Abstract
Purpose:
The study purpose was to evaluate the content of a proactive population health management intervention aimed at promoting uptake of smoking cessation treatments offered by the Illinois Tobacco Quitline (ITQL) among lesbian, gay, bisexual, and transgender (LGBT)-identified smokers.
Methods:
This study represents a partnership between a community-based health center and university researchers. As part of the study, focus groups and in-depth interviews were conducted with LGBT smokers (N = 30). First, we conducted focus groups to obtain feedback on the readability, acceptability, and motivational salience of a targeted and nontargeteed proactive outreach letter. After revisions, a series of in-depth interviews were conducted to evaluate finalized materials. Focus groups and interviews were systematically analyzed.
Results:
Based on feedback, the revised intervention letter was rated more positively than the initial version, with 80% of participants indicating that they found the information in the letter to be useful. Further, more participants reported that the letter would motivate them to accept a call from a quitline counselor compared with the initial version (47.6% vs. 60.0%, respectively). In the final iteration, 60% of participants preferred the targeted letter, 30% preferred the nontargeted letter, and 10% had no preference. In the first iteration, outreach text messages were rated as unacceptable or completely unacceptable by 54% of participants. The revised text messages and protocols were seen as unacceptable by only 10% of participants.
Conclusions:
The development and testing of population-based and cost-effective interventions is critical to the reduction of LGBT smoking disparities. The study protocol and intervention materials were well-received by participants. In a future study, we will evaluate the efficacy of the intervention in increasing use of the quitline among LGBT smokers.
Keywords: LGBT, smoking cessation interventions, proactive, quitlines, culturally targeted
The burden of smoking is particularly high within LGBT community. Current estimates place LGBT tobacco use at almost double the rate of the general population.1,2 A range of risk factors account for the elevated tobacco rates among LGBT populations including heavy drinking,3 permissive social norms,4 few factors that deter smoking,5 targeted advertising by the tobacco industry,6 increased stress owing to stigma and discrimination,7 increased risk for low income owing to underemployment,8 and victimization experiences.9 A lack of awareness of and access to smoking cessation resources also represents an important driver of persistent smoking.10 State tobacco quitlines provide free and accessible smoking cessation pharmacological (nicotine patches) and behavioral treatment offered by trained counselors.11 Despite the demonstrated efficacy of quitline services,12 only 8% of smokers who are trying to quit and who are aware of quitlines actually use them.13 Research suggests that LGBT smokers are even less likely to know about or use quitlines.14 Targeted interventions aimed at increasing LGBT smokers’ awareness of and engagement with quit lines represent a cost-effective strategy for addressing tobacco use disparities in this underserved population of smokers.
CLINIC-BASED INTERVENTIONS LINKING PATIENTS TO STATE QUITLINES
Clinicians play an important role in identifying and referring patients to smoking cessation resources.12,13,15 Although provider advice to quit is associated with an increased likelihood of a patient making a quit attempt,16 clinicians cite multiple barriers to engaging their patients in smoking cessation activities.17 Primary among those barriers is low motivation and/or readiness to quit smoking among patient groups.18 Despite most smokers being interested in quitting,19 only about 10% of smokers are ready to set a quit date in the next 30 days.20 A willingness to set a quit date is a recommended measure for health care providers to identify patients who are appropriate for smoking cessation treatment.15 An additional barrier for clinicians is that many patients who smoke do not see their primary care provider on a regular basis and, therefore, do not have an opportunity for clinician advice and assistance in quitting. A provider’s confidence in their smoking cessation training and time constraints in a primary care setting represent further barriers.21
Electronic medical record-based population health management interventions may help to reduce barriers to offering smoking cessation resources to patients who are not ready to set a quit date or who do not routinely access health care services.22 Using this approach, all smokers in a health care facilities’ electronic medical record are contacted and offered information about smoking cessation. In collaboration with a federally qualified health care (FQHC) system, our research team has developed a population-based proactive smoking cessation intervention that aims to facilitate the linkage of patients receiving treatment at FQHC’s to the state tobacco quit line. Patients identified as smokers in the Electronic medical record are sent a single-page letter with content targeted to low-income, low-literacy smokers who may or may not be ready to quit smoking. This proactive outreach letter, sent to patients on behalf of their health care provider, offered advice to quit smoking and informed smokers that they would receive a call from a quitline counselor. Importantly, patients were informed that they could select their own goal of quitting smoking or cutting down the number of cigarettes they smoke. In addition, participants were given the option of opting-out of the study entirely.
Based on self-determination theory,23 the main hypothesis being tested in our ongoing research is whether offering patients the choice to either quit or reduce their smoking gradually may increase their engagement and use of the state tobacco quit line. Self-determination theory is a theory of motivation that stresses the importance of competence, relatedness, and autonomy in goal-directed behavior, such as health behavior change.23 Choice is central to autonomy support and can be achieved by providing effective options for behavior change. Integration of autonomy support into intensive clinic-based smoking cessation treatment has been shown to increase long-term abstinence.24 In our prior research, trained smoking cessation counselors for the state tobacco quitline used readiness to quit to tailor treatment to each individual smoker (http://quityes.org/about-the-quitline/what-to-expect-when-you-call.html). Smokers who are ready to quit smoking are encouraged to set a quit date and are supported in abstinence focused treatment goals. Among smokers who are interested in quitting, abrupt cessation results in significantly higher shorter and longer term abstinence rates compared with gradual reduction (at 4 weeks 49% vs. 39.2% and at 6 months, 22.0% vs. 15.5%).25 However, for smokers who are not ready to make a quit attempt, reduction is offered as an alternative and reduction focused treatment goals are established.26 Gradual reduction among patients who are not currently interested in quitting completely has been demonstrated to increase the probability of future abstinence.27,28
Study Purpose
Despite high tobacco use rates, few studies focus on LGBT smokers and, to our knowledge, no population-based approaches have been developed for FQHC serving predominately LGBT patients. To address this gap in the literature, the purpose of this study was to evaluate the content of a proactive population health management intervention, delivered in the context of a FQHC, aimed at promoting uptake of smoking cessation treatment offered by the ITQL among LGBT-identified smokers. Building on our prior research, we specifically sought to obtain feedback on 1) our proposed proactive smoking cessation intervention approach, 2) personal choice in smoking cessation goal setting (cutting down vs. quitting) as part of the intervention approach, and 3) the readability, acceptability, and motivational salience of the LGBT-targeted and nontargeted intervention materials.
