Abstract
Objectives:
Assess outcomes of a clinical cohort of patients with endometrioid endometrial cancer (EEC) harboring somatic POLE exonuclease domain mutations (EDMs).
Methods:
Patients were consented to a protocol of tumor-normal massively parallel sequencing of 410–468 cancer related genes. EECs subjected to sequencing from 2014 to 2018 were reviewed. Tumors with somatic POLE EDMs were identified. EECs were assessed for microsatellite instability (MSI) using MSIsensor and immunohistochemical analysis for mismatch repair (MMR) proteins.
Results:
Of the 451 EECs sequenced, 23 had a POLE EDM (5%): 20 primary and 3 recurrent tumors sequenced. Nineteen cases (83%) were stage I/II and 4 (17%) were stages III/IV. Thirteen EECs (57%) were of FIGO grades 1/2, 10 (43%) grade 3. All patients were treated with surgery and 17 (89%) received adjuvant therapy. Five (22%) demonstrated loss of DNA MMR protein expression, none were due to Lynch syndrome. MSIsensor scores were conclusive for 21 samples: 19 were microsatellite stable and 2 MSI-high. After median follow-up of 30 months, 4/23 (17%) developed recurrences: 3 with initial grade 3 stage I and 1 with grade 1 stage III disease. One patient with grade 2 stage IV EEC had progressive disease after treatment.
Conclusions:
Patients with POLE EDM EEC have been shown to have a favorable prognosis. In this real-world cohort of patients, de novo metastatic disease and recurrences in initially uterine-confined cases were observed. Further research is warranted before incorporating the presence of POLE EDM into decision-making regarding adjuvant therapy.
Keywords: POLE exonuclease domain, POLE EDM, Recurrent endometrioid endometrial adenocarcinoma
INTRODUCTION
Endometrial cancer is the most common gynecologic malignancy in the United States, affecting nearly 62,000 women annually [1]. Prognosis varies based on the histologic grade and surgical stage of the disease at time of diagnosis. Low-grade (Fédération Internationale de Gynécologie et d’Obstétrique, FIGO grade 1 or 2), endometrioid histology, and early pathologic stage portend superior prognosis compared to high-grade (grade 3) or advanced pathologic stage disease. While grade and stage remain paramount to prognosis, in 2013, The Cancer Genome Atlas (TCGA) identified four distinct molecular subtypes in endometrioid endometrial cancer (EEC), which have since been shown to be predictive of survival [2]. These include the POLE (ultramutated) subtype, the MSI (hypermutated) subtype of microsatellite unstable tumors, copy-number low (endometrioid) subtype characterized by CTNNB1 mutations, and the copy-number high (serous-like) subtype with high levels of copy number alterations and recurrent TP53 mutations.
The POLE (ultramutated) subtype is characterized by polymerase epsilon (POLE) exonuclease domain mutations (EDMs) and very high mutation rates. POLE encodes the catalytic subunit of the DNA polymerase epsilon and contains both the catalytic active site and the proofreading exonuclease domain [3]. POLE is involved in DNA replication, and increases replication fidelity to ensure low mutation rates in cells undergoing replication. Dysfunction in POLE is linked to genome instability and cancer, including colorectal and endometrial cancer, resulting in an “ultramutated” phenotype [4, 5].
POLE EDMs are present in about 5–8% of all sporadic endometrial cancers and in up to 10–20% of FIGO grade 3 EECs [6–8]. Despite the high number of mutations observed in POLE EDM EECs, patients with these tumors have been described to have excellent clinical outcomes [6, 9, 10]. In the selected EECs included in TCGA, 17 patients with stage I-III disease had POLE ED-mutated tumors, none had recurrent disease after a median follow-up of 32 months (range, 1–95) [2]. Further, sequencing data from the PORTEC-1 and −2 trials (n=788), of adjuvant radiation therapy in patients with stage I intermediate risk and I/II high-to-intermediate risk, respectively, reported pathogenic POLE EDM in 48 (6%) patients and noted that only 3 patients with a POLE ED-mutant tumor had a distant recurrence, while no patients developed locoregional recurrence [6]. Overall, patients with a POLE EDM EECs had fewer recurrences and cancer-associated deaths, and this effect was particularly pronounced among those with high-grade tumors [6].
As recurrence and death rates among patients with POLE mutated tumors have been reported to be low, it has been suggested that patients with early stage, high-grade POLE mutated EECs, may not require adjuvant therapy following surgery and may not need intensive long-term surveillance [6, 9, 11].
Here, we aim to assess the clinical outcomes in a clinical cohort of patients with POLE EDM EECs. In addition, we sought to define the MSI status and mutational signatures of EECs with POLE EDMs.
METHODS
Patient selection
This study was approved by the Memorial Sloan Kettering Cancer Center (MSKCC) Institutional Review Board (IRB). Patients with endometrial cancer consented to an IRB-approved protocol of tumor-normal massively parallel sequencing of 410–468 cancer-related genes (Integrated Mutation Profiling of Actionable Cancer Targets, MSK-IMPACT) [12, 13]. From 2016 onward, all patients with a new diagnosis of EEC were offered enrollment onto the MSK-IMPACT protocol at their preoperative clinic visit. From May 2015 onward, patients were also offered optional secondary germline analysis of 76 genes initially, and subsequently 88 genes, included in the MSK-IMPACT panel [14]. These are the genes that have been associated with hereditary cancer predisposition per American College of Medical Genetics (ACMG) guideline [15] [14].
The database was queried for all EECs sequenced between 2014 and 2018. EECs with somatic mutations in the POLE exonuclease domain (residues 268–471) were identified. The mutations of interest have been described as hotspots or pathogenic mutations, and those that are recurrent and/or associated with an ultramutated phenotype, and include p.A456P, p.V411L, p.P286R, p.F367V, and p.P436R mutations [12, 16–19].
