Abstract
Study Objective:
To identify predictors of anticipated pain with intrauterine device (IUD) insertion in adolescents and young women.
Design:
We performed linear regression to identify demographic, sexual/gynecologic history, and mood covariates associated with anticipated pain using visual analog pain scores (VAS) collected as part of a single-blind randomized trial of women receiving a 13.5 mg levonorgestrel IUD.
Setting:
Three academic family planning clinics in Philadelphia PA.
Participants:
Ninety-three adolescents and young adult women age 14–22.
Intervention:
Participants received either a 1% lidocaine or sham paracervical block.
Main Outcome Measures:
Anticipated pain measured using a Visual Analog Scores (VAS) before and perceived pain at 6 time points during the IUD insertion procedure.
Results:
Black or African-American participants had a median anticipated pain score of 68 (IQR 52, 83), White participants had a median anticipated pain of 51 (IQR 35, 68), while participants of other races had a median anticipated pain score of 64 (IQR 36, 73); p=0.012. In multivariate analysis, race was the only covariate that significantly predicted anticipated pain at IUD insertion. Women with anticipated pain scores above the median had significantly higher perceived pain during all timepoints of the IUD insertion procedure.
Conclusions:
Increased anticipated pain is associated with increased perceived pain with IUD insertion. Black adolescent women experience greater anticipated pain with IUD insertion. This population may benefit from counseling and clinical measures to reduce this barrier to IUD use.
Keywords: Intrauterine Devices, Contraceptive Devices, Adolescent, Pain
Introduction:
Among sexually active women of reproductive age, adolescents and young adult women have the highest rates of unintended pregnancy.1 Given the public health demands and personal implications of teen pregnancy, the importance of highly effective contraception in this population is paramount. However, while intrauterine devices (IUDs) are twenty times more effective than oral contraceptives, oral contraceptives remain the most commonly used form of contraception among adolescents and young adult women. Only 8.2% of sexually active adolescents (age 15 to 19) use long-acting reversible contraceptives (IUDs and implants) compared to 13.1% of sexually active women between ages 20 to 29.2
Varying levels of contraceptive knowledge among adolescent women may be barrier to IUD use. Overall, fewer than half of all young women between the ages of 14 and 27 are aware of IUDs, but those with prior knowledge of IUDs are more likely to select an IUD as their contraceptive choice than those without.3 Adolescent women frequently learn about IUDs informally through social references who shape their view of IUDs. These references often hold negative perspectives,4 and offer anecdotal knowledge of varying depth and accuracy, which shape adolescents’ interest in using these methods.5
One of the most pervasive barriers to IUD placement in adolescents is fear. Among adolescents interviewed for a study of IUD acceptability, fears related to having an IUD placed was almost universal. These fears took multiple forms, including fear of pain during insertion, as well as fear of expulsion, having a foreign body and potential physical harm caused by an IUD. Adolescents indicate that these fears pose a major barrier to seeking an IUD.6 The fear of pain during IUD insertion is not only a significant barrier to choosing this method of contraception but is also a likely contributor to pain experienced during IUD insertion. Women with higher levels of anticipated pain prior to IUD insertion are more likely to have higher experienced pain during IUD insertion.7, 8, 9, 10, 11
It has been shown that additional counseling prior to IUD insertion can reduce pain complaints with IUD insertion.12, 13 Identifying patients with high anticipated pain is challenging, yet this population may benefit most from interventions to reduce pain during IUD insertion. Moreover, although prior research has shown that anticipated pain predicts pain experienced at IUD deployment, the impact of anticipated pain on pain perceived throughout all steps of an IUD insertion procedure has not been explored.14 In this study, our objectives were to identify predictors of anticipated pain with IUD insertion in adolescents and young women, and to characterize the association between anticipated pain and perceived pain during each step of IUD insertion procedures in women participating in a randomized clinical trial of a pain management strategy during IUD insertion.
