Abstract
Background:
Little is known about the impact of the Affordable Care Act (ACA) on people living with HIV and cancer (PLWHC), who have lower cancer treatment rates and worse cancer outcomes. To investigate this research gap, we examined the effect of the ACA on insurance coverage and cancer treatment receipt among PLWHC in the U.S.
Methods:
HIV-infected people aged 18–64 with cancer diagnosed from 2011–2015 were identified in the National Cancer Database. Health insurance coverage and cancer treatment receipt were compared pre- and post-ACA in non-Medicaid expansion and Medicaid-expansion states using difference-in-differences (DD) analysis.
Results:
Of 4,794 PLWHC analyzed, 49% resided in non-expansion states and were more often uninsured (16.7%% vs. 4.2%), non-White (65.2% vs. 60.2%), and low income (36.3% vs. 26.9%) than those in expansion states. After 2014, the percent uninsured decreased in expansion (4.9% to 3%, p=0.01) and non-expansion states (17.6% to 14.6%, p=0.06), possibly due to increased Medicaid coverage in expansion states (36.9% to 39.2%) and increased private insurance coverage in non-expansion states (29.5% to 34.7%). There was no significant difference in cancer treatment receipt between expansion and non-expansion states. However, the percent of PLWHC treated at academic facilities increased significantly only in expansion states (40.2% to 46.7%, p<0.0001; DD: 7.2 pp, p=0.02).
Conclusion:
The implementation of the ACA was associated with improved insurance coverage among PLWHC. Lack of insurance is still common in non-expansion states. Patients with minority or low socioeconomic status more often resided in non-expansion states, highlighting the need for further insurance expansion.
Keywords: HIV, Neoplasms, Insurance Coverage, Patient Protection and Affordable Care Act, Healthcare Disparities
Precis:
The implementation of the ACA was associated with improved insurance coverage among patients living with HIV and cancer. Post-ACA, the percent uninsured was five times greater in non-Medicaid expansion states than Medicaid-expansion states, highlighting the need for further insurance expansion to ensure adequate access to cancer care.
INTRODUCTION
The Patient Protection and Affordable Care Act (ACA) has been associated with a substantial reduction in the number of uninsured adults throughout the United States.1 Specifically, the ACA improved health insurance coverage options by allowing dependents to remain on parents’ private health insurance plans, facilitating the purchase of individual policies through the Marketplace, and expanding Medicaid in some states.2–4 It also eliminated cost-sharing for evidence-based preventive services, including cancer screening. Prior research has demonstrated that Medicaid expansions are associated with improved access to cancer screening and therapies.5–7 Medicaid expansions are also associated with shifts toward early-stage cancer diagnosis3, 4, 8 and decreased patient out-of-pocket costs.9 Together, these effects could translate to better cancer care.
The ACA has improved care maintenance for people with HIV by eliminating preexisting condition exclusions10 and has improved care receipt through reducing premiums and out-of-pocket expenses for a population disproportionally comprised of lower-income and uninsured/underinsured patients.11 This has led to increased insurance availability and Medicaid coverage in HIV-infected patients in states with Medicaid expansion.12 This growth of insurance coverage has led to better control of HIV and increased accessibility to primary care services,13 which may lead to improved downstream health outcomes in this population.
While the reported effects of the ACA on patients with cancer2, 9, 14, 15 and patients with HIV12, 13 have been established separately, little is known about the specific impact of the ACA on people living with HIV and cancer (PLWHC). Prior studies have demonstrated that PLWHC are at risk for not receiving cancer treatment, in spite of greater longevity due to improvements in HIV control.16 Additionally, PLWHC have worse cancer-specific survival as compared to patients without HIV, partly due to disparities in cancer treatment.17–20 Since insurance status and access to healthcare influence cancer treatment rates and outcomes, investigating the impact of the ACA on cancer treatment receipt is especially relevant as the public health burden of cancer in the aging HIV population continues to grow.21, 22
The purpose of this study is to assess the impact of the ACA on health insurance coverage and cancer treatment among PLWHC in Medicaid-expansion and non-expansion states in the U.S.
MATERIALS AND METHODS
Patient Population
We used the National Cancer Database (NCDB), a hospital-based cancer registry jointly sponsored by the American College of Surgeons and the American Cancer Society that captures approximately 70% of all U.S. cancer cases,23 to analyze data from HIV-infected patients aged 18–64 diagnosed with cancers of the head and neck (oral cavity, pharynx, and larynx), upper GI tract, colorectum, anus, lung, female breast, cervix, prostate, Hodgkin lymphoma and diffuse large B-cell lymphoma between January 2011 and December 2015. New cancer diagnosis and date of diagnosis were determined using the ICD-9-CM codes 140–209, 230–239 and ICD-10-CM codes C00-D49 and the initial recorded diagnosis date.24 HIV status was determined from reported comorbidities using the ICD-9-CM diagnosis codes 04200–044.90 and ICD-10-CM codes B20-B22, B24. Although certain comorbidities are underreported in the NCDB, prior studies have demonstrated high concordance between HIV/AIDS reporting in the NCDB and claims data in the SEER-Medicare database.25 Patients with both cancer and HIV ICD codes in their medical record were used for this study. Patients aged 65 and older were excluded due to age-eligibility for Medicare coverage. Patients with stage 0, occult, not any, or unknown cancer stage (N=1,951) and those with missing insurance status (N=54) were also excluded.
