Abstract
Purpose:
The purpose of this study was to assess treatment choices among men with prostate cancer presenting at the MD Anderson Cancer Center MultiD clinic compared with nationwide trends.
Patients and Methods:
We analyzed 4,451 men with prostate cancer presenting at MultiD clinic in 2004–2016. To assess nationwide trends, we analyzed 392,710 men with prostate cancer diagnosed in 2004–2015 from the Surveillance, Epidemiology, and End Results (SEER) database. The primary endpoint was treatment choice as a function of pretreatment demographics.
Results:
Univariate analyses revealed similar treatment trends in the MultiD and SEER cohorts. Utilization of procedural forms of definitive therapy decreased with age, including brachytherapy and prostatectomy (all P<0.05). Later year of diagnosis/clinic visit was associated with decreased use of definitive treatments, while higher risk grouping was associated with increased use (all P<0.001).
Patients with low-risk disease treated at MultiD clinic were more likely to receive non-definitive therapy than were SEER patients, while the opposite trend was observed for patients with high-risk disease, with a substantial portion of SEER high-risk patients not receiving definitive therapy. In the MultiD clinic, African American men with intermediate and high-risk disease were more likely to receive definitive therapy than white men, but for SEER the opposite was true.
Conclusion:
Presentation at a MultiD clinic facilitates the appropriate disposition of patients with low-risk disease to non-definitive strategies, those with high-risk disease to definitive treatment, and may obviate the influence of race.
Keywords: Prostate Cancer, Multidisciplinary Clinic, Treatment Access, SEER
Precis:
Presentation at a multidisciplinary clinic facilitates appropriate disposition of low risk patients into non-definitive strategies, high risk patients into definitive treatment, and may obviate the confounding influence of race. In comparison, nationwide disposition of patients may be confounded by pre-treatment demographic factors.
INTRODUCTION
The treatment paradigm for prostate cancer has undergone significant shifts. Multiple standard-of-care options are available based on the patient’s risk grouping and life expectancy. However, given variations in referral and practice patterns, a large proportion of patients may not be fully informed of all treatment options.1,2 To provide a more balanced presentation of treatment choices, institutions have developed multidisciplinary (MultiD) clinics, in which patients are presented multiple choices by specialists in the participating disciplines.3–5 At The University of Texas MD Anderson Cancer Center MultiD clinic for prostate cancer, patients with a new diagnosis of prostate cancer discuss treatment options with both a urologist and a radiation oncologist. This approach allows the simultaneous presentation of therapy choices, which facilitates informed decision-making and expedites time to treatment initiation. To assess the effects of having such clinics on decision-making, we present an analysis of treatment choices made at MD Anderson prostate MultiD clinics in comparison to US national trends assessed by reviewing the Surveillance, Epidemiology, and End Results (SEER) database.
PATIENTS AND METHODS
Multidisciplinary Clinic
The MD Anderson MultiD prostate clinic in Houston, Texas was implemented in 2004. The goal of this clinic is to offer balanced opinions on initial definitive local therapies from the perspective of practitioners in their respective specialties. Typically in these clinics 3–4 new patients are seen per day at the same location by both a radiation oncologist and an urologist. To be eligible for the MultiD clinic, patients must present with newly diagnosed prostate cancer that has not been definitively treated. All patients must have prostate biopsy tissue reviewed by MD Anderson pathologists to confirm diagnosis and assign a Gleason score and have no evidence of metastatic disease. At the time of patient intake a pre-specified script was utilized by patient intake coordinators which screened for the above criteria and only scheduled patients if they did not express a specific interest in a single modality. In the event that a patient expressed an interest in a single modality they were scheduled with a single practitioner in lieu of the MultiD clinic. In the event that a decision is not made during the initial MultiD appointment, the patient then either contacts staff with their choice or clinic staff make a follow-up inquiry.
Patients
The MultiD group in this study comprised patients who presented at MD Anderson prostate MultiD clinic from March 11, 2004 through December 29, 2016. Exclusion criteria included initial diagnosis of M1 or N1 disease, missing staging information (prostate-specific antigen [PSA] levels, clinical examination, or Gleason score), and prior receipt of definitive prostate treatment. Patients were included only if they were seen by both a radiation oncologist and an urologist and a treatment choice was known. Time-related variables (patient age and year of clinic visit) were referenced to the date of the clinic visit.