Microsatellite instability/mismatch repair deficiency analysis
The presence of microsatellite instability (MSI) was defined in the paired tumor-normal sequencing data of all EECs using MSIsensor, as previously described, and samples with an MSIsensor score ≥10 were considered MSI-high [19–21]. In addition, all EECs included in this study were subjected to immunohistochemical (IHC) analysis for the DNA mismatch repair (MMR) proteins MLH1, MSH2, PMS2 and MSH6, as previously described [20]. DNA MMR protein expression was defined as abnormal if there was complete absence from all tumor cell nuclei [22]. When loss of MLH1 and PMS2 proteins were observed, the sample was subjected to MLH1 promoter methylation analysis [23].
Mutational signature analysis
Mutational signatures described by Alexandrov et al., were inferred from all somatic single nucleotide variants (SNVs) in a given EEC using deconstructSigs at default parameters, as previously described [19, 24, 25].
Statistical analysis
Patient data including age, tumor grade, pathologic stage, and treatment information were abstracted from electronic medical records. Time to recurrence was defined as time between pathologic diagnosis of primary tumor until pathologic diagnosis of recurrence, and was calculated using the Kaplan-Meier method. Descriptive statistics were performed using SPSS software, version 25.0 (IBM, Armonk, NY).
RESULTS
Clinico-pathologic characteristics and outcome of EECs with POLE EDMs
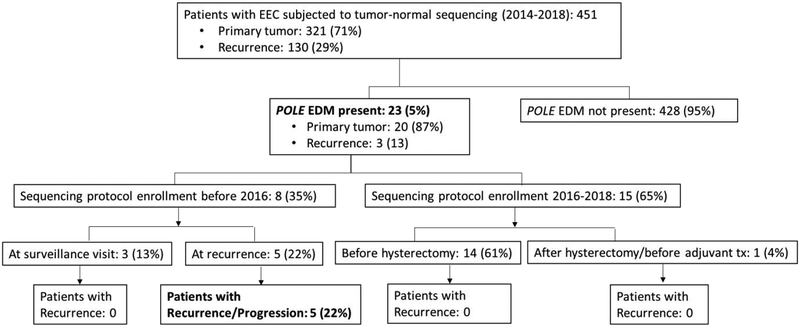
From 2014–2018, 451 EECs were subjected to clinical MSK-IMPACT sequencing of cancer-related genes (Figure 1). The majority of EECs (n=321, 71%) sequenced were primary tumors. Of the 451 EECs, 23 (5%) harbored a somatic POLE EDM; these patients are presented here.
Figure 1. Selection of cases for study inclusion.
Tumors of patients with EEC were subjected to tumor-normal sequencing between 2014–2018 and those with a POLE EDM mutation were selected for inclusion in this report. Those patients that were enrolled onto the tumor sequencing protocol before 2016 were enrolled either during their surveillance visit or at time of recurrence. Those enrolled onto the sequencing protocol after 2016 were enrolled at their initial pre-operative visit or during their first appointment at MSKCC. There were 4 patients with a cancer recurrence and 1 with cancer progression immediately after completion of treatment that were identified in this cohort. EEC, endometrioid endometrial cancer; Tx, treatment; EDM, exonuclease domain.
Of the 23 patients included in this study, 20 received care at MSKCC from the time of their diagnosis, 1 transferred care to MSKCC following surgery, and 2 presented for treatment at time of cancer recurrence. Fifteen (65%) patients had surgery in 2016 or later and 8 (34%) were diagnosed before 2016 (Figure 1). Fourteen of the 16 patients in the 2016–2018 cohort were offered tumor sequencing at the time of their initial preoperative clinic visit (1 patient transferred care to MSKCC following hysterectomy and was offered enrollment at that time). The 8 patients in the pre-2016 cohort had the following breakdown for enrollment onto the MSK-IMPACT protocol: 3 patients were offered enrollment during a surveillance visit (none had a cancer recurrence) and 5 were offered enrollment at the time of cancer recurrence/progression (of these, 2 had their primary tumor sequenced and 3 had a metastasis subjected to sequencing). Altogether, 20 patients (87%) had germline multigene panel testing and none harbored a germline POLE mutation, or any other germline mutation in genes included on the panel.
Of the 23 patients with POLE EDM included in this study, the median age at endometrial cancer diagnosis was 54 years (range, 40–76) (Table 1). Nineteen patients (83%) had stage I disease at time of diagnosis, 2 (9%) had stage III and 2 (9%) had stage IV. The FIGO grade of the POLE EDM EECs was evenly distributed, with 6 (26%) patients having grade 1, 7 (30%) grade 2, and 10 (44%) grade 3 EECs. Among the 10 patients with grade 3 POLE-mutant EECs, 9 were diagnosed with stage I, and 1 with stage IV disease.
Table 1.
Clinical characteristic of patients with POLE-mutant endometrioid endometrial adenocarcinomas.
