Abstract
Objective:
The purpose of the present study was to detail the patient flow and establish the feasibility of a brief three-week intensive treatment program (ITP) for veterans with PTSD.
Method:
The present study examined data from 648 veterans referred to a non-VA ITP for PTSD from January 2016 to February 2018 to determine the flow of patients into and through the ITP and evaluate individuals’ satisfaction with treatment.
Results:
On average, 25.9 individuals contacted the ITP each month expressing interest in the program. A large proportion of individuals who completed an intake evaluation were accepted (72.2%) into the ITP. Of those accepted, 70.6% ultimately attended the ITP and the vast majority of veterans who attended the ITP completed treatment (91.6%). Logistic regression results suggested that among veterans who were accepted to the program, those who were legally separated or divorced had significantly greater odds of attending the program compared to single veterans. Veterans were highly satisfied with the 3-week ITP and rated Cognitive Processing Therapy components as the most helpful part of the program.
Conclusions:
The present study demonstrates that ITP formats for PTSD are of interest and acceptable to veterans, and that this format allows individuals to receive high doses of EBTs in a short amount of time.
Keywords: Implementation, Feasibility, PTSD Treatment, Veterans, Intensive Treatment
Clinical Impact Statement
Our findings suggest that delivering evidence-based trauma treatments daily as part of a three-week-long intensive treatment program for PTSD is acceptable and that veterans are highly satisfied with this treatment delivery model. Evidence-based treatment completion rates in intensive treatment programs are greater than 90%, and this treatment delivery model allows veterans to receive more than an adequate dose of evidence-based treatment in a short amount of time. Thus, when developing treatment programs for PTSD, practice administrators and clinicians are strongly encouraged to consider developing brief intensive programs in which evidence-based treatments for PTSD are delivered daily for maximum therapeutic benefit.
A recent meta-analysis suggested that approximately 23% of Operation Enduring Freedom and Operation Iraqi Freedom veterans suffer from posttraumatic stress disorder (PTSD; Fulton et al., 2015). Although evidence-based treatments (EBTs), such as Cognitive Processing Therapy (CPT), have been shown to be effective for the treatment of PTSD in veterans (Chard, Schumm, Owens, & Cottingham, 2010; Forbes et al., 2012; Monson et al., 2006), only a relatively small number of veterans receive these treatments. Although research has shown that providers are likely to offer EBTs as first-choice interventions when they are trained in them (Hundt, Harik, Barrera, Cully, & Stanley, 2016), data from outpatient settings in the Department of Veterans Affairs (VA) report the national average for EBT penetration to be around 20% (Sayer et al., 2017). Other studies have suggested that between 6.3% and 11.4% of veterans seen in VA clinics receive EBTs (Mott et al., 2014; Shiner, Drake, Watts, Desai, & Schnurr, 2012). It is important to note that rates of EBT initiation differ greatly by clinic, with VA specialty clinics reporting EBT initiation, defined as attending at least one session, as high as 72% (Keller & Tuerk, 2016). However, research suggests that even among those who initiate treatment, the majority of individuals receiving cognitive behavioral interventions for PTSD discontinue treatment prior to receiving an adequate dose, which has been defined as eight or more sessions (Gutner, Gallagher, Baker, Sloan, & Resick, 2016; Imel, Laska, Jakupcak, & Simpson, 2013; Kehle-Forbes, Meis, Spoont, & Polusny, 2016). Thus, it is important to identify alternative methods to deliver EBTs to improve treatment uptake and completion.
One alternative is to deliver EBTs in intensive treatment programs (ITPs). Through ITPs, veterans have the opportunity to receive EBTs in a shorter amount of time (i.e., 2–3 weeks; Beidel, Frueh, Neer, & Lejuez, 2017; Zalta et al., 2018) compared to outpatient care where EBTs are commonly delivered once per week over several months (Cook et al., 2014; Harvey et al., 2017). Recent research has demonstrated that ITPs can produce similar PTSD symptom reductions to those obtained in relatively highly controlled EBT efficacy trials with weekly therapy sessions (Beidel et al., 2017; Foa et al., 2018; Zalta et al., 2018). Brief ITPs may reduce barriers to treatment that have been identified both in standard outpatient settings and in longer-term residential programs including avoidance, and practical barriers, including employment and transportation (Hundt et al., 2014; Johnson et al., 2016; Keller & Tuerk, 2016). Housing veterans at the treatment facility during the course of an ITP may reduce logistical concerns that are often raised as reasons for not initiating EBTs (Keller & Tuerk, 2016), and may increase veterans’ ability to focus on treatment by reducing psychosocial stressors as well as reducing opportunities for avoidance and missed treatment sessions. Similar to longer-term residential programs, ITPs also provide an opportunity to offer adjunctive treatments that may improve retention, such as mindfulness, yoga, and skills groups (Cushing & Braun, 2018; Staples, Hamilton, & Uddo, 2013). Compared to longer-term residential treatment programs, which often span over the course of several weeks (i.e., 4–12 weeks; Cook et al., 2013), participating in a brief ITP for two to three weeks may be more feasible for veterans, as there is less potential for conflict with other responsibilities, such as family duties or work schedules. Moreover, the short timeframe may seem less daunting for veterans compared to longer-term residential programs or weekly therapy for several weeks and may provide veterans with a sense of being able to accomplish treatment relatively quickly, which in turn may reduce treatment avoidance.
