Abstract
Objective:
To evaluate the relationships between perceived stigma and duration of untreated psychosis (DUP), demographic characteristics, and clinical and psychosocial functioning in persons with first episode of psychosis (FEP).
Method:
A total of 399 participants with FEP presenting for treatment at 34 sites in 21 states throughout the U.S. were evaluated using standardized instruments to assess diagnosis, symptoms, psychosocial functioning, perceived stigma, well-being, and subjective recovery.
Results:
Perceived stigma was correlated with a range of demographic and clinical variables, including DUP, symptoms, psychosocial functioning, and subjective experience. After controlling for symptom severity, perceived stigma was related to longer DUP, schizoaffective disorder diagnosis, more severe depression, and lower well-being and recovery. The associations between stigma and depression, well-being, and recovery were stronger in individuals with long than short DUP, suggesting the effects of stigma on psychological functioning may be cumulative over the period of untreated psychosis.
Conclusion:
The findings suggest that independent of symptom severity, perceived stigma may contribute to delay in seeking treatment for FEP, and this delay may amplify the deleterious effects of stigma on psychological functioning. The results point to the importance of reducing DUP and validating interventions targeting the psychological effects of stigma in people with FEP.
Keywords: Stigma, schizophrenia, first episode psychosis, duration of untreated psychosis
In modern usage, the word stigma is used to refer to “any attribute, trait or disorder that marks an individual as being unacceptably different from the ‘normal’ people with whom he or she routine interacts, and that elicits some form of community sanction.”1 The effects of the stigma of mental illness on persons with psychiatric disorders are profound and widespread.2–4 The majority of people with a severe mental illness report experiencing discrimination related to their psychiatric condition,5 which contributes to reduced employment, housing, and social opportunities,6 and is associated with poorer treatment of medical problems76 and lower credibility as crime victims with law enforcement officials.8 While the cost of stigma in lost human potential is high to individuals, families, and society,4 a more pernicious effect is its impact on engagement in treatment.
Negative, stigmatizing attitudes and beliefs about mental illness held by family members, other people, and individuals themselves play a major role in reducing the willingness of people with a psychiatric disorder to seek treatment.9–11 This delay in involvement in care can prolong the distress and disability associated with the untreated disorder. The consequences of increasing the duration of untreated psychosis (DUP) are especially dire. Extensive research documents that the longer the DUP, the worse the outcome.12–14 Furthermore, a longer DUP is associated with an attenuated response to comprehensive treatment for first episode psychosis.15–17.
Perceptions of stigma have been reported to be associated with a delay in seeking treatment for individuals with a first episode of psychosis,16–18 and are moderately correlated with internalized negative beliefs about mental illness or self-stigma in this population.19 In addition, people who have developed psychosis often experience significant social anxiety and shame about their disorder, and feelings of social marginalization that can contaminate their social interactions with others.20 Consequently, among people with a recent onset of psychosis, there is some evidence that experienced stigma is associated with a worse quality of life,19,21 greater levels of distressing symptoms such as depression and anxiety,22–24 and more impaired psychosocial functioning.25,26
While stigma appears to play a role in both engagement in treatment and functioning following a first episode of psychosis, there are inconsistent findings across the studies, often due to small sample sizes.19,26 Furthermore, little is known about the potential interactions between stigma, DUP, and adjustment in this population.
Aims of the Study
The present study was conducted in order to evaluate the demographic, clinical, and functional correlates of stigma in a large sample of individuals recently engaged in treatment for a first episode of psychosis. Analyses were also undertaken to explore whether clinical and psychosocial correlates of stigma differed as a function of DUP.
Material and methods
The study is based on baseline data collected in the Recovery After Schizophrenia Episode-Early Treatment Program (RAISE-ETP) project, a cluster randomized control trial conducted at 34 sites across the U.S., with sites randomized to provide either coordinated specialty care (the NAVIGATE program) or usual community care.15 A previous publication from this study examined demographic and clinical correlates of DUP,27 and found that longer DUP was associated with a younger age at onset of psychotic symptoms, an older age at enrollment in the RAISE-ETP study, more severe positive symptoms and overall symptoms, and worse psychosocial functioning. Correlates of DUP with perceived stigma, well-being, or sense of recovery were not reported. Out of 404 participants in the study, 399 completed stigma measures and were therefore included in this analysis.
Participants and Sites
Study inclusion criteria were: between 16 and 40 years of age; currently experiencing a first episode of psychosis (defined as the first experience of a period of psychotic symptoms in the absence of a full symptom remission); no more than six months prior use of antipsychotic medication; diagnosis of schizophreniform disorder, schizophrenia, schizoaffective disorder, brief psychotic episode, or psychosis NOS. Study exclusion criteria included: diagnoses of substance-induced psychosis, psychosis due to general medical condition or affective psychosis; clinically significant head trauma; or other serious medical conditions. All participants spoke English. Written informed consent was obtained from participants age 18 or over; individuals younger than 18 years of age provided assent, while their parents or guardians provided consent for participation. Participant characteristics can be found in Table 1. The study was approved by the institutional review boards of the participating sites and all procedures were overseen by the NIMH Data and Safety Monitoring Board.
Table 1.
