Abstract
Introduction:
In the present era, percutaneous nephrolithotomy (PCNL) is the standard treatment for large (>2 cm) renal or staghorn renal stones. Both air and iodinated contrast has been used to opacify the pelvicalyceal system (PCS) before the dilatation of the tract. There are rare reports of air embolism following air pyelogram on mere presumptions.
Materials and Methods:
This is a prospective observational study. A total of 164 patients underwent PCNL in which air was used to opacify the PCS by placing a ureteric catheter for initial access.
Results:
None of our patients developed any complication during the procedure or in the postoperative period, which could be attributed to air embolism.
Conclusions:
The present study ascertains that using air for opacification of PCS for initial puncture access is a safe and acceptable alternative to iodinated contrast.
Keywords: Air embolism, air pyelogram, percutaneous nephrolithotomy
INTRODUCTION
Percutaneous nephrolithotomy (PCNL) was first reported in 1976.[1] In the present era, PCNL is the standard treatment for large (>2 cm) renal or staghorn stones.[2] Fluoroscopy is most commonly used to achieve initial access to the pelvicalyceal system (PCS) during PCNL.[3] Both air and iodinated contrast has been used to delineate PCS before the dilatation of the tract.[4] Using air to enhance the PCS has certain advantages such as initial filling of the posterior calyx, reduced risk of extravasation, and reduced radiation exposure.[5] However, there are reports that air embolism may take place during air pyelography.[6,7,8,9] We here report our observation using air to enhance the PCS while performing PCNL.
MATERIAL AND METHODS
This prospective observational study was conducted between June 2016 and May 2018 in our department. During this period, 164 PCNL procedures were done. In all procedures, air was used to enhance the PCS. All these procedures were done in the prone position and putting ureteric catheter beforehand in the lithotomy position using the rigid cystoscope. About 15–30 ml of room air was instilled through ureteric catheter to enhance the PCS [Figure 1]. The initial puncture was done using 18G, 15 cm two-piece needle. 0.035″ hydrophilic guidewire was passed through the lumen of the needle and parked into PCS [Figure 2]. We use Bull's eye technique to puncture the PCS. We have been using Alken telescopic dilators for the dilatation of the tract. Depending on the stone size, we dilate the tract maximum up to 30 Fr and deploy the appropriate size Amplatz sheath. At the end of the procedure, a double J stent was deployed, and percutaneous nephrostomy tube was placed routinely. More than one puncture was done only for large or staghorn stones. Duration of access was calculated from after lithotomy followed by prone positioning of the patient. Duration of radiation exposure during access was noted.
Figure 1.
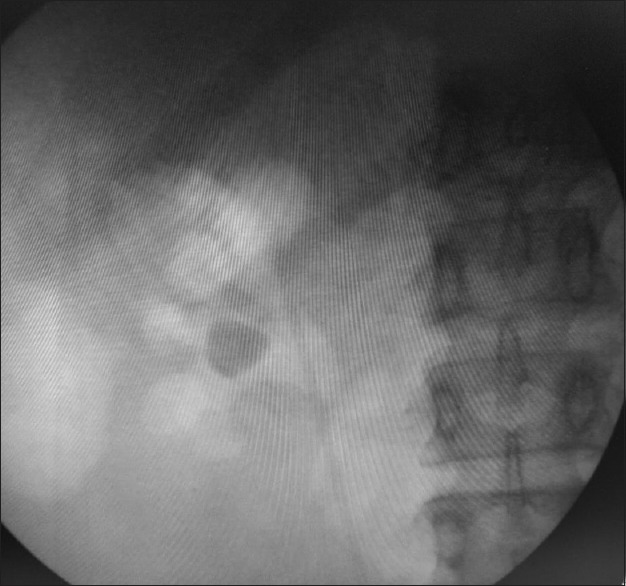
Retrograde air pyelogram using the ureteric catheter
Figure 2.