METHODS
Study Design
A mixed methods design (focus group and survey data) were used to adapt an existing proactive population health smoking cessation intervention to the needs of LGBT smokers. The main intervention approach, a proactive outreach letter, was developed in our previous research to be easily understood by patients with low health literacy, and contained statements designed to motivate, support, and provide resources to low-income adult smokers. The language of the letter was based on self-determination theory and motivational interviewing principles.24 Choice is central to autonomy support and can be achieved by providing effective options for behavior change. Integration of autonomy support into intensive clinic-based smoking cessation treatment has been shown to increase long-term abstinence.25 This letter was used as the foundation of the targeted LGBT proactive letter developed in this study (Appendix A). LGBT targeting was based on the scientific literature, input from our advisory board, and prior research conduct by the team.4,5,7
Community Partnership
This qualitative study was conducted in collaboration with Howard Brown Health (HBH). HBH is a FQHC center with nine locations throughout the greater Chicago metropolitan area that provides services to LGBT and other underserved populations. The agency serves more than 27,000 adults and youth each year in its diverse health and social service delivery system focused around seven major programmatic divisions: primary medical care, behavioral health, research, HIV/STI prevention, youth services, elder services, and community initiatives. One of the study authors (A.K.M.) has served as an academic research partner with HBH since 1997 and has collaborated on five funded and nonfunded research projects related to cancer-related health disparities among LGBT populations. Given the high rates of smoking in their clinic populations, the majority of prior collaborations have focused on smoking cessation research and programming. The current project was first discussed with the Chief Executive Officer, HBH Medical Director, the Director of Behavioral Health, and the Director of Research. The project was determined to meet the needs of the HBH patients, clinical providers, and to be consistent with prior research collaborations between the first study author and the organizational leadership. Although community and academic partnerships create important opportunities for improving health for underserved populations, challenges can also exist in these relationships. As such, before finalization of the study, we discussed important issues such as ownership of data, equitable balance of resources and leadership, and conflict resolution approaches.
After approval by the executive team, the director of research at HBH (D.B.) was involved in all aspects of the current study including design, implementation, and manuscript preparation. In order to obtain the perspectives of clinicians providing services for LGBT patients, we established an advisory group of providers employed at HBH (n = 3). Members of the provider advisory board met with the research team on three separate occasions and provided input on the intervention procedures, the content of the targeted outreach letter and text messages, and helped to ensure that the proposed intervention methods met all FQHC regulatory and Health Insurance Portability and Accountability Act of 1996 requirements. Further, members of the advisory committee provided input on how future intervention procedures would impact provider behaviors associated with smoking cessation. All study procedures were approved by the Institutional Review Board at Northwestern University, and registered with the institutional review boards of the University of Illinois at Chicago and Northeastern Illinois University. Additionally, the research committee at HBH reviewed and approved the study.
Participant Recruitment and Study Enrollment
In this developmental study aimed at adapting a proactive smoking cessation intervention to the needs of sexual and gender minorities, LGBT smokers were recruited using a variety of strategies including passive recruitment activities (e.g., posted flyers, social media, snowball sampling) and clinic based recruitment (e.g., posted flyers). Study eligibility criteria included 1) self-identity as LGBT, 2) age 18 or over, 3) current smoker, 4) English speaking, and 5) ability to provide informed consent to participate in the focus groups or individual interviews. Trained research staff screened interested individuals for study eligibility over the telephone. Eligible and interested individuals were given appointment times to participate in a 90-minute focus group or a semistructured interview lasting 30 to 45 minutes. Informed consent was conducted in person by a trained research assistant before the focus groups and in-depth interviews. Study participants received a $20 gift card.
Study Procedures
The study was conducted in two phases. In phase 1, focus groups (n = 3) were conducted with LGBT smokers (n = 23) at three separate locations affiliated with HBH. Focus groups were conducted according to standardized methodology including the use of trained interviewers, a focused interviewer guide, and careful review of transcribed audio-recordings. The interviewer’s guide was developed by members of the advisory board and research team to obtain feedback regarding 1) awareness of the services offered by the ITQL, 2) the acceptability of receiving a proactive letter from their HBH provider and a call from a ITQL smoking cessation counselor, 3) attitudes regarding being offered options in smoking cessation treatment goals, 4) feedback on the readability, acceptability, and motivation salience of the information provided in the outreach letters, 5) attitudes regarding the LGBT-specific information in the targeted proactive letter, and 6) preferences regarding the frequency, time, and content of text messages aimed at increasing participation in ITQL services. Participants also completed a brief paper and pencil survey (approximately 10 minutes) measuring demographic and smoking characteristics.
During the focus groups, participants were asked to review and discuss two versions of the proactive outreach letter (a standard letter developed for low-income smokers and a version adapted for LGBT smokers) and sample text messages aimed at reminding patients about the upcoming quitline call and to motivate participation. After the group discussion, participants were then asked to provide individual feedback on the letter and text messages via a paper and pencil survey to measure the 1) acceptability of receiving letters and text messages from their health care provider, 2) clarity of the language used, 3) clarity of the materials’ purpose, 4) usefulness of information provided, 5) motivational salience of the letters and texts, and 6) likelihood that the letter and texts would motivate a change in their smoking behavior. Responses were given using Likert-scale response options (from 1 [strongly disagree] to 10 [strongly agree]). Participants also answered a range of questions to determine prior knowledge of the LGBT-specific information provided in the targeted proactive outreach letter (e.g., “Were you aware that LGBT persons smoke at rates higher than non-LGBT persons?”).
