Abstract
Introduction
Bladder neck sclerosis is a rare late complication of transurethral resection of the prostate (TURP). Endoscopic resection or incision of the bladder neck is usually successful in the management of such cases. In some cases, even repeated endoscopic management always followed with recurrent sclerosis. In these cases, the Y-V plasty of the bladder neck provides a final option of treatment.
Material and methods
Retrospective evaluation of 24 patients who underwent Y-V plasty of the bladder neck from 2007 to 2014 was performed. All patients had TURP once and presented after at least 2 failed attempts of endoscopic management. The principle of this technique is to insert a V-shaped part of the bladder wall into the fibrosed bladder neck. The patient evaluation included measuring Q max, residual urine volume and asking about their satisfaction. All patients were operated in the same center by the same surgeon.
Results
The mean age of patients at surgery was 66.8 years (range 56–74 years). All patients presented preoperatively with obstructive micturition with mean Qmax 2.2 ml/s (SD ±1.9) and mean residual urine volume of 381 ±169 ml. After a mean follow-up of 46 months (SD ±22), the mean Qmax reached 16.4 ml/s (SD 3.3) while the mean residual urine volume was 18 ml (SD ±6). Recurrent sclerosis occurred in three patients (12.5%). A total of 94.1% of patients reported satisfactory micturition with significant improvement in the quality of life.
Conclusions
The Y-V plasty can provide a final option with a high success rate for patients with bladder neck sclerosis after failed endoscopic treatment.
Keywords: benign, prostatic hypertrophy, bladder neck contracture, bladder reconstruction, hyperplasia, stricture recurrence
INTRODUCTION
Transurethral resection of the prostate (TURP) is considered the gold standard in treatment for benign prostatic hypertrophy [1]. Bladder neck contracture (BNC) was reported to range between 0.5–4% following TURP [2, 3]. Different risk factors have been proposed, including smaller prostate size, pervasive cauterization, extensive scarring process and extended resection of the bladder neck [4]. Usually, BNC is discovered during the 2nd year after surgery with a declining urine stream and recurring obstructive voiding pattern. Most cases are first treated endoscopically, with a success rate reaching up to 86% [5]. After the failure of the second endoscopic attempt, patients with BNC are considered resistant for endoscopic management and usually offered a more radical solution including open reconstruction versus urinary diversion [6]. Urethrovesical reconstruction has been endorsed as the last resort after the failure of endoscopic treatments. Young [7] has introduced the retropubic approach for vesical neck obstruction repair in children, and these techniques are gaining popularities in such devastating situations. In our study, we are evaluating the outcome of Y-V plasty as a final option in patients with recurrent bladder neck sclerosis after failed endoscopic treatment.
MATERIAL AND METHODS
We retrospectively evaluated 24 patients who underwent Y-V plasty of the bladder neck from 2007 to 2014. All patients had TURP for bothersome lower urinary tract symptoms or urine retention. All patients reported recurrence of bothersome obstructive symptoms and underwent at least two trials of endoscopic bladder neck resection or incision.
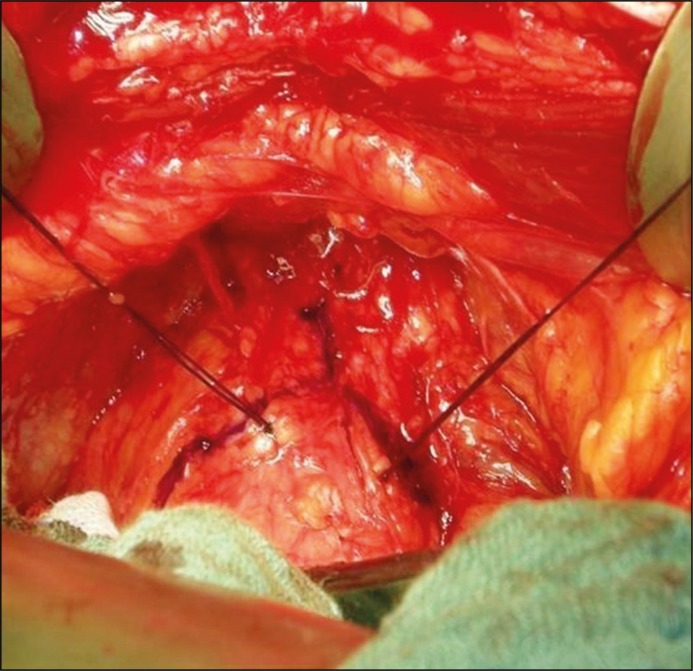
Preoperative evaluation included: uroflowmetry to assess the degree of urine flow obstruction, combined ascending urethrogram and cystogram (Figure 1) to assess the bladder capacity, stricture site, and the patency of the prostatic urethra. A diagnostic cystoscopy was performed prior to surgery to assess and conclude the site of obstruction.
