #Zelber-Sagi (2017) | Nutrition habits | • | • | Cross-sectional | Path analysis | Specialty |
| Medication-related | ||||||
| Al-Noumani (2017) | Adherence | ° | • | Cross-sectional | Multiple linear regression | Primary care |
| #Mann (2009) | Adherence | • | • | Cross-sectional | Multivariable logistic regression | Primary care |
| #Massey (2015) | Adherence | ° | ° | Prospective | Multilevel linear regression | Specialty |
| #Meinema (2015) | Baseline adherence | ° | • | Secondary analysis of cluster RCT | Multivariate logistic regression | Primary care |
| Change in CSM or self-efficacy on adherence at 6M | ° | • | Multivariate logistic regression | Primary care | ||
| #Platt (2014) | Adherence | • | • | Cross-sectional | Hierarchical multiple regression | Primary care |
| #Theunissen (2003) | Adherence | ° | • | RCT | Multivariate analysis of variance for general linear modeling | Primary care |
| #Unni (2011) | Adherence to cholesterol medication due to | Cross-sectional | Regression | Other | ||
| Multiple medication issues | • | • | Cross-sectional | Regression | Other | |
| Managing issues | ° | • | Cross-sectional | Regression | Other | |
| Forgetfulness | ° | • | Cross-sectional | Regression | Other | |
| Medication belief issues | ° | • | Cross-sectional | Regression | Other | |
| Adherence to asthma medication due to | Cross-sectional | Regression | Other | |||
| Managing and availability issues | ° | • | Cross-sectional | Regression | Other | |
| Forgetfulness | ° | • | Cross-sectional | Regression | Other | |
| Beliefs and convenience issues | ° | • | Cross-sectional | Regression | Other | |
| Cost issues | • | • | Cross-sectional | Regression | Other | |
| Other | ||||||
| #Tahmasebi (2015) | Diabetes self-management behaviors | • | ° | Cross-sectional | Path analysis | Specialty |
| #Theunissen (2003) | Lifestyle adherence | ° | • | RCT | Multivariate analysis of variance for general linear modeling | Primary care |
CSM: Common Sense Model; NR: not reported; RCT: randomized controlled trial; M: month.
•Denotes significant correlate; °denotes not significant correlate. Other indicates settings other than primary care or specialty settings, and specific information is supplied in Table 1. Statistical models and study design are described as written in the article. #All references are provided in Supplement 1.
Table 3.
Correlations among Common Sense Model constructs, self-efficacy, and health outcomes.
| First author (year) | Health outcome | CSM as correlate | Self-efficacy as correlate | Study design | Statistical model | Setting |
|---|---|---|---|---|---|---|
| Symptom-related | ||||||
| #Bishop (2015) | Pain related disability over time | • | • | Prospective longitudinal observational cohort | Longitudinal multilevel linear regression | Specialty |
| * Campbell (2013) | Pain grade at 6M FU | • | ° | Prospective cohort | Multivariable linear regression | Primary care |
| Pain grade at 5Y FU | • | ° | Cross-sectional | Multivariable linear regression | Primary care | |
| * Foster (2010) | Pain related disability at 6M | • | • | Prospective cohort | Multistage linear regression | Primary care |
| * Gandy (2013) | Depressive disorder | • | ° | Cross-sectional | Multivariate logistic regression | Specialty |
| Suicide risk | • | ° | Cross-sectional | Multivariate logistic regression | Specialty | |
| * Gandy (2015) | Meeting anxiety disorder criteria | ° | ° | Cross-sectional | Logistic regression | Specialty |
| #Glattacker (2018) | Disability at the end of cardiac rehabilitation | ° | ° | Prospective | Multivariate regression | Specialty |
| * Greco (2014) | Depression at cardiovascular rehabilitation BL | • | • | Prospective | Path analysis | Specialty |
| Depression at 2M FU | • | • | Prospective | Path analysis | Specialty | |