For comparison, the SEER database was searched to assess national trends in the types of treatment used for prostate cancer. Because the data range of the current SEER database was 1973–2015, we selected patients diagnosed from Jan 1, 2004 through December 31, 2015. Inclusion criteria included presentation with a confirmed diagnosis of prostate adenocarcinoma that represented their first malignancy. Exclusion criteria were similar to those for the MultiD group and included a diagnosis of M1 or N1 disease, missing staging information, a PSA level >90, or missing information regarding treatment. SEER treatment facilities were categorized as urban versus rural based on the National Center for Health and Statistics (NCHS) urban-rural classification scheme for counties6. The county of the treatment facility was categorized as urban if the 2010 county-level census population exceeded 250,000, which was the NCHS criteria for a medium urban county6. Urban counties and their corresponding federal information processing standards (FIPS) code are listed in Supplemental Table 1. This study was approved by the appropriate institutional review board. Time-related variables (patient age and year of diagnosis) for SEER patients were referenced to the date of disease diagnosis.
Men who received brachytherapy alone or a brachytherapy boost with external beam radiation were both grouped as having received brachytherapy. Patients were categorized as receiving prostatectomy if they received radical prostatectomy or prostatectomy with resection in continuity with other organs (e.g. cystoprostatectomy). Other locally destructive therapies such as cryotherapy and high-intensity focused ultrasound were not included in the analysis because of their low frequency. Patients were classified as receiving a non-definitive therapy if they had not received definitive local therapy to the prostate; the non-definitive treatments were active surveillance, watchful waiting, and androgen deprivation alone. Among patients seen in the MultiD clinic, non-definitive therapy consisted exclusively of active surveillance and no patients received watchful waiting or primary ADT as an initial treatment strategy.
Statistical analysis
All data were analyzed with SAS ver. 9.3 and JMP Pro ver. 12 (both Cary, NC). Multinomial logistic regression was used to assess univariate and multivariate associations between baseline patient characteristics and treatment received, with significance set at P<0.05. Multivariate regressions included race, clinic year, patient location (analyzed for MultiD clinics only), risk group, and age. Descriptive statistics were used to assess trends in cancer treatment and their association with pretreatment factors and demographics.
RESULTS
Patients
A total of 4,451 patients seen in the MultiD clinic and 392,710 patients in the SEER database met the inclusion criteria. Median ages was similar in both cohorts (MultiD 62 years, SEER 65 years), with the SEER cohort being slightly older. In both databases the most prevalent risk grouping was intermediate (MultiD 51%, SEER 46%), and the most common treatment received was prostatectomy (MultiD 48%, SEER 38%). In the MultiD clinic, patient location was divided evenly between the greater Houston metropolitan area (31%), Texas outside the Houston metropolitan area (35%), and USA outside Texas (34%). The baseline characteristics of both cohorts are presented in Table 1.
Table 1.
Baseline Characteristics
| Baseline Characteristics | MultiD (n=4,451) | SEER (n=392,710) | ||
|---|---|---|---|---|
| No. | % | No. | % | |
| Age at visit, median, years (IQR) | 62 (57–68) | 65 (59–71) | ||
| NCCN Risk Groups | ||||
| Low | 1,422 | 32 | 136,941 | 35 |
| Intermediate | 2,256 | 51 | 179,569 | 46 |
| High | 773 | 17 | 76,200 | 19 |
| Treatment Group | ||||
| Non-Definitive | 880 | 20 | 88,154 | 22 |
| Prostatectomy | 2,154 | 48 | 148,351 | 38 |
| External Beam Radiation | 1,028 | 23 | 98,280 | 25 |
| Other Locally Destructive Therapies | 69 | 2 | 5,664 | 1 |
| Brachytherapy/Brachy Boosts | 322 | 7 | 52,261 | 13 |
| Patient’s Residence | ||||
| Greater Houston Metro | 1,373 | 31 | ||
| Texas outside Houston Metro | 1,555 | 35 | ||
| USA outside Texas | 1,492 | 34 | ||
| Outside USA | 31 | 1 | ||
| Race | ||||
| White | 3,644 | 82 | 304,084 | 78 |
| African American | 483 | 11 | 61,582 | 16 |
| Other | 324 | 7 | 27,044 | 7 |
| Facility County Classification** | ||||
| Urban | 4,451 | 100 | 284,249 | 72 |
| Rural | 108,328 | 28 | ||
Cryotherapy, high-frequency focused ultrasound, and laser ablation
Patients treated in Alaska (n=133), could not be classified has having been treated in an urban or rural facility as county level data was not available.
