Abstract
The current study examined the moderating role of friendship quality on the relation between maternal anxiety and internalizing symptoms in a 3-year prospective study of adolescent development. Participants included 177 adolescents (Mage = 16.05, SDage = 0.91) and their mothers. Mothers reported their own levels of anxiety; youth completed self-reports of internalizing symptoms and friendship quality. Positive friendship quality moderated the relation between maternal anxiety and initial levels of internalizing symptoms. Maternal anxiety was associated with steeper increases in internalizing symptoms over time, but only for those with greater negative peer interactions. Findings underscore the important role of both parental and peer relationships in the development of internalizing symptoms and highlight specific avenues for clinical interventions.
Keywords: Internalizing symptoms, Maternal anxiety, Friendship Quality, Adolescence
Adolescence is a period of transition during which individuals undergo substantial physical, psychological and social changes (Negriff & Susman, 2011). One such significant change is the increase in the importance and influence of peer relationships. Past research indicates that the relative importance of parental influence decreases during this period, and adolescents become more strongly influenced by their peers (Beal, Ausiello, & Perrin, 2001; Brown, 2004; Collins & Laursen, 2004; Sumter, Bokhorst, Steinberg, & Westenberg, 2009).
Alongside these changes in relationships are concomitant increases in psychopathology, especially internalizing disorders. Anxiety and depressive disorders are the most prevalent disorders among adolescents (Costello, Egger, & Angold, 2005). Indeed, recent research suggests that 25.1% and 12.5% of youth between the ages of 12 and 18, experience an anxiety disorder and a major depressive episode, respectively (Center for Behavioral Health Statistics and Quality, 2016; Merikangas et al., 2010). This, in turn, negatively affects academic, interpersonal and emotional domains (Piacentini, Peris, Bergman, Chang, & Jaffer, 2007). Findings from longitudinal studies suggest that the prevalence of internalizing disorders is relatively low during childhood, but that it rises significantly during adolescence (Nivard et al., 2017; Roza, Hofstra, van der Ende, & Verhulst, 2003). Moreover, experiencing these disorders during adolescence increases the risk of reoccurrence in adulthood (Epkins & Heckler, 2011; Kessler et al., 2005). Thus, identifying risk factors as well as protective factors associated with the development and maintenance of internalizing disorders is critical. Parental psychopathology has been established as an important predictor of a wide range of negative outcomes in children (Dowling et al., 2016; van der Pol et al., 2016), including offspring depressive and anxiety symptoms (Burstein, Ginsburg, & Tein, 2010; Gluschkoff et al, 2017). The current study aims to examine the impact of maternal anxiety as a potential risk factor, and the protective role of friendships in predicting internalizing symptoms during this important period of adolescence.
Parental Anxiety and Internalizing Symptoms
The effects of parental anxiety have been extensively researched (Asselmann, Wittchen, Leib, & Beesdo-Baum, 2016; Biederman et al., 2006; Francis & Chorpita, 2011). Several studies have found that parental anxiety increases the risk of internalizing disorders in children (Beesdo, Pine, Lieb, & Wittchen, 2010; Merikangas, Lieb, Wittchen, & Avenevoli, 2003; 2009); children of parents with anxiety disorders were at 3.5 (range 1.3–13.3) times greater risk Micco et al., for anxiety disorders than children of parents without anxiety disorders (Merikangas, Avenevoli, Dierker, & Grillon, 1999).
There have been relatively fewer studies examining the effects of parental anxiety during the critical period of adolescence. Moreover, findings in this area have also been decidedly mixed. For example, with regard to child’s gender, a study by Burstein, Ginsburg, Petras, and Ialongo (2009) on adolescents in grades s 6 through 12 found that parental anxiety disorders uniquely predicted the rate of ge in depression symptoms, but only among male adolescents; on the other hand, no gender differences with relation to effects of parental psychopathology on child psychopathology were found in other studies (e.g. Bouma, Ormel, Verhulst, & Oldehinkel, 2008; Hirshfeld-Becker et al., 2012). With regard to culture, in a study by Essau et al. (2013) examinin g the relation between parental and adolescent psychopathology in two countries, the authors found a significant correlation only among the participants in England, and not in Japan. Moreover, studies have reported conflicting findings in relation to the presence of depressive symptoms in children of parents with anxiety disorders. While some studies reported elevated levels of depressive symptoms among offspring of anxious parents (Beidel & Turner, 1997; Sylvester, Hyde, & Reichler, 1987), others did not (Merikangas, Dierker, & Szatmari, 1998; Warner, Mufson, & Weissman, 1995).
These inconsistencies in the literature may be due to a number of factors. First, many studies were cross-sectional in nature, making it impossible to examine causal links between variables (e.g. Challacombe & Salkovskis, 2009; Essau et al., 2013). Second, several of these studies utilized parental reports of child psychopathology or adolescent reports of parental psychopathology (e.g. Biederman et al., 2001; Rasing, Creemers, Janssens, & Scholte, 2015), thus giving rise to the possibility of biased reporting. Indeed, studies across different cultures have demonstrated that parents may not be reliable informants of their adolescent children’s emotional and behavioral problems, including internalizing symptoms (De Los Reyes & Kazdin, 2005; Tillery, Disabatino, Parra, Buckholdt, & Jobe-Shields, 2014). Third, several of these studies utilized small sample sizes (e.g. Biederman et al., 2006) or samples that only included one sex or race/ethnicity (e.g. Burstein et al., 2009; Rasing et al., 2015). Fourth, most studies have not considered the specific effects of m aternal anxiety (above and beyond general maternal distress or emotion regulation) on the development of adolescent internalizing symptoms. Given that studies have found strong associations between maternal anxiety and maternal emotion dysregulation, which in turn have been linked to higher levels of anxiety and negative affect in the child (Edwards et al., 2017; Kerns, Pincus, McLaughin, & Comer; 2017), examining the specificity of maternal anxiety (as opposed to general emotion dysregulation) is critical for better understanding these relations. Finally, inconsistent results may reflect the presence of important moderators of the relation between maternal anxiety and youth internalizing symptoms. Indeed, very few studies considered potential buffers of the effect of maternal anxiety on youth psychopathology, specifically those which may come online across adolescence.
Friendship quality and Internalizing Symptoms
One such potential moderator of the relation between maternal anxiety and adolescent symptomology is peer social support (Parker, Rubin, Erath, Wojslawowicz, & Buskirk, 2006). Research indicates that support from peers, friends and classmates reduces adolescents’ vulnerability to depression and anxiety (La Greca, & Harrison, 2005; Newman, Newman, Griffen, O’Connor, & Spas, 2007). Moreover, positive friendship quality, a specific facet of social support including peer intimacy, care and support, has been negatively associated with maladaptive behaviors, and internalizing problems (Berndt, 1996).
The buffering effects of positive friendship on the relation between stress and internalizing symptoms, however, is less clear. Findings from several studies indicate that social support protects adolescents from the negative effects of unhealthy family environments, one’s own chronic illness, dating violence and natural disasters (Herzer, Umfress, Aljadeff, Ghai, & Zakowski, 2009; Holt & Espelage, 2005; Kliewer, Murrelle, Mejia, Torres de, & Angold, 2001; Paul et al., 2015). Similar findings have emerged from studies conducted on adults; social support moderated the effects of stressful work environments, child abuse or neglect, and sexual abuse on mental health symptoms (Evans, Steel, & DiLillo, 2013; Murthi & Espelage, 2005, Woodhead, Northrop, & Edelstein, 2016). However, a recent meta-analytic review that included adolescents (Rueger, Malecki, Pyun, Aycock, & Coyle, 2016) did not find that social support significantly moderated the relation between stress and psychopathology. Conversely, findings from studies investigating the relation between internalizing symptoms and negative friendship quality suggest a positive relation, such that negative friendship quality may lead to worse mental health outcomes. For instance, a recent study examining the impact of a large flood on posttraumatic stress symptoms (PTSS) found that youth who reported greater levels of negative friendship quality (defined as conflict, antagonism and criticism) experienced significantly steeper increases of PTSS after the disaster, even after controlling for level of disaster exposure and other child and environmental characteristics (Martin, Felton & Cole, 2016). Other studies found that negative interactions in best friendships (including conflict, criticism, exclusion, dominance, and pressure), poor friendship quality, and peer rejection predicted internalizing symptoms (Festa & Ginsberg, 2011; La Greca & Harrison, 2005; Su, Pettit, & Erath, 2016). Moreover, negative friendship quality (i.e. antagonism and conflict) also predicts loneliness, low self-esteem and internalizing problems (Nangle, Erdley, Newman, Mason, & Carpenter, 2003; Rubin et al., 2004). As opposed to positive friendship quality, no study, to our knowledge, has examined whether negative friendship quality exacerbates the impact of specific risk factors for the development of internalizing symptoms.