| #Knowles (2016) | Psychological distress | • | • | Cross-sectional | SEM | Other |
| #Knowles (2017) | Depression | • | • | Cross-sectional | SEM | Specialty |
| Steca (2013) | Depression | • | ° | Cross-sectional | Path analysis | Specialty |
| #Treharne (2007) | Change in sleep disruption | ° | ° | Longitudinal | Linear regression | Specialty |
| #Treharne (2008) | Fatigue at 1Y | • | ° | Longitudinal | Hierarchical linear regression | Primary care |
| Quality of life/satisfaction | ||||||
| * Greco (2015) | Health satisfaction at cardiovascular rehabilitation BL | • | ° | Prospective | Path analysis | Specialty |
| Health satisfaction at 2M FU | • | • | Prospective | Path analysis | Specialty | |
| #La (2016) | Physical health–related quality of life | • | • | Cross-sectional | SEM | Specialty |
| Mental health–related quality of life | • | • | Cross-sectional | SEM | Specialty | |
| Steca (2013) | Health satisfaction | • | ° | Cross-sectional | Path analysis | Specialty |
| Life satisfaction | • | • | Cross-sectional | Path analysis | Specialty | |
| #*Steca (2013a) | Health satisfaction | • | ° | Cross-sectional | Path analysis | Specialty |
| Life satisfaction | ° | • | Cross-sectional | Path analysis | Specialty | |
| Chou (2019) | Multidimensional quality of life | • | ° | Cross-sectional | Heretical regression | Specialty |
| #Johannsson (2018 | Health-related quality of life | • | ° | Prospective observational | Path analysis | Specialty |
| #Glattacker (2018) | Physical health quality of life at the end of cardiac rehabilitation | ° | ° | Prospective | Multivariate regression | Specialty |
| Physical health quality of life 6M after cardiac rehabilitation | ° | • | Prospective | Multivariate regression | Specialty | |
| Mental health quality of life 6M after cardiac rehabilitation | ° | ° | Prospective | Multivariate regression | Specialty | |
| Hemoglobin A1c | ||||||
| #Houle (2016) | Mediation of living in poverty on hemoglobin A1c | • | ° | Cross-sectional | Bootstrapped regression | Specialty |
| Mediation of education level on hemoglobin A1c | ° | ° | Cross-sectional | Bootstrapped regression | Specialty | |
CSM: Common Sense Model; M: month; FU: follow-up; Y: year; BL: baseline; SEM: structural equation modeling.
•Denotes significant correlate; °denotes not significant correlate.
Articles marked with * are groups of articles reporting on different outcomes among the same study: (1) Foster et al. (2010) and Campbell et al. (2013); (2) Gandy et al. (2013, 2015); and (3) Greco et al. (2014, 2015) and Steca et al. (2013). Statistical models and study design are described as written in the article. Other indicates settings other than primary care or specialty settings, and specific information is supplied in Table 1. #All references are provided in Supplement 1.
Table 4.
Proportion of statistical models finding both Common Sense Model constructs and self-efficacy, only Common Sense Model constructs, only self-efficacy, or neither was correlated with self-management behavior or health outcomes.
| Self-management behavior |
Health outcome |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Exercise | Diet | Medication adherence | Other behaviors | Total | Symptoms | Quality of life/satisfaction | A1c | Total | |
| Total no. of studies | 2 | 4 | 7 | 2 | 15 | 10 | 6 | 1 | 17 |
| Total no. of articles | 2 | 4 | 7 | 2 | 15 | 12 | 7 | 1 | 20 |
| Total no. of models | 3 | 5 | 15 | 2 | 25 | 15 | 13 | 2 | 30 |
| Significant predictors | |||||||||
| Both (%) | 0 | 40 | 27 | 0 | 24 | 40 | 31 | 0 | 33 |
| CSM only (%) | 33 | 40 | 0 | 50 | 16 | 40 | 38 | 50 | 40 |
| Self-efficacy only (%) | 33 | 20 | 67 | 50 | 52 | 0 | 15 | 0 | 7 |
| Neither (%) | 33 | 0 | 7 | 0 | 8 | 20 | 15 | 50 | 20 |
CSM: Common Sense Model
Both refers to both Common Sense Model constructs and self-efficacy.
