Abstract
Background:
The burden of substance abuse among patients with heart failure and its association with subsequent emergency department visits and hospital admissions are poorly characterized.
Methods:
We evaluated the medical records of patients with a diagnosis of heart failure treated at the University of California, San Diego from 2005–16. We identified substance abuse via diagnosis codes and/or urine drug screens. We used Poisson regression to evaluate the incidence rate ratios (IRR) of substance abuse for emergency department visits and/or hospitalizations with a primary diagnosis of heart failure, adjusted for age, sex, race, medical insurance status, and medical diagnoses.
Results:
We identified 11,268 patients with heart failure and 15,909 hospital encounters for heart failure over 49,712 person-years of follow-up. Substance abuse was diagnosed in 15.2% of patients. Disorders such as methamphetamine abuse (prevalence 5.2%, IRR 1.96, 95% confidence interval [CI] 1.85–2.07), opioid use/abuse (8.2%, IRR 1.54, 95% CI 1.47–1.61), and alcohol abuse (4.5%, IRR 1.51, 95% CI 1.42–1.60) were associated with a greater number of hospital encounters for heart failure, with associations that were comparable to diagnoses such as atrial fibrillation (37%, IRR 1.78, 95% CI 1.73–1.84), ischemic heart disease (24%, IRR 1.67, 95% CI 1.62–1.73), and chronic kidney disease (26%, IRR 1.57, 95% CI 1.51–1.62).
Conclusions:
Although less prevalent than common medical co-morbidities in patients with heart failure, substance abuse disorders are significant sources of morbidity that are independently associated with emergency department visits and hospitalizations for heart failure. Greater recognition and treatment of substance abuse may improve outcomes among patients with heart failure.
Keywords: Heart failure, Substance abuse, Re-admission
Introduction
Heart failure is a growing epidemic in the United States. The lifetime risk of developing heart failure is approximately 1 in 5; with an aging population, the prevalence of heart failure is projected to increase swiftly over the next few decades.1–3 Hospital encounters for acute decompensated heart failure are associated with high rates of morbidity and mortality, and are a significant burden on healthcare systems worldwide.3 After being hospitalized for heart failure, approximately 1 in 4 patients are readmitted within 30 days of discharge,4 and a history of hospitalization for heart failure is associated with higher cardiovascular mortality.5 Hence, it is imperative to identify and treat patients with heart failure who are at risk for hospitalization in an effort to improve clinical outcomes.
Substance abuse is common and associated with substantial morbidity and mortality in the general population.6,7 Many substances with high addiction potential, such as cocaine, alcohol, and methamphetamine, exert adverse effects on the cardiovascular system and may affect the disease course of patients with heart failure.8–11 Thus, the diagnosis and management of substance abuse is an important consideration in patients with heart failure. However, the prevalence of substance abuse and its association with outcomes in heart failure has not been well described.
In this study, we aimed to better characterize substance abuse among patients with heart failure treated at a single institution between 2005 and 2016. We specifically sought to describe the prevalence of substance abuse and its independent association with hospital encounters and heart failure readmissions.
Methods
Study Sample
The study protocol was approved by the Institutional Review Board of the University of California, San Diego (UCSD). We retrospectively evaluated the electronic health record of the UCSD Healthcare System from January 1, 2005 through June 30, 2016. We abstracted International Classification of Diseases, 9th Revision (ICD-9) diagnosis codes to identify patients with heart failure based on ICD-9 code 428.xx, from both inpatient and outpatient encounters. Patients were excluded if they were less than 18 years of age at the time of identification. We abstracted data on substance abuse among patients with heart failure using ICD-9 codes for substance abuse and dependence along with urine drug toxicology where available. We also abstracted ICD-9 codes for common medical co-morbidities and contributors to heart failure. A full list of ICD-9 codes utilized in this study is included in a supplementary table.
For each patient, the follow up period extended from the time of first diagnosis of heart failure to patient death or June 30th, 2016. We tallied the total number of hospital encounters (emergency department visits and hospital admissions) with a primary diagnosis of heart failure over the study period for each patient. When an emergency department visit was directly followed by a hospital admission, only the hospital admission was counted. In order to assess the association of substance abuse with heart failure readmissions, we identified patients with more than one recorded hospital admission with a primary admission diagnosis of heart failure, and determined the interval between the first and second hospital admissions.