| Clinical characteristics |
POLE-mutant EECs (n=23) n (%) |
|---|---|
| Age at diagnosis; years (range) | 54 (43–76) |
| Stage at diagnosis | |
| I | 19 (83) |
| II | 0 (0) |
| III | 2 (9) |
| IV | 2 (9) |
| Histologic grade | |
| 1 | 6 (26) |
| 2 | 7 (30) |
| 3 | 10 (44) |
| Adjuvant therapy | |
| No adjuvant treatment | 6 (26) |
| Radiation | 9 (39) |
| Chemotherapy | 2 (9) |
| Radiation and chemotherapy | 5 (22) |
| Hormonal treatment | 1 (4) |
| Metastatic disease | |
| De novo stage IV | 2 (9) |
| Recurred | 4 (17) |
| Progression of disease after initial treatment | 1 (4) |
| Did not recur | 17 (74) |
| Status at last follow up | |
| No evidence of disease | 20 (87) |
| Alive with disease | 2 (9) |
| Deceased | 1(4) |
EEC, endometrioid endometrial cancer
All patients received surgery as their primary treatment. The majority received adjuvant treatment: 17 (89%) patients had adjuvant radiation therapy (RT) and/or chemotherapy, and 1 patient (with grade 1, stage IA disease) initiated hormonal treatment with megestrol acetate. Of note, patient PE20 had uterine confined disease and a morphologically distinct synchronous stage IB grade 3 endometrioid ovarian carcinoma. Therefore, she received both vaginal brachytherapy and chemotherapy as adjuvant therapy. She had an isolated rectal recurrence that was resected and was pathologically confirmed as consistent with a recurrence of her primary endometrial cancer. Of those who were treated with RT, 11 had intravaginal brachytherapy (IVRT) and 2 had whole pelvic radiation (WPRT). Of interest, 8 of 9 (89%) patients with grade 3 stage I disease received adjuvant therapy (5 patients received IVRT only and 3 received IVRT and chemotherapy). The ninth patient declined treatment.
After a median follow-up of 30 months (range, 2–193), 4 patients had a cancer recurrence and 1 had progressive disease (Table 2). Median time to recurrence was 21 months (95% Confidence Interval, 18.9–23.1). Patients with a recurrence were as follows: 3 had grade 3 stage I disease (of 9 total, 33%) and 1 had grade 1 stage III disease (of 1 total, 100%). An additional patient with grade 2 stage IV disease had progression of disease after completion of initial treatment (Table 2). Of the 4 recurrences, 3 were with distant metastases only. One patient (initially diagnosed with grade 1 stage III disease) had both vaginal and distant metastases. Of interest, 2 patients had brain metastases: patient PE2 was initially diagnosed with stage I disease and then recurred with brain metastases, and patient PE9 was diagnosed with stage IV disease and subsequently developed brain metastases. Recurrences in the cohort were treated with a combination of surgery, chemotherapy, and radiation therapy, as applicable. At last follow-up, 22 of 23 patients were alive, 2 with active disease. One patient (case PE9) was deceased, after an overall survival of 33 months.
Table 2.
Clinical characteristics of patients with recurrent EEC.
| Case | Stage | Grade | Adjuvant treatment | Time to recurrence (m) | Recurrence location | Length of FU (m) | Status at last FU |
|---|---|---|---|---|---|---|---|
| PE20 | IA | 3 | IVRT & chemo | 146 | Rectum | 165 | NED |
| PE2 | IB | 3 | IVRT | 20 | Brain | 42 | NED |
| PE18 | IB | 3 | IVRT | 21 | Chest wall | 88 | NED |
| PE17 | III | 1 | IVRT | 35 | Vagina, liver | 165 | AWD |
| PE9 | IV | 2 | Chemo | Progressed | Breast, then brain | 33 | Deceased |
IVRT, Intravaginal radiation therapy; Chemo, chemotherapy; NED, No Evidence of disease; AWD, Alive with disease; FU, Follow up; m, months; LND, lymphadenopathy
One patient (case PE2) was treated with immunotherapy. This patient was diagnosed with grade 3 stage I disease and received adjuvant IVRT following surgery. Her tumor was noted to have POLE p.F367V and p.P476S mutations, to be MSI-indeterminate, and to have retained MMR proteins. Twenty months following completion of treatment, she was diagnosed with an isolated brain metastasis and was treated with surgical resection followed by stereotactic radiation therapy. Twelve months later she was noted to have a new isolated brain lesion, which was again treated with stereotactic radiation followed by initiation of checkpoint inhibitor antibody, pembrolizumab. As of this report, she has been on treatment with pembrolizumab for 4 months, with no evidence of disease and no treatment-related side effects.
Microsatellite instability and mutational signatures of POLE EDM EECs
The EECs harboring POLE EDMs had a median of 262 somatic mutations (range, 51–757) and a median of 219 non-synonymous mutations (range, 47–582) in the 410–468 genes assessed (Table 3). Of the 23 POLE-mutant EECs included in this study, 19 (83%) were microsatellite stable (MSS) and 2 (9%) were MSI-high (MSI-H); 2 (9%) were MSI-indeterminate. Immunohistochemical analysis revealed that 5 (22%) EECs displayed loss of DNA MMR protein expression (Table 3). One case (PE11) showed PMS2/MLH1 loss of expression and was noted to be MLH1 hypermethylated. Three cases (PE16, PE18 primary, PE21) lacked MSH6 protein expression, and on genomic profiling were shown to harbor dual somatic MSH6 gene mutations, accounting for the protein loss. One case (PE10) showed MSH6 loss of expression, but no germline or somatic MMR gene mutations were identified. Of the 20 patients who underwent germline mutation testing, none harbored DNA MMR germline mutations/Lynch syndrome.
Table 3.
Genomic characteristics of POLE-mutated endometrioid endometrial adenocarcinomas.
| Genomic characteristic |
POLE mutant EECs (n=23) n (%) |
|---|---|
| Median number total mutations (range) | 262 (51–757) |
| Median number non-synonymous mutations (range) | 219 (47–582) |
| Exonuclease domain mutation | |
| p.V411L | 9 (41) |
| p.P286R | 8 (36) |
| p.A456P | 4 (18) |
| p.F367V and p.P476S (1 sample) | 1 (5) |
| p.P436R | 1 (5) |
| MSIsensor score | |
| MSI-high | 2 (9) |
| MSI-indeterminate | 2 (9) |
| MSS | 19 (83) |
| DNA Mismatch repair protein IHC | |
| Proficient | 18 (78) |
| Deficient | 5 (22) |
| MLH1 hypermethylation | 1 |
| MSH6 somatic mutation* | 3 |
| Unexplained** | 1 |
| Germline mutation | |
| None identified | 20(87) |
| No germline testing | 3 (13) |
All 3 samples had dual somatic MSH6 mutation.