In phase 2, information derived from the focus group participants and input from the advisory group members was used to revise the provider letter and text messages. Next, semistructured, in-depth interviews were conducted with a second group of LGBT smokers (n = 10) to obtain feedback on the revised materials. Eligibility criteria, recruitment approaches, data collection sites and demographic and smoking characteristic survey measures were the same as in phase one. Participants completed a 30-minute interview that included reviewing materials and providing input on the readability, acceptability, cultural appropriateness, and satisfaction with revised materials. Respondents were asked to provide feedback on the proactive letters and text messages using the same approaches as the focus group participants in phase 1. Participants in phase 1 of the study were not eligible to participate in phase 2.
Data Analysis
A quantitative analysis of participant’s demographic surveys and feedback ratings forms was conducted in SPSS29 via standard descriptive and frequency statistics. Qualitative data analyses for both the focus groups and the in-depth interviews went through a three-step process: 1) each interview audio file was transcribed verbatim to a text document, 2) each document was hand-coded using coding schemes developed based on interview guide described above, and 3) subthemes were identified.30 As is standard in qualitative research,30 we used an iterative process of analysis by examining and re-examining the facts and meanings contained in these data to develop more refined subthemes. The total sample size of 30 participants is appropriate for qualitative research studies aimed at developing intervention research studies.30
RESULTS
Study Participants
Tables 1 and 2 display the demographic and smoking characteristics of the study participants. The mean ± standard deviation age of participants (n = 33) was 30.90 ± 12.97 years. The participants were diverse in terms of race/ethnicity, gender identity, and sexual orientation which is representative of the patient populations served by HBH. The majority of participants were daily smokers (60%) and smoked an average of 6.2 ± 4.4 cigarettes per day. Forty-three percent of smokers preferred a mentholated brand of cigarette (43.3%). Forty-three percent of participants reported smoking within the first 30 minutes of waking, which is an indicator of a high degree of nicotine dependence.31
Table 1.
Participant Demographic Characteristics (N = 30)
| Characteristics | n (%) |
|---|---|
| Age (mean ± standard deviation) | 30.90 ± 12.97 |
| Race | |
| Black/African American | 10 (33.3) |
| White | 15 (50.0) |
| Latino | 5 (16.6) |
| Gender identity | |
| Male | 12 (40.0) |
| Female | 11 (36.7) |
| Transgender or gender nonconforming | 7 (23.3) |
| Sexual orientation | |
| Bisexual | 5 (16.7) |
| Gay | 11 (36.7) |
| Lesbian | 4 (13.3) |
| Queer | 6 (20.0) |
| Other | 4 (13.4) |
| Education | |
| Less than high school graduate | 2 (6.7) |
| High school graduate | 9 (30.0) |
| Some college | 7 (23.3) |
| Bachelor’s degree and above | 12 (40.0) |
| Employment | |
| Currently employed, full or part time | 19 (63.3) |
| Not currently employed | 11 (36.7) |
| Health insurance | |
| Yes | 27 (90.0) |
| No | 3 (10.0) |
| Self-rated health | |
| Excellent | 3 (10.0) |
| Very good | 12 (40.0) |
| Good | 10 (33.3) |
| Fair | 5 (16.7) |
| Poor | 0 (0.0) |
Table 2.
Smoking Characteristics of Study Participants (N = 30)
| n (%) | |
|---|---|
| Have you smoked at least 100 cigarettes (5 packs) in your life? | |
| Yes | 28 (93.3) |
| No | 2 (6.7) |
| What type of cigarettes do you usually smoke? | |
| Regular | 7 (23.3) |
| Menthol | 13 (43.3) |
| Both | 10 (33.3) |
| How often do you smoke? | |
| 6–7 days a week | 18 (60.0) |
| 4–5 days a week | 2 (6.7) |
| 2–3 days a week | 3 (10.0) |
| ≤ 1 day a week | 7 (23.3) |
| How many cigarettes do you smoke on the days that you smoke (mean)? | 6.2 |
| How soon is your first cigarette after waking on days when smoke? | |
| Within 5 minutes | 6 (20.0) |
| Within 6–30 minutes | 7 (23.3) |
| 31–60 minutes | 15 (50.0) |
| Missing | 2 (6.7) |
| Has your health care provider suggested you quit smoking? | |
| Yes | 21 (70.0) |
| No | 9 (30.0) |
| Have you tried to quit smoking in the last 12 months? | |
| Yes, I tried to quit completely | 14 (46.7) |
| No, I have reduced or cut back but not tried to quit | 13 (43.3) |
| No, I have not tried to quit or cut back | 3 (10.0) |
| Did you use nicotine replacement therapy (n = 26)? | |
| Yes | 8 (30.8) |
| No | 18 (69.2) |
| The last time you tried to quit smoking, did your provider recommend that you cut down or quit? | |
| Yes | 9 (34.6) |
| No | 15 (57.7) |
| Don’t know | 2 (7.7) |
| The last time you tried to quit, did your provider link you to any stop smoking resources? | |
| Yes | 1 (3.8) |
| No | 23 (88.5) |
| Don’t know | 2 (7.7) |
| How motivated are you to quit smoking right now? (scale from 1 [not at all motivated] to 10 [extremely motivated]), mean ± standard deviation | 5.3 ± 3.1 |
Qualitative Results
Key qualitative findings from the focus group and in-depth interviews are described in the next section and organized based on broad categories examined during the study and the subthemes that emerged. Where appropriate, illustrative quotes are also provided. In addition, we included participants’ paper and pencil survey ratings of the intervention procedures and materials.
Feedback on the Proactive Smoking Cessation Intervention
Issues of Privacy and Consent.