Statistical Analysis
Baseline characteristics of patients with heart failure with evidence of any substance abuse were compared to heart failure patients without evidence of substance abuse. We compared continuous variables using the Student’s t-test or the Mann-Whitney U test, and categorical variables using the chi-square test. We determined the annual incidence of substance abuse diagnoses among patients with heart failure starting in 2006, after excluding patients with heart failure and prevalent substance abuse diagnoses in 2005. In longitudinal analyses, we constructed multivariable models mutually-adjusting for substance abuse and medical diagnoses in addition to age, sex, race/ethnicity, and medical insurance status. We used Poisson regression to evaluate the associations of substance abuse and medical diagnoses with the count of hospital encounters for heart failure, and plotted incidence rate ratios (IRR) with 95% confidence intervals (CI) for each diagnosis. We used Cox proportional hazards regression to evaluate the associations of substance abuse and medical diagnoses with time to first hospital readmission for heart failure and time to all-cause mortality, and plotted hazard ratios and 95% CI for each diagnosis.
We performed statistical analyses using SPSS Statistics version 22.0 (IBM Corporation, Armonk, NY, USA). We considered a p-value of less than 0.05 statistically significant.
Results
From 2005 to 2016, 11,268 unique patients with heart failure were identified. Substance abuse was diagnosed in 15.2% of patients. Characteristics of patients with heart failure stratified by the presence or absence of a diagnosis of any substance abuse disorder are listed in Table 1. Patients with heart failure and substance abuse were younger (55 ±14 vs. 68 ±15 years, p<0.01), more often male (69% vs. 56%. p<0.01), African American (22% v. 9%), and without medical insurance (40% vs. 18%, p<0.01). Diagnoses of ischemic heart disease, cerebrovascular accident, and endocarditis were slightly more common among patients with heart failure and drug abuse, and atrial fibrillation/flutter was less common.
Table 1: Patient characteristics stratified by diagnosis of any substance abuse.
Patients with heart failure treated at the University of California, San Diego between January 1, 2005 and June 30, 2016 were identified via International Classification of Diseases, 9th revision, diagnosis code 428.xx. Substance abuse was determined via urine drug toxicology and/or ICD-9 diagnosis codes. Substances evaluated were opioids, methamphetamines, alcohol, marijuana, cocaine, barbiturates, and phencyclidine. Medical diagnoses were determined via ICD-9 diagnosis codes.
| Patients with Heart Failure | |||
|---|---|---|---|
| Any substance abuse | No substance abuse | p-value | |
| N (% of total) | 1,718 (15.2%) | 9,550 (84.8%) | |
| Age in years (standard deviation) | 55 (14) | 68 (15) | <0.01 |
| Male sex | 69.0% | 55.5% | <0.01 |
| Race/ethnicity | <0.01 | ||
| Caucasian | 56.5% | 56.6% | |
| Hispanic | 15.3% | 18.9% | |
| African American | 21.8% | 8.9% | |
| Asian | 2.9% | 7.6% | |
| Other/mixed | 3.5% | 7.9% | |
| No medical insurance | 40.0% | 17.5% | <0.01 |
| Hypertension | 64.9% | 64.6% | 0.83 |
| Atrial fibrillation/flutter | 29.6% | 38.4% | <0.01 |
| Diabetes mellitus | 28.3% | 27.7% | 0.59 |
| Chronic kidney disease | 24.5% | 26.0% | 0.19 |
| Ischemic heart disease | 29.3% | 23.0% | <0.01 |
| Cerebrovascular accident | 12.9% | 10.3% | <0.01 |
| Endocarditis | 3.7% | 2.5% | <0.01 |
| Median follow up in years (interquartile range) | 3.7 (1.8, 6.9) | 3.6 (1.6, 6.9) | 0.10 |
| Median heart failure emergency department and/or inpatient encounters (interquartile range) | 1 (0, 3) | 1 (0, 1) | <0.01 |
| Mortality Rate | 16.5% | 19.0% | 0.02 |
Table 2 lists the prevalence of substance abuse disorders among all patients with heart failure over the study period. Opioid use/abuse was the most common (8.4%), followed by methamphetamine abuse (5.2%), alcohol abuse (4.5%), and marijuana use/abuse (2.2%). Figure 1 shows the annual incidence of substance abuse among patients with heart failure from 2006 to 2016. The annual incidence of any substance abuse diagnosis varied by year and ranged from 13.0% to 20.2%. Opioid use/abuse declined over the study period (9.6% to 4.1%), while methamphetamine (1.8% to 6.4%) and alcohol abuse (3.3% to 4.4%) rose.