No germline or somatic MMR gene mutation to explain IHC MMR protein deficiency.
MSI, microsatellite; MSI-high, microsatellite unstable; MSS, microsatellite stable; IHC, immunohistochemistry
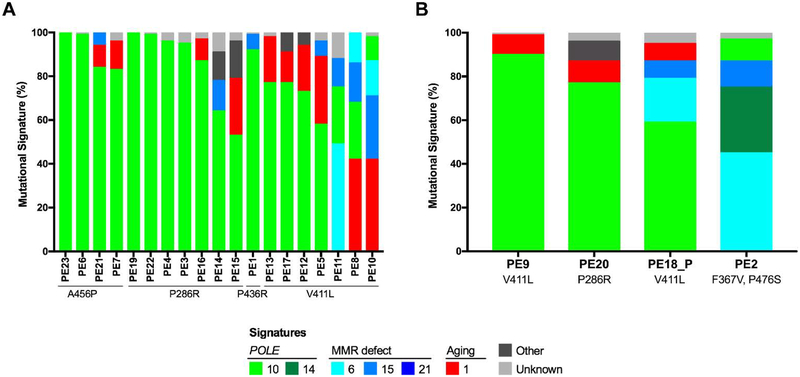
The somatic mutations present in a given tumor are the consequence of multiple mutational processes, including exposure to mutagens or DNA repair defects, which generate unique combinations of mutation types, the so-called “mutational signatures” [24]. We defined the mutational signatures for all POLE-mutant EECs included in this study (Figure 2). Consistent with previous reports, the percentage of the POLE-associated mutational signature 10 present in a given EEC varied according to the specific POLE EDM [19]. All EECs with a POLE p.A456P, p.P286R, or p.P436R somatic mutation harbored a dominant mutational signature 10 associated with POLE EDM mutations. In contrast, of the 9 EECs with a p.V411L mutation, only 6 (67%) harbored a dominant POLE mutational signature 10. The remaining 3, p.V411L-mutant EECs harbored dominant mutational signature 1 associated with aging (n=2) or a dominant mutational signature 6 associated with DNA MMR defects/MSI (n=1). The case with a dominant mutational signature 6 (case PE11) was noted to be MSI-H, and to have PMS2/MLH1 protein deficiency (due to MLH1 hypermethylation). EEC case PE2, with p.F367V and p.P476S somatic POLE mutations, harbored a dominant mutational signature 6 associated with DNA MMR defects. No clear differences in the distribution of specific POLE mutations or mutational signatures between EECs that did not develop recurrences (Figure 2A) and that did have a recurrence (Figure 2B) were observed.
Figure 2. Mutational signatures of endometrioid endometrial cancers with POLE exonuclease domain mutations.
A. Mutational signatures of endometrioid endometrial cancers (EECs) from patients that did not develop a recurrence. B. Mutational signatures of EECs from patients that did develop a recurrence. Cases are sorted by their specific POLE exonuclease mutation (EDM) and by their proportion of POLE-associated mutational signature 10. MMR, mismatch repair.
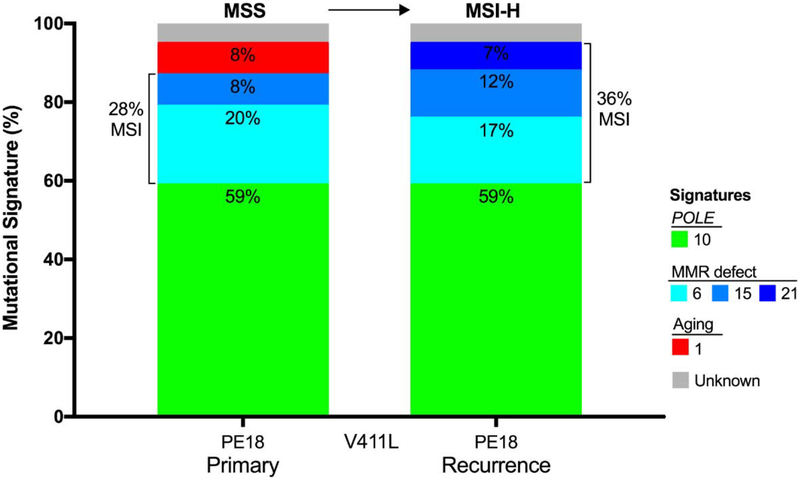
For 1 patient (PE18), both the primary and matched recurrent tumor were subjected to MSK-IMPACT sequencing (Figure 3). This was a 57-year-old with FIGO grade 3, stage IB EEC diagnosed in 2011. The primary tumor was noted to have a POLE p.V411L hotspot mutation, to be MSS by MSIsensor, and to have absence of expression of MSH6 on immunohistochemical analysis (likely related to presence of dual somatic MSH6 gene mutations). The mutational signatures present in this primary EEC were a dominant POLE signature 10 (59%), and DNA MMR signatures 6 and 15 (28%). The patient received post-operative adjuvant therapy with intravaginal brachytherapy and recurred 21 months after completing treatment. The recurrence was multi-focal, including intra-abdominal and thoracic implants. This recurrent tumor specimen also had a p.V411L POLE hotspot mutation. Interestingly, while the recurrent EEC displayed a dominant POLE mutational signature 10 (59%) akin to the primary tumor, there was an increase in the DNA MMR-associated signatures 6 and 15 (36% MMR), and the recurrent tumor specimen was MSI-H by MSIsensor (immunohistochemistry analysis for expression of MMR protein was not performed). The patient was treated with chemotherapy and RT to the chest lesion. Following completion of treatment, she had an additional solitary chest recurrence 9 months later, which was treated with surgery. As of last follow-up, 88-months since diagnosis, she is without evidence of disease.