Materials and Methods:
Study Design
This study was a secondary analysis of data from a multisite, single-blind, randomized trial comparing pain before and during 6 IUD insertion timepoints in women who received a paracervical block of 10 mL 1% lidocaine, or a sham block. The trial was conducted at three clinics in Philadelphia, Pennsylvania from March 2015 to July 2016. The protocol is available upon request. Institutional Review Board (IRB) approval was obtained from the Children’s Hospital of Philadelphia (CHOP), the IRB of record, the Hospital of the University of Pennsylvania and Thomas Jefferson University, all of which performed study visits. Approval was also obtained from AccessMatters, a non-profit organization which funds Title X clinics in southeastern Pennsylvania, which allowed study recruitment flyers to be posted in Title X clinics that refer adolescents to CHOP for IUD insertions. The trial was registered with Clinicaltrials.gov ().
Recruitment, Eligibility and Consent
Women presenting to an enrolling study site requesting a hormonal IUD were asked by a clinician if they were interested in talking with research staff about the study. Interested women who saw a recruitment flyer at a non-enrolling site called the study coordinator who described the study and scheduled a study visit. Patients were eligible for inclusion if they were between 14 and 22 years of age, nulliparous, not currently pregnant, had not been pregnant in the 6 weeks prior to enrollment, interested in the levonorgestrel 13.5mg IUD and English speaking. The cutoff age of 22 years, rather than 24 years, was chosen to minimize the number of older, young adult women. Patients were excluded if they did not meet medical eligibility criteria for an IUD, had a contraindication to taking amino-amide anesthetics or non-steroidal anti-inflammatory agents, were unwilling to be randomized, were at high risk for pregnancy, had used narcotics or benzodiazepine in the prior 24 hours, had previously used an IUD, or had previously had an unsuccessful IUD insertion. Women could enroll at a later date if the inclusion criteria were not initially met. Written informed consent was obtained from all participants.
Trial Procedures and Treatment Group Description
Participants completed a questionnaire assessing demographic characteristics and their medical and reproductive history. All participants received counseling prior to IUD insertion including a description of the risks and benefits of IUD placement and use, risk of pregnancy with IUD placement, and continued risk of STD transmission. Randomization was performed by a research coordinator in the Research Data Capture (REDCap) software in block sizes of 4 with stratification by age (14 – 17 or 18 – 22 years), race, and recruitment site, after completion of the demographic questionnaire. Only participants were blinded to group assignment.
IUD insertion was performed by multiple clinicians. After IUD insertion, clinicians completed a questionnaire assessing procedural details including uterine size and depth, need for dilation or ultrasound guidance and adverse events. Clinicians assessed patient anxiety by asking if the patient’s general affect seemed “pleasant and appropriately engaging” or “anxious.” A post-procedure questionnaire was administered to participants by a research coordinator to rate their satisfaction with and discomfort during the procedure.
Dependent Variables
Measurements of anticipated pain were collected using a 100mm Visual Analog Scale (VAS). Anticipated pain scores were collected as part of the initial questionnaire. Participants were asked, “how much pain do you think you’ll experience?” To collect VAS scores, research staff held an iPad in front of the participant during the IUD insertion process to facilitate the participant entering the data. When asked by research staff, participants first tapped a line on the iPad indicating their pain level, from “no pain” (0mm) to “worst pain in my life” (100mm), and then confirmed that the value generated was accurate before the data was transmitted to the database. We defined participants with high or low anticipated pain based on whether their VAS anticipated pain score was above or below the median value.
Using the same 100mm VAS scale, perceived pain was measured at seven points throughout the IUD insertion process: at baseline (prior to placement in dorsal lithotomy position), immediately after speculum placement, at tenaculum placement, paracervical or sham block administration, uterine sounding, IUD insertion, and at speculum removal.
Predictor Variables
We included the following baseline demographic variables in our analysis: age, race, ethnicity, marital status, insurance status, and education level. We included sexual and reproductive history variables: whether participants had ever engaged in penile-vaginal intercourse, if they had had a prior pregnancy, whether they had ever received a gynecologic exam with a speculum, and if they had a history of a prior sexually transmitted infection. We also included the 4-item Patient Health Questionnaire-4 (PHQ-4), a screening questionnaire that consists of a 2-item depression scale and a 2-item anxiety scale.