Table 2: Period prevalence of substance abuse disorders among patients with heart failure, 2005 to 2016.
Patients with heart failure were identified at the University of California, San Diego using ICD-9 diagnosis code 428.xx. Substance abuse disorders were identified using ICD-9 diagnosis codes and urine drug toxicology.
| Prevalence | |
|---|---|
| Opioid use/abuse | 8.4% |
| Methamphetamine abuse | 5.2% |
| Alcohol abuse | 4.5% |
| Marijuana use/abuse | 2.2% |
| Cocaine abuse | 0.6% |
| Barbiturate abuse | 0.3% |
| Phencyclidine (PCP) abuse | 0.2% |
Figure 1: Trends in substance abuse among patients with heart failure, 2006–2016.
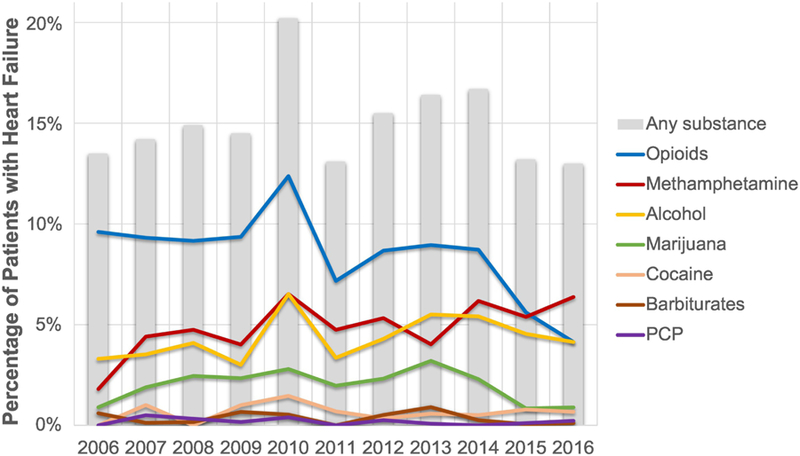
The annual incidence of substance use disorders among patients with heart failure treated at the University of California, San Diego are plotted. Patients with heart failure were identified based on ICD-9 diagnosis code 428.xx. Substance abuse was defined by a urine drug toxicology test positive for the given drug or the presence of the relevant ICD-9 code.
Over a median follow up of 3.6 years (interquartile range [IQR] 1.6–6.9), 15,909 hospital encounters with a primary diagnosis of heart failure occurred. Duration of follow-up for patients with substance abuse (3.7 years, IQR 1.8–6.9) and without substance abuse (3.6 years, IQR 1.6–6.9) did not differ significantly (p=0.10). Figure 2 plots the incidence rate ratios (IRR) and 95% CI from the Poisson regression model evaluating the associations of substance abuse and medical diagnoses with the total number of heart failure hospital encounters over follow up. Red bars indicate substance abuse disorders and blue bars indicate medical diagnoses. Disorders such as methamphetamine abuse (period prevalence 5.2%, IRR 1.96, 95% CI 1.85–2.07), opioid use/abuse (8.2%, 1.54, 1.47–1.61), and alcohol abuse (4.5%, 1.51, 1.42–1.60) were significantly associated with hospital encounters for heart failure, with IRR that were comparable to diagnoses such as atrial fibrillation (37%, 1.78, 1.73–1.84), ischemic heart disease (24%, 1.67, 1.62–1.73), and chronic kidney disease (26%, 1.57, 1.51–1.62).
Figure 2: Risks of hospital encounter for heart failure associated with medical and drug abuse diagnoses.