Figure 3. Mutational signatures and microsatellite instability status in the primary and matched metastatic POLE-mutant endometrioid endometrial cancer (PE18).
Mutational signatures of the primary p.V411L POLE-mutant endometrioid endometrial cancer (EEC) from patient PE18 (left) and of the matched distant chest wall metastasis (right). Mutational signatures are color-coded according to the legend. The DNA microsatellite instability status is displayed on top of each bar. MMR, mismatch repair; MSI-H, microsatellite unstable; MSS, microsatellite stable.
DISCUSSION
We present the clinical outcomes of a real-world cohort of 23 patients with a POLE EDM mutated EEC. POLE EDMs are found in a subset of preferentially high-grade EECs and have been shown to be associated with improved clinical outcomes, particularly among patients with high-grade tumors [10].
In their initial analysis of all patients with EEC, Billingsley et al., did not identify a survival advantage for the 30 patients with a POLE EDM EECs (of 544 patients with EEC), but a subanalysis of the 72 patients with a grade 3 EEC did note that the 7 patients with a POLE EDM tumor had a lower risk of recurrence and death than those with POLE wild-type tumors [7, 9]. McConechy and colleagues performed a pooled multivariate analysis of five studies of grade 3 tumors and demonstrated improved progression-free survival for patients with tumors harboring a POLE EDM, although there was no significant difference in disease-free or overall survival compared to patients with POLE wild-type endometrial cancers [26]. Meng et al., assessed patients with grade 3 EECs by combining the TCGA cohort (49 tumors) with a locally collected series (53 tumors): there were 16 patients (15%) with grade 3 tumors harboring a POLE EDM [10]. After a median follow-up of 33 months, none of the patients with a POLE-mutant EEC had a cancer recurrence, compared to 25 recurrences among the 86 patients with POLE wild-type EEC. In this cohort, one-quarter of the patients with POLE-mutated tumors received adjuvant RT and none received chemotherapy, while about a third of patients with POLE wild-type tumors received RT and half received chemotherapy.
In our cohort of POLE-mutant EECs, de novo metastatic disease was noted, and recurrences were seen, even among patients with early stage disease receiving adjuvant radiation therapy. Specifically, 4 patients had disease recurrence. Although 1 had metastatic disease at the time of diagnosis, it is notable that 3 patients had uterine-confined, grade 3 disease. All of these patients were treated with adjuvant IVRT, and 1 patient also received chemotherapy. All of the patients who had localized disease at the time of diagnosis, and recurred, had distant metastases rather than pelvic-confined recurrences. It is also notable that 2 patients had brain metastases at the time of their recurrence. Brain metastases are rare, seen in less than 1% of EECs, and confer a poor overall prognosis [27, 28].
Rather than being at variance with previously published data, our study identified patients with both de novo metastatic disease and recurrences after initial diagnosis of uterine-confined disease. In contrast, Church et al. analyzed patients enrolled on the PORTEC-1 and −2 trials, all of whom had stage I and II disease, and therefore, by definition, no POLE mutated tumors with metastases were included [6]. Furthermore, although Church and colleagues concluded that the presence of POLE mutations in endometrial cancers were associated with a favorable prognosis, they also noted that there were recurrences among early stage endometrial cancer patients with POLE mutated tumors. In fact, of the 48 patients with POLE EDM EEC, 3 recurred (amounting to a 6% recurrence rate), and 1 patient died of disease. All the recurrences in the data presented by Church et al. were in uterine-confined disease, in patients with low-grade tumors reflective of their inclusion criteria/cohort. The authors specifically noted that overall survival of women with POLE mutated EECs was not statistically different from that of other patients, although patients with POLE mutated tumors who had grade 3 disease did have a survival advantage.
Mutational analysis did not reveal any specific POLE EDMs or specific mutational signatures to be associated with disease recurrence. We have previously found that, in the progression from primary to metastatic endometrial cancer, a shift from POLE- to MSI-related mutational processes can occur [19]. In the current study, we similarly observed the acquisition of defects in DNA MMR in the case for which both primary and recurrent EEC was available. In this case (PE18), the primary tumor was MSS while the recurrence was MSI, which was accompanied with an increase in DNA MMR-associated mutational signatures. These data suggest that in the process of tumor evolution/progression, POLE-mutant EEC may acquire additional molecular alterations resulting in further impairment in DNA repair. Previous work by Ashley et al., noted that based on mutational signature analysis the biological processes that drive the initial development of endometrial cancers may differ from those that lead to progressive or metastatic disease, which included the acquisition of DNA mismatch repair (MMR)-related signatures in a subset of cases [19]. Furthermore, discordant MMR protein expression by immunohistochemistry between primary and metastatic endometrial cancers has been reported, with a subset of metastatic sites being MMR-deficient as compared to their matched primary tumor [29]. Case PE18 from this study further supports these findings and suggests that for patients being considered for targeted therapy for treatment of cancer recurrence, repeat molecular analysis and/or DNA MMR immunohistochemical analysis of the metastatic tumors should be considered [19, 29].
The National Comprehensive Cancer Network treatment guidelines advocate adjuvant treatment for high-grade EECs; however, the best approach to adjuvant therapy remains uncertain [30]. The reports of excellent outcomes in the POLE subgroup, despite having high-grade EECs, supports the rationale for integrating POLE EDM status into patient care, and stratification for clinical trials. Some authors have even advocated for identifying this subset of patients and then minimizing their adjuvant therapy [6, 9]. At present, it remains unclear whether the presence of a POLE EDM is prognostic or predictive. Specifically, it is still not known whether these patients have a good prognosis regardless, or whether the good outcomes reflect a superior response to treatment [31]. It is, however, worth noting that, although we identified patients with recurrences and de novo metastatic disease, 22 of the 23 patients were alive as of last follow-up. In fact, 3 of the 4 patients who had a recurrence were without evidence of disease at time of publication. The association of POLE EDM with overall survival should be explored in future prospective research. As Cosgrove and colleagues noted, the suggestion that these patients may be cured by surgery alone requires additional prospective supportive evidence [32].