Despite the apparent advantages of intensively-delivered EBTs for PTSD, it is currently unclear whether veterans are interested in the ITP format, whether or not it is feasible for most veterans to attend and complete a 3-week program, and whether veterans who attend are satisfied with the ITP format. To our knowledge, no study to date, including those focused on longer-term residential treatment programs, has yet detailed the patient flow to and through intensive treatment programs for PTSD. Moreover, little is known about predictors of treatment initiation in the context of intensively delivered treatments. Patient characteristics, such as younger age (specifically veterans who served in Afghanistan or Iraq) have been shown to be associated with lower EBT initiation and completion (Keller & Tuerk, 2016; Mott et al., 2014). However, it is possible that different patient characteristics may impact initiation of traditional outpatient treatment compared to intensive treatments.
Given the lack of prior studies examining this important area, we conducted a feasibility study of an existing 3-week non-VA CPT-based ITP. The ITP offers PTSD treatment for individuals affected by combat or military sexual traumas and has been shown to produce large effects comparable to those produced by PTSD treatment efficacy research (Zalta et al., 2018). Moreover, symptom improvements achieved over the course of the 3-week-long treatment period have been shown to be maintained long-term for up to 12 months (Held et al., under review). To determine the feasibility of this ITP model, we focused on and evaluated several key criteria proposed by Bowen and colleagues (Bowen et al., 2009), including treatment demand, the acceptability of the ITP, and the practicality of treatment. Specifically, we examined the expressed interest (demand), actual program attendance (practicality), the extent to which veterans attended different program components (practicality), and barriers to treatment and satisfaction with different ITP components (acceptability).
Methods
Participants
Data for the present study was collected from service members and veterans (hereafter referred to as veterans) who requested an evaluation to participate in a non-VA 3-week ITP for PTSD housed within the Road Home Program: Center for Veterans and Their Families at Rush University Medical Center in Chicago, IL from January 2016 to February 2018. This philanthropically-funded program offers free outpatient and intensive mental health treatment services regardless of individuals’ service duration and their military discharge status. This study was approved by the Institutional Review Board at Rush University Medical Center with a waiver of consent because all assessments were collected as part of routine care. Table 1 contains demographic characteristics, service history, and prior treatment information of veterans who requested a clinical evaluation for the ITP (N = 648).
Table 1.
Descriptive statistics and group comparisons of demographic characteristics.
| Not Accepted into ITP | Accepted into ITP but Did Not Attend | Accepted into ITP and Attended (including treatment non-completers) | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | χ2 | p | |
| Gender | - | - | - | - | - | - | 3.17 | .205 |
| Female | 87 | 28.0 | 27 | 27.3 | 82 | 34.5 | - | - |
| Male | 224 | 72.0 | 72 | 72.7 | 156 | 65.5 | - | - |
| Race | - | - | - | - | - | - | 8.17 | .613 |
| American Indian/Alaska Native | 5 | 1.6 | 0 | 0.0 | 6 | 2.5 | - | - |
| Asian | 6 | 1.9 | 1 | 1.0 | 1 | 0.4 | - | - |
| Black/African American | 64 | 20.6 | 16 | 16.5 | 45 | 18.9 | - | - |
| Native Hawaiian/Pacific | 4 | 1.3 | 0 | 0.0 | 4 | 1.7 | - | - |
| Islander | ||||||||
| White | 199 | 64.2 | 69 | 71.1 | 159 | 66.8 | - | - |
| Other | 32 | 10.3 | 11 | 11.3 | 23 | 9.7 | - | - |
| Ethnicity | - | - | - | - | - | - | 1.79 | .409 |
| Hispanic/Latino | 52 | 16.7 | 22 | 22.4 | 46 | 19.4 | - | - |
| Not Hispanic/Latino | 259 | 83.3 | 76 | 77.6 | 191 | 80.6 | - | - |
| Marital Status | - | - | - | - | - | - | 14.65 | .023* |
| Single | 83 | 26.7 | 34 | 34.3 | 43 | 18.1 | - | - |
| Legally Separated/Divorced | 82 | 26.4 | 17 | 17.2 | 69 | 29.0 | - | - |
| Partnered/Married | 145 | 46.6 | 47 | 47.5 | 123 | 51.7 | - | - |
| Widowed | 1 | 0.3 | 1 | 1.0 | 3 | 1.3 | - | - |
| Children | - | - | - | - | - | - | 4.46 | .108 |
| Yes | 215 | 69.1 | 64 | 64.6 | 179 | 75.2 | - | - |
| No | 96 | 30.9 | 35 | 35.4 | 59 | 24.8 | - | - |
| Employment Status | 17.93 | .022* | ||||||
| Employed | 46 | 14.8 | 28 | 28.6 | 42 | 17.6 | - | - |
| Out of work/Looking for work | 188 | 60.6 | 50 | 51.0 | 149 | 62.6 | - | - |
| Retired | 18 | 5.8 | 2 | 2.0 | 12 | 5.0 | - | - |
| Student | 15 | 4.8 | 9 | 9.2 | 8 | 3.4 | - | - |
| No response | 18 | 13.9 | 0 | 9.2 | 0 | 11.3 | ||
| Last/Current Military Pay Grade | - | - | - | - | - | - | 7.23 | .124 |
| E1–E3 | 38 | 12.2 | 11 | 11.3 | 26 | 10.9 | - | - |
| E4–E9 | 257 | 82.6 | 74 | 76.3 | 199 | 83.6 | - | - |
| Officer | 16 | 5.1 | 12 | 12.4 | 13 | 5.5 | - | - |
| Branch of Service | - | - | - | - | - | - | 9.41 | .309 |
| Air Force | 22 | 7.1 | 8 | 8.1 | 20 | 8.4 | - | - |
| Army | 213 | 68.5 | 61 | 61.6 | 158 | 66.4 | - | - |
| Coast Guard | 1 | 0.3 | 0 | 0.0 | 3 | 1.3 | - | - |
| Marines | 39 | 12.5 | 22 | 22.2 | 33 | 13.9 | - | - |
| Navy | 36 | 11.6 | 8 | 8.1 | 24 | 10.1 | - | - |
| Post-9/11 | - | - | - | - | - | - | 4.14 | .126 |
| Yes | 293 | 94.2 | 91 | 91.9 | 213 | 89.5 | - | - |
| No | 18 | 5.8 | 8 | 8.1 | 25 | 10.5 | - | - |
| Service Status | - | - | - | - | - | - | .48 | .786 |
| Currently Serving | 11 | 3.5 | 5 | 5.1 | 10 | 4.2 | - | - |
| Not Currently Serving | 300 | 96.5 | 94 | 94.9 | 228 | 95.8 | - | - |
| Not Accepted into ITP | Accepted into ITP but Did Not Attend | Accepted into ITP and Attended | ||||||
| M | SD | M | SD | M | SD | F | p | |
| Age | 38.5 | 8.8 | 37.4 | 9.4 | 40.2 | 9.3 | 4.19 | .016* |
Note: n = 648 for Gender, Marital Status, Children, Branch of Service, Post 9/11, and Service Status. n = 646 for Ethnicity and Last/Current Military Pay Grade. n = 645 for Race. ITP = Intensive Treatment Program.