We extracted clinical and demographic data, including age at diagnosis, sex, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other), health insurance coverage, zip-code level median income quintile (<$36,000; $36,000 – $43,999; $44,000 – $52,999; $53,000 – $68,999; and $69,000+), year of cancer diagnosis, cancer type, reporting facility type, and receipt of cancer treatment. Insurance status was determined according to coding for primary payer at diagnosis and was categorized as private, Medicaid, Medicare, uninsured, or other. Facility type was categorized as Community Cancer Program, Comprehensive Community Cancer Program, Teaching/Academic Research Program, National Cancer Institute (NCI) Program/Network, and Other. Receipt of cancer treatment was defined as receiving any surgery, radiation therapy, and/or systemic therapy in inpatient and outpatient settings for the first course of treatment.
Insurance Coverage and Cancer Care
This study’s primary outcomes were insurance coverage, receipt of cancer treatment, and facility type pre- and post-ACA and in Medicaid-expansion versus non-Medicaid expansion states in PLWHC. The pre-ACA era was defined as January 2011 to December 2013. The post-ACA era was defined as January 2014 to December 2015 as a majority of states expanded Medicaid in 2014. Other time periods (before ACA, early ACA, and late ACA) were also evaluated (Supporting Table 1), with similar findings as the comparison between pre- and post-ACA time periods.
Medicaid-expansion states were defined as “expansion states” if they chose to exercise the expansion option through the ACA by developing a new state plan or using a Section 1115 waiver in 2010 to 2013, or if they chose to expand Medicaid to 138% of the Federal Poverty Level beginning in 2014. “Expansion states” were time-varying, and were considered to be “non-expansion states” until the time of Medicaid expansion. Twenty five states expanded Medicaid eligibility. All states that did not fully expand Medicaid by the end of 2015 were defined as non-expansion states. Cancers diagnosed in 2015 in Arkansas, Indiana, and Pennsylvania (N=64) were excluded from the analysis because these states expanded Medicaid eligibility in 2015, the last year of our study period.
Statistical Analysis
Wald chi-square analysis was used for comparisons of proportions. Changes in the proportion of health insurance type at cancer diagnosis, the cancer treatment receipt rate, and the percentage of PLWHC who received cancer treatment at each facility type through the two ACA periods were calculated for expansion and non-expansion states. Paired comparisons of the changes between insurance coverage, treatment receipt, and facility type where treatment was received between the two ACA periods were calculated. Difference in differences (DD) analyses was used to assess the association between Medicaid expansion states and changes in health insurance coverage, receipt of cancer treatment, and the facility type. Patients in Medicaid-expansion states were the intervention group and patients in non-expansion states were the control group. To calculate DD estimates, we fitted crude and multivariable linear probability models adjusting for age, sex, race/ethnicity, year of diagnosis, and zip-code level median income quintile. All statistical analyses were executed using SAS statistical software version 9.4 (SAS Institute Inc.). This study was granted exemption from full review by the Morehouse School of Medicine Institutional Review Board.
RESULTS
Of 4,794 PLWHC diagnosed with cancer between 2011 and 2015, 2,331 (48.8%) lived in non-expansion states and 2,448 (51.2%) lived in expansion states. Across the entire PLWHC population analyzed in this study, the median age at cancer diagnosis was 50 years (IQR: 44–57) and the majority of patients were male (75%) and non-white (13.5% Hispanic, 49.3% Black). The two most common malignancies diagnosed in PLWHC were diffuse large B-cell lymphoma (22.9%) and lung cancer (17.9%). PLWHC most commonly received cancer treatment in health facilities characterized as teaching/academic research programs (40.8%). All patient demographic and clinical characteristics for the expansion cohorts are shown in Table 1.