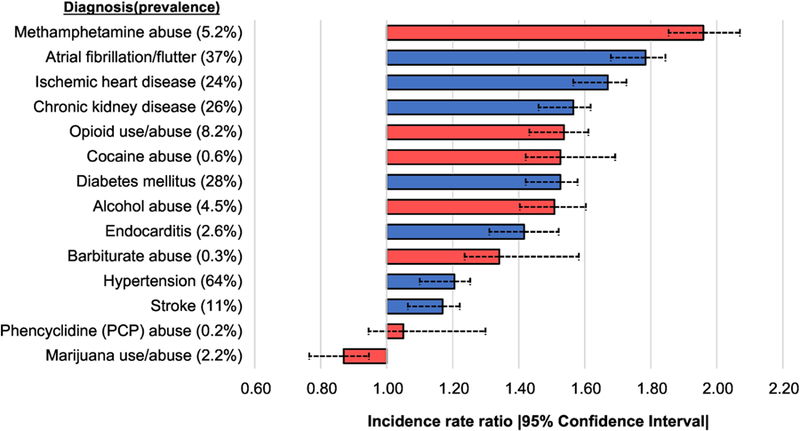
Incidence rate ratios and 95% confidence intervals are plotted. 11,268 patients with a history of heart failure were evaluated in a multivariable Poisson regression model for the number of emergency department visits and/or hospitalizations with a primary encounter diagnosis of heart failure. Over a median follow-up of 3.6 years (interquartile range 1.6 to 6.9 years), 15,909 heart failure hospital encounters occurred. The multivariable model includes mutual adjustment for the variables listed above as well as age, sex, race/ethnicity, and medical insurance status. Red bars indicate substance abuse disorders and blue bars indicate medical diagnoses
Of the patients with heart failure included in this study, 6,283 had a hospital admission with a primary diagnosis of heart failure, and 2,857 of these patients (45%) experienced a readmission with a primary diagnosis of heart failure over a median follow-up of 324 days (IQR 47–947). Figure 3 plots the hazard ratios (HR) and 95% CI from the Cox regression model evaluating the associations of substance abuse and medical diagnoses with time to first heart failure readmission. Methamphetamine abuse had the largest association (period prevalence 7.2%, HR 1.58, 95% CI 1.38–1.82), followed by atrial fibrillation (41%, 1.52, 1.41–1.64), hypertension (66%, 1.34, 1.23–1.47), and other medical diagnoses. Opioid use/abuse was also associated with higher risk (11%, 1.22, 1.08–1.37), while the remaining substance abuse disorders were not significantly associated with heart failure readmission.
Figure 3: Risks of heart failure readmission associated with medical and drug abuse diagnoses.
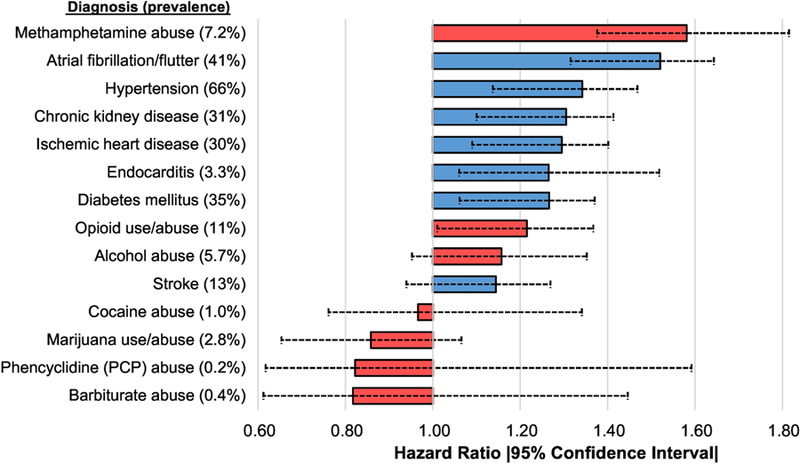
Hazard ratios and 95% confidence intervals are plotted. 6,283 patients with a prior hospital admission with heart failure as the primary admission diagnosis were evaluated in a multivariable Cox regression model for time to first readmission with heart failure as the primary admission diagnosis. Over a median follow-up of 324 days (interquartile range 47 to 947 days), 2,857 heart failure readmissions occurred. Multivariable model includes mutual adjustment for the variables listed above as well age, sex, race/ethnicity, and medical insurance status. Red bars indicate substance abuse disorders and blue bars indicate medical diagnoses
Among the total sample, there were 2,094 deaths over follow-up. Figure 4 plots the hazard ratios and 95% confidence intervals from the Cox regression model evaluating the associations of substance abuse and medical diagnoses with time to all-cause mortality. Medical diagnoses were found to be significantly associated with all-cause mortality; chronic kidney disease with the largest association (HR 1.54, 95% CI 1.40–1.70), followed by endocarditis (1.37, 1.09–1.72) and diabetes mellitus (1.25, 1.14–1.38). Substance abuse disorders were not significantly associated with all-cause mortality.
