Abstract
Background:
E-cigarettes are the most popular tobacco product among youth. As more states adopt cannabis legalization policies, youth cannabis use in e-cigarettes is a mounting concern.
Methods:
Data were from the 2016 and 2017 National Youth Tobacco Survey, a nationally-representative repeated cross-sectional survey administered to US middle and high school students. Ever use groups were categorized into e-cigarette ever users, cannabis in e-cigarette ever users, other tobacco ever users, and never users. Weighted multinomial logistic regression compared ever use groups, while controlling for state-level cannabis legalization and tobacco prevention polices, tobacco perceptions and exposures, and sociodemographic variables. Weighted prevalence of ever and current, or past 30 day, tobacco product use was determined by ever use groups.
Results:
Compared to e-cigarette ever users, cannabis in e-cigarette ever users increased (Adjusted Relative Risk Ratio (ARRR)=1.65; p<0.01) from 2016 to 2017. Medical-only and medical and recreational cannabis laws, and no e-cigarette minimum legal sales age (MLSA) and increased e-cigarette MLSA at 19 or 21 were positively associated with cannabis in e-cigarette ever users (ARRR=1.34–1.85; p<0.01, each). Ever and current use of all individual tobacco products was highest among cannabis in e-cigarette ever users compared to e-cigarette and other tobacco ever users.
Conclusions:
Cannabis use in e-cigarettes has increased among youth, and these trends will likely continue as e-cigarettes continue to gain popularity and cannabis legalization policies proliferate. Targeted tobacco and cannabis prevention strategies are needed for youth, especially in states that have implemented cannabis medical and recreational laws.
Keywords: e-cigarette, cannabis, tobacco, youth, policy, survey research
1. INTRODUCTION
In 2018, nearly five million US youth reported being current users of any tobacco product, of whom 40% had reported use of two or more tobacco products (Cullen et al., 2018). Currently, e-cigarettes are the most popular tobacco product among youth (Gentzke et al., 2019). E-cigarette use has steadily increased since 2011, with the most significant rise from 2017 to 2018 among middle (3.3% to 4.9%) and high (11.7% to 20.8%) school students (Cullen et al., 2018). While the long-term health effects of e-cigarettes are unknown, many contain nicotine, a highly addictive chemical that can harm brain and cognitive development and lead to addiction among youth (U.S. Department of Health & Human Services, 2016; Yuan et al., 2015).
With the rapid increase in e-cigarette use, cannabis use in e-cigarettes is an additional concern. E-cigarette use among youth is problematic, given that several studies demonstrate an association between e-cigarette use and other substance use including cannabis (Audrain-Mcgovern et al., 2018; Curran et al., 2018; Dai et al., 2018). Heavy cannabis use in adolescence is associated with cognitive impairment, such as issues with learning and memory, particularly when used at earlier ages (Schweinsburg et al., 2008). Further, cannabis use can lead to dependence and abuse of cannabis, as well as the development of depression and psychosis (Arseneault et al., 2002; Huang et al., 2010; Lev-Ran et al., 2014). E-cigarette devices are used to vaporize propylene glycol and/or glycerol containing nicotine and flavorings for inhalation (Breland et al., 2017). The same devices can be modified to allow for the delivery of cannabis, in ways that are easily concealed. In Connecticut, 5.4% of high school students were vaporizing cannabis in an e-cigarette in 2014 (Morean et al., 2015). According to the 2015 Monitoring the Future, 6% of 8th, 10th, and 12th grade US students had reported using cannabis in a vaporizer, such as e-cigarettes, and highest among 8th graders (Miech et al., 2017). In Canada, where cannabis rates among youth are the highest globally, 8.2% of high school students in Ontario vaped cannabis in e-cigarettes (Mammen et al., 2016). Since cannabis use in e-cigarettes is relatively novel, limited literature exists on this topic.
Changes in the design, availability, and use of e-cigarettes to allow for cannabis use have coincided with major shifts in the landscape of state-level cannabis policies. While recent state-level policies legalizing recreational cannabis were predicted to increase cannabis use among youth (Hopfer, 2014), empirical evidence on the policy effects of legalization have been mixed. One study found that US youth in states with medical cannabis legalization were more likely to initiate cannabis use (Wen et al., 2015), while other studies found no change (Hasin et al., 2015; Martins et al., 2016), or a decrease in youth cannabis use (Cerdá et al., 2018; Coley et al., 2019). The lack of consistency in policy effects may be due to variation in samples, measurement of cannabis-related outcomes, and heterogeneity in the cannabis laws themselves (Choo and Emery, 2017; Johnson et al., 2017; Pacula et al., 2015). Given these conflicting findings and ongoing policy changes, research on changes in youth cannabis use is a high priority. Our study aims to help clarify the association between cannabis legalization policies and cannabis use in e-cigarettes, using a large national sample of youth.
Youth cannabis use represents a challenge for public health. Clarifying associations between cannabis legalization laws and youth cannabis use in e-cigarettes is necessary with the rapid uptake of e-cigarettes that can deliver nicotine and cannabis. In addition, determining correlates associated with cannabis in e-cigarette ever use can help identify factors that put youth at risk for initiation of cannabis use in e-cigarettes. Further, including several covariates known to be associated with tobacco use, such as perceived harm (Amrock et al., 2015) and e-cigarette advertising (Nicksic et al., 2017a), can help identify youth at risk for co-use of tobacco and cannabis. The purpose of this study was to characterize youth cannabis in e-cigarette ever users according to state-level cannabis legalization and tobacco prevention policies, tobacco perceptions and exposures, and sociodemographic variables compared to ever use groups. Further, we wanted to determine whether cannabis in e-cigarette ever users were at increased risk of using other tobacco products compared to ever use groups.
2. METHODS
2.1. Study Population
This study analyzes public use data from the 2016 and 2017 National Youth Tobacco Survey (NYTS), a nationally-representative repeated cross-sectional survey completed by youth in grades 6–12 attending private and public schools. Using a three-stage, stratified cluster sample approach, the survey was administered in urban and rural middle and high schools of varying size. Survey participants were asked questions on tobacco behaviors, knowledge, attitudes, and exposures. Schools in Alaska, Hawaii, Massachusetts, Montana, Nebraska, New Hampshire, North Dakota, Rhode Island, South Dakota, Vermont, Wyoming, and the District of Colombia were not represented. The total sample size was n=20,675 (response rate=87.9%) in 2016 and n=17,872 (response rate=88.7%) in 2017. After eliminating youth who did not respond to substance use in e-cigarettes, the final sample size was n=36,841 (n=19,969 in 2016 and n=16,872 in 2017) representing a population (N) of 52,032,641 middle and high school students nationwide.
