Nearly one-third of individuals in the United States meet lifetime criteria for an alcohol use disorder (AUD)(Grant et al., 2015). Fortunately, most individuals who develop an AUD will eventually resolve their problem, with “recovery” defined in various ways across studies (Dawson et al., 2005; Tucker et al., 2006, 2009; Witkiewitz et al., 2019). Having scientifically sound definitions of recovery from AUD that can be shared across population and individual levels of analysis is fundamental to recovery research. Alcoholics Anonymous (AA; 1939) advanced the seminal definition of recovery as a spiritual journey to overcome the effects of uncontrollable alcohol use and to rebuild one’s inner and outer life, a lifelong journey for which abstinence was necessary, but not sufficient to effect this life-altering transformation. Eighty years of subsequent research and practice in the alcohol field has focused nearly exclusively on the drinking practices dimension (i.e., abstinence) included in the AA definition as the defining feature of recovery, to the neglect of considering improvements in well-being, functioning, and life circumstances. Abstinence may be a necessary recovery component for some individuals with AUD, yet research indicates that it is not essential for all, and positive changes in functioning and well-being often are more fundamental elements. These issues are very much intertwined in the Fan et al. (2019) study, which has many strengths that advance understanding of positive changes related to AUD recovery, but also raises questions for future research and continued development of conceptual and operational definitions of recovery.
The study by Fan and colleagues (2019) is a fine exemplar of modern epidemiological research on recovery that replicated and extended previous population-based studies on the topic (Dawson et al 2005). The study built on Dawson et al. (2005), who examined the past year prevalence of recovery from alcohol dependence in the United States using data from the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative general population survey. Individuals (n = 4422) who met Diagnostic and Statistical Manual for Mental Disorders (DSM), fourth edition (APA, 1994) criteria for alcohol dependence prior to the year preceding the survey were assessed for current alcohol dependence and “risk drinking” status. Risk drinking was defined using a combination of drinking quantity-frequency criteria considered indicative of higher risk drinking practices (any occasions of > 14 drinks weekly or > 5 drinks daily for men; > 7 drinks weekly or > 4 drinks daily for women in the past year). Fan and colleagues (2019) updated the Dawson et al. study (2005) by conducting similar analyses using the NESARC-III data (Grant et al., 2015) and DSM-5 (APA, 2013) diagnostic criteria for AUD. Individuals (n = 7785) who met AUD criteria prior to the past year were assessed for current (past year) AUD and risk drinking status. Most individuals had some level of problem reduction, and only 34.2% had persistent AUD. Across the two studies, the proportion of individuals who achieved non-abstinent recovery (17.7% in 2001–2002; 17.9% in 2012–2013) and abstinent recovery (18.2% in 2001–2002; 16.0% in 2012–2013) were remarkably similar.
The findings of Fan et al (2019) are consistent with prior work, including the high rates of recovery and, in particular, the high rates of non-abstinent recovery that occur outside of the context of treatment. In this commentary, we summarize what we view as the primary strengths of Fan et al. (2019). We also discuss study limitations relevant to refining definitions of recovery, with a particular focus on advancing research on recovery from AUD.
Measuring Recovery from Alcohol Use Disorder in the General Population
One of the most important contributions of Fan et al. (2019) is examining AUD and recovery patterns in a nationally representative general adult population sample. Building on Dawson et al (2005), Fan et al. (2019) investigated the behavioral epidemiology of recovery and relationships with treatment-seeking and AUD severity, which help contextualize and qualify the large clinical literature on treatment-assisted recoveries. The Fan et al (2019) results were consistent with many established features of AUD, including:
-
(1)
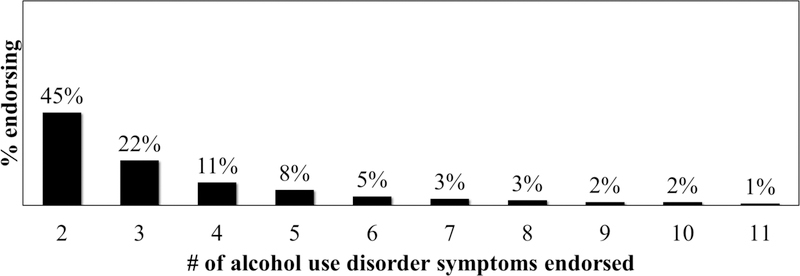
Alcohol consumption and AUD occur on severity continua, and the majority of individuals who engage in harmful alcohol use either do not meet criteria for AUD or meet criteria for a mild disorder based on having relatively lower levels of symptomology. As shown in Figure 1 based on data from the 2015 National Survey on Drug Use and Health (Substance Abuse and Mental Health Services Administration [SAMSHA]; 2016), about two-thirds of persons with AUD in the past year reported only 2–3 symptoms (i.e., “mild” AUD) based on the DSM-5 diagnostic system. Notably, 55.4% of respondents in the Fan et al (2019) sample were in asymptomatic drinker or abstainer outcome status groups based on the preceding year. This adds to evidence that alcohol use and AUD severity lie on continua and that the majority of individuals with history of AUD in nationally representative samples are in the asymptomatic or mild range of AUD.