Abbreviations: MultiD, multidisciplinary clinics;
SEER, Surveillance, Epidemiology and End Results database;
NCCN, National Comprehensive Cancer Network; IQR, interquartile range.
Univariate association of baseline characteristics with treatment choice
Multinomial logistic regression identified several trends in therapy selection among MultiD and SEER patients (Table 2). For all logistic regressions, treatment decisions were made in reference to the use of non-definitive treatment. In the MultiD clinic, older age was associated with decreased use of brachytherapy (odds ratio [OR] =0.98 per year, P=0.02) and prostatectomy (OR=0.94 per year, P<0.001). Conversely, older age was associated with increased use of EBRT (OR=1.06 per year, P<0.001). Similar associations with age were observed in the SEER cohort, with decreased use of brachytherapy (OR=0.95 per year, P<0.001) and prostatectomy (OR=0.89 per year, P<0.001) in older patients (Table 2). With regard to the year of clinic visit/diagnosis in the MultiD and SEER cohorts, later year was associated with decreased use of definitive treatments (all P<0.001). All of these associations held on multivariate analysis.
Table 2.
Multinomial Logistic Regression of Associations Between Baseline Patient Characteristics and Treatment Received
| Treatment Choice (Ref = Non-Definitive) |
Brachytherapy MultiD |
Brachytherapy SEER |
EBRT MultiD |
EBRT SEER |
Prostatectomy MultiD |
Prostatectomy SEER |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | P | OR | P | OR | P | OR | P | OR | P | |||
| Age at visit (per year) | 0.98 | 0.02 | 0.95 | <0.001 | 1.06 | <0.001 | 0.999 | 0.08 | 0.94 | <0.001 | 0.89 | <0.001 |
| Year of diagnosis/clinic (per year) | 0.91 | <0.001 | 0.88 | <0.001 | 0.87 | <0.001 | 0.97 | <0.001 | 0.90 | <0.001 | 0.97 | <0.001 |
| NCCN Risk Grouping | ||||||||||||
| Low | Ref | Ref | Ref | |||||||||
| Intermediate | 6.35 | <0.001 | 0.80 | <0.001 | 11.68 | 0.43 | 2.72 | <0.001 | 9.98 | 0.42 | 1.26 | <0.001 |
| High | 6.10 | 0.05 | 1.39 | <0.001 | 101.50 | <0.001 | 2.57 | <0.001 | 74.82 | <0.001 | 2.53 | <0.001 |
| Patient’s Residence | ||||||||||||
| Greater Houston Metro | Ref | Ref | Ref | |||||||||
| Texas outside Houston Metro | 1.20 | 0.95 | 0.75 | 0.62 | 1.06 | 0.73 | ||||||
| USA outside Texas | 1.51 | 0.94 | 0.66 | 0.83 | 0.97 | 0.32 | ||||||
| Outside USA | NA* | 0.45 | 0.39 | 1.45 | 0.44 | |||||||
| Race | ||||||||||||
| White | Ref | Ref | Ref | |||||||||
| Africa American | 1.17 | 0.005 | 1.002 | <0.001 | 1.41 | 0.007 | 1.04 | <0.001 | 1.52 | <0.001 | 0.71 | <0.001 |
| Other | 0.28 | <0.001 | 0.58 | <0.001 | 0.77 | 0.02 | 0.84 | <0.001 | 0.80 | 0.005 | 0.61 | <0.001 |
Too few events in this category
Abbreviations: MultiD, multidisciplinary clinic; EBRT, external-beam radiation therapy; SEER, Surveillance, Epidemiology and End Results database; NCCN, National Comprehensive Cancer Network.
For multinomial logistic regressions assessing risk groupings, the reference group for comparison was the low-risk group. In the MultiD clinics, intermediate risk was associated with increased use of brachytherapy (OR=6.35, P<0.001) and high risk was associated with increased use of EBRT and prostatectomy (all P<0.001). In the SEER cohort, intermediate risk was associated with decreased use of brachytherapy (OR=0.80, P<0.001) and increased use of EBRT (OR=2.72, P<0.001) and prostatectomy (OR=1.26, P<0.001), and high risk was associated with increased use of all definitive treatment modalities (all P<0.001). All of these associations held on multivariate analysis as well.
