Abstract
Objective:
Parents’ comments about their adolescents’ weight have been linked with adolescents’ disordered eating, but we know little about the personal and contextual conditions that promote or mitigate the effects of parents’ perceptions on adolescents’ weight concerns. This study examined whether the prospective association between parents’ perceptions of adolescents’ weight and adolescents’ weight concerns differed as a function of exposure to interparental conflict or adolescent gender.
Method:
Participants were 386 adolescents (52% female; ages 11–18 years; predominately Caucasian/European American) from 197 families (i.e., up to two adolescents per family), and their parents. Two-parent families with a firstborn child in 8th, 9th, or 10th grade and a secondborn child 1–4 years younger were recruited to participate in a short-term longitudinal study of adolescent development and family relationships. Annual home interviews were conducted with adolescents and parents. Multilevel models tested whether parents’ perceptions of adolescents’ weight predicted adolescents’ weight concerns one year later and whether interparental conflict and youth gender moderated this prospective association.
Results:
A significant three-way interaction revealed that when interparental conflict was low, increases in fathers’ but not mothers’ perceptions of daughters’ overweight predicted increases in daughters’ weight concerns the following year. In contrast, girls exposed to high interparental conflict reported elevated weight concerns the following year regardless of parents’ perceptions. Results for boys were not significant.
Discussion:
Findings highlight the role of personal and family context characteristics in the development of weight concerns and the value of addressing family processes within preventive interventions for adolescent girls’ weight concerns.
Keywords: body image, family relations, family conflict, adolescent development, prospective studies
Weight concerns are a marker of body image and eating pathology, encompassing a fear of gaining weight, concern with body shape and weight, perception of overweight, and weight control behaviors (Killen et al., 1996). Subclinical levels of weight concerns are common during adolescence, with over 55% of adolescent girls and 30% of adolescent boys engaging in disordered eating behaviors, the behavioral component of weight concerns (Croll, Neumark-Sztainer, Story, & Ireland, 2002). Weight concerns present during adolescence tend to increase and persist into young adulthood (Neumark-Sztainer, Wall, Larson, Eisenberg, & Loth, 2011). Adolescents’ weight concerns also predict negative psychological and physical health outcomes, including: eating disorders, low self-esteem, depressive symptoms, risky behaviors, overweight, and a lower perceived quality of life (Farhat, Iannotti, & Summersett-Ringgold, 2015; Hochgraf, McHale, & Fosco, 2018; Killen et al., 1994; Killen et al., 1996; Neumark-Sztainer et al., 2006; Stice & Bearman, 2001). To maximize the impact of prevention efforts, research should address the significant gaps in our understanding of risk factors for the development of weight concerns.
Family systems are primary developmental contexts for youth and thus key for risk factor research (Collins, Maccoby, Steinberg, Hetherington, & Bornstein, 2000). However, the developmental literature on risk factors for weight concerns has emphasized individual characteristics, (e.g., body mass index, gender), or distal contextual factors (e.g., sociocultural pressure to be thin), thereby overlooking the role of potential malleable and proximal family dynamics. Research on clinically-diagnosable eating disorders has primarily used cross-sectional or retrospective studies to examine characteristics of individuals and families associated with eating disorders, but the lack of prospective study designs precludes establishment of risk factors (Kraemer et al., 1997). Identifying malleable family processes that promote differential susceptibility for developing weight concerns, and how these combine with individual characteristics, can inform development of targeted prevention programs. Accordingly, the current study was designed to test how family processes interact with youth characteristics to predict weight concerns during adolescence, a developmental period of heightened vulnerability for weight concerns.
One potential family risk factor is parents’ perceptions of the extent of their adolescents’ overweight. Although parents are most likely to underestimate their children’s weight (Towns & D’Auria, 2009), parents who see their adolescents as overweight are more likely to encourage them to diet (Neumark-Sztainer, Wall, Story, & van den Berg, 2008), and mothers are more likely to perceive daughters than sons as overweight (Boutelle, Fulkerson, Neumark-Sztainer, & Story, 2004; Maynard, Galuska, Blanck, & Serdula, 2003). Gender socialization and sociocultural theories of eating disorders suggest that parents’ concerns about daughters’ overweight are part of a gender socialization process through which girls learn about the objectification of their bodies, and differences in perceptions of boys’ and girls’ weight may stem from gendered standards of beauty (McHale, Corneal, Crouter, & Birch, 2001; Smolak, 2004). Importantly, parents’ perceptions of their adolescents’ weight status may affect their interactions with that adolescent; parents who believe their child is overweight may attempt to change their child’s eating or weight control behaviors out of concern for their child’s health and wellbeing. In many cases, this concern may be appropriate and stem from discussions with health care providers. However, daughters may be at elevated risk compared to sons because gender socialization and norms emphasize the importance of physical appearance for girls.
Although the impact of parents’ perceptions of adolescents’ weight status on weight concerns is unclear, research has linked parents’ weight related teasing, comments, and pressure to be thin to weight concerns. Weight-related teasing, which entails an evaluation of a person as overweight and related criticism, predicts eating pathology (Haines, Neumark-Sztainer, Eisenberg, & Hannan, 2006; Haines, Neumark-Sztainer, Hannan, Berg, & Eisenberg, 2008; Neumark-Sztainer et al., 2010). Similarly, parents’ weight-related comments and encouragement to diet have been linked to adolescents’ disordered eating and body dissatisfaction (Berge et al., 2018; Eisenberg, Berge, Fulkerson, & Neumark-Sztainer, 2012; Taylor et al., 2006). Perhaps most closely related to parents’ perceptions of adolescents’ weight, adolescents’ reports of pressure to be thin from their mothers have been found to predict increases in disordered eating the following year, and mothers’ reports of pressure on their adolescents to be thin were positively associated with adolescents’ concurrent disordered eating (Shomaker & Furman, 2009). An important next step is to determine whether and how parents’ perceptions of adolescents’ weight predict adolescents’ weight concerns after taking into account adolescents’ actual weight and to test whether these processes differ according to youth gender.
Interparental conflict may affect the degree to which parents’ perceptions shape adolescents’ weight concerns. Adolescents are expected to become increasingly autonomous as they approach adulthood, and conflict may ensue as parents and adolescents negotiate changes in rules, independence, and responsibilities (Steinberg, 2001). Prior research suggests, however, that the frequency, intensity, and the meaning that adolescents ascribe to interparental conflicts have implications for conflicts’ effects on adolescents’ adjustment (Cummings & Davies, 2002; Grych & Fincham, 1990). Even in relatively well-adjusted community samples, interparental conflict is a stressor that has long been linked to adolescents’ psychological adjustment (Harold, Fincham, Osborne, & Conger, 1997).