Analysis
Participants were treated as a single group, analyzing the variable of anticipated pain prior to IUD insertion as the exposure of primary interest. We performed univariate analysis of the median anticipated pain VAS scores by predictor variables hypothesized to influence the outcome: age category (14–17 years versus 18–22 years), race (Black or African American, White, or other), PHQ-4 (screen negative versus positive), randomization group (sham block versus lidocaine block), prior sexual activity (yes versus no), and prior speculum exam (yes versus no). Between-group differences were compared using the Student t-test, ANOVA, and Wilcoxon rank-sum tests, as appropriate. Using these variables, we performed a backward stepwise linear regression analysis to determine predictors of anticipated pain, and retained variables in the model that yielded p<0.05.
We assessed differences in perceived pain scores at each point of the IUD insertion process by anticipated pain category. A linear mixed effects regression model with robust variance (generalized estimating equation) assumption was used to adjust for within women correlation resulting from repeated measures. This model was used to compare estimates of perceived pain in the low and high anticipated pain groups at each of the 7 procedural steps in an unadjusted analysis and was then adjusted for the variables noted to be significant in the univariate analysis. All analyses were performed using SAS statistical software (Cary, NC).
Results:
Ninety-five participants enrolled in the study between March 2015 and July 2016, and ninety-three were included in the analysis. One was removed due to missing insurance information and another due to a missing pain score at IUD insertion. All participants had successful IUD insertion with no adverse events. Mean participant age was 19.4 with most participants (80.0%) between the ages of 18 and 22. Almost half of the participants were non-Hispanic White (47.4%) and more than a third were Black or African American (36.0%). The majority were non-Hispanic. The vast majority of participants were never married and were not living with a partner (95.8%), and most had some college or higher education (67.4%). Most participants had private insurance (66.0%).
The majority of participants had been sexually active (91.6%), and 4 participants had previously been pregnant (4.2%). The majority had used hormonal birth control at some time (79.0%) and 43% were currently using hormonal birth control. The majority reported a prior gynecological exam (69.5%). Nearly a quarter of participants (24.2%) had a history of a sexually transmitted infection, including chlamydia (10.5%), gonorrhea (2.1%), genital warts, genital herpes (1%), HIV (1%), pelvic inflammatory disease (3.2%), syphilis (1%), and trichomonas (6.3%). The majority of participants were not clinically depressed (95%) or clinically anxious (93%), although 10% of participants were rated as anxious by the health care provider (Table 1).14
Table 1).
Demographic distribution of the data overall, and by level of anticipated pain.
| Variable | Total Sample n=95 (%) | Low anticipated pain N=47 (%) |
High anticipated pain n=48 (%) | P value | ||