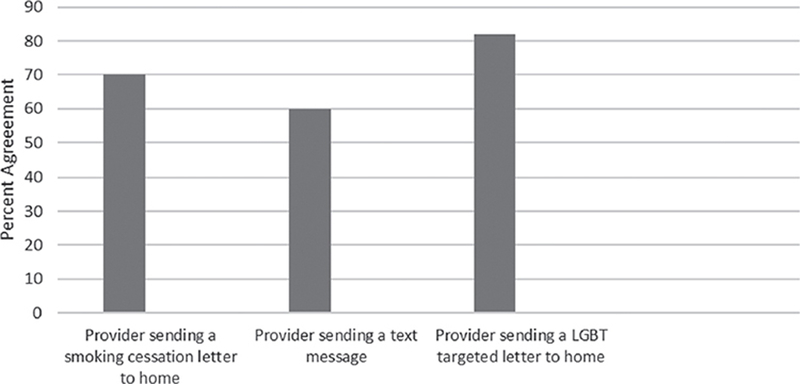
The proposed smoking cessation intervention is a proactive smoking cessation intervention counseling call from the ITQL. The contact is proactive in that interaction with a counselor from the ITQL is initiated by health care providers and not by patients (patients can opt-out of the contact at any time by texting or phoning the study research assistant). Patient acceptability is central to the success of this type of intervention. Figure 1 displays participants’ acceptability ratings at baseline for each of the core aspects of the proactive intervention. Initial ratings suggested a moderate degree of acceptability of proposed intervention procedures. During phase 1, focus group participants raised questions and concerns related to patient privacy and informed consent. Specifically, participants expressed discomfort with being sent a letter based on their smoking status and being contacted by a ITQL counselor without requesting or providing consent for the communication.
Figure 1.
Acceptability of Elements of Proactive Intervention (N = 30); y-axis = percent agreement
If I just admitted to my provider that I smoked, and all of the sudden I get something in the mail. I didn’t say I wanted to quit. I just said that I smoked. I feel it’s bordering on invasion of privacy.
If you haven’t asked for help, to somebody actually reach into your life in that way seems overstepping.
All patients at HBHC sign a universal consent form that allows their health care providers to contact them about issues related to their health care. The proactive letter offering advice and assistance with smoking cessation would fall under the scope of the universal consent for contact. Nevertheless, health care providers in our advisory board also expressed similar reservations about the proactive nature of the intervention. Based on results from the focus groups, adjustments were made to the proposed study design and proactive outreach letter to try and alleviate the specific concerns noted. First, the language in the letter was modified to emphasize that the letter is being sent from their provider because of the organizations commitment to health promotion and their provider’s concerns about their health and well-being. Although the original letter included an opt-out statement, we revised all of our materials to provide greater emphasis on the participant’s ability to opt-out of the call from the quitline counselor. Additionally, every communication associated with the proposed study now includes the option to opt-out of all further contact.
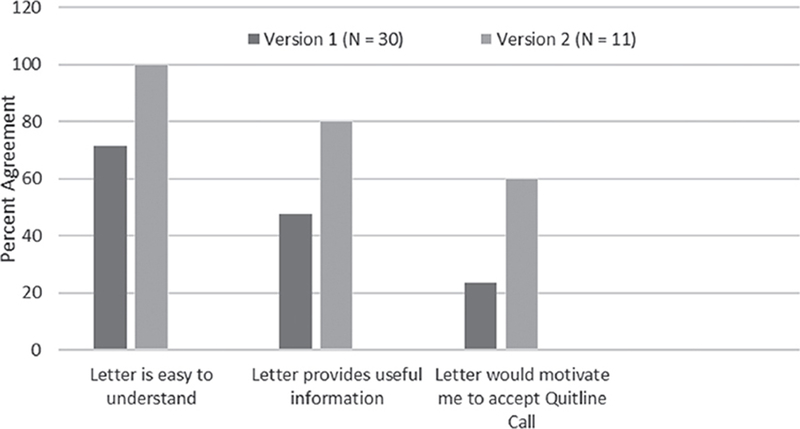
As shown in Figure 2, the revised provider outreach letter was met with much higher approval ratings compared with the original version.
Figure 2.
Participant Ratings of the Acceptability of Standard Proactive Letter; y-axis = Percent Agreement
They’re going to call you in 2 weeks kind of slaps me in the face at first. I thought that was very imposing. Then I realized making that call is the hardest thing, so maybe that’s not such a bad thing. I think the letter did a good job of calming me down from it.
Attitudes Regarding Engagement with the ITQL
Another goal of the study was to better understand awareness of and comfort with interactions with the ITQL. In a finding consistent with prior research,12 study participants were largely unfamiliar with the ITQL which was established in 2000 and which has materials specifically for LGBT smokers (http://map.naquitline.org/profile/usa/il/).
I haven’t seen or heard about it.
The Quitline—this is a new service that is being developed, is that right?
Consequently, participants had many questions about the ITQL including, staff training and credentials, continuity of care once enrolled in the program (e.g., working with the same counselor), costs associated with the program, the effectiveness of the treatment offered, and the various types of services that would be offered.
I think it would be important to know that you would be working with the same counselor so people don’t feel like they’re just calling in to AT&T customer service.
Some focus group participants expressed concern that the ITQL staff would not be trained or experienced in working with LGBT clients. In response to this feedback, we included an ITQL factsheet with the intervention letter that answered many of the most common questions asked including highlighting the fact that ITQL counselors have received specialized counseling on LGBT populations (see Appendix B for a copy of the fact sheet). The revised letter was rated more positively than the initial version, with 80% of participants indicating that they found the information in the letter about the ITQL to be useful. Further, more participants reported that the letter would motivate them to accept a call from an ITQL counselor compared with the initial version (47.6% vs. 60.0%, respectively; Figure 2).
Evaluation of the Proactive Provider Letter
Readability.
One purpose of the qualitative study was to refine the language in the targeted outreach letter to improve its readability, motivational salience, and acceptability to LGBT smokers (Figure 2). Prior research has shown a strong association between health literacy and health promoting behaviors among a range of racial/ethnic populations.32 In our original study, the proactive letter was designed to address the health literacy needs of low-income populations and measured at approximately a sixth-grade reading level using the Flesch-Kincaid readability test.33 Although health literacy has not been extensively studied in LGBT populations, reading level and reading comprehension were considered when targeting the letter to LGBT-specific smoking issues. The letter measured at a sixth-grade reading level using the Coleman-Liau index,34 the SMOG index,35 and the Automated Readability Index.36 In the final version of the proactive letter, most participants had no difficulty reading and comprehending the materials; 100% of participants rated the letter as easy or very easy to read.