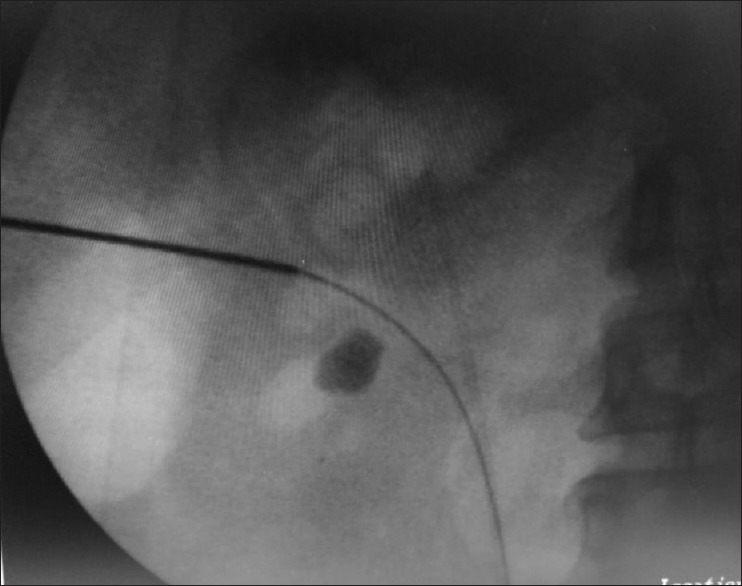
Initial access utilizing retrograde air pyelogram
RESULTS
The results are summarized in Table 1. A total of 164 patients underwent PCNL at our institute during the study. One hundred and thirteen patients were male and 97 patients had the involvement of the right kidney. Seven (4.25%) patients needed more than one tract for complete stone removal. Post-PCNL fever developed in seven (4.25%) patients. None of our patients developed anesthetic complication during surgery, and all procedures were uneventful. Postoperative blood transfusion was required in seven (4.25%) patients. Mean hospital stay was 3.04 days, with a minimum of 3 days and maximum of 4 days. Follow-up images showed residual stones in only four (2.43%) patients.
Table 1.
Results
| Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|
| Age (years) | 8 | 75 | 34.75 | 13.57 |
| Male/female (%) | 68.9/31.09 | |||
| Stone size (cm) | 1.8 | 4.3 | 2.67 | 0.456 |
| Duration of access (min) | 15 | 28 | 20.23 | 2.29 |
| Duration of radiation (s) | 54 | 85 | 63.76 | 5.88 |
SD: Standard deviation
DISCUSSION
PCNL is the preferred treatment for large renal stones.[10] Although fluoroscopy, ultrasonography, and computed tomography are being used to achieve the initial access to PCS, it is the fluoroscopy which is commonly used by urologists worldwide to achieve the initial access to PCS.[3] Both air and iodinated contrast has been used to enhance the PCS before the dilatation of the tract.[4] However, there is skepticism among the urologists about using air to enhance the PCS. This is despite the established advantages of air, such as no risk of extravasation, no risk of contrast allergy, and preserving the differentiation between residual stone and residual contrast, in case iodinated contrast was used to enhance the PCS. The most common complication reported in literature using air to enhance the PCS is air embolism. However, these are only case reports or mere presumptions with no concrete scientific data to support this.[6,7,8,9]
For example, Parikh et al. reported venous air embolism in a 32-year-old patient during PCNL when air was used to enhance the PCS. During procedure, end-tidal Co2 and SPO2 dropped and hemodynamic instability ensued. They suspected air embolism as a probable cause after excluding other possibilities.[9] However, this was only a mere presumption without any clinical evidence. Similarly, Basiri et al. reported neurologic complications (cerebrovascular accident) in 11 patients who had undergone PCNL in various centers in Iran where air was used to enhance the PCS. They presumed that these neurologic complications were due to air embolism due to air pyelography. However, majority of their patients had some predisposing factors for developing cerebrovascular accident, such as patent foramen ovale, aortic valve insufficiency, hypokinetic ventricular wall, and hypercoagulable state.[8]
In our center, we are regularly performing PCNL using air to opacify the PCS. In this study, 164 patients underwent PCNL. None of our patients developed any complication during the procedure or in the postoperative period, which could be attributed to air embolism. Jangid et al. compared antegrade air pyelogram and retrograde air pyelogram for initial puncture access during PCNL. They did not report any case of air embolism in their study.[4] Our results are comparable to their retrograde air pyelogram group. The contrasting feature of this study is that we only used retrograde air pyelogram for initial puncture access. Lipkin et al. studied whether air pyelogram was associated with a decrease in radiation exposure compared with standard retrograde pyelogram. They concluded that air retrograde pyelogram was associated with decreased radiation exposure during PCNL when compared with a contrast retrograde pyelogram.[5] Similar to this study, they also did not report any case of air embolism while using air to opacify the PCS.