Figure 1.
Preoperative ascending urethrogram showing bladder neck contracture.
Preoperative urine analysis and treatment of any urinary tract infection according to culture and sensitivity was also performed. A single shot of cefuroxime 1.5 g (i.v.) was given at the time of surgery. No routine antibiotic prophylaxis was given afterward.
Surgical technique
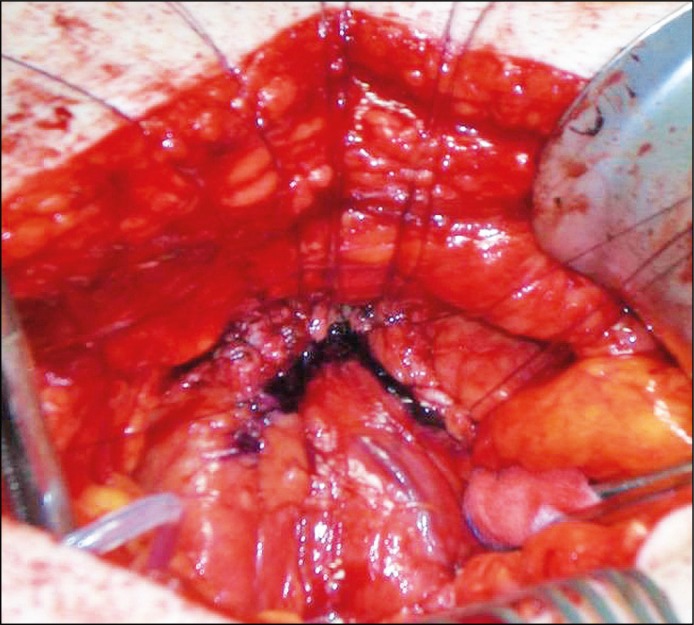
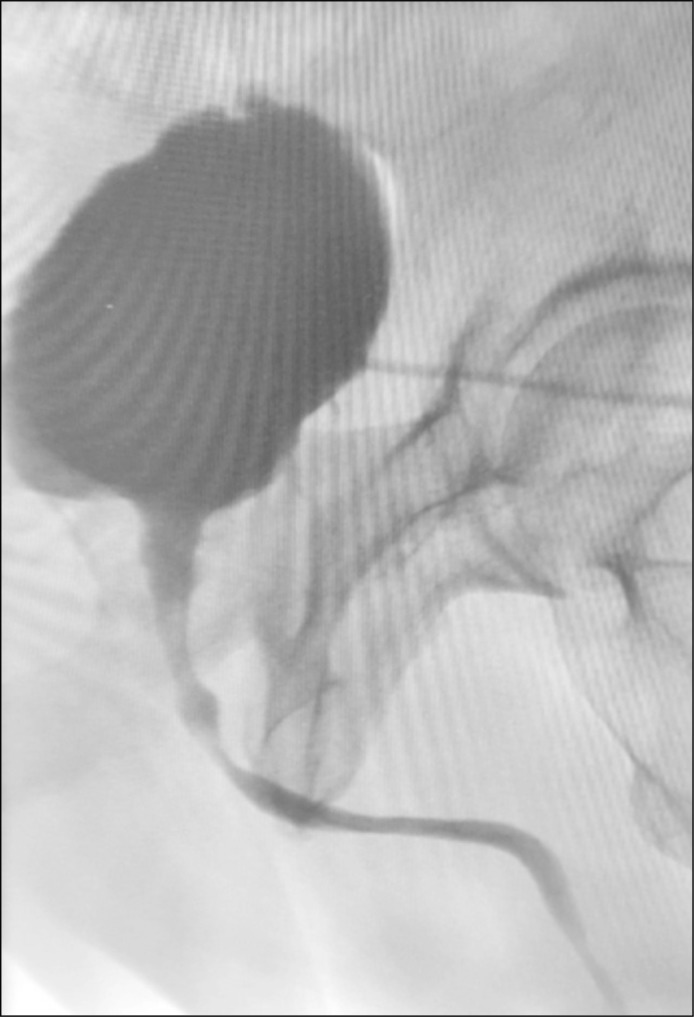
Patients were placed in a supine position. Access was gained through an abdominal midline or Pfannenstiel incision. Removal of the peri-prostatic fat and filling the bladder with saline helped to define the bladder neck using the typical retropubic approach. It is not routinely needed to ligate the dorsal venous complex to expose the anterior surface of the prostate unless a significant bleeding occurs. After proper exposure of the bladder neck, the anterior bladder wall was incised in a V-shaped manner with the apex of the V at the bladder neck. Incision of the stenotic bladder neck ring was done through a distal incision extending from the apex of the V toward the wide urethra to complete the Y- shaped incision (Figure 2). The next step was excision of the fibrotic tissue at the bladder neck followed by insertion of both transurethral and suprapubic catheters. Mobilization of a tension-free well-vascularized flap (Y-V plasty) to reconstruct a wide bladder neck and anterior prostatic urethra was performed. The flap was sutured to the healthy urethra distally to the bladder neck in a V-shape using interrupted 3/0 polygalactic acid sutures (Figure 3). The bladder was closed in layers over a suprapubic catheter and control for leak tightness was performed. On the 10th post-operative day, after exclusion of extravasation via cystogram, the transurethral catheter was removed and a voiding cystourethrogram was perormed (Figure 4). Micturition was then allowed, and the suprapubic catheter remained closed for another day to control the residual urine volume. With enough spontaneous micturition and non-significant residual urine, the suprapubic catheter was removed. Statistical analyses were performed using JMP™ software utilizing the chi-square test for comparing discrete variables, whereas the Wilcoxson signed-rank test was used for continuous variables.
Figure 2.
Incision of the stenotic bladder neck ring in Y shaped fashion.
Figure 3.
Mobilization of a tension-free well-vascularized flap (Y become V).
Figure 4.
Voiding cysto- uerthrogram showing resolution of the stenotic bladder neck.
RESULTS