Acceptability.
Participants responded negatively to the language and tone of the intervention letter and text messages. Phrases that our team thought were either neutral or stating factual information were sometimes perceived as condescending, shaming, or nagging. Information that is widely known, for instance, that cigarettes are addictive and expensive, or bad for your health, was perceived by several participants as patronizing. Phrases like, “you can learn to control your cravings—don’t let them control you,” were also viewed as condescending. Some participants similarly took offense at statements that they found presumptuous, for instance, “Quitting smoking is the most important thing that you can do for your health.”
Members of our HBH advisory board provided suggestions and were highly instrumental in improving the language of the letter, emphasizing people-first language and positive framing of messaging approaches.
I might reframe that first sentence instead of being negative . . . something positive about cutting down. Like, “If you’d like to cut down, we can help you.”Also, if you’re gonna say “people who are HIV positive,” I would ask you to change it to living with—“people who are living with HIV,” so make it people-first language.
As shown in Figure 2, revisions to the letter based on feedback from the focus group participants and HBH advisory board improved participant response to the language. When asked how they felt about the intervention letter, responses from participants in phase 1 of the study were decidedly mixed. After removing language in the letter that was perceived as negative and increasing the supportive language, 80% of participants in phase 2 felt positively or very positively about the language in the final version of the letter.
Patient Choice in Goal Setting.
Central to our smoking cessation intervention is autonomy or choice. In the proactive provider letter, patients are offered the freedom to decide to work with an ITQL counselor toward quitting smoking or toward cutting back on the number of cigarettes they currently smoke. By offering choices about treatment, we hope to empower participants to see themselves as partners in the smoking cessation process, and thus, increase their engagement with ITQL counselors. The preponderance of participants responded well to the option of choice.
I found [the letter] to be very empathetic to the plight of the smoker and the smoker who wants to quit. Understanding that you may not be ready to now but we can help you at least cut down if that’s something you’re interested in. Giving you a variety of options I think is cool.
Feedback on the Culturally Targeted Language in the Provider Letter
Lack of Awareness of LGBTQ-Specific Issues and Smoking.
Using the outreach letter that was originally developed to address the informational and health literacy needs of general populations of low-income smokers receiving treatments at FQHC, we added information targeted to LGBT smokers. Specifically, we included information about higher rates of smoking in the LGBT community, targeting of the LGBT community by the tobacco industry, and highlighted health risks that are exacerbated by smoking (i.e., complications with hormone use and contraindications with HIV/AIDS medication).37–39 Based on survey responses, we found knowledge deficits regarding LGBT-specific smoking issues: 45% of study participants were unaware of higher rates of smoking among LGBT individuals, 64% were unaware of LGBT targeting by the tobacco industry, 45% were unaware that smoking may pose additional risks for those taking hormonal therapy, and 73% were unaware that smoking may pose additional risks for those taking some HIV/AIDS treatments (data not shown).
Attitudes Regarding the LGBT-Specific Information.
Prior research has identified a preference among LGBT smokers for a culturally targeted smoking cessation intervention.5 In the current study, inclusion of LGBT community-specific language elicited varying responses. Some participants felt their sexual orientation or gender identity was unrelated to their smoking behaviors and should not be addressed in the letter. Others felt more supported and validated by LGBT-specific language in the letter.
I think it’s a little silly . . . to target LGBTQ primarily. People are people, and people are stressed out whether you’re gay or not.
This being addressed to my LGBT membership makes it more personal. I can imagine that if I were to get this in the mail highlighting my identity as a lesbian that I would be more willing to try the Illinois Tobacco Quitline. Because somebody from my community is referring me.
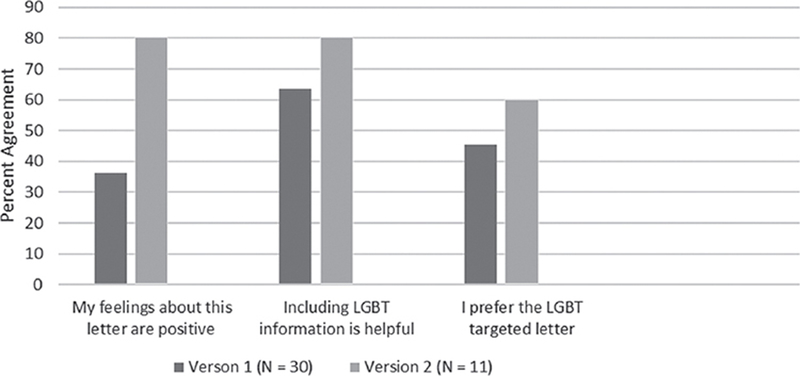
Although participants expressed mixed opinions about language that was inclusive of information specific to the LGBT community, revisions to the letter improved the acceptability of the content. In the first iteration, only 36.4% of participants rated feeling positive about the targeted language in the LGBT letter. Acceptability levels increased substantially following revision with 80% of participants reporting feeling positive about the LGBT-specific language. In the final iteration, 60% of participants preferred the targeted letter, 30% preferred the nontargeted letter, and 10% had no preference (Figure 3).
Figure 3.
Participant Ratings of Targeted Elements of Proactive Letter; y-axis = percent agreement
Participant Responses to the Intervention’s Use of Text Messaging
Text messaging is proposed for the future intervention study as a means for reminding patients about the ITQL counselor’s call and encouraging engagement. Although the effectiveness of text messaging in a health care environment has been demonstrated,40 we found that receiving multiple reminder text messages was unacceptable to many participants. Based on the feedback, we reduced the number of planned text messages from five to three. In addition, we added opt-out language to each of the text messages, as requested. We also edited the content of the texts, so that they contained messages of support and information about ITQL services. In the first iteration of text messages was considered somewhat acceptable by 27% of participants and unacceptable or completely unacceptable by 54%. The second iteration of text messages were seen as acceptable by 60% of participants and unacceptable by only 10% of participants.
