Abstract
Introduction
Laparoscopic nephrectomy (LN) is the most performed laparoscopic procedure by urologic residents (Res). A large amount of data exists on laparoscopic nephrectomies in terms of safety and surgical outcomes, but only a little is known about the influence of residents. The purpose of this study was to evaluate this influence on the clinical outcome of a laparoscopic nephrectomy.
Material and methods
Retrospectively, patients who had undergone a LN between 2010 and 2018 were assessed. Data included patient demographics, date of surgery, pre- and postoperative results and complications. The patients who had undergone a LN were divided into two groups: one where residents were involved and another group where only a staff surgeon (Sur) performed the operation. All training residents had a questionnaire sent to them to evaluate their role during the LN.
Results
A total of 229 patients met the study criteria, of which 78 patients were operated together with a resident and 151 by a staff surgeon alone. Both groups were homogeneous in terms of age, comorbidities, left/right sided LN and tumor-stage. Between these two groups, no significant differences were observed in median estimated blood loss (Res 87 ml vs. Sur 100 ml), intraoperative adverse events (Res 10.3% vs. Sur 6% p = 0.24), conversion to open surgery (Res 6.4% vs. Sur 6%) and high-grade postoperative complications (Res 3.9% vs. Sur 4.6%). However, when a resident participated, the LN lasted on average 20 minutes longer (Res mean 130 min vs. Sur 110 min p ≤0.001).
Conclusions
Our data shows that involvement of a resident in laparoscopic nephrectomy has no effect on the clinical outcome. Therefore, it is safe to perform a laparoscopic nephrectomy together with a resident, but it is important to take the additional surgical time into account.
Keywords: complications, laparoscopy, nephrectomy, outcome assessment, quality of health care and residency
INTRODUCTION
Progression in surgery has led to the development of minimally invasive surgery. Nowadays, laparoscopy is becoming more dominant in most surgical fields because of its advantages over open surgery [1–4]. Compared to open surgery, however, laparoscopy is more difficult to teach and has longer learning curves [5–9]. In general, it requires more skill due to the importance of hand-eye coordination and adaptation to two-dimensional vision.
Participation of residents (Res) during surgery is integral to any surgical curriculum. Laparoscopy can be learned in general surgery on the basis of relatively simple and harmless procedures such as cholecystectomy and appendectomy. In urology, laparoscopic nephrectomy (LN) is the most frequent laparoscopic operation in which residents are involved [10]. Compared to laparoscopic appendectomy or cholecystectomy, LN is fairly difficult and can be risky, especially during preparation of the renal hilum [8].
In the Netherlands, the curriculum of urologic residents consists of one and half years of general surgical training, which is often spent in the emergency room and patient ward. During this period, urologic residents gain minimal laparoscopic experience. Subsequently, they have four years of urologic surgical training where they learn about the common laparoscopic procedures in urology. At the end of the educational program, the residents should be able to perform laparoscopic pelvic lymph node dissection and nephrectomy independently [10].
Nowadays, society demands maximum efficiency of training and transparency of surgical results, and exposing patients to the risk of a learning curve is not accepted. It is however, unexplored what influence residents have on the outcome of laparoscopic procedures. Therefore, we examined the intra- and postoperative outcomes of the most frequently performed laparoscopic procedure in which urologic residents are involved, i.e. laparoscopic nephrectomy, in a teaching hospital for residents and a general, non-teaching hospital without residents.
MATERIAL AND METHODS
Local approval was granted to acquire the records of every patient who underwent a LN between November 2010 and December 31st 2017 in two separate hospitals with minimally invasive surgery as a focus area; one with teaching facilities (Canisius Wilhelmina Hospital, two staff surgeons for LN) and a general, non-teaching hospital without teaching facilities (Hospital Gelderse Vallei, one staff surgeon for LN). Retrospective data was obtained from the electronic patient record system. Surgical as well as anaesthesiological reports were fully reviewed.
A LN procedure was included if the transabdominal approach was used. The retroperitoneal approach was reserved for staff surgeons solely and therefore excluded from analysis. Also, all primarily open and partial nephrectomies were excluded from this trial.
The patient characteristics included gender, age, body mass index (BMI), age-adjusted Charlson comorbidity index (CCI), and side and size of the renal tumor. Intraoperative data included resident involvement, blood loss, operating time, adjacent organ injuries, and conversion to open surgery. Postoperative complications were recorded according to the Clavien-Dindo (CD) system [11].
