Abstract
Nursing home information technology (NH IT) adoption trends are not measured regularly. Evidence indicates digital footprints are growing, but gaps about NH IT adoption and quality impacts remain. We hypothesize as NH IT adoption grows, quality improves. This research assessed ternary (2014-2017) trends in IT and quality measures using a primary survey of U.S. NHs. Survey measures included nine dimensions/domains and total IT sophistication. Administrators completed 815 Year 1 surveys. Each year mean total IT sophistication scores in nine dimensions/domains consistently increased. Eighteen significant correlations (r > .13, absolute value) between IT sophistication and quality measures existed. Regression shows that for every 10 units increase in administrative activity extent of IT use, a decrease of 1.3% occurs in the percentage of low-risk long-stay residents with bowel or bladder incontinence. Increases in NH IT sophistication positively impact quality. Estimating ongoing trends in NH IT sophistication provides new information that should be consistently available.
Keywords: nursing homes, information technology, informatics, technology assessment, health care surveys
Introduction
Current health information technology (HIT) strategic plans are striving to improve the health and well-being of individuals and communities by improving the nation’s HIT infrastructure (Office of the National Coordinator for Health Information Technology [ONC], 2015). Subsequently, health care’s digital footprint has increased dramatically due to important legislation incentivizing hospitals and physicians to adopt technology (U.S. Department of Health & Human Services, 2016). For example, the percentage of nonfederal acute care hospitals using technology to exchange clinical information with other ambulatory providers or hospitals outside their organization increased from 41% to 82% between 2008 and 2015. Furthermore, patients’ access to electronically view their health information has increased from 24% to 95% from 2012-2015, respectively (ONC, 2016). Increasing trends in IT capabilities offer an opportunity for persons in health care settings outside of ambulatory or hospital environments, for example, nursing homes (NHs), to make vital electronic connections to partners who care for the same patients transitioning between settings. However, policies incentivizing IT adoption in health care oftentimes did not include NHs (Vest et al., 2018). At the same time, HIT adoption trends in NHs were not measured on a regular basis, creating a knowledge gap about technology adoption and its impact on quality. The purpose of this article is to address this gap with a report demonstrating 3-year national trends in NH HIT adoption and quality measures (QMs).
Policy Driving NH IT Implementation
Regulatory provisions have stimulated growth of HIT to facilitate compliance and promote patient safety for many years. The 1987 Omnibus Budget Reconciliation Act introduced electronic data collection and sharing of patient data using technology (“U.S. Congress Omnibus Budget Reconciliation Act of 1987,” 1987). The 1997 Balanced Budget Act required a Minimum Data Set (MDS) that elevated the importance of electronic patient data use in payment systems (“Balanced Budget Act of 1997,” 1997). In 2009, the Health Information Technology for Economic and Clinical Health (HITECH) Act promoted HIT, including electronic health records (EHRs) and health information exchange (HIE) as conduits for enhancing the quality, safety, and efficiency of health care. The HITECH Act set into motion meaningful use of HIT, which incentivized interoperable EHR adoption as a national health care goal (“American Reinvestment and Recovery Act,” 2009). More specifically, HITECH established regional extension centers to support providers adopting HIT, supported programs for HIE development, created workforce training and education, and so on (Blumenthal, 2010). In 2012, the Food and Drug Administration Safety and Innovation Act (FDASIA; 2012) required the FDA to consult with the ONC, and Federal Communications Commission to recommend a strategy for a regulatory HIT framework that included mobile medical applications, innovation, and improved patient safety. In 2015, the Medicare Access and CHIP Reauthorization Act (MACRA) sought to transform the nation’s health care system through better care, smarter spending, and healthier people by providing incentives, improving care delivery, and enhancing information sharing with technology (Centers for Medicare & Medicaid Services [CMS], 2015). The focus of the act was not particularly on NH HIT; however, the act required use of shared electronic continuity of care documents by providers when transitioning residents to other providers, which frequently happens in NH. Finally, the 2016 21st Century Cures Act accelerated medical device development and innovation in health care. The most pressing problem with these policies is they did not include or were not specific to NH HIT, beyond Omnibus Budget Reconciliation Act (OBRA) of 1987 and mandating the MDS assessment, contributing to the lack of NH IT adoption.
Significance of NH IT Assessment
NH HIT assessments are becoming increasingly common in the literature to substantiate claims that HIT improves safety, quality, and productivity (Vest et al., 2018). The growing technology revolution in aged care is not limited to certain geographical areas. The revolution is taking place worldwide (Scott-Kruse et al., 2017). Many policy setting organizations around the globe are beginning to establish future agendas for use of NH technology (Carretero, 2015). As NH administrators are envisioning the future of their organizations, they must be proactive and include technology innovation as a resource to promote better care.
Evidence appears in rigorous systematic reviews incorporating search strategies on NH HIT implementation. For example, a recent review led to the discovery of 46 separate research studies since 2004, categorized under four major themes, including barriers/facilitators to IT adoption, care processes and productivity, staff satisfaction, and quality of care (Ko, Wagner, & Spetz, 2018). Within themes are stark reminders why NH HIT trends are important to assess regularly. For example, there are little to no systematic process for NH HIT implementation, staff report frustration because HIT support is insufficient or nonexistent and are rarely on site, and there is limited empirical evidence that HIT improves quality of care. Furthermore, trends identifying developing disparities in IT resources based on regional location, ownership, bedsize have been reported (Scott-Kruse et al., 2017). A few rigorous NH studies conducted incorporate IT as a mechanism to improve QMs, costs, and impact on staffing (Rantz et al., 2010). Furthermore, other NH studies have examined the extent of useful IT capabilities including EHR and HIE adoption (Abramson, McGinnis, Moore, Kaushal, & HITEC Investigators, 2014). However, it is difficult to generalize results of these studies beyond the multisite statewide assessments conducted in other settings. In addition, national studies that have been reported are not longitudinal in nature. Therefore, progressive change in IT maturity is not measured consistently (Resnick, Manard, Stone, & Alwan, 2009).