p < .05.
Procedures
Recruitment.
The program’s main referral source was Wounded Warrior Project, which announced the ITP to its alumni via email, advertised the ITP on television and billboards, and evaluated and referred veterans who contacted their resource center. The ITP was also advertised online through the Road Home Program’s website and veteran outreach coordinators connected with local and national community partner organizations, including VAs, to provide information about the program.
ITP Eligibility and Evaluation.
All veterans underwent an intake evaluation with a licensed clinician (i.e., psychologist or social worker) or a clinician who was practicing under the license of another clinician (i.e., psychology postdocs, social workers who were working toward their clinical license). The intake evaluations occurred over at least two 90-minute sessions and included an overview of the ITP and a general bio-psycho-social and diagnostic assessment. In addition, the intake clinician administered the Clinician-Administered PTSD Scale (Weathers et al., 2013) to determine whether the veteran met the diagnostic criteria for PTSD (American Psychiatric Association, 2013), which is one of the key eligibility requirements for admission to the ITP. Most veterans who expressed interest in the ITP were non-local and intake evaluations, including the administration of the Clinician Administrated PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2013), frequently occurred over the phone. Exclusion criteria for the ITP included clinical issues that would require a higher level of care, such as active suicidality or homicidality in the past three months; engagement in severe non-suicidal self-harm in the past three months; mania or psychosis; eating disorders that would place the individual at medical risk; or substance use that would interfere with ability to participate. Veterans were also excluded if the clinician determined during the intake evaluation that current medical, legal, or other psychosocial issues would interfere with treatment. No specific measures were used to assess the exclusion criteria. Following the completed intake evaluations, a multidisciplinary treatment team, which included the psychologists, psychiatrists, and social workers, decided whether or not the individual was eligible to participate.
ITP Overview.
To reduce as many logistical barriers as possible, veterans who were accepted for treatment were provided transportation to and from the ITP and housing near the treatment facility at no cost to them. The ITP is based on a cohort model, with each cohort consisting of approximately 12 individuals. The program offers a combat trauma track and a military sexual trauma track based on the individuals’ index trauma. Each treatment day lasted from 08:00–17:00, with a one-hour lunch break, and four 15-minute breaks between activities. The core interventions of the ITP are Cognitive Processing Therapy (CPT; Resick, Monson, & Chard, 2016), an adaptation of Mindfulness-Based Stress Reduction (Kabat-Zinn, 2003), and yoga. During the 3-week ITP, individuals are scheduled for 14 50-minute sessions of individual CPT, 13 120-minute sessions of group CPT, 13 75-minute sessions of mindfulness, and 12 50-minute sessions of yoga in addition to several other 60-minute educational classes on relevant topics. The primary goal of the ITP is to help individuals recognize and learn how challenge maladaptive trauma-related beliefs through Socratic questioning and completing worksheets that takes place during individual and group CPT sessions. Mindfulness and yoga sessions are intended to offer individuals additional skill sets to cope with overwhelming emotions. ITP participants have the option meet with a psychiatric provider for medication management. Legal, financial, and other psychosocial needs are addressed through meetings with a case manager. We have detailed elsewhere (cf. Zalta et al., 2018) that the ITP is effective for reducing PTSD and depression symptoms; we have demonstrated that the participation in the ITP described here results in large and clinically meaningful reductions in PTSD (d = 1.40) and depression symptoms (d = 1.04). See Zalta et al., 2018 for a detailed description of treatment services and clinical outcomes.
ITP Satisfaction Survey.
Following treatment completion, veterans were asked to complete an anonymous satisfaction survey to evaluate the ITP. This survey assessed obstacles to receiving care, overall experience of the program, and experience of specific treatment components using a 5-point scale ranging from 1 (Strongly disagree/Not at all helpful) to 5 (Strongly agree/Extremely helpful). The survey also contained questions about the length of the program, and open-ended questions about program components that participants found most or least helpful.