Table 1:
Demographic and clinical characteristics among HIV-infected cancer patients in Medicaid expansion versus non-Medicaid expansion states.
| Non-Expansion States† N(%) | Expansion States‡ N(%) | P-value | |
|---|---|---|---|
| Total | 2,331 (100.0) | 2,448 (100.0) | |
| Pre-ACA | 1,457 (62.5) | 1,426 (58.3) | |
| Post-ACA | 874 (37.5) | 1,022 (41.7) | 0.0027 |
| Median (SD) | 49.0 (9.2) | 50.6 (8.9) | <0.0001 |
| Male | 1,734 (74.4) | 1,849 (75.5) | |
| Female | 597 (25.6) | 599 (24.5) | 0.3621 |
| White | 784 (33.8) | 915 (37.7) | |
| Black | 1,257 (54.2) | 1,085 (44.7) | |
| Hispanic | 255 (11.0) | 376 (15.5) | |
| Other | 25 (1.1) | 51 (2.1) | <0.0001 |
| Private | 743 (31.9) | 808 (33.0) | |
| Medicare | 526 (22.6) | 592 (24.2) | |
| Medicaid | 642 (27.5) | 935 (38.2) | |
| Uninsured | 390 (16.7) | 102 (4.2) | |
| Other | 30 (1.3) | 11 (0.4) | <0.0001 |
| NCI Designated | 287 (12.6) | 456 (19.3) | |
| Comprehensive | 612 (26.9) | 441 (18.6) | |
| Teaching | 849 (37.3) | 1,050 (44.3) | |
| Community | 105 (4.6) | 185 (7.8) | |
| Other | 426 (18.7) | 236 (10.0) | <0.0001 |
| < $36000 | 842 (36.3) | 656 (26.9) | |
| $36000 – $43999 | 492 (21.2) | 432 (17.7) | |
| $44000 – $52999 | 454 (19.6) | 405 (16.6) | |
| $53000 – $68999 | 358 (15.4) | 498 (20.4) | |
| $69000+ | 174 (7.5) | 447 (18.3) | <0.0001 |
| DLBCL | 559 (24.0) | 538 (22.0) | |
| HL | 227 (9.7) | 230 (9.4) | |
| Head and Neck | 178 (7.6) | 225 (9.2) | |
| Cervix | 86 (3.7) | 64 (2.6) | |
| Lung | 436 (18.7) | 422 (17.2) | |
| Colorectal | 149 (6.4) | 161 (6.6) | |
| Esophagus | 24 (1.0) | 38 (1.6) | |
| Stomach | 39 (1.7) | 34 (1.4) | |
| Pancreas | 56 (2.4) | 62 (2.5) | |
| Breast | 126 (5.4) | 124 (5.1) | |
| Anal | 283 (12.1) | 307 (12.5) | |
| Prostate | 168 (7.2) | 243 (9.9) | 0.0001 |
Non-expansion states include: AK, AL, FL, GA, ID, IN, KS, LA, ME, MO, MS, MT, NE, NC, OK, PA, SC, SD, TN, TX, UT, VA, WI, WY
Expansion states include: AZ, AR, CA, CO, CT, DC, DE, HI, IL, IA, KY, MA, MD, MN, NJ, NM, NV, NY, ND, OH, OR, RI, VT, WA, WV
Abbreviations: ACA = Affordable Care Act, SD = Standard Deviation, NCI = National Cancer Institute, DLBCL = Diffuse Large B-Cell Lymphoma, HL = Hodgkin Lymphoma
In non-expansion states, PLWHC were more often uninsured (16.7% vs 4.2%, p<0.0001), treated at comprehensive community cancer programs (26.9% vs. 18.6%, p<0.0001), identified as Black race (54.2% vs. 44.7%, p<0.0001), and resided in areas with lower median incomes (36.3% vs 26.9% in areas with median income <$36,000, p<0.0001) as compared to PLWHC in expansion states. PLWHC in expansion states were more likely to be White (37.7% vs. 33.8%) and to be treated at a teaching/academic research program (44.3% vs. 37.3%) compared to those in non-expansion states (all p<0.0001).