Self-management behaviors
The studies assessing correlates of self-management behaviors included at least one of the following outcomes: medication adherence (n = 15 models, n =7 articles), dietary adherence (n = 5 models, n = 4 articles), exercise adherence (n = 3 models, n = 2 articles), and diabetes self-management (n = 2 models, n = 2 articles; Table 2). These studies included data on a total of 25 statistical models. Of these models, 20 were based on cross-sectional designs, 2 were from the same randomized control trial, 2 were from the same secondary analysis of a cluster randomized control trial, and 1 was based on data from a prospective design. Patterns were similar across different sample sizes and length of follow-up.
Among the 20 cross-sectional models, 45 percent of the statistical models found self-efficacy, but not Common Sense Model constructs correlated with self-management behaviors, 30 percent found that both frameworks were correlated with self-management behaviors, 20 percent found that only Common Sense Model constructs were correlated with self-management behaviors, and 5 percent (one study) found that neither framework was correlated with self-management behaviors. All four models based on randomized control trial data found that only self-efficacy was associated with self-management behaviors. The prospective study found that neither framework was associated with self-management behaviors.
Health outcomes
The studies testing correlates of health outcomes assessed symptoms (n = 15 models, n = 12 articles), quality of life and/or health satisfaction (n = 13 models, n = 7 articles), and hemoglobin A1c (n = 2 models, n = 1 article; Table 3). Patterns were similar across sample sizes, length of follow-up, and study design. Of the 15 statistical models based on data from cross-sectional designs, 47 percent found that Common Sense Model constructs, but not self-efficacy, were correlated with health outcomes, 33 percent found that both frameworks were correlated with health outcomes, 13 percent found that neither framework was associated with health outcomes, and 7 percent found that self-efficacy, but not Common Sense Model constructs, was correlated with health outcomes. Of the 15 statistical models based on data from prospective designs, 33 percent found that Common Sense Model constructs, but not self-efficacy, were correlated with health outcomes, 33 percent found that both frameworks were correlated with health outcomes, 27 percent found that neither framework was associated with health outcomes, and 7 percent found that self-efficacy, but not Common Sense Model constructs, was correlated with health outcomes.
Discussion
This review demonstrates an increasing interest in understanding the relative effects of the Common Sense Model and the self-efficacy framework, with 79 percent of papers published within 7 years of the search. When included in the same statistical model, constructs from both the Common Sense Model and self-efficacy were unique correlates of chronic illness self-management behaviors and health outcomes. Self-efficacy was more consistently linked with self-management behaviors (76% of models for self-efficacy vs 40% for the Common Sense Model), particularly with regard to medication adherence, which was the most commonly assessed behavior. The Common Sense Model had more consistent associations with overall health outcomes (73% of models for the Common Sense Model vs 40% for self-efficacy), particularly for quality of life. The results offer empirical support for the simultaneous inclusion of Common Sense Model constructs and self-efficacy in statistical models.
The theoretical basis of the Common Sense Model provides one possible explanation for why its constructs were more consistently linked with health outcomes than self-management behaviors. The Common Sense Model suggests that illness representations are based on perceptions (e.g. pain, fatigue) and abstract concepts (e.g. labeling a group of symptoms arthritis). Therefore, illness representations, as opposed to self-efficacy, may be more likely to conceptually map onto many patient-reported health outcomes, which are also based on perceptions (e.g. pain or fatigue preventing daily activity) and abstract concepts (e.g. general beliefs about pain or fatigue levels among peers). It is also possible that illness representations influence health indirectly through increasing or decreasing emotional distress, optimism, and other factors that are known to influence quality of life. This match between latent constructs may be missing with regard to associations between Common Sense Model constructs and self-management behaviors, as measures of the latter tend to focus on concrete behaviors as opposed to abstract beliefs. Therefore, while our results suggest that illness representations are related to self-management behaviors, it is not necessarily surprising that they had a less consistent relationship with self-management behaviors than self-efficacy.
