Abstract
AIM:
Mobile phone has been used daily by almost everyone. This Research surveyed microbial contamination of mobile phones in the faculty of Medicine Universitas Swadaya Gunung Jati and identify the most influential fungal microbial species.
METHODS:
A group of 15 samples was analysed to identify fungal isolates. The mobile phones were swabbed firmly passing its touch screen using sterile swabs then inoculated into media for fungi. Frequency distribution of isolates was calculated.
RESULTS:
There were fungal isolates as follows: Aspergillus Orchareus, Aspergillus flavus, Alternaria, Aspergillus niger, Penicillium sp., Cladosporium sp., Candida sp., Aspergillus Fumigatus, and Mucor sp. at the rate of 19, 6, 1, 3, 2, 10, 2, 52, 2%, respectively.
CONCLUSION:
The research indicates that all mobile phones were considerably having microbial infection, mostly from humans’ natural flora and also from the air and soil. This determines that it is necessary to sterilize hands prior to a contact with mobile phones since it could lead into disease transmission.
Keywords: Fungal microbioal, Mobile phone, Contamination
Introduction
Data from the last 2 decades shows that Asian countries are increasing in mobile phone usage numbers in the world [1]. It was reported in China, that in the end of june 2017, there are 724 million mobile phone users, increasing from the previous data in 2016, that only 228.3 million users. Most of the users are aged 20 to 29, which are 29.7% of all the users [2]. With its affordable price, and ease of use of applications contained in the mobile phone, makes people interested in using the mobile phone. There are various features that make the mobile phone screen more comfortable to use, such as calculators, the internet, social media, games, cameras and more. In line with the advance of technology the mobile phone becomes an indispensable accessory in social life [3], [4].
In spite of that, mobile phones can cause electromagnetic radiation effects that can cause sleeplessness, headaches, reduce memory and reduce sperm quality [5]. Conveniences of mobile phones to be carried, allowing users to store them in various places such as pants, dining tables, kitchens or even toilets. This can be potentially dangerous to health and can be a carrier of a number of microorganisms that live in every inch of the mobile phone screen [6], [7], [8]. Microbes that live and thrive on mobile phones are due to daily contact with body parts such as the face, ears, and hands and can survive on the surface of the cellphone for weeks. These microbes can cause a risk of infection from contaminated mobile phone [9], [10], one of which make nosocomial infection [11], [12]. The application of personal hygiene with hand washing habits before and after using a mobile phone is an effort to prevent disease transmission through a mobile phone [6], [13]. However, the results of the study show that the hands and instruments of health workers have the potential as carriers of microorganisms, although control and prevention efforts have been carried out such as hand hygiene, environmental decontamination, still have the potential for various objects such as laboratory equipment and mobile phones [12].
In this study, we focused on mobile phones used by laboratory officers and administrative officers in the education area, especially in the faculty of medicine.
Methods
The research subjects were 15 participants who worked in the UGJ faculty of Medicine consisting of laboratory staff, lecturers, academic staff and signed informed consent and disclosure of identification. Samples was taken using sterile cotton swab sticks, then rubbed over the surfaces of mobile phone and streaked immediately on Saburoud dextrose agar and incubated at a temperature of 35°C for 5 days and fungal growth was observed on the plate.
Results
Research is an effort to minimize the exposure of microbes that surround our lives. The habit of holding a mobile phone with an unclean hand makes the cellphone’s surface greasy and sticky, allowing variations in the microfungi colonies. environmental factors where mobile phone users live and work can affect the diversity of pathogenic microfungi on mobile phones [12],[14], [15]. The results of the analysis show that the largest Colony forming unit (CFU) value is 0.2066 CFU, while the lowest CFU value is 0.036 which is isolated from the 2 subjects of mobile phone owners.
Table 1 show some microfungi that grow are those exposed to the environment, various microfungi environmental conditions allow a large diversity of microfungi [17]. Microfungi of the genus Aspergillus and Candida have pathogenic microorganism. So that microfungi of identified pathogens can indicate that mobile phones can be a vectors towards infectious transmissions for other individuals.