Insurance Coverage
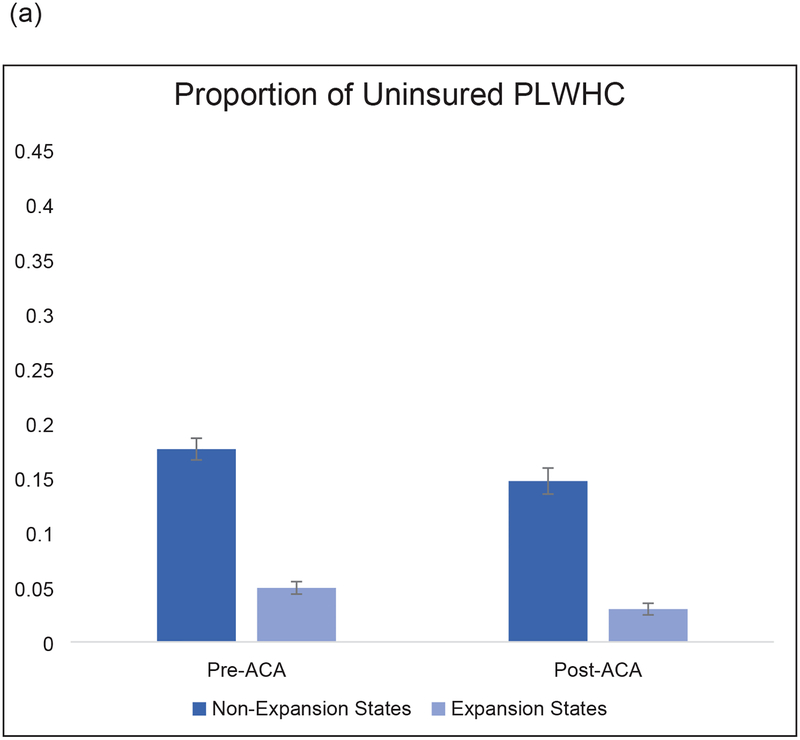
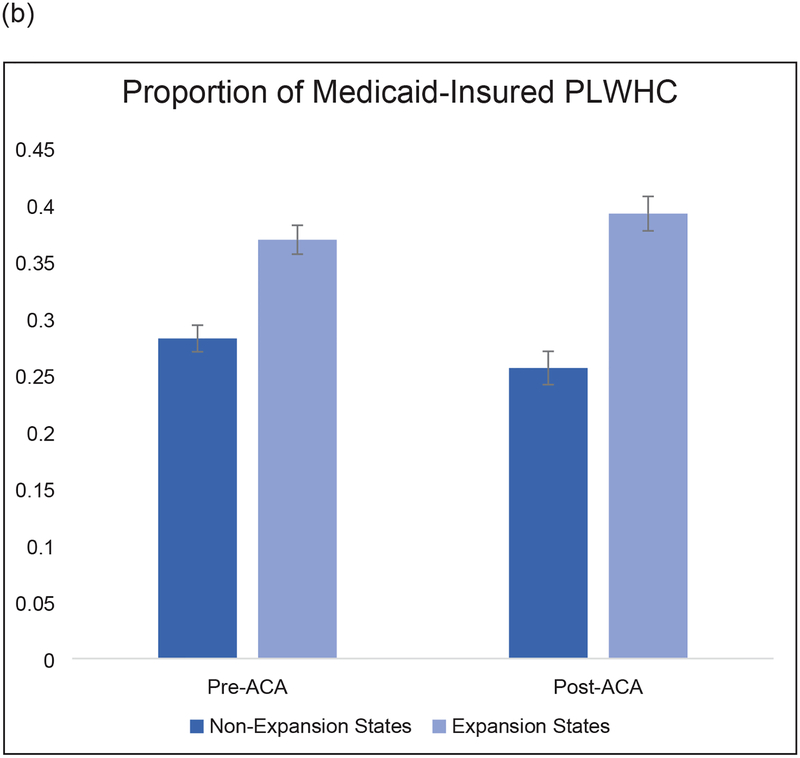
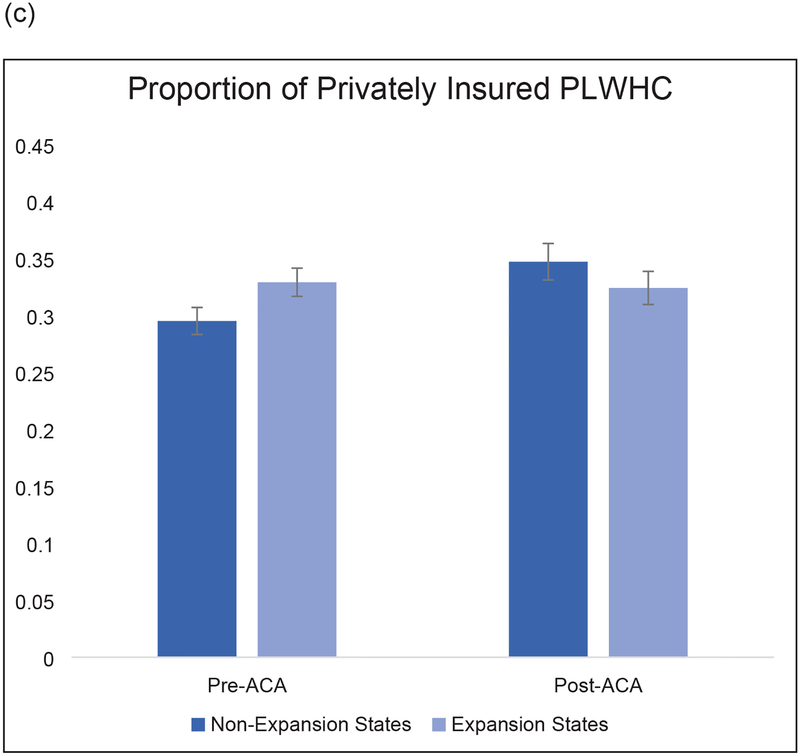
Across all states, the percent uninsured among PLWHC decreased from 11.5% pre-ACA to 8.5% post-ACA. The number of uninsured PLWHC was significantly higher in non-expansion states compared with expansion states (Figure 1a). Table 2a shows DD estimates of the changes in percentage of PLWHC with Medicaid, private insurance, or no insurance. As expected, after adjustment for sociodemographic factors, there was increased Medicaid coverage in expansion states as compared to non-expansion states (DD: 5.8 percentage points (pp); p=0.02) post-ACA (Figure 1b). In contrast, there was a significant increase in privately insured PLWHC in non-expansion states compared to expansion states (DD: −5.6 pp; P=0.03) (Figure 1c). As a result, the percentage of uninsured patients decreased in both expansion and non-expansion states (DD: 1.0 pp; p=0.6).