Importantly, according to family systems theory, conflict within family subsystems affects all members of the family system, even when members are not directly involved in the conflict (Cox & Paley, 1997). Research on emotional transmission within families, for example, suggests that interparental negativity may spill over into parent-child interactions (Almeida, Wethington, & Chandler, 1999; Larson & Almeida, 1999). Prior work suggests that interparental conflict is associated with less accepting and more harsh parenting (Buehler, Benson, & Gerard, 2006; Krishnakumar & Buehler, 2000). This may create a context in which parents’ perceptions of adolescents’ weight are conveyed or interpreted as criticism, leading to increased weight concerns among adolescents. This idea is congruent with models of eating disorder development which suggest that individuals engage in unhealthful eating behaviors as a means of coping with negative affect (Hawkins & Clement, 1984; Heatherton & Baumeister, 1991; McCarthy, 1990; Sim & Zeman, 2005; Stice, Shaw, & Nemeroff, 1998). Grounded in the idea that a stressor in the family context may alter the impact of parents’ perceptions on adolescents’ weight concerns, this prospective study examined interparental conflict as a moderator of the association between parents’ perceptions of their children’s overweight and adolescents’ weight concerns and tested whether these processes differed for girls and boys.
The Current Study
This study was designed to investigate whether mothers’ and/or fathers’ perceptions of their adolescents’ weight status interacted with youth gender and interparental conflict to predict adolescents’ weight concerns the following year. Prior studies of parents’ perceptions of adolescents’ weight status and most studies of family characteristics associated with weight concerns have omitted fathers. From a family systems perspective, however, each member of the family system makes a unique contribution to family functioning, meaning that both mothers and fathers merit attention (Cox & Paley, 1997). Indeed, the limited research in this area that has included both mothers and fathers has revealed gendered differences in mothers’ and fathers’ influence on adolescents’ weight concerns (e.g., May et al., 2006). Thus, we examined mothers’ and fathers’ perceptions as separate predictors.
Hypotheses
We tested the following hypotheses: (a) Both mothers’ and fathers’ perceptions of the extent of their adolescents’ overweight will predict higher levels of adolescent weight concerns the following year; and (b) interparental conflict and gender will moderate these associations, such that higher levels of interparental conflict will strengthen the association between parents’ perceptions and adolescents’ weight concerns, particularly for girls.
Method
Participants
Participants were part of a longitudinal study of adolescent development and family relationships. The purpose of the parent study was to investigate adolescent siblings’ differential family experiences, and how parents’ work characteristics and family dynamics were linked to adolescents’ developmental trajectories of psychosocial functioning. The sample included 386 adolescents (52.1% female, 47.9% male) from 197 families and their mothers and fathers. All families had a firstborn child in 8th, 9th, or 10th grade, and at least one sibling 1–4 years younger. We used data from study Years 2 and 3, when the measures of interest were collected. The retention rate was 98% in Year 2, the first year used in this study, and 100% of families who participated at Year 2 participated in Year 3. Across these time points adolescents ranged in age from 11 to 18 years (mean age at first measurement = 13 years for younger siblings, SD = 1.02, and 16 years for older siblings, SD = .72). Mean annual household income (averaged across the two time points) was $65,620 (SD = $26,850; range = $12,000 - $215,300). Families included in the study were comprised of employed, married parents, a firstborn child in 8th, 9th, or 10th grade, and a sibling 1–4 years younger. The present analyses used self-report data from both siblings and parents in each family. Nearly all families were Caucasian/European American, which is representative of the northeastern state from which participants were recruited: Approximately 85% of the population of this region was White at the time of data collection (U.S. Census Bureau, 2001). The communities sampled for this study included small cities, towns, and rural areas.
Procedures
Participants provided informed consent/assent, and families were given a $100 honorarium. Trained research assistants completed annual separate home interviews with adolescents and parents to collect information on family demographics, relationships, and adolescent development. All study procedures were approved by the university’s Institutional Review Board.
Measures
Adolescent Weight Concerns.
Adolescents completed the six-item Stanford Weight Concerns Scale (Killen et al., 1994). The scale captures body image and eating pathology (e.g., “How afraid are you of gaining three pounds?”), has been validated for adolescents (Killen et al., 1994; Killen et al., 1996). Internal consistency was acceptable (α = .82 for younger siblings and α = .85 for older siblings at Time 1 and α = .84 for younger siblings and α = .83 for older siblings at Time 2). Response scales for the items varied, with one item on a 2-point scale, one item on a 4-point scale, three items on 5-point scales, and one item on a 6-point scale. Therefore, items were re-scaled to a 6-point scale prior to calculating sum scores. Higher scores indicate elevated weight concerns. Jacobi and colleagues suggested a clinical cut off score of 47 on a 100 point scale, which transformed to our scale, would be 20.1.
Parent Perceptions of Youth Weight Status.
Mothers and fathers reported their perception of their adolescents’ weight using a one-item, 7-point scale (1 = underweight, 4 = just about right, 7 = overweight). Test-retest reliability over one year was acceptable for mothers (r = .75) and fathers (r = .75).
Interparental Conflict.
Conflict between parents was measured with the five-item conflict scale of the Relationships Questionnaire (Braiker & Kelley, 1979), which captures both frequency (e.g., “How often do you and your partner argue with each other?”) and intensity (e.g., “When you and your partner argue, how serious are the problems or arguments?”) of conflict on a nine-point response scale ranging from 1 = not at all/never/very infrequently to 9 = very much/very often/frequently. Mothers’ and fathers’ interparental conflict scores were calculated by summing responses to the items. Internal consistency was acceptable for mothers (α = .77) and fathers (α = .80). To increase model parsimony, interparental conflict scores for each family were calculated by adding mothers’ and fathers’ reports of interparental conflict (r = .38, p < .001).
Covariates.