Twenty-four patients were included in our study with a mean age at surgery of 68 (SD ±7) years and mean follow-up was 46 (SD ±22) months. All patients had at least 2 transurethral surgeries. The etiology of stricture was TURP in 96% of patients and holmium laser enucleation in 4% of patients. All patients had BPH in histologic examination. The mean size of the prostate before the endoscopic treatment was 54 g (SD ±26). Pre-operative Qmax was 2.2 ml/s (SD ±1.9) and the international prostate symptom-quality of life (IPSS-QoL) score was 25 (SD ±2). Mean operative time was 79 minutes (SD ±10), the mean blood loss was 144 ml (SD ±112). The mean hospital stay was 12 days (SD ±3). There was no need for blood transfusion and there were no intraoperative complications. The success rate at the time of follow-up reached 87.5% with 3 cases that required another intervention (1 patient required a urinary diversion and 2 other patients required endoscopic resection). Mean post-operative Qmax reached 16.4 (SD ±3.3) and the IPSS-QoL score was 2 (SD ±1) (Table 1). There were no reported cases of stress or total incontinence while urge incontinence declined after 2 months follow-up with a prescribed anticholinergic.
Table 1.
Comparison between pre- and post-operative voiding parameters
| Variables | Pre-operative | Post-operative | P Value |
|---|---|---|---|
| Qmax (mean) ml/sec | 2.2 ±1.9 | 16.4 ±3.3 | 0.0001 |
| Post-void residual volume (mean) ml | 381 ±169 | 18 ±6 | 0.0001 |
| IPSS (mean) | 25 | 2 ±1 | 0.0001 |
IPSS – International Prostate Symptom Score
DISCUSSION
Recurrent bladder neck fibrosis following endoscopic resection of the prostate is considered one of the urologic dilemmas for both patients and urologists. The patient often presents with various degrees of obstructive lower urinary tract symptoms or retention. Management usually begins with endoscopic incision [8] or resection [9] of the stricture, with an adjunctive injection of anti-inflammatory agents [10] in some situations. Some authors have provided more simplified solutions; including a regimen of urethral dilation to 18F followed by a 3-month period of intermittent self-catheterization, but with more increased risk of urethral trauma and erosion [11]. Cold knife incision (CKI) has been suggested for initial management of BNC after the failure of filiform and follower dilation, with a 74% success rate [12]. Introduction of mitomycin C (MMC) after balloon dilatation [13] or cold knife incision [14] was hindered by the reported incidence of anaphylaxis, extravasation, or bladder neck necrosis with possible recourse to cystectomy caused by the injection of MMC [15].