For logistic regressions assessing race, the reference group for comparison was white. In the MultiD clinics, being African American was associated with increased use of definitive therapy (brachytherapy OR=1.17, EBRT OR=1.41, and prostatectomy OR=1.52, all P<0.01). Similar to the MultiD clinics group, being African American in the SEER cohort was associated with increased use of brachytherapy/brachytherapy boost and EBRT, although the magnitude of this association was considerably less (brachytherapy OR=1.002 and EBRT OR=1.04, both P<0.001). In contrast to the MultiD cohort, being African American in the SEER cohort was associated with decreased use of prostatectomy (OR=0.71, P<0.001). In both cohorts, being a non-black minority was associated with decreased use of definitive therapy (all P<0.001). These associations held on multivariate analysis.
Finally, assessment of treatment use among MultiD clinics patients with respect to where the patient lived, with respect to Houston and Texas, revealed no significant associations with treatment selection (all P>0.05).
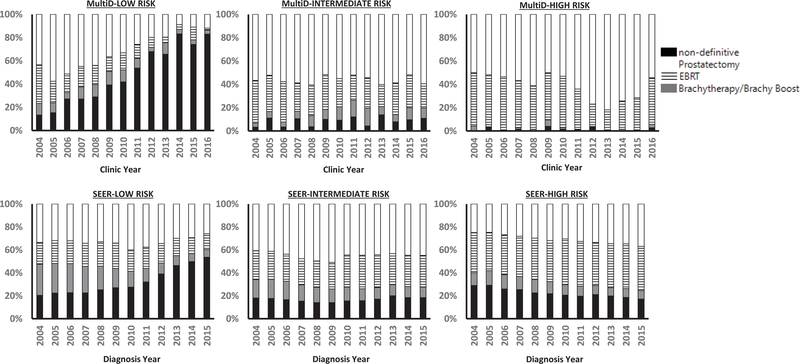
Treatment choice with respect to time
To examine the interaction of clinic year/diagnosis with respect to treatment choice, treatment use was graphed with respect to clinic year (Fig. 1). In the MultiD clinics, the most pronounced trend was increased use of non-definitive therapy for patients with low-risk disease over time. In 2004, the frequency of non-definitive treatment in the low-risk group was 13%, which substantially increased to 74% in 2015. An inflection point was noted in 2008–2009, when a more rapid increase in the use of non-definitive treatment began (Fig. 1). In comparison, SEER patients with low-risk disease also experienced increased use of non-definitive therapy, from 18% in 2004 compared with 54% in 2015. A similar inflection point appeared later for the SEER database, at approximately 2010–2011 (Fig. 1).
Fig. 1.
Treatment choice by year of clinic visit (for patients in the multidisciplinary clinics group [MultiD]) or diagnosis (for patients in the Surveillance, Epidemiology and End Results database [SEER]).
With regard to high-risk disease, in the SEER cohort the use of non-definitive therapy declined gradually over time, from 27% in 2004 to 16% in 2015. Use of non-definitive therapy was very infrequent for men with high-risk disease in the MultiD clinics cohort (Fig. 1).
Finally, the SEER database showed decreased use of brachytherapy/brachy boost over time. This trend was most prominent in the low-risk group (26% in 2004 vs. 7% in 2015), but was also present in the intermediate-risk group (16% in 2004 vs. 9% in 2015) and high-risk group (11% in 2004 vs. 7% in 2015). No consistent trends in brachytherapy use over time were noted in MultiD patients.