We included adolescent body mass index, age, and parent weight concerns as covariates because weight concerns are influenced by body weight and vary over the course of adolescence, and parents’ weight concerns may indicate that adolescents have biological and/or social vulnerabilities for developing weight concerns. Adolescents’ body mass indices (BMI) were calculated from self-reports of height and weight via the formula, kg/m2. Although the meaning of BMI scores varies by age and gender, the use of BMI scores (as opposed to BMI percentiles, which take age and sex into account) was appropriate in this study because the analytic models estimate each individual’s weight concerns based on their BMI, age, and gender (as well as all other predictors in the models). Adolescents’ age in years at Time 1 and gender were included as covariates. Parents’ weight concerns were measured with the Stanford Weight Concerns Scale (Killen et al., 1994), which has been used to index adults’ weight concerns in previous studies (e.g., Lam & McHale, 2012). Internal consistency was acceptable for parents (mothers’ α = .82, fathers’ α = .77 at Time 1). Scoring procedures for parents’ weight concerns were identical to adolescents’. Parents’ reports of total income at Times 1 and 2 were averaged to create a composite score of household income and included as a covariate.
Analyses
Multilevel modeling was used to accommodate the clustered data (i.e., siblings within families). Multilevel modeling explicitly accounts for shared variance between siblings by partitioning variance by level of hierarchical clustering, in this case, family (Level 2) and individual (Level 1; Hox, 2010; Singer, 1998). A series of nested models were estimated to test the prospective associations between mothers’ and fathers’ perceptions of their adolescents’ weight status and adolescent weight concerns, as well as two- and three-way interactions involving adolescent gender and interparental conflict. The first model included main effects only (Step 1), and was followed by a two-way interaction model (Step 2), and finally a three-way interaction model to test hypotheses (Step 3). Level 1 predictors captured the characteristics and experiences of individual adolescents and included: adolescents’ weight concerns at Time 1, mothers’ and fathers’ perceptions of adolescents’ weight status, and adolescent body mass index, gender, and age. Level 2 predictors captured family characteristics (shared by siblings) and included: interparental conflict, mothers’ and fathers’ weight concerns, and household income. Predictors were grand mean centered. A random intercept was specified for families to allow for differences in mean levels of adolescent weight concerns across families. Terms that were not significant (p < .05) in the main effects model and unnecessary for estimation of higher order effects were dropped for model parsimony. As there is currently no standard method for reporting effect sizes from multilevel modeling and approaches such as variance explained are not straightforward to interpret (e.g., negative R2 values), we re-estimated the models using standardized variables so that the magnitudes of gamma coefficients could be compared.
Correlation and stability coefficients are presented in Table 1. Because the stability coefficients for Times 1 and 2 were relatively high for all study variables, a time varying effects model was not warranted. The equations for the model were:
Where the “i” and “j” subscripts refer to individual and family respectively, the “M” and “F” prefixes refer to mother and father respectively, Percep = perception of adolescent’s weight, and Conflict = interparental conflict.
Table 1.
Correlations between Study Variables at Time 1 and Stability Coefficients
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Adolescent Weight Concerns | .78*** | |||||||||
| 2. Mother Perception of Child’s Weight | .34*** | .75*** | ||||||||
| 3. Father Perception of Child’s Weight | .28*** | .63*** | .75*** | |||||||
| 4. Interparental Conflict | .11* | −.04 | −.10 | .78*** | ||||||
| 5. Mother Weight Concerns | .22*** | .20*** | .07 | .14** | .80*** | |||||
| 6. Father Weight Concerns | .07 | .01 | −.01 | .12* | .04 | .80*** | ||||
| 7. Body Mass Index | .23*** | .59*** | .54*** | −.09 | −.03 | .02 | .87*** | |||
| 8. Gender | −.38*** | −.13* | −.11* | −.04 | .03 | −.01 | .12* | --- | ||
| 9. Household Income | −.05 | −.10 | −.00 | −.00 | −.03 | .12* | −.09 | −.02 | --- | |
| 10. Age | .04 | −.02 | −.00 | .01 | .02 | −.01 | .31*** | .15** | .02 | --- |
Note. Time 1 correlation coefficients are displayed below the diagonal. Stability coefficients (Times 1–2) are displayed on the diagonal.
p < .05,
p < .01,
p < .001
Results
Descriptive statistics (Table 2) indicated that mean levels of weight concerns were higher for girls than boys at Times 1 and 2, although girls’ mean body mass index was lower than boys’. Mean body mass index was within a healthy range for both girls and boys. Mothers’ and fathers’ mean perceptions of daughters’ and sons’ weight were close to the value for ideal weight. The mean level of interparental conflict was moderate, with a range of 15.00 – 67.00 for the sample.
Table 2.
Means, Standard Deviations (SD) and Ranges for Study Variables by Adolescent Gender
| Girls | Boys | |||||
|---|---|---|---|---|---|---|
| Variable | Mean | SD | Range | Mean | SD | Range |
| Adolescent Weight Concerns (Time 1) | 14.91 | 6.99 | 6.00–36.00 | 10.23 | 4.21 | 6.00–33.50 |
| Adolescent Weight Concerns (Time 2) | 14.52 | 6.96 | 6.00–34.37 | 9.97 | 3.80 | 6.00–24.62 |
| Mother Perception of Adolescent’s Weight | 4.09 | 0.95 | 1.00–7.00 | 3.84 | 0.96 | 1.00–7.00 |
| Father Perception of Adolescent’s Weight | 4.02 | 0.71 | 1.00–7.00 | 3.86 | 0.81 | 2.00–7.00 |
| Interparental Conflict | 40.09 | 10.82 | 21.00–67.00 | 39.17 | 10.51 | 15.00–67.00 |
| Mother Weight Concerns | 16.64 | 6.97 | 6.00–34.37 | 17.07 | 7.05 | 6.00–34.37 |
| Father Weight Concerns | 12.97 | 5.21 | 6.00–32.67 | 12.91 | 5.04 | 6.00–32.67 |
| Body Mass Index (kg/m2) | 20.35 | 3.57 | 13.58–35.44 | 21.29 | 4.17 | 14.37–41.47 |
| Household Income (in USD) | 66173.36 | 28264.34 | 19500.00–215300.00 | 65293.06 | 25550.06 | 12000.00–215300.00 |
As presented in Table 3, in Step 1 of the model, fixed effects for adolescent age (γ10; standardized γ = −0.03, SE = 0.04), BMI (γ20; standardized γ = −0.08, SE = 0.25), household income (γ03; standardized γ = 0.01, SE = 0.03), and mothers’ (γ01; standardized γ = 0.05, SE = 0.03) and fathers’ (γ02; standardized γ = 0.02, SE = 0.03) own weight concerns were not statistically significant predictors of adolescents’ weight concerns the following year. As household income and parents’ weight concerns were neither statistically significant nor theoretically important to the model, they were dropped from subsequent analyses to improve model parsimony. The fixed effect for the intercept (γ00) was significantly different from zero and indicated that, after taking family level clustering into account, adolescents’ estimated weight concerns averaged 12.72, controlling for age, gender, BMI, household income, parents’ weight concerns, prior weight concerns, parents’ perceptions, and interparental conflict. Given the range of weight concerns from 6 to 36 in this subclinical sample, and a clinical cut off score of 20.1, 12.72 represents a low to moderate level of weight concerns (Jacobi et al., 2003; note that this cut off score has been rescaled. See measures section for details). There were statistically significant fixed effects for gender (γ30; standardized γ = −0.19, SE = 0.07), and prior weight concerns (γ40; standardized γ = 0.69, SE = 0.04), indicating that girls reported more weight concerns than boys and that weight concerns at Times 1 and 2 were positively related. Neither mothers’ (γ50; standardized γ = 0.06, SE = 0.05) nor fathers’ (γ60; standardized γ = 0.06, SE = 0.04) perceptions or interparental conflict (γ; standardized γ = 0.05, SE = 0.03) were significant predictors of adolescents’ weight concerns in this main effect model.