Demographic and Diagnostic Characteristics of Participants (N = 399)
| Characteristic | M | SD |
|---|---|---|
| Age | 23.12 | 5.05 |
| N | % | |
| Gender | ||
| Male | 290 | 72.7 |
| Female | 109 | 27.3 |
| Ethnicity | ||
| Hispanic or Latino | 73 | 18.3 |
| Not Hispanic or Latino | 326 | 81.7 |
| Race | ||
| American Indian or Alaska Native | 21 | 5.3 |
| Asian | 12 | 3.0 |
| Black or African American | 151 | 37.8 |
| Native Hawaiian or Other Pacific Islander | 1 | 0.3 |
| White | 214 | 53.6 |
| Marital status | ||
| Married | 24 | 6.0 |
| Divorced, widowed, or separated | 21 | 5.3 |
| Never married | 354 | 88.7 |
| Currently in school | ||
| Yes | 76 | 19.0 |
| No | 323 | 81.0 |
| Currently working | ||
| Yes | 57 | 14.3 |
| No | 342 | 85.7 |
| Living situation | ||
| Live alone | 38 | 9.5 |
| Supported living arrangement | 3 | 0.8 |
| Structured environment | 11 | 2.8 |
| Family (parents/grandparents) | 283 | 70.9 |
| Family (spouse/children) | 33 | 8.3 |
| Homeless | 17 | 4.3 |
| Other | 14 | 3.5 |
| Education | ||
| Some graduate school | 5 | 1.3 |
| Completed college | 15 | 3.8 |
| Some college | 103 | 25.9 |
| Completed high school | 132 | 33.2 |
| Some high school | 123 | 30.9 |
| Completed 8th grade | 14 | 3.5 |
| Some grade school | 6 | 1.4 |
| Diagnosis | ||
| Schizophrenia | 211 | 52.9 |
| Schizoaffective disorder | 81 | 20.3 |
| Schizophreniform disorder | 65 | 16.3 |
| Other | 42 | 10.5 |
Note: One participant is missing education data.
Measures
Trained interviewers conducted all diagnostic and symptom assessments at baseline of the study using two-way live video conferencing, which has been shown to be a reliable assessment format.28 Abbreviated versions of three self-report measures (see below) were used to reduce assessment burden on the study participants.
Diagnosis.
The Structured Clinical Interview for Axis I DSM-IV disorders (SCID-IV)29 was administered to obtain primary psychiatric diagnosis and duration of untreated psychosis at study entry. When examining the association between stigma and DUP, due to the wide range in DUP, the median split (74 weeks) was used to dichotomize participants into low vs. high DUP.15,27
Stigma.
Seven items were drawn from the Stigma Scale30 to evaluate perceived mental health stigma in the RAISE-ETP study. The Stigma Scale is a 28-item self-report measure assessing perceived prejudice and discrimination related to mental illness, with items rated on a 5-point Likert scale ranging from strongly disagree (0) to strongly agree (4), with higher scores pertaining to greater perceived stigma. For this study, in order to use a similar scale for all the self-report measures, participants rated the seven items from the Stigma Scale on a 7-point scale ranging from strongly disagree (1) to strongly agree (7). The seven items were selected based on the investigators’ evaluations of representative questions tapping the construct of perceived stigma, and included: “Sometimes I feel that I am being talked down to because of my mental health problems,” “Some people with mental health problems are dangerous,” “Very often I feel alone because of my mental health problems,” “People’s reactions to my mental health problems make me keep to myself,” “People have avoided me because of my mental health problems,” “I feel the need to hide my mental health problems from my friends,” and “I do not feel embarrassed because of my mental health problems.” Examination the item-to-total correlations of these seven items indicated that all were significant at p < .001 (range: rs = .31-.74), except for the last item (r = −.01, NS), which was subsequently dropped. The remaining six items had a moderate internal consistency at the baseline assessment (α = .72), which was slightly higher (α = .78) at the six month assessment. The test-retest reliability of the abbreviated Stigma Scale between baseline and six months among the participants in the usual community care group was highly significant (r = .40, p < .001).
Clinical measures.
Psychiatric symptoms were assessed using the Positive and Negative Syndrome Scale (PANSS).31 The analyses utilized a five factor structure including: positive, negative, disorganization, excitement, and depression.32 Depression ratings were also obtained using the Calgary Depression Scale for Schizophrenia (CDSS).33
Fifteen of the 30 items on the Mental Health Recovery Measure (MHRM) were used to obtain self-reported ratings of general recovery,34 with items selected based on the investigators’ judgments of which questions most tapped the construct of recovery. All items were rated on a 7-point scale ranging from strongly disagree (1) to strongly agree (7), with higher scores reflecting greater sense of recovery. The fifteen items showed high internal reliability (α = .93) in this sample. Eighteen of the 84 items from the Scales of Psychological Well-Being (SPWB)35 were used to obtain self-report ratings of well-being. Items were rated on a 7-point scale ranging from strongly disagree (1) to strongly agree (7), with higher scores reflecting better well-being. Three items from each of the following six SPWB subscales were selected: environmental mastery, autonomy, personal growth, positive relationships, purpose in life, and self-acceptance. The internal consistency for all 18 items within this sample was fair (α = .51).
Psychosocial functioning.