Data Analysis
We used SPSS 22.0 and Stata 15 for all analyses. We performed descriptive statistics to evaluate ITP demand, practicality, and acceptability. We were then interested in exploring factors predictive of patient flow through the program (i.e., predictors of acceptance to the program and predictors of attendance after acceptance to the program). We first examined bivariate associations between demographic variables of interest and patient status (not accepted, accepted but did not attend, accepted and attended). All variables that were significantly bivariate predictors were included in two separate logistic regression analyses examining ITP acceptance (outcome 1; 0 = not accepted; 1 = accepted) or attendance (outcome 2; 0 = did not attend; 1 = attended). Analyses were re-conducted to examine alternate reference categories for categorical predictors. Goodness of fit for logistic regression models was assessed using McFadden’s pseudo-R2 which is based on log likelihood (McFadden, 1974). Finally, to examine satisfaction with the program, study authors met to review the qualitative feedback that was provided in response to the open-ended questions in the satisfaction survey. Study authors selected quotes which appeared to accurately represent experiences shared by ITP participants.
Results
ITP Demand
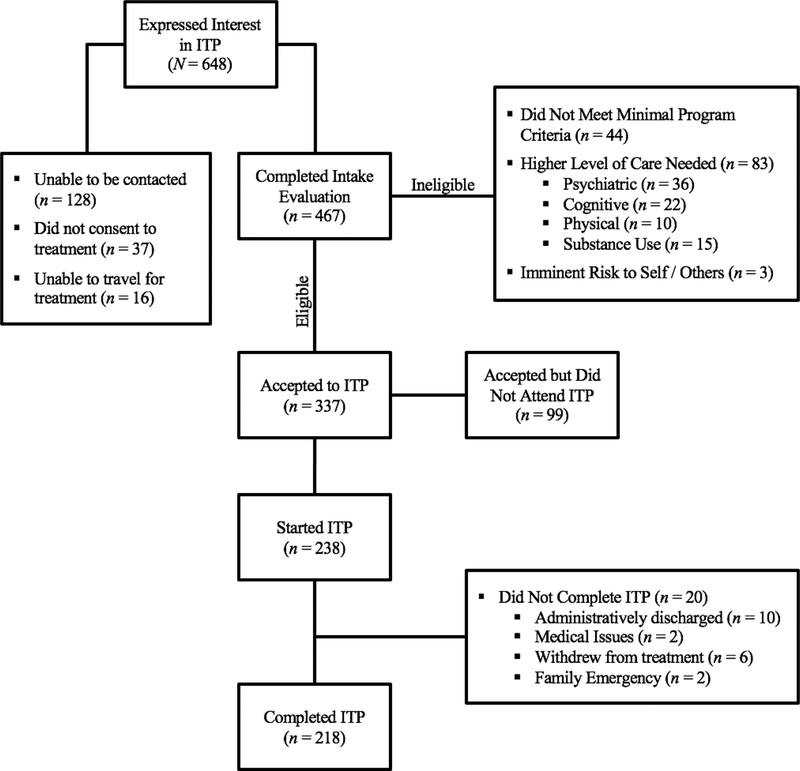
Figure 1 details the patient flow through the program from initial interest in the ITP to program completion. From January 2016 to February 2018, 648 veterans (on average 25.9 individuals per month) expressed initial interest in receiving ITP treatment and contacted the program to schedule an intake evaluation. Of the 648 veterans who expressed initial interest, 66.8% of the sample reported hearing about the program through the Wounded Warrior Project, followed by the 12.8% through the VA, 11.1% through peers, friends, and family members, 4.8% through social media, and 4.5% through other sources. Of those who expressed interest in the program, 467 veterans (72.1% of those referred) completed an intake evaluation and were considered for participation in the ITP and 337 out of these 467 individuals (72.2%) were accepted into the ITP. Of the 337 individuals who were accepted, 99 (29.4%) did not attend treatment for mostly unknown reasons (e.g., lack of contact with program staff, scheduling conflicts, etc.). For those who attended the ITP, the average time between the initial call to the program and the start of the ITP was 13.84 weeks (SD = 9.04; median = 12.43 weeks). Figure 1 is an acceptance flowchart, which details veteran-reported reasons for not completing intakes or the program itself, as well as clinician-reported reasons for not accepting veterans into the program.
Figure 1.
ITP flowchart.
ITP Practicality: Treatment Attendance and Dose
Of the 238 veterans who started treatment, 218 (91.6%) completed treatment. Reasons for non-completion including reasons for administrative discharge are reported in Figure 1. We also evaluated the extent to which veterans attended the core treatment components. On average, the ITP completers attended 13.07 of 14 sessions of individual CPT (SD = 2.24; mode = 14), 12.27 of 13 sessions of group CPT (SD = 1.49; mode = 13), 11.75 of 13 sessions of mindfulness (SD = 1.74; mode = 13), and 10.12 of 12 sessions of yoga (SD = 1.97; mode = 10). ITP participants did not attend various sessions due to health reasons, conflicting external appointments, and feeling tired. Of all individuals who started the ITP, including those who ultimately did not complete the program, only 5.0% (n = 12) did not attend at least eight ITP treatment days.
Table 1 reports initial tests of association between demographic variables and acceptance into the ITP and attendance following acceptance. Specifically, comparisons were examined for veterans who were not accepted, those who were accepted but did not attend, and those who were accepted and attended (including non-completers). Results of the initial tests of association suggested that those who were accepted and attended the program were older, and that differences also existed based on employment and marital status. Table 2 presents the results of logistic regression analyses examining these statistically significant demographic characteristics (i.e., marital status, employment status, and age) as predictors of program acceptance and attendance following acceptance (see Table 2). None of the demographic variables significantly predicted acceptance into the program (χ2(6) = 7.62, p = .27, R2 = .001). Marital status significantly predicted attendance among those who were accepted (χ2(6) = 25.47, p < .001, R2 = .071). Specifically, veterans had significantly greater odds of attending than if they were divorced or separated than single. Older applicants, those who were married, and those who were out of work relative to being employed or students also had a greater likelihood of attending, though these variables did not reach statistical significance (ps = .056 to .075).
Table 2.