Table 3.
Unstandardized Coefficients (and Standard Errors) from a Two Level Model Testing whether Interparental Conflict and Adolescent Gender Moderate the Prospective Link between Mothers’ and Fathers’ Perceptions of Adolescents’ Weight and Adolescents’ Weight Concerns
| Step 1 | Step 2 | Step 3 | ||||
|---|---|---|---|---|---|---|
| γ | (SE) | γ | (SE) | γ | (SE) | |
| Fixed Effects | ||||||
| Intercept (γ00) | 12.72*** | 0.30 | 12.62*** | 0.30 | 12.55*** | 0.30 |
| Age (γ10) | −0.11 | 0.14 | −0.13 | 0.14 | −0.11 | 0.14 |
| BMI (γ20) | −0.02 | 0.07 | −0.03 | 0.07 | −0.03 | 0.07 |
| Gender (γ30) | −1.16* | 0.44 | −1.14* | 0.43 | −1.07* | 0.42 |
| Household Income (γ03) | 0.00 | 0.00 | ||||
| Prior Weight Concerns (γ40) | 0.67*** | 0.04 | 0.66*** | 0.04 | 0.65*** | 0.04 |
| Mother Weight Concerns (γ01) | 0.04 | 0.03 | ||||
| Father Weight Concerns (γ02) | 0.02 | 0.04 | ||||
| MPercep (γ50) | 0.35 | 0.29 | 0.53 | 0.40 | 0.47 | 0.40 |
| FPercep (γ60) | 0.48 | 0.35 | 1.07* | 0.53 | 1.52* | 0.54 |
| Conflict (γ04) | 0.03 | 0.02 | 0.07* | 0.03 | 0.07* | 0.03 |
| Gender*MPercep (γ70) | −0.32 | 0.51 | −0.18 | 0.51 | ||
| Gender*FPercep (γ80) | −0.74 | 0.67 | −1.17 | 0.68 | ||
| Gender*Conflict (γ31) | −0.08* | 0.04 | −0.07 | 0.04 | ||
| MPercep*Conflict (γ51) | 0.03 | 0.02 | 0.06 | 0.03 | ||
| FPercep*Conflict (γ61) | −0.08* | 0.03 | −0.18*** | 0.05 | ||
| Gender*MPercep*Conflict (γ71) | −0.08 | 0.05 | ||||
| Gender*FPercep*Conflict (γ81) | 0.19** | 0.06 | ||||
| Random Effects | ||||||
| Intercept Variance (σ2u0) | 0.34 | 1.07 | 1.00 | 1.05 | 0.71 | 1.03 |
| Residual Variance (σ2e) | 13.20*** | 1.43 | 12.22*** | 1.33 | 12.23*** | 1.33 |
| −2 Log Likelihood | 2022.10 | 2026.30 | 2025.60 | |||
| Akaike Information Criterion | 2026.10 | 2030.30 | 2029.60 | |||
Note.
p < .05;
p < .01;
p < .001.
BMI = body mass index; MPercep = mother’s perception of adolescent’s weight; FPercep = father’s perception of adolescent’s weight; Conflict = interparental conflict. Unstandardized estimates. In the empty model, intercept variance was 6.52 (SE = 2.68, p = .01), residual variance was 29.27 (SE = 3.02, p < .001), −2 Log Likelihood was 2462.9, and Akaike Information Criterion was 2466.9. Terms that were not statistically significant, necessary for higher order model estimation, or theoretically essential were dropped. The final model was estimated based on data from 370 adolescents in 190 families.
In Step 2 of the model, fathers’ perceptions were significant (standardized γ = 0.14, SE = 0.07), as were the fixed effects for the intercept, gender (standardized γ = −0.19, SE = 0.07), prior weight concerns (standardized γ = 0.68, SE = 0.04), and interparental conflict (standardized γ = 0.13, SE = 0.05), and the two-way interactions between both gender and interparental conflict (γ31; standardized γ = −0.14, SE = 0.06) and fathers’ perceptions and interparental conflict (γ61; standardized γ = −0.11, SE = 0.04).