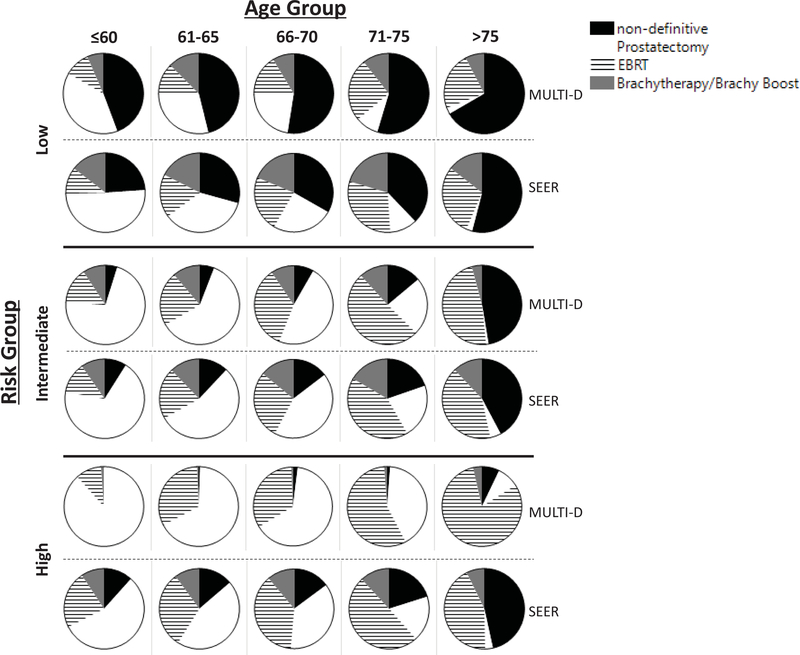
Treatment choice for the MultiD versus SEER patients with respect to risk group and age
To assess the relationship between age, risk group, and treatment choice, a series of pie charts were constructed to display the relative treatment use with respect to age and risk group (Fig. 2). In the low-risk groups, use of non-definitive therapy was increased in the MultiD clinics compared with the SEER cohort across all age groups. The opposite trend was observed in the high-risk groups, where a high proportion of non-definitive therapy was used in the SEER cohort versus almost none in the MultiD clinic (Fig. 2). In both cohorts, use of non-definitive therapy increased with patient age for all risk groups (Fig. 2). Given that MDACC is located in the center of Houston, a sensitivity analysis was conducted comparing patient treatment choices in the MultiD clinic versus Urban SEER facilities. This analysis revealed similar results (Supplemental Fig. 1).
Fig. 2.
Treatment choice in the multidisciplinary clinics group (MultiD) and the Surveillance, Epidemiology, and End Results group (SEER) with respect to risk group and patient age.
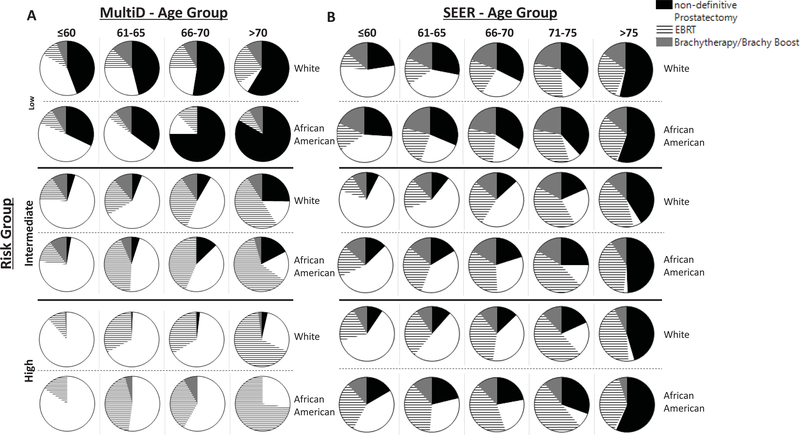
Treatment choice for African Americans versus whites with respect to risk group and age
Two separate series of pie charts were then constructed to display the relative proportions of treatment use stratified by race for the MultiD clinic and the SEER groups (Fig. 3). For the MultiD clinic group, patients who were 71–75 years old and ≥75 years old were combined into a >70 years group owing to the relatively small number of older African American patients (Fig. 3a). Among low-risk patients in the MultiD clinic, older (>70 years) African American patients were more likely to receive non-definitive therapy than older white patients (Fig. 3a). Among low-risk patients in the SEER group, African American and white patients were treated with non-definitive therapy with approximately equal frequency across all age groups (Fig. 3b).
Fig. 3.
Treatment choice among patients in the multidisciplinary clinics group (MultiD; A) and in the Surveillance, Epidemiology, and End Results group (SEER; B) with respect to age, risk group, and race (white vs. African American).
When assessing the intermediate-risk and high-risk groups, African American patients in the MultiD clinic received non-definitive therapy less often than did their white counterparts (Fig. 3a). In contrast, intermediate-risk and high-risk African American patients in all age groups in the SEER cohort received non-definitive therapy more often than did white patients (Fig. 3b). These trends generally held for all age groups.
