Abstract
Background:
Alcohol and other drug (AOD) problems are among the most stigmatized conditions globally diminishing help-seeking due to fear of discrimination. Discrimination is common also among people already in AOD recovery, but little is known about the prevalence and nature of perceived discrimination. Greater knowledge would inform treatment and policy.
Method:
Nationally representative cross-sectional sample of U.S. adults who reported resolving an AOD problem (final weighted sample n = 2002). Participants were asked, “Since resolving your problem with alcohol or drugs, how frequently have the following occurred because someone knew about your alcohol or drug history?”.
Measures:
Item response models yielded two types of discrimination: 1. Micro discrimination (personal slights) 2. Macro discrimination (violations of personal rights); psychological distress, quality of life, and recovery capital.
Results:
About one quarter of participants reported some type of micro discrimination (e.g., held to a higher standard) with slightly less reporting a violation of personal rights (e.g., couldn’t get a job). After adjusting for addiction severity and years since problem resolution, greater micro and macro discrimination were associated with higher psychological distress (β = .45, 95% CI = .35,.55 and β = .59, 95% CI = .45,.73), lower quality of life (β =−.41, 95% CI=−.57,−.26 and β =−.49, 95% CI=−.76,−.21) and recovery capital (β =−.33, 95% CI=−.54,−.12 and β =−.68, 95% CI=−.97,−.40) respectively.
Conclusions:
Despite being in recovery, different types of discrimination are experienced. These are associated with increased distress, and lower quality of life and recovery capital. Prospective studies are needed to help clarify the exact nature and impact of such discrimination on AOD problem recurrence.
Keywords: Recovery, Addiction, Discrimination, Substance, Remission, Item response modeling
1. Introduction
Alcohol and other drug (AOD) problems are common in middle and high income countries and confer a prodigious burden in terms of disease, disability, and premature mortality, as well as economic cost (Bouchery et al., 2011; Gore et al., 2011; World Health Organization [WHO], 2008, 2011). Unlike other chronic disorders, such as diabetes or hypertension, AOD disorders tend to have negative effects on significant others and society more broadly in terms of public safety and crime (e.g., driving under the influence; assault; theft) (Humphreys, 2017; Office of the Surgeon General, 2016; Sacks et al., 2015) resulting in more stigmatizing and discriminatory practices towards those with AOD problems. AOD disorders’ greater propensity to generate stigmatizing attitudes can result in greater public, and internalized, shame and stigma among sufferers, that may lower the chances that affected individuals will acknowledge a problem, seek treatment (Kelly and Westerhoff, 2010; Keys et al., 2010), remain in treatment (Brener et al., 2010), and seek or receive social support (Birtel et al., 2017). In turn, this can result in a lengthy clinical course for these disorders (Dennis et al., 2005; Fleury et al., 2016; Kelly et al., 2017). Furthermore, there has been an emphasis (Office of the Surgeon General, 2016) to understand recovery not only among those with provider defined remission but also among person-centered definitions of problem resolution (National Academies of sciences, Engineering, and Medicine, 2017) given three-quarters of the yearly economic burden is attributable to consequences of hazardous / harmful alcohol consumption patterns that do not meet diagnostic criteria (Center for Behavioral Health Statistics and Quality, 2016). Discriminatory practices against people with AOD disorders can increase psychological distress (Cruz et al., 2018) and lower quality of life (Sarin et al., 2013). Anecdotal reports suggest affected individuals suffer continued discrimination even after they have resolved a significant AOD problem and achieved long-term remission and recovery, which may undermine ongoing recovery efforts and quality of life. This may be especially true during the first five years of recovery when vulnerability to relapse remains elevated (White, 2012).
Such discrimination can take the form of perceived personal slights, or what we call “micro discriminations” (e.g., an individual is perceived as untrustworthy, dishonest, or always about to relapse); or, violations of personal rights, or what we label, “macro discriminations” (e.g., being denied the right to vote or obtain employment or accommodation) all because someone knew of that individual’s prior AOD problem history.
While such anecdotes are common enough, almost nothing is known from a systematic standpoint regarding the nature, prevalence, and correlates, of micro and macro discriminations that may be experienced by individuals after successful resolution of significant AOD problems. Further, it is unclear the extent to which recovery-related discrimination may be related to psychological distress, quality of life, and the accrual of recovery capital. Greater knowledge obtained through national prevalence estimates would enhance understanding regarding just how common such experiences are after resolving an AOD problem and inform clinical and public health efforts designed to help individuals cope more effectively with specific perceived discrimination and to identify and reduce any systematic societal discriminatory barriers to recovery.
The principal aim of this study was to address this knowledge gap of micro and macro discriminations in a nationally-representative sample of U.S. adults who have successfully resolved an AOD problem in order to determine the nature, prevalence, and correlates of recovery-related discrimination. To this end, this study had the following aims: 1. estimate the nature and national prevalence of micro and macro discriminations that are experienced by people after resolving an AOD problem in the U.S.; 2. Examine the preliminary psychometric properties of a novel scale of micro and macro discriminations; and, 3. Test the associations between the experiences of micro discrimination and macro discrimination and psychological distress, quality of life, and recovery capital. It was hypothesized that individuals who reported high levels of recovery-related discrimination, would report higher levels of psychological distress, and lower levels of quality of life and recovery capital.
2. Method
2.1. Study design
The National Recovery Survey (NRS) target population was the U.S. noninstitutionalized civilian population 18 years or older that screened positive to the web-based survey item, “Did you used to have a problem with drugs or alcohol, but no longer do?” Data were collected by the survey company GfK, using its “KnowledgePanel” pool of participants who, when necessary, were provided with web-enabled computer and free Internet service to include households that a) have unlisted telephone numbers, b) do not have landline telephones, c) are cell phone only, d) do not have current internet access, and e) do not have devices to access the internet.
The NRS employed a cross-sectional, equal probability of selection method sampling to recruit from an address-based sampling frame that covered 97% of U.S. households from which a representative subset of 39,809 were invited to participate and 25,229 (63.4%) responded to the screener item (yes/no) yielding a weighted prevalence estimate of 9.1% (SE = 0.3) of U.S. adults who endorsed having resolved a problem with drugs or alcohol. Of the participants who responded “yes” to the screener a representative 2047 were invited to complete the full survey and 2002 remained in the final sample after excluding surveys deemed invalid (e.g., unrealistic survey completion time, qualitative responses indicated they accidently selected “yes”). The survey was piloted on 20 individuals over 3 days in July 2016. Data were collected in July and August 2016.