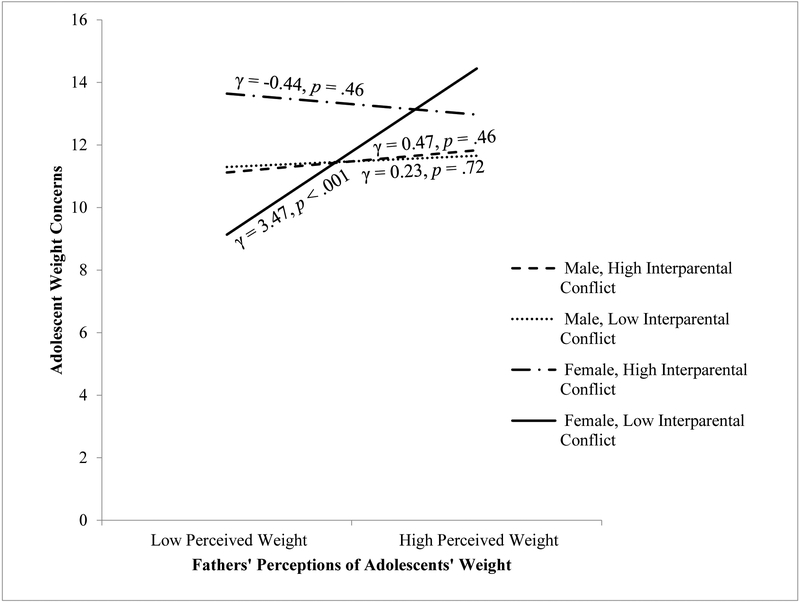
These significant effects, however, were qualified in Step 3. With three-way interactions included, fixed effects for the intercept, gender (standardized γ = −0.18, SE = 0.07), prior weight concerns (standardized γ = 0.66, SE = 0.04), fathers’ perceptions (standardized γ = 0.19, SE = 0.07), and interparental conflict (standardized γ = 0.13, SE = 0.05) were again statistically significant. The significant two-way interaction between fathers’ perceptions and interparental conflict (standardized γ = −0.25, SE = 0.06) was qualified by a significant three-way interaction of gender, fathers’ perceptions, and interparental conflict (γ81; Figure 1; standardized γ = 0.26, SE = 0.09). This three-way interaction was probed at one standard deviation above and below the mean of interparental conflict. Results indicated that only the simple slope for girls from families with low interparental conflict was significant, γ = 3.47, p < .001, meaning that on average for these girls, a one unit increase in fathers’ perception of their overweight was associated with a 3.47 unit increase in their weight concerns. The three-way interaction involving mothers’ perceptions (γ71; standardized γ = 0.13, SE = 0.08) was not statistically significant. The intercept variance was not significant in the main effects model (σu02 = 0.34, p > .05), nor in the two-way (σu02 = 1.00, p > .05) or three-way (σu02 = 0.71, p > .05) interaction models, indicating that the predictors included in these models explained the between-family variability in weight concerns.
Figure 1.
Three-way interaction between fathers’ perceptions of adolescents’ weight, interparental conflict, and adolescent gender predicting adolescents’ weight concerns.
Note. The three-way interaction between fathers’ perceptions of adolescents’ weight, gender, and interparental conflict was probed at one standard deviation above and below the mean of interparental conflict. Only the simple slope for girls with parents with low interparental conflict was statistically significant, indicating that on average for these girls, a one unit increase in fathers’ perceptions of their weight was associated with a 3.47 unit increase in weight concerns, controlling for girls’ prior level of weight concerns, adolescent age, body mass index, and mothers’ perceptions of adolescents’ weight.
Follow-up analyses.
We conducted follow-up analyses to verify that the results were the same if mother and father reports of conflict were included as distinct predictors rather than in an aggregate interparental conflict score for each family. When mother and father reports of conflict were included in the same model, the results were consistent with the original model, except that the three-way interaction between gender, father perceptions, and interparental conflict was significant when fathers’ but not mothers’ reports of conflict were used. To determine whether this apparent gender difference was due to collinearity between mother and father reports of conflict, we also ran the analyses with mother and father reports of conflict in separate models and found substantively similar results to the original model. Consistent with the idea that collinearity between mother and father reports of conflict led to significant effects for father- but not mother-reported conflict, there were significant three-way interactions between gender, father perceptions, and father reported conflict, as well as gender, father perceptions, and mother reported conflict, and coefficients were similar to the original model. These follow-up analyses suggest that an aggregate score of interparental conflict was appropriate as presented in our original, more parsimonious model.
Finally, to help interpret our findings, we utilized a paired t-test to check whether the mean difference in mothers’ and fathers’ perceptions of adolescents’ weight was statistically significant, and found that it was not (t = 0.06, p > .05, Cohen’s d = 0.003).
Discussion
This study tested whether parents’ perceptions of adolescents’ weight predicted adolescents’ weight concerns the following year and whether the association between parents’ perceptions and adolescents’ weight concerns depended on youth gender and interparental conflict. The hypothesis that parents’ perceptions of their adolescents as overweight would predict higher levels of weight concerns was partially supported: Fathers’ but not mothers’ perceptions of the extent of their adolescents’ overweight were positively associated with adolescents’ weight concerns the following year. Consistent with study hypotheses, gender and interparental conflict moderated the association between fathers’ perceptions of adolescents’ weight and adolescents’ weight concerns. However, the effects of fathers’ perceptions emerged only for girls in low conflict families; girls in high conflict families reported high levels of weight concerns regardless of fathers’ perceptions. Importantly, adolescent age, BMI, and prior weight concerns were controlled, which eliminates these as confounding variables in the observed associations.
Based on prior research on parent weight-related comments and criticism (Haines et al., 2006; Haines et al., 2008; Neumark-Sztainer et al., 2010; Taylor et al., 2006), we had hypothesized that parents’ perceptions of their adolescents’ weight would predict weight concerns. The finding that fathers’ but not mothers’ perceptions of adolescents’ weight status predicted weight concerns is important given the limited research on fathers’ influence on adolescents’ weight concerns. Few other studies have included reports from mothers and fathers within the same model to examine their unique contributions to adolescents’ weight concerns. The differential effects of fathers’ and mothers’ perceptions highlight the importance of considering both parents when examining family processes related to development of weight concerns. This finding is also consistent with the family systems idea that each parent provides distinct experiences and has a unique relationship with their child (Cox & Paley, 1997). On average, mothers’ and fathers’ perceptions of their adolescents’ weight were not statistically different, indicating that the source of the perception was more important than the degree to which parents perceived their adolescent to be overweight. In addition, fathers exhibited less variability in their perceptions than mothers, lending additional support for the idea that differences in the effect of mothers’ and fathers’ perceptions on weight concerns are based on differences in the value adolescent girls ascribe to each parent’s evaluation of their body rather than statistical considerations. Prior research suggests that parents spend more time with their same-sex child, and parent-child shared time tends to decrease across adolescence for mother-daughter, mother-son, and father-daughter dyads, but not father-son dyads (Lam, McHale, & Crouter, 2012). Given that higher-order interaction effects revealed that fathers’ perceptions were important for girls’ weight concerns but not boys’, it may be that fathers’ attitudes toward daughters’ weight are especially salient due to girls’ limited shared time with fathers. In addition, as suggested by Hochgraf and colleagues (2018), girls may use their fathers’ perceptions about their weight as a reference for how males in general perceive them. Given that ideals of beauty for Caucasian/European American women favor a slim physique and that girls typically begin to engage in romantic relationships with boys during adolescence, girls may monitor and value their fathers’ perceptions of their weight to a greater degree than they do their mothers’.