2.2. Measures
2.2.1. Ever Use Groups
Ever use groups were comprised of e-cigarette ever users, cannabis in e-cigarette ever users, other tobacco ever users, and never tobacco users. E-cigarette ever users reported ever using an e-cigarette, even once or twice. Beginning in 2016, youth were asked “Have you ever used an e-cigarette device with a substance besides nicotine?” Cannabis in e-cigarette ever users selected the response “Yes, I have used an e-cigarette device with Marijuana, THC or hash oil, or THC wax”. Importantly, youth defined as e-cigarette ever users in this study had never used any form of cannabis in an e-cigarette device, making them a discrete group from cannabis in e-cigarette ever users. Other tobacco ever users had used any other tobacco product (i.e. cigarettes, cigars, cigarillos, little cigars, chewing tobacco, snuff, dip, hookah, roll-your-own cigarettes, pipes, snus, dissolvables, bidis), even just one time, except e-cigarettes or cannabis use in e-cigarettes. Never tobacco users were defined as youth who had never used any tobacco product, including e-cigarettes or cannabis use in e-cigarette devices.
2.2.2. State-Level Policies
State-level policies relative to cannabis legalization and tobacco prevention in 2016 and 2017 were collected, coded, and merged into the NYTS data. Each state in the NYTS was categorized as having implemented either no or limited cannabis legalization policies (e.g. cannabidiol (CBD) oil, hemp, or low-THC products are decriminalized for possession and/or used for specific medical conditions and/or university research), medical-only cannabis legalization policies (Arizona, California, Connecticut, Delaware, Illinois, Maine, Maryland, Michigan, Minnesota, New Jersey, New Mexico, and New York; Nevada in 2016; Florida, Ohio, and Pennsylvania in 2017), or medical and recreational cannabis legalization policies (Colorado, Oregon, and Washington; Nevada in 2017; National Conference of State Legislatures, 2019).
Implementing restrictions on e-cigarette sales to minors, or minimum legal sales age (MLSA) laws, for each state included prohibiting sale to those under 18, having no policy in effect in 2016 before the FDA deeming rule (Michigan and Pennsylvania), and increasing the age of sale to either 19 or 21 years old (Alabama, New Jersey, and Utah; California in 2017; Centers for Disease Control & Prevention, 2018). An indicator was created for each state in both years for comprehensive smoke-free indoor air laws, defined as states that prohibited cigarette smoking in indoor areas of private worksites, restaurants, and bars (Arizona, Colorado, Delaware, Illinois, Iowa, Kansas, Maine, Maryland, Michigan, Minnesota, New Jersey, New Mexico, New York, Ohio, Oregon, Utah, Washington, Wisconsin; California in 2017; Centers for Disease Control & Prevention, 2018). State cigarette taxes were collected from the Campaign for Tobacco-Free Kids and included for each state in 2016 and 2017 (Campaign for Tobacco-Free Kids, 2018).
2.2.3. Tobacco Perceptions
E-cigarette harm perception was measured by asking “How much do you think people harm themselves when they use e-cigarette some days but not every day?” Response options included ‘A lot of harm,’ ‘Some harm,’ ‘Little harm,’ and ‘No harm.’ For ease of access, youth were provided with the response options of ‘Not easy at all,’ ‘Somewhat easy,’ and ‘Easy’ to the question “How easy do you think it is for kids your age to buy tobacco products in the store?”
2.2.4. Tobacco Exposures
Someone in home uses tobacco was measured by asking “Does anyone who lives with you now…?” and dichotomized to No (selecting “No one who lives with me now uses any form of tobacco” versus Yes (selecting any tobacco product). Secondhand smoke and vapor exposure were determined by asking “During the past 30 days, on how many days did you breathe the smoke/vapor from someone who was smoking tobacco products/using an e-cigarette in an indoor or outdoor public place?” and dichotomized to No (0 days) versus Yes (1–30 days). Four individual questions measured “how often do you see ads or promotions for e-cigarettes?” when using the internet; reading newspapers or magazines; going to a convenience store, supermarket, or gas station; watching TV. Responses were summed on a 1–5 scale (‘Never’, ‘Rarely’, ‘Sometimes’, ‘Most of the time’, ‘Always’) to create a continuous e-cigarette ad exposure (range: 4–20).
2.2.5. Sociodemographics
Survey year was included as a sociodemographic variable. State-level indicators merged into NYTS were median household income from the US Census Bureau (Guzman, 2018) and unemployment rates from the Bureau of Labor Statistics (Bureau of Labor Statistics, 2019). Individual-level variables were speaking another language other than English at home, difficulty focusing (responding ‘yes’ to the question “Because of a physical, mental, or emotional condition, do you have serious difficulty concentrating, remembering, or making decisions?”), age (12 or younger, 13–15, 16–17, 18 or older), sex, and race/ethnicity (White, Black, Hispanic, Asian, and Other).
2.3. Statistical Analysis
Survey weights were applied to adjust for nonresponse and to generalize results to the US middle and high school student population. Weighted characteristics and bivariate analyses (i.e. Pearson’s Chi-Square for categorical variables and t-tests for continuous variables) tested unadjusted associations between ever use groups and state-level polices, tobacco perceptions and exposures, and sociodemographic variables. Weighted multinomial logistic regression compared e-cigarette ever users to cannabis in e-cigarette ever users, other tobacco ever users, and never tobacco users, while controlling for state-level polices, tobacco perceptions and exposures, and sociodemographic variables. E-cigarette ever users were the referent group to address if living in a state with cannabis legalization laws was associated with cannabis use in e-cigarettes relative to e-cigarette ever users. Weighted prevalence of ever and current, or past 30 day, tobacco use by product was also estimated for e-cigarette ever users, cannabis in e-cigarette ever users, and other tobacco ever users. Analyses were performed with Stata 12.0 (College Station, TX) using statistical significance at p-value<0.05.
3. RESULTS
3.1. Sample Characteristics
The total sample in the 2016/2017 NYTS (n=36,841) surveys weighted to be representative of US youth were mostly White (56.8%), Male (50.7%), and between 13 and 15 years (44.9%; Table 1). One out of 10 youth had ever used cannabis in an e-cigarette, while 15.2% were e-cigarette ever users, 11.1% other tobacco ever users, and 63.7% never users. Nearly half of youth lived in states where medical cannabis is legalized (48.2%) and where there are comprehensive smoke-free indoor laws (46.6%). While 3.2% of youth lived in a state without an MLSA laws in 2016, 12.0% lived in states that increased their MLSA laws to 19 or 21 years old. Over one-third of youth lived with someone who used tobacco (36.7%). Within the past 30 days, over half (52%) had secondhand exposure to smoke and a quarter (26.2%) had secondhand exposure to vapor in public places.