DISCUSSION
To date, few interventions have focused on the reduction of tobacco use disparities among LGBT populations.10 Consequently, information about the treatment preferences of LGBT smokers is limited. Results from the current study suggest that LGBT smokers are interested in receiving additional support for smoking cessation, found a proactive provider letter advising a quit attempt and providing information about cessation resources as acceptable, and favored choice in setting smoking cessation goals. However, participants were largely unaware of services offered by the ITQL or LGBT-specific information associated with smoking. As such, the informational support offered as part of the proactive letter was viewed as necessary and beneficial. Significant alterations to the language used in the letter were made based on feedback viewed as condescending or otherwise unacceptable. Additionally, greater attention was paid to concerns regarding privacy and consent and the limitations of text messaging within the context of the intervention. Community input informed changes to our intervention design and materials resulting in higher acceptability ratings and underscoring the benefit of community engagement as part of intervention development research.
Implications
The study findings contribute to the extant literature on the development of culturally targeted smoking cessation interventions for LGBT smokers and have implications for future research in this population. The collaborative partnership between an LGBT-serving FQHC and university researchers was essential to the success of the project. Based on documented higher rates of smoking among their patient population, HBH has been invested in providing leadership in offering effective and culturally appropriate smoking cessation resources to their patients. Although having benefit, prior approaches developed by this established collaborative team at HBH have required high staffing rates, relied on patients being actively in treatment or being willing to come for intensive individual or group treatment sessions.41–43 If effective, this proactive approach being developed in collaboration with HBH offers substantial benefits for the organization and the patient population in terms of reach, cost effectiveness, and increasing access to culturally appropriate services. Currently, the standard of care at HBH is the five As,15 a brief and evidence-based approach that is recommended for clinical providers treating patients who smoke. Referral of patients to the ITQL is one option for providing assistance to patients interested in quitting. However, our data show that patients are largely unaware of the quitline and the free services that they offer. The fact sheet developed as part of this project should be offered to all patients at HBH who smoke, especially those being referred to the quitline by their providers. Further, study participants were largely unaware of LGBT-specific information associated with smoking. A stop smoking campaign by the clinic can use the information provided in our targeted letter to help better inform LGBT smokers about unique risk factors. For example, fact sheets can be located in the clinic setting describing the additional health risks associated with smoking for person who are HIV positive and individuals who are on hormonal therapies.
The next step in our collaborative program of research is to conduct a pilot randomized clinical trial to test the feasibility, acceptability, and benefits of the targeted proactive intervention for increasing engagement with the ITQL compared with usual care among LGBT smokers receiving care at HBH FQHC. The proposed study will contribute to the advancement of the literature on smoking cessation among disparity populations in three important ways. First, previous research has demonstrated that culturally targeted interventions increase the salience and satisfaction with behavioral change interventions41 and will be tested as part of the proposed study. Second, we will examine the application of social determination theory23 and autonomy support in enhancing the effectiveness of our proactive intervention among LGBT smokers along the readiness to quit continuum. Finally, a population management approach has not been explored as a means for reducing tobacco use disparities among LGBT smokers.10 If successful, a proactive intervention has the potential to be a cost-effective method for providing smoking cessation resources to LGBT smokers.
Limitations
Our study included a small sample of the target population from a single geographical location; thus, additional studies are required. Although participants were diverse in terms of race and ethnicity, Whites were over-represented and Latinos under-represented based on Chicago demographics.44 However, the participant sample recruited for this study is roughly similar to the population served by HBH. Although generalizability is not a specific goal of qualitative research,30 nonparticipants may have other opinions or experiences germane to understanding the promotion of smoking cessation in the LGBT community. As such, additional research with a larger and more generalizable population may be needed to confirm study findings.
CONCLUSIONS
Tobacco use disparities based on sexual orientation and gender identity are an important public health concern. The development and testing of population-based and cost-effective interventions is critical to the reduction of these disparities. This unique and well-developed community–academic partnership resulted in an important contribution to tobacco control in LGBT populations. After incorporating community feedback, the study protocol and intervention materials for a targeted, proactive smoking cessation intervention was well-received by participants. The next phase of the study will be to evaluate the efficacy of the intervention in increasing use of the ITQL among LGBT smokers.
ACKNOWLEDGMENTS
The research reported in this publication was supported, in part, by the National Institutes of Health’s National Cancer Institute, Grant NumbersU54CA202995, U54CA202997, U54CA203000 and U54CA203000-02S1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
APPENDIX A: COMMUNITY TARGETED INTERVENTION LETTER
Dear [Preferred Name]:
As part of a new program to serve patients at Howard Brown Health Center better, we have teamed up with the Illinois Tobacco Quitline. We know how hard it can be to quit smoking. We want to help.
We can help you quit smoking, or we can help you to cut down. If you are not sure about quitting, you are not alone. Most smokers want to quit, but do not feel ready. You do have other choices! Cutting down can be a great first step, and at the same time, it saves money.
Rates of smoking are really high in our community. This might be because LGBTQ folks deal with a lot of stress. Stress makes it more likely that we will start smoking, and harder for us to quit. We are also targeted by cigarette companies, who make ads that talk about pride and choice, to try to get us to smoke more. This doesn’t apply to everyone, but smoking can also create more health risks for some LGBTQ people, like people who take hormones, or people who are living with HIV. If you’re thinking about quitting, we want to support you.
As a part of this program, your health care provider and I have asked a counselor from the Quitline (1-866-784-8937) to call you within the next two weeks to talk about quitting or cutting down. If you do not want to be called by a Quitline counselor, please call us at 773-893-0485. Everyone is different. You can choose to work with the counselor on quitting smoking or on cutting down. Other patients tell us that talking to a Quitline counselor is helpful and motivating. The counselors understand how hard it can be to stop smoking and will help you make your own goals. You can keep the same counselor for all your phone calls.