-
(2)
Although recovery definitions vary across studies (Dawson et al., 2005; Tucker et al., 2006, 2009; Witkiewitz et al., 2019), most individuals who develop an AUD will ultimately resolve their alcohol-related problems. In the Fan et al. study, most participants with prior to past year AUD had some level of problem reduction during the past year, and only 34% had persistent AUD. It is unclear from the reporting by Fan et al. whether the 66% who did not have persistent AUD experienced greater recovery of functioning and well-being, broadly conceived, although they did have reduced clinical symptomology. Recent research with the NESARC wave 1 and wave 2 data has found that drinking reductions among individuals in NESARC, including those with AUD, are associated with significant improvements in broader health functioning (Hasin et al., 2017; Knox et al., 2019).
-
(3)
Associations among AUD severity, treatment seeking, and recovery status are complex and heterogeneous. Most individuals with AUD never receive treatment; those who do are a self-selected (or other-selected, in the case of mandated treatment) group of individuals who tend to be at the higher end of the AUD severity continuum; recoveries occur with and without treatment (Tucker and Simpson, 2011); persons with more severe AUD tend to be more successful with abstinence than moderation drinking (Tucker et al., 2009); and non-abstinent recoveries are relatively more common in natural recovery attempts, in part because persons seeking treatment tend to have more severe AUD and most treatment programs in the United States are abstinence-based. Fan et al. found that only 23% of their sample reported having ever received alcohol treatment, and treated participants tended to fall into persistent AUD (26.1%) or abstinent (43.3%) outcome groups that are typically associated with higher problem severity. Low risk drinking with or without symptoms was more common among never treated than treated respondents. Given the differences between those who do and do not receive treatment, it is critically important to study recovery among treatment seeking and non-treatment seeking population segments (Tucker and Simpson, 2011) and to expand the definition and assessment of recovery beyond a singular focus on drinking practices and achievement of stable abstinence.
Figure 1.
Past year alcohol use disorder symptoms among those meeting diagnostic criteria for an alcohol use disorder in the 2015 National Survey on Drug Use and Health General Population Survey (n=5124) (Substance Abuse and Mental Health Services Administration, 2016)
The Limited Utility of Using Alcohol Consumption Thresholds to Define Recovery
Both Fan and colleagues (2019) and Dawson and colleagues (2005) used a 4+/5+ drinks per day cutoff for defining “high-risk” drinking. This cutoff has numerous limitations when applied to examining recovery from AUD (see Pearson et al., 2016 for a review). First, alcohol consumption levels are not used as a criterion in accepted diagnostic schemes for AUD (APA, 2013), and it is therefore unclear why a drinking practices dimension would be included in definitions of recovery from AUD. Diagnostic schemes instead emphasize drinking in harmful ways and under conditions that increase risk for adverse consequences in alcohol-related functioning and development of tolerance and physical dependence. The 4+/5+ consumption cutpoints were originally developed to screen for AUD risk in general and medical populations, and incorporating them into definitions of recovery, particularly as superordinate evidence of recovery, is a newer development of unproven scientific and clinical utility.
Second, research using the NESARC-III data found that risk of AUD continues to increase well beyond the 4+/5+ cutpoints, with risk increasing through approximately 10 drinks for women and 11 drinks for men (Linden-Carmichael et al., 2019). Thus, the 4+/5+ drink threshold does not offer a useful dimension to characterize levels of AUD severity, as emphasized in DSM-5 diagnostic criteria, and, conversely, it is inadequate to characterize risk reduction during a recovery attempt.
Third, consumption-based thresholds have not been well-validated in clinical or general population samples. Research has found that consumption cutoffs lack sensitivity and specificity for predicting problems related to alcohol use and they do not differentiate individuals based on other measures of health or functioning (Pearson et al., 2016; Wilson et al., 2016). Cutpoints also ignore the influence of weight, sex, and health status in determining the effects of different levels of alcohol consumption (e.g., blood alcohol level) (Pearson et al., 2016) and are based on single-episode drinking, whereas recovery is better conceptualized as a process of change (SAMSHA, 2011).