The Quality of Life Scale (QLS) was used to measure psychosocial functioning.36 The QLS is a 21-item interview-based scale consisting of four subscales (interpersonal relations, intrapsychic foundations, instrumental functioning, and common objects and activities), as well as a total score. Although the QLS was originally created in order to measure the deficit symptoms of schizophrenia, since its development it has been widely used as a measure of psychosocial functioning in persons with schizophrenia-spectrum disorders.37–41
Statistical Analyses
Because perceived stigma could reflect the social effects of more severe symptoms, parallel analyses were conducted to explore the associations between perceived stigma and demographic, clinical, and psychosocial variables both without statistically controlling for symptoms and controlling for symptom severity, using the PANSS total score. The zero-order correlates of stigma with the demographic, clinical, and psychosocial variables were examined by computing Pearson correlations, between groups t-tests, and χ2 analyses between the mean score on the abbreviated Stigma Scale and continuous, binary, and multi-level categorical variables, respectively. To explore the associations and possible interaction between living at the home with parents or grandparents (yes/no), marital status (ever/never married), and stigma, a two by two analysis of variance (ANOVA) was conducted. A one-way ANOVA comparing the three primary psychiatric diagnoses on stigma was also conducted. To control for symptom severity for these analyses, partial correlations were computed for continuous variables, and analyses of covariance (ANCOVAs), with PANSS total score included as a covariate, were conducted for the categorical variables and the analysis of the interaction between marital status and living situation.
In addition, because longer DUP was found to be related to higher stigma scores, worse depression (Calgary), and lower ratings of recovery (MHRM) and well-being (SPWB) after controlling for symptoms, we explored the associations between stigma and these clinical variables within the low and high DUP subgroups. Specifically, we computed correlations between stigma scores and the clinical measures within each DUP group (and partial correlations controlling for symptom severity), and then performed r to z transformations to determine whether any of these correlations were significantly different between the low vs. high DUP group.
Results
Demographic Characteristics
Stigma was significantly related to marital status (t(397) = −2.37, p = .018), with those who had ever been married reporting more stigma (M = 4.70) than those who had never married (M = 4.06). Living at home (with parents and grandparents) was also significantly related to stigma (t(397) = 3.39, p = .001), with those living at home reporting less stigma (M = 3.95) than those who did not (M = 4.58). Living at home and marital status were significantly related (χ2(1) = 41.60, p < .001), with most participants who had never married living with family (N = 269, 67.4%) and most participants who had married living elsewhere (N = 31, 7.7%). The ANOVA evaluating the relationship between living situation, marital status, their interaction, and stigma revealed a significant interaction effect (F(1, 395) = 6.98, p = .009), with unmarried individuals living at home and married persons living elsewhere having lower stigma than those who had married but lived at home and those who had never married and lived elsewhere. However, when symptom severity was included in the ANCOVA as a covariate, none of the group differences were significant, nor was the interaction.
Stigma was not significantly related to any other demographic characteristics, including age, gender, race, ethnicity, and education level, nor status as a student. Perceived stigma was marginally significantly related to employment status, with participants who were not working having higher stigma scores (M = 4.20) than those who were working (M = 3.73; t(397) = 1.92, p = .056). However, when symptom severity was statistically controlled in the ANCOVA, the effect of work status on stigma was no longer statistically significant, suggesting that more severe symptoms were uniquely related to employment status but stigma was not.
Diagnoses and Duration of Untreated Psychosis (DUP)
The associations between stigma, primary psychiatric diagnoses, and DUP are presented in Table 2. The t-test comparing the two DUP groups was also significant, with the long DUP group reporting more stigma than the short DUP group.
Table 2.
Associations between Mean Stigma, Diagnosis, and Duration of Untreated Psychosis (N = 399)
| Characteristic | M | SD | df | F | p |
|---|---|---|---|---|---|
| Psychosis diagnosis | 2, 354 | 6.926 | .001 | ||
| Schizophrenia (n = 211) | 4.09 | 1.24 | |||
| Schizoaffective (n = 81) | 4.56 | 1.18 | |||
| Schizophreniform (n = 65) | 3.83 | 1.28 | |||
| Duration of untreated psychosis | 396 | −4.28 | .001 | ||
| < 74 weeks (n = 200) | 3.84 | 1.23 | |||
| ≥ 74 weeks (n = 198) | 4.38 | 4.38 |
Note: One participant was missing duration of untreated psychosis data.
The one-way ANOVA comparing the three psychiatric diagnoses on stigma was significant, with post hoc Tukey tests indicating that participants with schizoaffective disorder reported significantly more stigma than those with schizophrenia or schizophreniform disorder, who did not differ. These results were unchanged when symptom severity was included as a covariate in the ANCOVA.
Clinical Variables
The correlations between perceived stigma and symptoms, well-being, and functioning with and without controlling for psychiatric symptoms are presented in Table 3. Higher perceived stigma was significantly correlated with more severe depression on the CDSS, and more severe symptoms on the PANSS total, as well as more severe symptoms on the PANSS positive, excitement, and depression subscales. Greater stigma was also significantly correlated with lower ratings of well-being (SPWB), recovery (MHRM), overall functioning (QLS total), and social relationships (QLS interpersonal). When partial correlations were computed controlling for symptom severity, stigma continued to be significantly correlated with more severe depression on the Calgary, lower well-being, and lower perceptions of recovery, but was no longer related to symptoms on the PANSS, overall functioning, or interpersonal functioning. Thus, perceived stigma was significantly related to depression, well-being, and recovery independent of symptom severity, but not to other symptoms or functioning.
Table 3.