Associations Between NH QMs and IT
IT is not linked to key NH quality measurement systems. If our prior results are replicated in the national data, such as if clinical documentation systems in resident care are associated with changes in quality (Alexander & Madsen, 2018), this finding would strongly support establishing ongoing national evaluations of NH IT and QMs as a way to manage resident care. Such a find would influence science by identifying IT use as a key component of quality measurement. With little evidence describing systematic NH HIT implementation processes or outcomes that proves HIT benefits care delivery in NH, there is likely going to be reduced or static adoption trends in this sector of health care (Gagnon et al., 2012). In this research, we focus on two specific aims:
Specific Aim 1: Describe the pattern of changes in IT sophistication over time and examine associations between the changes in IT sophistication and NH attributes (e.g., bedsize, ownership, location).
Specific Aim 2: Examine whether patterns of change in overall IT sophistication in NHs are associated with changes in MDS-derived QM scores over 3 years.
Method
Design
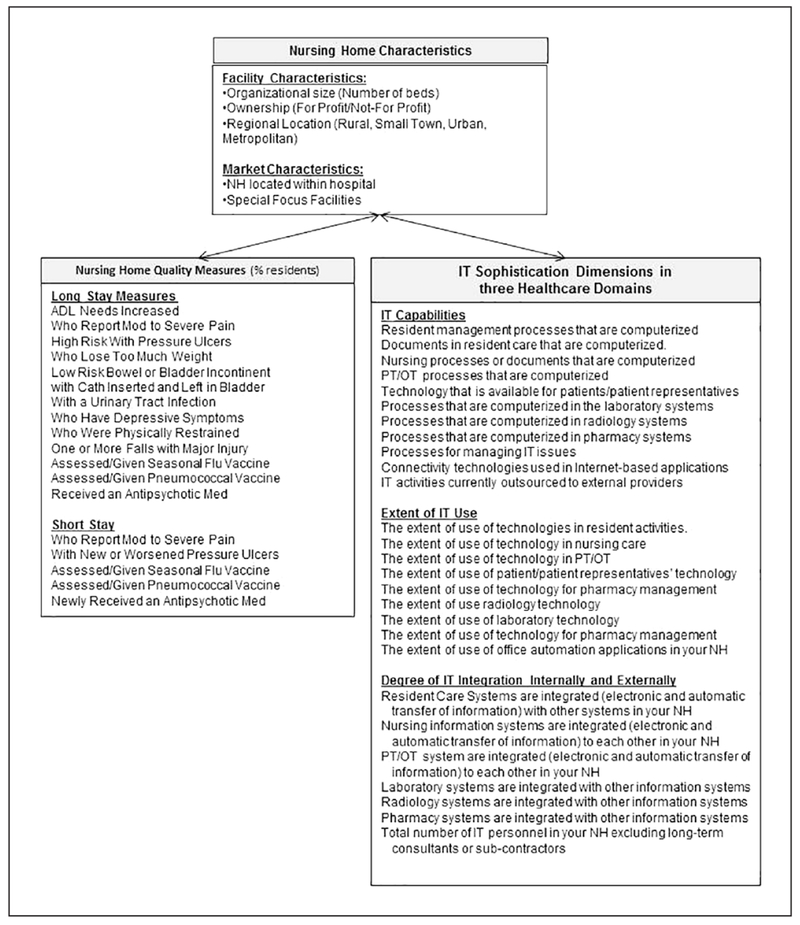
In this article, authors address this evidence gap, by describing results of a study that took place over 3 years (2014–2017) in U.S. NHs. The survey measured trends in NH IT sophistication each year. NH IT Sophistication is a measure defined in three health care domains including resident care, clinical support, and administrative activities. Within each domain, three dimensions of IT sophistication are defined including IT capabilities, extent of IT use, and degree of IT integration with internal/external stakeholders (Alexander & Wakefield, 2009). Therefore, this 3 × 3 (dimensions/domains) model has nine subscales with a minimum of 0 and maximum of 100 for each scale, plus a total IT sophistication score (maximum = 900). A model of independent variables (NH Characteristics, IT Sophistication Dimension and Domain Scores) and dependent variables (NH QMs) was used to guide this study (see Figure 1). The recruitment strategy and analytic plan is illustrated in Figure 2. The university’s institutional review board (Protocol #1209004) approved all protocols.
Figure 1.
A model to test nursing home quality measures and IT sophistication.
Note. IT = information technology; PT/OT = physical/occupational therapist.
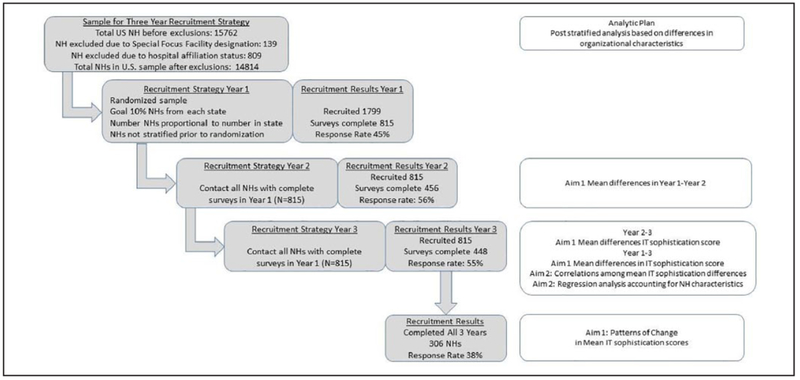
Figure 2.
Recruitment strategy and analysis plan for assessing 3-year trend in IT sophistication.
Note. NH = nursing home; IT = information technology.