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age group (y) | 0.31 | |||||
| 14–17 | 19 (20) | 7 (14.9) | 12 (25) | |||
| 18–22 | 76 (80) | 40 (85.1) | 36 (75) | |||
| Race category | ||||||
| Black or African American race | 34 (36) | 13 (27.7) | 21 (43.8) | 0.1 | ||
| Non Hispanic ethnicity | 86 (91) | 43 (91.5) | 43 (89.6) | 1 | ||
| Marital Status | 1 | |||||
| Never married and not living with a partner | 91 (96) | 46 (97.9) | 45 (93.8) | |||
| Never married and living with a partner | 3 (3) | 1(2.1) | 2 (4.2) | |||
| Married and living with a partner | 1 (1) | 0 (0) | 1 (2.1) | |||
| Education | 0.81 | |||||
| Less than high school degree | 22 (23) | 10 (21.3) | 12 (25) | |||
| High school degree of equivalent | 9 (10) | 4 (8.5) | 5 (10.4) | |||
| Some college | 51 (54) | 28 (59.6) | 23 (47.9) | |||
| Associate degree | 1 (1) | 0 (0) | 1 (2.1) | |||
| Bachelor degree or higher | 12 (12.6) | 5 (10.6) | 7 (14.6) | |||
| Insurance | 0.19 | |||||
| Public insurance | 29 (30) | 11 (23.4) | 18 (37.5) | |||
| Private insurance | 62 (65) | 33 (70.2) | 30 (62.5) | |||
| None or other | 3 (3) | 1 (2) | 0 (0) | |||
| Mood assessment | ||||||
| Positive SPHQ-4 depression screen | 12 (13) | 9 (19.2) | 3 (6.3) | 0.07 | ||
| Reproductive and gynecologic history | ||||||
| Ever sexually active | 87 (92) | 42 (89.4) | 45 (93.8) | 0.49 | ||
| Prior pregnancy | 4 (4.2) | 1 (2.1) | 3 (6.3) | 0.61 | ||
| Ever had a speculum exam | 42 (44.2) | 18 (38.3) | 24 (50) | 0.3 | ||
| History of prior sexually transmitted infection | 23 (24.2) | 9 (19.2) | 14 (29.2) | 0.26 | ||
| Randomization group | 0.15 | |||||
| Lidocaine block | 47 (49) | 27 (57) | 20 (41.7) | |||
| Sham Block | 48 (51) | 20 (43) | 20 (58.3) | |||
In univariate analysis, increased familiarity with vaginal exams, prior sexual activity, prior pregnancy, past or current hormonal contraception use, prior history of sexually transmitted infections, and number of prior gynecological exams did not predict anticipated pain. The median anticipated pain score in participants with no prior sexual activity was 42 (IQR 23, 66), compared with 63 (IQR 39,72) in those with prior sexual activity (p=0.10). The median anticipated pain score in participants with no prior speculum exam was 63 (IQR 39,72) as compared with 53.5 (IQR 19,69.5) in those with prior speculum exam (p=0.49). Participants with a positive PHQ-4 screen for depression/anxiety had a median anticipated pain score of 63 (IQR 38, 72) as compared to 57 (IQR 35.5, 65.5) in those who did not screen positive for depression (p=0.46).
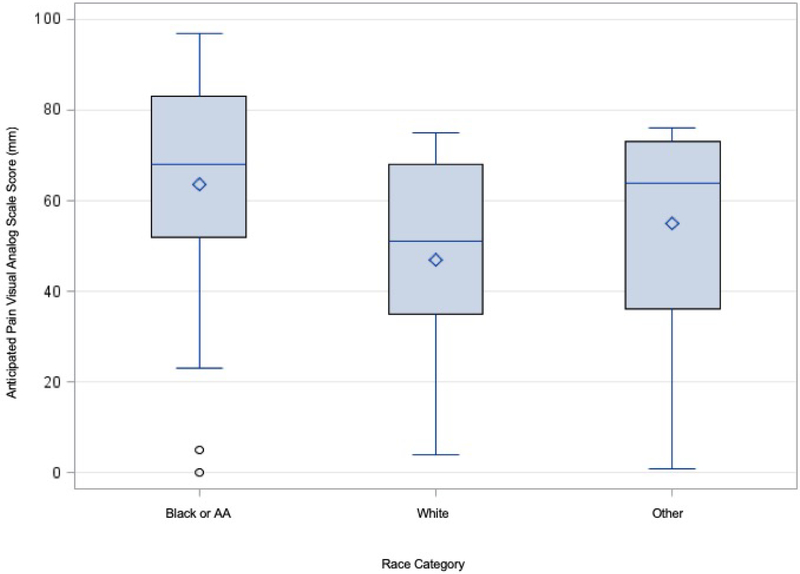
Univariate analysis identified age and race as potential predictors of anticipated pain of IUD insertion. Black or African-American participants had a median anticipated pain score of 68 (IQR 52, 83), White participants had a median anticipated pain of 51 (IQR 35, 68), while participants of other races had a median anticipated pain score of 64 (IQR 36, 73); p=0.012 (Figure 1). Younger participants (ages 14–17 years) had a median anticipated pain score of 69 (IQR 46, 86), while older participants (ages 18–22 years) had a median anticipated pain score of 59 (IQR 36, 71), p=0.016.