Fourth, research on the risks of alcohol consumption is more complex than the common generalization that any drinking is harmful to health. Increased volume of alcohol consumption is monotonically associated with greater relative risk of morbidity for many health conditions (Rehm et al., 2017; Wood et al., 2018), however the association between alcohol consumption and alcohol-related consequences (including health consequences) tends to be modest (i.e., correlations less than .35; Pearson et al., 2017), lower consumption levels are associated with relative reductions in health risks for some prevalent disorders (e.g., ischaemic diseases, diabetes, myocardial infarction) (Rehm et al., 2017; Wood et al., 2018), and emerging evidence suggests that excessive infrequent drinking is associated with greater risk than stable levels of consumption (Grønbaek, 2009). Thus, the temporal patterning and manner of drinking over time merits consideration when evaluating the role of drinking practices in risk and recovery. To date, however, most relevant studies used summary measures of alcohol volume that precluded explication of how patterning and manner of drinking affect health risks or variables considered important in recovery.
Contextual Factors and Broadening Definitions of Recovery to Include Functioning
In line with the AA (1939) seminal definition, recent definitions of recovery, including a working definition from SAMHSA (2011), have focused on the importance of functioning, including a common concern with general well-being in defining recovery. The AUD symptoms of DSM-5 are certainly relevant for determining functioning related to alcohol use, but neither the DSM-5 nor consumption-based criteria provide specific information about general or physical well-being, social or occupational functioning, or quality of life. DSM-5 and consumption-based criteria also do not provide any utility in measuring the cognitions, attitudes, beliefs, and lifestyle factors that are critically important in predicting long term recovery (Kelly et al., 2019; Moos and Moos, 2007). The same is true of the Fan et al. (2019) study, which focused exclusively on DSM-5 diagnosis and levels of consumption with no consideration given to functioning, cognitions, attitudes, beliefs, or contextual, social, and environmental factors that may be more important when defining recovery (Moos and Moos, 2007).
An individual may be abstaining from alcohol and not meet DSM-5 criteria for AUD, but be a miserable “dry drunk” (Pattison, 1968) with little or no improvement in functioning or well-being. According to the Fan et al. (2019) definition of recovery, an abstinent individual who is struggling with abstinence, experiencing considerable distress, and who disengages with their social environment would be considered “recovered,” solely because he or she is abstaining and does not meet criteria for AUD. This is an overly limited view of recovery based solely on drinking practices and DSM-5 symptomology and fails to reflect recovery as broadly conceived by AA (1939), recent consensus definitions (e.g., Substance Abuse and Mental Health Services Adminitsration, 2011), and empirical findings (Witkiewitz et al., 2019).
Recovery as a Process of Behavior Change
A final limitation of the Fan et al. study (2019) is the reliance on cross-sectional data to characterize a dynamic process of behavior change. Despite their cross-sectional design that did not assess status changes over time, the authors speculated how individuals in NESARC-III may be expected to progress. Specifically, “high-risk drinkers may be in the path [of] developing more severe AUD or in the transitionary stage toward recovery.” Analyses of the NESARC wave 1 and wave 2 data (Dawson et al., 2007) provided a glimpse at what would likely happen if the NESARC-III sample was followed prospectively. First, consistent with a “sick quitter” effect (i.e., individuals who abstain because their health is too poor to continue drinking; Sarich et al., 2019), Dawson et al. (2007) found that, among abstainers at wave 1, there was a relatively greater loss to follow-up at wave 2 due to death, institutionalization, or incapacitation. They also reported remarkable stability of recovery status and found that it was far more likely for asymptomatic high-risk drinkers to remain asymptomatic (31.3%) or transition to low-risk (21.4%) or abstainer (7.4%) status than to develop AUD (6%) at wave 2. Therefore, we can predict that, over time, the high-risk drinkers in Fan et al. (2019) will be more likely to have positive outcomes than a worsening of AUD symptoms.
Summary and Future Directions
Fan and colleagues (2019) provided an important replication of prior work by Dawson et al. (2005) by showing that many individuals with AUD in a nationally representative sample achieve recovery, and that some achieve a non-abstinent recovery, often without treatment. Despite the study’s strengths and contributions, the results warrant qualification with respect to: (1) the conflation of alcohol consumption with AUD diagnosis in defining recovery; (2) the lack of assessment of contextual factors, general functioning, and well-being in determining recovery status; and (3) the use of a cross-sectional design and retrospective data to investigate a dynamic process of behavior change that unfolds over time.
Broadening the conceptualization of recovery to include both “low-risk” and even some “high-risk” asymptomatic drinking would have potentially increased the impact of Fan et al. (2019) by examining those individuals who are able to experience substantial recovery of functioning, regardless of the amount they are drinking. This work could also be extended by following nationally representative samples over time to gain a better understanding of the various pathways to recovery, including recovery in the context of treatment, recovery that occurs outside of the treatment context, and recovery among those who engage in occasional heavy drinking and still achieve a fulfilling life (Witkiewitz et al., 2019). Studying the temporal course and patterning of drinking, and associated functional consequences, over longer intervals is critical for characterizing and supporting the multiple heterogeneous pathways to recovery from an AUD. Definitions of recovery based on occasional episodes of heavy drinking are likely less important than definitions that consider changes over time in the patterns of drinking, functioning in other areas of life-health, and overall well-being and life satisfaction.