Current Study
Given the limited research on maternal anxiety and adolescent internalizing problems, and the disparities in findings highlighted in the sections above, there is a need to examine the role of maternal anxiety specifically during adolescence. Moreover, no studies to the best of our knowledge have investigated the moderating role of both positive and negative friendship quality on maternal anxiety in relation to internalizing symptoms during adolescence. Thus, the current study aims to add to the understanding of the subject area by examining the role of maternal anxiety as a predictor of adolescent internalizing symptoms and the impact of both positive and negative friendship quality on these relations over time. Specifically, we will evaluate whether positive friendship quality buffers the relation between maternal anxiety and adolescent internalizing symptoms while negative friendship quality exacerbates these associations in a three-year prospective study of youth. We will also examine the role of maternal anxiety above and beyond general maternal emotion dysregulation. We hypothesize that:
negative friendship quality and maternal anxiety (at baseline), controlling for broader difficulties with emotion regulation, will predict increases in adolescent internalizing symptomatology over time, while positive friendship quality will predict decreases in internalizing symptoms over time
positive friendship quality will buffer the effects of maternal anxiety on changes in internalizing symptoms, while negative friendship quality will exacerbate the effects of maternal anxiety on adolescent internalizing.
Method
Participants and Procedures
Participants were recruited from a metropoli an area as part of a larger, 10-year longitudinal study investigating the predictors of risk-taking behavior in adolescents. Flyers about the study were put up at schools, libraries, community centers and Boys and Girls clubs, and information about the study was posted on social media. Interested families were screened for inclusion based on having a child between the ages of 9 and 13 (Mage = 11.01, SDage = 0.82), their ability to participate in annual assessments, and their English proficiency. Participating youth and their parents were asked to come into the lab annually to complete a series of self-report questionnaires. Because key measures were not included until the later years of the project, data presented here is from year 6 through 8 (re-labeled waves 1 – 3 for clarity).
Of the original sample of 277 youth, a total of 177, 153 and 153 adolescents participated in waves 6, 7, and 8 (respectively). Youth who engaged in these waves did not differ from adolescents who dropped out of the study on age, race/ethnicity, sex or internalizing scores (p > .050). The final sample used in the current analyses was composed of 58% boys and ranged in age from 14 to 18 years old (Mage = 16.05, SDage = 0.91). Mothers of participants ranged in age from 34 to 68 (Mage = 51.33, SDage = 12.24). The sample was diverse and representative of the geographic area it was recruited from, with 53.6% White, 41.6% Black, .6% Native American or Alaska Native, .6% “other race” and 3.6% multiple race/ethnicities.
Measures
Maternal anxiety.
In order to measure the mothers’ anxiety symptoms, we used the state anxiety subscale of the State-Trait Anxiety Inventory (STAI-S; Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983), which is a 20-item self-report measure of anxiety. The tool was completed by mothers at wave 1. Given that research suggests that the STAI trait (STAI-T) scale has been more strongly correlated with depression rather than anxiety (e.g. Bados, Gomez-Benito, & Balaguer, 2010; Bieling, Antony, & Swinson, 1998), and that the STAI-S mean scores may be a better predictor of current and future anxiety disorders compared to the STAI-T mean scores (Hishinuma et al., 2001), we chose to use the STAI-S in our study. Sample items on the STAI-S scale include, “I am tense”, “I am worried”, “I feel secure.” Mothers were asked to rate their anxiety on a 4-point rating scale, ranging from (1) “not at all” to (4) “very much so.” The STAI is a psychometrically sound tool with internal consistency coefficients ranging from .86 to .95, and test-retest reliability coefficients ranging from .65 to .75 over a two-month interval. In the current study, the measure demonstrated good internal consistency with coefficient alpha = 0.94.
Maternal emotional dysregulation.
The Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) was used to measure mothers’ emotion dysregulation. Mothers were administered the questionnaire at wave 1. The tool consists of 36 items. Sample items include, “I am clear about my feelings”, “When I am upset, I become out of control”, and “When I am upset, I feel like I am weak.” Items are answered on a 5-point rating scale based on how frequently an item applied to their current emotion regulation skills, ranging from (1) “almost never” to (5) “almost always.” The total score was computed by adding each item; higher scores are indicative of greater emotion regulation difficulties. The tool has demonstrated good psychometric qualities including construct validity and internal consistency (Gratz & Roemer, 2004), and is a good predictor of depression (Weinberg & Klonsky, 2009), and anxiety disorders (Roemer et al., 2009; Tull, Stipelman, Salters-Pedneault, & Gratz, 2009) The The internal consistency of the measure in our study was 0.93.
Internalizing symptoms.
The Revised Children’s Anxiety and Depression Scale (RCADS; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000) is a youth self-report measure of internalizing symptoms. It consists of 47 items, and participants were asked to rate how often each item applies to them on a 4-point rating scale from (0) “never” to (3) “always.” Sample items include: “I have problems with my appetite”, “I feel restless.” Adolescents were administered the tool at each wave. The measure yields a total score on internalizing symptoms, and a score for the following scales: generalized anxiety disorder, panic disorder, social anxiety disorder, separation anxiety disorder, obsessive compulsive disorder and major depressive disorder. For the current study, only the total internalizing symptoms score was used. The total score was computed by summing each item, with higher scores indicating higher levels of internalizing symptoms. The RCADS has demonstrated good factor structure, reliability, and validity in school-based and clinical samples (Chorpita et al., 2000; Chorpita, Moffitt, & Gray, 2005). The measure demonstrated excellent internal reliability, with coefficient alphas of .95 at each wave.
Friendship quality.
In order to assess friendship quality, we used the Network of Relationships Inventory (NRI; Furman & Buhrmester, 1985), which consists of 33 questions. In its original format, the tool measures the quality of relationship and social support from key individuals in one’s life like mother, father, sibling, relative, boy/girlfriend, same-sex friend, other sex friend and extra person. However, since we were interested in capturing the effects of their relationship with their best friend only, for the purposes of our study, we asked adolescents to answer the questions keeping only their best friend in mind. The tool was administered at wave 1. The measure yields a positive friendship quality construct composed of seven subscales (reliable alliance, reassurance of worth, instrumental aid, companionship, affection, intimate disclosure, and nurturance) and a negative friendship quality construct composed of two subscales (conflict and antagonism). Participants were asked to rate the items on a 5-point Likert scale, ranging from (1) “little or none” to (5) “the most.” Sample items include: “How often do you spend fun time with this person?”, “How often do you and this person disagree and quarrel with each other?” Items within each subscale are summed to create a total score for positive and negative friendship quality. The measure has demonstrated good internal consistency, with a Cronbach’s Alpha of .80 (Furman & Buhrmester, 1985). For the current sample, the questionnaire demonstrated good internal consistency, coefficient alpha = .95 and .91 for the positive and negative friendship qualities respectively.
Data Analytic Plan
In order to examine the relations between maternal anxiety, friendship quality, and internalizing symptoms we utilized a latent growth modeling (LGM) approach. LGM is a specific case of structural equation modeling that estimates trajectories of internalizing symptoms over the three years included in the study. All analyses were conducted using Mplus 6 (Muthén & Muthén, 2010) with full information maximum likelihood estimation, which is both robust to violations of normality among variables and provides less bias estimates than other missing data approaches (such as listwise or pairwise deletion).
Growth modeling approaches allow for the determination of latent intercept (baseline) and slope (change over time) factors. These models are estimated by fixing the regression weight from each manifest variable (in this case, internalizing symptoms at Waves 1 through 3) to be 1.0. In order to estimate linear change over time, we constrained the regression weights of each manifest variable to be 0.0, 1.0, and 2.0, respectively. Next, we constrained the error variances to be the same across each wave. If this more parsimonious model continues to fit the data, then the constraint is included in each subsequent model. Intercept and slope factors were allowed to correlate. Several fit indices were used to evaluate the fit of the model to the data, including the χ2 statistic, the Comparative Fit Index (CFI; Bentler, 1990), the Tucker-Lewis Index (TLI, Tucker & Lewis, 1973) and the Root Mean Square Error of Approximation (RMSEA; Steiger, 1990). Good fit was indicated by CFI and TLI values ≥ .90, RMSEA values ≤ .08, and nonsignificant chi-square values (Schweizer, 2010). Because χ2 values are sensitive to sample size, the CFI, TLI, and RMSEA were used as primary measures of model fit.