Figure 4: Risks of all-cause mortality associated with medical and drug abuse diagnoses.
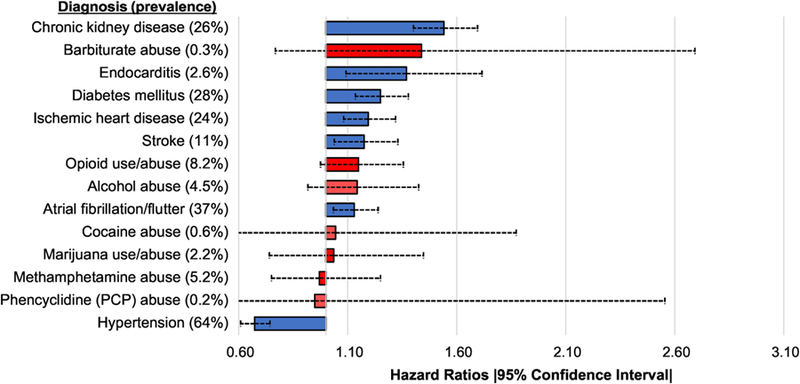
Hazard ratios and 95% confidence intervals are plotted. 11,268 patients with a history of heart failure were evaluated in a multivariable Cox regression model for time to all-cause mortality. Over a median follow-up of 324 days (interquartile range 47 to 947 days), 2,094 deaths occurred. Multivariable model includes mutual adjustment for the variables listed above as well age, sex, race/ethnicity, and medical insurance status.
Discussion
In this analysis of patients with heart failure, we found substance abuse to be independently associated with a greater risk of emergency department visits and hospitalizations for heart failure, as well as hospital readmission for heart failure. Methamphetamine abuse, alcohol abuse, and opioid use/abuse were independently associated with hospital encounters for heart failure, with incidence rate ratios that were comparable to comorbidities such as atrial fibrillation, ischemic heart disease, and chronic kidney disease. Methamphetamine and opioid use/abuse were also independently associated with heart failure readmission. However, unlike medical diagnoses, the substance abuse diagnoses evaluated in this study were not significantly associated with heightened mortality.
Opioids were the most commonly used substance (8.4%) in our study, followed by methamphetamine (5.2%), alcohol (4.5%), marijuana (2.2%), and cocaine (0.6%). We observed a decrease in the annual incidence of opioid use (9.6% to 4.1%) over the study period, paralleling the recent reduction of opioid use/abuse observed in the general population.12 Methamphetamine abuse, on the other hand, demonstrated a 4-fold increase between 2006 and 2016 (1.8% to 6.4%). In another study also conducted in San Diego, Sliman et al. reported an increase in the prevalence of methamphetamine associated heart failure from 1.8 to 5.6% between 2009 and 2014.13 Methamphetamine abuse has grown increasingly common worldwide, and is a known cardiotoxin, implicated in the development of a severe form of dilated cardiomyopathy.6,14 Importantly, we found that methamphetamine abuse is independently associated with heart failure hospital encounters and readmissions among patients with heart failure, with a magnitude of association that was as high or higher than any other medical and substance abuse comorbidity evaluated.
We found important demographic and clinical differences between patients with heart failure with and without a history of substance abuse. Patients with heart failure who had a history of substance abuse were younger, more likely to be male, to be African American, and to lack medical insurance. Despite being younger on average, patients with heart failure with substance abuse had similar or greater rates of comorbidities. Rates of hypertension, diabetes, and chronic kidney disease were similar between the two groups, whereas higher proportions of ischemic heart disease, cerebrovascular accidents, and endocarditis were observed in patients with substance abuse. Atrial fibrillation was the only comorbid condition examined which was more common in patients with heart failure without substance abuse. The differences in comorbidities between the groups are likely due to several factors, including socioeconomic barriers to care such as a lack of medical insurance. Moreover, many abused substances are known to exert toxic effects. For example, cocaine has been shown to cause a wide range of adverse cardiovascular effects including hypertension, myocardial ischemia, arrhythmia, aortic dissection, and stroke.8,10 Alcohol has been associated with hypertension, atrial fibrillation, and development of alcoholic cardiomyopathy.10 Cardiovascular complications of methamphetamine use are also increasingly recognized, including methamphetamine associated heart failure and pulmonary hypertension.9,15 These factors make patients with concomitant heart failure and substance abuse a particularly vulnerable patient population.