Table 1.
Weighted Characteristics and Bivariate Associations between Ever Use Groups among Youth in the National Youth Tobacco Survey 2016–2017
| Total Sample n=36,841; N=52,032,641 | Never Users of Tobacco (n=23,077; 63.7%) % (95% CI) | E-cigarette Ever Usersb (n=5,491; 15.2%) % (95% CI) | Cannabis in E-cigarette Ever Users (n=3,758; 10.0%) % (95% CI) | Other Tobacco Users (n=4,515; 11.1%) % (95% CI) | p-valuec | ||
|---|---|---|---|---|---|---|---|
| na | % (95% CI) | ||||||
| State-Level Policies | |||||||
| Cannabis Policy | <0.01 | ||||||
| None or limited | 17,713 | 43.4 (35.2–52.0) | 42.6 (34.3–51.4) | 46.3 (37.5–55.4) | 37.9 (29.4–47.3) | 48.7 (40.0–57.5) | |
| Medical | 16,811 | 48.2 (39.8–56.6) | 49.0 (40.4–57.6) | 45.3 (36.7–54.3) | 51.4 (42.1–60.6) | 44.3 (36.0–53.0) | |
| Medical and recreational | 2,317 | 8.4 (4.3–15.9) | 8.4 (4.3–15.8) | 8.4 (4.2–15.9) | 10.7 (5.1–21.0) | 6.9 (3.4–13.7) | |
| Restrictions on Minor E-cigarette Sales | 0.01 | ||||||
| 18 years old | 31,996 | 84.8 (77.3–90.1) | 84.2 (76.1–89.9) | 87.2 (80.6–91.8) | 81.4 (71.7–88.4) | 87.8 (81.4–92.2) | |
| No policy in effect in 2016 | 1,582 | 3.2 (1.4–7.3) | 3.0 (1.3–6.9) | 3.5 (1.5–8.4) | 3.8 (1.6–8.6) | 3.2 (1.4–7.4) | |
| 19 or 21 years old | 3,263 | 12.0 (7.2–19.3) | 12.8 (7.6–20.7) | 9.2 (5.4–15.2) | 14.8 (8.4–24.6) | 12.0 (7.2–19.3) | |
| Comprehensive Smoke-free Indoor Laws | 14,802 | 46.6 (37.9–55.5) | 47.0 (38.1–56.1) | 45.7 (36.7–54.9) | 51.0 (41.1–60.8) | 41.3 (32.8–50.4) | 0.02 |
| Cigarette Tax, mean (SD) | 1.62 | 1.71 (0.09) | 1.72 (0.09) | 1.68 (0.10) | 1.76 (0.10) | 1.64 (0.10) | 0.41 |
| Tobacco Perceptions and Exposures | |||||||
| Harm of E-cigarette Use Some Days | <0.001 | ||||||
| A lot of harm | 9,788 | 27.1 (26.2–28.1) | 34.1 (33.0–35.3) | 7.1 (6.2–8.1) | 13.8 (12.3–15.6) | 26.2 (24.5–28.0) | |
| Some harm | 12,816 | 36.5 (35.7–37.4) | 40.5 (39.5–41.4) | 26.2 (24.7–27.8) | 28.9 (26.6–31.3) | 34.9 (32.9–36.7) | |
| Little harm | 9,669 | 27.3 (26.4–28.1) | 20.7 (19.9–21.6) | 48.2 (46.5–49.9) | 37.8 (35.3–40.3) | 26.7 (25.1–28.3) | |
| No harm | 3,570 | 9.1 (8.5–9.7) | 4.7 (4.2–5.2) | 18.5 (17.2–19.8) | 19.5 (17.4–21.7) | 12.2 (11.1–13.5) | |
| Ease of Peers Buying Tobacco | <0.001 | ||||||
| Not easy at all | 12,344 | 34.4 (32.9–36.0) | 39.3 (37.5–41.1) | 24.2 (22.3–26.2) | 21.2 (19.2–23.3) | 32.3 (30.0–34.7) | |
| Somewhat easy | 15,890 | 45.2 (43.9–46.4) | 45.7 (44.1–47.2) | 47.2 (45.1–49.2) | 41.6 (39.4–43.8) | 42.4 (40.5–44.4) | |
| Easy | 7,329 | 20.4 (19.5–21.4) | 15.0 (14.3–15.8) | 28.6 (26.9–30.4) | 37.2 (35.1–39.4) | 25.3 (23.5–27.2) | |
| Someone in Home Uses Tobacco | 12,717 | 36.7 (34.9–38.6) | 27.8 (25.9–29.7) | 55.7 (53.5–57.9) | 55.9 (52.9–58.9) | 46.0 (43.6–48.3) | <0.001 |
| Secondhand Smoke in Public | 17,901 | 52.0 (50.8–53.3) | 46.6 (45.2–47.9) | 64.4 (62.6–66.3) | 67.4 (65.1–69.6) | 53.4 (51.2–55.6) | <0.001 |
| Secondhand Vapor in Public | 8,879 | 26.2 (25.0–27.4) | 18.3 (17.2–19.4) | 46.1 (43.6–48.7) | 51.3 (48.5–54.1) | 22.5 (20.8–24.2) | <0.001 |
| E-cigarette Ad Exposure, mean (SD) | 8.9 | 8.8 (0.08) | 8.5 (0.09) | 9.4 (0.09) | 9.8 (0.11) | 8.9 (0.11) | <0.001 |
| Sociodemographic variables | |||||||
| Year | <0.001 | ||||||
| 2016 | 19,969 | 50.7 (41.7–59.6) | 49.5 (40.3–58.6) | 55.7 (46.2–64.8) | 45.2 (35.8–54.9) | 55.7 (46.5–64.5) | |
| 2017 | 16,872 | 49.3 (40.4–58.3) | 50.5 (41.4–59.7) | 44.3 (35.2–53.8) | 54.8 (45.1–64.2) | 44.3 (35.4–53.5) | |
| Household Median Income, mean (SD) | 5.96 | 6.06 (0.08) | 6.09 (0.08) | 5.95 (0.08) | 6.09 (0.09) | 5.95 (0.08) | <0.001 |
| Unemployment Rate, mean (SD) | 4.8 | 4.7 (0.05) | 4.7 (0.05) | 4.7 (0.06) | 4.7 (0.06) | 4.7 (0.05) | 0.32 |