Figure 1:
Proportion of (a) uninsured (b) Medicaid-insured and (c) privately-insured HIV-infected cancer patients in non-Medicaid expansion states and Medicaid expansion states.
Table 2:
Difference-in-differences analysis for (a) insurance coverage and (b) cancer treatment receipt with cancer treatment facility type in non-Medicaid expansion states versus Medicaid expansion states.
| Non-Expansion | Expansion | Unadjusted | Adjusted† | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-ACA | Post-ACA | Difference | P-value | Pre-ACA | Post- ACA | Difference | P-value | DID (95% CI) | P-value | DID (95% CI) | P-value | |
| Uninsured | 17.6% | 14.7% | −2.9 (−6.0, 0.1) | 0.0605 | 4.94% | 3% | −1.9 (−3.5, −0.4) | 0.0129 | 1.0 (−2.4, 4.4) | 0.5761 | 1.0 (−2.9, 4.9) | 0.6045 |
| Medicaid Insurance | 28.2% | 25.6% | −2.6 (−6.3, 1.1) | 0.163 | 36.9% | 39.2% | 2.3 (−1.6, 6.2) | 0.2432 | 4.9 (−0.4, 10.3) | 0.0708 | 5.8 (0.8, 10.9) | 0.0236 |
| Private Insurance | 29.5% | 34.7% | 5.2 (1.3, 9.1) | 0.0092 | 32.9% | 32.4% | −0.5 (−4.2, 3.3) | 0.7959 | −5.7 (−11.1, −0.3) | 0.0396 | −5.6 (−10.8, −0.5) | 0.0333 |
| Non-Expansion | Expansion | Unadjusted | Adjusted† | |||||||||
| Pre-ACA | Post-ACA | Difference | P-value | Pre-ACA | Post- ACA | Difference | P-value | DID (95% CI) | P-value | DID (95% CI) | P-value | |
| Received Cancer Treatment | 82.2% | 85.2% | 3.1 (−0.9, 7.0) | 0.1316 | 83.7% | 85.1% | 1.4 (−2.5, 5.3) | 0.4872 | −1.7 (−7.2, 3.9) | 0.5555 | −1.1 (−6.5, 4.3) | 0.6921 |
| NCI Designated | 13.6% | 13.2% | −0.4 (−3.5, 2.7) | 0.7955 | 20% | 19.6% | −0.4 (−3.8, 3.1) | 0.8201 | 0.0 (−4.6, 4.6) | 0.9969 | −0.5 (−5.1, 4.2) | 0.8477 |
| Comprehensive | 22.9% | 27.4% | 4.5 (0.6, 8.5) | 0.0253 | 17.4% | 19.7% | 2.3 (−1.1, 5.7) | 0.1856 | −2.3 (−7.5, 3.0) | 0.397 | −3.1 (−8.1, 2.0) | 0.2368 |
| Teaching | 37.1% | 37% | −0.1 (−4.4, 4.3) | 0.9821 | 40.2% | 46.7% | 6.5 (2.2, 10.8) | 0.0029 | 6.6 (0.4, 12.7) | 0.0363 | 7.2 (1.1, 13.3) | 0.0217 |
| Community | 3.79% | 5.59% | 1.8 (−0.2, 3.8) | 0.0718 | 8.2% | 5.06% | −3.1 (−5.3, −1.0) | 0.0036 | −4.9 (−7.8, −2.1) | 0.0008 | −4.6 (−7.5, −1.8) | 0.0015 |
| Other | 19.3% | 16% | −3.3 (−6.7, 0.1) | 0.0599 | 9.6% | 8.88% | −0.7 (−3.2, 1.8) | 0.5692 | 2.6 (−1.7, 6.8) | 0.2356 | 2.8 (−1.5, 7.0) | 0.1984 |
Adjusted for: age, sex, race/ethnicity, year of diagnosis, and zip-code level median income quintile
Cancer Treatment Receipt
Table 2b shows DD estimates of the changes in percentage of PLWHC who received cancer treatment and the facilities where these patients received their treatment. While there was no change in the percent of patients who received cancer treatment post-ACA, there was a significant increase in the percent of PLWHC who received treatment at teaching/academic research programs in expansion states, from 40.2% pre-ACA to 46.7% post-ACA (p=0.003), but not in non-expansion states (DD: 7.2 pp; p=0.02). Overall, PLWHC with private insurance were more likely to receive treatment (87.2%) than those with Medicaid coverage (80.8%) or who were uninsured (79.7%) (Table 3).