Indeed, the self-efficacy framework puts a primacy on specific behaviors. As a result, there was more often an unambiguous link between the measurement of self-efficacy for a self-management behavior (e.g. exercise self-efficacy) and patient-reported self-management behaviors (e.g. adherence to exercise recommendations). Given that chronic illness self-management often requires many different behaviors, most studies in this review included self-efficacy measures that encompassed many types of behaviors (e.g. diabetes self-management self-efficacy). Studies that included multiple behavior-specific self-efficacy measures (e.g. exercise self-efficacy and diet self-efficacy) were more likely find a significant relationship between self-efficacy and self-management behaviors. It is possible that these designs more accurately capture the true nature of the association between self-efficacy and corresponding self-management behaviors.
Our results offer further support for the theoretical integration of the Common Sense Model and self-efficacy frameworks because they provide different, but complementary information. At the same time, past work has found statistically significant correlations between the control domain of the Common Sense Model and self-efficacy (Bonsaksen et al., 2013; Griva et al., 2000). One interpretation of these findings is that self-efficacy and the control domain assess the same underlying construct. While not the focus of this review, the incuded studies suggest that this is not always the case. Chou (2019) found that the control domain, but not self-efficacy, significantly affected quality of life (the two frameworks were added in separate steps), whereas Foster et al. (2010) found that both self-efficacy and control were associated with pain-related disability.
Finally, our results highlight the complexity inherent in understanding, predicting, and affecting human thoughts and behaviors. An illustrative example is provided by the longitudinal work presented in two studies from a single cohort of patients with low back pain (Campbell et al., 2013; Foster et al., 2010). These studies had the largest sample sizes of included work. The first tested 20 psychological predictors including factors related to the Common Sense Model, self-efficacy, depression and anxiety, coping, and fear avoidance (Foster et al., 2010). Common Sense Model constructs (personal control, acute/chronic timeline, and illness identity) and self-efficacy were the only psychological variables to predict disability over 6 months in the final model (Foster et al., 2010). Conversely, a second study of the same cohort over a different time frame found Common Sense Model constructs, but not self-efficacy, predicted pain over 5 years (Campbell et al., 2013), suggesting the explanatory power of the theories may differ depending on time frames and outcomes of interest.
Clinical implications
Our finding that the two frameworks offer unique and complementary information suggests there is value in developing and testing interventions based on both frameworks. Specifically, we propose that illness representations provide a way to tailor mastery experiences to ensure they are sufficiently specific to enhance self-efficacy and subsequently encourage behaviors to improve health. Chronic illness self-management behaviors are complex, which can make it difficult for individuals to understand how specific self-management experiences relate to future self-management and medical outcomes (Bandura, 1997). Because mastery experiences motivate both effective and ineffective behaviors, maladaptive illness representations can lead patients to engage in ineffective self-management behaviors that increase self-efficacy but do not improve health. For instance, individuals who believe they have asthma only when they have symptoms (i.e. a maladaptive illness representation) are less likely to adhere to maintenance medications (Kaptein et al., 2008). Connecting mastery experiences to existing illness and treatment representations may clarify the value and effectiveness of specific behaviors. For example, in the case of diabetes, some individuals eschew dietary change because it results in stress and stress increases glucose levels (Breland et al., 2013). For these patients, validating illness representations (i.e. stress as a cause of the health threat of increased glucose levels) while simultaneously creating mastery experiences to demonstrate that it is possible to eat healthfully without increasing stress (e.g. by providing access to healthful food) and/or that it is possible to manage stress (e.g. deep breathing as a way to control stress) should lead to better self-efficacy, self-management, and health.
Limitations and future directions
Common limitations in the reviewed studies included cross-sectional designs, small sample sizes, and little information on statistical power and response rates among eligible persons. Structural equation modeling was quite common, but some studies failed to specify the paths that were included/excluded in final models, which restricted comparisons across studies. Comparisons were also complicated when reported estimates were not defined as either standardized or unstandardized. In addition, the included studies were generally not designed to determine whether the Common Sense Model and self-efficacy should be theoretically integrated. Therefore, while this review provides initial evidence to support the integration of the Common Sense Model and self-efficacy, the field could benefit from work designed specifically to answer questions regarding that integration. Such work can also address practical implications of integrating the two models, including increased measurement burden and greater complexity of study design and analyses, which could reduce statistical power. In addition, this future research must contend with the fact that outcomes of interest will differ depending on stakeholders and strive to consider multiples points of view (e.g. patients, providers, and payors).