DISCUSSION
Key findings from our analyses include the following. (1) Men with low-risk disease were more likely to receive non-definitive therapy in MultiD clinics than were their SEER counterparts (Figs. 1 and 2). (2) Over time, higher percentages of men with low-risk disease received non-definitive therapy in both cohorts; however, this trend was more pronounced in the MultiD clinics group (Fig. 1). (3) A significant proportion of men with high-risk disease were treated with non-definitive therapy in the SEER cohort, whereas almost all men with high-risk disease received definitive therapy in the MultiD clinics group (Fig. 2). (4) In the MultiD clinics, older (>70 years) African American men with low-risk disease were more likely to receive non-definitive therapy than were older white men with low-risk disease (Fig. 3a); however, in all other age and risk groups, African Americans were more likely to receive definitive therapy (Fig. 3a). This trend was opposite that observed in the SEER cohort, where African Americans among all risk groups were more likely to receive non-definitive therapy across age groups (Fig. 3b).
The trend toward increased use of non-definitive therapy for patients with low-risk prostate cancer is supported by current National Comprehensive Cancer Network (NCCN) guidelines and national trends.7,8 In the MultiD clinics, an inflection point was noted at approximately 2008–2009 in the rate of increase in the use of non-definitive treatment for low-risk disease (Fig. 1). This increase most likely reflects early adoption of active surveillance, as promoted by a series of publications appearing around that time.9–11 In 2015, the observed 74% rate of non-definitive therapy among men with low-risk disease in the MultiD clinics was higher than the 54% observed in the SEER group. This magnitude and trend over time toward use of non-definitive therapy for low-risk prostate cancer in the SEER cohort are concordant with other SEER and National Cancer Data Base analyses2,8,12.
On the opposite side of the spectrum, the NCCN guidelines recommend that men with high-risk prostate cancer with >5 years of life expectancy receive definitive therapy.7 According to Social Security–based and other life expectancy estimators, men aged 65 years are predicted to have a life expectancy of 78–85 years,13 suggesting that most men with high-risk prostate cancer who are <70 years old should be treated with definitive therapy. However, in the current SEER cohort, a substantial proportion of men with high-risk disease <70 years old received non-definitive treatment (16% for ≤60 years, 19% for 61–65 years, and 21% for 66–70 years, Fig. 2). The use of non-definitive therapy for high-risk disease is not supported by high-level evidence, as both the MRC PR07 and SPCG-7/SFUO-3 trials provided phase III randomized data showing a survival benefit from definitive radiation for such patients.14,15 In concordance with these trial results, almost no men with high-risk disease received non-definitive therapy in the MultiD clinics.
Regarding the association of race with treatment, numerous studies have demonstrated increased use of definitive therapy among white patients compared with African American patients.2,12,16,17 Among MultiD clinics patients, we observed the opposite trend for high-risk, intermediate-risk, and young (≤70 years) low-risk patients, with African American patients having higher rates of definitive therapy (Fig. 3a). The observation that older African American men (>70) with low-risk prostate cancer had higher rates of active surveillance is concordant with NCCN guidelines. In contrast, in the current SEER cohort, African American men received non-definitive therapy more often than white patients for all risk and age groups (Fig. 3b). Although non-definitive therapy may be encouraged by national guidelines for low-risk and some intermediate-risk patients,7 social factors may have driven this difference for many of these African American men, especially those with high-risk disease. These results suggest than when presented treatment options by a multidisciplinary team, African American men may opt for more definitive treatment choices, a result that contrasts with national trends observed in this and other analyses.2,12
Overall, the treatment choices made at the MD Anderson MultiD clinics are similar to those observed at other MultiD clinics. Aizer et al. reported on 239 men with low-risk disease treated at MultiD clinics at Massachusetts General Hospital, Brigham and Women’s Hospital, and Beth Israel Deaconess Medical Center in 2009.4 As was the case in our study, presentation at a MultiD clinic in that study was associated with increased use of active surveillance relative to a contemporary cohort of 462 patients seen by individual practitioners (43% vs. 22%).4 Further, the general trends in treatment choices reflect those observed in other MultiD clinics. Hurwitz et al. reported on 925 patients seen at the Walter Reed National Military Medical Center MultiD clinic in 2006–2014.5 As was the case at the MD Anderson MultiD clinics, most men with low-risk or intermediate-risk disease at the Walter Reed MultiD clinic chose surgery (54%) followed by EBRT (20%) and active surveillance (12%).5 Stewart et al. published on 701 patients seen at the Duke MultiD clinic in 2005–2009. Once again, most patients chose prostatectomy (52%) or radiation therapy (33%), followed by non-definitive therapy (13% active surveillance or androgen blockade).18
The current study had several limitations that deserve mention. The current SEER database contains data through 2015, whereas our MultiD clinics database contains mature data through 2016. The current SEER data also lacks significant details regarding systemic therapy and does not have data on whether patients were treated with active surveillance, watchful waiting, hormones alone, or “benign neglect.” To create comparable categories, we categorized SEER and MultiD clinics patients who did not receive definitive therapy as having received “non-definitive” therapy. Furthermore, data regarding patient comorbidities are not available in SEER thus making interpretation of the appropriateness of non-definitive therapy within this cohort difficult. It should be noted that research analyzing the sensitivity of the SEER data in terms of capturing initial treatment decisions (including no treatment) found approximately 90% concordance with hospital records.19–21 Another consideration is that given the large number of patients (especially in the SEER group), clinically insignificant differences can become statistically significant. We therefore focused on visualizing trends and de-emphasized statistical testing.