Figure 1).
Anticipated pain of IUD insertion as measured by a 100 mm Visual Analog Scale, stratified by race category. The box represents the interquartile range, the horizontal line represents the median, and diamonds represent the mode. Whiskers represent the scores outside the interquartile range. Circles indicate outliers.
The overall median anticipated VAS pain score in the full cohort was 63 (IQR 38,72). We categorized those with an anticipated pain score less than 63 as having low anticipated pain, and those with anticipated pain score of greater than or equal to 63 as having high anticipated pain. In the full cohort, backward stepwise linear regression identified only randomization group (p<0.001) and anticipated pain score (p<0.001) as predictors of perceived pain at the time of IUD insertion.
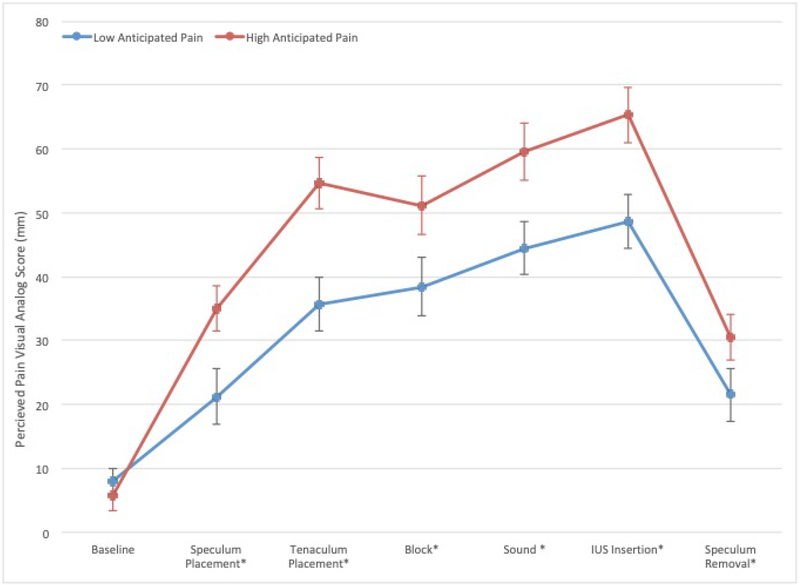
Using GEE analysis for repeated measures, we found that at each IUD insertion procedure step except for the baseline assessment, participants with high anticipated pain scores had significantly higher perceived pain scores (Figure 2), even when adjusting for race and age. After adjusting for treatment group, women with high anticipated pain had a mean perceived pain score of 65±29mm, and those with low anticipated pain had adjusted mean perceived pain score of 44.5±28mm at the time of IUD insertion (p<0.003).
Figure 2).
Adjusted perceived pain VAS scores (±SE) in women with high and low anticipated pain. High anticipated pain scores were those above the median (red); low anticipated pain scores were those below the median (blue). VAS scores were adjusted for race, age, and randomization group. Difference in VAS scores with P<0.05 are marked with a *.
Backward stepwise linear regression analysis including all above-noted variables showed that only race category was associated with anticipated pain. In a linear regression model that adjusted for age as a confounder, Black participants had an anticipated VAS pain score that was 15.1 mm higher on average compared to White participants (p=0.017), and those of other races had an anticipated VAS pain scores that was 6.4 mm higher on average than White participants (p=0.38).