Once we determined the best fitting and most parsimonious model, we examined the means and variances of the latent intercept and slope factors. Statistically significant estimates of the mean of the intercept and slope indicate that the baseline value and change over time differs from zero. Significant estimates of the variances indicate individual differences around these estimates, supporting the inclusion of predictors in the model.
Utilizing a model building approach, we first examined an unconditional latent growth model. We then added maternal anxiety, positive and negative friendship quality as a predictor of the intercept and slope of internalizing symptoms. In order to examine the effects of maternal anxiety specifically (above and beyond maternal emotional dysregulation broadly), we controlled for maternal emotion regulation. Given noted effects of child sex on internalizing symptom trajectories (Angold, Costello, & Worthman, 1998; Wichstrom, 1999), we also included sex as covariates. Finally, we examined the interaction between maternal anxiety and both positive and negative friendship interactions (controlling for sex and maternal emotion dysregulation) in a single model.
Results
Preliminary Analyses
We examined the data to assess missing data patterns in two ways. First, we conducted a Little’s MCAR analyses, which suggested that the data were missing completely at random, χ2 (61) = 53.57, p = .739. Second, we examined correlations between missingness and values of key study variables and found that participants who were missing on any wave of data did not differ significantly from participants who completed that wave (ps > .05).
Next, we examined skew and kurtosis statistics for all dependent variables. All distributions appeared to be within the normal range (≤ 3.0). Means, standard deviations, and correlations between key study variables are included in Table 1. Of note, being female was significantly associated with reporting more positive friendship interactions and evidencing greater levels of internalizing symptoms at every wave. Curiously, higher levels of positive friendship interactions were associated with internalizing symptoms at baseline only, while maternal state anxiety was correlated with children’s internalizing symptoms at every wave.
Table 1.
Summary of Intercorrelations, Means and Standard Deviations on key study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
|---|---|---|---|---|---|---|---|---|---|
| 1. | RCADS Wave 1 | - | |||||||
| 2. | RCADS Wave 2 | .73** | - | ||||||
| 3. | RCADS Wave 3 | .61** | 74** | - | |||||
| 4. | STAI Wave 1 | .18* | .30** | .19* | - | ||||
| 5. | DERS Wave 1 | .17* | .10 | .17 | 41** | - | |||
| 6. | NRI Negative Wave 1 | .05 | .12 | .16 | −.11 | .07 | - | ||
| 7. | NRI Positive Wave 1 | .21** | .17 | .10 | .08 | −.04 | .15 | - | |
| 8. | Sex (male) | −.26** | −.18* | − 21** | −.12 | −.02 | .09 | − 35** | - |
| M | 23.65 | 24.19 | 25.18 | 28.22 | 60.49 | 10.18 | 73.86 | .56 | |
| SD | 15.30 | 15.76 | 17.25 | 9.23 | 16.59 | 4.38 | 15.90 | .50 |
Note. RCADS = Revised Children’s Anxiety and Depression Scale: Total Score; STAI = Mother-Reported State Trait Anxiety Inventory; DERS = Difficulties in Emotion Regulation Scale; NRI Negative = Network of RelationshipsI Inventory, Negative Friendship Quality Subscale Score; NRI Positive = Network of Relationships Inventory: Positive Friendship Quality Subscale Score.
p < .05,
p < .01.
Latent Growth Models: Unconditional Growth Model
Next, we examined a univariate latent growth curve modeling changes in internalizing symptoms over time. The linear growth model fit the data well; χ2 (df=1) = 0.03,p = 0.860; CFI = 1.00; TLI = 1.00; RMSEA = 0.00 (90%CI = 0.00 – 0.10). We then constrained the residuals to be homoscedastic. This resulted in a more parsimonious model that continued to fit well: χ2 (df=3) = 0.74, p = 0.863; CFI = 1.00; TLI = 1.00; RMSEA = 0.00 (90%CI = 0.00 – 0.06); thus, these constraints were retained throughout subsequent analyses. The mean of the intercept (M = 23.88, SE = 1.09, p < .001) was significant, suggesting that youth start with non-zero levels of internalizing, while the slope (M = 0.36, SE = 0.59, p = .547) was not, indicating that rates of internalizing symptoms stay, on average, consistent over time. Further, the variances of the intercept (Var. = 175.63, SE = 24.74,p < .001) and the slope (Var. = 23.46, SE = 7.47,p = .002) were both significant, supporting the utility of adding predictors to the model. The correlation between the intercept and slope, however, was not significant (r = −0.18, p = .183).
Conditional Model 1: Main Effects of Maternal Anxiety and Friendship Quality
Our first hypothesis predicted that state maternal anxiety and both positive and negative friendship quality would be associated with children’s internalizing symptoms at baseline and over time. In order to test this hypothesis, we examined a conditional growth curve model of internalizing symptoms in which we regressed the intercept and slope onto maternal anxiety and friendship quality controlling for youth sex and maternal emotion dysregulation. The model continued to fit the data well: χ2 (df=8) = 11.09, p =.196, CFI = 0.99, TLI = 0.97, RMSEA = 0.05 (90%CI = 0.00 – 0.12). Sex (std. est. = −0.21 p = .016), maternal emotion dysregulation (std. est. = 0.32 p = .002) and positive friendship interactions (std. est. = 0.32 p = .024) each predicted baseline internalizing symptoms. These results indicate that girls and children with mothers who evidenced greater emotion dysregulation reported higher baseline levels of internalizing symptoms. Unexpectedly, positive friendship quality was associated with greater initial levels of internalizing symptoms.
Consistent with our hypotheses, maternal anxiety (std. est. = .31, p = .026) and negative friendship quality (std. est. = .22, p = .049) predicted changes in internalizing symptoms over time. Specifically, children with more anxious mothers and those reporting more negative friendship quality experienced greater increases in internalizing symptoms over time.
Conditional Model 2: Interactive Effects of Maternal Anxiety and Friendship Quality
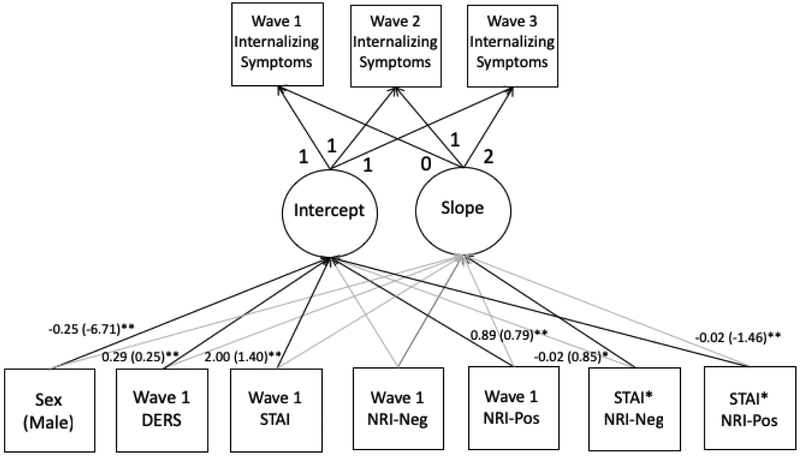
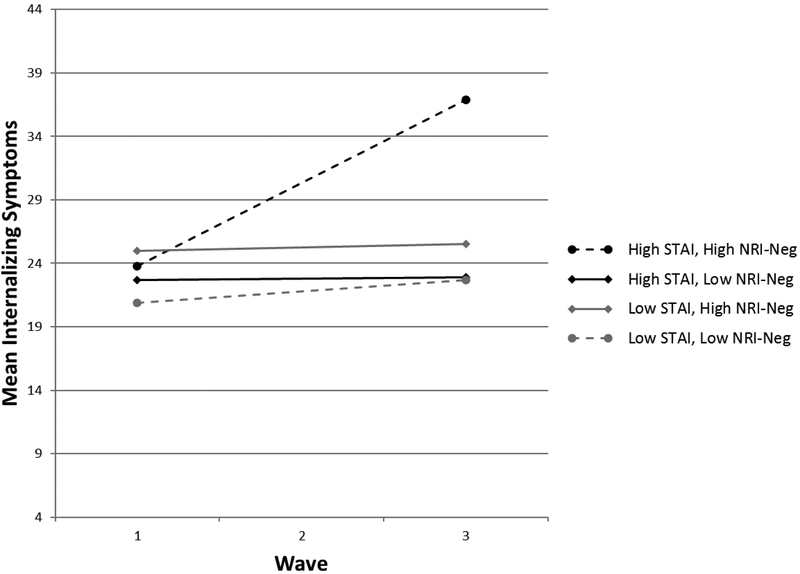
Our final model included interactions between maternal anxiety and both positive and negative friendship interactions (see Figure 1), controlling for maternal emotion dysregulation and child sex. This model also fit the data well: χ2(df=ιo) = 14.12, p =.168, CFI = 0.98, TLI = 0.96, RMSEA = 0.05 (90%CI = 0.00 – 0.11). Higher levels of maternal emotion dysregulation (std. est. = .29, p = .005), and being female (std. est. = −.25, p = .003) were significantly associated with baseline internalizing symptoms only. The interaction between positive friendship quality and maternal anxiety was a significant predictor of the intercept (std. est. = −1.46, p = .006), indicating that maternal anxiety is more strongly (and positively) related with greater initial levels of internalizing symptoms for children with lower positive friendship quality. Only the interaction between negative friendship quality and maternal anxiety significantly predicted the slope (std. est. = .85, p = .041). These results suggest that maternal over time for youth reporting higher levels of negative friendship quality (see Figure 2).