Table 1.
Results of isolation and identification of pathogenic microfungi in mobile phones
| No | Code | Mikrofungi Spesies | Colony Number | Total Colony Found Unit (CFU) |
|---|---|---|---|---|
| 1 | AI | Aspergillus Orchareus | 2 | 0.0328 |
| Aspergillus flavus | 2 | |||
| Alternaria | 2 | |||
| Aspergillus niger | 2 | |||
| Penicillium sp. | 1 | |||
| Candida Sp | 1 | |||
| Aspergillus Fumigatus | 1 | |||
| 2 | AII | Aspergillus Orchareus | 2 | 0.0459 |
| Mucor sp. | 1 | |||
| Aspergillus Fumigatus | 10 | |||
| 3 | AIII | Aspergillus Orchareus | 3 | 0.2066 |
| Mucor sp. | 1 | |||
| Aspergillus Fumigatus | 58 | |||
| Penicillium sp. | 1 | |||
| 4 | AIV | Aspergillus Orchareus | 1 | 0.1082 |
| Aspergillus flavus | 1 | |||
| Cladosporium sp. | 6 | |||
| Aspergillus Fumigatus | 25 | |||
| 5 | AV | Aspergillus flavus | 10 | |
| Penicillium sp. | 3 | |||
| Candida Sp. | 1 | |||
| 6 | BI | Aspergillus Fumigatus | 26 | 0.0853 |
| 7 | BII | Aspergillus Orchareus | 1 | 0.036 |
| Mucor sp. | 1 | |||
| Cladosporium sp. | 7 | |||
| Syncephalastrum sp. | 1 | |||
| Candida Sp | 1 | |||
| 8 | BIII | Aspergillus Orchareus | 22 | 0.0885 |
| Cladosporium sp. | 1 | |||
| Penicillium sp. | 2 | |||
| Syncephalastrum sp. | 2 | |||
| 9 | BIV | Aspergillus Orchareus | 1 | 0.0098 |
| Aspergillus niger | 2 | |||
| 10 | BV | Mucor sp. | 1 | 0.0131 |
| Aspergillus niger | 1 | |||
| Aspergillus Fumigatus | 2 | |||
| 11 | C1 | Mucor sp. | 1 | 0.0328 |
| Aspergillus flavus | 1 | |||
| Cladosporium sp. | 7 | |||
| Candida Sp | 1 | |||
| 12 | C2 | Aspergillus Orchareus | 19 | 0.1279 |
| spergillus Fumigatus | 15 | |||
| Penicillium sp. | 1 | |||
| Aspergillus Versicolor | 4 | |||
| 13 | C3 | Cladosporium sp. | 3 | 0.0098 |
| 14 | C4 | Aspergillus niger | 1 | 0.0065 |
| Cladosporium sp. | 1 | |||
| 15 | C5 | Mucor sp. | 2 | 0.036 |
| Aspergillus flavus | 2 | |||
| Aspergillus niger | 3 | |||
| Aspergillus Fumigatus | 3 | |||
| Candida Sp | 1 |
Fungal growth on the mobile phone can be caused by heat is delivered mobile phone, the heat temperature is the same as the temperature of the human skin [18], [19]. fungi can grow and thrive in the humid temperature; humidity Cleaner can spur fungus grows in a very optimum.
WHO 2009 states that fungal growth can be categorized as heavy (humidity > 90%), namely Aspergillus fumigates, Mucor plumbeus, Rhizopus spp, medium (humidity 80-90%), namely Mucor circinelloides, Rhizopus oryzae, Aspergillus flavus and mild (Humidity < 80%) namely Sebi Wallemia, Aspergillus niger. Some of these microfungi were found in this study. It is possible that the air also has an influence on the growth of fungi on a mobile phone, the fungal spores float in the air can be attached to the media on the mobile phone [20].