Discussion:
In this secondary analysis of a randomized controlled trial, Black race was the only predictor of higher levels of anticipated pain. Age, mood, sexual experience, familiarity with gynecological exams, prior history of a sexually transmitted infection, and gynecological history did not predict anticipated pain at any of the steps during the IUD insertion process. The association between Black race and anticipated pain is not likely to have a biological basis. Rather, this likely stems from complex social and structural realities within the lived experiences of Black women in the United States. For example, Black patients are more likely to distrust the medical system, due to a history of exploitation and racial discrimination in the healthcare in the United States.15, 16 It is well documented African American women today unequally bear the burdens of maternal mortality, infant mortality, and sexually transmitted infections.17 They may therefore experience heightened anticipated pain and anxiety during medical encounters.18 Physician beliefs regarding pain severity and underreporting of pain among patients from minority racial groups are thought to contribute to less adequate treatment of pain in minority patients.19 Moreover, Black and Hispanic children experience adverse childhood events at higher rates than White children, and these adverse childhood events have negative mental and physical health effects that may persist throughout the life course, notably increased heightening self-reported pain and anxiety.20, 21 Taken together, these findings support the notion that disparities in anticipated pain among minority populations are likely multifactorial, and result from both systemic and personal complexities that impact both acceptance and receipt of pain management modalities and heighten pain awareness.22
Provider underestimation of pain and anxiety during IUD insertion has been previously documented and was corroborated in the current study, as only 10% of patients were noted to be anxious by providers. When patients and providers were asked to estimate the pain experienced by women undergoing an IUD insertion using a 100mm VAS, the mean patient reported pain score was 64.8 mm compared to the mean pain score estimated by providers of 35.3 mm.23 Given that providers may find it difficult to accurately assess anxiety and pain among women undergoing IUD placement, we recommend that providers ask all women about their anxiety, anticipated pain, preferences regarding pain management, and actual experienced pain level. Providers should offer evidence-based pain management interventions when warranted.
Several effective pharmacologic interventions to reduce pain with IUD insertion exist, including pre-procedure oral naproxen, and lidocaine-prilocaine cream.24 Tramadol has also shown effectiveness in pain reduction, but given recommendations to use the minimum effective opioid dose to reduce unintended long-term use, we recommend avoiding narcotic receptor agonists in favor of other effective pain management strategies.25 Non-pharmacologic interventions to increase understanding and reduce anxiety should always be employed, including counseling about effectiveness, the insertion and removal process, risks, benefits, costs, effect on fertility, menstrual effects, length of use, and similarities and differences among the various types of IUDs.13 Finally, efforts to increase provider awareness of racial disparities in pain experience and training to increase racial sensitivity are appropriate.
We found that anticipated pain predicted perceived pain at every step of the IUD insertion process in adolescent and young adult women. Notably, having high anticipated pain resulted in perceived pain levels similar to women who did not receive a paracervical block. Our findings agree with previous studies examining the association between anticipated pain and experienced pain with IUD insertion.7, 9, 10, 11, 26 For example, an analysis of 1,149 subjects in the CHOICE project receiving an IUD found that for every one point increase in the level of anticipated pain on a 10-point VAS scale, the likelihood of experiencing significant pain increased by 19%.7
More broadly, anticipated pain has been found to be a predictor of experienced pain in many gynecological and obstetrical,27 general surgical,28 and dental procedures.29,30 In a qualitative analysis of 21 participants undergoing urodynamic studies, Shaw et al. identified anxiety as a common concern in patients undergoing procedures,31 which likely contributed to experienced discomfort. While a definitive mechanism of the effect of anticipated pain on perceived pain has not been established, emerging evidence suggests that both psychological and biological phenomena are involved. Current recommended approaches to pain management consider the contributions of psychological, biological, cognitive, behavioral, affective, and social factors in the variability of pain experiences.32 The strengths of our study include the use of a data from a high quality randomized controlled trial with a racially diverse population. However, this was an overall young population, limiting generalizability to older age groups. Only the 13.5 mg IUD was studied; it is possible that anticipated pain levels noted for this IUD may not be generalizable to other IUD types as the 13.5mg IUD is a smaller device marketed at adolescent women for this reason. Provider characteristics that might have influenced patient comfort before and during the procedure, such as demographic factors and level of experience, were not collected or analyzed. Finally, this was a secondary analysis, limiting the demographic, sexual/gynecologic history, and mood variables available for analysis to those previously collected, and the study cannot conclusively reject the association between these variables and anticipated pain.