Future research should also explore contextual factors that influence these relationships, such as race and/or ethnicity (which were not reported in many of the included studies). There were also few studies per disease group, and only one study assessed an objective health outcome, so we could not assess differences in findings across conditions or compare differences between objective and perceived outcomes. Given the dynamic nature of the Common Sense Model and self-efficacy, outcomes likely vary over different time points, which should be examined in future work. Furthermore, the small to medium effect sizes for Common Sense Model constructs and self-efficacy mean there are multiple other factors influencing health behaviors and health outcomes that can be explored in the future.
The almost exclusive use of the Illness Perception Questionnaires to assess the Common Sense Model is both a strength and limitation. It is a strength because it allows for potential comparisons across illness domains in the future. At the same time, Phillips et al. (2017) have persuasively argued that the Illness Perception Questionnaire is inadequate to capture the dynamic nature of the Common Sense Model, which may explain why the questionnaires are not excellent predictors of self-management behaviors. Mixed-methods research, that combines static self-report measures with dynamic, qualitative descriptions of beliefs and behaviors, could address some of these measurement problems. Ecological momentary assessment may be another useful approach as it offers a way to assess illness beliefs and behaviors in real time.
Conclusion
In studies and statistical models designed to understand self-management behaviors and health outcomes related to chronic conditions, Common Sense Model constructs and self-efficacy are both consistent correlates. The Common Sense Model may be particularly useful when trying to understand health outcomes and self-efficacy when trying to understand and/or change self-management behaviors. Our results support the inclusion of both frameworks in analyses and theoretical interpretations. The integration of the frameworks in statistical models may better explain the antecedents of self-management behaviors and health outcomes. The integration of the Common Sense Model and the self-efficacy framework in interventions and research practice could help in the design of interventions, thereby advancing theory, expanding understanding of health behaviors, identifying targets for intervention, and improving health outcomes.
Supplemental Material
Supplemental material, Supplement_1_12-6-19_FINAL_1 for Are Common Sense Model constructs and self-efficacy simultaneously correlated with self-management behaviors and health outcomes: A systematic review by Jessica Y Breland, Jessie J Wong and Lisa M McAndrew in Health Psychology Open
Supplemental material, Supplement_2_FINAL_Dec2019_FINAL for Are Common Sense Model constructs and self-efficacy simultaneously correlated with self-management behaviors and health outcomes: A systematic review by Jessica Y Breland, Jessie J Wong and Lisa M McAndrew in Health Psychology Open
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Department of Veterans Affairs (VA), Health Services Research & Development Service (CDA 15-257 to J. Breland; CDA 13-017 to L. McAndrew), the VA Office of Academic Affiliations, the VA HSR&D Advanced Fellowship Program, and for J. Breland, the Implementation Research Institute (IRI), at the George Warren Brown School of Social Work, Washington University in St Louis, through an award from the National Institute of Mental Health (5R25MH08091607) and the Department of Veterans Affairs, HSR&D, Quality Enhancement Research Initiative (QUERI).
Supplemental material: Supplemental material for this article is available online.
