Abstract
Objective
To compare the role of UA Doppler versus CPR in the prediction of neonatal SGA and short term adverse neonatal outcome in a high-risk population.
Study design
We conducted a prospective study on women referred for fetal growth ultrasounds between 26 and 36 weeks of gestation and with an EFW < 20th percentile by Hadlock standard. UA and middle cerebral artery (MCA) Doppler assessments were performed. Abnormal UA doppler was defined as: pulsatility index (PI) above the 95th percentile and absent or reverse end diastolic flow. The CPR, calculated as a ratio of the MCA PI by the UA PI, was defined as low if < 1.08. The primary outcome was the sensitivity and specificity of the two Doppler assessments to predict neonatal SGA, defined as birthweight < 10th percentile by using Alexander curves. The secondary outcomes included umbilical cord arterial pH < 7.10, APGARS at 5 minutes < 7, NICU admission, respiratory distress syndrome (RDS), hypoglycemia or a composite including any of these secondary outcomes. Chi square was performed for statistical analysis.
Results
Of 199 women meeting inclusion criteria, 94 (47.2%) had SGA and 68 (34.2%) had a composite adverse outcome. A total of 7 pregnancies with FGR had a low CPR. Abnormal UA Doppler showed a better sensitivity for predicting SGA and adverse neonatal outcomes, with comparable specificity to low CPR. The area under the ROC curve (AUC) using abnormal UA Doppler for predicting SGA was 0.54, 95% CI 0.50–0.58; and 0.51, 95% CI 0.48–0. 53 for low CPR. The AUC for predicting a composite adverse neonatal outcome are: 0.60, 95% CI 0.51– 0.68 for abnormal UA Doppler; and 0.54, 95% CI 0.47– 0.84 for low CPR.
Conclusion
The CPR did not improve our ability to predict neonatal SGA or other short-term adverse outcomes.
Introduction
Fetal growth restriction (FGR) is a significant obstetrical complication associated with increased perinatal morbidity and mortality. Despite the implementation of fetal monitoring and surveillance by ultrasound, the assessment of fetal well-being is still challenging, even more on the fetus that is presumed to have chronic hypoxia. Currently, measurement of the umbilical artery (UA) Doppler is the standardized tool to establish the risk of adverse perinatal outcomes in the setting of fetal growth restriction, including acute hypoxia and acidosis and stillbirth1.
Some researchers have proposed that the implementation of the Doppler measurements of the middle cerebral artery (MCA) in combination with the umbilical artery pulsatility indices, referred as the cerebroplacental ratio (CPR), may be useful in the assessment of fetal well-being for fetuses with growth restriction in order predict and avoid adverse perinatal outcomes2–5. The mechanism of brain sparring effect will show decreased pulsatility index as part of a lower resistance system which could be associated to poor fetal prognosis6,7. Old and recent studies suggest that the CPR improves identification of pregnancies at risk for adverse neonatal outcomes8–10. The main aim of our study was to compare CPR to the role of UA Doppler in the prediction of neonatal SGA and short term adverse neonatal outcome in a high-risk population.
Materials and Methods
This is a multicenter prospective cohort study on women referred for fetal growth ultrasound. It was started at Washington University in St. Louis in November 2013 and completed at University of South Florida in Tampa, in July 2017. All patients provided written informed consent and were enrolled in research protocols approved by the Institutional review board at both centers.
Inclusion criteria were singleton pregnancies, gestational ages (GA) between 26.0 weeks and 36.6 weeks and dating by ultrasound prior to 24.0 weeks. Multiple gestations and fetuses with chromosomal or congenital malformations were excluded. The GA was estimated from the last menstrual period and revised by ultrasound dates when there was significant discrepancy using the American Congress of Obstetricians and Gynecologists guidelines11. The biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), and femur length (FL) measurements were obtained by following the recommendations of the International Society of Ultrasound in Obstetrics and Gynecology12.
Socio-demographic data of all enrolled subjects were collected, including maternal age, body mass index (BMI), smoking, alcohol, socioeconomic status, ethnicity, parity and coexisting maternal medical disorders, previous and current pregnancy information and ultrasound examinations.
Following delivery, we reviewed records and collected information on pregnancy complications, type of labor, mode of delivery, delivery complications, gestational weight at delivery, birth weight, Apgar scores, cord blood gases, neonatal intensive care unit (NICU) admission and discharge. Newborn outcomes were also collected including respiratory distress syndrome, intraventricular hemorrhage (IVH), hypoglycemia, necrotizing enterocolitis, periventricular leukomalacia, and seizures.