Correlations between Stigma and Clinical Measures
| Clinical measure | Correlation | Partial Correlation Controlling for PANSSa | ||
|---|---|---|---|---|
| r | p | r | p | |
| .27 | .001 | .19 | .001 | |
| Well-being Scale | −.39 | .001 | −.36 | .001 |
| Mental Health Recovery Scale | −.14 | .004 | −.14 | .007 |
| Quality of Life Scale | ||||
| Interpersonal subscale | −.15 | .003 | −.06 | .272 |
| Instrumental subscale | −.03 | .533 | .05 | .321 |
| Intrapsychic subscale | −.10 | .055 | .03 | .605 |
| Common objects subscale | −.01 | .931 | .07 | .164 |
| Total score | −.12 | .015 | .003 | .951 |
| Positive and Negative Syndrome Scale | ||||
| Positive factor | .20 | .001 | ||
| Negative factor | .04 | .474 | ||
| Disorganization factor | .04 | .481 | ||
| Excitement factor | .18 | .001 | ||
| Depression factor | .26 | .001 | ||
| Total score | .27 | .001 | ||
Note:
Positive and Negative Syndrome Scale total score.
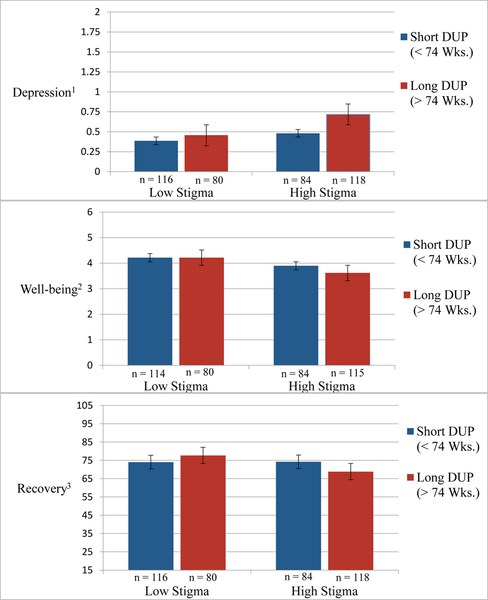
Comparison of the correlations between stigma and depression, well-being, and recovery between the two DUP groups indicated that perceived stigma was more strongly associated with each measure in the long DUP group than the short DUP group. Specifically, for the long vs. short DUP group, the correlations between stigma and depression were r = .29 vs. .17, respectively; for stigma and well-being the correlations were r = −.46 vs. −.27, respectively; and for stigma and recovery the correlations were r = .29 vs. .02, respectively (all rs except .02 significant at p < .001). The differences in the strength of the correlations between the short vs. long DUP groups was statistically significant for stigma and well-being (z = 2.18, p = .015) and recovery (z = 3.21, p = .001), but not for depression (z = −1.26, p = .15). These significant differences were unchanged when controlling for psychiatric symptoms.
In order to illustrate the stronger associations between stigma, depression, and the subjective ratings in the high DUP group than the low DUP group, we used a mean split on the Stigma Scale to divide the entire sample into low or high stigma (M = 4.11). We then created histograms to compare the average depression, well-being, and recovery ratings of participants with high levels of perceived stigma in the high vs. low DUP groups, and participants with low stigma in the two DUP groups. As illustrated in Figure 1, participants in the long DUP group with high levels of stigma had more severe depression on the CDSS, and worse well-being and recovery than similar participants with high stigma in the short DUP group. In contrast, participants in the low stigma group tended to have less severe depression and better subjective functioning regardless of DUP group.
Figure 1. Depression, Well-being, and Recovery Ratings for Participants with Low Perceived Stigma (vs. High) and with Short (vs. Long) Duration of Untreated Psychosis (DUP).
Note: 1Calgary Depression Scale, 2Scales of Psychological Well-Being, 3Mental Health Recovery Measure.
Discussion
Perceived stigma was associated with a broad range of variables in this large, multi-site sample of persons beginning treatment for a first episode of psychosis. Specifically, perceptions of stigma were related to sociodemographic characteristics (living situation, marital status), longer DUP, diagnosis of schizoaffective disorder (vs. schizophrenia or schizophreniform), more severe symptoms (PANSS, CDSS), worse psychosocial functioning (QLS, current employment status), lower subjective well-being (SPWB), and less perceived recovery (MHRM). Individuals who have more severe symptoms may have more social experiences with stigma, raising the question of whether perceptions of stigma merely reflect symptom severity. Indeed, in the present study perceived stigma was related to higher levels of depression on the Calgary, as well as more severe symptoms on the four most socially conspicuous PANSS subscales (Positive, Disorganization, Depression, Excitement); only the Negative subscale was not related to stigma. Statistically controlling for symptom severity rendered the relationships between stigma and sociodemographic characteristics and psychosocial functioning non-significant. However, the associations between stigma and the other variables remained significant after controlling for symptom severity, suggesting that perceptions of stigma may have important clinical implications independent of symptoms.
An important finding was that perceived stigma was significantly associated with a longer DUP. Stigma has long been hypothesized to lead to delays in initiating treatment for mental health conditions,42–44 and meta-synthetic reviews identify either self-stigma or perceived stigma as a common reason for not seeking treatment.45,46 Among persons with an FEP, numerous qualitative studies point to the role of stigma in contributing to a longer DUP.16,19,47–50 However, there is a dearth of quantitative studies addressing this question in persons with FEP.