Figure 1.
Final latent growth curve model with sis nt standardized (and unstandardized) path estimates
DERS = Difficulties in Emotion Regulation Scale; STAI = Mother-Reported State Trait Anxiety Inventory; NRI-Pos = Network of Relationships Inventory, Positive Friendship Quality Subscale; NRI-Neg = Network of Relationships Inventory, Negative Friendship Quality Subscale. *p < 0.05, **p < 0.01.
Figure 2.
Linear trajectories of inter ψtoms in youth with low and high levels of maternal anxiety and negative friendship quality
For pictorial clarity, group membership was determined using a mean split of maternal anxiety and negative friend) qualility. STAI = Mother-Reported State Trait Anxiety Inventory; NRINeg = Network of Relationships Inventory, Negative Friendship Quality Subscale.
Discussion
It has been well established that children of anxious parents are at risk for developing psychopathology, but there is limited research examining the effects of maternal anxiety in adolescents, and factors that may buffer or exacerbate this relation. Thus, the primary aims of the current study were to investigate the effects of maternal anxiety on their adolescent children’s internalizing symptoms, and examine if positive or negative friendship quality moderated these relations. Three major results emerged. First, maternal anxiety was a significant predictor of adolescent internalizing symptoms over time. Second, negative friendship quality (but not positive friendship quality) was associated with changes in adolescent internalizing symptoms over time, such that higher levels of negative friendship quality predicted increases in internalizing. Unexpectedly, positive friendship quality was also associated with greater initial levels of internalizing. Third, positive friendship quality moderated the relation between maternal anxiety and adolescent internalizing symptoms at baseline only, while negative friendship quality interacted with maternal anxiety to predict greater increases in internalizing symptoms over time. These findings along with their implications are discussed below.
Consistent with our expectations, maternal anxiety was associated with increases in internalizing symptoms in adolescents over time. The results are in line with several previous studies that have found that parental anxiety predicted child psychopathology (Beesdo et al., 2010; Knappe et al., 2009). This finding is of special importance since it is generally believed that parents become less influential during adolescence. However, our results suggest that parents continue to impact their children’s mental health during adolescence. Genetic and psychosocial factors in the transmission of anxiety may help explain this finding. Past research indicates that anxiety disorders are highly inheritable (Gregory & Eley, 2007). Moreover, several studies have shown correlations between parental anxiety and parental behaviors like greater intrusiveness and control, and lesser warmth and supportiveness in both clinical (Teetsel, Ginsburg, & Drake, 2014; Ginsburg, Grover, & Ialongo, 2004; van der Bruggen, Stams, & Bögels, 2008) and non-clinical (Coplan, Arbeau, & Armer, 2008; Möller, MajdandziC, & Bögels) samples. These behaviors, in turn, have been linked to depression and anxiety in children (see Rapee, 1997 for a review) and adolescents (Rudolph & Zimmer-Gembeck, 2014).
Our findings, however, counter some prior work that found no relation between maternal and adolescent anxiety (e.g. Challcombe and Salkovskis, 2009; Liberman and Öst, 2015). These inconsistencies could be explained by the differences in methodology and design between the studies. For example, utilizing longitudinal data helped us to understand the temporality of the relations between these variables, and how maternal anxiety may influence the longer term trajectory of internalizing symptoms, which would have been impossible to understand using cross-sectional designs that were employed by other studies. Also, the current study used adolescents’ and parents’ report of their own internalizing and anxiety symptoms respectively, thereby reducing the possibility of bias related to parents’ reporting of youth symptoms.
Our next hypothesis examining the effects of friendship quality on adolescent internalizing symptoms predicted that positive friendship quality would be associated with decreases in internalizing symptoms over time, while negative friendship quality would be a significant predictor of increases in internalizing symptoms. Our results supported this hypothesis with regard to negative friendship quality, finding that it was associated with increases in internalizing symptoms in adolescents over time. This finding is consistent with previous studies that suggest that negative interactions and poor friendship quality predicted anxiety and depressive symptoms in adolescents (Humphreys et al., 2015; Martin et al., 2016). The results also suggest that the harmful impact of negative interactions in friendships is not short-lived, but that it affects adolescents’ mental health negatively over a long period of time. What was surprising, though, was that positive friendship quality did not predict decreases in internalizing symptoms. In fact, contrary to our expectations and previous research (Kugbey, Osei-Boadi, Atefoe, 2015; Salzinger, Feldman, Rosario, & Ng-Mak, 2011), we found that positive friendship quality was associated with greater initial levels of internalizing. One possible reason for this finding is that depressed/anxious youth may affiliate with other peers that exacerbate these symptoms. Indeed, a recent review examining the development of personality and friendships (Wrzus & Neyer, 2016) suggests that individuals with certain personality characteristics select or elicit relationship experiences that reinforce those specific characteristics. Alternatively, the finding may also be explained by the effect of a third variable, like co-rumination, which has been associated with simultaneous increases in both positive friendship quality (Felton, Cole, Havewala, Kurdziel, & Brown, 2018; Rose, 2002) and depression (Calmes & Roberts, 2008; Schwartz-Mette & Rose, 2012).
Our next hypothesis predicted that positive friendship quality would buffer the effects of maternal anxiety on internalizing symptoms while negative friendship quality would exacerbate them. Consistent with prior research on stress buffering (Carter, Dellucci, Turek, & Mir, 2015; Folger & Wright, 2013; Paul et al., 2015; Zhang, Yan, Zhao, & Yuan, 2015), we found that positive friendship quality moderated he relation between maternal anxiety and adolescent internalizing symptoms, but only at baseline. While this was expected, it was an interesting, but on]finding given that positive friendship quality was also associated with higher levels of internalizing symptoms at baseline as discussed above. This suggests that two distinct process may be at play: while a third variable like co-rumination could be driving increases in both, positive friendship quality and internalizing symptoms, causing them to covary, positive friendship quality may also buffer the harmful effects of maternal anxiety, separate from the relation of any other variables. Negative friendship quality, on the other hand, exacerbated the effects of maternal anxiety over time. This finding reflects that while positive friendships may not long-lasting. On the other hand, negative interactions in friendships, in the form of conflicts and antagonism, may set the trajectory of internalizing symptoms over time. This may reflect that the collective stress arising from the negative effects of maternal anxiety and negative friendship interactions may lead to the exacerbation of internalizing symptoms. Given the importance placed on friendships during adolescence, conflicts in friendships are likely to be stressful (Buhrmester, 1998). These negative interactions in friendships could lead to even higher levels of stress when coupled with the negative effects of maternal anxiety. Thus, maternal anxiety could worsen the impact of negative friendship quality, and vice-versa, on internalizing symptoms.
Clinical Implications
Our research has several important clinical implications. Maternal anxiety was associated with children’s internalizing symptoms at each wave, suggesting that youth with mothers with higher levels of anxiety are prone to greater symptomatology. Treatment protocols for adolescents with depressive and anxiety symptoms should thus include a formalized screening of psychiatric symptoms of their parents as well. This would provide a holistic understanding of adolescent symptomatology, which in turn could help clinicians tailor. treatment accordingly. Our study also highlighted the importance of assessing social factors, while working with adolescents. Results suggesting that negative interactions in friendship were associated with increases in internalizing symptoms in adolescents underscores the need to include components of social skills training into traditional interventions of treating depression or anxiety, such as cognitive behavioral therapy (CBT). Indeed, research shows that interventions integrating social skills training with CBT proved to be effective in improving social interactions, as well as led to significant reductions in social and general anxiety among children with social phobia (Beidel, Turner, & Morris, 2000; Spence, Donovan, & Brechman-Toussaint, 2000).