All training residents involved were contacted and had a questionnaire sent to them to assess their involvement during the LN and the total amount of LNs they participated in while they worked at CWH. Furthermore, they could score their independency during the LN by a 4-point scale: only a little (1), intermediate (2), mostly (3) or complete (4) independence.
The primary outcome of this analysis was to compare the risk of complications when training residents are involved in a LN. Secondary outcomes were operating time (OT) and hospital admission. Additionally, the results of the teaching hospital were compared to those of the non-teaching hospital.
All statistical analyses were done by SPSS v25.0. Baseline characteristics were dichotomized by resident involvement (yes/no). Dichotomous variables were compared using the Chi-square or Fisher’s exact test. The independent t-test was used to differentiate between continuous variables when normality was met. The Mann-Whitney test was used for non-normal distributions. P <0.05 was considered statistically significant.
RESULTS
A total of 232 consecutive patients underwent a LN and were included for analysis. Because retrospective data could not determine if a resident was involved or not, three cases had to be excluded. The remaining 229 cases were all performed or supervised by a total of three staff-urologists (two in CWH and one urologist in HGV). In 78 of these cases, a resident was involved, whereas in 151 cases the surgery was performed by a staff surgeon together with a colleague or experienced operating nurse.
A comparison was made between the cohorts that were operated with and without involvement of residents. Patient demographics and tumor characteristics are shown in Table 1. Both cohorts were comparable in age, sex, BMI and CCI score, and had comparable frequencies of left/right-sided and benign/radical nephrectomies. Also, the tumor (T) stage and mean tumor size were comparable between both groups.
Table 1.
Patient demographics and tumor characteristics
| With Res (n = 78) | Without Res (n = 151) | p-Value | |
|---|---|---|---|
| Males, No. (%) | 51 (65.4) | 80 (53) | 0.072 |
| Age, median (IQR), years | 67 (60–73) | 68 (59–74) | 0.76 |
| BMI, mean (SD), kg/l2 | 27.9 (5.1) | 28.4 (5.8) | 0.523 |
| CCI, median (IQR) | 4 (2–5) | 4 (3–5) | 0.338 |
| Left sided, No. (%) | 38 (48.7) | 70 (46.4) | 0.735 |
| Tumor size, mean (SD), cm | 5.7 (2.6) | 5.9 (2.9) | 0.57 |
| Benign nephrectomy, No. (%) | 12 (15.4) | 17 (11.3) | – |
| Tumor nephrectomy, No. (%) | 66 (84.6) | 134 (88.7) | 0.374 |
| Pathologic tumor stage (T) | 0.41 | ||
| T0 (benign), No. (%) | 14 (21.2) | 15 (11.3) | – |
| T1 (a/b), No. (%) | 27 (40.9) | 67 (50.4) | – |
| T2 (a/b), No. (%) | 12 (18.2) | 25 (18.8) | – |
| T3 (a/b/c), No. (%) | 12 (18.2) | 23 (17.3) | – |
| T4, No. (%) | 1 (1.5) | 3 (2.3) | – |
Res – residents; CCI – age-adjusted Charlson comorbidity index; IQR – interquartile range; BMI – body mass index; SD – standard deviation; T – pathologic tumor stage
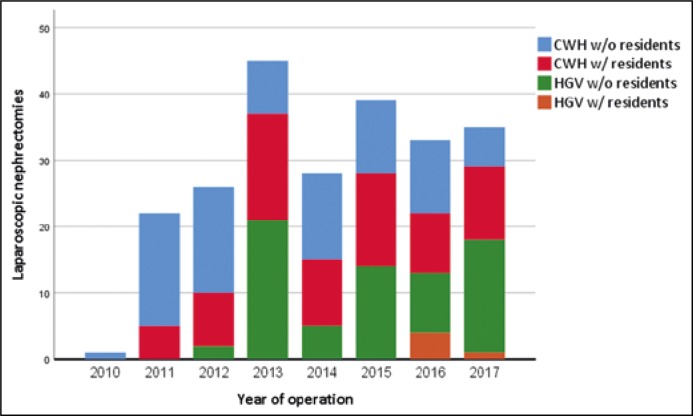
In the teaching hospital, 47% of the LNs were performed with involvement of residents (Figure 1). When the laparoscopic nephrectomies with residents were excluded, no discrepancies were found between the teaching and non-teaching hospital respectively in terms of mean OT (respectively, 109 minutes vs. 110 minutes), median estimated blood loss (both 100 ml, p = 0.209), intraoperative lesions (6.0% vs. 5.9%, p = 0.971), postoperative complications (both 26.5%, p = 0.996) and duration of hospital admission (5.9 days vs. 5.3 days, p = 0.530).