To produce unbiased estimates of population parameters from the participants we used iterative proportional fitting (Battaglia et al., 2009) which accounts for unequal selection probabilities. Weights were first computed from a general population sample via comparisons to benchmarks from the March 2015 Current Population Survey (United States Census Bureau, 2015) along eight dimensions: (1) gender (male/female); (2) age (18–29, 30–44, 45–59, and 60+ years); (3) race/Hispanic ethnicity (White/Non-Hispanic, Black/Non-Hispanic, Other/Non-Hispanic, 2+ Races/Non-Hispanic, Hispanic); (4) education (Less than High School, High School, Some College, Bachelor and beyond); (5) census geographical region (Northeast, Midwest, South, West); (6) household income (under $10k, $10 K–$25k, $25 K– < $50k, $50 K– < $75k, $75+); (7) home ownership status (Own, Rent/ Other); and (8) metropolitan area (yes/no). A second weight was then derived from the qualified respondents only (i.e., the 9.1% of U.S. adults who endorsed yes to the screener item) to realign the geodemographic composition of the final sample (N = 2002 adults) to the target population (i.e., U.S. adults who have resolved a problem with alcohol or drugs) to produce unbiased estimates from the survey data. Thus, the NRS is the first nationally representative survey of adults who identify as having resolved a problem with drugs or alcohol. Details regarding the sampling procedures of the NRS can be found elsewhere (Kelly et al., 2017). Protocols were approved by the institutional review boards at Partners Healthcare and GfK.
2.2. Sample
Weighted responses are presented in Table 1 to describe the demographic and clinical characteristics of the 22.35 million adults, or 9.1% of the U.S. population who self-identify as having resolved a problem with drugs or alcohol.
Table 1.
Characteristics of the 9.1% of U.S. adults who endorsed they used to have a problem with drugs or alcohol, but no longer do (weighted percentages based off N = 2002).
| Characteristics | weighted % | SE |
|---|---|---|
| Age | ||
| 18-24 | 7.1 | 1.2 |
| 25-49 | 45.2 | 1.6 |
| 50-60 | 34.7 | 1.4 |
| 65+ | 13.0 | 0.8 |
| Male | 60.0 | 1.5 |
| White non-Hispanic | 61.4 | 1.6 |
| Employed Currently | 54.7 | 0.9 |
| Homeless in Past 90 Days | 0.9 | 0.4 |
| Arrested Ever | 51.0 | 1.6 |
| Heterosexual or Straight | 84.1 | 1.3 |
| Clinical Characteristics | ||
| Years since problem resolution | ||
| 0-5 years | 34.5 | 1.6 |
| 5-15 years | 35.2 | 1.5 |
| 15+ years | 29.3 | 1.3 |
| did not indicate | 0.6 | 0.3 |
| Abstinent from all substances currently | 51.6 | 0.9 |
| Number of problem substances lifetime | 1.5 | 1.4 |
| Age of onset regular weekly use | 17.7 | 6.0 |
| Primary substance | ||
| Alcohol primary substance | 51.2 | 1.6 |
| Cannabis | 11.0 | 1.1 |
| Cocaine (e.g., coke, crack, freebase) | 10.0 | 0.9 |
| Methamphetamine (crank, meth, crystal) | 7.3 | 0.9 |
| Opioids (e.g., heroin, unprescribed fentanyl, methadone) | 5.3 | 0.8 |
| Other | 2.6 | 0.5 |
| did not identify a problem substance | 12.7 | 1.1 |
| Ever received substance use disorder diagnosis | 17.0 | 1.9 |
| Ever received mental health diagnosis | 36.0 | 1.3 |
| Ever used treatment or recovery support services | 53.9 | 1.6 |
2.3. Measures
2.3.1. The recovery-related discrimination scale (RRDS)
The recovery-related discrimination scale (RRDS) was designed to assess the self-reported perceived frequency of experiences with personal slights and violation of personal rights that occurred among people who have resolved an AOD problem due to people finding out about their prior AOD history. We derived an original pool of items using a rational keying approach, which is based on theory (Cucina et al., 2012), that included a review of the mental health literature regarding discrimination against individuals with mental illness and addiction and recovery literature more broadly, in addition to the literature on race-based discrimination. We also reviewed policies that govern the rights of those convicted of drug offenses such as the Higher Education Act which delayed or denied federal financial aid assistance for higher education, the Personal Responsibility and Work Opportunity Reconciliation Act which enacted a lifetime ban for receipt of food or cash assistance (and was imposed for no other offense but drug crimes), felony disenfranchisement laws which restrict or deny the right to vote, and the Alcohol Exclusion Law which allowed insurance companies to deny reimbursement to hospitals for treatment to those who are injured while impaired by unprescribed drugs or alcohol. This resulted in an initial pool of 25 items reflecting a variety of different types of micro and macro discriminations (see Appendix A). The frequency of the occurrence of each item was tested in response to a stem question: “Since resolving your problem with alcohol or drugs, how frequently have the following occurred because someone knew about your alcohol or drug history?” with respondents asked to choose from one of four possible frequency response options: never, once or twice, a few times, often (coded from 1 to 4, respectively). Scale refinement is detailed below. Ultimately the recovery-related micro discrimination sub-scale (α = .92; M = 12.4, SE = 0.2; scores can range between 8–32), macro discrimination sub-scale (α = .91; M = 9.4, SE = 0.1; scores can range between 8–32), and total score (α = .92; M = 21.8, SE = 0.3; scores can range 16–62) had high reliability.
2.3.2. Psychological distress
Psychological distress refers to nonspecific serious mental illness. Psychological distress was measured with the K6 (Kessler et al., 2003) using the self-reported six item measure with a 4 point Likert scale. A cut point of 13 or higher is a positive K6 score for serious mental illness in national population studies on the 0–24 scale. The mean score was 4.9 (SE = 0.2) which is well below the cut for serious mental illness; internal consistency was high α = .92.