POLE mutant endometrial cancers have been shown to be genetically distinct from MSI-high tumors. However, up to 30% of POLE mutated tumors are MMR-deficient or MSI-high [2, 7]. Although 4 POLE EDM EECs in this study were MMR-deficient, none of the patients had Lynch syndrome. As universal screening for Lynch syndrome by MMR IHC has become widely adapted, POLE EDM EECs with MMR-deficiency may be a confounder in the screening process [33].
Knowledge of a tumor’s POLE status may be even more important in the recurrent setting, as emerging data suggests that ultramutated tumors may be more likely to respond to immunotherapy [34]. One patient in this cohort was treated with immunotherapy following disease recurrence. Immunotherapy drugs have been shown to be efficacious in tumors that are MMR deficient or MSI-high; pembrolizumab, an antibody targeting anti-programmed cell death protein 1 (PD-1), is approved by the Food and Drug Administration for use in these cancers. However, the role of these drugs in tumors which are MMR proficient or MSS but with a POLE EDM and ultramutated phenotype is less clear [35]. Despite most POLE mutated tumors being MSS, preclinical data supports the rationale for using PD-1 inhibitors (or programmed death ligand 1, PDL-1, inhibitors) in this ultramutated tumor subset, as the genomic instability inherent in tumors with a POLE EDM leads to a high number of neo-antigens and a high amount of tumor infiltrating lymphocytes [34]. Successful use of anti-PD1 immune checkpoint inhibitors for management of recurrent POLE mutated EEC has been reported by several groups [31, 36, 37]. Prospective research into the efficacy of PD-1/PDL-1 inhibitor in patients with POLE-mutated tumors is promising [38].
While the rate of POLE mutated tumors seen in our series is similar to that seen in other reports, the series is limited by its small size and retrospective nature [26]. However, these patients represent a real-world cohort, and 87% of these patients were treated at one institution from the time of their initial diagnosis. We acknowledge that there is some degree of ascertainment bias, given that 8 of the 23 patients, including all of those with recurrence or progression, were enrolled onto the sequencing protocol retrospectively at the time of their recurrent disease. As of 2016, it became a standard of care to offer enrollment onto the MSK-IMPACT protocol to all patients with endometrial cancer at the time of their initial preoperative visit. We look forward to the additional data which will come from this ongoing prospective sequencing effort.
Our study adds to the current literature on the role of POLE EDMs in endometrial cancer, and describes a prospective real-world clinical cohort. Importantly, it serves as a word of caution that additional data are required prior to changing treatment or surveillance strategy for this group of patients with a seemingly good prognosis. Despite the excellent prognosis reported in POLE-mutated EEC, in this clinical cohort we report on patients with cancer recurrences, including patients with grade 3 stage I disease, and de novo metastatic disease. Current trials, including PORTEC-4a () [39], are underway to evaluate the utility of treating patients based on molecular subtyping rather than clinicopathologic staging. As such, we advise caution with incorporating molecular subtyping into management of POLE-mutant EEC until the results of these studies are available.
HIGHLIGHTS.
In this prospective cohort, 5% of endometrioid endometrial carcinoma have POLE EDM
17% of POLE-mutant cases developed recurrences
Recurrences were observed in uterine-confined G3 disease after adjuvant RT
De novo metastatic disease was observed
Further research is warranted before changes in treatment/management are considered
ACKNOWLEDGEMENTS
Funding: This study was funded in part through the NIH/NCI Support Grant P30 CA008748.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement: None of the authors declare any conflicts of interest.
Disclosures:
Dr. Aghajanian reports personal fees from Tesaro, personal fees from Immunogen, personal fees from Mateon Therapeutics, personal fees from Cerulean Pharma; grants and personal fees from Clovis; grants from Genentech, grants from AbbVie, grants from Astra Zeneca, outside the submitted work.
Dr. Abu-Rustum reports grants from Stryker/Novadaq, grants from Olympus, grants from GRAIL, outside the submitted work.
Dr. Cadoo reports other* from Astra Zeneca, other** from Syndax Pharmaceuticals, outside the submitted work. (*Travel, accommodation, meal; institutional support for therapeutic trial; **institutional support for therapeutic trial)
Dr. Friedman reports institutional research support from BMS; service on Advisory Board for Astra Zeneca; institutional research support from Genentech; Steering Committee Membership for Genentech (compensation waived); research support from Merck, outside the submitted work.
Dr. Hyman reports stock ownership in Fount; consultancy for Chugai Pharma, consultancy for Boehringer Ingelheim, consultancy from AstraZeneca, consultancy for Pfizer, consultancy for Bayer, consultancy for Genentech, consultancy for Fount; research support from AstraZeneca, research support from Puma Biotechnology, research support from Loxo, research support from Bayer; travel, accommodations and expenses from Genentech; travel, accommodations and expenses from Chugai Pharma, outside the submitted work.
Dr. Makker reports grants and personal fees from Esai; grants and personal fees from Merck; other from International PI 775–03/E7080-G000–309; grants from Takeda (MSKCC PI C31004); personal fees from ArQule; grants and personal fees from Karyopharm; grants from AstraZeneca, grants from Lilly; personal fees from IBM Watson, outside the submitted work.
Dr. Soslow reports personal fees from Ebix/Oakstone*; personal fees from Cambridge University Press**; personal fees from Springer Publishers**; personal fees from Roche***, outside the submitted work. (*Preparation of recorded lectures; **royalties; ***one lecture)
Dr. Zamarin reports grants from Merck; personal fees from Merck, personal fees from Synlogic Therapeutics, personal fees from Psioxus Therapeutics, personal fees from Biomed Valley Discoveries, personal fees from Tizona Therapeutics, personal fees from ACM Biolabs, personal fees from Tesaro, outside the submitted work; a patent Newcastle Disease Virus and uses thereof with royalties paid to Merck, a patent Chimeric Newcastle Disease Virus and uses thereof with royalties paid to Merck, outside the submitted work.