Other literature states that the colonies were found on the mobile phone can also lead to nosocomial infections [ 21], [22]. As in this study, we can find fungal species such as Alternaria sp., Pencillium sp., Aspergillus sp., Which are known to cause respiratory infections, allergic asthma, and irritation [23]. Long and Continuous exposure to these microfungi could leads into negative effectst towards humans, although the microfungi does not by itself clinically develops the disease. The infection occured partly depending on microorganisms’ characteristics, such as intrinsic virulence resistance, and also the infective material amount. Thus, exposure to recurrent moldy material can also cause respiratory or allergic irritation in some individuals [24].
Figure 2 shows that there is a variation of CFU on mobile phones for each mobile phone user, the diverse CFU shows that this fungal microbial can grow and develop through the skin on the hands or use handheld phones by exchanging hands with other users, allowing isolate populations.
Figure 2.
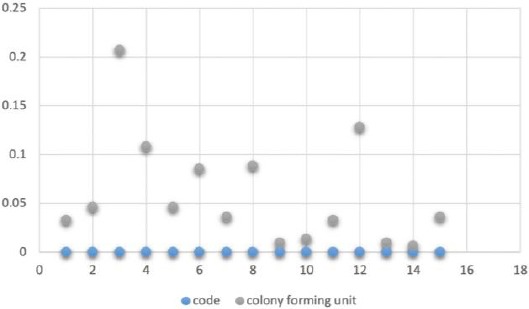
Variance colony forming unit in subject
Figure 1.
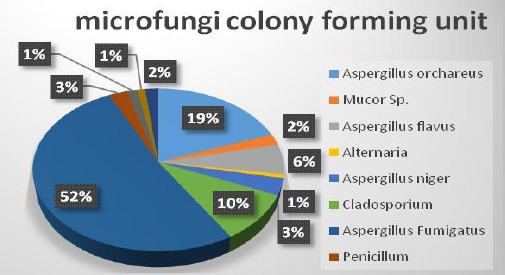
Presentage colony forming unit
Mobile phones really need sanitation procedures in order to suppress the growth of microfungi, especially developing dynamics such as Indonesia, especially in Cirebon, which is a tropical climate. Sanitation efforts on mobile phones could make microbial exposure minimal. Furthermore, tend to antibiotics usage reduction for infectious diseases [25]. It is necessary to suppress the number of infectious colonies and spores, eventhough the concentration is not high.
We can conclude:
There are 8 species in mobile phone; Apergillus orchareus, Aspergillus flavus, Aspergillus niger, Alternaria, Mucor sp, Cladosporium, Penicillum, Apergillus fumigatus
Analysis show that the largest Colony forming unit (CFU) value is 0.2066 CFU, while the lowest CFU value is 0.036
Footnotes
Funding: This research was financially supported by the University Competitive Reseach on Universitas Swadaya Gunung Jati Cirebon (UGJ), Indonesia
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Al-Abdalall AH. Isolation and identification of microbes associated with mobile phones in Dammam in eastern Saudi Arabia. Journal of Family and Community Medicine. 2010;17(1):11–14. doi: 10.4103/1319-1683.68783. https://doi.org/10.4103/1319-1683.68783 PMid:22022665 PMCid:PMC3195068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.>China Internet Network Information Center 2017. 40th Statistical Report on Internet Development in China. 2017. Retrieved September 21. http://cnnic.com.cn/IDR/ReportDownloads/201706/P0201706085237405←4.pdf .