Finally, there exists inherent patient referral bias to this single center MultiD clinic. Specifically MDACC MultiD population may select for a population who are more urban, motivated and able to travel, and possess significant resources. To this end, modest demographic differences are noted between the analyzed populations including the SEER population exhibiting a higher age (65 vs 62) and higher proportion of African Americans (16% vs 11%). With regard to the first two limitations it is notable that comparing MultiD patients who live in the Houston Metro area versus those who do not did not reveal a difference in treatment selection, furthermore analyzing SEER patients treated in urban facilities compared to the MultiD clinic revealed similar trends (Supplemental Fig. 1). However we are unable to fully separate these referral biases given the available data and thus caution is warranted in generalizing the results of this analysis.
Despite these weaknesses, numerous strengths deserve mention. First, to the best of our knowledge these findings present the largest analysis of a MultiD clinics database over the longest timeframe. Given the large MultiD patient cohort, which to the best of our knowledge, is an order of magnitude larger than the next largest analyses,4,5,18 the current analysis is able to subdivide patients into specific patient binds based on variables such as year of presentation, risk group, minority race groups, and 5 year age increments. The extent of follow-up in both these clinics (through 2016) and in the SEER database (through 2015) affords a continuous perspective of temporal treatment trends in a practice landscape shaped by new paradigm-shifting research and guidelines. Further, our comparison of treatment choices in the MultiD clinic group with the SEER group allows us a unique look at treatment choices among relatively socially and economically unfettered patient populations versus the reality of treatment administration nationwide.
CONCLUSIONS
Our analysis of a large cohorts of consecutive patients suggest that a MultiD clinic visit facilitates presentation of and adherence to evidence-based national guidelines that span race and may bridge social divides that exist on the national level. Although biases may exist in the patient acceptance of multidisciplinary care, both of these outcomes offer a significant incentive to providing multidisciplinary clinical care on the national level. This analysis may also serve as a tool for patients to compare their treatment options with the decisions made by men with similar demographic and cancer characteristics.
Supplementary Material
Supplemental Fig. 1. Treatment choice in the multidisciplinary clinics group (MultiD) and the Surveillance, Epidemiology, and End Results group (SEER), with respect to risk group and patient age, limiting patients to only those treated in urban counties.
Acknowledgement:
We would like to acknowledge Christine Wogan for her assistance in editing and formatting this manuscript
Funding Support: Supported in part by Cancer Center Support (Core) Grant NCI CA016672 to The University of Texas MD Anderson Cancer Center. Chad Tang is supported in part by grants from CPRIT, Radiation Oncology Institute, and the Anna Fuller Foundation.
Footnotes
Conflict of Interest Statement: Chad Tang has acted as a paid consultant for RefleXion for work outside the current scope of study.