A recent quantitative study by Kular et al.18 did show that perceived stigma (using the full version of the Stigma Scale30 used in this study) was significantly associated with a longer DUP in a sample of 89 persons beginning treatment for FEP, although data on symptoms were not reported. The present study extends the findings of Kular et al. by demonstrating that perceived stigma is predictive of a longer DUP after controlling for symptom severity. The findings are consistent with anecdotal reports and qualitative studies in the FEP population and suggest that the association between stigma and DUP is not simply an artifact of delays in treatment leading to more severe symptoms and ensuing social experiences with stigma. The results also support efforts targeting the reduction of DUP through public education campaigns aimed at reducing the stigma of mental illness.51,52
In addition to the possible effects of stigma on delaying seeking treatment, the findings suggest that perceived stigma has significant psychological effects on individuals with first episode psychosis, independent of the overall severity of their symptoms. Perceived stigma was significantly related to greater depression, in line with other first episode psychosis studies.22–24 Relatedly, greater levels of perceived stigma were also related to lower subjective well-being and sense of personal recovery, even after controlling for symptom severity. These findings are consistent with other research in first episode psychosis populations showing that higher internalized or perceived stigma are associated with lower levels of well-being,53 satisfaction with life19,21 and family and social relationships,26,54 and defeatist thinking.54
Furthermore, the results suggest that delaying treatment for a first episode of psychosis may have dire effects of the impact of stigma on depression, well-being, and recovery, independent of overall symptom severity. When correlations between perceived stigma and these subjective dimensions were examined separately within the two DUP groups, a clear pattern emerged in which stigma was more strongly associated with worse psychological functioning in the long DUP group than the short DUP group, with the differences in the correlations between the groups significant for well-being and recovery (Table 3). As illustrated in Figure 1, the negative impact of elevated perceptions of stigma on these subjective dimensions appears to be amplified in the long DUP group, suggesting that the effects of stigma on psychological functioning may accumulate over the period of untreated psychosis. Since well-being and recovery are both correlated with depression (rs = −.38, −.14 in this study, respectively), it may be speculated that the long-term impact of stigma on the erosion of subjective well-being and sense of recovery is to increase risk of depression. The significantly higher levels of stigma in participants with a diagnosis of schizoaffective disorder than schizophrenia or schizophreniform disorder, controlling for symptom severity, is also consistent with the cumulative impact of stigma on depression. However, as the data are cross-sectional and the direction of effects cannot be established, other interpretations for the increased associations between stigma and psychological functioning are possible.
Participants in the current study had moderate levels of perceived stigma, with an average score on the abbreviated Stigma Scale of 4.11 (on a 7-point scale, ranging 1–7), indicating slightly more perceived stigma than the midpoint of “neutral” (4). As would be expected when compared to individuals with multiple episodes of mental illness, this level of perceived stigma is somewhat lower than the average level of stigma in the sample of 193 service users (27% schizophrenia-schizoaffective disorder) reported on for the development of the Stigma Scale,30 for which the average score for the total Stigma Scale was 2.23 (on a 5-point scale, ranging 0–4) and for the 6-item abbreviated scale was 2.43, between the “neither agree nor disagree” (2) and “agree” (3) anchors. The level of perceived stigma in this study also appears slightly higher than that reported in the Kular et al. study18 of 89 persons with FEP, where the average rating on the 5-point Stigma Scale was 1.7, between the “disagree” (1) and “neither agree nor disagree” (2) anchors. Interestingly, the DUP of participants in the RAISE-ETP study was somewhat longer (median = 74 weeks) than in the Kular et al. study (median = about 52 weeks), which could account for some of the higher rate of perceived stigma in this study. Overall, the level of perceived stigma in this study appears in line with what would expect based on previous research on the Stigma Scale with multi-episode service users and other FEP populations.
Several limitations of the present study should be noted. Only one measure of perceived stigma was used, and self-stigma was not directly assessed (i.e., the personal endorsement of stigmatizing beliefs about mental illness). Although, these two dimensions of stigma are different, they are moderately strongly correlated with one-another (e.g. r = .67 in one first episode study19), suggesting they both reflect a shared experience related to the stigma of mental illness. In addition, abbreviated versions were used of the Stigma Scale, the SPWB, and the MHRS. This precluded our ability to examine different subscales of the Stigma Scale and the SPWB, and may have compromised the integrity of the scales as they were originally developed. On the other hand, the internal consistency of the abbreviated SPWB was fair, and for the abbreviated Stigma Scale and MHRS it was moderate to high, suggesting that each scale tapped a single construct.
These limitations notwithstanding, several strengths of the present study are also noteworthy. The study sample was a large number of individuals seeking treatment for a first episode of psychosis at their local treatment provider, drawn from 34 community mental health centers located in 21 states across the continental U.S., and thus is broadly representative of the first episode population in this country. Rigorous standardized assessments were conducted to evaluate psychiatric diagnoses and DUP, symptoms, psychosocial functioning, and subjective well-being and recovery. The study is the first to show that perceived stigma is related to DUP in persons with a first episode of psychosis, controlling for the effects of symptom severity. Furthermore, stigma was found to be related to higher depression and worse well-being and sense of recovery after controlling for symptoms, with stronger associations among participants with a longer DUP, suggesting the effects of stigma on psychological functioning are cumulative during the period of time following the onset of symptoms before treatment begins. The findings underscore the importance of increasing the speed at which individuals with a first episode of psychosis can access comprehensive treatment, and highlight the further need for research on interventions targeting the effects of stigma on well-being and psychosocial functioning in this population.55,56
Significant Outcomes and Limitations.