References
- Baines T, Wittkowski A. (2013) A systematic review of the literature exploring illness perceptions in mental health utilising the self-regulation model. Journal of Clinical Psychology in Medical Settings 20: 263–274. [DOI] [PubMed] [Google Scholar]
- Bandura A. (1997) Self-efficacy: The Exercise of Self-control. Gordonsville, VA: WH Freeman. [Google Scholar]
- Bandura A, Locke EA. (2003) Negative self-efficacy and goal effects revisited. Journal of Applied Psychology 88: 87–99. [DOI] [PubMed] [Google Scholar]
- Baumann LJ, Leventhal H. (1985) I can tell when my blood pressure is up, can’t I? Health Psychology 4: 203–218. [DOI] [PubMed] [Google Scholar]
- Birken SA, Powell BJ, Presseau J, et al. (2017) Combined use of the Consolidated Framework for Implementation Research (CFIR) and the Theoretical Domains Framework (TDF): A systematic review. Implementation science 12: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonsaksen T, Lerdal A, Fagermoen MS. (2013) Trajectories of illness perceptions in persons with chronic illness: An explorative longitudinal study. Journal of Health Psychology 20: 942–953. [DOI] [PubMed] [Google Scholar]
- Breland JY, McAndrew LM, Gross RL, et al. (2013) Challenges to healthy eating for people with diabetes in a low-income, minority neighborhood. Diabetes Care 36: 2895–2901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broadbent E, Donkin L, Stroh JC. (2011) Illness and treatment perceptions are associated with adherence to medications, diet, and exercise in diabetic patients. Diabetes Care 34: 338–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell P, Foster NE, Thomas E, et al. (2013) Prognostic indicators of low back pain in primary care: Five-year prospective study. The Journal of Pain 14: 873–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou F-Y. (2019) Cancer illness perception and self-management of Chinese patients. Asia-Pacific Journal of Oncology Nursing 6: 57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster NE, Thomas E, Bishop A, et al. (2010) Distinctiveness of psychological obstacles to recovery in low back pain patients in primary care. Pain 148: 398–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandy M, Sharpe L, Perry KN, et al. (2013) The psychosocial correlates of depressive disorders and suicide risk in people with epilepsy. Journal of Psychosomatic Research 74: 227–232. [DOI] [PubMed] [Google Scholar]
- Gandy M, Sharpe L, Perry KN, et al. (2015) Anxiety in epilepsy: A neglected disorder. Journal of Psychosomatic Research 78: 149–155. [DOI] [PubMed] [Google Scholar]
- Gherman A, Schnur J, Montgomery G, et al. (2011) How are adherent people more likely to think? A meta-analysis of health beliefs and diabetes self-care. Diabetes Educator 37: 392–408. [DOI] [PubMed] [Google Scholar]
- Greco A, Steca P, Pozzi R, et al. (2014) Predicting depression from illness severity in cardiovascular disease patients: Self-efficacy beliefs, illness perception, and perceived social support as mediators. International Journal of Behavioral Medicine 21: 221–229. [DOI] [PubMed] [Google Scholar]
- Greco A, Steca P, Pozzi R, et al. (2015) The influence of illness severity on health satisfaction in patients with cardiovascular disease: The mediating role of illness perception and self-efficacy beliefs. Behavioral Medicine 41: 9–17. [DOI] [PubMed] [Google Scholar]
- Griva K, Myers LB, Newman S. (2000) Illness perceptions and self efficacy beliefs in adolescents and young adults with insulin dependent diabetes mellitus. Psychology & Health 15: 733–750. [Google Scholar]
- Hagger MS, Orbell S. (2003) A meta-analytic review of the common-sense model of illness representations. Psychology & Health 18: 141–184. [Google Scholar]
- Hagger MS, Koch S, Chatzisarantis NLD, et al. (2017) The common sense model of self-regulation: Meta-analysis and test of a process model. Psychological Bulletin 143: 1117–1154. [DOI] [PubMed] [Google Scholar]
- Jones F, Riazi A. (2011) Self-efficacy and self-management after stroke: A systematic review. Disability and Rehabilitation 33: 797–810. [DOI] [PubMed] [Google Scholar]
- Kaptein AA, Hughes BM, Scharloo M, et al. (2008) Illness perceptions about asthma are determinants of outcome. Journal of Asthma 45: 459–464. [DOI] [PubMed] [Google Scholar]
- Lau-Walker M. (2004) Relationship between illness representation and self-efficacy. Journal of Advanced Nursing 48: 216–225. [DOI] [PubMed] [Google Scholar]