Figure 1.
Number of yearly laparoscopic nephrectomies performed by each hospital with or without residents.
CWH – Canisius Wilhelmina Hospital (accredited teaching hospital); HGV – Hospital Gelderse Vallei (general, non-teaching hospital); w/ – with; w/o – without
In Table 2, the intra- and postoperative results are shown after dichotomization for residents. Mean OT was significantly longer in the group with residents. This was not the case for median estimated blood loss (EBL). Six percent of the laparoscopic procedures (n = 14) were converted to open. Reasons were adhesions (n = 6), and insufficient progression during surgery (n = 5). Two patients needed conversion because of gross hilar bleeding. In one procedure, a resident was involved. Another patient needed conversion because of bowel injury. A resident was involved in this case also. Perioperative injuries to adjacent organs occurred in 17 cases; 8 in the group with residents and 9 in the group without residents. Both groups had similar numbers as well as severity of postoperative complications. High-grade complications included ileus with need for surgical intervention (n = 2) and drainage of intra-abdominal abscess (n = 4). Four patients suffered from postoperative hemorrhage with need for surgical re-intervention. Between the two groups, no difference was found between non-radical surgical resections; 1.3% and 3.3% respectively in the group with and without residents (p = 0.667). Pathology reports showed two cases with pT4 urothelial cell carcinoma, two with pT3a renal cell carcinoma and one with an invasive growing liposarcoma.
Table 2.
Operative data and intra- and postoperative complications
| With Res (n = 78) | Without Res (n = 151) | p-Value | |
|---|---|---|---|
| OT, Mean (SD), min. | 130 (±39) | 110 (±34) | <0.001 |
| EBL, Median, (IQR), ml. | 87.5 (50–200) | 100 (50–200) | 0.835 |
| >500 ml EBL, No. (%) | 6 (8.3) | 8 (5.4) | 0.394 |
| Intraoperative lesions, No. (%) | 8 (10.3) | 9 (6.0) | 0.24 |
| Spleen laceration, No. | 1 | 3 | – |
| Liver laceration, No. | 0 | 1 | – |
| Gallbladder laceration, No. | 0 | 1 | – |
| Diaphragm laceration, No. | 3 | 1 | – |
| Intestinal serosal laceration, No. | 4 | 3 | – |
| Conversion to open, No. (%) | 5 (6.4) | 9 (6) | 1 |
| Duration of hospital stay, mean (SD), days | 5.8 (10) | 5.7 (6) | 0.876 |
| No complications, No. (%) | 55 (70.5) | 111 (73.5) | |
| Complications, No. (%) | 23 (29.5) | 40 (26.5) | 0.630 |
| CD grade 1, No. (%) | 12 (15.4) | 19 (12.6) | 0.557 |
| CD grade 2, No. (%) | 8 (10.3) | 14 (9.3) | 0.811 |
| CD grade 3, No. (%) | 2 (2.6) | 4 (2.6) | 1 |
| CD grade 4, No. (%) | 1 (1.3) | 3 (2.0) | – |
| CD grade 5, No. (%) | 0 (0) | 0 (0) | – |
Res – residents; OT – operating time; SD – standard deviation; IQR – interquartile range; EBL – estimated blood loss; CD – Clavien-Dindo; OT – operating time
Between 2010 and 2017, a total of 10 residents were involved during LNs and were sent a questionnaire. Eight of 10 completed this questionnaire. All were trained at the teaching hospital for about 2 years. During that time, each resident participated in a median of 9 LNs (range 2–20). Five of these 8 residents completed the LN with only minor support of a staff surgeon (questionnaire: score 3 or 4 on independency) and three did less than half of the surgical procedure themselves. Compared to a staff surgeon alone, those residents who completed the procedure with minor support did not have worse results. They had an equal amount of: estimated blood loss (Res 100 ml vs. Sur 100 ml, median, p = 0.782), intraoperative lesions (Res 8.1% vs. Sur 6% p = 0.707), conversion rates (Res 5.4% vs. Sur 6%, p = 0.897) and postoperative complications (Res 21.6% vs. Sur 26.5%, p = 0.543). We did not observe any high-grade postoperative complications in this subgroup. However, these residents needed more operating time (mean 127 min SD 33 min) compared to a staff surgeon alone (p = 0.005).