FGR was defined as an EFW <10th percentile using Hadlock standards13. Neonatal SGA was defined as birthweight < 10th percentile for GA by Alexander chart14.
UA and middle cerebral artery (MCA) Doppler assessments were performed. Abnormal UA Doppler was defined as: pulsatility index (PI) above the 95th percentile and absent or reverse end diastolic flow. The CPR, calculated as a ratio of the MCA PI by the UA PI, was defined as low if < 1.0815,16. The primary outcome was the sensitivity and specificity of the two Doppler assessments to predict neonatal SGA, defined as birthweight < 10th percentile by using Alexander curves. The secondary outcomes included umbilical cord arterial pH < 7.10, Apgar scores at 5 minutes < 7, NICU admission, respiratory distress syndrome (RDS), hypoglycemia or a composite including any of these secondary outcomes.
Chi square was performed for statistical analysis using STATA 13 (College Station, Texas, USA). The risk ratios and 95% confidence intervals (CI) were estimated using the non-SGA group as the reference group. Sensitivity, specificity and positive and negative predictive values for the primary and secondary outcomes using Doppler assessments were calculated. The likelihood ratios for a positive (LR+) or negative test (LR-) were also calculated. An LR+ >10 or LR- <0.10 indicates a highly efficient predictive test.The discriminatory ability of each Doppler measurement modality was compared using area under receiver operating characteristic curves (AUC).
Results
Over the study period, 1068 singleton pregnancies were recruited, where 199 women had complete information on CPR and met the inclusion criteria. Demographic information of the current study population is detailed in Table 1. Most of the women in this study were African American (49.4%) or Caucasian (26.1%). The mean BMI was 28.5 kg/m2. Abnormal CPR was noted in 7 (3.5%) of the population. As referenced in Table 1 there were no statistically significant differences in maternal demographic characteristics between the groups with normal CPR and abnormal CPR.
Table 1.
Comparison of maternal demographic and pregnancy characteristics for cases with fetal growth restriction and cerebroplacental ratio (CPR) assessment
| Normal *CPR (n= 192) | Abnormal *CPR (n=7) | p-value | |
|---|---|---|---|
| Mean age, years (±SD) | 27.3 (5.7) | 30.6 (4.2) | 0.08 |
| Nulliparous (%) | 100 (52.1) | 2 (28.6) | 0.22 |
| Ethnicity (%) | 0.48 | ||
| African American | 80 (41.7%) | 4 (57.1%) | |
| Hispanic | 23 (12%) | 2(28.6%) | |
| Asian | 11 (5.7%) | 0 | |
| European /white | 73 (38.0%) | 1 (14.2%) | |
| Multiracial/other | 5 (2.6%) | 0 | |
| Mean BMI, Kg/m2 (±SD) | 29.3 (2) | 27.8 (6.2) | 0.60 |
| Chronic hypertension | 22 (11.5%) | 2 (28.6%) | 0.17 |
| Preeclampsia | 19 (9.9%) | 2 (28.6%) | 0.11 |
| Pre-gestational diabetes | 8 (4.2%) | 0 | 0.58 |
| Smoking (%) | 19 (9.9%) | 1 (14.3%) | 0.70 |
| Gestational age at first growth ultrasound, weeks (±SD) | 31.6 (2.8) | 32.2 (3.1) | 0.64 |
| Gestational age at delivery, weeks (±SD) | 38.0 (1.8) | 34.6 (4.6) | 0.09 |
| Birthweight, grams (±SD) | 2675 (518) | 1890 (971) | 0.07 |
SD= standard deviation; BMI = body mass index
UA Doppler was obtained in 208 women and 17 (8.2%) were abnormal and 191 (91.8%) were normal.
The positive (PPV) and negative (NPV) predictive values using abnormal UA Doppler to predict SGA are 70.6% and 57.1%, respectively. The PPV and NPV using low CPR to predict SGA are 57.1% and 54.4%, respectively. For the prediction of the composite adverse neonatal outcome, the PPV and NPV using UA Doppler are: 41.2% and 88.0%, respectively; and for low CPR are 42.9% and 86.9%, respectively.