Quitline services are free. The Quitline is paid for by the state, and they can give you free counseling and free nicotine patches, gum, or lozenges to help you quit or cut down. Nicotine patches/gums/lozenges are safe and work very well. If you are not ready to quit right now, these medicines can help you cut down, so that it is easier for you to quit once you are ready. Quitline counselors can help you decide if one of these free medicines is right for you.
Quitting smoking is life changing. Quitting smoking is hard, and it can take a few steps. Choosing to talk to a Quitline counselor is a powerful first step. You can choose to change and make your own goals. We look forward to hearing how it goes for you.
Sincerely,
Magda Houlberg, MD Chief Clinical Officer
APPENDIX B: ILLINOIS STATE TOBACCO QUIT LINE FACTSHEET
More Information About the Illinois State Tobacco Quitline
What is the Illinois State Tobacco Quitline?
The Quitline is a free service to help you quit or cut down smoking. It’s paid for by the state of Illinois.
What can they do for me?
The Quitline has counselors and coaches, who you can talk to for FREE. They’ll help talk you through how you feel about smoking and how hard it is to quit. They’ll help you make a plan that works for your life.
What about nicotine gum or patches?
The Quitline counselors can provide you with FREE nicotine gum and patches.
Do I have to call them?
Nope! If you’re receiving this letter, they will call you. You can set up a weekly phone appointment with them to talk about your smoking.
What kind of training do the counselors/coaches have?
The counselors and coaches are nurses, respiratory therapists and tobacco-cessation specialists. They’ve attended accredited nicotine dependence training programs at renowned medical research and education centers to become skilled and certified in tobacco-cessation therapies. They know their stuff, and they want to help.
The counselors have also received some education on the LGBTQ community, and the unique challenges we face.
Can I keep the same counselor over multiple phone calls?
Yes! You can speak with the same counselor each time you call.
Footnotes
Author Disclosure Statement: The authors have no potential conflicts of interests or financial relationships relevent to this article to disclose.
REFERENCES
- 1.Jamal A, Phillips E, Gentzke AS, Homa DM, Babb SD, King BA, & Neff LJ (2018). Current Cigarette Smoking Among Adults—United States, 2016. MMWR Morb Mort Wkly Rep. 2018;67(2):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drope J, Liber AC, Cahn Z, Stoklosa M, Kennedy R, Douglas CE, et al. Who’s still smoking? Disparities in adult cigarette smoking prevalence in the United States. CA Cancer J Clin. 2018. March;68(2):106–15. [DOI] [PubMed] [Google Scholar]
- 3.Matthews AK, Riley BB, Everett B, Hughes TL, Aranda F, Johnson T. A longitudinal study of the correlates of persistent smoking among sexual minority women. Nicotine Tob Res. 2014. April 11;16(9):1199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matthews AK, Steffen A, Hughes T, Aranda F, Martin K. Demographic, healthcare, and contextual factors associated with smoking status among sexual minority women. LGBT Health. 2017. February 1;4(1):17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matthews AK, Cesario J, Ruiz R, Ross N, King A. A qualitative study of the barriers to and facilitators of smoking cessation among lesbian, gay, bisexual, and transgender smokers who are interested in quitting. LGBT Health. 2017. February 1;4(1):24–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dilley JA, Spigner C, Boysun MJ, Dent CW, Pizacani BA. Does tobacco industry marketing excessively impact lesbian, gay and bisexual communities? Tob Control. 2008. August 22;17(6):385–90. [DOI] [PubMed] [Google Scholar]
- 7.McCabe SE, Hughes TL, Matthews AK, Lee JG, West BT, Boyd CJ, et al. Sexual orientation discrimination and tobacco use disparities in the United States. Nicotine Tob Res. 2019. March 30; 21(4):523–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gruskin EP, Greenwood GL, Matevia M, Pollack LM, Bye LL. Disparities in smoking between the lesbian, gay, and bisexual population and the general population in California. Am J Public Health. 2007. August;97(8):1496–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matthews AK, Cho YI, Hughes TL, Wilsnack SC, Aranda F, Johnson T. The effects of sexual orientation on the relationship between victimization experiences and smoking status among US women. Nicotine Tob Res. 2017. March 1;20(3):332–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JG, Matthews AK, McCullen CA, Melvin CL. Promotion of tobacco use cessation for lesbian, gay, bisexual, and transgender people: A systematic review. Am J Prev Med. 2014. December 1;47(6):823–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Telephone quitlines: A resource for development, implementation, and evaluation. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, Final Edition; 2004. September 15. [Google Scholar]
- 12.Stead LF, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2006. July 19; 3(3). [DOI] [PubMed] [Google Scholar]
- 13.Schauer GL, Malarcher AM, Zhang L, Engstrom MC, Zhu SH. Prevalence and correlates of quitline awareness and utilization in the United States: An update from the 2009–2010 National Adult Tobacco Survey. Nicotine Tob Res. 2013. November 19;16(5):544–53. [DOI] [PubMed] [Google Scholar]
- 14.Fallin A, Lee YO, Bennett K, Goodin A. Smoking cessation awareness and utilization among lesbian, gay, bisexual, and transgender adults: An analysis of the 2009–2010 National Adult Tobacco Survey. Nicotine Tob Res. 2015. May 25;18(4):496–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fiore MC, Jaen CR, Baker T, Bailey WC, Benowitz NL, Curry SE, et al. Treating tobacco use and dependence: 2008 update. Rockville, MD: US Department of Health and Human Services; 2008. [Google Scholar]