Sample
Investigators recruited a randomized NH sample from a national database downloaded from the CMS (2005) NH Compare in September 2013. The database contained information on all 15,623 U.S. NHs. The sample and recruitment strategy for Year 1 (N = 815) of this study is described in (Alexander, Madsen, Miller, et al., 2017). Researchers recruited NH administrators from the same 815 NH facilities in Year 1 to participate in Year 2 and Year 3 of this study using the same recruitment strategy each year. The only difference in recruitment strategy was an increasing compensation amount each year (Year 1 = US$25, Year 2 = US$35, Year 3 = US$40) totaling up to a maximum of $100.00 for three complete surveys.
Survey Measures
The IT sophistication survey was developed and validated by the primary author over several studies since 2007 (Alexander, Madsen, & Wakefield, 2010). The entire survey had 61 questions; of those, 50 questions related to the nine IT sophistication dimensions and domains and 11 questions are descriptive. Within the nine dimensions/domains are 27 content areas used by researchers to describe and trend a full range of IT sophistication measures (see Figure 1; Alexander & Madsen, 2018). Eleven content areas measuring IT capabilities incorporated responses using dichotomous variables. For example, respondents checked IT capabilities supporting electronic physician discharge summaries or order entry, if they were available. Furthermore, researchers measured IT capabilities used in resident care by nurses and physical therapists. Using Likert-type scales, nine content areas specify the extent of IT use and seven content areas specify IT integration internally and externally to each NH. For example, extent of IT use was measured (not available to extensively used) for technologies used in resident care (e.g., telemedicine devices, artificial intelligence, or access to radiologic images). Extent of IT use included measurements of nursing services such as proliferation of personal computing devices that matured from use solely at nursing stations in Year 1 to bedside portable computing devices in Year 3 (e.g., tablets or smart phones). Finally, the survey assessed integration, for example, if resident care systems integrated with other computerized laboratory systems internally in the NH using Likert-type scales (not at all to very much integration). Reliability estimates were assessed by calculating Cronbach’s alpha values for the IT sophistication in three domains, which were resident care (.87-.88), clinical support (.86-.91), and administrative activities (.69-.80; Alexander, Madsen, Miller, et al., 2017). Validity was also assessed with qualitative observations of clinical communication strategies in 16 NHs with diverse levels of IT sophistication (Alexander, Steege, Pasupathy, & Strecker, 2015).
Survey Procedures
Administrators were sent electronic or paper surveys after agreeing to participate. The team conducted at least three follow-up calls per facility at 2-week intervals to increase response rates. Researchers used double-entry procedures entering each paper survey received into separate excel files and then cross-checking files for accuracy.
NH QMs
NH Compare was used to capture independent and dependent variables for the study. All NH facilities in the United States receiving Medicare or Medicaid dollars electronically report QMs through NH Compare. At the time this study started, in 2013, 18 QMs were reported. Thirteen long-stay measures including information about NH residents that are in facilities for longer than 100 days and five short-stay QMs are also included representing residents who are in facilities for less than 100 days (see Figure 1). NHs report QMs quarterly into NH Compare. CMS derives QMs from nursing MDS assessments, which nurses collect upon NH resident admission, when there is a change in NH resident condition, and/or quarterly for each NH resident.
NH Compare also contains facility characteristics about each NH. Investigators collected facility characteristics as independent variables and differences were examined. For instance, researchers collected information about bedsize (<60, 60-120, >120), ownership (for profit, not for profit), and zip code to determine differences in regional variation (rural, small town, urban, and metropolitan). To examine regional variations, investigators use Rural Urban Commuting Area (RUCA) codes as a resource to align zip code information with county population data for each NH location in the United States.
Facility market characteristics were collected from NH Compare and incorporated into the study’s sampling methods. In NH Compare, facilities that identified and reported severe quality of care problems may be classified as special focus facilities. As long as a facility is a special focus facility, they receive special attention by state health departments for their quality problems and often are required to implement special quality improvement projects. Facilities with preexisting quality problems, already focused on quality improvement processes, could confound the effects of NH IT on quality. These facilities were excluded from the sample. In addition, NH facilities that are part of hospitals may have access to resources, such as IT departments, that stand-alone facilities do not typically have access to. For this reason, NH facilities that were part of hospitals were identified and excluded from our sample. Finally, a NH was included only if located in the continental United States, Alaska, and Hawaii.
Analysis
The initial weights in this analysis related to the proportions of homes in a state that responded to the survey. The responding homes typically differed to some degree relative to the numbers of homes with characteristics of bedsize, ownership, and location. Investigators incorporated post-stratification methods to reflect the distribution of homes with these characteristics in the population. Using post-stratified weights, researchers estimated mean scores using percentile ranks for each of the nine IT sophistication dimension/domains and Total IT sophistication. For each pair of years (Year 2-Year 1, Year 3-Year 1, and Year 3-Year 2), we obtained estimates of the mean differences and 99% confidence intervals (CIs) estimates. Investigators considered the change significant if the CI did not contain zero.
In another analysis, incorporating data from facilities completing surveys, researchers assessed the patterns in total IT sophistication that developed over the course of 3 years. A strictly increasing trend in mean total IT sophistication scores overall by year (IT Year 1 < IT Year 2 < IT Year 3) is just one of several emerging patterns. For example, the team found six patterns of interest among individual facilities completing three surveys:
1 = consistent positive increase each year,
2 = positive start, net positive increase after 3 years,
3 = negative start, net positive increase after 3 years,
4 = positive start, net negative loss after 3 years,
5 = negative start, net negative loss after 3 years, and
6 = consistent negative loss over 3 years.
Numbers 1, 2, and 3 have in common the fact that Year 3 total IT sophistication is higher than Year 1 (net increase from Year 1 to Year 3), while 4, 5, and 6 have in common that Year 3 total IT sophistication is lower than Year 1 (net loss Year 1 to Year 3). It was hypothesized that relationships existed between these patterns and NH characteristics. For example, if small homes show different proportions among the patterns than medium or large homes. Rao Scott’s chi-square test was used to examine differences.