REFERENCES
- 1.Siegel RL KD Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69:7–34. DOI: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Cancer Genome Atlas Research Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y, Shen H, et al. Integrated genomic characterization of endometrial carcinoma. Nature 2013;497:67–73. DOI: 10.1038/nature12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pursell ZF, Isoz I, Lundström EB, Johansson E, Kunkel TA. et al. Yeast DNA polymerase epsilon participates in leading-strand DNA replication. Science 2007;317:127–130. DOI: 10.1126/science.1144067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park VS, Pursell ZF. POLE proofreading defects: Contributions to mutagenesis and cancer. DNA Repair (Amst) 2019;76:50–59. DOI: 10.1016/j.dnarep.2019.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shinbrot E, Henninger EE, Weinhold N, Covington KR, Göksenin AY, Schultz N et al. Exonuclease mutations in DNA polymerase epsilon reveal replication strand specific mutation patterns and human origins of replication. Genome Res 2014;24:1740–1750. DOI: 10.1101/gr.174789.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Church DN, Stelloo E, Nout RA, Valtcheva N, Depreeuw J, ter Haar N, Noske A, et al. Prognostic significance of POLE proofreading mutations in endometrial cancer. J Natl Cancer Inst 2015;107:402 DOI: 10.1093/jnci/dju402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Billingsley CC, Cohn DE, Mutch DG, Stephens JA, Suarez AA, Goodfellow PJ. Polymerase varepsilon (POLE) mutations in endometrial cancer: clinical outcomes and implications for Lynch syndrome testing. Cancer 2015;121:386–394. DOI: 10.1002/cncr.29046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bosse T, Nout RA, McAlpine JN, McConechy MK, Britton H, Hussein YR, et al. Molecular Classification of Grade 3 Endometrioid Endometrial Cancers Identifies Distinct Prognostic Subgroups. Am J Surg Pathol 2018;42:561–568. DOI: 10.1097/PAS.0000000000001020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Billingsley CC, Cohn DE, Mutch DG, Hade EM, Goodfellow PJ. Prognostic Significance of POLE Exonuclease Domain Mutations in High-Grade Endometrioid Endometrial Cancer on Survival and Recurrence: A Subanalysis. Int J Gynecol Cancer 2016;26:933–938. DOI: 10.1097/IGC.0000000000000681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meng B, Hoang LN, McIntyre JB, Duggan MA, Nelson GS, Lee CH, et al. POLE exonuclease domain mutation predicts long progression-free survival in grade 3 endometrioid carcinoma of the endometrium. Gynecol Oncol 2014;134:15–19. DOI: 10.1016/j.ygyno.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 11.McAlpine J, Leon-Castillo A, Bosse T. The rise of a novel classification system for endometrial carcinoma; integration of molecular subclasses. J Pathol 2018;244:538–549. DOI: 10.1002/path.5034. [DOI] [PubMed] [Google Scholar]
- 12.Zehir A, Benayed R, Shah RH, Syed A, Middha S, Kim HR, et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat Med 2017;23:703–713. DOI: 10.1038/nm.4333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheng DT, Mitchell TN, Zehir A, Shah RH, Benayed R, Syed A, et al. Memorial Sloan Kettering-Integrated Mutation Profiling of Actionable Cancer Targets (MSK-IMPACT): A Hybridization Capture-Based Next-Generation Sequencing Clinical Assay for Solid Tumor Molecular Oncology. J Mol Diagn 2015;17:251–264. DOI: 10.1016/j.jmoldx.2014.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mandelker D, Zhang L, Kemel Y, Stadler ZK, Joseph V, Zehir A, et al. Mutation Detection in Patients With Advanced Cancer by Universal Sequencing of Cancer-Related Genes in Tumor and Normal DNA vs Guideline-Based Germline Testing. JAMA 2017;318:825–835. DOI: 10.1001/jama.2017.11137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalia SS, Adelman K, Bale SJ, Chung WK, Eng C, Evans JP, et al. Recommendations for reporting of secondary findings in clinical exome and genome sequencing, 2016 update (ACMG SF v2.0): a policy statement of the American College of Medical Genetics and Genomics. Genet Med 2017;19:249–255. DOI: 10.1038/gim.2016.190. [DOI] [PubMed] [Google Scholar]
- 16.Church DN, Briggs SE, Palles C, Domingo E, Kearsey SJ, Grimes JM,et al. DNA polymerase epsilon and delta exonuclease domain mutations in endometrial cancer. Hum Mol Genet 2013;22:2820282–8. DOI: 10.1158/2159-8290.CD-17-0321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang MT, Bhattarai TS, Schram AM, Bielski CM, Donoghue MTA, Jonsson P, et al. Accelerating Discovery of Functional Mutant Alleles in Cancer. Cancer Discov 2018;8:174–183. DOI: 10.1158/2159-8290.CD-17-0321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal 2013;6:pl1 DOI: 10.1126/scisignal.2004088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashley CW, Da Cruz Paula A, Kumar R, Mandelker D, Pei X, Riaz N, et al. Analysis of mutational signatures in primary and metastatic endometrial cancer reveals distinct patterns of DNA repair defects and shifts during tumor progression. Gynecol Oncol 2019;152:11–19. DOI: 10.1016/j.ygyno.2018.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Middha S, Zhang L, Nafa K, Jayakumaran G, Wong D, Kim HR, et al. Reliable Pan-Cancer Microsatellite Instability Assessment by Using Targeted Next-Generation Sequencing Data. JCO Precis Oncol 2017;2017 DOI: 10.1200/PO.17.00084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Niu B, Ye K, Zhang Q, Lu C, Xie M, McLellan MD, et al. MSIsensor: microsatellite instability detection using paired tumor-normal sequence data. Bioinformatics;2014;30:1015–1016. DOI: 10.1093/bioinformatics/btt755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Modica I, Soslow RA, Black D, Tornos C, Kauff N, Shia J. Utility of immunohistochemistry in predicting microsatellite instability in endometrial carcinoma. Am J Surg Pathol 2007;31:744–751. DOI: 10.1097/01.pas.0000213428.61374.06. [DOI] [PubMed] [Google Scholar]