| Speak Other Language | 11,044 | 28.0 (25.6–30.5) | 27.0 (24.3–29.8) | 26.4 (23.8–29.3) | 32.7 (29.6–36.0) | 32.1 (29.3–35.0) | <0.001 |
| Difficulty Focusing | 5,535 | 15.4 (14.8–16.0) | 11.6 (11.0–12.2) | 20.8 (19.4–22.2) | 27.5 (25.5–29.6) | 19.4 (17.8–21.0) | <0.001 |
| Age | <0.001 | ||||||
| 12 years or younger | 7,383 | 19.4 (17.7–21.3) | 25.2 (23.1–27.4) | 7.3 (5.9–9.1) | 6.8 (5.4–8.5) | 14.3 (12.5–16.4) | |
| 13–15 years old | 16,013 | 44.9 (43.7–46.0) | 47.9 (46.7–49.0) | 41.8 (39.6–44.0) | 33.2 (31.0–35.4) | 42.2 (39.8–44.6) | |
| 16–17 years old | 10,270 | 27.7 (25.9–29.5) | 21.6 (19.8–23.6) | 38.7 (36.5–41.0) | 43.9 (41.4–46.4) | 32.8 (30.5–35.1) | |
| 18 years or older | 3,038 | 8.0 (7.4–8.7) | 5.3 (4.7–6.0) | 12.2 (10.9–13.5) | 16.1 (14.7–17.7) | 10.7 (9.5–12.1) | |
| Female | 18,191 | 49.3 (48.4–50.2) | 51.1 (50.1–52.0) | 47.0 (44.8–49.1) | 44.7 (42.1–47.3) | 46.5 (44.4–48.7) | <0.001 |
| Race/Ethnicity | <0.001 | ||||||
| White | 16,660 | 56.8 (53.5–60.1) | 57.5 (53.9–61.1) | 62.7 (59.1–66.1) | 54.2 (50.0–58.2) | 46.6 (42.8–50.4) | |
| Black | 6,063 | 12.9 (11.2–14.9) | 12.9 (11.1–15.0) | 8.5 (7.3–10.1) | 12.1 (9.9–14.7) | 20.2 (17.2–23.5) | |
| Hispanic | 9,909 | 24.7 (22.2–27.3) | 23.1 (20.5–25.9) | 25.1 (22.3–28.2) | 30.2 (26.6–34.1) | 28.4 (25.4–31.5) | |
| Asian | 1,782 | 4.3 (3.5–5.3) | 5.4 (4.3–6.7) | 2.3 (1.7–3.1) | 1.5 (1.1–2.1) | 3.1 (2.4–4.1) | |
| Other | 865 | 1.3 (1.1–1.5) | 1.1 (0.9–1.3) | 1.4 (1.1–1.8) | 2.0 (1.5–2.6) | 1.7 (1.3–2.2) | |
Unweighted sample size for categorical variables and mean for continuous variables
E-cigarette ever users have never used marijuana, THC or hash oil, or THC wax in an e-cigarette device.
Bivariate tests included Pearson’s Chi Square for categorical variables and t test for continuous variables at a statistical significance of 0.05.
3.2. Unadjusted Associations
For state-level policies, significant differences were seen in ever use group by cannabis policy, restrictions on minor e-cigarette sales, comprehensive smoke-free indoor laws (p<0.05, all), but not for cigarette tax (p=0.41). Significant differences were observed for all tobacco perceptions and exposure variables and ever use groups as well (p<0.001, all). Cannabis in e-cigarette ever users increased from 2016 (8.9%) to 2017 (11.1%), as did never users of tobacco (62.2% to 65.3%; not shown). E-cigarette ever users and other tobacco ever users both increased from 2016 to 2017 (16.7 to 13.7% and 12.1 to 9.9%, respectively). There were significant differences between ever use groups and year (p<0.001). Additionally, there were significant differences among ever use groups and all sociodemographic variables (p<0.001, all), except unemployment rate (p=0.32).
3.3. Adjusted Associations
Compared to e-cigarette ever users, cannabis in e-cigarette ever users increased from 2016 to 2017 after adjustment for state-level polices, tobacco perceptions and exposures, and sociodemographic variables (Adjusted Relative Risk Ratio [ARRR]=1.65; 95% CI 1.35×2.02; Table 2). Regarding state-level cannabis legalization and tobacco prevention laws, living in states with medical (ARRR=1.34; 95% CI 1.04–1.74) or medical and recreational (ARRR=1.85; 95% CI 1.26–2.71) cannabis policies compared to no or limited cannabis policies increased the risk of ever use of cannabis in e-cigarettes. Youth living in states with no e-cigarette MLSA laws in 2016 (ARRR=1.65; 95% CI 1.26–2.15) and in states with e-cigarette MLSA laws at 19 or 21 years (ARRR=1.54; 95% CI 1.09–2.17) were more likely to be cannabis in e-cigarette ever users than ever e-cigarette users who did not use cannabis in e-cigarettes. Additionally, youth living in states with no e-cigarette MLSA laws in 2016 were more likely to be never users of tobacco (ARRR=1.24; 95% CI 1.01–1.51).
Table 2.