- 3.Pal S, Juyal D, Adekhandi S, Sharma M, Prakash R, Sharma N, Rana A, Parihar A. Mobile phones:Reservoirs for the transmission of nosocomial pathogens. Advanced biomedical research. 2015;4 doi: 10.4103/2277-9175.161553. https://doi.org/10.4103/2277-9175.161553 PMid:26322292 PMCid:PMC4549928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ekrakene T, Igeleke CL. Micro-organisms associated with public mobile phones along Benin-sapele Express Way, Benin City, Edo State of Nigeria. J Appl Sci Res. 2007;3(12):2009–12. [Google Scholar]
- 5.World health organization [WHO]. Electromagnetic Fields and Public Health:Mobile Phones. Factsheet N 193. 2014. Available at: http://www.who.int/ mediacentre/factsheets/fs193/en/
- 6.Dave S, Shende K. Isolation and Identification of Microbes Associated With Mobile Phones in Durg District in Chhattisgarh Region, India. Journal of Environmental Science, Toxicology and Food Technology. 2015;1(6):71–3. [Google Scholar]
- 7.Al-Ghamdi AK, Ashshi SA, Faidah H, Shukri H, Jiman-Fatani AA. Bacterial contamination of computer keyboards and mice, elevator buttons and shopping carts. African Journal of Microbiology Research. 2011;5(23):3998–4003. https://doi.org/10.5897/AJMR11.770. [Google Scholar]
- 8.Brady RR, Hunt AC, Visvanathan A, Rodrigues MA, Graham C, Rae C, Kalima P, Paterson HM, Gibb AP. Mobile phone technology and hospitalized patients:a cross-sectional surveillance study of bacterial colonization, and patient opinions and behaviours. Clinical Microbiology and Infection. 2011;17(6):830–5. doi: 10.1111/j.1469-0691.2011.03493.x. https://doi.org/10.1111/j.1469-0691.2011.03493.x PMid:21615607. [DOI] [PubMed] [Google Scholar]
- 9.Cosgrove K, Coutts G, Jonsson M, Tarkowski A, Kokai-Kun JF, Mond JJ, Foster SJ. Catalase (KatA) and alkyl hydroperoxide reductase (AhpC) have compensatory roles in peroxide stress resistance and are required for survival, persistence, and nasal colonization in Staphylococcus aureus. Journal of bacteriology. 2007;189(3):1025–35. doi: 10.1128/JB.01524-06. https://doi.org/10.1128/JB.01524-06 PMid:17114262 PMCid:PMC1797328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaibenjawong P, Foster SJ. Desiccation tolerance in Staphylococcus aureus. Archives of microbiology. 2011;193(2):125–35. doi: 10.1007/s00203-010-0653-x. https://doi.org/10.1007/s00203-010-0653-x PMid:21088825. [DOI] [PubMed] [Google Scholar]
- 11.Ulger F, Dilek A, Esen S, Sunbul M, Leblebicioglu H. Are healthcare workers'mobile phones a potential source of nosocomial infections?Review of the literature. The journal of infection in developing countries. 2015;9(10):1046–53. doi: 10.3855/jidc.6104. https://doi.org/10.3855/jidc.6104 PMid:26517478. [DOI] [PubMed] [Google Scholar]
- 12.Beckstrom AC, Cleman PE, Cassis-Ghavami FL, Kamitsuka MD. Surveillance study of bacterial contamination of the parent's cell phone in the NICU and the effectiveness of an anti-microbial gel in reducing transmission to the hands. Journal of Perinatology. 2013;33(12):960–963. doi: 10.1038/jp.2013.108. https://doi.org/10.1038/jp.2013.108 PMid:24008502. [DOI] [PubMed] [Google Scholar]
- 13.Rahi P, Kurli R, Pansare AN, Khairnar M, Jagtap S, Patel NB, Dastager SG, Lawson PA, Shouche YS. Microbacterium telephonicum sp. nov., isolated from the screen of a cellular phone. Int J Syst Evol Microbiol. 2018;68(4):1052–8. doi: 10.1099/ijsem.0.002622. https://doi.org/10.1099/ijsem.0.002622 PMid:29458489. [DOI] [PubMed] [Google Scholar]