Logistic regressions predicting acceptance into the ITP and attendance among accepted veterans.
| Acceptance into ITP | Attendance among accepted | |||
|---|---|---|---|---|
| Predictor | OR (95% CT) | p | OR (95% CI) | p |
| Marital Status | ||||
| Single (reference) | -- | -- | ||
| Separated/Divorced | 1.19(0.79–1.79) | .403 | 2.98(1.37–6.45) | .006* |
| Partnered/Married | 0.83 (0.52–1.32) | .425 | 1.76(0.94–3.29) | .079 |
| Employment Status | ||||
| Out of work (reference) | -- | -- | ||
| Employed | 1.48(0.96–2.28) | .075 | 0.58(0.32–1.06) | .075 |
| Retired | 0.64(0.30–1.37) | .250 | 1.51(0.31–7.26) | .606 |
| Student | 1.12(0.53–2.36) | .770 | 0.35(0.12–1.04) | .059 |
| Age | 1.00(0.98–1.02) | .893 | 1.04(1.00–1.08) | .056 |
Note: OR represents Odds Ratio for acceptance or attendance based on demographic factor. Acceptance into ITP: 0 = not accepted; 1 = accepted. Attendance among accepted: 0 = did not attend; 1 = attended. Marital status ‘widowed’ and employment status ‘no response’ were excluded due to low numbers across all groups.
represents p < .05. No significant differences were found between non-reference categories for marital or employment status in either analysis.
ITP Acceptability: Barriers to Care and Satisfaction with Treatment
A total of 213 veterans (97.7% of ITP completers) completed the satisfaction survey. The majority of participants (69.5%) indicated no barriers to receiving care in the ITP. Financial barriers (15.0%), childcare (9.4%), and distance from home (7.0%) were the most commonly perceived barriers (individuals were able to select more than one barrier). Perceived stigma was reported to be relatively low among ITP completers with 63.4% disagreeing or strongly disagreeing that they worry other veterans would see them as weak for seeking treatment, and 79.3% agreeing or strongly agreeing with feeling comfortable to let family and friends know they received care in the ITP. Participants reported high satisfaction with the ITP, with 96.2% of individuals either agreeing or strongly agreeing with feeling satisfied with the clinical care they received, and 91.6% agreeing or strongly agreeing that the ITP had improved the problems they needed help with. Regarding the three-week timeframe, 68.3% indicated that it was “Just right”, 30.3% found it “Too short”, and 1.4% reported it “Too long”.
Regarding the specific program components, individual and group CPT was rated as either quite helpful or very helpful by 96.3% and 93.9% of the sample, respectively. Mindfulness and yoga were rated as quite helpful or very helpful by 62.4%, and 64.3%, respectively. Group CPT was most commonly selected as the most helpful aspect of the treatment (48.1%), followed by individual CPT (43.4%). Means and standard deviations of satisfaction ratings are displayed in Table 3. Based on the free text responses, the main criticism voiced by a minority of ITP completers was the length of the treatment days; individuals suggested that each treatment day should be shortened to allow for more free time, even if this would require the ITP to be longer (e.g., four weeks). Table 4 provides exemplars of descriptive responses the participants provided.
Table 3.
Means and standard deviations of ITP satisfaction ratings.
| Prompt | Mean (SD) | Mode |
|---|---|---|
| Overall, I feel satisfied with the clinical care I received.a | 4.78 (0.66) | 5 |
| The care I received has helped me function better in my life.a | 4.55 (0.79) | 5 |
| Knowing there is a fellow veteran that I can talk to at the program is important to me.a | 4.72 (0.75) | 5 |
| I have confidence and trust in the clinicians I met with.a | 4.74 (0.68) | 5 |
| The help I received has made a difference in my life.a | 4.65 (0.76) | 5 |
| The care I received has improved the problems I needed help with.a | 4.56 (0.78) | 5 |
| The program has helped me gain skills to better handle challenges in my life.a | 4.63 (0.75) | 5 |
| The program helped me overcome barriers to seek the care I needed.a | 4.62 (0.80) | 5 |
| I feel comfortable letting my family/friends know I received care at the program.a | 4.33(1.10) | 5 |
| I worry other service members/veterans see me was weak for seeking treatmenta | 2.28(1.53) | 1 |
| If I meet another veteran who is having a difficult time, I will recommend the program.a | 4.87 (0.64) | 5 |
| How helpful was individual CPT?b | 4.87 (0.50) | 5 |
| How helpful was the CPT group?b | 4.77 (0.63) | 5 |
| How helpful was the mindfulness group?b | 3.74(1.44) | 5 |
| How helpful was yoga?b | 3.89(1.31) | 5 |
| How helpful was case management?b | 4.41 (0.89) | 5 |
| How helpful was medication management?b | 4.13(1.27) | 5 |
| How helpful was nutrition and fitness?b | 3.83(1.36) | 5 |
| How helpful was the family/relationship group?b | 3.87(1.30) | 5 |
| How helpful was the sleep hygiene group?b | 3.51 (1.40) | 5 |
| How helpful was art therapy?b | 4.45(1.01) | 5 |
Note.Rating scale: 1 = Strongly disagree; 5 = Strongly agree;
Rating scale: 1 = Not at all helpful; 5 = Extremely helpful.
Table 4.