Ninety-four (47.2%) had SGA and 68 (34.2%) had a composite adverse neonatal outcome. Abnormal UA Doppler showed a better sensitivity for predicting SGA (12.8%) than CPR (4.4%). The sensitivity for predicting the composite adverse neonatal outcomes using abnormal UA Doppler was also better than using CPR, 17.6% versus 7.7%, respectively (Table 2). The specificity of abnormal UA Doppler for predicting SGA was 95.6%, which is similar to that of a low CPR of 96.5% for predicting the same outcome. The specificity for predicting a composite adverse neonatal outcome was also similar. The likelihood ratio positive (LR+) for using abnormal UA Doppler to predict SGA is 2.9 and the negative LR (LR-) is 0.91. The LR+ and LR- using low CPR to predict SGA are 1.2 and 0.99, respectively. For predicting the composite adverse neonatal outcome, the LR+ and LR- using abnormal UA Doppler are 4.9 and 0.85, respectively; and using low CPR are 3.3 and 0.94, respectively.
Table 2.
Umbilical artery Doppler, low cerebroplacental ratio (CPR) and short term adverse neonatal outcomes
| Abnormal UA doppler* | CPR < 1.08 | |||||||
|---|---|---|---|---|---|---|---|---|
| Sensitivity (%) | Specificity (%) | Relative risk | 95% CI | Sensitivity (%) | Specificity (%) | Relative risk | 95% CI** | |
| SGA (n=94) | 12.8 | 95.6 | 2.9 | 1.1–8.0 | 4.4 | 96.3 | 1.2 | 0.3–4.6 |
| Cord pH < 7.10 (n=5) | 20.0 | 89.8 | 2.0 | 0.3–12.2 | 20 | 96.8 | 6.2 | 0.8–45.8 |
| 5-min APGARS < 7 (n=7) | 28.6 | 92.9 | 4.0 | 1.1–14.5 | 14.3 | 97.3 | 5.4 | 0.7–40.1 |
| NICU admission (n=25) | 28.0 | 95.0 | 5.6 | 2.3–13.8 | 13.0 | 97.7 | 5.6 | 1.3–23.6 |
| RDS (n=6) | 33.3 | 92.9 | 4.7 | 1.4–16.3 | 20 | 96.8 | 6.3 | 0.9–43.3 |
| Hypoglycemia (n=45) | 13.3 | 93.7 | 2.1 | 0.8–5.5 | 4.65 | 96.7 | 1.4 | 0.3–7.0 |
| Composite (n=68) | 17.6 | 96.4 | 4.9 | 1.8–13.5 | 7.7 | 97.7 | 3.4 | 0.8–13.8 |
PI > 95th percentile, absent or reverse UA diastolic flow
95% Confidence Interval
There were 89 (44.7%) women out of 199 with EFW < 10%ile, of whom 3 (3.4%) had abnormal CPR. 10 (11%) with EFW <10% had abnormal UA. There were 3 pregnancies with EFW <10th %ile and abnormal CPR, of which 2(66.7%) had a composite adverse outcome. There were 10 pregnancies with EFW <10th %ile and abnormal UA Doppler, of which 9 (90%) had a composite adverse outcome.
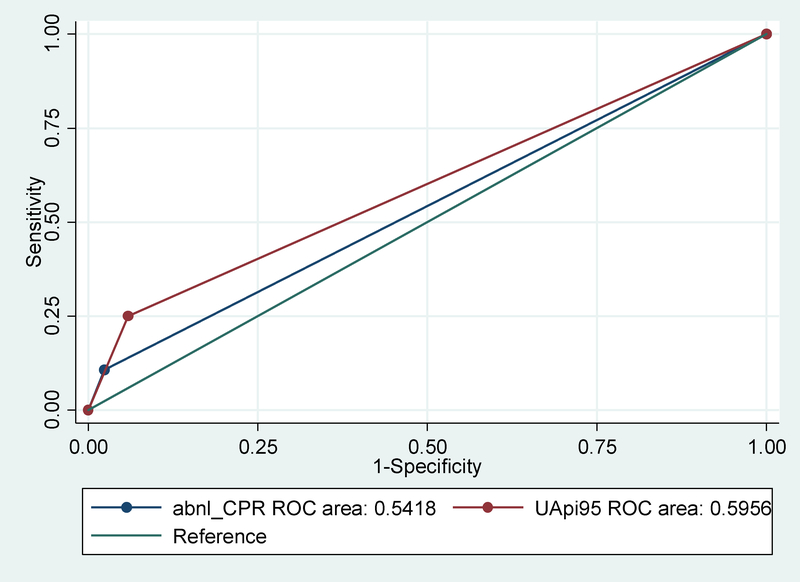
The area under the ROC curve (AUC) using abnormal UA Doppler for predicting SGA was 0.54, 95% CI 0.50–0.58; and 0.51, 95% CI 0.48–0. 53 for low CPR. The AUC for predicting a composite adverse neonatal outcome are: 0.60, 95% CI 0.51–0.68 for abnormal UA Doppler; and 0.54, 95% CI 0.47–0.84 for low CPR. Figures 1 and 2 are examples of the ROC curve comparing abnormal UA Doppler to low CPR for prediction of neonatal SGA and composite adverse neonatal outcomes, respectively.