Weighted Multinomial Logistic Regression of Ever Use Groups and Cannabis Legalization and Tobacco Prevention Policies among Youth in the National Youth Tobacco Survey 2016–2017, n=36,841; N=52,032,641a
| Never Users of Tobacco (n=23,077) ARRR (95% CI) | Cannabis in E-cigarette Ever Users (n=3,758) ARRR (95% CI) | Other Tobacco Ever Users (n=4,507) ARRR (95% CI) | |
|---|---|---|---|
| State-Level Policies | |||
| Cannabis Policy | |||
| None or limited | Ref | Ref | Ref |
| Medical | 1.06 (0.87–1.29) | 1.34 (1.04–1.74) | 0.97 (0.79–1.21) |
| Medical and recreational | 1.05 (0.79–1.39) | 1.85 (1.26–2.71) | 0.97 (0.67–1.39) |
| Restrictions on Minor E-cigarette Sales | |||
| 18 years old | Ref | Ref | Ref |
| No policy in effect in 2016 | 1.24 (1.01–1.51) | 1.65 (1.26–2.15) | 1.11 (0.85–1.44) |
| 19 or 21 years old | 1.19 (0.88–1.61) | 1.54 (1.09–2.17) | 0.99 (0.76–1.30) |
| Comprehensive Smoke-free Indoor Laws | 0.86 (0.69–1.07) | 0.85 (0.66–1.08) | 0.88 (0.67–1.15) |
| Cigarette Tax, mean (SD) | 0.99 (0.91–1.08) | 0.94 (0.84–1.04) | 1.03 (0.91–1.16) |
| Tobacco Perceptions and Exposures | |||
| Harm of E-cigarette Use Some Days | |||
| A lot of harm | Ref | Ref | Ref |
| Some harm | 0.38 (0.32–0.46) | 0.63 (0.51–0.78) | 0.43 (0.35–0.53) |
| Little harm | 0.12 (0.10–0.15) | 0.45 (0.37–0.56) | 0.19 (0.16–0.23) |
| No harm | 0.07 (0.05–0.08) | 0.60 (0.47–0.77) | 0.18 (0.14–0.23) |
| Ease of Peers Buying Tobacco | |||
| Not easy at all | Ref | Ref | Ref |
| Somewhat easy | 0.93 (0.82–1.05) | 0.94 (0.79–1.12) | 0.87 (0.75–1.01) |
| Easy | 0.63 (0.55–0.72) | 1.18 (0.99–1.41) | 0.88 (0.75–1.05) |
| Someone in Home Uses Tobacco | 0.42 (0.38–0.46) | 1.07 (0.94–1.22) | 0.85 (0.76–0.96) |
| Secondhand Smoke in Public | 0.87 (0.79–0.97) | 1.06 (0.94–1.19) | 1.08 (0.96–1.21) |
| Secondhand Vapor in Public | 0.40 (0.36–0.45) | 1.15 (0.99–1.34) | 0.40 (0.36–0.46) |
| E-cigarette Ad Exposure, mean (SD) | 0.96 (0.95–0.98) | 1.05 (1.03–1.06) | 0.98 (0.96–0.99) |
| Sociodemographic variables | |||
| Year | |||
| 2016 | Ref | Ref | Ref |
| 2017 | 1.14 (0.99–1.32) | 1.65 (1.35–2.02) | 0.94 (0.79–1.12) |
| Household Median Income, mean (SD) | 1.12 (1.03–1.21) | 1.02 (0.90–1.16) | 0.99 (0.89–1.11) |
| Unemployment Rate, mean (SD) | 0.99 (0.89–1.10) | 1.05 (0.90–1.23) | 1.05 (0.90–1.21) |
| Speak Other Language | 0.85 (0.75–0.96) | 1.21 (1.04–1.42) | 1.09 (0.93–1.28) |
| Difficulty Focusing | 0.65 (0.58–0.72) | 1.40 (1.24–1.59) | 1.06 (0.90–1.23) |
| Age | |||
| 12 years or younger | Ref | Ref | Ref |
| 13–15 years old | 0.38 (0.31–0.47) | 0.90 (0.69–1.18) | 0.64 (0.50–0.81) |
| 16–17 years old | 0.18 (0.14–0.22) | 1.25 (0.95–1.65) | 0.56 (0.45–0.69) |
| 18 years or older | 0.15 (0.11–0.19) | 1.43 (1.06–1.95) | 0.57 (0.43–0.74) |
| Female | 1.14 (1.03–1.26) | 0.87 (0.76–0.99) | 0.96 (0.84–1.09) |
| Race/Ethnicity | |||
| White | Ref | Ref | Ref |
| Black | 1.34 (1.15–1.56) | 1.65 (1.33–2.05) | 2.52 (2.13–2.98) |
| Hispanic | 0.83 (0.71–0.97) | 1.15 (0.97–1.36) | 1.17 (0.97–1.41) |
| Asian | 1.86 (1.37–2.54) | 0.59 (0.39–0.89) | 1.29 (0.91–1.85) |
| Other | 0.68 (0.49–0.95) | 1.43 (1.01–2.04) | 1.27 (0.90–1.81) |
ARRR=Adjusted relative risk ratio
E-cigarette ever users represent the reference category for the outcome variable.
Compared to ever e-cigarette users, youth exposed to e-cigarette ads were more likely to be cannabis in e-cigarette ever users (ARRR=1.05; 95% CI 1.03–1.06), yet less likely to be never users (ARRR=0.96; 95% CI 0.95–0.98) or other tobacco ever users (ARRR=0.98; 95% CI 0.96–0.99). Difficulty focusing was associated with cannabis in e-cigarette ever users (ARRR=1.40; 95% CI 1.24–1.59). Cannabis in e-cigarette ever users were also more likely than ever e-cigarette users to be 18 years or older (ARRR=1.43; 95% CI 1.06–1.95), speak another language at home (ARRR=1.21; 95% CI 1.04–1.42), and identify as Black (ARRR=1.65; 95% CI 1.33–2.05) and as Other race/ethnicity (ARRR=1.43; 95% CI 1.01–2.04). Finally, cannabis in e-cigarette ever users were less likely to be female (ARRR=0.87; 95% CI 0.76–0.99) and Asian (ARRR=0.59; 95% CI 0.39–0.89).
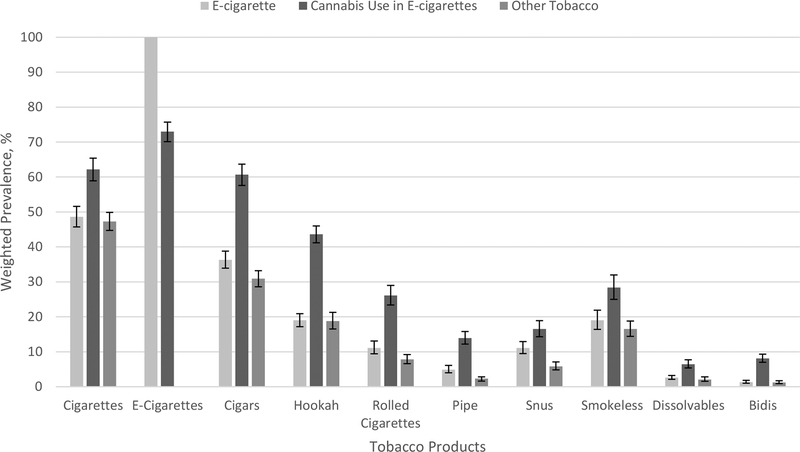
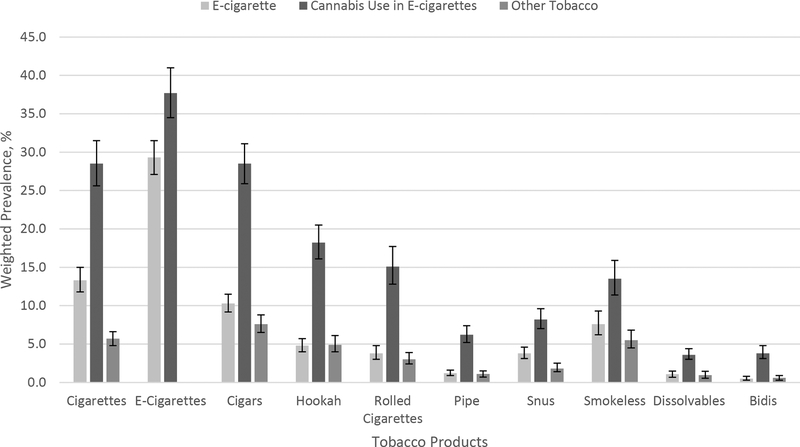
3.4. Ever and Current Tobacco Use by Ever Use Group
Given the contrasts in associations between cannabis legalization and tobacco prevention policies, perceptions about e-cigarette use, and sociodemographics across e-cigarette ever use groups, we next examined whether the profile of tobacco product use differed between these groups of youth. Cannabis in e-cigarette users (n=3,758) were more likely to report ever use and current use of every tobacco product compared to e-cigarette (n=5,491) and other tobacco (n=4,515) ever use groups (p<0.001, all) with exception to ever use of e-cigarettes. Specifically, e-cigarette (73.0%), cigarette (62.2%), cigar (60.7%), hookah (43.6%), and smokeless (28.4%) ever use was highest among cannabis in e-cigarette ever users (Figure 1a). In comparison, ever e-cigarette users reported lower rates of ever use of cigarettes (48.6%), cigars (36.3%), and hookah and smokeless (19.0% each). Among ever users of other tobacco products, ever use of cigarettes (47.3%), cigars (30.9%), and hookah (18.8%) were most commonly reported. Regarding current tobacco use, the prevalence of current use was again significantly highest in cannabis in e-cigarette ever users across all tobacco products compared to e-cigarette and other tobacco ever use groups (p<0.001, all; Figure 1b). For example, compared to e-cigarette ever users, cannabis in e-cigarette ever users were more likely to report current use of e-cigarette (37.7% vs. 29.3%), cigarettes (28.5% vs. 13.3%), cigars (28.5% vs. 10.3%), and hookah (18.2% vs 4.8%).