The interaction between fathers’ perceptions of adolescents’ weight status, gender, and interparental conflict is consistent with an emotional transmission explanation for how parents’ perceptions may promote weight concerns, although not in the way anticipated. The interaction revealed that girls embedded in family systems with low interparental conflict may be particularly vulnerable to fathers’ perceptions that they are overweight: Girls who experienced low interparental conflict and whose fathers perceived them to be slim tended to report the fewest weight concerns, but girls who experienced low interparental conflict and whose fathers perceived them to be heavier had the highest levels of weight concerns. Girls embedded in family systems with high interparental conflict experienced high levels of weight concerns regardless of how heavy their fathers perceived them to be. These findings are congruent with prior work showing that girls are more vulnerable to weight concerns than boys (Neumark-Sztainer et al., 2002), and extend this work to demonstrate that, in line with a cumulative support model, the combination of low interparental conflict and fathers’ supportive attitudes helps protect girls from developing weight concerns. Our findings also build on research indicating that interparental conflict is a stressful experience for adolescents (Grych, Fincham, Jouriles, & McDonald, 2000). It appears that in the context of high interparental conflict, this stressor is more salient to girls than parents’ perceptions of their weight. Rather than creating a context in which parental perceptions of adolescents’ weight are perceived as criticism, high interparental conflict appears to be a risk factor for weight concerns with the potential to overshadow the effects of parental perceptions. Additional research is warranted to identify the mechanisms through which interparental conflict predicts weight concerns and whether the presence of related family stressors, such as harsh parenting, may partially account for this finding. Consistent with affect regulation models of eating disorders, it may be that girls exposed to high interparental conflict cope with this stressor by engaging in disordered eating behaviors to reduce negative affect (Hawkins & Clement, 1984; Heatherton & Baumeister, 1991; McCarthy, 1990; Sim & Zeman, 2005; Stice, Shaw, & Nemeroff, 1998).
Our findings also suggest that the effects of interparental conflict on psychological adjustment in this domain differ for boys and girls. Boys’ simple slopes for high and low interparental conflict did not differ and were not significantly different from zero, indicating that this family process was not predictive of boys’ weight concerns. A potential direction for future research is to test these associations using adolescent reports of interparental conflict. Grych and colleagues (2000) argue that although parent and child reports of interparental conflict are correlated, they may differ in their relation to processes underlying the link between conflict and youth adjustment problems. Youth reports of conflict may reflect the conflicts that are most salient to them, which may differ from parents’ recollections of conflict (Grych et al., 2000). Additional research should examine other family processes, such as appearance-related sibling differential treatment, that may better predict boys’ weight concerns.
Results should be interpreted in light of limitations of the study, which include the generalizability of findings given this study’s focus on Caucasian/European American, married, two-parent families and a correlational study design that does not permit causal inferences. Future research should investigate how these associations may differ in diverse populations and family structures. The current study was limited to the two measurement occasions when both perceptions of adolescents’ weight and weight concerns were assessed, which prevented analysis of differences that may occur due to transitions into adolescence or young adulthood. This study also relied on self-reports of height and weight to calculate body mass index and a one-item measure of parents’ perceptions of their adolescents’ weight, which was not ideal. However, acceptable test-retest reliability was observed over a one year interval for mothers’ and fathers’ perceptions.
Despite these limitations, this study demonstrates the value of examining how family processes may give rise to weight concerns and extends prior correlational research on the links between interparental conflict and adolescents’ weight concerns with a prospective design and inclusion of reports from both mothers and fathers. The findings from this study suggest a prospective relation between fathers’ perceptions of adolescents’ weight and weight concerns during adolescence. Further, results are consistent with the idea that fathers’ perceptions may influence adolescents’ weight concerns differentially depending on other characteristics of the family system, including the level of interparental conflict, and individual characteristics such as youth gender. Together, these findings reveal the need for continued research investigating how adolescents’ risk for weight concerns may vary depending on both individual characteristics and family processes.
Results from this study have important implications for the design of eating disorder prevention programs. Findings suggest that eating disorder prevention programs may need to be individual and family centered to optimally address adolescents’ weight concerns, and should involve fathers. Currently, the most promising eating disorder prevention programs are individual centered and aim to reduce body dissatisfaction among adolescents through cognitive and behavioral exercises (e.g., The Body Project; Stice, Rohde, & Shaw, 2013). However, the present study adds to a growing body of literature suggesting that family processes play a key role in the development of weight concerns (Hochgraf, Kahn, & Kim-Spoon, 2017; Hochgraf, McHale, & Fosco, 2018; Lam & McHale, 2012). Interventions that target family processes may be the next step for eating disorder prevention. Such interventions could include cognitive behavioral components but also address family dynamics that have been shown to predict or protect against development of weight concerns. Viable targets for prevention programs may include interpersonal relationships generally (Miniati, Callari, Maglio, & Calugi, 2018; Tanofsky-Kraff et al., 2007), interparental conflict (Cummings, Faircloth, Mitchell, Cummings, & Schermerhorn, 2008), and positive parent-adolescent relationships (Van Ryzin & Nowicka, 2013). Future research should continue to examine how individual and family processes interact to predict weight concerns with the goal of informing preventive efforts.