2.3.3. Quality of life
Quality of life represents an individual's perception of their expectations, standards and concerns regarding their psychological, physical, social, and environmental domains. Quality of life was measured with the 8 item EUROHIS-QOL (Schmidt et al., 2006) which is internationally validated in epidemiological studies, uses a 5 point Likert scale, had high internal consistency α = .90, and a mean score of 29.8 (SE = 0.2) on the 8–40 scale with higher scores indicating greater quality of life.
2.3.4. Recovery capital
Recovery capital represents the personal, social, physical, and professional resources in an individual’s environment that are used to initiate and sustain remission and recovery from substance use disorder. The Brief Assessment of Recovery Capital (BARC-10; Vilsaint et al., 2017) is a ten item measure with a 5 point Likert scale that is internationally validated, had high internal consistency α = .91, scores can range between 10–60 with higher scores indicating more recovery capital. The mean score was 47 (SE = 0.3) for adults in the U.S. who have resolved a former drug or alcohol problem.
2.3.5. Covariates
Severity of former drug or alcohol problem was modeled using six variables which have been associated with a more chronic course of illness, health and social consequences, and thus potentially quality of recovery. Lifetime number of problem substances (M = 1.5, SE = 1.4) (John et al., 2018), age of onset for regular weekly use (M = 17.7 years, SE = 6.0) (Chen et al., 2009; Grant and Dawson, 1998), primary substance alcohol (51.2%, SE = 1.6) versus other drugs (NIDA, 2017), ever received a substance use disorder diagnosis from a healthcare provider (17%, SE = 1.9), ever received a mental health diagnosis from healthcare provider (36%, SE = 1.3) (NIDA, 2018), ever utilized treatment or recovery support services (45.8%, SE = 1.6) (Blanco et al., 2015; Kessler et al., 2001), and number of years since resolving a problem with alcohol or other drugs including 0–5 years (34.4%, SE = 1.6), 5–15 years (35.2%, SE = 1.5), and 15 years or more (29.3%, SE = 1.3).
2.4. Data analysis plan
2.4.1. U.S. Prevalence estimates
First, we describe the nature and U.S. national prevalence rates of perceived recovery-related discrimination among individuals who have resolved a problem with alcohol or other drugs using weighted proportions.
2.4.2. Factor structure and unidimensionality
Next, in order to construct sub-scales of micro and macro discrimination to examine their relationship to other indices of quality of life and functioning, we conducted factor analyses combined with parallel analysis (i.e., data simulation) to eliminate items that failed to yield unidimensional constructs. Parallel analysis resembles that of resampling in the sense that the number of factors extracted should have eigenvalues greater than those in a simulated matrix (Yu et al., 2007). We simulated 1000 permutations based on the observed data of 2002 cases, 24 variables (the item I felt discriminated against was excluded to use later in validity analyses), at the 95th percentile, with principal axis factoring and an oblique Promax rotation (Costello and Osborne, 2005). The unidimensionality analysis was done in SPSS v.24 with aid of publicly available parallel analysis syntax (O’Connor, 2000). Unweighted data was used during measurement construction (section 2.4.2 - 2.4.4) so each observation is modeled to contribute one unit of independent statistical information. The effect of weighting is to distort the distribution of independent statistical information in the data. (Linacre, 2019a).
2.4.3. Differential item functioning (DIF) and item retention
Next, the Partial Credit Model (PCM; Masters, 1982) was used to eliminate items that showed differential item functioning (DIF) in the difficulty parameter according with Mantel Haenszel p < .05. A test item is flagged for DIF when examinees with equal ability (i.e., matched or “controlled for” on the underlying latent trait referred to as theta [θ]), but from different groups, have an unequal probability of endorsing the item. For example, if participants who have been homeless in the past 3 months are more likely to endorse an item compared to non-homeless participants, despite having equivalent levels of recovery-related discrimination, then the item may be detecting discrimination due to homelessness as opposed to recovery-related discrimination. DIF testing can serve as a way to eliminate items that are detecting other constructs or forms of discrimination as evidenced by their invariance across group membership (previously referred to as item bias). We eliminated items flagged for DIF between groups of race-ethnicity (white non-Hispanic, all other race-ethnicity), gender identity (male, female), currently employed (yes, no), mental health diagnosis ever (yes, no), sexual orientation (heterosexual, non-heterosexual), residence (mostly homeless in the past 90 days, non-homeless in the past 90 days) and ever been arrested (yes, no).
2.4.4. Psychometric properties of final scale items
The PCM will be used to perform scale analysis by reporting counts in each response category (n), percentages in each response category, participant ability level (θ) in each response category which is a parameter for the underlying latent trait (i.e., recovery-related discrimination), and the item difficulty parameter (b) which can be used to eliminate items that capture the same degree of difficulty (i.e., item redundancy) using WINSTEPS software (Linacre, 2019b).
2.4.5. Regression models
Then in the final analysis, in order to examine the extent to which the experience of micro and macro discrimination were independently related to psychological distress, quality of life, and recovery capital we computed six multiple regression models, adjusting for addiction severity indicators (i.e., number of problem substances over during their life, age of onset for regular weekly use, primary substance alcohol versus other drugs, ever received substance use disorder diagnosis from healthcare provider, ever received mental health diagnosis from healthcare provider, ever utilized treatment or recovery support services) and number of years since resolution of alcohol or other drug problems. Multiple regression models and prevalence estimates were weighted to represent the adult U.S. population who identify as once having a problem with drugs or alcohol and no longer do, and standard errors were computed using the Taylor linearization method to account for the complex survey design using svyset in STATA version 14 (StataCorp, 2015). We report regression coefficients and R2. To test the significance of change in R2 when micro discrimination and macro discrimination were independently added to a base model of addiction severity, we drew inferences from F-tests. We evaluated statistical significance via two-sided 0.05-level design-based tests.