Figure 1a.
Weighted prevalence (%) (95% CI) of ever tobacco use by tobacco product, separated by ever use groups (e-cigarette, cannabis use in e-cigarettes, and other tobacco). Tobacco products included cigarettes, e-cigarettes, cigars, hookah, rolled cigarettes, pipe tobacco, snus, smokeless tobacco, dissolvables, and bidis.
Figure 1b.
Weighted prevalence (%) (95% CI) of current tobacco use by tobacco product, separated by ever use groups (e-cigarette, cannabis use in e-cigarettes, and other tobacco). Tobacco products included cigarettes, e-cigarettes, cigars, hookah, rolled cigarettes, pipe tobacco, snus, smokeless tobacco, dissolvables, and bidis.
4. DISCUSSION
The findings from this study indicate that ever use of cannabis in e-cigarette devices is increasing among youth and positively associated with state-level cannabis legalization policies and e-cigarette advertising, but evidence was mixed on how state-level tobacco prevention policies relate to cannabis in e-cigarette ever use when compared to youth who were ever users of e-cigarettes who do not use cannabis in their devices. Cannabis use in e-cigarettes in 2017 was nearly double the prevalence found in 2015 from Monitoring the Future at 6.0% (Miech et al., 2017). Regarding state-level cannabis legalization policies and cannabis use in e-cigarettes among youth, the current study found medical only and medical and recreational cannabis laws were associated with increased risk for cannabis in e-cigarette ever use. Although this is the first study to examine cannabis legalization policies and cannabis use in e-cigarettes among youth, our findings align with previous research indicating that rates of cannabis initiation are higher in states with medical cannabis policies (Hasin et al., 2015; Wen et al., 2015), and the availability and acceptability of cannabis in these states could influence the rate of initiation among youth. Importantly, research on the long-term effects of legalizing recreational cannabis use on youth uptake and continued use of cannabis and other substances, including tobacco products, is limited and appears to differ by state. In younger youth in Washington, perceived harms of cannabis are lower and prevalence of use increased following recreational legalization, but the same association was not found in Colorado (Cerdá et al., 2017).
Cannabis in e-cigarette ever use among youth was higher than e-cigarette ever use in states with no e-cigarette MLSA laws in 2016. Interestingly, and somewhat surprisingly, cannabis in e-cigarette ever use was also positively associated with living in states that have MLSA e-cigarette laws at 19 or 21 years of age. However, states with recreational legalization require consumers to be 21 years of age to purchase cannabis. By 2017, only four states, Alabama, California (in 2017), New Jersey, and Utah, had implemented an increased age limit for e-cigarette sales. Both California and New Jersey have medical cannabis policies, while Alabama and Utah have limited access cannabis policies. Although it is unclear why stricter MLSA laws for purchasing tobacco products were associated with increased cannabis in e-cigarette ever use among youth, it seems that prevention efforts in these states cannot be directed only at restricting access to e-cigarettes among youth and young adults. In supplemental analyses conducted for this study, including state-specific dummy variables in regressions to account for any unobserved differences in state prevalence substance use or other contextual variables did not substantively change our results. This suggests that future work is needed to using additional cross-sections of data or using panel data to allow for statistical methods that can further disentangle state-level differences in e-cigarette and cannabis use and the role of policies targeting each, including determining if MLSA laws of cannabis sales and tobacco product sales are enforced.
Although exposures to tobacco, such as someone in the household using tobacco and secondhand smoke or vapor, were prominent among cannabis ever users, these exposures were not statistically different from e-cigarette ever users. Surprisingly, cumulative e-cigarette ad exposure across online, print, store, and TV sources was associated with cannabis in e-cigarette ever use, compared to e-cigarette ever use. In addition to e-cigarette use, e-cigarette advertising could potentially influence other substance use, such as cannabis (Nicksic and Barnes, 2019). Restrictions on e-cigarette advertising could improve youth prevention efforts across multiple tobacco products and substances. As the literature accumulates on the association between e-cigarette advertising and use (Mantey et al., 2016; Nicksic et al., 2017a, 2017b), there are still limited federal restrictions on e-cigarette advertising.
The implications of sociodemographic variables with ever use groups suggest diversity among those who initiate cannabis use in e-cigarette devices, compared to youth who are e-cigarette ever users. Cannabis ever use in e-cigarettes was associated with being 18 years or older; however, the majority of youth initiating cannabis use were 16 or 17 years (43.9%) followed by 13 to 15 years (33.2%). While previous research indicates that younger youth are currently using cannabis (Miech et al., 2017), NYTS does not measure current cannabis use. Black males were also more likely to use cannabis in an e-cigarette device. Youth who speak another language other than English at home were also at risk, as previous studies found that acculturation was associated with higher youth substance use (Pokhrel et al., 2013; Thai et al., 2010). These findings provide an indication of youth at risk for tobacco and cannabis initiation in a tobacco landscape that is constantly changing and could support the development of prevention programs and policies tailored to these specific groups.