Using post-stratified weights, correlations were determined among differences in mean averages of QMs and differences in the nine dimensions/domains and total IT sophistication score. To estimate these relationships, the larger set of facilities completing Year 1 and Year 3 surveys was used (n = 448). Mean averages for each QM were calculated from four quarters of scores reported in NH Compare retrospective to the date the NH administrator completed the survey. Estimated correlations r > .13 (in absolute value) were significant at the .05 level and were explored using regression models; correlations that were not significant were not reported. The QM difference was the dependent variable. The primary independent variables were the IT sophistication differences in each dimension/domain that showed a significant correlation. Additional, independent variables were bedsize, location, ownership. Investigators kept the variables in the model as explanatory variables even if they were not significant. We fit a linear regression model in SAS 9.4 using PROC SURVEYREG with post-stratified weights and state as the strata. PROC SURVEYREG does linear regression analysis for sample survey data, which takes into account designs with stratification, clustering, and unequal weighting. A backward elimination approach was incorporated by dropping IT variables that were not significant at the p < .05 variable with the home variables in model.
Results
Figure 2 provides the numbers of total surveys, contacts, and response rates for the 3 years of the study. A total of 815 administrators completed Year 1 surveys, while 306/815 (38% response rate) completed surveys all 3 years. Every year, surveys were collected from every U.S. state.
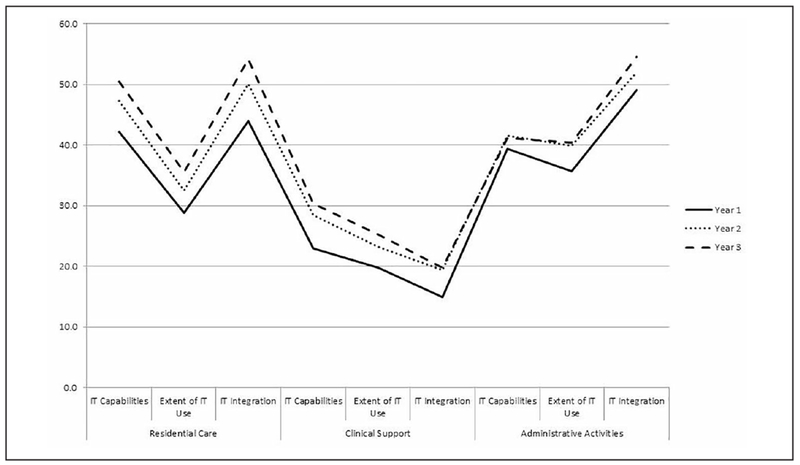
From Figure 3, for each subscale, the total IT sophistication mean scores in each of the nine dimensions/domains for facilities participating in all 3 years are consistently in the order Year 1 < Year 2 < Year 3. Although the means are consistently increasing over 3 years, changes may not be statistically significant. To address this issue, researchers used the 306 homes that returned surveys in all 3 years. For Year 2-Year 1 changes, all were significant EXCEPT IT integration in clinical support and all IT sophistication dimensions (IT capabilities, extent of IT use, and IT integration) within administrative activities. The Year 3-Year 2 change was not as significant, with ONLY IT integration in resident care and administrative activities, and total IT sophistication having positive CIs. When looking at the 2-year change Year 3-Year 1, all changes were significant EXCEPT IT capabilities in administrative activities.
Figure 3.
Post-stratified weighted estimates of mean IT sophistication scales trends over 3 years (N = 306).
Note. IT = information technology.
When we examined the individual facilities patterns of total IT sophistication over 3 years, just over 71% exhibited net positive increase over 3 years. Nearly 19% had a net negative decrease in total IT sophistication, while 10% had a consistently negative pattern of adoption over 3 years. Next, patterns were examined to determine their association with NH characteristics. None of the associations were significant (p = .19, .21, and .59 for bedsize, ownership, and location, respectively).
We used data from Year 3-Year 1 surveys to assess how responding NHs differed to some degree relative to characteristics of bedsize, ownership, and location (e.g., metropolitan or rural; Table 1). NH facilities participating in the survey were typically medium facilities (60-120 beds; 58.5%) with fewer large facilities (>120 beds; 21.2%) participating. The number of small facilities (<60 beds; 20.3%) closely approximated facilities not participating (19.5%). Participating facilities were characteristically for-profit (63.5%) but represented less than those not participating (69.6%). Rural and small town facilities represented 29.9% of participating NH, but the majority (55.1%) was from metropolitan areas. Due to these differences, investigators used post-stratification to re-weight homes to reflect the distribution of NHs with these characteristics in the population. Using post-stratified weights, we looked at the effect of NH characteristics on the mean total IT sophistication score change (Year 3-Year 1). For bedsize, change in mean total IT sophistication score was not significant (p = .16). Although, larger homes had greater increase in mean total IT sophistication score (73.9) than smaller homes (34.7), maximum change possible = 100 (in absolute value). Ownership was not significant (p = .23), for profits had a mean increase of 61.1 in mean total IT sophistication score while nonprofits increased 45.3. Location was also not significant (p = .07); although, there is a suggestion that the estimated mean difference in total IT sophistication in small towns (80.2) improved more than in rural areas (18.3).
Table 1.