3. Results
3.1. Prevalence of perceived micro and macro discrimination among individuals who have resolved a drug or alcohol problem
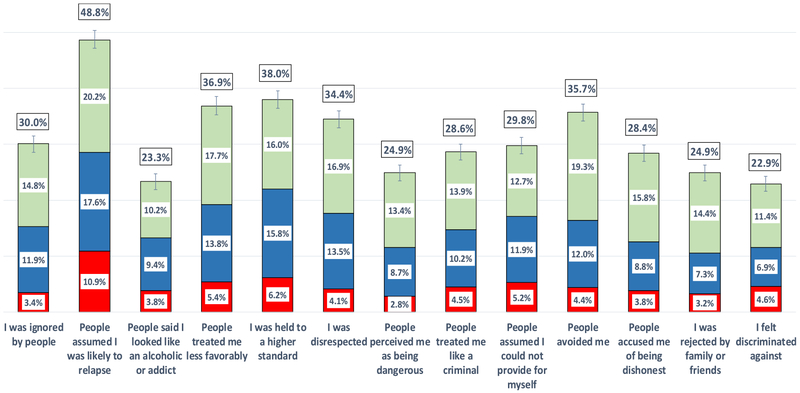
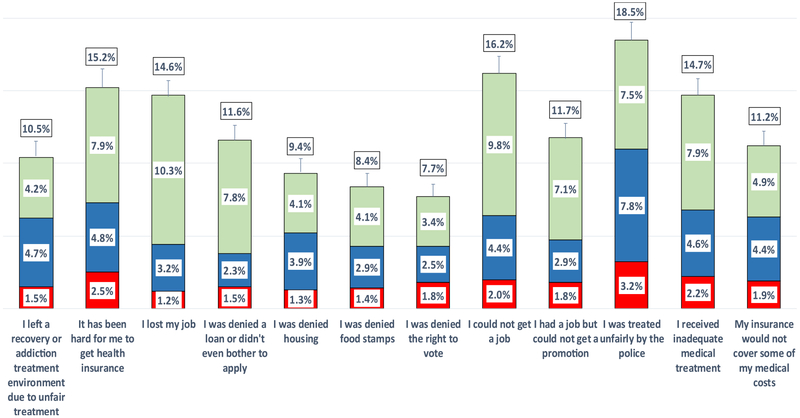
The national prevalence rates of the initial 25 recovery-related discriminations experienced by adults who self-identify as having resolved a drug or alcohol problem are displayed in Fig. 1. This shows experiences that occurred in the context of social-interpersonal exchanges, hereafter referred to as micro discriminations (i.e., personal slights). Fig. 2 shows experiences that occurred at the structural, organizational, or policy level, also referred to as macro discriminations (i.e., violations of personal rights). Overall, experiences that occurred at the level of social-interpersonal exchanges were the most commonly reported. Just under a quarter of the U.S. population (22.9%) who self-identify as having resolved an AOD problem report feeling discriminated by way of at least one micro discrimination because someone knew about their AOD history. The prevalence of these different types of micro discrimination is detailed in Fig. 1. The most commonly reported were People assumed I was likely to relapse experienced by almost half (48.8%), followed by I was held to a higher standard (38.0%), People treated me less favorably (36.9), and People avoided me (35.7%) each of which was reported by more than one third. Overall, rates of micro discrimination were higher than rates of macro discrimination, with the most common macro discrimination being, I was treated unfairly by the police (18.5%), followed by I could not get a job (16.2%), It was hard for me to get health insurance (15.2%), I received inadequate medical treatment (14.7%), and the least common being I was denied the right to vote (7.7%).
Fig. 1.
U.S. prevalence of perceived recovery-related micro discriminations reported by the 9.1% of U.S. adults who have resolved an alcohol or other drug problem.
Fig. 2.
U.S. prevalence of perceived recovery-related macro discriminations reported by the 9.1% of U.S. adults who have resolved an alcohol or other drug problem.
3.2. Scale construction
3.2.1. Factor structure and unidimensionality
Exploratory factor analysis combined with parallel analysis yielded two eigenvalues (λ = 11.6 and 2.0) from the raw data of 24 of the 25 piloted items (one items was excluded to be used in validity analyses following scale construction) that were greater than the 95th percentile criterion value from the simulated data (.24 and .21); therefore, there were two significant and extractable components which accounted for 56% and 9.2% of the variance respectively.
3.2.2. Factor loadings, item retention, and factor labels
The following criteria were used to identify and retain items for further testing on the first component: positive primary loadings above .32 (Tabachnick and Fidell, 2001) that did not produce a negative cross-loading on the second factor (the second factor was characterized by negative loadings). Items were retained in the second factor if it had a negative loading greater than .32. As a result, the following four items were dropped from the second component: I left a recovery or addiction treatment environment because I was treated unfairly, It has been hard for me to get health insurance, I was treated unfairly by the police, I received inadequate medical treatment. Twelve items were retained for further testing on the first factor which loadings ranged from .67-.81. Eight items were retained for additional testing on the second component which loadings ranged from .34-.55.
We labeled the first factor “micro discriminations” as they were characterized by experiences that occurred at the level of interpersonal exchanges such as slights and insults that communicate disparaging or negative messages. The negatively loaded items on the second factor were conceptually distinct in that they described experiences of rights violations that occurred at the level of structural and institutionalized policies and practices, thus we labeled the second component, “macro discriminations.”
3.2.3. Differential item functioning (DIF) and item retention
We found significant DIF in four items from the micro discrimination scale. I was held to a higher standard was more difficult for non-White racial-ethnic groups to endorse compared to White non-Hispanics at the same average level of recovery-related discrimination. People perceived me as being dangerous was more difficult for males and those with an arrest history to endorse, I was rejected by family or friends was harder for females to endorse. People assumed I could not provide for myself was harder for non-White racial-ethnic groups and males to endorse. We eliminated the items flagged for DIF from the micro discrimination scale before completing the scale analysis and final item selection.
3.2.4. Psychometric properties of final micro and macro discrimination sub-scales
Table 2 displays the final 16 items retained in the micro discrimination (8 items) and macro discrimination sub-scales (8 items). Inspection of the average ability parameter (θ) showed a monotonical increase as the rating scale response options moved from lower to higher categories. The category response curves (not displayed) also showed successive response categories each located in the expected order. This meant that each category was the most likely to be endorsed according to a corresponding trait level and the scale is functioning in a way that is consistent with measurement theory. Inspection of the difficulty parameter shows no item redundancy in that each item captured a different level of difficulty, thus improving precision measurement at each level of ability.