Holmium lasers have been used for incision of the stenotic segment at the 3 and 9 o'clock positions followed by injection of 80 mg triamcinolone with a reported success rate of 83% [16]. Recently [17], Sun and colleagues reported the safety and efficacy of both thulium laser enucleation and thulium laser resection of the prostate for prevention of bladder neck contracture in a small prostate.
Patients with refractory BNC, are advocated for more invasive procedures. Although urinary diversion is considered the only permanent recurrence-free option, it comes with a great risk of functional and psychological co-morbidities [18]. Pfalzgraf et al. [19] reported 60% success rates of open re-anastomosis for recurrent bladder neck stenosis over a 60-month follow-up period.
Unfortunately, with a 40%, failure rate, and 31% new-onset incontinence; this technique did not receive much consideration. For that reason, the consideration for another more favorable radical solution, through the utilization of the principle of vesicourethral anastomosis after excision of the stenotic segment is prompted.
The Young Y-V plasty principle and bladder flap surgery allowed successful reconstruction of the bladder neck utilizing a healthy bladder flap to replace the sclerotic bladder neck. However, the literature for such surgeries is extremely scarce with only a few reports available.
In our series, the result approached 87.5% with mean post-operative uroflowmetry, 16.4 – ±3.3 m/sec, after a mean follow-up of 46 ±22 months that seems to be comparatively good, considering that Reiss et al. [20] reported a 100% success rate with no need for further instrumentation over a period of 22 months.
Our objective measures such as the mean Qmax and post-void urine residual (PVUR) improved significantly, reaching 16.4 ±3.3 ml/s and 18 ±6 ml with 94% of patients reporting satisfactory micturition with significant improvement of the quality of life.
With such results, the burden of open reconstructive plasty technique seems favorable and the introduction of robotic-assisted Y-V plasty [21] with a similar promising result would overcome the morbidity of recurrent bladder neck sclerosis following endoscopic prostatectomy. This study has some limitations. Its retrospective nature and the limited number of patients represent our main limitations, however, the rarity of the condition and the requested longer follow-up period would justify these limitations.
CONCLUSIONS
Recurrent BNC represents a challenging therapeutic condition. After repeated transurethral treatment failures, the Y-V plasty is a valuable option in treatment for recurrent BNC caused by transurethral surgery of the prostate, which offers multiple advantages compared to other approaches and techniques. The high success rate, low rate of complications and no de novo incontinence are highly satisfactory results.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest
References
- 1.Mayer EK, Kroeze SG, Chopra S, Bottle A, Patel A. Examining the 'gold standard': a comparative critical analysis of three consecutive decades of monopolar transurethral resection of the prostate (TURP) outcomes. BJU Int. 2012;110:1595–601. doi: 10.1111/j.1464-410X.2012.11119.x. [DOI] [PubMed] [Google Scholar]
- 2.Sikafi Z, Butler MR, Lane V, O'Flynn JD, Fitzpatrick JM. Bladder neck contracture following prostatectomy. Br J Urol. 1985;57:308–310. doi: 10.1111/j.1464-410x.1985.tb06351.x. [DOI] [PubMed] [Google Scholar]
- 3.Li X, Pan JH, Liu QG, et al. Selective trans-urethral resection of the prostate combined with transurethral incision of the bladder neck for bladder outlet obstruction in patients with small-volume benign prostate hyperplasia (BPH): a prospective randomized study. PLoS ONE. 2013;9:e63227. doi: 10.1371/journal.pone.0063227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cindolo L, Marchioni M, Emiliani E, et al. Bladder neck contracture after surgery for benign prostatic obstruction. Minerva Urol Nefrol. 2017;69:133–143. doi: 10.23736/S0393-2249.16.02777-6. [DOI] [PubMed] [Google Scholar]
- 5.Pansadoro V, Emiliozzi P. Iatrogenic prostatic urethralstrictures: classification and endoscopic treatment. Urology. 1999;53:784–789. doi: 10.1016/s0090-4295(98)00620-7. [DOI] [PubMed] [Google Scholar]