- 16.Kreuter MW, Chheda SG, Bull FC. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med. 2000. May 1;9(5):426. [DOI] [PubMed] [Google Scholar]
- 17.Blumenthal DS. Barriers to the provision of smoking cessation services reported by clinicians in underserved communities. J Am Board Fam Med. 2007. May 1;20(3):272–9. [DOI] [PubMed] [Google Scholar]
- 18.Sarna L, Wewers ME, Brown JK, Lillington L, Brecht ML. Barriers to tobacco cessation in clinical practice: Report from a national survey of oncology nurses. Nurs Outlook. 2001. July 1;49(4):166–72. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC). Quitting smoking among adults—United States, 2001–2010. MMWR Morb Mort Wkly Rep. 2011. November 11;60(44):1513. [PubMed] [Google Scholar]
- 20.Mauriello LM, Johnson SS, Prochaska JM. Meeting patients where they are at: Using a stage approach to facilitate engagement In: Practical Strategies and Tools to Promote Treatment Engagement 2017. (pp. 25–44). New York: Springer. [Google Scholar]
- 21.Schroeder SA. What to do with a patient who smokes. JAMA. 2005. July 27;294(4):482–7. [DOI] [PubMed] [Google Scholar]
- 22.Tzelepis F, Paul CL, Walsh RA, McElduff P, Knight J. Proactive telephone counseling for smoking cessation: Meta-analyses by recruitment channel and methodological quality. J Natl Can Inst. 2011. June 10;103(12):922–41. [DOI] [PubMed] [Google Scholar]
- 23.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000. January;55(1):68. [DOI] [PubMed] [Google Scholar]
- 24.Williams GC, Niemiec CP, Patrick H, Ryan RM, Deci EL. The importance of supporting autonomy and perceived competence in facilitating long-term tobacco abstinence. Ann Behav Med. 2009. April 17;37(3):315–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lindson-Hawley N, Banting M, West R, Michie S, Shinkins B, Aveyard P. Gradual versus abrupt smoking cessation: A randomized, controlled noninferiority trial. Ann Intern Med. 2016. May 3;164(9):585–92. [DOI] [PubMed] [Google Scholar]
- 26.Asfar T, Ebbert JO, Klesges RC, Klosky JL. Use of smoking reduction strategies among US tobacco quitlines. Addict Behav. 2012. April 1;37(4):583–6. [DOI] [PubMed] [Google Scholar]
- 27.Hughes JR, Carpenter MJ. Does smoking reduction increase future cessation and decrease disease risk? A qualitative review. Nicotine Tob Res. 2006. December 1;8(6):739–49. [DOI] [PubMed] [Google Scholar]
- 28.Lindson-Hawley N, Hartmann-Boyce J, Fanshawe TR, Begh R, Farley A, Lancaster T. Interventions to reduce harm from continued tobacco use. Cochrane Library. 2016. January 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: Author. [Google Scholar]
- 30.Patton MQ. Qualitative research and evaluation methods, 3rd ed. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 31.Baker TB, Piper ME, McCarthy DE, Bolt DM, Smith SS, Kim SY, et al. Time to first cigarette in the morning as an index of ability to quit smoking: Implications for nicotine dependence. Nicotine Tob Res. 2007. December;9(Suppl. 4):S555–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sentell TL, Tsoh JY, Davis T, Davis J, Braun KL. Low health literacy and cancer screening among Chinese Americans in California: A cross-sectional analysis. BMJ Open. 2015. January 1;5(1):e006104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kincaid JP, Fishburne RP, Rogers RL, Chissom BS. Derivation of New Readability Formulas (Automated Readability Index, Fog Count and Flesch Reading Ease Formula) for Navy Enlisted Personnel. Naval Technical Training, U. S. Naval Air Station; 1975. p. 1–48. [Google Scholar]
- 34.Coleman M, Liau TL. A computer readability formula designed for machine scoring. J Appl Psychol. 1975. April;60(2):283–284. [Google Scholar]
- 35.Mc Laughlin GH. SMOG grading-a new readability formula. J. Res Read. 1969. May 1;12(8):639–46. [Google Scholar]
- 36.Smith EA, Kincaid JP. Derivation and validation of the automated readability index for use with technical materials. Human Factors 1970. October;12(5):457–564. [Google Scholar]
- 37.Clifford GM, Polesel J, Rickenbach M, Dal Maso L, Keiser O, Kofler A, et al. Cancer risk in the Swiss HIV Cohort Study: Associations with immunodeficiency, smoking, and highly active antiretroviral therapy. J Natl Cancer Inst. 2005. March 16;97(6):425–32. [DOI] [PubMed] [Google Scholar]
- 38.Crothers K, Goulet JL, Rodriguez-Barradas MC, Gibert CL, Oursler KA, Goetz MB, et al. Impact of cigarette smoking on mortality in HIV-positive and HIV-negative veterans. AIDS Educ Prev. 2009. June;21(3 Suppl.):40–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vittecoq D, Escaut L, Monsuez JJ. Vascular complications associated with use of HIV protease inhibitors. Lancet. 1998. June 27;351(9120):1959. [DOI] [PubMed] [Google Scholar]
- 40.Krishna S, Boren SA, Balas EA. Healthcare via cell phones: A systematic review. Telemed J E Health. 2009. April 1;15(3):231–40. [DOI] [PubMed] [Google Scholar]
- 41.Matthews AK, Li CC, Kuhns LM, Tasker TB, Cesario JA. Results from a community-based smoking cessation treatment program for LGBT smokers. J Environ Public Health. 2013; 2013:984508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matthews AK, Conrad M, Kuhns L, Vargas M, King AC. Project Exhale: Preliminary evaluation of a tailored smoking cessation treatment for HIV-positive African American smokers. AIDS Patient Care STD. 2013;27(1):22–32. [DOI] [PubMed] [Google Scholar]
- 43.Matthews AK, Steffen AD, Kuhns LM, Ruiz RA, Ross NA, Burke LA. Evaluation of a randomized clinical trial comparing the effectiveness of a culturally targeted and nontargeted smoking cessation intervention for lesbian, gay, bisexual, and transgender smokers. Nicotine Tob Res. 2018. August 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Joo JY. Effectiveness of culturally tailored diabetes interventions for Asian immigrants to the United States: A systematic review. Diabetes Educ. 2014. September;40(5):605–15. [DOI] [PubMed] [Google Scholar]