Exemplar qualitative feedback from ITP participants.
| What part of your treatment did you find most helpful? Why? | |
| |
| Was talking or writing about the details of your trauma an important part of your treatment? Why or why not? | |
| |
| What did you like best about the ITP? | |
| |
| What did you like least about the ITP? | |
| |
Discussion
The present study suggests that a large number of veterans are interested in receiving a three-week intensive treatment for PTSD. On average, more than one veteran contacted the program per business day each month to initiate an intake. Moreover, only 7.1% of veterans who expressed initial interest and spoke with an intake clinician declined to participate in the ITP after learning about the structure of the program. Anecdotally, the compressed time schedule appealed to many veterans who expressed that they were lacking progress in their routine outpatient care. Only 3.1% of veterans who were evaluated explicitly declined to participate for logistical reasons, which is much lower compared to rates reported for some outpatient PTSD specialty clinics in the VA (e.g., Keller & Tuerk, 2016). However, it is possible that the rate of individuals who decline participation in an ITP might be higher if travel, housing, and treatment costs are not fully covered by the treatment facility.
The overall acceptance rate of veterans who completed an intake evaluation was high (72.2%). The majority of veterans who were not accepted into the program presented with clinical features that indicated a higher level of care for psychiatric, substance use, cognitive, or physical and other medical issues was warranted; this represented only 17.8% of all veterans evaluated. The second most common reason for non-acceptance was not meeting the minimal program criteria (e.g., did not meet the diagnostic criteria for PTSD on the CAPS-5); this represented 9.4% of all veterans evaluated. Although our analyses suggested that none of the demographic factors were statistically significant predictors of acceptance into the program, individuals who were employed had slightly greater odds of being accepted compared those who were out of work. This is likely because those who required a higher level of care than our ITP due to the severity of their symptoms would have a hard time maintaining employment.
Treatment initiation following acceptance into the program was high compared to standard outpatient care (Keller & Tuerk, 2016; Mott et al., 2014); only 29.4% of individuals who were accepted into the ITP did not present for treatment. Because the vast majority of these individuals were lost to contact, which is relatively common for veterans who are accepted for treatment but choose not to begin care (Keller & Tuerk, 2016), we were unable to inquire about their reasons for not attending the program. Marital status emerged as the only statistically significant predictor of program attendance following acceptance. Specifically, being legally separated or divorced significantly increased the odds of attending the ITP compared to being single. It is plausible that the legal separation or divorce may function as a motivator to attend PTSD treatment, potentially to mend a severed relationship with a partner and/or children. Notably, individuals who were partnered or married also had greater odds of attending the ITP following acceptance compared to those who are single, though this finding was only marginally significant when adjusting for age and employment status. Our findings corroborate the notion that being or having been in a committed relationship is a protective factor against pre-treatment dropout (e.g., Mott et al., 2014).
We identified several additional predictors of program attendance that were only marginally significant. Specifically, we found that veterans who were employed or students at the time of the intake evaluation were slightly less likely to attend the program compared to those currently out of work and younger age increased the risk of non-attendance. Thus, our findings suggest that age, marital status, and employment status may each have an impact on treatment initiation, though further research is needed to disentangle the relative contributions of these factors. Moreover, additional research is needed to examine strategies that would help to retain veterans that have been accepted in ITP treatments to reduce pre-treatment dropout. For example, single veterans who are at greater risk of not attending the program following acceptance may benefit from a connection with other single peers who have attended and successfully completed the treatment program to help provide accountability and overcome any perceived barriers that may prevent them from attending. It may also be helpful to explore how to reduce potential barriers experienced by those currently employed or students to ensure they are able to receive effective treatment.
The majority of veterans who started the ITP completed treatment (91.6%) and nearly two-thirds of individuals who did not complete the ITP still received an adequate dose of 8 or more EBT sessions. These rates are higher than those commonly reported for outpatient clinics (e.g., Gutner, Gallagher, Baker, Sloan, & Resick, 2016; Imel, Laska, Jakupcak, & Simpson, 2013; Wang et al., 2005) and suggests that EBTs delivered daily are tolerable for the majority of individuals and may be one way to ensure that veterans receive adequate treatment doses. Notably, the ITP completion rate was much higher than EBT completion rates in standard outpatient care (approximately 40%; Kehle-Forbes et al., 2016). It is possible that rapid symptom improvement may encourage patients to stay in treatment, although it is also possible that access to a multitude of services in the ITP, low logistical barriers due to all treatment costs covered by the program, high cohort cohesion, limited opportunities for avoidance, and/or reduced distractions may have contributed to high ITP completion rates. Future research should examine which aspects of ITP delivery drive adherence and also impact outcomes.
Our data suggest that veterans who completed the program were highly satisfied with the ITP model. Interestingly, individual and group CPT were ranked as the most helpful aspects of the program by the majority of veterans. However, it is notable that veterans reported less satisfaction with mindfulness compared to CPT. Based on the open text responses, it appears that veterans like the group format because they value input from their peers and are able to recognize that they are not alone in their struggles. A point of criticism from a minority of ITP completers was that the treatment days were too long. This is consistent with the finding that one-third of participants reported that the treatment was too short. Future studies should examine how changes to the treatment length may affect patient satisfaction, feasibility, and effectiveness of the ITP.
Those who completed the ITP reported relatively few barriers to care, with financial, childcare, and travel as the most commonly cited barriers. In most cases, individuals were nonlocal and completed their intake evaluation over the phone, indicating that the distance from intake providers or treatment centers is not necessarily a barrier to completing intake evaluations or interest in the program overall. It is important to note that 59.7% of the all 648 veterans who initially contacted the program reported being out of work and looking for work, which may have contributed to being able to attend a three-week long program. Indeed, our findings suggested that employed veterans were slightly less likely to attend than those who were out of work, though this was only marginally significant. Moreover, data regarding treatment barriers were only collected from individuals who attended and completed the ITP. It is possible that some barriers associated with ITP treatment impacted veterans’ ability to complete the intake process or attend the program. Overall, the ITP model appears capable of addressing practical barriers that might impede individuals’ progress in routine outpatient care.