Limitations and Future directions
study should be considered in light of several limitations. Firstly, we were unable to examine if gender Findings from the current further moderated the relation between maternal anxiety and friendship quality on adolescent internalizing symptoms. Past research indicates that gender could affect these relations. For example, according to a study by Lee and Goldstein (2016), the adverse impact of lack of support from friends on loneliness was greater in females than in males. On similar lines, social support moderated the effects of stress and depressive symptoms only in adolescent girls, but not in boys (e.g. Landman-Peeters, Hartman, van der Pompe, & den Boer, 2005). In contrast, other studies found that social support exacerbated the relation between stress and internalizing symptoms only in adolescent females (e.g. Brittian, Toomey, Gonzales, & Dumka, 2013; Grant et al., 2000). On the other hand, some studies found that social support moderated the relation between stress and depression equally for adolescent boys and girls (e.g. Cohen et al., 2015; Rueger et al., 2016). Given that there are inconsistencies in the findings with regards to how gender differences could affect these relations, future research utilizing larger samples should aim at examining the role of gender in relation to the variables of maternal anxiety, adolescent internalizing and friendships. Secondly, the study was conducted on a community sample. Although past research has demonstrated relations between subthreshold symptomology and later depressive disorders (Georgiades, Lewinsohn, Monroe, & Seeley, 2006), given that community samples have lower levels of depressive and anxiety symptoms, it is unclear if the findings from our study would generalize to clinical samples. Thus, investigating the relation between maternal anxiety and friendship quality in clinical samples would further extend these findings. Thirdly, the tool that was used to measure the quality of friendships assessed adolescents’ perception of friendships versus actual friendship quality. It is likely that youth with internalizing symptoms could perceive their relationships more negatively (Siegel & Alloy, 1990). Thus, future research should examine these relations using multi-informant approaches, including peer-reports of friendship quality and observational methods. Also, while investigating friendship quality, only relationship with best friends were taken into consideration. Future research may benefit from extending the findings to other forms of friendships and peer relationships. Finally, the current study focused solely on the role of maternal anxiety. Fathers have been historically underrepresented in research on parent-child relations, and additional research on the role of paternal parenting behaviors and psychopathology on the development of adolescent internalizing symptoms would be beneficial (Liber et al., 2008; Teetsel et al., 2014).
Conclusion
Notwithstanding the limitations, the current study revealed important risk and protective factors in relation to adolescent internalizing symptoms. While there are numerous studies on the links between parental anxiety and child psychopathology, and on stress-buffering, the current study is one of the first to examine the variables of maternal anxiety, friendship quality and internalizing symptoms during the critical period of adolescence. Our findings also highlight the importance of developing future interventions targeted at both parental psychopathology and social influences.
Funding:
This research was funded in part by a grant from the National Institute of Drug Abuse Grant R01DA018647 (primary investigator, C.W. Lejuez).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest: The authors declare that they have no conflict of interest.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was conducted in compliance with all procedures approved by the University of Maryland Institutional Review Board. All protocols were consistent with national and international ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- Angold A, Costello EJ, & Worthman CM (1998). Puberty and depression: The roles of age, pubertal status, and pubertal timing. Psychological Medicine, 28, 51–61 [DOI] [PubMed] [Google Scholar]
- Asselmann E, Wittchen H−, Lieb R, Höfler M, & Beesdo-Baum K (2016). Does low coping efficacy mediate the association between negative life events and incident psychopathology? A prospective-longitudinal community study among adolescents and young adults. Epidemiology And Psychiatric Sciences, 25(2), 171–180. doi: 10.1017/S204579601500013X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bados A, Gómez-Benito J, & Balaguer G (2010). The State-Trait Anxiety Inventory, Trait Version: Does it really measure anxiety? Journal of Personality Assessment, 92(6), 560–567. 10.1080/00223891.2010.513295 [DOI] [PubMed] [Google Scholar]
- Beal AC, Ausiello J, & Perrin JM (2001). Social influences on health-risk behaviors among minority middle school students. Journal Of Adolescent Health, 28(6), 474–480. doi: 10.1016/S1054-139X(01)00194-X [DOI] [PubMed] [Google Scholar]
- Beesdo K, Pine DS, Lieb R, & Wittchen H (2010). Incidence and risk patterns of anxiety and depressive disorders and categorization of generalized anxiety disorder. Archives Of General Psychiatry, 67(1), 47–57. doi: 10.1001/archgenpsychiatry.2009.177 [DOI] [PubMed] [Google Scholar]
- Beidel DC, & Turner SM (1997). At risk for anxiety: I. Psychopathology in the offspring of anxious parents. Journal Of The American Academy Of Child & Adolescent Psychiatry, 36(7), 918–924. doi: 10.1097/00004583-199707000-00013 [DOI] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, & Morris TL (2000). Behavioral treatment of childhood social phobia. Journal Of Consulting And Clinical Psychology, 68(6), 1072–1080. doi: 10.1037/0022-006X.68.6.1072 [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Hirshfeld-Becker DR, Friedman D, Robin JA, & Rosenbaum JF (2001). Patterns of psychopathology and dysfunction in high-risk children of parents with panic disorder and major depression. The American Journal Of Psychiatry, 158(1), 49–57. doi: 10.1176/appi.ajp.158.1.49 [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty C, Faraone SV, Henin A, Hirshfeld-Becker D, Pollack MH, & … Rosenbaum JF (2006). Effects of parental anxiety disorders in children at high risk for panic disorder: A controlled study. Journal Of Affective Disorders, 94(1–3), 191–197. doi: 10.1016/j.jad.2006.04.012 [DOI] [PubMed] [Google Scholar]
- Bieling PJ, Antony MM, & Swinson RP (1998). The State-Trait Anxiety Inventory, Trait version: Structure and content re-examined. Behaviour Research and Therapy, 36(7–8), 777–788. 10.1016/S0005-7967(98)00023-0 [DOI] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. structu Psychological Bulletin, 107(2), 238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berndt TJ (1996). Exploring the effects of friendship quality on social development In Bukowski WM, Newcomb AF, & Hartup WW (Eds.), The company they keep: Friendship in childhood and adolescence (pp. 346–365). New York: Cambridge University Press. [Google Scholar]
- Bouma EMC, Ormel J, Verhulst FC, & Oldehinkel AJ (2008). Stressful life events and depressive problems in early adolescent boys and girls: The influence of parental depression, temperament and family environment. Journal of Affective Disorders, 105(1–3), 185–193. 10.1016/j.jad.2007.05.007 [DOI] [PubMed] [Google Scholar]
- Brittian AS, Toomey RB, Gonzales NA, & Dumka LE (2013). Perceived discrimination, coping strategies, and Mexican origin adolescents’ internalizing and externalizing behaviors: Examining the moderating role of gender and cultural orientation. Applied Developmental Science, 17(1), 4–19. 10.1080/10888691.2013.748417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown BB (2004). Adolescents’ relationships with peers In Lerner RM & Steinberg L (Eds.), Handbook of Adolescent Psychology, 2nd edition (pp. 363–394). New York: Wiley. [Google Scholar]
- Buhrmester D (1998). Need fulfillment, interpersonal competence, and the developmental contexts of early adolescent friendship In Bukowski WM, Newcomb AF, & Hartup WW (Eds.), The company they keep: Friendship in childhood and adolescence (pp. 158–185). New York, NY: Cambridge University Press [Google Scholar]