- 14.Brady RR, Hunt AC, Visvanathan A, Rodrigues MA, Graham C, Rae C, Kalima P, Paterson HM, Gibb AP. Mobile phone technology and hospitalized patients:a cross-sectional surveillance study of bacterial colonization, and patient opinions and behaviours. Clin. Microbiol. Infect. 2011;17(6):830–5. doi: 10.1111/j.1469-0691.2011.03493.x. https://doi.org/10.1111/j.1469-0691.2011.03493.x PMid:21615607. [DOI] [PubMed] [Google Scholar]
- 15.Ulger F, Esen S, Dilek A, Yanik K, Gunaydin M, Leblebicioglu H. Are we aware how contaminated our mobile phones with nosocomial pathogens. Ann Clin Microbiol Antimicrob. 2009;8:1–4. doi: 10.1186/1476-0711-8-7. https://doi.org/10.1186/1476-0711-8-7 PMid:19267892 PMCid:PMC2655280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beckstrom AC, Cleman PE, Cassis-Ghavami FL, Kamitsuka MD. Surveillance study of bacterial contamination of the parent's cell phone in the NICU and the effectiveness of an anti-microbial gel in reducing transmission to the hands. J Perinatol. 2013;33(12):960–963. doi: 10.1038/jp.2013.108. https://doi.org/10.1038/jp.2013.108 PMid:24008502. [DOI] [PubMed] [Google Scholar]
- 17.Meadow JF, Altrichter AE, Green JL. Mobile phones carry the personal microbiome of their owners. PeerJ. 2014;2:e447. doi: 10.7717/peerj.447. https://doi.org/10.7717/peerj.447 PMid:25024916 PMCid:PMC4081285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pérez-Cano HJ, Santos MR, Moreno BC. Microbiota in mobile phones of medical ophthalmologists. Archsocespoftalmol. 2019;94(2):55–59. doi: 10.1016/j.oftal.2018.11.006. https://doi.org/10.1016/j.oftale.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 19.Kotris I, Drenjancevic D, Talapko J, Bukovski S. Identification of microorganisms on mobile phones of intensive care unit health care workers and medical students in the tertiary hospital. Med Glas (Zenica) 2017;14:85–90. doi: 10.17392/878-16. [DOI] [PubMed] [Google Scholar]
- 20.WHO. Dampness and Mould. WHO Guidel Indoor Air Qual. 2009 [Google Scholar]
- 21.Akinyemi K, Atapu A, Adetona O, Coker A. 2009. The potential roleof mobile phones in the spread of bacterial infections. J Infect Dev Ctries. 2009;3:628–32. doi: 10.3855/jidc.556. https://doi.org/10.3855/jidc.556 PMid:19801807. [DOI] [PubMed] [Google Scholar]
- 22.Pollard. Evaluating Passive and Active Source Terms at Green Waste Facility For Improved Risk Assesment. Bioaerosol Releases From Compost Facil. 2006. Fletcher. Journal University of Leeds:The Importance of Bioaerosols in Hospital Infections and the Potential for Control using Germicidal Ultraviolet Irradiation. 2010 [Google Scholar]
- 23.Eduard W. Fungal spores:a critical review of the toxicological and epidemiological evidence as a basis for occupational exposure limit setting. Critical reviews in toxicology. 2009;39(10):799–864. doi: 10.3109/10408440903307333. https://doi.org/10.3109/10408440903307333 PMid:19863384. [DOI] [PubMed] [Google Scholar]
- 24.Brandt M, Warnock D. Clinical Mycology:Laboratory Apects Of Medical Mycology. 2003 [Google Scholar]
- 25.Bloomfield SF, Rook GA, Scott EA, Shanahan F, Stanwell-Smith R, Turner P. Time to abandon the hygiene hypothesis:new perspectives on allergic disease, the human microbiome, infectious disease prevention and the role of targeted hygiene. Perspectives in public health. 2016;136(4):213–24. doi: 10.1177/1757913916650225. https://doi.org/10.1177/1757913916650225 PMid:27354505 PMCid:PMC4966430. [DOI] [PMC free article] [PubMed] [Google Scholar]