Acknowledgements
This study was funded by the National Institute of Child Health and Human Development (R01 HD029409, PIs: Susan M. McHale and Ann C. Crouter). We are grateful to the families who participated in our study. This project was also supported by the Prevention and Methodology Training Program (T32 DA017629, PI: Linda M. Collins), funded by the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse, the National Institute of Child Health and Human Development, or the National Institutes of Health.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Almeida DM, Wethington E, & Chandler AL (1999). Daily transmission of tensions between marital dyads and parent-child dyads. Journal of Marriage and the Family, 61, 49–61. doi: 10.2307/353882 [DOI] [Google Scholar]
- Berge JM, Winkler MR, Larson N, Miller J, Haynos AF, & Neumark-Sztainer D (2018). Intergenerational transmission of parent encouragement to diet from adolescence into adulthood. Pediatrics, 114, 1–8. doi: 10.1542/peds.2017-2955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutelle K, Fulkerson JA, Neumark-Sztainer D, & Story M (2004). Mothers’ perceptions of their adolescents’ weight status: Are they accurate? Obesity, 12, 1754–1757. doi: 10.1038/oby.2004.217 [DOI] [PubMed] [Google Scholar]
- Braiker HB & Kelley HH (1979). Conflict in the development of close relationships In Burgess R and Huston T (Eds.). Social Exchange in Developing Relationships (pp. 135–168). New York: Academic Press. [Google Scholar]
- Buehler C, Benson MJ, & Gerard JM (2006). Interparental hostility and early adolescent problem behavior: The mediating role of specific aspects of parenting. Journal of Research on Adolescence, 16, 265–292. doi: 10.1111/j.1532-7795.2006.00132.x [DOI] [Google Scholar]
- Collins WA, Maccoby EE, Steinberg L, Hetherington EM, & Bornstein MH (2000). Contemporary research on parenting: The case for nature and nurture. American Psychologist, 55, 218–232. doi: 10.1037/0003-066X.55.2.218 [DOI] [PubMed] [Google Scholar]
- Cox MJ & Paley B (1997). Families as systems. Annual Review of Psychology, 48, 243–267. doi: 10.1146/annurev.psych.48.1.243 [DOI] [PubMed] [Google Scholar]
- Croll J, Neumark-Sztainer D, Story M, & Ireland M (2002). Prevalence and risk and protective factors related to disordered eating behaviors among adolescents: Relationship to gender and ethnicity. Journal of Adolescent Health, 31, 166–175. doi: 10.1016/S1054-139X(02)00368-3 [DOI] [PubMed] [Google Scholar]
- Cummings EM, & Davies PT (2002). Effects of marital conflict on children: Recent advances and emerging themes in process-oriented research. Journal of Child Psychology and Psychiatry, 43, 31–63. doi: 10.1111/1469-7610.00003 [DOI] [PubMed] [Google Scholar]
- Cummings EM, Faircloth WB, Mitchell PM, Cummings JS, & Schermerhorn AC (2008). Evaluating a brief prevention program for improving marital conflict in community families. Journal of Family Psychology, 22, 193–202. doi: 10.1037/0893-3200.22.2.193. [DOI] [PubMed] [Google Scholar]
- Eisenberg ME, Berge JM, Fulkerson JA, & Neumark-Sztainer D (2012). Associations between hurtful weight-related comments by family and significant other and the development of disordered eating behaviors in young adults. Journal of Behavioral Medicine, 35, 500–508. doi: 10.1007/s10865-011-9378-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farhat T, Iannotti RJ, & Summersett-Ringgold F (2015). Weight, weight perceptions and health-related quality of life among a national sample of US girls. Journal of Developmental and Behavioral Pediatrics, 36, 313–323. doi: 10.1097/DBP.0000000000000172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grych JH & Fincham FD (1990). Marital conflict and children’s adjustment: A cognitive-contextual framework. Psychological Bulletin, 108, 267–290. doi: 10.1037/0033-2909.108.2.267 [DOI] [PubMed] [Google Scholar]
- Grych JH, Fincham FD, Jouriles EN, & McDonald R (2000). Interparental conflict and child adjustment: Testing the mediational role of appraisals in the cognitive-contextual framework. Child Development, 71, 1648–1661. doi: 10.1111/1467-8624.00255 [DOI] [PubMed] [Google Scholar]
- Haines J, Neumark-Sztainer D, Eisenberg ME, & Hannan PJ (2006). Weight teasing and disordered eating behaviors in adolescents: Longitudinal findings from Project EAT (Eating Among Teens). Pediatrics, 117, e209–e215. doi: 10.1542/peds.2005-1242 [DOI] [PubMed] [Google Scholar]
- Haines J, Neumark-Sztainer D, Hannan PJ, Berg P, & Eisenberg ME (2008). Longitudinal and secular trends in weight-related teasing during adolescence. Obesity, 16, s18–s23. doi: 10.1038/oby.2008.447 [DOI] [PubMed] [Google Scholar]
- Harold GT, Finchum FD, Osborne LN, & Conger RD (1997). Mom and dad are at it again: Adolescent perceptions of marital conflict and adolescent psychological distress. Developmental Psychology, 33, 333–350. doi: 10.1037//0012-1649.33.2.333 [DOI] [PubMed] [Google Scholar]
- Hawkins RC II, & Clement PF (1984). Binge eating: Measurement problems and a conceptual model In Hawkins RC, Fremouw WJ, & Clement PF (Eds.), The Binge Purge Syndrome: Diagnosis, Treatment, and Research (pp. 229–251). New York: Springer. [Google Scholar]
- Heatherton TF, & Baumeister RF (1991). Binge eating as escape from self-awareness. Psychological Bulletin, 110, 86–108. doi: 10.1037/0033-2909.110.1.86 [DOI] [PubMed] [Google Scholar]
- Hochgraf AK, Kahn RE, & Kim-Spoon J (2017). The moderating role of emotional reactivity in the link between parental hostility and eating disorder symptoms in early adolescence. Eating Disorders, 25, 1–16. doi: 10.1080/10640266.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochgraf AK, McHale SM, & Fosco GM (2018). Parent responsiveness and gender moderate bidirectional links between self-esteem and weight concerns during adolescence. Journal of Family Psychology. doi: 10.1037/fam0000434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hox J (2010). Multilevel analysis, techniques and applications. New York, NY: Routledge. [Google Scholar]
- Jacobi C, Abascal L, & Taylor CB (2004). Screening for eating disorders and high-risk behavior: Caution. International Journal of Eating Disorders, 36, 280–295. doi: 10.1002/eat.20048 [DOI] [PubMed] [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Haydel KF, Wilson DM, Hammer L,… & Strachowski D (1996). Weight concerns influence the development of eating disorders: A 4-year prospective study. Journal of Consulting and Clinical Psychology, 64, 936. doi: 10.1037/0022-006X.64.5.936 [DOI] [PubMed] [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Wilson DM, Haydel KF, Hammer LD, … & Kraemer H (1994). Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: A three-year prospective analysis. International Journal of Eating Disorders, 16, 227–238. doi: [DOI] [PubMed] [Google Scholar]