- Burstein M, Ginsburg GS, Petras H, & Ialongo N (2010). Parent psychopathology and youth internalizing symptoms in an urban community: A latent growth model analysis. Child Psychiatry And Human Development, 41(1), 61–87. doi: 10.1007/s10578-009-0152-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burstein M, Ginsburg GS, & Tein J (2010). Parental anxiety and child symptomatology: An examinzation of additive and interactive effects of parent psychopathology. Journal Of Abnormal Child Psychology, 38(7), 897–909. doi: 10.1007/s10802-010-9415-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calmes CA, & Roberts JE (2008). Rumination in interpersonal relationships: Does Corumination explain gender differences in emotional distress and relationship satisfaction among college students?. Cognitive Therapy And Research, 32(4), 577–590. doi: 10.1007/s10608-008-9200-3 [DOI] [Google Scholar]
- Carter JS, Dellucci T, Turek C, & Mir S (2015). Predicting depressive symptoms and weight from adolescence to adulthood: Stressors and the role of protective factors. Journal Of Youth And Adolescence, 44(11), 2122–2140. doi: 10.1007/s10964-015-0301-5 [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2016). Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16–4984, NSDUH Series H-51). Retrieved from http://www.samhsa.gov/data/
- Challacombe F, & Salkovskis P (2009). A preliminary investigation of th : impact of maternal obsessive-compulsive disorder and panic disorder on parenting and children. Journal Of Anxiety Disorders, 23(7), 848–857. doi: 10.1016/j.janxdis.2009.04.002 [DOI] [PubMed] [Google Scholar]
- Cheng Y, Li X, Lou C, Sonenstein FL, Kalamar A, Jejeebhoy S, & … Ojengbede O (2014). The association between social support and mental health among vulnerable adolescents in five cities: Findings from the study of the well-being of adolescents in vulnerable environments. Journal Of Adolescent Health, 55(6, Suppl), S31–S38. doi: 10.1016/j.jadohealth.2014.08.020 [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Moffitt CE, & Gray J (2005). Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample. Behaviour Research And Therapy, 43(3), 309–322. doi: 10.1016/j.brat.2004.02.004 [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, & Francis SE (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy, 38(8), 835–855. doi: 10.1016/S0005-7967(99)00130-8 [DOI] [PubMed] [Google Scholar]
- Cohen JR, Spiro CN, Young JF, Gibb BE, Hankin BL, & Abela JRZ (2015). Interpersonal risk profiles for youth depression: A person-centered, multi-wave, longitudinal study. Journal of Abnormal Child Psychology, 43(8), 1415–1426. 10.1007/s10802-015-0023-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins WA, & Laursen B (2004). Changing Relationships, Changing Youth: Interpersonal Contexts of Adolescent Development. The Journal Of Early Adolescence, 24(1), 55–62. doi: 10.1177/0272431603260882 [DOI] [Google Scholar]
- Coplan RJ, Arbeau KA, & Armer M (2008). Don’t fret, be supportive! Maternal characteristics linking child shyness to psychosocial and school adjustment in kindergarten. Journal Of Abnormal Child Psychology, 36(3), 359–371.doi: 10.1007/s10802-007-9183-7 [DOI] [PubMed] [Google Scholar]
- Costello EJ, Egger HL, & Angold A (2005). The Developmental Epidemiology of Anxiety Disorders: Phenomenology, Prevalence, and Comorbidity. Child And Adolescent Psychiatric Clinics Of North America, 14(4), 631–648. doi: 10.1016/j.chc.2005.06.003 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, & Kazdin AE (2005). Informant Discrepancies in the Assessment of Childhood Psychopathology: A Critical Review, Theoretical Framework, and Recommendations for Further Study. Psychological Bulletin, 131(4), 483–509. doi: 10.1037/0033-2909.131.4.483 [DOI] [PubMed] [Google Scholar]
- Dowling NA, Shandley K, Oldenhof E, Youssef GJ, Thomas SA, Frydenberg E, & Jackson AC (2016). The intergenerational transmission of problem gambling: The mediating role of parental psychopathology. Addictive Behaviors, 5912–17. doi: 10.1016/j.addbeh.2016.03.002 [DOI] [PubMed] [Google Scholar]
- Edwards ES, Holzman JB, Burt NM, Rutherford HJV, Mayes LC, & Bridgett DJ (2017). Maternal emotion regulation strategies, internalizing problems and infant negative affect. Journal of Applied Developmental Psychology, 48, 59–68. https://doi-org.proxy-um.researchport.umd.edu/10.1016/j.appdev.2016.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epkins CC, & Heckler DR (2011). Integrating etiological models of social anxiety and depression in youth: Evidence for a cumulative interpersonal risk model. Clinical Child And Family Psychology Review, 14(4), 329–376. doi: 10.1007/s10567-011-0101-8 [DOI] [PubMed] [Google Scholar]
- Essau CA, Ishikawa S, Sasagawa S, Otsui K, Sato H, Okajima I, & … Bray D (2013). Psychopathological symptoms in two generations of the same family: A cross-cultural comparison. Social Psychiatry And Psychiatric Epidemiology, 48(12), 2017–2026. doi: 10.1007/s00127-013-0673-3 [DOI] [PubMed] [Google Scholar]
- Evans SE, Steel AL, & DiLillo D (2013). Child maltreatment severity and adult trauma symptoms: Does perceived social support play a buffering role?. Child Abuse & Neglect, 37(11), 934–943. doi: 10.1016/j.chiabu.2013.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felton JW, Cole DA, Havewala M, Kurdziel G, & Brown V (2018). Talking together, thinking alone: Relations among co-rumination, peer relationships, and rumination. Journal of Youth and Adolescence 10.1007/s10964-018-0937-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Festa CC, & Ginsburg GS (2011). Parental and peer predictors of social anxiety in, youth. Child Psychiatry And Human Development, 42(3), 291–306. doi: 10.1007/s10578-011-0215-8011-0215-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folger SF, & Wright MO (2013). Altering risk following child maltreatment: Family and friend support as protective factors. Journal of Family Violence, 28, 325–337. doi: 10.1007/s10896-013-9510-4 [DOI] [Google Scholar]
- Francis SE, & Chorpita BF (2011). Parental beliefs about child anxiety as a mediator of parent and child anxiety. Cognitive Therapy And Research, 35(1), 21–29. doi: 10.1007/s10608-009-9255-9 [DOI] [Google Scholar]
- Furman W & Buhrmester D (1985). Children’s perceptions of the personal relationships in their social networks. Developmental Psychology, 21, 1016–1022. [Google Scholar]
- Georgiades K, Lewinsohn PM, Monroe SM, & Seeley JR (2006). Major Depressive Disorder in Adolescence: The Role of Subthreshold Symptoms. Journal Of The American Academy Of Child & Adolescent Psychiatry, 45(8), 936–944. doi: 10.1097/01.chi.0000223313.25536.47 [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Grover RL, & Ialongo N (2004). Parenting Behaviors Among Anxious and Non-Anxious Mothers: Relation with Concurrent and Long-Term Child Outcomes. Child & Family Behavior Therapy, 26(4), 23–41. doi: 10.1300/J019v26n04_02 [DOI] [Google Scholar]
- Grant KE, O’Koon JH, Davis TH, Roache NA, Poindexter LM, Armstrong ML, … McIntosh JM (2000). Protective factors affecting low-income urban African American youth expos stress. The Journal of Early Adolescence, 20(4), 388–417. 10.1177/0272431600020004002 [DOI] [Google Scholar]
- Gratz KL & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26, 41–54. [Google Scholar]
- Gregory AM, & Eley TC (2007). Genetic influences on anxiety in children: What we’ve learned and where we’re heading. Clinical Child And Family Psychology Review, 10(3), 199–212. doi: 10.1007/s10567-007-0022-8 [DOI] [PubMed] [Google Scholar]
- Gluschkoff K, Keltikangas-Järvinen L, Pulkki-Råback L, Jokela M, Viikari J, Raitakari O, & Hintsanen M (2017). Hostile parenting, parental psychopathology, and depressive symptoms in the offspring: A 32-year follow-up in the Young Finns study. Journal Of Affective Disorders, 208436–442. doi: 10.1016/j.jad.2016.11.002 [DOI] [PubMed] [Google Scholar]