Fig 1.
ROC curve comparing abnormal UA Doppler to low CPR for predicting neonatal SGA
Fig 2.
ROC curve comparing abnormal UA Doppler to low CPR for predicting neonatal composite adverse neonatal outcomes
Discussion
Our study shows that applying the use of CPR for the prediction of adverse neonatal outcome is not superior to using umbilical artery Doppler alone. Despite the better performance of UA Doppler, the overall screening efficiency was at best modest and was poor for most outcomes evaluated.
Our findings differ from various studies suggesting that the combination of the assessments of UA and MCA Doppler has a superior role in the prediction of adverse perinatal outcomes in the setting of fetal growth restriction when compared to using these Doppler modalities separately. Similarly, other retrospective studies have shown an association between CPR and adverse intrapartum and neonatal adverse outcomes including urgent cesarean deliveries for fetal heart rate abnormalities, low cord pH, lower APGAR scores and admission to the neonatal intensive care unit2–4,7,17–19. Specifically, a recent prospective study shows that the CPR < 10th percentile has the best diagnostic performance for the prediction of low birthweight, emergency cesarean section for intrapartum fetal complications and composite adverse neonatal outcomes when used as a screening test including low risk term pregnancies prior to labor20.
The strengths of this study rely on its prospective design and the use of simple, reproducible and validated ultrasound modalities. The results of the CPR test were not used for clinical management as this was not a standard of care test in both facilities, which strengthens the validity of our findings.
Some of the limitations of our study must be recognized. These include a relatively small cohort and as the prevalence of growth restriction may vary depending on the population, our findings may not be generalizable to some higher risk populations. In addition, the number of patients with abnormal CPR in our cohort was very limited. It is therefore possible that we may be underpowered to find a more positive association. Larger studies are therefore needed to address this subject before adopting the use of CPR routinely. Our findings highlight the findings from a recent meta-analysis by Oros et al, showing considerable methodological heterogeneity in studies reporting reference ranges for Doppler indices of UA, MCA and CPR. They further caution that the resulting references have important implications for clinical practice21. Thus, standardization of this methods is needed in order to improve their role in the management of pregnancies complicated by fetal growth restriction.
In conclusion, this small cohort study did not find the CPR to be superior to using UA Doppler for predicting adverse outcomes in pregnancies complicated by fetal growth restriction. Larger studies with well standardized definitions of abnormal CPR are needed prior to introducing CPR to routine evaluation of these pregnancies.