- Lau-Walker M. (2006) A conceptual care model for individualized care approach in cardiac rehabilitation—Combining both illness representation and self-efficacy. British Journal of Health Psychology 11: 103–117. [DOI] [PubMed] [Google Scholar]
- Leventhal H. (1971) Fear appeals and persuasion: The differentiation of a motivational construct. American Journal of Public Health 61: 1208–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal H, Cameron L. (1987) Behavioral theories and the problem of compliance. Patient Education and Counseling 10: 117–138. [Google Scholar]
- Leventhal H, Trembly G. (1968) Negative emotions and persuasion. Journal of Personality 36: 154–168. [Google Scholar]
- Leventhal H, Brissette I, Leventhal EA. (2003) The common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal H. (eds) The Self-regulation of Health and Illness Behaviour, vol. 1 London: Routledge, pp. 42–65. [Google Scholar]
- Leventhal H, Leventhal EA, Breland JY. (2011) Cognitive science speaks to the “common-sense” of chronic illness management. Annals of Behavioral Medicine 41: 152–163. [DOI] [PubMed] [Google Scholar]
- Leventhal H, Meyer D, Nerenz D. (1980) The common sense representation of illness danger. Contributions to Medical Psychology 2: 7–30. [Google Scholar]
- Leventhal H, Phillips LA, Burns E. (2016) The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. Journal of Behavioral Medicine 39: 935–946. [DOI] [PubMed] [Google Scholar]
- Leventhal H, Singer R, Jones S. (1965) Effects of fear and specificity of recommendation upon attitudes and behavior. Journal of Personality and Social Psychology 2: 20–29. [DOI] [PubMed] [Google Scholar]
- McAndrew LM, Martin JL, Friedlander ML, et al. (2018) The common sense of counseling psychology: Introducing the Common-Sense Model of self-regulation. Counselling Psychology Quarterly 31: 497–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer D, Leventhal H, Gutmann M. (1985) Common-sense models of illness: The example of hypertension. Health Psychology 4: 115–135. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, et al. (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health (2014) Quality assessment tool for observational cohort and cross-sectional studies. Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- Nezami BT, Lang W, Jakicic JM, et al. (2016) The effect of self-efficacy on behavior and weight in a behavioral weight-loss intervention. Health Psychology. Epub ahead of print 16 May DOI: 10.1037/hea0000378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips LA, Leventhal H, Burns EA. (2017) Choose (and use) your tools wisely: “Validated” measures and advanced analyses can provide invalid evidence for/against a theory. Journal of Behavioral Medicine 40: 373–376. [DOI] [PubMed] [Google Scholar]
- Schepens S, Sen A, Painter JA, et al. (2012) Relationship between fall-related efficacy and activity engagement in community-dwelling older adults: A meta-analytic review. American Journal of Occupational Therapy 66: 137–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeran P, Maki A, Montanaro E, et al. (2016) The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: A meta-analysis. Health Psychology 35: 1178–1188. [DOI] [PubMed] [Google Scholar]
- Steca P, Greco A, D’Addario M, et al. (2013) Relationship of illness severity with health and life satisfaction in patients with cardiovascular disease: The mediating role of self-efficacy beliefs and illness perceptions. Journal of Happiness Studies 14: 1585–1599. [Google Scholar]
- Villanti AC, McKay HS, Abrams DB, et al. (2010) Smoking-cessation interventions for U.S. young adults: A systematic review. American Journal of Preventive Medicine 39: 564–574. [DOI] [PubMed] [Google Scholar]
- Webb TL, Sheeran P. (2006) Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychological Bulletin 132: 249–268. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplement_1_12-6-19_FINAL_1 for Are Common Sense Model constructs and self-efficacy simultaneously correlated with self-management behaviors and health outcomes: A systematic review by Jessica Y Breland, Jessie J Wong and Lisa M McAndrew in Health Psychology Open
Supplemental material, Supplement_2_FINAL_Dec2019_FINAL for Are Common Sense Model constructs and self-efficacy simultaneously correlated with self-management behaviors and health outcomes: A systematic review by Jessica Y Breland, Jessie J Wong and Lisa M McAndrew in Health Psychology Open