Table 2.
Final perceived micro discrimination and macro discrimination sub-scale items with unweighted response category counts (n), response category percentages (%), participant ability estimates (θ), item difficulty, and item-measure correlation.
| Micro Discrimination Items (α = .92) | Never | Once or Twice | A Few Times | Often | Difficulty of Item (b) | Item-Measure Correlation (r) | |
|---|---|---|---|---|---|---|---|
| 1. I was ignored | Count (n) | 1456 | 251 | 203 | 63 | −.35 | 73 |
| % | 73.80 | 12.72 | 10.29 | 3.19 | |||
| Ability (θ) | −3.42 | −1.07 | −0.44 | 0.89 | |||
| 2. People assumed I was likely to relapse | Count (n) | 1101 | 393 | 310 | 172 | .07 | .71 |
| % | 55.72 | 19.89 | 15.69 | 8.70 | |||
| Ability (θ) | −3.91 | −1.79 | −0.94 | 0.03 | |||
| 3. People said I looked like an alcoholic or addict | Count (n) | 1620 | 169 | 140 | 47 | .25 | .7 |
| % | 81.98 | 8.55 | 7.09 | 2.38 | |||
| Ability (θ) | −3.20 | −0.97 | −0.14 | 1.55 | |||
| 4. People treated me less favorably | Count (n) | 1318 | 364 | 214 | 83 | .47 | .64 |
| % | 66.60 | 18.39 | 10.81 | 4.19 | |||
| Ability (θ) | −3.67 | −1.28 | −0.43 | 1.11 | |||
| 5. I was disrespected | Count (n) | 1374 | 312 | 207 | 79 | .46 | .61 |
| % | 69.68 | 15.82 | 10.50 | 4.01 | |||
| Ability (θ) | −3.56 | −1.25 | −0.40 | 1.07 | |||
| 6. People treated me like a criminal | Count (n) | 1533 | 236 | 145 | 61 | −.44 | .77 |
| % | 77.62 | 11.95 | 7.34 | 3.09 | |||
| Ability (θ) | −3.36 | −0.91 | −0.12 | 1.48 | |||
| 7. People avoided me | Count (n) | 1348 | 347 | 193 | 86 | −.14 | .73 |
| % | 68.29 | 17.58 | 9.78 | 4.36 | |||
| Ability (θ) | −3.61 | −1.24 | −0.42 | 1.03 | |||
| 8. People accused me of being dishonest | Count (n) | 1537 | 263 | 121 | 56 | −.31 | .68 |
| % | 77.74 | 13.30 | 6.12 | 2.83 | |||
| Ability (θ) | −3.33 | −0.91 | −0.12 | 1.36 | |||
| Macro Discrimination Items (α = .91) | Never | Once or Twice | A Few Times | Often | Difficulty of Item (b) | Item-Measure Correlation (r) |
|
| 1. I lost my job | Count (n) | 1732 | 171 | 49 | 21 | 0.02 | .68 |
| % | 87.79 | 8.67 | 2.48 | 1.06 | |||
| Ability (θ) | −3.65 | −1.75 | −0.38 | 0.49 | |||
| 2. I was denied a loan or didn’t even both to apply | Count (n) | 1812 | 100 | 35 | 24 | −1.08 | .77 |
| % | 91.93 | 5.07 | 1.78 | 1.22 | |||
| Ability (θ) | −3.61 | −1.02 | −0.46 | 0.65 | |||
| 3. I was denied housing | Count (n) | 1847 | 59 | 45 | 22 | 0.58 | .62 |
| % | 93.61 | 2.99 | 2.28 | 1.12 | |||
| Ability (θ) | −3.57 | −0.93 | −0.16 | 0.85 | |||
| 4. I was denied food stamps | Count (n) | 1868 | 50 | 34 | 21 | −0.32 | .78 |
| % | 94.68 | 2.53 | 1.72 | 1.06 | |||
| Ability (θ) | −3.54 | −0.68 | −0.02 | 0.53 | |||
| 5. I was denied the right to vote | Count (n) | 1877 | 42 | 30 | 27 | −0.59 | .62 |
| % | 94.99 | 2.13 | 1.52 | 1.37 | |||
| Ability (θ) | −3.53 | −0.65 | −0.01 | 0.11 | |||
| 6. I could not get a job | Count (n) | 1746 | 136 | 59 | 33 | −0.19 | .75 |
| % | 88.45 | 6.89 | 2.99 | 1.67 | |||
| Ability (θ) | −3.68 | −1.34 | −0.78 | 0.33 | |||
| 7. I had a job but could not get a promotion | Count (n) | 1776 | 134 | 41 | 23 | 0.54 | .65 |
| % | 89.97 | 6.79 | 2.08 | 1.17 | |||
| Ability (θ) | −3.63 | −1.48 | −0.14 | 0.44 | |||
| 8. My insurance would not cover some of my medical costs | Count (n) | 1788 | 84 | 68 | 34 | 0.3 | .70 |
| % | 90.58 | 4.26 | 3.44 | 1.72 | |||
| Ability (θ) | −3.62 | −1.41 | −0.69 | −0.30 |
Note. Stem question: “Since resolving your problem with alcohol or drugs, how frequently have the following occurred because someone knew about your alcohol or drug history?” Respondents were asked to choose from one of four possible response options (i.e., never, once or twice, a few times, often) scored 1, 2, 3, and 4, respectively.
The recovery-related micro discrimination sub-scale (α = .92; M = 12.4, SE = 0.2; scores can range between 8–32), macro discrimination sub-scale (α = .91; M = 9.41, SE = 0.1; scores can range between 8–32), and total score (α = .92; M = 21.8, SE = 0.3; scores can range 16–62) had high reliability. Exploratory factor analysis of the 8 micro discrimination items confirmed that scale refinement process yielded a single component (eigenvalue λ = 5.2 accounting for 65% of the variance) as did an exploratory factor analysis of the 8 item macro discrimination items (eigenvalue λ = 4.8 accounting for 60.6% of the variance). The two sub-scales have a moderate and significant correlation (r = .55*). The single raw item (I felt discriminated against) reserved for validity tests was correlated with micro discriminations (r = .63*) and macro discriminations (r = .60*).