Sample NH Characteristics.
| No. Survey | % | Survey | % | Total | |
|---|---|---|---|---|---|
| Bedsize | |||||
| Small NH <60 | 2,964 | 19.5 | 91 | 20.3 | 3,055 |
| Medium NH = 60-120 | 7,790 | 51.2 | 262 | 58.5 | 8,052 |
| Large NH >120 | 4,450 | 29.3 | 95 | 21.2 | 4,545 |
| Ownership | |||||
| For profit—Corporation | 8,773 | 57.7 | 233 | 52.0 | 9,006 |
| For profit—Individual | 545 | 3.6 | 15 | 3.4 | 560 |
| For profit—Limited liability company | 107 | 0.7 | 3 | 0.7 | 110 |
| For profit—Partnership | 1,154 | 7.6 | 33 | 7.4 | 1,187 |
| Government—City | 86 | 0.6 | 0 | 0.0 | 86 |
| Government—City/country | 95 | 0.6 | 2 | 0.5 | 97 |
| Government—County | 459 | 3.0 | 0 | 0.0 | 459 |
| Government—Federal | 6 | 0.0 | 0 | 0.0 | 6 |
| Government—Hospital district | 131 | 0.9 | 0 | 0.0 | 131 |
| Government—State | 149 | 1.0 | 0 | 0.0 | 149 |
| Nonprofit—Church related | 679 | 4.5 | 27 | 6.0 | 706 |
| Nonprofit—Corporation | 2,726 | 17.9 | 130 | 29.0 | 2,856 |
| Nonprofit—Other | 295 | 1.9 | 5 | 1.1 | 300 |
| Location | |||||
| Metropolitan >50,000 | 9,679 | 63.8 | 247 | 55.1 | 9,926 |
| Micropolitan = 10,000-50,000 | 2,245 | 14.8 | 67 | 15.0 | 2,312 |
| Small town = 2,500-9,999 | 1,840 | 12.1 | 75 | 16.7 | 1,915 |
| Rural <2,500 | 1,411 | 9.3 | 59 | 13.2 | 1,470 |
Note. NH = nursing home.
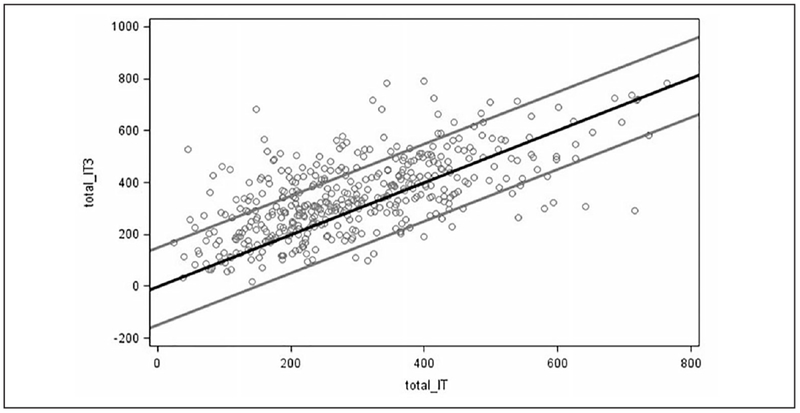
To illustrate mean total IT sophistication score change over time researchers plotted Year 1 (Total_IT) scores against Year 3 scores (Total_IT 3). The result plot diagram (Figure 4) illustrates that more homes improved (points above the central black line) than got worse. In addition, more homes improved “a lot” (by more than 150 points, points above upper limit) than worsened by “a lot” (by more than 150 points, points below lower limit).
Figure 4.
Total IT sophistication differences Year 1-Year 3.
Note. Points above central line Year 3 total IT score higher; points beyond outer reference lines total IT score differ by 150. IT = information technology.
In our post-stratified analysis of correlations between IT sophistication scales and total IT with each QM, correlations r > .13 (absolute value) in magnitude appeared to be significant at the .05 level. Other nonsignificant correlations are not reported. In our analysis, 18 such correlations were significant and are reported (see Table 2), although a magnitude r > .13 is still not terribly large in explanatory value. The most common IT sophistication dimension/domain in the list of 18 is resident care extent of IT use, which shows significant correlation with five different QMs. One of the most interesting QMs of the 18 is the percentage of residents who are low-risk long-stay residents with bowel or bladder incontinence, which shows significant direct correlation with all three resident care IT sophistication scales, one scale in administrative activities, and total IT sophistication. In addition, the percentage of residents with urinary tract infections showed an inverse relation with two scales (IT capabilities, extent of IT use) in resident care. Finally, the percentage of resident receiving antipsychotic/hypnotic medications showed a significant inverse relationship with IT sophistication in every health care domain and total IT sophistication. Significant correlations occurred between total IT sophistication score and three different QMs.
Table 2.
Correlations Between IT Dimension/Domain Scores and Quality Measures.
| Health care domain | IT dimension | Quality measure | pa | ra | R2 |
|---|---|---|---|---|---|
| Resident care | IT capabilities | Low-risk LS bowel or bladder incontinence | .01 | .14 | .02 |
| LS with a urinary tract infection | .00 | −.19 | .03 | ||
| LS assessed/given seasonal flu vaccine | .03 | −.15 | .02 | ||
| Extent of IT use | High-risk LS with pressure ulcers | .00 | −.18 | .03 | |
| Low-risk LS bowel or bladder incontinence | .00 | .19 | .04 | ||
| LS with a urinary tract infection | .02 | −.14 | .02 | ||
| SS with new or worsened pressure ulcers | .00 | −.16 | .02 | ||
| SS newly received an antipsychotic medication | .05 | −.15 | .02 | ||
| IT integration | Low-risk LS bowel or bladder incontinence | .00 | .20 | .04 | |
| Clinical support | IT capabilities | SS who report moderate to severe pain | .00 | −.18 | .03 |
| Extent of IT use | LS who report moderate to severe pain | .00 | −.16 | .03 | |
| Integration | LS received antianxiety/hypnotic medication | .00 | −.17 | .03 | |
| Administrative activities | IT capabilities | Low-risk LS bowel or bladder incontinence | .00 | .20 | .04 |
| IT integration | LS worsened ability to move independently | .01 | .16 | .03 | |
| LS received antianxiety/hypnotic medication | .01 | −.16 | .03 | ||
| Total IT | Low-risk LS bowel or bladder incontinence | .03 | .15 | .02 | |
| LS with a urinary tract infection | .01 | −.15 | .02 | ||
| LS received antianxiety/hypnotic medication | .01 | −.15 | .02 |
Note. IT = information technology; LS = long-stay residents; SS = short-stay residents.