Higher levels of perceived stigma were significantly associated with a longer duration of untreated psychosis when controlling for psychiatric symptoms.
Perceived stigma was significantly related to more severe symptoms, worse psychosocial functioning, and lower subjective well-being and sense of recovery.
When overall symptom severity was statistically controlled, perceived stigma was related to worse depression, and lower well-being and recovery.
Only one (abbreviated) measure of perceived stigma was used and self-stigma was not directly assessed.
Acknowledgements
We thank all of our core collaborators and consultants for their invaluable contributions, without whom this study would not have been possible.
Executive Committee: John M. Kane, M.D., Delbert G. Robinson, M.D., Nina R. Schooler, Ph.D., Kim T. Mueser, Ph.D., David L. Penn, Ph.D., Robert A. Rosenheck, M.D., Jean Addington, Ph.D., Mary F. Brunette, M.D., Christoph U. Correll, M.D., Sue E. Estroff, Ph.D., Patricia Marcy, B.S.N., James Robinson, M.Ed.
NIMH Collaborators: Robert K. Heinssen, Ph.D., ABPP, Joanne B. Severe, M.S., Susan T. Azrin, Ph.D., Amy B. Goldstein, Ph.D.
Additional contributors to design and implementation of NAVIGATE: Susan Gingerich, M.S.W., Shirley M. Glynn, Ph.D., Jennifer D. Gottlieb, Ph.D., Benji T. Kurian, M.D., M.P.H.,
David W. Lynde, M.S.W., Piper S. Meyer-Kalos, Ph.D., L.P., Alexander L. Miller, M.D. Ronny Pipes, M.A., LPC-S.
Additional Collaborators: MedAvante for the conduct of the centralized, masked diagnostic interviews and assessments; the team at the Nathan Kline Institute for data management. Thomas Ten Have and Andrew Leon played key roles in the design of the study, particularly for the statistical analysis plan. We mourn the untimely deaths of both. We gratefully acknowledge the contributions of Haiqun Lin and Kyaw (Joe) Sint to statistical analysis planning and conduct.
We are indebted to the many clinicians, research assistants, and administrators at the participating sites for their enthusiasm and terrific work on the project as well as the participation of the hundreds of patients and families who made the study possible with their time, trust and commitment.
The participating sites include:
Burrell Behavioral Health (Columbia), Burrell Behavioral Health (Springfield), Catholic Social Services of Washtenaw County, Center for Rural and Community Behavior Health New Mexico, Cherry Street Health Services, Clinton-Eaton-Ingham Community Mental Health Authority, Cobb County Community Services Board, Community Alternatives, Community Mental Health Center of Lancaster County, Community Mental Health Center, Inc., Eyerly Ball Iowa, Grady Health Systems, Henderson Mental Health Center, Howard Center, Human Development Center, Lehigh Valley Hospital, Life Management Center of Northwest Florida, Mental Health Center of Denver, Mental Health Center of Greater Manchester, Nashua Mental Health, North Point Health and Wellness, Park Center, PeaceHealth Oregon/Lane County Behavioral Health Services, Pine Belt Mental HC, River Parish Mental Health Center, Providence Center, San Fernando Mental Health Center, Santa Clarita Mental Health Center, South Shore Mental Health Center, St. Clare’s Hospital, Staten Island University Hospital, Terrebonne Mental Health Center, United Services and University of Missouri-Kansas City School of Pharmacy.
This work has been funded in whole or in part with funds from the American Recovery and Reinvestment Act and from NIMH under contract HHSN271200900019C.
This project was conducted with grant funding from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR Grant #90AR5018). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). Results do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government
Footnotes
Data Availability Statement: n/a
References
- 1.Goffman E. Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs, NJ: Prentice Hall; 1963. [Google Scholar]
- 2.Corrigan PW, ed On the Stigma of Mental Illness: Practical Strategies for Research and Social Change. Washington, DC: American Psychological Association; 2005. [Google Scholar]
- 3.Thornicroft G. Shunned: Discrimination against People with Mental Illness. Oxford: Oxford University Press; 2006. [Google Scholar]
- 4.Yanos PT. Written Off: Mental Health Stigma and the Loss of Human Potential. Cambridge, England: Cambridge University Press; 2018. [Google Scholar]
- 5.Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M, INDIGO Study Group. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet. 2009;373:408–415. [DOI] [PubMed] [Google Scholar]
- 6.Stigma Farina A. In: Mueser KT, Tarrier N, eds. Handbook of Social Functioning in Schizophrenia. Boston: Allyn and Bacon; 1998:247–279. [Google Scholar]
- 7.Druss BG, Rosenheck RA, Desai MM, Perlin JB. Quality of preventive medical care for patients with mental disorders. Medical Care. 2002;40:129–136. [DOI] [PubMed] [Google Scholar]
- 8.Pettitt B, Greenhead S, Khalifeh H, et al. At Rsk, Yet Dismissed: The Criminal Victimisation of People with Mental Health Problems. London: Victim Support; 2013. [Google Scholar]