- Herzer M, Umfress K, Aljadeff G, Ghai K, & Zakowski SG (2009). Interactions with parents and friends among chronically ill children: Examining social networks. Journal of Developmental and Behavioral Pediatrics, 30(6), 499–508. https://doi-org.proxy-um.researchport.umd.edu/10.1097/DBP.0b013e3181c21c82 [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker DR, Micco JA, Henin A, Petty C, Faraone SV, Mazursky H, … Biederman J (2012). Psychopathology in adolescent offspring of parents with panic disorder, major depression, or both: A 10-year follow-up. The American Journal of Psychiatry, 169(11), 1175–1184. 10.1176/appi.ajp.2012.11101514 [DOI] [PubMed] [Google Scholar]
- Hishinuma ES, Miyamoto RH, Nishimura ST, Goebert DA, Yuen NYC, Makini GK Jr., … Carlton BS (2001). Prediction of anxiety disorders using the State-Trait Anxiety Inventory for multiethnic adolescents. Journal of Anxiety Disorders, 15(6), 511–533. 10.1016/S0887-6185(01)00079-2 [DOI] [PubMed] [Google Scholar]
- Holt MK, & Espelage DL (2005). Social Support as a Moderator Between Dating Violence Vi ctimiza.icn and Depression/Anxiety Among African American and Caucasian Adolescents. School Psychology Review, 34(3), 309–328. [Google Scholar]
- Humphreys KL, Katz SJ, Lee SS, Hammen C, Brennan PA, & Najman JM (2013). The association of ADHD and depression: Mediation by peer problems and parent-child difficulties in two complementary samples. Journal Of Abnormal Psychology, 122(3), 854–867. doi: 10.1037/a0033895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerns CE, Pincus DB, McLaughlin KA, & Comer JS (2017). Maternal emotion regulation during child distress, child anxiety accommodation, and links between maternal and child anxiety. Journal of Anxiety Disorders, 50, 52–59. https://doi-org.proxy-um.researchport.umd.edu/10.1016/j.janxdis.2017.05.002 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, & … Zaslavsky AM (2005). Prevalence and Treatment of Mental Disorders, 1990 to 2003. The New England Journal Of Medicine, 352(24), 2515–2523. doi: 10.1056/NEJMsa043266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kliewer W, Murrelle L, Mejia R, Torres de G,Y, & Angold A (2001). Exposure to violence against a family member and internalizing symptoms in Colombian adolescents: The protective effects of family support. Journal Of Consulting And Clinical Psychology, 69(6), 971–982. doi: 10.1037/0022-006X.69.6.971 [DOI] [PubMed] [Google Scholar]
- Knappe S, Beesdo K, Fehm L, Höfler M, Lieb R, & Wittchen H (2009). Do parental psychopathology and unfavorable family environment predict the persistence of social phobia?. Journal Of Anxiety Disorders, 23(7), 986–994. doi: 10.1016/j.janxdis.2009.06.010 [DOI] [PubMed] [Google Scholar]
- Kugbey N, Osei-Boadi S, Atefoe EA (2015). The Influence of Social Support on the Levels of Depression, Anxiety and Stress among Students in Ghana. Journal of Education and Practice, 6(25), 135–140. [Google Scholar]
- La Greca AM, & Harrison HM (2005). Adolescent Peer Relations, Friendships, and Romantic Relationships: Do They Predict Social Anxiety and Depression?. Journal Of Clinical Child And Adolescent Psychology, 34(1), 49–61. doi: 10.1207/s15374424jccp3401_5 [DOI] [PubMed] [Google Scholar]
- Landman-Peeters KMC, Hartman CA, van der Pompe G, den Boer JA, Minderaa RB, & Ormel J (2005). Gender differences in the relation between social support, problems in parent-offspring communication, and depression and anxiety. Social Science & Medicine, 60(11), 2549–2559. 10.1016/j.socscimed.2004.10.024 [DOI] [PubMed] [Google Scholar]
- Lee CS, & Goldstein SE (2016). Loneliness, stress, and social support in young adulthood: Does the source of support matter?. Journal Of Youth And Adolescence, 45(3), 568–580. doi: 10.1007/s10964-015-0395-9 [DOI] [PubMed] [Google Scholar]
- Liber JM, van Widenfelt BM, Goedhart AW, Utens EJ, van der Leeden AM, Markus MT, & Treffers PA (2008). Parenting and parental anxiety and depression as predictors of treatment outcome for childhood anxiety disorders: Has the role of fathers been underestimated?. Journal Of Clinical Child And Adolescent Psychology, 37(4), 747–758. doi: 10.1080/15374410802359692 [DOI] [PubMed] [Google Scholar]
- Liberman LC, & Öst L (2016). The relation between fears and anxiety in children with specific phobia and parental fears and anxiety. Journal Of Child And Family Studies, 25(2), 598–606. doi: 10.1007/s10826-015-0222-7 [DOI] [Google Scholar]
- Martin NC, Felton JW, & Cole DA (2016). Predictors of youths’ posttraumatic stress symptoms following a natural disaster: The 2010 Nashville, Tennessee, flood. Journal Of Clinical Child And Adolescent Psychology, 45(3), 335–347. doi: 10.1080/15374416.2014.982279 [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Avenevoli S, Dierker L, & Grillon C (1999). Vulnerability factors among children at risk for anxiety disorders. Biological Psychiatry, 46(11), 1523–1535. doi: 10.1016/S0006-3223(99)00172-9 [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Dierker LC, & Szamari P (1998). Psychopathology among offspring of parents with substance abuse and/or anxiety disorders: A high risk study. Journal Of Child Psychology And Psychiatry, 39(5), 711–720. doi: 10.1017/S0021963098002522 [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, & … Swendsen J (2010). Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A). Journal Of The American Academy Of Child & Adolescent Psychiatry, 49(10), 980–989. doi: 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Lieb R, Wittchen H−, & Avenevoli S (2003). Family and high-risk studies of social anxiety disorder. Acta Psychiatrica Scandinavica, 108(Suppl417), 28–37. doi: 10.1034/j.1600-0447.108.s417.5.x [DOI] [PubMed] [Google Scholar]
- Micco JA, Henin A, Mick E, Kim S, Hopkins CA, Biederman J, & Hirshfeld-Becker DR (2009). Anxiety and depressive disorders in offspring at high risk for anxiety: A meta-analysis. Journal Of Anxiety Disorders, 23(8), 1158–1164. doi: 10.1016/j.janxdis.2009.07.021 [DOI] [PubMed] [Google Scholar]
- Möller EL, Majdandzic M, & Bögels SM (2015). Parental anxiety, parenting behavior, and infant anxiety: Differential associations for fathers and mothers. Journal Of Child And Family Studies, 24(9), 2626–2637. doi: 10.1007/s10826-014-0065-7 [DOI] [Google Scholar]
- Murthi M, & Espelage DL (2005). Childhood sexual abuse, social support, and psychological outcomes: A loss framework. Child Abuse & Neglect, 29(11), 1215–1231. doi: 10.1016/j.chiabu.2005.03.008 [DOI] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (2010). Mplus User’s Guide. Sixth Edition Los Angeles, CA: Muthén & Muthén [Google Scholar]
- Nangle DW, Erdley CA, Newman JE, Mason CA, & Carpenter EM (2003). Popularity, Friendship Quantity, and Friendship Quality: Interactive Influences on Children’s Loneliness and Depression. Journal Of Clinical Child And Adolescent Psychology, 32(4), 546–555. doi: 10.1207/S15374424JCCP3204_7 [DOI] [PubMed] [Google Scholar]
- Negriff S, & Susman EJ (2011). Pubertal timing, depression, and externalizing problems: A framework, review, and examination of gender differences. Journal Of Research On Of Research Adolescence, 21(3), 717–746. doi: 10.1111/j.1532-7795.2010.00708.x [DOI] [Google Scholar]
- Newman BM, Newman PR, Griffen S, O’Connor K, & Spas J (2007). The relationship of social support to depressive symptoms during the transition to high school. Adolescence, 42(167), 441–459. [PubMed] [Google Scholar]
- Nivard MG, Lubke GH, Dolan CV, Evans DM, St. Pourcain B, Munafò MR, & Middeldorp CM (2017). Joint developmental trajectories of internalizing and externalizing disorders between childhood and adolescence. Development And Psychopathology, doi: 10.1017/S0954579416000572 [DOI] [PubMed] [Google Scholar]
- Parker JG, Rubin KH, Erath SA, Wojslawowicz JC, & Buskirk AA (2006). Peer relationships, child development, and adjustment: A developmental psychopathology perspective In Cicchetti D & Cohen DJ (Eds.), Developmental psychopathology: Vol. 1. Theory and method (2nd ed., pp. 419–493). New York: Wiley. [Google Scholar]
- Paul LA, Felton JW, Adams ZW, Welsh K, Miller S, & Ruggiero KJ (2015). Mental health among adolescents exposed to a tornado: The influence of social support and its interactions with sociodemographic characteristics and disaster exposure. Journal Of Traumatic Stress, 28(3), 232–239. doi: 10.1002/jts.22012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piacentini J, Peris TS, Bergman RL, Chang S, & Jaffer M (2007). Functional impairment in childhood OCD : Development and psychometrics properties of the Child Obsessive-Compulsive Impact Scale--Revised (COIS--R). Journal Of Clinical Child And Adolescent Psychology, 36(4), 645–653. doi: 10.1080/15374410701662790 [DOI] [PubMed] [Google Scholar]