Table 3:
Receipt of cancer treatment among PLWHC from 2011 to 2015, stratified by insurance type.
| Insurance Type | Cancer Treatment Receipt Rate‡ |
|---|---|
| Private | 87.20% |
| Medicare | 86.05% |
| Medicaid | 80.77% |
| Uninsured | 79.70% |
| Other† | 83.88% |
Other includes: Non-Medicare and Non-Medicaid government-funded insurance
Adjusted for: age, sex, race/ethnicity, year of diagnosis, and zip-code level median income quintile
DISCUSSION
In this national study of people living with HIV and newly diagnosed with cancer, we found that insurance coverage improved in both Medicaid-expansion and non-expansion states after the ACA’s implementation. The improved insurance coverage in non-expansion states was driven by increases in private insurance as compared to the increased Medicaid coverage which occurred primarily in expansion states. However, even post-ACA, the percentage uninsured was five times higher in non-expansion states than in expansion states. Nearly half of the U.S. HIV population lives in non-expansion states, and PLWHC in these states are more likely to have lower income. Thus, the most vulnerable PLWHC live in geographic locations associated with poor insurance coverage accessibility.
In the general cancer population, certain demographic risk factors, such as non-White race and low income, are associated with decreased receipt of cancer treatment.26–28 Though there was no difference in receipt of cancer treatment between non-expansion and expansion states in our study, PLWHC in non-expansion states were more likely to be non-White race and reside in low-income areas, therefore suggesting that they may be at higher risk for sub-optimal cancer treatment and subsequently poor outcomes due to sociodemographic factors. Post-ACA, PLWHC in expansion states were more likely to be treated at teaching and academic research programs, where they may receive more specialized or integrated cancer and HIV care with greater access to clinical trials.29, 30 This could be due to Medicaid expansion or other factors. However, further insurance coverage options are needed to ensure access to appropriate cancer services, including prevention, screening, diagnosis, management, and surveillance, for uninsured PLWHC in non-expansion states.
Other studies of the general cancer population have demonstrated that access to cancer control services is enhanced by the ACA. People living in Medicaid-expansion states are more likely to be up-to-date with cancer screening as compared to those living in non-expansion states.6, 31 Medicaid expansion is also associated with earlier stage at diagnosis among newly diagnosed cancer patients3, 4 and receipt of radiation therapy as part of their cancer treatment regimen.2 Furthermore, cancer survivors living in expansion states have greater access to cancer surveillance and routine follow-up care.32 Finally, people living in expansion states are more likely to be tested and treated for HIV.13, 33 Although our study demonstrates similar benefits from the ACA among those living in expansion states, we found that a large proportion of the non-white and low income population of PLWHC lived in non-expansion states. Thus, our results highlight the need for additional Medicaid expansion particularly to populations at risk for receiving less or suboptimal cancer care.
We did not find significant differences in receipt of cancer treatment among PLWHC, potentially due to the relatively short follow-up period after the full implementation of Medicaid expansion, introduction of private insurance coverage options through Marketplace, and other ACA policy changes in 2014. Healthcare access is complex and multifactorial, and although insurance status is an important contributor, there are other factors leading to cancer care disparities and poor cancer outcomes.34, 35 Our prior work has demonstrated that even after controlling for insurance status, HIV was associated with lack of cancer treatment receipt.17 Nonetheless, insurance coverage for basic cancer services is an important first step towards mitigating disparities among PLWHC.
This study has several strengths, including the use of a nationwide comprehensive database, which makes this among the largest published studies of PLWHC. This study also has several limitations. First, this data is not population-based because the NCDB data comes only from hospitals that have cancer programs accredited through the American College of Surgeons Commission on Cancer. However, the NCDB covers 72% of newly diagnosed cancer patients in the United States36 and prior studies of the effects of the ACA on insurance coverage and stage at diagnosis based on the NCDB4 were remarkably similar to those based on population-based cancer registries.3 Second, health insurance coverage is collected only once in the NCDB. Therefore, we are not able to distinguish patients who were uninsured before diagnosis and gained Medicaid coverage due to their cancer diagnosis from those who were continuously insured by Medicaid. We were also not able to include patients with liver cancer in this analysis due to the wide range of therapy options (e.g. transarterial chemoembolization, transplantation) that are not captured in detail in the NCDB. Finally, due to the delay between healthcare policy implementation and causative survival benefit, currently available data are insufficient to fully evaluate the association between insurance expansion and cancer outcomes. The period following full implementation of the ACA in 2014 was somewhat limited, particularly for states which expanded in 2015. Accordingly, our small effect size was anticipated given the limited follow-up in the post-ACA period. Ongoing evaluation of the potential benefits of the ACA on cancer survival for PLWHC will be important for future research.