- 9.Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychological Science in the Public Interest. 2014;15:37–70. [DOI] [PubMed] [Google Scholar]
- 10.Hasan AA, Musleh M. Barriers to seeking early psychiatric treatment amongst first-episode psychosis patients: A qualitative study. Issues in Mental Health Nursing. 2017;38:669–677. [DOI] [PubMed] [Google Scholar]
- 11.Mittal D, Drummond K, Blevins D, Curran J, Corrigan PW, Sullivan G. Stigma associated with PTSD: Perceptions of treatment seeking combat veterans. Psychiatric Rehabilitation Journal. 2013;36:86–92. [DOI] [PubMed] [Google Scholar]
- 12.Boonstra N, Klaassen R, Sytema S, et al. Duration of untreated psychosis and negative symptoms--a systematic review and meta-analysis of individual patient data. Schizophrenia Research. 2012;142. [DOI] [PubMed] [Google Scholar]
- 13.Cotter J, Zabel E, French P, Yung AR. Prolonged duration of untreated psychosis: A problem that needs addressing. Early Intervention in Psychiatry. 2017;11:163–168. [DOI] [PubMed] [Google Scholar]
- 14.Perkins DO, Gu H, Boteva K, Lieberman JA. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: A critical review and meta-analysis. American Journal of Psychiatry. 2005;162:1785–1804. [DOI] [PubMed] [Google Scholar]
- 15.Kane JM, Robinson DE, Schooler NR, et al. Comprehensive versus usual care for first episode psychosis: Two-year outcomes from the NIMH RAISE Early Treatment Program. American Journal of Psychiatry. 2016;173:362–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Franz L, Carter T, Leiner AS, Bergner E, Thompson NJ, Compton M,T. Stigma and treatment delay in first-episode psychosis: a grounded theory study. Early Intervention in Psychiatry. 2010;4:46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ho RWH, Chang W-C, Kwong VWY, et al. Prediction of self-stigma in early psychosis: 3-year follow-up of the randomized-controlled trial on extended early intervention. Schizophrenia Research. 2018;195:463–468. [DOI] [PubMed] [Google Scholar]
- 18.Kular A, Perry BI, Brown L, et al. Stigma and access to care in first-episode psychosis. Early Intervention in Psychiatry. 2018. Online. [DOI] [PubMed] [Google Scholar]
- 19.Chen ESM, Chang W-C, Hui CLM, Chan SKW. Self-stigma and affiliate stigma in first-episode psychosis patients and their caregivers. Social Psychiatry and Psychiatric Epidemiology. 2016;51:1225–1231. [DOI] [PubMed] [Google Scholar]
- 20.Birchwood M, Trower PE, Brunet K, Gilbert P, Iqbal Z, Jackson C. Social anxiety and the shame of psychosis: A study in first episode psychosis. Behaviour Research and Therapy. 2006;45:1025–1037. [DOI] [PubMed] [Google Scholar]
- 21.Chio FHN, Mak WWS, Chan RCH, Tong ACY. Unraveling the insight paradox: One-year longitudinal study on the relationships between insight, self-stigma, and life satisfaction among people with schizophrenia spectrum disorders. Schizophrenia Research. 2018;197:124–130. [DOI] [PubMed] [Google Scholar]
- 22.Noyman-Vekslera G, Weinberg D, Fennig S, Davidson L, Shahar G. Perceived stigma exposure in schizophrenia: The key role of self-concept clarity. Self and Identity. 2013;12:663–674. [Google Scholar]
- 23.O’Connor LK, Yanos PT, Firmin RL. Correlates and moderators of stigma resistance among people with severe mental illness. Psychiatry Research. 2018;270:198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zäske H, Linden M, Degner D, et al. Stigma experiences and perceived stigma in patients with first- episode schizophrenia in the course of 1 year after their first in-patient treatment. European Archives of Psychiatry and Clinical Neuroscience. 2018. Online. [DOI] [PubMed] [Google Scholar]
- 25.Firmin RL, Lysaker PH, Luther L, et al. Internalized stigma in adults with early phase versus prolonged psychosis. Early Intervention in Psychiatry. 2018. Online. [DOI] [PubMed] [Google Scholar]
- 26.Lasalvia A, Zoppei S, Bonetto C, et al. The role of experienced and anticipated discrimination in the lives of people with first-episode psychosis. Psychiatric Services. 2014;65:1034–1040. [DOI] [PubMed] [Google Scholar]
- 27.Addington J, Heinssen RK, Robinson DG, et al. Duration of untreated psychosis in community treatment settings in the United States. Psychiatric Services. 2015;66:753–756. [DOI] [PubMed] [Google Scholar]
- 28.Zarate CAJ, Weinstock L, Cukor P, et al. Applicability of tele-medicine for assessing patients with schizophrenia: acceptance and reliability. Journal of Clinical Psychiatry. 1997;58:22–25. [DOI] [PubMed] [Google Scholar]
- 29.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis-I Disorders - Patient Edition (SCID-I/P, Version 2.0). New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 30.King M, Dinos S, Shaw J, et al. The Stigma Scale: Development of a standardised measure of the stigma of mental illness. British Journal of Psychiatry. 2007;190:248–254. [DOI] [PubMed] [Google Scholar]
- 31.Kay SR, Opler LA, Fiszbein A. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophrenia Bulletin. 1987;13:261–276. [DOI] [PubMed] [Google Scholar]