Only values with p value of .05 or less are shown in the table; other values with nonsignificant p values are not shown.
Next, we looked at differences in QMs and differences in IT sophistication scores. A positive correlation means that as IT sophistication gets larger from Year 1 to Year 3, the QM also gets larger from Year 1 to Year 3 (i.e., they move in the same direction). Seven of these correlations are >.15. Only one QM, percentage of short-stay residents assessed/given seasonal flu vaccine, has a significant positive relationship with administrative activities and extent of IT use (r = .15, p = .008). Two other correlations have p < .05. The first had a significant negative correlation between the QM percentage of residents who are low-risk long-stay residents with bowel or bladder incontinence and extent of IT use in administrative activities (r = −.19, p = .03). The second had a significant negative correlation between the QM percentage short-stay residents newly received an antipsychotic medication and extent of IT use in clinical support (r = −.16, p = .05).
A final regression analysis was conducted to determine whether the relationships held up when accounting for characteristics of the NH (see Table 3). In addition, where there were multiple IT scales showing a relationship, including other variables, tests were completed to see whether relationships maintained. There was only one IT sophistication scale with a relationship holding up when accounting for characteristics of the homes, the QM percentage of residents who are low-risk long-stay residents with bowel or bladder incontinence and extent of IT use in administrative activities. As the difference in extent of IT use in administrative activities from Year 1 to Year 3 increased, the change in the QM percentage of low-risk long-stay residents with bowel or bladder incontinence from Year 1 to Year 3 decreased. More specifically, for every 10 units increase in extent of IT use in administrative activities score from Year 1 to Year 3, an expected decrease of 1.3% may occur in the QM percentage of low-risk long-stay residents with bowel or bladder incontinence. Furthermore, the change in QM percentage of long-stay residents who have depressive symptoms and percentage of long-stay residents assessed/given seasonal flu vaccine and relationship with IT did not hold up when accounting for characteristics of the NH. However, a result of interest for percentage of long-stay residents assessed/given seasonal flu vaccine when accounting for NH characteristics, although the relationship with change in extent of IT use in administrative activities did not hold, facilities in micropolitan areas showed a significantly larger (p = .01) change in QM score than facilities in small towns. As the percentage of short-stay residents with newly received antipsychotic medications showed relationships with four IT measures, they were all fit in the same model where none of the IT measures were significant (all p > .05). A stepwise backward selection method was employed, and the IT measures stayed nonsignificant. The measures were also examined alone, where none of their relationships held up when accounting for home characteristics.
Table 3.
Regression Analysis: Relationships Between IT Scales and Quality Measures Accounting for NH Characteristics.
| Variable | % low-risk long-stay residents with bowel or bladder incontinence |
% long-stay residents assessed/given seasonal flu vaccine |
% long-stay residents who have depressive symptoms |
% short-stay residents newly received an antipsychotic medication |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Estimate | SE | p | Estimate | SE | p | Estimate | SE | p | Estimate | SE | p | ||
| Intercept | −8.63 | 2.96 | .00 | −2.65 | 1.91 | .17 | −0.02 | 1.61 | .99 | 1.49 | 0.81 | .07 | ||
| Medium NH = 60-120 | 3.15 | 1.91 | .10 | −0.32 | 1.61 | .84 | 0.73 | 1.44 | .61 | −0.60 | 0.30 | .05* | ||
| Small NH <60 | −3.02 | 4.68 | .52 | −3.02 | 2.43 | .22 | 4.06 | 2.48 | .10 | −1.09 | 0.57 | .06 | ||
| Large NH >120 | 0.00 | 0.00 | . | 0.00 | 0.00 | . | 0.00 | 0.00 | 0.00 | 0.00 | ||||
| For profit | 3.31 | 1.93 | .09 | 0.04 | 1.31 | .97 | 0.77 | 0.97 | .43 | −0.08 | 0.29 | .77 | ||
| Non profit | 0.00 | 0.00 | . | 0.00 | 0.00 | . | 0.00 | 0.00 | 0.00 | 0.00 | ||||
| Metropolitan <50,000 | 2.79 | 2.42 | .25 | 2.03 | 1.57 | .20 | −0.74 | 1.30 | .57 | −1.06 | 0.76 | .16 | ||
| Micropolitan = 10,000-50,000 | 1.81 | 3.07 | .56 | 4.81 | 1.87 | .01* | 0.98 | 1.41 | .49 | −1.08 | 0.90 | .23 | ||
| Rural = 2,500-9,999 | 2.63 | 2.87 | .36 | 0.27 | 3.40 | .94 | −1.12 | 1.15 | .33 | −1.04 | 0.84 | .22 | ||
| Small town <2,500 | 0.00 | 0.00 | . | 0.00 | 0.00 | . | 0.00 | 0.00 | 0.00 | 0.00 | ||||
| Administrative activities extent IT use | −0.13 | 0.05 | .02* | 0.03 | 0.03 | .24 | Clinical Support IT Integration | 0.05 | 0.04 | .25 | Administrative Activities IT Integration | −0.01 | 0.01 | .16 |
| Residential Care IT Use | −0.01 | 0.01 | .56 | |||||||||||
| Clinical Support IT Use | 0.00 | 0.01 | .70 | |||||||||||
| Clinical Support IT | 0.00 | 0.01 | .44 | |||||||||||
| Integration | ||||||||||||||
Note. NH = nursing home; IT = information technology.
In NHs participating in all 3 years of this national study, mean total IT sophistication scores overall are increasing in every dimension/domain. Furthermore, in facilities that have only partial participation rates (2 or less years), there are also increasing trends in mean IT sophistication rates. Trend rates do not appear to have statistically significant change in each dimension/domain every year, but do reach statistically significant change in eight out of nine of the subscales used in this evaluation from Year 1 to Year 3. These changes are consistent with recent reports by the ONC that some capabilities of health IT like EHR and HIE use are increasing in skilled nursing facilities (Alvarado, Zook, & Henry, 2017). In addition, this same report indicates that there is wide variation of IT adoption based on facility characteristics similar to those evaluated in this sample. Increasing trends and wide variation in adoption patterns demonstrate the importance for sustained efforts to monitor and report use of IT in these health sectors.