Despite the encouraging findings, several limitations need to be considered. First, as mentioned, all costs associated with services, including travel, housing, and food, were covered by the organization. Barriers related to costs or insurance coverage may be more salient in other treatment contexts. Second, Wounded Warrior Project, which is one of the program’s main referral sources, knew the specific inclusion criteria for the program and attempted to refer individuals who were likely a good fit. Thus, the acceptance rate for this program may be higher compared to others whose referral sources may not be aware of specific program eligibility criteria. Third, because veterans self-selected to inquire about the ITP treatment, it cannot be assumed that findings from this study generalize to all veterans with PTSD. Fourth, the satisfaction data presented in this study may be artificially high given that only ITP completers provided satisfaction data.
Conclusion
The present study demonstrates that ITP formats for PTSD are of interest and feasible for a large number of veterans, and that this format allows individuals to receive high doses of EBTs in a short amount of time. Despite the effectiveness and high satisfaction associated with the ITP model, not every individual who expressed interest received treatment. We identified key timepoints at which individuals drop off (i.e., before completing the intake evaluation and following acceptance into the program). Future research should examine clinical characteristics that may predict pre-treatment attrition and identify ways to increase continued engagement so that more veterans can receive effective care. Given the similarities in the structure of brief ITPs, such as the one presented in this manuscript, and residential PTSD treatment programs (i.e., delivery of EBTs, utilization of adjunctive services, provided housing, etc.), additional research is needed to establish whether these types of programs differ significantly from one another with regards to patient flow and satisfaction ratings. Another important area for future research involves assessing clinical outcomes and participants’ ability to maintain symptom gains long-term. Specifically, it will be important to determine if individuals are able to generalize the skills learned over the course of highly structured intensive treatments to their everyday lives. Finally, feasibility has been defined in a multitude of ways (Bird et al., 2014; Bowen et al., 2009) and the present study was only able to address a subset of the feasibility criteria. Future research should examine other important aspects including cost and general financial considerations, staff training, and sustainability to more comprehensively examine the feasibility as well as the limitations of ITPs.
Acknowledgments
We thank the Wounded Warrior Project for their support of the Warrior Care Network and the resulting research. We would also like to thank the participating veterans and their families, as well as acknowledge the administrators, research assistants, and clinicians at the Road Home Program. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, Wounded Warrior Project, or any other funding agency.
Philip Held receives grant support from the Boeing Company and the Robert R. McCormick Foundation. Alyson Zalta is supported by a career development award from the National Institute of Mental Health (K23 MH103394). Shannon Wiltsey Stirman receives funding from the National Institute of Mental Health and the Canadian Institute of Health Research. Mark Pollack receives support from the Wounded Warrior Project and research funding from National Institute of Health and Janssen Pharmaceuticals; he provides consultation to Aptinyx, Clintara, and Palo Alto Health Sciences; he has equity in Argus, Doyen Medical, Mensante Corporation, Mindsite, and Targia Pharmaceuticals; he receives royalties from SIGH-A, SAFER interviews. Niranjan Karnik receives grant support from Welcome Back Veterans, an initiative of the Robert R. McCormick Foundation and Major League Baseball, the Substance Use & Mental Health Services Administration; the National Institute on Drug Abuse; and the National Center for Advancing Translational Science of the National Institutes of Health (UL1-TR002398). All other authors declare that they have no competing interests.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington D.C.: American Psychiatric Association; 10.1176/appi.books.9780890425596.744053 [DOI] [Google Scholar]
- Beidel DC, Frueh BC, Neer SM, & Lejuez CW (2017). The efficacy of Trauma Management Therapy: A controlled pilot investigation of a three-week intensive outpatient program for combat-related PTSD. Journal of Anxiety Disorders, 50, 23–32. 10.1016/j.janxdis.2017.05.001 [DOI] [PubMed] [Google Scholar]
- Bird VJ, Boutillier C Le, Leamy M, Williams J, Bradstreet S, & Slade M (2014). Evaluating the feasibility of complex interventions in mental health services: Standardised measure and reporting guidelines. British Journal of Psychiatry, 204(04), 316–321. 10.1192/bjp.bp.113.128314 [DOI] [PubMed] [Google Scholar]
- Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, … Fernandez M (2009). How we design feasibility studies. American Journal of Preventive Medicine, 36(5), 452–457. 10.1016/j.amepre.2009.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chard KM, Schumm JA, Owens GP, & Cottingham SM (2010). A comparison of OEF and OIF veterans and Vietnam veterans receiving Cognitive Processing Therapy. Journal of Traumatic Stress, 23(1), 25–32. 10.1002/jts.20500 [DOI] [PubMed] [Google Scholar]
- Cook JM, Dinnen S, Simiola V, Bernardy N, Rosenheck R, & Hoff R (2014). Residential treatment for posttraumatic stress disorder in the Department of Veterans Affairs: A national perspective on perceived effective ingredients. Traumatology, 20(1), 43–49. 10.1037/h0099379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook JM, O’Donnell C, Dinnen S, Bernardy N, Rosenheck R, & Hoff R (2013). A formative evaluation of two evidence-based psychotherapies for PTSD in VA residential treatment programs. Journal of Traumatic Stress, 26(1), 56–63. 10.1002/jts.21769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cushing RE, & Braun KL (2018). Mind–body therapy for military veterans with post-traumatic stress disorder: A systematic review. Journal of Alternative and Complementary Medicine, 24(2), 106–114. 10.1089/acm.2017.0176 [DOI] [PubMed] [Google Scholar]