DISCUSSION
For residents in urology, LN is the operation in which they acquire the most laparoscopic experience [10, 12]. However, this is a rather difficult procedure to learn as it involves critical steps such as preparation of the hilar vessels. In this article, we described the impact residents have on LN in terms of surgical safety and postoperative results. To minimize single center bias, we acquired data from a teaching hospital and a general, non-teaching hospital. Both hospitals have minimally invasive surgery as a focus area. Sub-analysis showed no differences between the two hospitals in terms of patient demographics or pre- and postoperative results. The teaching hospital is an accredited minimally-invasive technique teaching center. In this hospital residents frequently participate during surgery, as we observed in roughly 50% of LNs. Since 2010, the non-teaching hospital has had 5 occasions in which a resident participated during a LN. They were invited guests and were only allowed to hold the camera. All five procedures were uneventful.
After stratification for resident involvement, we observed that residents were not withheld from more difficult cases as both groups had homogeneous baseline demographics. Analysis did not show an increased risk of complications when residents participated. Similar results were published by others [13–19], even with LN being more challenging than laparoscopic appendectomy or cholecystectomy on which these groups did their analysis in [8, 16, 18]. Although surgery took a mean 20 minutes longer to complete, it did not end up with more blood loss or complications. The increased operating time was observed by others too [13–20]. This effect is understandable as the surgeon has to dedicate time explaining the procedure, and residents tend to be less efficient as their experience is lacking. No high-grade postoperative complications (CDIII–IV) were observed in the subgroup that did most of the LN independently. A reason for this could be that these residents had more experience or were more skilled, which also makes them more attentive for possible complications. Overall, we did not observe an increase in duration of hospital stay when residents took part in the surgery. Again, this shows that the teaching situation is not disadvantageous for patients. However, teaching is time consuming and requires extra minutes operating time which is expensive [21]. Nevertheless, this does not have an impact on the vital importance of training residents as surgical skill develops over repetitive exposure to increasing difficult situations [22].
Our study has some limitations concerning the retrospective nature of the data collection and the inherent subjectivity among the various series on the reporting of complications. Due to its retrospective nature, it was unknown which steps the resident exactly did during LN. This is a problem other studies had too. They often used the year of surgical training (PGY) [14, 15, 19]. This gives only little insight as laparoscopy skill differs between residents and is not exclusively dependent on year of training [22]. Also, their ability to participate varies between the days and cases, and is highly influenced by the experience and teaching skill of the surgeon. We evaluated this missing data by sending a questionnaire to all training residents involved. This more individual approach is a particular strength of this study. Another quality we provided is the comprehensive review of every LN performed. By doing so, it was possible to review intraoperative mistakes and lesions, even if it did not have postoperative consequences. Furthermore, the inclusion of a non-teaching hospital that served as a reference is another important asset of this study.
CONCLUSIONS
In conclusion, our data shows that resident involvement is not disadvantageous for the outcome of laparoscopic nephrectomies. Moreover, no differences in results between a teaching or non-teaching hospital setting were observed. Teaching during laparoscopic nephrectomies is safe but extra operating time has to be taken into account.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Liu G, Ma Y, Wang S, Han X, Gao D. Laparoscopic Versus Open Radical Nephrectomy for Renal Cell Carcinoma: a Systematic Review and Meta-Analysis. Transl Oncol. 2017;10:501–510. doi: 10.1016/j.tranon.2017.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Permpongkosol S, Chan DY, Link RE, et al. Long-term survival analysis after laparoscopic radical nephrectomy. J Urol. 2005;174:1222–1225. doi: 10.1097/01.ju.0000173917.37265.41. [DOI] [PubMed] [Google Scholar]