- 32.Wallwork RS, Fortgang R, Hashimoto R, Weinberger DR, Dickinson D. Searching for a consensus five-factor model of the Positive and Negative Syndrome Scale for schizophrenia. Schizophrenia Research. 2012;137:246–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Addington D, Addington J, Maticka-Tyndale E. Assessing depression in schizophrenia: The Calgary Depression Scale. British Journal of Psychiatry. 1993;163(Suppl 22):39–44. [PubMed] [Google Scholar]
- 34.Young SL, Bullock WA. Mental Health Recovery Measure (MHRM). In: Campbell-Orde T, Chamberlin J, Carpenter J, Leff HS, eds. Measuring the Promise: A Compendium of Recovery Measures. Vol II Cambridge, MA: Evaluation Center @ Human Services Research Institute; 2005:36–41. [Google Scholar]
- 35.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology. 1989;57:1069–1081. [Google Scholar]
- 36.Heinrichs DW, Hanlon TE, Carpenter WTJ. The Quality of Life Scale: An instrument for rating the schizophrenia deficit syndrome. Schizophrenia Bulletin. 1984;10:388–396. [DOI] [PubMed] [Google Scholar]
- 37.Addington J, Addington D. Neurocognitive and social functioning in schizophrenia: A 2.5 year follow-up study. Schizophrenia Research. 2000;7:47–56. [DOI] [PubMed] [Google Scholar]
- 38.Bellack AS, Morrison RL, Wixted JT, Mueser KT. An analysis of social competence in schizophrenia. British Journal of Psychiatry. 1990;156:809–818. [DOI] [PubMed] [Google Scholar]
- 39.Bosia M, M. B, Marino E, et al. Influence of catechol-O-methyltransferase Val158Met polymorphism on neuropsychological and functional outcomes of classical rehabilitation and cognitive remediation in schizophrenia. Neuroscience Letters. 2007;417: 271–274. [DOI] [PubMed] [Google Scholar]
- 40.Nahum M, Fisher M, Loewy R, et al. A novel, online social cognitive training program for young adults with schizophrenia: A pilot study. Schizophrenia Research Cognition. 2014;1:e11–e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Siu CO, Harvey PD, Agid O, et al. Insight and subjective measures of quality of life in chronic schizophrenia. Schizophrenia Research Cognition. 2015;2:127–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fink PJ. Stigma and Mental Illness. Washington, DC: American Psychiatric Press; 1992. [Google Scholar]
- 43.Link BG, Cullen FT, Struening EL, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: An empirical assessment. American Sociological Review. 1989;54:400–423. [Google Scholar]
- 44.McGorry PD, Killackey EJ. Early intervention in psychosis: A new evidence based paradigm. Epidemiologia e Psichiatria Sociale. 2002;11:237–247. [DOI] [PubMed] [Google Scholar]
- 45.Clement S, Schauman O, Graham T, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine. 2015;45:11–27. [DOI] [PubMed] [Google Scholar]
- 46.Gronholm PC, Thornicroft G, Laurens KR, Evans-Lacko S. Mental health-related stigma and pathways to care for people at risk of psychotic disorders or experiencing first-episode psychosis: A systematic review. Psychological Medicine. 2017;47:1867–1879. [DOI] [PubMed] [Google Scholar]
- 47.Anderson KK, Fuhrer R, Malla AK. ‘There are too many steps before you get to where you need to be’: Help-seeking by patients with first-episode psychosis. Journal of Mental Health. 2013;22:384–395. [DOI] [PubMed] [Google Scholar]
- 48.Ferrari M, Flora N, Anderson KK, et al. The African, Caribbean and European (ACE) path- ways to care study: A qualitative exploration of similarities and differ- ences between African-origin, Caribbean-origin and European-origin groups in pathways to care for psychosis. BMJ Open. 2015;5:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stewart KD. Factors contributing to engagement during the initial stages of treatment for psychosis. Qualitative Health Research. 2013;23:336–347. [DOI] [PubMed] [Google Scholar]
- 50.Welsh P, Tiffin PA. Observations of a small sample of adolescents experiencing an at-risk mental state (ARMS) for psychosis. Schizophrenia Bulletin. 2012;38:215–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Joa I, Johannessen JO, Auestad BH, et al. The key to reducing duration of untreated first psychosis: Information campaigns. Schizophrenia Bulletin. 2008;34:466–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Melle I, Larsen TK, Haahr U, et al. Reducing the duration of untreated first-episode psychosis: Effects on clinical presentation. Archives of General Psychiatry. 2004;61:143–150. [DOI] [PubMed] [Google Scholar]
- 53.Rüsch N, Angermeyer MC, Corrigan PW. Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. European Psychiatry. 2005;20:529–539. [DOI] [PubMed] [Google Scholar]
- 54.Park SG, Bennett ME, Couture SM, Blanchard JJ. Internalized stigma in schizophrenia: Relations with dysfunctional attitudes, symptoms, and quality of life. Psychiatry Research. 2013;205:43–47. [DOI] [PubMed] [Google Scholar]
- 55.Russinova Z, Rogers ES, Gagne C, Bloch P, Drake K, Mueser KT. A randomized controlled trial of a peer-run anti-stigma photovoice intervention. Psychiatric Services. 2014;65:242–246. [DOI] [PubMed] [Google Scholar]
- 56.Yanos PT, Roe D, Lysaker PH. Narrative enhancement and cognitive therapy: A new group-based treatment for internalized stigma among persons with severe mental illness. International Journal of Group Psychotherapy. 2011;61:577–595. [DOI] [PMC free article] [PubMed] [Google Scholar]