Importantly, the prevalence of ever and current use of individual tobacco products was highest for those who had ever used cannabis in an e-cigarette compared to e-cigarette and other tobacco ever users. Among cannabis and e-cigarette ever users, current use was highest for e-cigarettes followed by cigarettes. Nearly 20% of cannabis in e-cigarette ever users believed that e-cigarette use on some days caused no harm. While perceived harms of cannabis use was not measured in this survey, determining harm perceptions across substances can be important for educational purposes. Cigar ever and current use surpassed hookah in all groups, making cigars the third most popular tobacco product among youth, which aligns with recent findings on youth tobacco use (Gentzke et al., 2019). Rolled cigarettes were also increased among cannabis in e-cigarette ever users, although not in the other groups. Cigars and rolled cigarettes may be popular in this group as another vehicle for cannabis use (Delnevo et al., 2011). While this study provided an overview of potential correlates of initiating cannabis use in e-cigarettes, these ever use groups could be studied over longer periods of time and in more detail if current cannabis use prevalence was also available.
Results from this study need to be interpreted while considering a few limitations. First, responses were self-reported, allowing for the possibility of recall bias. Additionally, questions from the NYTS were limited and did not include items measuring detailed behavior or other substance use, such as marijuana use outside of e-cigarette devices and alcohol, and other substance use perception questions (e.g. the perceived harm of using cannabis in an e-cigarette). However, as youth who were cannabis in e-cigarette ever users were more likely to live in states with cannabis legalization, these youth are likely using cannabis in other forms, such as edibles, and thus all forms of cannabis use are necessary to study. Further, the association between cannabis policy and cannabis use in e-cigarette is not considered causal and requires longitudinal state data before implementation of cannabis policies (Wall et al., 2016). Importantly, generalizability of results are limited, as not all states were in the public use file and only youth attending school were surveyed. There is also a possibility of overrepresentation, since we do not know if any youth answered the survey in both years. Despite these youth attending school within the US, a critical population of interest for public health and policy makers. E-cigarette specific policies, including smoke-free indoor air laws specific to e-cigarettes, e-cigarette retail license required for over-limitations, this study included over 36,000 youth representing a population of more than 52 million the-counter sales, and e-cigarette taxes, were considered in analyses; however, too few states had enacted these policies to see any potential effects.
4.2. Conclusions
This study found state-level policies were potential risk factors for using cannabis in e-cigarette devices among youth. Cannabis legalization policy and e-cigarette MLSA laws at 19 or 21 years were positively associated with cannabis use in e-cigarettes. Further, using cannabis in e-cigarettes is increasing among middle and high school students. Cannabis use is harmful to cognitive development among youth, and using e-cigarettes can be inconspicuous. Even more problematic, tobacco use was highest among cannabis in e-cigarette ever users across every tobacco product assessed. While tobacco exposures are high and perceptions of e-cigarette harm are low among cannabis in e-cigarette ever users, exposure to e-cigarette advertising was positively associated to cannabis in e-cigarettes ever users. The effects that cannabis policies have on youth cannabis use reported here need to be carefully followed over time. For public health programs seeking to minimize harms from substance use among youth in a rapidly evolving policy and tobacco product landscape, innovations in tailored prevention and education programs that acknowledge the potential combined influences of cannabis and tobacco laws are needed.
Highlights.
The US regulatory landscape of tobacco and cannabis products continues to evolve.
This study characterized youth who had ever used cannabis in e-cigarettes.
Cannabis laws were associated with increased cannabis in e-cigarette ever use.
Tobacco prevention laws should consider how cannabis laws influence tobacco use.
Role of Funding Source
NEN is supported by the National Cancer Institute of the National Institutes of Health (T32CA093423). EKD is supported by the Virginia Foundation for Healthy Youth (RFP852R009). AJB is supported by the National Institute on Drug Abuse (R03DA043005; U54DA036105) and the Center for Tobacco Products of the U.S. Food and Drug Administration and by the National Cancer Institute (5UG1CA189869). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
None.
REFERENCES
- Amrock SM, Zakhar J, Zhou S, Weitzman M, 2015. Perception of e-cigarette harm and its correlation with use among U.S. adolescents. Nicotine Tob. Res 17, 330–6. 10.1093/ntr/ntu156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arseneault L, Cannon M, Poulton R, Murray R, Caspi A, Moffitt TE, 2002. Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study. BMJ 325, 1212–3. 10.1136/bmj.325.7374.1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audrain-Mcgovern J, Stone MD, Barrington-Trimis J, Unger JB, Leventhal AM, 2018. Adolescent e-cigarette, hookah, and conventional cigarette use and subsequent marijuana use. Pediatrics 142 10.1542/peds.2017-3616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breland A, Soule E, Lopez A, Ramôa C, El-Hellani A, Eissenberg T, 2017. Electronic cigarettes: what are they and what do they do? Ann. N. Y. Acad. Sci 1394, 5–30. 10.1111/nyas.12977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics, 2019. Local Area Unemployment Statistics. Accessed 30 April 2019 https://www.bls.gov/lau/tables.htm.
- Campaign for Tobacco-Free Kids, 2018. Cigarette Tax Increases by State per Year 2000–2018.
- Centers for Disease Control & Prevention, 2018. STATE System E-Cigarette Fact Sheet.