3.3. Regression models
Last, we computed six multiple regression models statistically adjusted for indicators of addiction severity and number of years since problem resolution and found that micro discrimination had a positive association which independently explained an additional 19% of the variance in psychological distress, a negative association which explained 11% of the variance in quality of life, and a negative association which explained 4% of recovery capital. With regard to macro discrimination, the same adjusted regression analyses found it explained 16%, 8%, and 8%, in psychological distress, quality of life, and recovery capital, respectively (Table 3). Results are displayed separately for participants in long-term recovery (i.e, five years since resolving a problem with alcohol or other drugs) (Dupont et al., 2015). A bivariate correlational analysis showed that time since problem resolution had a significant negative association with micro (−0.23) and macro discrimination (−0.16) implying that the effect of discriminatory experiences decreases with time in recovery. The effect of micro or macro discrimination in early recovery was 2–3 times bigger than in long-term recovery. People in early recovery who are perceiving discrimination are more likely to have significant psychological distress.
Table 3.
Regression coefficients (β), confidence intervals (CI), total percent of variance accounted for (R2), and change in percent of independent variance accounted for by perceived micro discriminations and macro discriminations regressed separately on psychological distress, quality of life, and recovery capital.
| ≤ 5 Years since resolution of alcohol or other drug problem |
> 5 Years since resolution of alcohol or other drug problem |
|||||||
|---|---|---|---|---|---|---|---|---|
| β | 95% CI | Total R2 | Change in R2 | β | 95% CI | Total R2 | Change in R2 | |
| Psychological Distress | ||||||||
| Micro discrimination | .45 | .35, .55 | .36 | .19* | .27 | .18, .36 | .22 | .06* |
| Macro discrimination | .59 | .45, .73 | .33 | .16* | .51 | .31, .70 | .22 | .06* |
| Quality of Life | ||||||||
| Micro discrimination | −.41 | −.57,−.26 | .20 | .11* | −.23 | −.34.−.14 | .12 | .03* |
| Macro discrimination | −.49 | −.76,−.21 | .17 | .08* | −.46 | −.63,−.28 | .12 | .03* |
| Recovery Capital | ||||||||
| Micro discrimination | −.33 | −.54,−.12 | .10 | .04* | −.21 | −.38,−.05 | .06 | .01* |
| Macro discrimination | −.68 | −.97,−.40 | .14 | .08* | −.28 | −.61, .05 | .06 | .01 |
Note. All six models were run separately and adjusted for severity indicators: number of problem substances in lifetime, age of onset for regular weekly use, primary substance alcohol versus other drugs, ever received substance use disorder diagnosis from healthcare provider, ever received mental health diagnosis from healthcare provider, ever utilized treatment or recovery support services, and number of years since problem resolution.
Statistically significant at the .01 level.
4. Discussion
Substance use disorders and related problems are among the most stigmatized problems in many societies globally (Room et al., 2001). While fear of discrimination due to having such a stigmatized AOD condition is known to serve as a barrier to acknowledging a problem and seeking help, little was known about the experience and nature of discrimination after entering recovery from an AOD problem. This nationally-representative study of U.S. adults resolving a significant AOD problem is novel in that it provides estimates of different types of perceived discrimination that occurred because someone knew of that individual’s AOD history. Findings suggest individuals in recovery continue to experience different forms of social-interpersonal and structural discrimination, greater amounts of which are correlated with greater psychological distress, poorer quality of life, and lower recovery capital.
We found that roughly one quarter of U.S. adults recovering from significant AOD problems report experiencing some kind of social-interpersonal discrimination because someone knew of their AOD history. Most common among these were other people fearing that the person would relapse, being held to a higher standard, being treated less favorably, and being avoided by other people. Further, detailed research is needed, however, to understand more about the impact of such experiences and the extent to which these may serve to destabilize recovery or increase resolve to stay in recovery. Similarly, although to a lesser degree, a substantial minority of individuals reported macro-level, structural discrimination, including being treated unfairly by the police and difficulty obtaining employment which is consistent with previous research (Baldwin et al., 2010; Sarin et al., 2013). Once again, more detailed prospective investigation is needed to understand if and how these experiences do actually serve to block recovery progress or the attainment of recovery capital.
Sophisticated psychometric analyses of the pool of initial items gathered to measure discrimination in recovery, yielded two distinct, but moderately correlated, factors reflecting features of both micro and macro discrimination. The internal consistency of these two sub-scales were high suggesting these multiple items, while assessing many different types of social-interpersonal and structural discrimination, appear to be capturing the same underling latent constructs. Thus, if desired, these sub-scale items may be summed to produce an overall dimensional scale score measuring differing degrees of discrimination. These sub-scales may be of use in clinical, public health, or policy research either at the item level, or at the sub-scale score level, in order to document the types and degrees of experienced discrimination and whether these differ for different sub-groups or fluctuate over time.
The significant correlations observed between the micro and macro discrimination sub-scales and other indices of psychological distress, quality of life, and the accrual of recovery capital, are suggestive of either a potentially negative effect of experiencing discrimination on these indices, or more negative levels of these indices perhaps giving rise to greater discrimination. It is also plausible that there is a reciprocal interchange between these variables whereby greater discrimination leads to poorer well-being/functioning, and then, in turn, poorer functioning and well-being leads to greater discrimination. That said, it makes greater conceptual sense that greater discrimination would lead to the poorer outcomes than the other way around. These cross-sectional data cannot answer such speculations - further prospective work will help uncover the directionality and magnitude of such associations. Noteworthy too, was the slightly greater relative importance of micro compared to macro discriminations in terms of its impact on distress and quality of life. This suggests the social-interpersonal types of discrimination (personal slights) may be more detrimental than the structural barriers (violation of personal rights). The exact reasons for this remain to be clarified in more detailed research.
Also of note in Table 3 was that micro and macro discrimination had a more pronounced association in the first 5 years than in the later 5 years suggesting there is a more profound period of impact of perceived discrimination in early recovery. It is possible that people learn to cope with perceived discrimination better as they progress through recovery as observed by the waning effect on indices of functioning and wellbeing. Future research is needed to clarify this.