REFERENCES
- 1.Muralidhar V, Rose BS, Chen YW, et al. : Association Between Travel Distance and Choice of Treatment for Prostate Cancer: Does Geography Reduce Patient Choice? International Journal of Radiation Oncology Biology Physics 96:313–317, 2016 [DOI] [PubMed] [Google Scholar]
- 2.Krishna S, Fan Y, Jarosek S, et al. : Racial Disparities in Active Surveillance for Prostate Cancer. J Urol 197:342–349, 2017 [DOI] [PubMed] [Google Scholar]
- 3.Gabel M, Hilton NE, Nathanson SD: Multidisciplinary breast cancer clinics. Do they work? Cancer 79:2380–4, 1997 [PubMed] [Google Scholar]
- 4.Aizer AA, Paly JJ, Zietman AL, et al. : Multidisciplinary Care and Pursuit of Active Surveillance in Low-Risk Prostate Cancer. Journal of Clinical Oncology 30:3071–3076, 2012 [DOI] [PubMed] [Google Scholar]
- 5.Hurwitz LM, Cullen J, Elsamanoudi S, et al. : A prospective cohort study of treatment decision-making for prostate cancer following participation in a multidisciplinary clinic. Urologic Oncology-Seminars and Original Investigations 34, 2016 [DOI] [PubMed] [Google Scholar]
- 6.Ingram DD, Franco SJ, National Center for Health Statistics (U.S.): 2013 NCHS urban-rural classification scheme for counties. Hyattsville, Maryland, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, 2014 [Google Scholar]
- 7.Network NCC: NCCN Gudielines Version 4.2018 Prostate Cancer, 2018 [Google Scholar]
- 8.Weiner AB, Patel SG, Etzioni R, et al. : National trends in the management of low and intermediate risk prostate cancer in the United States. J Urol 193:95–102, 2015 [DOI] [PubMed] [Google Scholar]
- 9.Klotz L, Zhang L, Lam A, et al. : Clinical results of long-term follow-up of a large, active surveillance cohort with localized prostate cancer. J Clin Oncol 28:126–31, 2010 [DOI] [PubMed] [Google Scholar]
- 10.van den Bergh RC, Vasarainen H, van der Poel HG, et al. : Short-term outcomes of the prospective multicentre ‘Prostate Cancer Research International: Active Surveillance’ study. BJU Int 105:956–62, 2010 [DOI] [PubMed] [Google Scholar]
- 11.van As NJ, Norman AR, Thomas K, et al. : Predicting the probability of deferred radical treatment for localised prostate cancer managed by active surveillance. Eur Urol 54:1297–305, 2008 [DOI] [PubMed] [Google Scholar]
- 12.Friedlander DF, von Landenberg N, Loppenberg B, et al. : Facility Level Variation in Rates of Definitive Therapy for Low Risk Prostate Cancer in Men with Limited Life Expectancy: An Opportunity for Value Based Care Redesign. J Urol, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sammon JD, Abdollah F, D’Amico A, et al. : Predicting Life Expectancy in Men Diagnosed with Prostate Cancer. Eur Urol 68:756–65, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mason MD, Parulekar WR, Sydes MR, et al. : Final Report of the Intergroup Randomized Study of Combined Androgen-Deprivation Therapy Plus Radiotherapy Versus Androgen-Deprivation Therapy Alone in Locally Advanced Prostate Cancer. J Clin Oncol 33:2143–50, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Widmark A, Klepp O, Solberg A, et al. : Endocrine treatment, with or without radiotherapy, in locally advanced prostate cancer (SPCG-7/SFUO-3): an open randomised phase III trial. Lancet 373:301–8, 2009 [DOI] [PubMed] [Google Scholar]
- 16.Underwood W, De Monner S, Ubel P, et al. : Racial/ethnic disparities in the treatment of localized/regional prostate cancer. J Urol 171:1504–7, 2004 [DOI] [PubMed] [Google Scholar]
- 17.Schmid M, Meyer CP, Reznor G, et al. : Racial Differences in the Surgical Care of Medicare Beneficiaries With Localized Prostate Cancer. JAMA Oncol 2:85–93, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart SB, Banez LL, Robertson CN, et al. : Utilization trends at a multidisciplinary prostate cancer clinic: initial 5-year experience from the Duke Prostate Center. J Urol 187:103–8, 2012 [DOI] [PubMed] [Google Scholar]
- 19.Kraus RD, Hamilton AS, Carlos M, et al. : Using hospital medical record data to assess the accuracy of the SEER Los Angeles Cancer Surveillance Program for initial treatment of prostate cancer: a small pilot study. Cancer Causes & Control 29:815–821, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noone AM, Lund JL, Mariotto A, et al. : Comparison of SEER Treatment Data With Medicare Claims. Medical Care 54:E55–E64, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kraus RD, Hamilton A, Ballas LK: Using Re-abstracted Hospital Medical Record Data to Assess the Accuracy of the SEER Database for Prostate Cancer Treatment. International Journal of Radiation Oncology • Biology • Physics 99:E250, 2017 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Fig. 1. Treatment choice in the multidisciplinary clinics group (MultiD) and the Surveillance, Epidemiology, and End Results group (SEER), with respect to risk group and patient age, limiting patients to only those treated in urban counties.