- Cerdá M, Sarvet AL, Wall M, Feng T, Keyes KM, Galea S, Hasin DS, 2018. Medical marijuana laws and adolescent use of marijuana and other substances: Alcohol, cigarettes, prescription drugs, and other illicit drugs. Drug Alcohol Depend. 183, 62–68. 10.1016/j.drugalcdep.2017.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá M, Wall M, Feng T, Keyes KM, Sarvet A, Schulenberg J, O’Malley PM, Pacula RL, Galea S, Hasin DS, 2017. Association of State Recreational Marijuana Laws With Adolescent Marijuana Use. JAMA Pediatr. 171, 142–149. 10.1001/jamapediatrics.2016.3624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choo EK, Emery SL, 2017. Clearing the haze: the complexities and challenges of research on state marijuana laws. Ann. N. Y. Acad. Sci 1394, 55–73. 10.1111/nyas.13093 [DOI] [PubMed] [Google Scholar]
- Coley RL, Hawkins SS, Ghiani M, Kruzik C, Baum CF, 2019. A quasi-experimental evaluation of marijuana policies and youth marijuana use. Am. J. Drug Alcohol Abuse 45, 292–303. 10.1080/00952990.2018.1559847 [DOI] [PubMed] [Google Scholar]
- Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA, 2018. Notes from the Field: Use of Electronic Cigarettes and Any Tobacco Product Among Middle and High School Students — United States, 2011–2018. MMWR Morb. Mortal. Wkly. Rep 67, 1276–1277. 10.15585/mmwr.mm6745a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran KA, Burk T, Pitt PD, Middleman AB, 2018. Trends and Substance Use Associations With E-Cigarette Use in US Adolescents. Clin. Pediatr. (Phila) 57, 1191–1198. 10.1177/0009922818769405 [DOI] [PubMed] [Google Scholar]
- Dai H, Catley D, Richter KP, Goggin K, Ellerbeck EF, 2018. Electronic Cigarettes and Future Marijuana Use: A Longitudinal Study. Pediatrics 141, e20173787 10.1542/peds.2017-3787 [DOI] [PubMed] [Google Scholar]
- Delnevo CD, Bover-Manderski MT, Hrywna M, 2011. Cigar, marijuana, and blunt use among US adolescents: Are we accurately estimating the prevalence of cigar smoking among youth? Prev. Med. (Baltim) 52, 475–476. 10.1016/J.YPMED.2011.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentzke AS, Creamer M, Cullen KA, Ambrose BK, Willis G, Jamal A, King BA, 2019. Vital Signs: Tobacco Product Use Among Middle and High School Students — United States, 2011–2018. MMWR. Morb. Mortal. Wkly. Rep 68, 157–164. 10.15585/mmwr.mm6806e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzman GG, 2018. Household Income: 2017. American Community Survey Briefs. ACSBR/17–01 United States Census Bureau. [Google Scholar]
- Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O’Malley PM, Galea S, Pacula R, Feng T, 2015. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. The Lancet Psychiatry 2, 601–608. 10.1016/S2215-0366(15)00217-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopfer C, 2014. Implications of marijuana legalization for adolescent substance use. Subst. Abus 35, 331–5. 10.1080/08897077.2014.943386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang HL, Chen FL, Hsu CC, Yen YY, Chen T, Huang CM, Shi HY, Hu CY, Lee CH, 2010. A multilevel-based study of school policy for tobacco control in relation to cigarette smoking among children in elementary schools: gender differences. Health Educ. Res 25, 451–463. 10.1093/her/cyq014 [DOI] [PubMed] [Google Scholar]
- Johnson J, Hodgkin D, Harris SK, 2017. The design of medical marijuana laws and adolescent use and heavy use of marijuana: Analysis of 45 states from 1991 to 2011. Drug Alcohol Depend. 170, 1–8. 10.1016/j.drugalcdep.2016.10.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lev-Ran S, Roerecke M, Le Foll B, George TP, McKenzie K, Rehm J, 2014. The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol. Med 44, 797–810. 10.1017/S0033291713001438 [DOI] [PubMed] [Google Scholar]
- Mammen G, Rehm J, Rueda S, 2016. Vaporizing cannabis through e-cigarettes: Prevalence and socio-demographic correlates among Ontario high school students. Can. J. Public Heal 107, e337–e338. 10.1111/add.13237.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantey DS, Cooper MR, Clendennen SL, Pasch KE, Perry CL, 2016. E-Cigarette Marketing Exposure Is Associated With E-Cigarette Use Among US Youth. J. Adolesc. Heal 58, 686–90. 10.1016/j.jadohealth.2016.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Mauro CM, Santaella-Tenorio J, Kim JH, Cerda M, Keyes KM, Hasin DS, Galea S, Wall M, 2016. State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug Alcohol Depend. 169, 26–32. 10.1016/j.drugalcdep.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech R, Patrick ME, O’Malley PM, Johnston LD, 2017. E-cigarette use as a predictor of cigarette smoking: results from a 1-year follow-up of a national sample of 12th grade students. Tob. Control 10.1136/tobaccocontrol-2016-053291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morean ME, Kong G, Camenga DR, Cavallo DA, Krishnan-Sarin S, 2015. High School Students’ Use of Electronic Cigarettes to Vaporize Cannabis. Pediatrics 136, 611–616. 10.1542/peds.2015-1727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Conference of State Legislatures, 2019. State Medical Marijuana Laws. Accessed 30 April 2019 http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx.
- Nicksic NE, Barnes AJ, 2019. Is susceptibility to E-cigarettes among youth associated with tobacco and other substance use behaviors one year later? Results from the PATH study. Prev. Med 121, 109–114. 10.1016/j.ypmed.2019.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicksic NE, Harrell MB, Perez A, Pasch KE, Perry CL, 2017a. Recall of E-cigarette Advertisements and Adolescent E-cigarette Use. Tob. Regul. Sci 3, 210–221. 10.18001/TRS.3.2.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicksic NE, Snell LM, Barnes AJ, 2017b. Does Exposure and Receptivity to E-cigarette Advertisements Relate to E-cigarette and Conventional Cigarette Use Behaviors among Youth ? Results from Wave 1 of the Population Assessment of Tobacco and Health Study. J. Appl. Res. Child 8: 2,3.29379673 [Google Scholar]
- Pacula RL, Powell D, Heaton P, Sevigny EL, 2015. Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. J. Policy Anal. Manage 34, 7–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokhrel P, Herzog TA, Sun P, Rohrbach LA, Sussman S, 2013. Acculturation, social self-control, and substance use among Hispanic adolescents. Psychol. Addict. Behav 27, 674–86. 10.1037/a0032836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweinsburg AD, Brown SA, Tapert SF, 2008. The Influence of Marijuana Use on Neurocognitive Functioning in Adolescents. Curr. Drug Abuse Rev 1, 99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thai ND, Connell CM, Tebes JK, 2010. Substance use among Asian American adolescents: Influence of race, ethnicity, and acculturation in the context of key risk and protective factors. Asian Am. J. Psychol 1, 261–274. 10.1037/A0021703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health & Human Services, 2016. E-cigarette Use Among Youth and Young Adults: A Report of the Surgeon General.
- Wall MM, Mauro C, Hasin DS, Keyes KM, Cerda M, Martins SS, Feng T, 2016. Prevalence of marijuana use does not differentially increase among youth after states pass medical marijuana laws: Commentary on Stolzenberg et al. (2015) and reanalysis of US National Survey on Drug Use in Households data 2002–2011. Int. J. Drug Policy 10.1016/j.drugpo.2016.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, Cummings JR, 2015. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J. Health Econ 42, 64–80. 10.1016/J.JHEALECO.2015.03.007 [DOI] [PubMed] [Google Scholar]
- Yuan M, Cross SJ, Loughlin SE, Leslie FM, 2015. Nicotine and the adolescent brain. J. Physiol 593, 3397–412. 10.1113/JP270492 [DOI] [PMC free article] [PubMed] [Google Scholar]