CONCLUSIONS
This study ascertains that initial access for PCNL using air for opacification of PCS is a safe and acceptable alternative to iodinated contrast. However, further studies are needed to confirm this.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fernström I, Johansson B. Percutaneous pyelolithotomy. A new extraction technique. Scand J Urol Nephrol. 1976;10:257–9. doi: 10.1080/21681805.1976.11882084. [DOI] [PubMed] [Google Scholar]
- 2.Ramakumar S, Segura JW. Renal calculi. Percutaneous management. Urol Clin North Am. 2000;27:617–22. doi: 10.1016/s0094-0143(05)70111-7. [DOI] [PubMed] [Google Scholar]
- 3.Basiri A, Ziaee AM, Kianian HR, Mehrabi S, Karami H, Moghaddam SM. Ultrasonographic versus fluoroscopic access for percutaneous nephrolithotomy: A randomized clinical trial. J Endourol. 2008;22:281–4. doi: 10.1089/end.2007.0141. [DOI] [PubMed] [Google Scholar]
- 4.Jangid DK, Sharma G, Yadav SS, Tomar V, Mathur R. A comparative study of antegrade air pyelogram and retrograde air pyelogram for initial puncture access during percutaneous nephrolithotomy. J Clin Diagn Res. 2017;11:PC01–3. doi: 10.7860/JCDR/2017/24821.9724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lipkin ME, Mancini JG, Zilberman DE, Raymundo ME, Yong D, Ferrandino MN, et al. Reduced radiation exposure with the use of an air retrograde pyelogram during fluoroscopic access for percutaneous nephrolithotomy. J Endourol. 2011;25:563–7. doi: 10.1089/end.2010.0431. [DOI] [PubMed] [Google Scholar]
- 6.Varkarakis J, Su LM, Hsu TH. Air embolism from pneumopyelography. J Urol. 2003;169:267. doi: 10.1016/S0022-5347(05)64084-0. [DOI] [PubMed] [Google Scholar]
- 7.Song SH, Hong B, Park HK, Park T. Paradoxical air embolism during percutaneous nephrolithotomy: A case report. J Korean Med Sci. 2007;22:1071–3. doi: 10.3346/jkms.2007.22.6.1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basiri A, Soltani MH, Kamranmanesh M, Tabibi A, Mohsen Ziaee SA, Nouralizadeh A, et al. Neurologic complications in percutaneous nephrolithotomy. Korean J Urol. 2013;54:172–6. doi: 10.4111/kju.2013.54.3.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parikh GP, Sonde SR, Kadam P. Venous air embolism: A complication during percutaneous nephrolithotomy. Indian J Urol. 2014;30:348–9. [Google Scholar]
- 10.Ko R, Soucy F, Denstedt JD, Razvi H. Percutaneous nephrolithotomy made easier: A practical guide, tips and tricks. BJU Int. 2008;101:535–9. doi: 10.1111/j.1464-410X.2007.07259.x. [DOI] [PubMed] [Google Scholar]