Further investigation is required to identify the best techniques to reduce anticipated pain with IUD insertion and to identify which aspects of counseling are most effective at minimizing anticipated pain and anxiety. In addition, it remains unclear whether increased education is effective across all demographic groups. Although the best method of counseling remains undefined, identification of patients who are more likely to anticipate pain with IUD insertion, such as African American patients, would enable health care providers to provide additional education and sensitivity prior to IUD insertion in an effort to reduce anticipated pain and ensure the use of pharmacological agents to reduce experienced pain.
Acknowledgments:
This project was supported by an investigator-initiated grant from Bayer Healthcare Inc. (AYA) and the Health Services Research Administration and Women’s Reproductive Health Research award number K12-HD001265–19 (SS).
Footnotes
Publisher's Disclaimer: This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
An abstract for this study was presented as a poster at the American College of Obstetricians and Gynecologists Annual Clinical and Scientific Meeting on May 4th, 2019 in Nashville TN.
Disclosure/Conflict of Interest:
TA Hunter has nothing to disclose. SR Sonalkar has nothing to disclose. CA Schreiber is a consultant for Exeltis Pharmaceuticals and received research funding from Bayer Pharmaceuticals, Medicines360, ContraMed, and NICHD. LK Perriera has nothing to disclose. MD Sammel has nothing to disclose. AY Akers is a consultant for the Merck HPV advisory board and is a member of the Mylan Inc Women’s Health Advisory Board.
References:
- 1.Finer LB. Unintended pregnancy among U.S. adolescents: accounting for sexual activity. J Adolesc Health 2010;47(3):312–4. [DOI] [PubMed] [Google Scholar]
- 2.Daniels K. Current Contraceptive Status Among Women Aged 15–49: United States, 2015–2017. 2018;(327):8. [PubMed] [Google Scholar]
- 3.Fleming KL, Sokoloff A, Raine TR. Attitudes and beliefs about the intrauterine device among teenagers and young women. Contraception 2010;82(2):178–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubin SE, Felsher M, Korich F, Jacobs AM. Urban Adolescents’ and Young Adults’ Decision-Making Process around Selection of Intrauterine Contraception. J Pediatr Adolesc Gynecol 2016;29(3):234–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoopes AJ, Ahrens KR, Gilmore K, et al. Knowledge and Acceptability of Long-Acting Reversible Contraception Among Adolescent Women Receiving School-Based Primary Care Services. Journal of Primary Care & Community Health 2016;7(3):165–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Potter J, Rubin SE, Sherman P. Fear of intrauterine contraception among adolescents in New York City. Contraception 2014;89(5):446–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dina B, Peipert L, Zhao Q, Peipert JF. Anticipated pain as a predictor of discomfort with intrauterine device placement. Am J Obstet Gynecol 2017; [DOI] [PubMed] [Google Scholar]
- 8.Lopez LM, Bernholc A, Zeng Y, et al. Interventions for pain with intrauterine device insertion. Cochrane Database Syst Rev 2015;(7):CD007373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldstuck ND, Matthews ML. A comparison of the actual and expected pain response following insertion of an intrauterine contraceptive device. Clin Reprod Fertil 1985;3(1):65–71. [PubMed] [Google Scholar]
- 10.Murty J. Use and effectiveness of oral analgesia when fitting an intrauterine device. J Fam Plann Reprod Health Care 2003;29(3):150–1. [DOI] [PubMed] [Google Scholar]
- 11.Doty N, MacIsaac L. Effect of an atraumatic vulsellum versus a single-tooth tenaculum on pain perception during intrauterine device insertion: a randomized controlled trial. Contraception 2015;92(6):567–71. [DOI] [PubMed] [Google Scholar]
- 12.Whitaker AK, Endres LK, Mistretta SQ, Gilliam ML. Postplacental insertion of the levonorgestrel intrauterine device after cesarean delivery vs. delayed insertion: a randomized controlled trial. Contraception 2014;89(6):534–9. [DOI] [PubMed] [Google Scholar]