- 23.Walsh MD, Cummings MC, Buchanan DD, Dambacher WM, Arnold S, McKeone D, Byrnes R, et al. Molecular, pathologic, and clinical features of early-onset endometrial cancer: identifying presumptive Lynch syndrome patients. Clin Cancer Res 2008;14:1692–1700. DOI: 10.1158/1078-0432.CCR-07-1849. [DOI] [PubMed] [Google Scholar]
- 24.Alexandrov LB, Nik-Zainal S, Wedge DC, Aparicio SA, Behjati S, Biankin AV, et al. Signatures of mutational processes in human cancer. Nature, 2013;500:415–421. DOI: 10.1038/nature12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosenthal R, McGranahan N, Herrero J, Taylor BS, Swanton C. DeconstructSigs: delineating mutational processes in single tumors distinguishes DNA repair deficiencies and patterns of carcinoma evolution. Genome Biol 2016;17:31 DOI: 10.1186/s13059-016-0893-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McConechy MK, Talhouk A, Leung S, Chiu D, Yang W, Senz J, et al. Endometrial Carcinomas with POLE Exonuclease Domain Mutations Have a Favorable Prognosis. Clin Cancer Res 2016;22:2865–2873. DOI: 10.1158/1078-0432.CCR-15-2233. [DOI] [PubMed] [Google Scholar]
- 27.Cybulska P, Stasenko M, Alter R, Makker V, Cadoo KA, Sonoda Y, et al. Brain metastases in patients with low-grade endometrial carcinoma. Gynecol Oncol Rep 2018;26:87–90. DOI: 10.1016/j.gore.2018.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Uccella S, Morris JM, Multinu F, Cliby WA, Podratz KC, Gostout BS, et al. Primary brain metastases of endometrial cancer: A report of 18 cases and review of the literature. Gynecol Oncol 2016;142:70–75. DOI: 10.1016/j.ygyno.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 29.Ta RM, Hecht JL, Lin DI. Discordant loss of mismatch repair proteins in advanced endometrial endometrioid carcinoma compared to paired primary uterine tumors. Gynecol Oncol 2018;151:401–406. [DOI] [PubMed] [Google Scholar]
- 30.National Comprehensive Cancer Network. Uterine Neoplasm (Version 3.2019) [cited 2019 July 2]; Available from: https://www.nccn.org/professionals/physician_gls/pdf/uterine.pdf. [Google Scholar]
- 31.Veneris JT, Lee EK, Goebel EA, Nucci MR, Lindeman N, Horowitz NS, et al. Diagnosis and management of a recurrent polymerase-epsilon (POLE)-mutated endometrial cancer. Gynecol Oncol, 2019;153:471–478. DOI: 10.1016/j.ygyno.2019.03.247. [DOI] [PubMed] [Google Scholar]
- 32.Cosgrove CM, Cohn DE, Goodfellow PJ, Primum non nocere: Are we ready for POLE testing in endometrial cancer? Gynecol Oncol 2017;147:240–242. DOI: 10.1016/j.ygyno.2017.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Crosbie EJ, et al. The Manchester International Consensus Group recommendations for the management of gynecological cancers in Lynch syndrome. Genet Med 2019;21:2390–2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gargiulo P, Della Pepa C, Berardi S, Califano D, Scala S, Buonaguro L,et al. Tumor genotype and immune microenvironment in POLE-ultramutated and MSI-hypermutated Endometrial Cancers: New candidates for checkpoint blockade immunotherapy? Cancer Treat Rev 2016;48:61–68. DOI: 10.1016/j.ctrv.2016.06.008. [DOI] [PubMed] [Google Scholar]
- 35.U.S. Food and Drug Administration. FDA grants accelerated approval to pembrolizumab for first tissue/site agnostic indication. May 23, 2017; Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-pembrolizumab-first-tissuesite-agnostic-indication.
- 36.Mehnert JM, Panda A, Zhong H, Hirshfield K, Damare S, Lane K, et al. Immune activation and response to pembrolizumab in POLE-mutant endometrial cancer. J Clin Invest 2016;126:2334–2340. DOI: 10.1172/JCI84940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Santin AD, Bellone S, Buza N, Choi J, Schwartz PE, Schlessinger J, et al. Regression of Chemotherapy-Resistant Polymerase epsilon (POLE) Ultra-Mutated and MSH6 HyperMutated Endometrial Tumors with Nivolumab. Clin Cancer Res 2016;22:5682–5687. DOI: 10.1158/1078-0432.CCR-16-1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Konstantinopoulos PA, Luo W, Liu JF, Gulhan DC Krasner C, Ishizuka JJ, et al. Phase II Study of Avelumab in Patients With Mismatch Repair Deficient and Mismatch Repair Proficient Recurrent/Persistent Endometrial Cancer. J Clin Oncol, 2019: p. JCO1901021 DOI: 10.1200/JCO.19.01021. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.ClinicalTrials.gov. Identifier: NCT03469674, PORTEC-4a: Molecular Profile-based Versus Standard Adjuvant Radiotherapy in Endometrial Cancer (PORTEC-4a). 2019; Available from: https://clinicaltrials.gov/ct2/show/NCT03469674#moreinfo.