- Krishnakumar A, & Buehler C (2000). Interparental conflict and parenting behaviors: A meta-analytic review. Family Relations, 49, 25–44. doi: 10.1111/j.1741-3729.2000.00025.x [DOI] [Google Scholar]
- Lam CB, & McHale SM (2012). Developmental patterns and family predictors of adolescent weight concerns: A replication and extension. International Journal of Eating Disorders, 45, 524–530. doi: 10.1002/eat.20974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam CB, McHale SM, & Crouter AC (2012). Parent–child shared time from middle childhood to late adolescence: Developmental course and adjustment correlates. Child Development, 83, 2089–2103. doi: 10.1111/j.1467-8624.2012.01826.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson RW, & Almeida DM (1999). Emotional transmission in the daily lives of families: A new paradigm for studying family process. Journal of Marriage and the Family, 61, 5–20. doi: 10.2307/353879 [DOI] [Google Scholar]
- May AL, Kim JY, McHale SM, & Crouter A (2006). Parent–adolescent relationships and the development of weight concerns from early to late adolescence. International Journal of Eating Disorders, 39, 729–740. doi: 10.1002/eat.20285 [DOI] [PubMed] [Google Scholar]
- Maynard LM, Galuska DA, Blanck HM, & Serdula MK (2003). Maternal perceptions of weight status of children. Pediatrics, 111, 1226–1231. [PubMed] [Google Scholar]
- McCarthy M (1990). The thin ideal, depression and eating disorders in women. Behaviour Research and Therapy, 28, 205–214. doi: 10.1016/0005-7967(90)90003-2 [DOI] [PubMed] [Google Scholar]
- McHale SM, Corneal DA, Crouter AC, & Birch LL (2001). Gender and weight concerns in early and middle adolescence: Links with well-being and family characteristics. Journal of Clinical Child Psychology, 30, 338–348. doi: 10.1207/S15374424JCCP3003_6 [DOI] [PubMed] [Google Scholar]
- Miniati M, Callari A, Maglio A, & Calugi S (2018). Interpersonal psychotherapy for eating disorders: Current perspectives. Psychology Research and Behavior Management, 11, 353. doi: 10.2147/PRBM.S120584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Bauer KW, Friend S, Hannan PJ, Story M, & Berge JM (2010). Family weight talk and dieting: How much do they matter for body dissatisfaction and disordered eating behaviors in adolescent girls? Journal of Adolescent Health, 47, 270–276. doi: 10.1016/j.jadohealth.2010.02.001\ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Croll J, Story M, Hannan PJ, French SA, & Perry C (2002). Ethnic/racial differences in weight-related concerns and behaviors among adolescent girls and boys: Findings from Project EAT. Journal of Psychosomatic Research, 53, 963–974. doi: 10.1016/S0022-3999(02)00486-5 [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, & Eisenberg M (2006). Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: How do dieters fare 5 years later? Journal of the American Dietetic Association, 106, 559–568. doi: 10.1016/j.jada.2006.01.003 [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Larson NI, Eisenberg ME, & Loth K (2011). Dieting and disordered eating behaviors from adolescence to young adulthood: Findings from a 10-year longitudinal study. Journal of the American Dietetic Association, 111, 1004–1011. doi: 10.1016/j.jada.2011.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Story M, & van den Berg P (2008). Accurate parental classification of overweight adolescents’ weight status: Does it matter? Pediatrics, 121, e1495–e1502. doi: 10.1542/peds.2007-2642 [DOI] [PubMed] [Google Scholar]
- Shomaker LB, & Furman W (2009). Interpersonal influences on late adolescent girls’ and boys’ disordered eating. Eating Behaviors, 10, 97–106. doi: 10.1016/j.eatbeh.2009.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim L, & Zeman J (2005). Emotion regulation factors as mediators between body dissatisfaction and bulimic symptoms in early adolescent girls. The Journal of Early Adolescence, 25, 478–496. doi: 10.1177/0272431605279838 [DOI] [Google Scholar]
- Singer JD (1998). Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. Journal of Educational and Behavioral Statistics, 24, 323–355. doi: 10.2307/1165280 [DOI] [Google Scholar]
- Smolak L (2004). Body image in children and adolescents: Where do we go from here? Body Image, 1, 15–28. doi: 10.1016/S1740-1445(03)00008-1 [DOI] [PubMed] [Google Scholar]
- Steinberg L (2001). We know some things: Parent–adolescent relationships in retrospect and prospect. Journal of Research on Adolescence, 11, 1–19. doi: 10.1111/1532-7795.00001 [DOI] [Google Scholar]
- Stice E, & Bearman SK (2001). Body-image and eating disturbances prospectively predict increases in depressive symptoms in adolescent girls: a growth curve analysis. Developmental Psychology, 37, 597. doi: 10.1037/0012-1649.37.5.597 [DOI] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H (2013). The Body Project: A Dissonance-based Eating Disorder Prevention Intervention. New York: Oxford University Press. [Google Scholar]
- Stice E, Shaw H, & Nemeroff C (1998). Dual pathway model of bulimia nervosa: Longitudinal support for dietary restraint and affect-regulation mechanisms. Journal of Social and Clinical Psychology, 17, 129–149. doi: 10.1521/jscp.1998.17.2.129 [DOI] [Google Scholar]
- Tanofsky-Kraff M, Wilfley DE, Young JF, Mufson L, Yanovski SZ, Glasofer DR, & Salaita CG (2007). Preventing excessive weight gain in adolescents: Interpersonal psychotherapy for binge eating. Obesity, 15, 1345–1355. doi: 10.3945/ajcn.114.092536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor CB, Bryson S, Doyle AAC, Luce KH, Cunning D, Abascal LB, … & Wilfley DE (2006). The adverse effect of negative comments about weight and shape from family and siblings on women at high risk for eating disorders. Pediatrics, 118, 731–738. doi: 10.1542/peds.2005-180 [DOI] [PubMed] [Google Scholar]
- Towns N, & D’auria J (2009). Parental perceptions of their child’s overweight: an integrative review of the literature. Journal of Pediatric Nursing, 24, 115–130. doi: 10.1016/j.pedn.2008.02.032 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2001). Profile of general demographic characteristics: 2000. Retrieved from https://www2.census.gov/library/publications/2001/dec/2kh42.pdf?#
- Van Ryzin MJ, & Nowicka P (2013). Direct and indirect effects of a family-based intervention in early adolescence on parent− youth relationship quality, late adolescent health, and early adult obesity. Journal of Family Psychology, 27, 106. doi: 10.1037/a0031428 [DOI] [PMC free article] [PubMed] [Google Scholar]