This study is the first to measure the benefits of the ACA on insurance coverage and cancer treatment receipt in PLWHC. The findings highlight that a significant proportion of PLWHC in the U.S. are at risk for uninsurance, which may exacerbate already existing disparities in cancer treatment and outcomes. There is an urgent need for further insurance expansion to improve access to care and cancer outcomes for PLWHC in all states.
Supplementary Material
Acknowledgement:
The data used in the study are derived from a limited data set of the National Cancer Database (NCDB). The authors acknowledge the efforts of the American College of Surgeons, the Commission on Cancer, and the American Cancer Society in the creation of the NCDB. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology employed, or the conclusions drawn from these data by the authors.
Funding: This project was supported by American Cancer Society Intramural Research Funding and the intramural program of the National Cancer Institute. Gita Suneja is supported by grants K08CA228631 and P30AI064518 from the US National Institutes of Health.
Footnotes
Conflicts of Interest: At the time this work was completed, Leticia Nogueira, K. Robin Yabroff, Chun Chieh Lin, Xuesong Han, and Ahmedin Jemal were employed by the American Cancer Society, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector, for research outside the submitted work. They were not funded by or key personnel for any of these grants, and their salaries were solely funded through American Cancer Society funds. The other authors declared no conflicts of interest.
REFERENCES
- 1.Obama B. United States Health Care Reform: Progress to Date and Next Steps. Jama. 2016;316: 525–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chino F, Suneja G, Moss H, Zafar SY, Havrilesky L, Chino J. Health Care Disparities in Cancer Patients Receiving Radiation: Changes in Insurance Status After Medicaid Expansion Under the Affordable Care Act. Int J Radiat Oncol Biol Phys. 2017. [DOI] [PubMed] [Google Scholar]
- 3.Han X, Yabroff KR, Ward E, Brawley OW, Jemal A. Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act. JAMA Oncol. 2018;4: 1713–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jemal A, Lin CC, Davidoff AJ, Han X. Changes in Insurance Coverage and Stage at Diagnosis Among Nonelderly Patients With Cancer After the Affordable Care Act. J Clin Oncol. 2017;35: 3906–3915. [DOI] [PubMed] [Google Scholar]
- 5.Brooks GA, Hoverman JR, Colla CH. The Affordable Care Act and Cancer Care Delivery. The Cancer Journal. 2017;23: 163–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sabik LM, Tarazi WW, Bradley CJ. State Medicaid expansion decisions and disparities in women’s cancer screening. Am J Prev Med. 2015;48: 98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wharam JF, Zhang F, Landon BE, LeCates R, Soumerai S, Ross-Degnan D. Colorectal Cancer Screening in a Nationwide High-deductible Health Plan Before and After the Affordable Care Act. Med Care. 2016;54: 466–473. [DOI] [PubMed] [Google Scholar]
- 8.Soni A, Simon K, Cawley J, Sabik L. Effect of Medicaid Expansions of 2014 on Overall and Early-Stage Cancer Diagnoses. Am J Public Health. 2018;108: 216–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dixon MS, Cole AL, Dusetzina SB. Out-of-Pocket Spending Under the Affordable Care Act for Patients With Cancer. Cancer J. 2017;23: 175–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Obamacare and You If You Have a Pre Existing Condition Health Reform. Menlo Park, CA: Kaiser Family Foundation, 2013. [Google Scholar]
- 11.Brennan C. ACA and HIV: opportunities and challenges. HIV Clin. 2014;26: 1, 4–6. [PubMed] [Google Scholar]
- 12.Hood JE, Buskin SE, Anderson BJ, et al. A cross-jurisdictional evaluation of insurance coverage among HIV care patients following the Affordable Care Act. AIDS Care. 2017;29: 511–515. [DOI] [PubMed] [Google Scholar]
- 13.Satre DD, Altschuler A, Parthasarathy S, Silverberg MJ, Volberding P, Campbell CI. Implementation and Operational Research: Affordable Care Act Implementation in a California Health Care System Leads to Growth in HIV-Positive Patient Enrollment and Changes in Patient Characteristics. J Acquir Immune Defic Syndr. 2016;73: e76–e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silva A, Molina Y, Hunt B, Markossian T, Saiyed N. Potential impact of the Affordable Care Act’s preventive services provision on breast cancer stage: A preliminary assessment. Cancer Epidemiol. 2017;49: 108–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robbins AS, Han X, Ward EM, Simard EP, Zheng Z, Jemal A. Association Between the Affordable Care Act Dependent Coverage Expansion and Cervical Cancer Stage and Treatment in Young Women. Jama. 2015;314: 2189–2191. [DOI] [PubMed] [Google Scholar]