Overall growth trends are encouraging; however, some individual facility trends are not so encouraging. For example, nearly 30% of administrators reported a net negative decrease, with 10% of administrators reporting consistent negative decreases in IT sophistication over 3 years. These fluctuations in IT sophistication were not particularly associated with any facility characteristic but appeared to occur broadly regardless of the characteristics. Net decline in IT sophistication means that administrators reported reductions in some or all of a facility’s IT capabilities, extent of IT use, or degree of IT integration over 3 years. These findings are consistent with earlier research analyzing change in IT sophistication, where IT in clinical support areas including pharmacy, radiology, and laboratory appeared to have the most fluctuation (Alexander, Madsen & Newton, 2017). In fact, some administrators reported wide variation between consecutive years (Year 2-Year 1), moving from IT sophistication scores of 100 (maximum) to 0 (minimum) in a single year (Alexander et al., 2017). Exploring these variations in IT adoption, consistently, whether net increase or decrease, would be a worthwhile endeavor toward understanding decisions about IT adoption, influencers that are leading to reduced adoption (e.g., poor usability or interoperability), and quality and safety impacts for facility leaders, staff, and residents experiencing large amounts of system change (Alexander, Madsen & Newton, 2017).
There appears to be a significant amount of correlation that is detectable between increasing IT sophistication levels and QMs reported by the same facilities. After regression using backward elimination, we found that few of these correlations held up when including NH characteristics where multiple IT scales show relationships. However, one finding does indicate that as extent of IT use in administrative activities increases, the percentage of residents with bowel or bladder incontinence decreases. With the current design, investigators are not able to determine what influences IT sophistication may have on this QM directly. Hypothetically, increasing extent of IT use in administrative activities may provide better administrative oversight of clinical processes and risk management that might be useful for identifying residents at risk of bowel or bladder incontinence, thus providing notification that earlier interventions are needed such as toileting to prevent the condition. There is a need to test these theories and others with future large-scale national research studies using novel designs that incorporate more critical variables to understand relationships between quality measurement and trends in adoption of innovative IT systems in these settings.
Implications
It is crucial that we continuously assess policy drivers that are influencing technology sophistication in all health care sectors, including NHs. One way to assess policy drivers is to trend technology sophistication consistently using models that identify IT capabilities, the extent of IT use, and degree of IT integration in NHs to demonstrate where IT innovations are occurring in practice. Furthermore, consistent reports of NH IT sophistication trends could inform numerous stakeholders about existing IT infrastructures in NH settings. For example, regulatory agencies should incorporate knowledge of IT infrastructure trends (e.g., adoption of HIE or EHR) into their annual assessments of facilities’ quality and safety of care delivery. In many cases, regulatory agencies incorporate assessments of system processes that may be impacted by IT sophistication (e.g., electronic clinical documentation, decision support with risk identification, and electronic forms of communication), so there is a compelling argument that NH surveyors conducting assessments require knowledge of current IT system infrastructure to fully understand facilities’ compliance with regulations. For these reasons and others, establishing baseline and ongoing trends in NH IT sophistication provides new information about these care delivery systems that should be made consistently available on an annual basis.
Limitations
Defining the impact of IT sophistication on QMs is a difficult process to undertake. One reason is that other endogenous factors, which are present in an active health care system, are hard to control for to narrow the true effects of IT on quality of care. An example might be the NH workforce who is delivering resident care. Historically, the NH workforce has limited clinical training composed of mostly licensed practical nurses and certified nurse assistants and experience high turnover, which can also directly impact QMs (Castle, Engberb, Anderson, & Men, 2007; Lerner, Johantgen, Trinkoff, Storr, & Han, 2014). Another example is the significant gap between processes of care such as documentation of care and care that residents receive. For example, some studies have shown consistent bias in the direction of documentation that reflects higher care quality relative to care processes provided by staff (Schnelle, Bates-Jenson, Chu, & Simmons, 2004). Studies like these suggest that increased IT sophistication could lead to improvements in documentation quality and overall QMs without a clinically meaningful impact on quality of care provision. We recognize that a failure to account for endogeneity in our study can have important consequences, including biased coefficient estimates and faulty conclusions about theoretical propositions we have made about the influence of IT sophistication on QMs (Hamilton & Nickerson, 2003). To address this problem, we have incorporated critical variables into our design to help us to overcome possible variable bias. However, we also realize that some critical variables were not included (i.e., staffing, five-star ratings) primarily because these measures were being revised at some point during the longitudinal study. In future research, it will be important to include these variables in robust analyses to understand the influence of IT on quality in NHs.
Conclusion
Findings illustrated here show NH IT adoption is increasing and there does appear to be some evidence of positive impact on QMs as IT sophistication increases over time. However, there are still deficits in our understanding of the impact of IT. For example, why would nearly 30% of NH administrators participating over 3 years have a net negative decrease in IT sophistication? What is the impact of this net negative decrease on staff, residents, and quality of care? Health care researchers can learn from studies like these, which demonstrate, to some extent, how NH administrators are responding over time to influential drivers of care delivery, such as NH IT innovation.
Acknowledgments
The authors would like to thank Keely Wise, Project Coordinator, who help keep us all organized, moving forward through this project, and on target to accomplish goals. The authors wish to thank Matt Newton, Casey Jones, Allie Holms, and Melissa Schaumberg for their recruitment efforts during the project. Furthermore, this study would not be possible without the contributions of many nursing home leaders across the country who were consistent partners in our research.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by Grant No. R01HS022497 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Footnotes
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The corresponding author is the principal founder of TechNHOlytics, LLC a company that provides nursing home information technology analytics.