- 13.Newton JR, Reading AE. The effects of psychological preparation on pain at intrauterine device insertion. Contraception 1977;16(5):523–32. [DOI] [PubMed] [Google Scholar]
- 14.Akers AY, Steinway C, Sonalkar S, et al. Reducing Pain During Intrauterine Device Insertion: A Randomized Controlled Trial in Adolescents and Young Women. Obstet Gynecol 2017;130(4):795–802. [DOI] [PubMed] [Google Scholar]
- 15.Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/Ethnic Differences in Physician Distrust in the United States. Am J Public Health 2007;97(7):1283–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Armstrong K, Putt M, Halbert CH, et al. Prior Experiences of Racial Discrimination and Racial Differences in Health Care System Distrust. Med Care 2013;51(2):144–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prather C, Fuller TR, Jeffries WL, et al. Racism, African American Women, and Their Sexual and Reproductive Health: A Review of Historical and Contemporary Evidence and Implications for Health Equity. Health Equity 2018;2(1):249–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Corbie-Smith G, Thomas SB, St George DMM. Distrust, race, and research. Arch Intern Med 2002;162(21):2458–63. [DOI] [PubMed] [Google Scholar]
- 19.Mossey JM. Defining racial and ethnic disparities in pain management. Clin Orthop Relat Res 2011;469(7):1859–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sachs-Ericsson NJ, Sheffler JL, Stanley IH, Piazza JR, Preacher KJ. When Emotional Pain Becomes Physical: Adverse Childhood Experiences, Pain, and the Role of Mood and Anxiety Disorders. J Clin Psychol 2017;73(10):1403–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slopen N, Shonkoff JP, Albert MA, et al. Racial Disparities in Child Adversity in the U.S. American Journal of Preventive Medicine 2016;50(1):47–56. [DOI] [PubMed] [Google Scholar]
- 22.Green CR, Anderson KO, Baker TA, et al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med 2003;4(3):277–94. [DOI] [PubMed] [Google Scholar]
- 23.Maguire K, Morrell K, Westhoff C, Davis A. Accuracy of providers’ assessment of pain during intrauterine device insertion. Contraception 2014;89(1):22–4. [DOI] [PubMed] [Google Scholar]
- 24.Mody SK, Farala JP, Jimenez B, Nishikawa M, Ngo LL. Paracervical Block for Intrauterine Device Placement Among Nulliparous Women: A Randomized Controlled Trial. Obstet Gynecol 2018;132(3):575–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah A, Hayes CJ, Martin BC. Factors Influencing Long-Term Opioid Use Among Opioid Naive Patients: An Examination of Initial Prescription Characteristics and Pain Etiologies. J Pain 2017;18(11):1374–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Allen RH, Bartz D, Grimes DA, Hubacher D, O’Brien P. Interventions for pain with intrauterine device insertion. Cochrane Database Syst Rev 2009;(3):CD007373. [DOI] [PubMed] [Google Scholar]
- 27.Pan PH, Tonidandel AM, Aschenbrenner CA, Houle TT, Harris LC, Eisenach JC. Predicting Acute Pain after Cesarean Delivery Using Three Simple Questions. Anesthesiology 2013;118(5):1170–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Logan DE, Rose JB. Is Postoperative Pain a Self-Fulfilling Prophecy? Expectancy Effects on Postoperative Pain and Patient-Controlled Analgesia Use Among Adolescent Surgical Patients. J Pediatr Psychol 2005;30(2):187–96. [DOI] [PubMed] [Google Scholar]
- 29.Watkins CA, Logan HL, Kirchner HL. Anticipated and experienced pain associated with endodontic therapy. J Am Dent Assoc 2002;133(1):45–54. [DOI] [PubMed] [Google Scholar]
- 30.Beaudette JR, Fritz PC, Sullivan PJ, Piccini A, Ward WE. Investigation of factors that influence pain experienced and the use of pain medication following periodontal surgery. J Clin Periodontol 2018;45(5):578–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shaw C, Williams K, Assassa PR, Jackson C. Patient satisfaction with urodynamics: a qualitative study. J Adv Nurs 2000;32(6):1356–63. [DOI] [PubMed] [Google Scholar]
- 32.Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull 2007;133(4):581–624. [DOI] [PubMed] [Google Scholar]