4.1. Limitations
The study’s findings should be considered in light of important limitations. This sample was collected in the U.S. and it is unknown if these phenomena would generalize to other nations. Reported findings here rely on self-report, are largely descriptive, and reflect perceived discriminatory experiences; we cannot surmise from these data whether these actually occurred- only that they were perceived to have happened. It should be kept in mind also that the term “resolution of an AOD problem” that we use in this paper may overlap with, but not necessarily signify diagnostic remission. This study was intended to capture the broader population of individuals who perceive at least some kind of self-defined problem with AOD use, including those with substance use disorder. This level of AOD problem severity has high public health significance because there are a large proportion of individuals who engage in consequential AOD use (e.g., drive while intoxicated/get a DUI), but do not meet diagnostic criteria for AOD disorder. Our study is cross-sectional and correlational, therefore, appropriate caution should be taken when making inferences about dynamic changes in the same individuals, as well as any causal connections among variables. Future research should attempt to capture the directionality and causality of the relationships among these variables longitudinally in the same individuals over time to shed more light on these preliminary findings. Several demographics were not captured in this study including individuals currently without home addresses and individuals who have relapsed after experiencing recovery-related discrimination. The response options for gender identity did not include non-binary so the degree to which the results generalize to this population are unknown. Also, by design, this is a study of people in recovery from significant AOD problems, and thus, doesn’t address perceived discrimination among those currently engaged in unhealthy drug/alcohol use.
4.2. Conclusions
Different types of perceived discrimination continue to be experienced by a substantial minority of the U.S. population even after resolving a significant AOD problem. These experiences differ in nature and prevalence. Unclear is the extent to which these experiences serve to destabilize recovery efforts or perhaps bolster resolve and commitment to continue in the recovery process. More detailed longitudinal work is needed to unravel the impact of these experiences on psychological distress, quality of life, the accrual of recovery capital, and remission status and whether certain discriminatory experiences (e.g., being unable to get a job) may be more detrimental and destabilizing to recovery efforts than others (e.g., people expected I would relapse). To these ends, other clinical researchers and program evaluators might benefit also from the psychometrically validated scales developed in the current study to investigate these phenomena among recovering persons.
Supplementary Material
Acknowledgments
Funding
Dr. Vilsaint was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under Award Number F32AA025823, Dr. Kelly Award Number K24AA022136, and Dr. Hoffman the National Institute on Drug Abuse Award Number F32DA047741. Study was funded by MGH Recovery Research Institute. Funders played no role in the design or conduct of the research or in the collection, analysis, or interpretation of the data, the writing of the report, or in the decision to submit this work for publication.
Footnotes
Declaration of Competing Interest
No conflict declared.
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.drugalcdep.2019.107667.
References
- Baldwin ML, Marcus SC, Simone JD, 2010. Job loss discrimination and former substance use disorders. Drug Alcohol Depend. 110 (1-2), 107 10.1016/j.drugalcdep.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battaglia MP, Hoaglin DC, Frankel MR, 2009. Practical considerations in raking survey data. Surv. Prac. 2, 1–10. [Google Scholar]
- Birtel MS, Wood L, Kempa NJ, 2017. Stigma and social support in substance abuse: Implications for mental health and well-being. Psychiatry Res. 252, 1–8. 10.1016/j.psychres.2017.01.097. [DOI] [PubMed] [Google Scholar]
- Blanco C, Iza M, Rodriguez-Fernandez JM, Baca-Garcia E, Wang S, Olfson M, 2015. Probability and predictors of treatment-seeking for substance use disorders in the U.S. Drug Alcohol Depend. 149 (April 1), 136–144. 10.1016/j.drugalcdep.2015.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD, 2011. Economic costs of excessive alcohol consumption in the US 2006. Am. J. Prev. Med 41, 516–524. 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- Brener L, von Hippel W, von Hippel C, Resnick I, Treloar C, 2010. Perceptions of discriminatory treatment by staff as predictors of drug treatment completion: utility of a mixed methods approach. Drug Alcohol Rev. 29, 491–497. 10.1111/j.1465-3362.2010.00173.x. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2016. 2015 National Survey on Drug Use and Health (NSDUH): Methodological Summary and Definitions. Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Costello AB, Osborne JW, 2005. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Practical Assessment, Research, & Evaluation 10, 1–9. http://citeseerx.ist.psu.edu/viewdoc/summary?doi=10.1.1.110.9154. [Google Scholar]
- Chen C, Storr CL, Anthony JC, 2009. Early-onset drug use and risk for drug dependence problems. Addict. Behav 319–322. 10.1016/j.addbeh.2008.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucina JM, Caputo PM, Thibodeaux HF, Maclane CN, 2012. Unlocking the key to biodata scoring: A comparison of empirical, rational, and hybrid approaches at different sample sizes. Pers. Psychol 65, 385–428. 10.1111/j.1744-6570.2012.01244.x. [DOI] [Google Scholar]
- Dennis ML, Scott CK, Funk R, Foss MA, 2005. The duration and correlates of addiction and treatment careers. J. Subst. Abuse Treat 28, S51–62. 10.1016/j.jsat.2004.10.013. [DOI] [PubMed] [Google Scholar]
- Dupont RL, Compton WM, McLellan AT, 2015. Five-year recovery: a new standard for assessing effectiveness of substance use disorder treatment. J. Subst. Abuse Treat 58, 1–5. 10.1016/j.jsat.2015.06.024. [DOI] [PubMed] [Google Scholar]
- Cruz CC, Salom C, Maravilla J, Alati R, 2018. Mental and physical health correlates of discrimination against people who inject drugs: A systematic review. J. Stud. Alcohol Drugs 79, 350–360. 10.15288/jsad.2018.79.350. [DOI] [PubMed] [Google Scholar]