Footnotes
Declaration of Interest
The authors listed certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
References
- 1.Figueras F, Caradeux J, Crispi F, Eixarch E, Peguero A, Gratacos E. Diagnosis and surveillance of late-onset fetal growth restriction. American journal of obstetrics and gynecology. 2018;218(2s):S790–S802.e791. [DOI] [PubMed] [Google Scholar]
- 2.Morales-Rosello J, Khalil A. Fetal cerebral redistribution: a marker of compromise regardless of fetal size. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2015;46(4):385–388. [DOI] [PubMed] [Google Scholar]
- 3.Morales-Rosello J, Khalil A, Morlando M, Bhide A, Papageorghiou A, Thilaganathan B. Poor neonatal acid-base status in term fetuses with low cerebroplacental ratio. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2015;45(2):156–161. [DOI] [PubMed] [Google Scholar]
- 4.Khalil AA, Morales-Rosello J, Elsaddig M, et al. The association between fetal Doppler and admission to neonatal unit at term. American journal of obstetrics and gynecology. 2015;213(1):57.e51–57.e57. [DOI] [PubMed] [Google Scholar]
- 5.Dunn L, Sherrell H, Kumar S. Review: Systematic review of the utility of the fetal cerebroplacental ratio measured at term for the prediction of adverse perinatal outcome. Placenta. 2017;54:68–75. [DOI] [PubMed] [Google Scholar]
- 6.Chauhan SP, Magann EF. Screening for fetal growth restriction. Clinical obstetrics and gynecology. 2006;49(2):284–294. [DOI] [PubMed] [Google Scholar]
- 7.Khalil A, Morales-Rosello J, Townsend R, et al. Value of third-trimester cerebroplacental ratio and uterine artery Doppler indices as predictors of stillbirth and perinatal loss. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2016;47(1):74–80. [DOI] [PubMed] [Google Scholar]
- 8.Gramellini D, Folli MC, Raboni S, Vadora E, Merialdi A. Cerebral-umbilical Doppler ratio as a predictor of adverse perinatal outcome. Obstetrics and gynecology. 1992;79(3):416–420. [DOI] [PubMed] [Google Scholar]
- 9.DeVore GR. The importance of the cerebroplacental ratio in the evaluation of fetal well-being in SGA and AGA fetuses. American journal of obstetrics and gynecology. 2015;213(1):5–15. [DOI] [PubMed] [Google Scholar]
- 10.Vollgraff Heidweiller-Schreurs CA, De Boer MA, Heymans MW, et al. Prognostic accuracy of cerebroplacental ratio and middle cerebral artery Doppler for adverse perinatal outcome: systematic review and meta-analysis. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2018;51(3):313–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Committee opinion no 611: method for estimating due date. Obstetrics and gynecology. 2014;124(4):863–866. [DOI] [PubMed] [Google Scholar]
- 12.Salomon LJ, Alfirevic Z, Berghella V, et al. Practice guidelines for performance of the routine mid-trimester fetal ultrasound scan. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2011;37(1):116–126. [DOI] [PubMed] [Google Scholar]
- 13.Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK. Estimation of fetal weight with the use of head, body, and femur measurements--a prospective study. American journal of obstetrics and gynecology. 1985;151(3):333–337. [DOI] [PubMed] [Google Scholar]
- 14.Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstetrics and gynecology. 1996;87(2):163–168. [DOI] [PubMed] [Google Scholar]
- 15.Odibo AO, Goetzinger KR, Cahill AG, Odibo L, Macones GA. Combined sonographic testing index and prediction of adverse outcome in preterm fetal growth restriction. American journal of perinatology. 2014;31(2):139–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Odibo AO, Riddick C, Pare E, Stamilio DM, Macones GA. Cerebroplacental Doppler ratio and adverse perinatal outcomes in intrauterine growth restriction: evaluating the impact of using gestational age-specific reference values. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2005;24(9):1223–1228. [DOI] [PubMed] [Google Scholar]
- 17.Khalil AA, Morales-Rosello J, Morlando M, et al. Is fetal cerebroplacental ratio an independent predictor of intrapartum fetal compromise and neonatal unit admission? American journal of obstetrics and gynecology. 2015;213(1):54.e51–54.e10. [DOI] [PubMed] [Google Scholar]
- 18.Morales-Rosello J, Khalil A, Morlando M, Papageorghiou A, Bhide A, Thilaganathan B. Changes in fetal Doppler indices as a marker of failure to reach growth potential at term. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2014;43(3):303–310. [DOI] [PubMed] [Google Scholar]
- 19.Triunfo S, Crispi F, Gratacos E, Figueras F. Prediction of delivery of small-for-gestational-age neonates and adverse perinatal outcome by fetoplacental Doppler at 37 weeks’ gestation. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2017;49(3):364–371. [DOI] [PubMed] [Google Scholar]
- 20.Bligh LN, Al Solai A, Greer RM, Kumar S. Diagnostic Performance of Cerebroplacental Ratio Thresholds at Term for Prediction of Low Birthweight and Adverse Intrapartum and Neonatal Outcomes in a Term, Low-Risk Population. Fetal diagnosis and therapy. 2018;43(3):191–198. [DOI] [PubMed] [Google Scholar]
- 21.Oros D, Ruiz-Martinez S, Staines-Urias E, et al. Reference ranges for Doppler indices of umbilical and fetal middle cerebral arteries and cerebroplacental ratio: systematic review. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2018. [DOI] [PubMed] [Google Scholar]