- 16.Smith CJ, Ryom L, Weber R, et al. Trends in underlying causes of death in people with HIV from 1999 to 2011 (D:A:D): a multicohort collaboration. Lancet. 2014;384: 241–248. [DOI] [PubMed] [Google Scholar]
- 17.Suneja G, Lin CC, Simard EP, Han X, Engels EA, Jemal A. Disparities in cancer treatment among patients infected with the human immunodeficiency virus. Cancer. 2016;122: 2399–2407. [DOI] [PubMed] [Google Scholar]
- 18.Han X, Jemal A, Hulland E, et al. HIV Infection and Survival of Lymphoma Patients in the Era of Highly Active Antiretroviral Therapy. Cancer Epidemiol Biomarkers Prev. 2017;26: 303–311. [DOI] [PubMed] [Google Scholar]
- 19.Suneja G, Coghill A. Cancer care disparities in people with HIV in the United States. Curr Opin HIV AIDS. 2017;12: 63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coghill AE, Shiels MS, Suneja G, Engels EA. Elevated Cancer-Specific Mortality Among HIV-Infected Patients in the United States. J Clin Oncol. 2015;33: 2376–2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shiels MS, Pfeiffer RM, Gail MH, et al. Cancer burden in the HIV-infected population in the United States. J Natl Cancer Inst. 2011;103: 753–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seaberg EC, Wiley D, Martinez-Maza O, et al. Cancer incidence in the multicenter AIDS Cohort Study before and during the HAART era: 1984 to 2007. Cancer. 2010;116: 5507–5516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lerro CC, Robbins AS, Phillips JL, Stewart AK. Comparison of cases captured in the national cancer data base with those in population-based central cancer registries. Ann Surg Oncol. 2013;20: 1759–1765. [DOI] [PubMed] [Google Scholar]
- 24.Data Items and Record Layout for Submissions to NCDB Made During 2015 Using NAACCR Layout 12.0 Specifications (CS version 2.05) In: Cancer Co, editor. Chicago, IL: American College of Surgeons, 2014. [Google Scholar]
- 25.Lin CC, Virgo KS, Robbins AS, Jemal A, Ward EM. Comparison of Comorbid Medical Conditions in the National Cancer Database and the SEER-Medicare Database. Ann Surg Oncol. 2016;23: 4139–4148. [DOI] [PubMed] [Google Scholar]
- 26.Shavers VL, Brown ML. Racial and ethnic disparities in the receipt of cancer treatment. J Natl Cancer Inst. 2002;94: 334–357. [DOI] [PubMed] [Google Scholar]
- 27.Gross CP, Smith BD, Wolf E, Andersen M. Racial disparities in cancer therapy: did the gap narrow between 1992 and 2002? Cancer. 2008;112: 900–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Du XL, Lin CC, Johnson NJ, Altekruse S. Effects of individual-level socioeconomic factors on racial disparities in cancer treatment and survival: findings from the National Longitudinal Mortality Study, 1979–2003. Cancer. 2011;117: 3242–3251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meguid RA, Brooke BS, Chang DC, Sherwood JT, Brock MV, Yang SC. Are surgical outcomes for lung cancer resections improved at teaching hospitals? Ann Thorac Surg. 2008;85: 1015–1024; discussion 1024–1015. [DOI] [PubMed] [Google Scholar]
- 30.David JM, Ho AS, Luu M, et al. Treatment at high-volume facilities and academic centers is independently associated with improved survival in patients with locally advanced head and neck cancer. Cancer. 2017;123: 3933–3942. [DOI] [PubMed] [Google Scholar]
- 31.Choi SK, Adams SA, Eberth JM, et al. Medicaid Coverage Expansion and Implications for Cancer Disparities. Am J Public Health. 2015;105 Suppl 5: S706–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tarazi WW, Bradley CJ, Harless DW, Bear HD, Sabik LM. Medicaid expansion and access to care among cancer survivors: a baseline overview. J Cancer Surviv. 2016;10: 583–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wagner Z, Wu Y, Sood N. The Affordable Care Act may increase the number of people getting tested for HIV by nearly 500,000 by 2017. Health Aff (Millwood). 2014;33: 378–385. [DOI] [PubMed] [Google Scholar]
- 34.Pan HY, Walker GV, Grant SR, et al. Insurance Status and Racial Disparities in Cancer-Specific Mortality in the United States: A Population-Based Analysis. Cancer Epidemiol Biomarkers Prev. 2017;26: 869–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Walker GV, Grant SR, Guadagnolo BA, et al. Disparities in stage at diagnosis, treatment, and survival in nonelderly adult patients with cancer according to insurance status. J Clin Oncol. 2014;32: 3118–3125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mallin K, Browner A, Palis B, et al. Incident Cases Captured in the National Cancer Database Compared with Those in U.S. Population Based Central Cancer Registries in 2012–2014. Ann Surg Oncol. 2019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.