- Fleury MJ, Djouini A, Huỳnh C, Tremblay J, Ferland F, Ménard JM, Belleville G, 2016. Remission from substance use disorders: a systematic review and meta-analysis. Drug Alcohol Depend. 168, 293–306. 10.1016/j.drugalcdep.2016.08.625. [DOI] [PubMed] [Google Scholar]
- Gore FM, Bloem PJN, Patton GC, Ferguson D, Joseph V, Coffey C, 2011. Global burden of disease in young people aged 10-24 years: a systematic analysis. Lancet 377, 2093–2102. 10.1016/S0140-6736(11)60512-6. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, 1998. Age of onset of drug use and its association with DSM-IV drug abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. J. Subst. Abuse 10 (2), 163–173. [DOI] [PubMed] [Google Scholar]
- Humphreys K, 2017. How to deliver a more persuasive message regarding addiction as a medical disorder. J. Addict. Med 11 (May-Jun (3)), 174–175. 10.1097/ADM.0000000000000306. [DOI] [PubMed] [Google Scholar]
- John WS, Zhu H, Manelli P, Schwartz RP, Subramaniam GA, Wu LT, 2018. Prevalence, patterns, and correlates of multiple substance use disorders among adult primary care patients. Drug Alcohol Depend. 187 (June 1), 79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Bergman B, Hoeppner B, Vilsaint C, White WL, 2017. Prevalence and pathways of recovery from drug and alcohol problems in the United States population: implications for practice, research, and policy. Drug Alcohol Depend. 181, 162–169. 10.1016/j.drugalcdep.2017.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Westerhoff CM, 2010. Does it matter how we refer to individuals with substance- related conditions? a randomized study of two commonly used terms. Int. J. Drug Policy 21, 202–207. 10.1016/j.drugpo.2009.10.010. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SL, Manderscheid RW, Walters EE, Zaslavsky AM, 2003. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 60, 184–189. 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Berglund PA, Caraveo-Anduaga JJ, DeWit DJ, Greenfield SF, Kolody B, Olfson M, Vega WA, 2001. Patterns and predictors of treatment seeking after onset of a substance use disorder. Arch. Gen. Psychiatry 58 (11), 1065–1071. [DOI] [PubMed] [Google Scholar]
- Keys KM, Hatzenbuehler ML, McLaughlin KA, Link B, Olfson M, Grant BF, Hasin D, 2010. Stigma and treatment for alcohol disorders in the United States. Am. J. Epidemiol. 172, 1364–1372. 10.1093/aje/kwq304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linacre JM, 2019a. Winsteps® Rasch Measurement Computer Program User’s Guide. Beaverton: Winsteps.com, Oregon. [Google Scholar]
- Linacre JM, 2019b. Winsteps® (Version 4.4.1) [Computer Software]. Winsteps.com, Beaverton, Oregon: Available from https://www.winsteps.com/ Accessed on August 13, 2019. [Google Scholar]
- Masters GN, 1982. A Rasch model for partial credit scoring. Psychometrika 47, 149–174. 10.1007/BF02296272. [DOI] [Google Scholar]
- NIDA, 2017. Substance Use Disorders Are Associated With Major Medical Illnesses and Mortality Risk in a Large Integrated Health Care System. October 24 Available from https://www.drugabuse.gov/news-events/nida-notes/2017/10/substance-use-disorders-are-associated-major-medical-illnesses-mortality-risk-in-large-integrated Accessed on August 13, 2019. .
- NIDA, 2018. Common Comorbidities with Substance Use Disorders. February 27 Available from https://www.drugabuse.gov/publications/research-reports/common-comorbidities-substance-use-disorders Accessed on August 19, 2019. .
- O’Connor BP, 2000. SPSS and SAS programs for determining the number of components using parallel analysis and Velicer’s MAP test. Behav. Res. Methods Instrum. Comput 2, 396–402. 10.3758/BF03200807. [DOI] [PubMed] [Google Scholar]
- Room R, Rehm J, Trotter RT II, Paglia A, Üstün TB, 2001. Cross-cultural views on stigma valuation parity and societal attitudes towards disability In: Üstün TB, Chatterji S, Bickenbach JE, Trotter RT II, Room R, Rehm J, Saxena S (Eds.), Disability and Culture: Universalism and Diversity. Hofgrebe & Huber, pp. 247–291. [Google Scholar]
- Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, Brewer RD, 2015. 2010 National and state costs of excessive alcohol consumption. Am. J. Prev. Med 49 (5), e73–e79. 10.1016/j.amepre.2015.05.031. [DOI] [PubMed] [Google Scholar]
- Sarin E, Samson LJ, Sweat MD, 2013. Impact of acts of discrimination on quality of life among injecting drug users in Delhi, India. Soc. Indic. Res 113, 319–334. 10.1007/s11205-012-0095-8. [DOI] [Google Scholar]
- Schmidt S, Muhlan H, Power M, 2006. The EUROHIS-QOL 8-item index: psychometric results of a cross-cultural field study. Eur. J. Public Health 16, 420–428. 10.1093/eurpub/cki155. [DOI] [PubMed] [Google Scholar]
- StataCorp, 2015. Stata Statistical Software: Release 14. StataCorp LP. [Google Scholar]
- Tabachnick BG, Fidell LS, 2001. Using Multivariate Statistics, 4th ed. Harper Collins. [Google Scholar]
- United States Census Bureau, 2015. Current Population Survey (CPS). Accessed on May 16, 2019 https://www.census.gov/programs-surveys/cps/about.html.
- Vilsaint CV, Kelly JF, Bergman BG, Groshkova T, Best D, White W, 2017. Development and validation of a brief assessment of recovery capital (BARC-10) for alcohol and drug use disorder. Drug Alcohol Depend. 177, 71–76. 10.1016/j.drugalcdep.2017.03.022. [DOI] [PubMed] [Google Scholar]
- White WL, 2012. Recovery/Remission From Substance Use Disorders: an Analysis of Reported Outcomes in 415 Scientific Reports, 1868-2011. Philadelphia department of behavioral health and intellectual disability services. [Google Scholar]
- World Health Organization, 2008. The Global Burden of Disease: 2004 Update. World Health Organization; Available from https://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/ Accessed on August 13, 2019. [Google Scholar]
- World Health Organization, 2011. Global Status Report on Alcohol and Health. World Health Organization; Available from http://apps.who.int/iris/bitstream/handle/10665/44499/?sequence=1 Accessed on August 13, 2019. [Google Scholar]
- Yu CH, Popp SO, DiGangi S, Jannasch-Pennell A, 2007. Assessing unidimensionality: a comparison of Rasch Modeling, Parallel Analysis, and TETRAD. Practical Assessment, Research, and Evaluation. 12 (14), 1–19. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.