- 3.Portis AJ, Yan Y, Landman J, et al. Long-term followup after laparoscopic radical nephrectomy. J Urol. 2002;167:1257–1262. [PubMed] [Google Scholar]
- 4.Dunn MD, Portis AJ, Shalhav AL, et al. Laparoscopic versus open radical nephrectomy: a 9-year experience. J Urol. 2000;164:1153–1159. [PubMed] [Google Scholar]
- 5.Soulié M, Salomon L, Seguin P, et al. Multi-institutional study of complications in 1085 laparoscopic urologic procedures. Urology. 2001;58:899–903. doi: 10.1016/s0090-4295(01)01425-x. [DOI] [PubMed] [Google Scholar]
- 6.Permpongkosol S, Link RE, Su LM, et al. Complications of 2,775 Urological Laparoscopic Procedures: 1993 to 2005. J Urol. 2007;177:580–585. doi: 10.1016/j.juro.2006.09.031. [DOI] [PubMed] [Google Scholar]
- 7.Wille AH, Roigas J, Deger S, Tüllmann M, Türk I, Loening SA. Laparoscopic radical nephrectomy: Techniques, results and oncological outcome in 125 consecutive cases. Eur Urol. 2004;45:483–488. doi: 10.1016/j.eururo.2003.10.019. [DOI] [PubMed] [Google Scholar]
- 8.Stolzenburg JU, Truss MC, Rabenalt R, et al. Training in Laparoscopy. EAU-EBU Updat Ser. 2007;5:53–62. [Google Scholar]
- 9.Abboudi H, Khan MS, Guru KA, et al. Learning curves for urological procedures: A systematic review. BJU Int. 2014;114:617–629. doi: 10.1111/bju.12315. [DOI] [PubMed] [Google Scholar]
- 10.Furriel FTG, Laguna MP, Figueiredo AJC, Nunes PTC, Rassweiler JJ. Training of European urology residents in laparoscopy: Results of a pan-European survey. BJU Int. 2013;112:1223–1228. doi: 10.1111/bju.12410. [DOI] [PubMed] [Google Scholar]
- 11.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Okhunov Z, Safiullah S, Patel R, et al. Evaluation of Urology Residency Training and Perceived Resident Abilities in the United States. J Surg Educ. 2019;76:936–948. doi: 10.1016/j.jsurg.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 13.Ferraris VA, Harris JW, Martin JT, Saha SP, Endean ED. Impact of Residents on Surgical Outcomes in High-Complexity Procedures. J Am Coll Surg. 2016;222:545–555. doi: 10.1016/j.jamcollsurg.2015.12.056. [DOI] [PubMed] [Google Scholar]
- 14.Gifford E, Kim DY, et al. The effect of residents as teaching assistants on operative time in laparoscopic cholecystectomy. Am J Surg. 2016;211:288–293. doi: 10.1016/j.amjsurg.2015.06.019. [DOI] [PubMed] [Google Scholar]
- 15.Cunningham SC, Maqsood H, Sill AM, et al. Effect of Residents on Operative Time and Complications: Focus on Laparoscopic Cholecystectomy in the Community. J Surg Educ. 2016;73:836–843. doi: 10.1016/j.jsurg.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 16.Pariani D, Fontana S, Zetti G, Cortese F. Laparoscopic Cholecystectomy Performed by Residents: A Retrospective Study on 569 Patients. Surg Res Pract. 2014;2014:1–5. doi: 10.1155/2014/912143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fahrner R, Turina M, Neuhaus V, Schöb O. Laparoscopic cholecystectomy as a teaching operation: Comparison of outcome between residents and attending surgeons in 1,747 patients. Langenbeck’s Arch Surg. 2012;397:103–110. doi: 10.1007/s00423-011-0863-y. [DOI] [PubMed] [Google Scholar]
- 18.Siam B, Al-Kurd A, Simanovsky N, et al. Comparison of appendectomy outcomes between senior general surgeons and general surgery residents. JAMA Surg. 2017;152:679–685. doi: 10.1001/jamasurg.2017.0578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jolley J, Lomelin D, Simorov A, Tadaki C, Oleynikov D. Resident involvement in laparoscopic procedures does not worsen clinical outcomes but may increase operative times and length of hospital stay. Surg Endosc. 2016;30:3783–3791. doi: 10.1007/s00464-015-4674-z. [DOI] [PubMed] [Google Scholar]
- 20.Matulewicz RS, Pilecki M, Rambachan A, Kim JYS, Kundu SD. Impact of resident involvement on urological surgery outcomes: An analysis of 40,000 patients from the ACS NSQIP database. J Urol. 2014;192:885–890. doi: 10.1016/j.juro.2014.03.096. [DOI] [PubMed] [Google Scholar]
- 21.Childers CP, Maggard-Gibbons M. Understanding costs of care in the operating room. JAMA Surg. 2018;153:e176233. doi: 10.1001/jamasurg.2017.6233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stride HP, George BC, Williams RG, et al. Relationship of procedural numbers with meaningful procedural autonomy in general surgery residents. Surgery. 2018;163:488–494. doi: 10.1016/j.surg.2017.10.011. [DOI] [PubMed] [Google Scholar]