References
- Abramson EL, McGinnis S, Moore J, Kaushal R, & HITEC Investigators. (2014). A statewide assessment of electronic health record adoption and health information exchange among nursing homes. Health Services Research, 49, 361–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander GL, & Madsen D (2018). A national report of nursing home quality and information technology: Two-year trends. Journal of Nursing Care Quality, 33, 200–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander GL, Madsen R, & Newton M (2017). Analyzing change in nursing home information technology sophistication. Journal of Gerontological Nursing, 43, 17–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander GL, Madsen R, & Wakefield DS (2010). A regional assessment of information technology sophistication in Missouri nursing homes. Policy, Politics & Nursing Practice, 11, 214–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander GL, Madsen RW, Miller EL, Schaumber MK, Holm AE, Alexander RL, … Gugerty B. (2017). A national report of nursing home information technology: Year 1 results. Journal of the American Medical Informatics Association, 24, 67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander GL, Steege L, Pasupathy K, & Strecker EB (2015). Case studies of IT sophistication in nursing homes: A mixed method approach to examine communication strategies about pressure ulcer prevention practices. International Journal of Industrial Engineering, 49, 156–166. [Google Scholar]
- Alexander GL, & Wakefield DS (2009). Information technology sophistication in nursing homes. Journal of the American Medical Directors Association, 10, 398–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarado CS, Zook K, & Henry J (2017). Electronic health record adoption and interoperability among U.S. skilled nursing facilities in 2016. Retrieved from https://www.healthit.gov/sites/default/files/electronic-health-record-adoption-and-interoperability-among-u.s.-skilled-nursing-facilities-in-2016.pdf
- American Reinvestment and Recovery Act Title XIII Health Information Technology (HITECH) Act, 111 U.S. Congress (2009).
- Balanced Budget Act of 1997, Public Law 105-33, 111 Stat. 251 (1997).
- Blumenthal D (2010). Launching HITECH. New England Journal of Medicine, 362, 382–385. [DOI] [PubMed] [Google Scholar]
- Carretero S (2015). Technology-enabled services for older people living at home independently: Lessons for public long-term care authorities in the EU member states. Retrieved from http://publications.jrc.ec.europa.eu/repository/bitstream/JRC96022/lfna27256enn.pdf
- Castle NG, Engberb J, Anderson R, & Men A (2007). Job satisfaction of nurse aides in nursing homes: Intent to leave and turnover. The Gerontologist, 47, 193–204. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. (2005). Centers for Medicare and Medicaid nursing home compare. Retrieved from http://www.medicare.gov
- Centers for Medicare & Medicaid Services. (2015). Centers for Medicare and Medicaid the Medicare access & chip reauthorization act of 2015: Path to value. Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-LAN-PPT.pdf Accessed 2018-08-27
- Food and Drug Administration Safety and Innovation Act, Public Law 112-144 C.F.R. (2012).
- Hamilton BH, & Nickerson JA (2003). Correcting for endogeneity in strategic management research. Strategic Organization, 1, 51–78. [Google Scholar]
- Ko M, Wagner L, & Spetz J (2018). Nursing home implementation of health information technology: Review of the literature finds inadequate investment in preparation, infrastructure, and training. INQUIRY: The Journal of Health Care Organization, Provision, and Financing, Jan-Dec 55, 1–10, doi: 10.1177/0046958018778902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerner NB, Johantgen M, Trinkoff AM, Storr CL, & Han K (2014). Are nursing home survey deficiencies higher in facilities with greater staff turnover. Journal of the American Medical Directors Association, 15, 102–107. [DOI] [PubMed] [Google Scholar]
- Office of the National Coordinator for Health Information Technology. (2015). Office of the national coordinator for health information technology (ONC) federal health IT strategic plan 2015-2020. Retrieved from https://www.healthit.gov/sites/default/files/9-5-federalhealthitstratplanfinal_0.pdf
- Office of the National Coordinator for Health Information Technology. (2016). Office of the national coordinator for health information technology examining the HITECH Era and the future of health IT. Retrieved from https://www.healthit.gov/sites/default/files/2016_report_to_congress_on_healthit_progress.pdf
- Rantz MJ, Hicks L, Petroski GF, Madsen RW, Alexander GL, Galambos C, … Greenwald L. (2010). Cost, staffing, and quality impact of bedside electronic medical record (EMR) in nursing homes. Journal of the American Medical Directors Association, 11, 485–493. [DOI] [PubMed] [Google Scholar]
- Resnick HE, Manard BB, Stone RI, & Alwan M (2009). Use of electronic information systems in nursing homes: United States, 2004. Journal of the American Medical Informatics Association, 16, 179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnelle JF, Bates-Jenson BM, Chu L, & Simmons SF (2004). Accuracy of nursing home medical record information about care-process delivery: Implications for staff management and improvement. Journal of the American Geriatrics Society, 52, 1378–1383. [DOI] [PubMed] [Google Scholar]
- Scott-Kruse C, Mileski M, Vijaykumar AG, Viswanathan SV, Suskandla U, & Chidhambaram Y (2017). Impact of electronic health records on long-term care facilities: Systematic review. JMIR Medical Informatics, 5(3), e35. doi: 10.2196/medinform.7958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21 st Century Cures Act, Public Law 114-255 130 STAT 1033 (2016).
- U.S. Congress Omnibus Budget Reconciliation Act of 1987, Public Law 100-203 101 STAT 1330 (1987).
- U.S. Department of Health & Human Services. (2016). Health IT regulations and legislation. Office of the National Coordinator; Retrieved from https://www.healthit.gov/policy-researchers-implementers/health-it-legislation [Google Scholar]
- Vest JR, Jung HY, Wiley K, Kooreman H, Pettit L, & Unruh MA (2018). Adoption of Health Information Technology Among US Nursing Facilities. Journal of the American Medical Directors Association. Advance online publication 2018, Dec. 19, 10.1016/j.jamda.2018.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]