Despite the strong association between substance abuse and hospital encounters and readmissions for heart failure, we did not find a similar association between substance abuse and mortality. It is likely that given relative youth of the patients with substance abuse, the baseline level of risk for mortality was lower among patients with substance abuse compared to without. Furthermore, although substance abuse can have multiple deleterious health effects, some may be dose dependent and even reversible with cessation of abuse14.
Our study has several notable strengths. We examined a large population of patients with heart failure over an extended study period. Previous studies have demonstrated the association of comorbidities and demographic factors with hospital encounters and readmission.16–18 Our study demonstrates that substance use is independently associated with future hospital encounters for heart failure at rates comparable to established medical comorbidities. These findings suggest the importance of consideration of substance abuse, especially methamphetamine use, in identifying high-risk patients with heart failure.
Our study also has several limitations. It had an observational design and was conducted using data from a single health care system. As with any observational study, we cannot exclude the possibility that residual confounding explains our results despite adjusting for several demographic and medical factors. Moreover, findings in our patient population may not be generalizable to all patients with heart failure. We relied on diagnosis codes for substance abuse during routine clinical care for inclusion in our study. As substance abuse may frequently go unrecognized among medical practitioners and underreported by patients, we likely underestimated the true frequency of substance abuse among these patients.
In conclusion, our study demonstrates that patients with heart failure often have concomitant substance abuse. Several substance abuse disorders are independently associated with heart failure related hospital encounters, to a degree comparable with traditional heart failure risk factors. Evaluation of substance abuse history, particularly methamphetamine abuse, opioid use/abuse, and alcohol abuse, may identify patients at a greater risk for heart failure morbidity. Greater recognition and treatment of substance abuse disorders may lead to improved outcomes among heart failure patients.
Supplementary Material
Clinical significance.
Substance abuse is common among patients with heart failure.
Methamphetamine abuse, alcohol abuse, and opioid use/abuse were independently associated with hospital encounters for heart failure, with risks that were comparable to comorbidities such as atrial fibrillation and ischemic heart disease.
Methamphetamine and opioid use/abuse were independently associated with heart failure readmission.
Acknowledgments
Source of Funding: The Project described was partially supported by the National Institutes of Health, Grant UL1TR001442 of CTSA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Disclosures: All of the authors report no conflicts of interest related to this manuscript. All authors had had access to the data and a role in writing the manuscript
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Pina IL, Trogdon JG. Forecasting the Impact of Heart Failure in the United States : A Poly Statement from the American Heart Association. Circ Heart Fail 2014;6:606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huffman MD, Berry JD, Ning H, Dyer AR, Garside DB, Cai X, Daviglus ML, Lloyd-Jones DM. Lifetime Risk for Heart Failure Among White and Black Americans: Cardiovascular Lifetime Risk Pooling Project. J Am Coll Cardiol 2013;61:1510–1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, Ferranti SD de, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, et al. Heart Disease and Stroke Statistics—2018 Update: A Report From the American Heart Association. Circulation 2018;137:e67–e492. Available at: https://www.ahajournals.org/doi/10.1161/CIR.0000000000000558. Accessed October 25, 2018. [DOI] [PubMed] [Google Scholar]
- 4.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. N Engl J Med 2009;360:1418–1428. Available at: http://www.nejm.org/doi/abs/10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 5.Bello NA, Claggett B, Desai AS, McMurray JJV, Granger CB, Yusuf S, Swedberg K, Pfeffer MA, Solomon SD. Influence of previous heart failure hospitalization on cardiovascular events in patients with reduced and preserved ejection fraction. Circ Heart Fail 2014;7:590–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UNODC. World drug report 2017: Global overview of drug demand and supply; 2017. Available at: https://www.unodc.org/wdr2017/field/Booklet_2_HEALTH.pdf. Accessed 10 December 2017.