- 6.Spahn M, Kocot A, Loeser A, Kneitz B, Riedmiller H. Last resort in devastated bladder outlet: bladder neck closure and continent vesicostomy - long-term results and comparison of different techniques. Urology. 2010;75:1185–1192. doi: 10.1016/j.urology.2009.11.070. [DOI] [PubMed] [Google Scholar]
- 7.Young BW. The retropubic approach to vesical neck obstruction in children. Surg Gynecol Obstet. 1953;96:150–154. [PubMed] [Google Scholar]
- 8.Chiu AW, Chen MT, Chang LS, et al. Prophylactic bladder neck incision in the treatment of small benign prostatic hyperplasia. Zhonghua Yi Xue Za Zhi (Taipei). 1990;45:22–25. [PubMed] [Google Scholar]
- 9.Lee YH, Chiu AW, Huang JK. Comprehensive study of bladder neck contracture after transurethral resection of prostate. Urology. 2005;65:498–503. doi: 10.1016/j.urology.2004.10.082. [DOI] [PubMed] [Google Scholar]
- 10.Sikafi Z, Butler MR, Lane V, O'Flynn JD, Fitzpatrick JM. Bladder neck contracture following prostatectomy. Br J Urol. 1985;57:308–310. doi: 10.1111/j.1464-410x.1985.tb06351.x. [DOI] [PubMed] [Google Scholar]
- 11.Park R, Martin S, Goldberg JD, Lepor H. Anastomotic strictures following radical prostatectomy: insights into incidence, effectiveness of intervention, effect on continence, and factors predisposing to occurrence. Urology. 2001;57:742–746. doi: 10.1016/s0090-4295(00)01048-7. [DOI] [PubMed] [Google Scholar]
- 12.Giannarini G, Manassero F, Mogorovich A, et al. Cold-knife incision of anastomotic strictures after radical retropubic prosta- tectomy with bladder neck preservation: efficacy and impact on urinary continence status. Eur Urol. 2008;54:647–656. doi: 10.1016/j.eururo.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 13.Ramirez D, Simhan J, Hudak SJ, Morey AF. Standardized approach for the treatment of refractory bladder neck contractures. Urol Clin North Am. 2013;40:371–380. doi: 10.1016/j.ucl.2013.04.012. [DOI] [PubMed] [Google Scholar]
- 14.Redshaw JD, Broghammer JA, Smith TG, 3rd, et al. Intralesional injection of mitomycin C at transurethral incision of bladder neck contracture may offer a limited benefit: TURNS study group. J Urol. 2015;193:587–592. doi: 10.1016/j.juro.2014.08.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vanni AJ, Zinman LN, Buckley JC. Radial urethrotomy and intralesional mitomycin C for the management of recurrent bladder neck contractures. J Urol. 2011;186:156. doi: 10.1016/j.juro.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 16.Eltahawy E, Gur U, Virasoro R, Schlossberg SM, Jordan GH. Management of recurrent anastomotic stenosis following radical prostatectomy using holmium laser and steroid injection. BJU Int. 2008;102:796–798. doi: 10.1111/j.1464-410X.2008.07919.x. [DOI] [PubMed] [Google Scholar]
- 17.Sun Q, Guo W, Cui D, et al. Thulium laser enucleation versus thulium laser resection of the prostate for prevention of bladder neck contracture in a small prostate: a prospective randomized trial. World J Urol. 2018;37:853–859. doi: 10.1007/s00345-018-2463-8. [DOI] [PubMed] [Google Scholar]
- 18.Spahn M, Kocot A, Loeser A, Kneitz B, Riedmiller H. Last resort in devastated bladder outlet: bladder neck closure and continent vesicostomy – longtermresults and comparison of different techniques. Urology. 2010;75:1185–1192. doi: 10.1016/j.urology.2009.11.070. [DOI] [PubMed] [Google Scholar]
- 19.Pfalzgraf D, Beuke M, Isbarn H, Reiss CP, et al. Open retropubic re-anastomosis for highly recurrent and complex bladder neck stenosis. J Urol. 2011;186:1944–1947. doi: 10.1016/j.juro.2011.07.040. [DOI] [PubMed] [Google Scholar]
- 20.Reiss CP, Rosenbaum CM, Becker A, et al. The T-plasty: a modified YV-plasty for recurrent bladder neck contracture after transurethral surgery for benign hyperplasia of the prostate: clinical outcome and patient satisfaction. World J Urol. 2016;34:1437–1442. doi: 10.1007/s00345-016-1779-5. [DOI] [PubMed] [Google Scholar]
- 21.Musch M, Hohenhorst JL, Vogel A, Loewen H, Krege S, Kroepfl D. Robot-assisted laparoscopic YV-plasty in patients with refractory bladder neck contracture. J Urol. 2016;193(Suppl):e845. doi: 10.1007/s11701-017-0708-y. [DOI] [PubMed] [Google Scholar]