- Foa EB, McLean CP, Zang Y, Rosenfield D, Yadin E, Yarvis JS, … Peterson AL (2018). Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel. JAMA, 319(4), 354–364. 10.1001/jama.2017.21242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes D, Lloyd D, Nixon RDVDV, Elliott P, Varker T, Perry D, … Creamer M (2012). A multisite randomized controlled effectiveness trial of cognitive processing therapy for military-related posttraumatic stress disorder. Journal of Anxiety Disorders, 26(3), 442–452. 10.1016/j.janxdis.2012.01.006 [DOI] [PubMed] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, … Beckham JC (2015). The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans: A meta-analysis. Journal of Anxiety Disorders, 31, 98–107. 10.1016/j.janxdis.2015.02.003 [DOI] [PubMed] [Google Scholar]
- Gutner CA, Gallagher MW, Baker AS, Sloan DM, & Resick PA (2016). Time course of treatment dropout in cognitive–behavioral therapies for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 8(1), 115–121. 10.1037/tra0000062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey MM, Rauch SAM, Zalta AK, Sornborger J, Pollack MH, Rothbaum BO, … Simon NM (2017). Intensive treatment models to address posttraumatic stress among post-9/11 warriors: The Warrior Care Network. FOCUS, 15(4), 378–383. 10.1176/appi.focus.20170022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Held P, Zalta AK, Smith DL, Boley RA, Brennan MBA, Van Horn R, … Pollack MH (n.d.). Short-, medium-, and long-term outcomes of a cognitive processing therapy-based three-week intensive PTSD treatment program for veterans. [DOI] [PMC free article] [PubMed]
- Hundt NE, Harik JM, Barrera TL, Cully JA, & Stanley MA (2016). Treatment decision-making for posttraumatic stress disorder: The impact of patient and therapist characteristics. Psychological Trauma: Theory, Research, Practice, and Policy, 8(6), 728–735. 10.1037/tra0000102 [DOI] [PubMed] [Google Scholar]
- Hundt NE, Mott JM, Cully JA, Beason-Smith M, Grady RH, & Teng E (2014). Factors associated with low and high use of psychotherapy in veterans with PTSD. Psychological Trauma: Theory, Research, Practice, and Policy, 6(6), 731–738. 10.1037/a0036534 [DOI] [Google Scholar]
- Imel ZE, Laska K, Jakupcak M, & Simpson TL (2013). Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81(3), 394–404. 10.1037/a0031474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson EM, Barrie KA, Possemato K, Wade M, Eaker A, & Ouimette PC (2016). Predictors of mental health care utilization in veterans with post-traumatic stress disorder symptoms and hazardous drinking. Military Medicine, 181(10), 1200–1206. 10.7205/MILMED-D-15-00495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J (2003). Mindfulness-based stress reduction (MBSR). Constructivism in the Human Sciences, 8(2), 73–107. Retrieved from http://psycnet.apa.org/record/2004-19791-008 [Google Scholar]
- Kehle-Forbes SM, Meis LA, Spoont MR, & Polusny MA (2016). Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychological Trauma: Theory, Research, Practice, and Policy, 8(1), 107–114. 10.1037/tra0000065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller SM, & Tuerk PW (2016). Evidence-based psychotherapy (EBP) non-initiation among veterans offered an EBP for posttraumatic stress disorder. Psychological Services, 13(1), 42–48. 10.1037/ser0000064 [DOI] [PubMed] [Google Scholar]
- McFadden D (1974). Conditional logit analysis of qualitative choice behavior In Frontiers in Econometrics (pp. 105–142). Academic Press. [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, & Stevens SP (2006). Cognitive processing therapy for Veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 74(5), 898–907. 10.1037/0022-006X.74.5.898 [DOI] [PubMed] [Google Scholar]
- Mott JM, Mondragon S, Hundt NE, Beason-Smith M, Grady RH, & Teng EJ (2014).Characteristics of U.S. veterans who begin and complete prolonged exposure and cognitive processing therapy for PTSD. Journal of Traumatic Stress, 27(3), 265–273. 10.1002/jts.21927 [DOI] [PubMed] [Google Scholar]
- Resick PA, Monson CM, & Chard KM (2017). Cognitive processing therapy. New York, NY: Guilford Press. [Google Scholar]
- Sayer NA, Rosen CS, Bernardy NC, Cook JM, Orazem RJ, Chard KM, … Schnurr PP (2017). Context matters: Team and organizational factors associated with reach of evidence-based psychotherapies for PTSD in the Veterans Health Administration. Administration and Policy in Mental Health and Mental Health Services Research, 44(6), 904–918. 10.1007/s10488-017-0809-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiner B, Drake RE, Watts BV, Desai RA, & Schnurr PP (2012). Access to VA services for returning veterans with PTSD. Military Medicine, 177(7), 814–22. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22808888 [DOI] [PubMed] [Google Scholar]
- Staples JK, Hamilton MF, & Uddo M (2013). A yoga program for the symptoms of post-traumatic stress disorder in veterans. Military Medicine, 178(8), 854–860. 10.7205/MILMED-D-12-00536 [DOI] [PubMed] [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, & Kessler RC (2005). Twelve-month use of mental health services in the United States. Archives of General Psychiatry, 62(6), 629–640. 10.1001/archpsyc.62.6.629 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). PTSD: National Center for PTSD. Retrieved from www.ptsd.va.gov [Google Scholar]
- Zalta AK, Held P, Smith DL, Klassen BJ, Lofgreen AM, Normand PS, … Karnik NS (2018). Evaluating patterns and predictors of symptom change during a three-week intensive outpatient treatment for veterans with PTSD. BMC Psychiatry, 18(1), 242 10.1186/s12888-018-1816-6 [DOI] [PMC free article] [PubMed] [Google Scholar]