- 7.Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, Abdulkader RS, Abdulle AM, Abebo TA, Abera SF, Aboyans V, Abu-Raddad LJ, Ackerman IN, Adedeji IA, Adetokunboh O, Afshin A, Aggarwal R, Agrawal S, Agrawal A, Ahmed MB, Aichour MTE, Aichour AN, Aichour I, Aiyar S, Akinyemiju TF, Akseer N, Lami FH Al, Alahdab F, Al-Aly Z, Alam K, Alam N, Alam T, Alasfoor D, Alene KA, Ali R, Alizadeh-Navaei R, Alkaabi JM, Alkerwi A, Alla F, Allebeck P, Allen C, Al-Maskari F, AlMazroa MAA, Al-Raddadi R, Alsharif U, Alsowaidi S, Althouse BM, Altirkawi KA, Alvis-Guzman N, Amare AT, Amini E, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet 2017;390:1260–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Havakuk O, Rezkalla SH, Kloner RA. The Cardiovascular Effects of Cocaine. J Am Coll Cardiol 2017;70:101–113. [DOI] [PubMed] [Google Scholar]
- 9.Paratz ED, Cunningham NJ, MacIsaac AI. The Cardiac Complications of Methamphetamines. Heart Lung Circ 2016;25:325–332. Available at: 10.1016/j.hlc.2015.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Mladěnka P, Applová L, Patočka J, Costa VM, Remiao F, Pourová J, Mladěnka A, Karlíčková J, Jahodář L, Vopršalová M, Varner KJ, Štěrba M. Comprehensive review of cardiovascular toxicity of drugs and related agents. Med Res Rev 2018;38:1332–1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mirijello A, Tarli C, Vassallo GA, Sestito L, Antonelli M, D’Angelo C, Ferrulli A, Cosmo S De, Gasbarrini A, Addolorato G. Alcoholic cardiomyopathy: What is known and what is not known. Eur J Intern Med 2017;43:1–5. Available at: 10.1016/j.ejim.2017.06.014. [DOI] [PubMed] [Google Scholar]
- 12.Korff M von, Dublin S, Walker RL, Parchman M, Shortreed SM, Hansen RN, Saunders K. The impact of opioid risk reduction initiatives on high-dose opioid prescribing for chronic opioid therapy patients. J Pain 2016;17:101–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sliman S, Waalen J, Shaw D. Methamphetamine-Associated Congestive Heart Failure: Increasing Prevalence and Relationship of Clinical Outcomes to Continued Use or Abstinence. Cardiovasc Toxicol 2016;16:381–389. Available at: http://link.springer.com/10.1007/s12012-015-9350-y. [DOI] [PubMed] [Google Scholar]
- 14.Schürer S, Klingel K, Sandri M, Majunke N, Besler C, Kandolf R, Lurz P, Luck M, Hertel P, Schuler G, Linke A, Mangner N. Clinical Characteristics, Histopathological Features, and Clinical Outcome of Methamphetamine-Associated Cardiomyopathy. J Am Coll Cardiol HF 2017;5:435–445. Available at: http://linkinghub.elsevier.com/retrieve/pii/S2213177917301658. [DOI] [PubMed] [Google Scholar]
- 15.Won S, Hong RA, Shohet RV, Seto TB, Parikh NI. Methamphetamine-associated cardiomyopathy. Circ Cardiol 2013;36:737–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mirkin KA, Enomoto LM, Caputo GM, Hollenbeak CS. Risk factors for 30-day readmission in patients with congestive heart failure. Heart Lung 2017;46:357–362. Available at: 10.1016/j.hrtlng.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 17.Vader JM, LaRue SJ, Stevens SR, Mentz RJ, DeVore AD, Lala A, Groarke JD, AbouEzzeddine OF, Dunlay SM, Grodin JL, Davila-Roman VG, las Fuentes L de. Timing and Causes of Readmission After Acute Heart Failure Hospitalization-Insights from the Heart Failure Network Trials. J Card Fail 2016;22:875–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krumholz HM, Parent EM, Tu N, Vaccarino V, Wang Y, Radford MJ, Hennen J. Readmission After Hospitalization for Congestive Heart Failure Among Medicare Beneficiaries. Arch Intern Med 1997;157:99–104. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