- Rapee RM (1997). Potential role of childrearing practices in the development of anxiety and depression. Clinical Psychology Review, 17(1), 47–67. doi: 10.1016/S0272-7358(96)00040-2 [DOI] [PubMed] [Google Scholar]
- Rasing SA, Creemers DM, Janssens JM, & Scholte RJ (2015). The association between perceived maternal and paternal psychopathology and depression and anxiety symptoms in adolescent girls. Frontiers In Psychology, 6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Lee JK, Salters-Pedneault K, Erisman SM, Orsillo SM, & Mennin DS (2009). Mindfulness and emotion regulation difficulties in generalized anxiety disorder: Preliminary evidence for independent and overlapping contributions. Behavior Therapy, 40(2), 142–154. doi: 10.1016/j.beth.2008.04.0010.1016/j.b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose AJ (2002). Co-rumination in the friendships of girls and boys. Child Development, 73(6), 1830–1843. doi: 10.1111/1467-8624.00509 [DOI] [PubMed] [Google Scholar]
- Roza SJ, Hofstra MB, van der Ende J, & Verhulst FC (2003). Stable prediction of mood and anxiety disorders based on behavioral and emotional problems in childhood: A 14-year follow-up during childhood, adolescence, and young adulthood. The American Journal Of Psychiatry, 160(12), 2116–2121. doi: 10.1176/appi.ajp.160.12.2116 [DOI] [PubMed] [Google Scholar]
- Rubin KH, Dwyer KM, Booth-LaForce C, Kim AH, Burgess KB, & Rose-Krasnor L (2004). Attachment, Friendship, and Psychosocial Functioning in Early Adolescence. The Journal Of Early Adolescence, 24(4), 326–356. doi: 10.1177/0272431604268530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph J, & Zimmer-Gembeck MJ (2014). Parent relationships and adolescents’ depression and social anxiety: Indirect associations via emotional sensitivity to rejection threat. Australian Journal Of Psychology, 66(2), 110–121. doi: 10.1111/ajpy.12042 [DOI] [Google Scholar]
- Rueger SY, Malecki CK, Pyun Y, Aycock C, & Coyle S (2016). A meta-analytic review of the association between perceived social support and depression in childhood and adolescence. Psychological Bulletin, 142(10), 1017–1067. doi: 10.1037/bul0000058 [DOI] [PubMed] [Google Scholar]
- Salzinger S, Feldman RS, Rosario M, & Ng-Mak DS (2011). Role of parent and peer relationships and individual characteristics in middle school children’s behavioral outcomes in the face of community violence. Journal Of Research On Adolescence, 21(2), 395–407. doi: 10.1111/j.1532-7795.2010.00677.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz-Mette RA, & Rose AJ (2012). Co-rumination mediates contagion of internalizing symptoms within youths’ friendships. Developmental Psychology, 48(5), 1355–1365. doi: 10.1037/a0027484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweizer K (2010). Improving the interpretability of the variances of latent variables by uniform and factor-specific standardizations of loadings. Methodology: European Journal of Research Methods for the Behavioral and Social Sciences, 6(4), 152–159. doi: 10.1027/1614-2241/a000017 [DOI] [Google Scholar]
- Siegel SJ, & Alloy LB (1990). Interpersonal perceptions and consequences of depressive-significant other relationships: A naturalistic study of college roommates. Journal of Abnormal Psychology, 99, 361–373. [DOI] [PubMed] [Google Scholar]
- Spence SH, Donovan C, & Brechman-Toussaint M (2000). The treatment of childhood social phobia: The effectiveness of a social skills training-based, cognitive-behavioural intervention, with and without parental involvement. Journal Of Child Psychology And Psychiatry, 41(6), 713–726. doi: 10.1111/1469-7610.00659 [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, & Jacobs GA (1983). Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Steiger JH (1990). Structural model evaluation and modification: an interval estimation approach. Multivariate Behavioral Research, 25, 173–180. [DOI] [PubMed] [Google Scholar]
- Su S, Pettit GS, & Erath SA (2016). Peer relations, parental social coaching, and young adolescent social anxiety. Journal Of Applied Developmental Psychology, 4289–97. doi: 10.1016/j.appdev.2015.11.007 [DOI] [Google Scholar]
- Sumter SR, Bokhorst CL, Steinberg L, & Westenberg PM (2009). The developmental pattern of resistance to peer influence in adolescence: Will the teenager ever be able to resist?. Journal Of Adolescence, 32(4), 1009–1021. doi: 10.1016/j.adolescence.2008.08.010 [DOI] [PubMed] [Google Scholar]
- Sylvester CE, Hyde TS, & Reichler RJ (1987). The Diagnostic Interview for Children and Personality Inventory for Children in studies of children at risk for anxiety disorders or depression. Journal Of The American Academy Of Child & Adolescent Psychiatry, 26(5), 668–675. doi: 10.1097/00004583-198709000-00010 [DOI] [PubMed] [Google Scholar]
- Teetsel RN, Ginsburg GS, & Drake KL (2014). Anxiety-promoting parenting behaviors: A comparison of anxious mothers and fathers. Child Psychiatry And Human Development, 45(2), 133–142. doi: 10.1007/s10578-013-0384-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tillery R, Disabatino K, Parra GR, Buckholdt KE, & Jobe-Shields L (2014). Examination of consistency of adolescent and parent reports across several psychosocial constructs. Personal Relationships, 21(4), 599–611. doi: 10.1111/pere.12051 [DOI] [Google Scholar]
- Tucker LR, & Lewis C (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38(1), 1–10. doi: 10.1007/BF02291170. [DOI] [Google Scholar]
- Tull MT, Stipelman BA, Salters-Pedneault K, & Gratz KL (2009). An examination of recent non-clinical panic attacks, panic disorder, anxiety sensitivity, and emotion id emoti regulation difficulties in the prediction of generalized anxiety disorder in an analogue sample. Journal Of Anxiety Disorders, 23(2), 275–282. doi: 10.1016/j.janxdis.2008.08.002 [DOI] [PubMed] [Google Scholar]
- van der Bruggen CO, Stams GJ, & Bögels SM (2008). Research review: The relation between child and parent anxiety and parental control: A meta-analytic review. Journal Of Child Psychology And Psychiatry, 49(12), 1257–1269. doi: 10.1111/j.1469-7610.2008.01898.x [DOI] [PubMed] [Google Scholar]
- van der Pol LD, Groeneveld MG, Endendijk JJ, van Berkel SR, Hallers-Haalboom ET, Bakermans-Kranenburg MJ, & Mesman J (2016). Associations between fathers’ and mothers’ psychopathology symptoms, parental emotion socialization, and preschool ers’ social-emotional development. Journal Of Child And Family Studies, 25(11), 3367–3380. doi: 10.1007/s10826-016-0490-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner V, Mufson L, & Weissman MM (1995). Offspring at high and low risk for depression and anxiety: Mechanisms of psychiatric disorder. Journal Of The American Academy Of Child & Adolescent Psychiatry, 34(6), 786–797. doi: 10.1097/00004583-199506000-00020 [DOI] [PubMed] [Google Scholar]
- Weinberg A, & Klonsky ED (2009). Measurement of emotion dysregulation in adolescents. Psychological Assessment, 21(4), 616–621. doi: 10.1037/a0016669 [DOI] [PubMed] [Google Scholar]
- Wichstrom L (1999). The emergence of gender differences in depressed mood during adolescence: The role of intensified gender socialization. Developmental Psychology, 35, 232–245. [PubMed] [Google Scholar]
- Woodhead EL, Northrop L, & Edelstein B (2016). Stress, social support, and burnout among long-term care nursing staff. Journal Of Applied Gerontology, 35(1), 84–105. doi: 10.1177/0733464814542465 [DOI] [PubMed] [Google Scholar]
- Wrzus C, & Neyer FJ (2016). Co-development of personality and friendships across the lifespan: An empirical review on selection and socialization. European Psychologist, 21(4), 254–273. doi: 10.1027/1016-9040/a000277 [DOI] [Google Scholar]
- Zhang B, Yan X, Zhao F, & Yuan F (2015). The relationship between perceived stress and adolescent depression: The roles of social support and gender. Social Indicators Research, 123(2), 501–518. doi: 10.1007/s11205-014-0739-y [DOI] [Google Scholar]