Acknowledgments
This research was supported by the National Institute on Alcohol Abuse and Alcoholism Grant R01 AA022328 (Witkiewitz, PI).
References
- American Psychiatric Association, 1994. Diagnostic and statistical manual of mental disorders (4th ed.; DSM-IV), 4th ed ed. Author, Washington, DC, DC. [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders, 5th ed American Psychiatric Association, Washington, DC, US. [Google Scholar]
- Anonymous, 1939. Alcoholics Anonymous: The Story of How Many Thousands of Men and Women Have Recovered from Alcoholism. Works, New York, NY, US. [Google Scholar]
- Dawson DA, Goldstein RB, Grant BF, 2007. Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: a 3-year follow-up Alcohol Clin Exp Res 31, 2036–45. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ, Dawson Deborah A.; Grant Bridget F.; Stinson Frederick S.; Chou Patricia S.; Huang Boji; Ruan WJ, 2005. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction 100, 281–92. [DOI] [PubMed] [Google Scholar]
- Fan AZ, Chou SP, Zhang H, Jung J, Grant BF, 2019. Prevalence and Correlates of Past Year Recovery from DSM-5 Alcohol Use Disorder: Results from National Epidemiologic Survey on Alcohol and Related Conditions-III Alcohol Clin Exp Res [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, Hasin DS, 2015. Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry 72, 757–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Wall M, Witkiewitz K, Kranzler HR, Falk D, Litten R, Mann K, O’Malley SS, Scodes J, Robinson RL, Anton R, Fertig J, Isenberg K, McCann D, Meulien D, Meyer R, O’Brien C, Ryan M, Silverman B, Trinquet F, Wong C, Zakine B, 2017. Change in non-abstinent WHO drinking risk levels and alcohol dependence: a 3 year follow-up study in the US general population. The Lancet Psychiatry 4, 469–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Greene MC, Bergman BG, White WL, Hoeppner BB, 2019. How Many Recovery Attempts Does it Take to Successfully Resolve an Alcohol or Drug Problem? Estimates and Correlates From a National Study of Recovering U.S. Adults. Alcohol Clin Exp Res 43, 1533–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knox J, Scodes J, Wall M, Witkiewitz K, Kranzler HR, Falk D, Litten R, Mann K, O’Malley SS, Anton R, Hasin DS, Alcohol Clinical Trials (ACTIVE) Workgroup, 2019. Reduction in non-abstinent WHO drinking risk levels and depression/anxiety disorders: 3-year follow-up results in the US general population. Drug Alcohol Depend 197, 228–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Russell MA, Lanza ST, 2019. Flexibly modeling alcohol use disorder risk: How many drinks should we count? Psychol Addict Behav 33, 50–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Moos BS, 2007. Protective resources and long-term recovery from alcohol use disorders. Drug Alcohol Depend 86, 46–54. [DOI] [PubMed] [Google Scholar]
- Pattison EM, 1968. A Critique of Abstinence Criteria in the Treatment of Alcoholism. Int J Soc Psychiatry 14, 268–276. [DOI] [PubMed] [Google Scholar]
- Pearson MR, Kirouac M, Witkiewitz K, 2016. Questionning the validity of the 4+/5+ binge or heavy drinking criterion in college and clinical populations. Addiction 111, 1720–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Gmel GE, Gmel G, Hasan OSM, Imtiaz S, Popova S, Probst C, Roerecke M, Room R, Samokhvalov AV, Shield KD, Shuper PA, 2017. The relationship between different dimensions of alcohol use and the burden of disease-an update. Addiction 112, 968–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarich P, Canfell K, Banks E, Paige E, Egger S, Joshy G, Korda R, Weber M, 2019. A Prospective Study of Health Conditions Related to Alcohol Consumption Cessation Among 97,852 Drinkers Aged 45 and Over in Australia. Alcohol Clin Exp Res 43, 710–721. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2016. 2015 National Survey on Drug Use and Health [WWW Document]. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Adminitsration, 2011. SAMHSA working definition of recovery: 10 guiding principles of recovery. Department of Health and Human Services, Rockville, MD. [Google Scholar]
- Tucker JA, Roth DL, Vignolo MJ, Westfall AO, 2009. A behavioral economic reward index predicts drinking resolutions: Moderation revisited and compared with other outcomes. J Consult Clin Psychol 77, 219–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JA, Simpson CA, 2011. The recovery spectrum: from self-change to seeking treatment. Alcohol Res Heal 33, 371–9. [PMC free article] [PubMed] [Google Scholar]
- Tucker JA, Vuchinich RE, Black BC, Rippens PD, 2006. Significance of a behavioral economic index of reward value in predicting drinking problem resolution. J Consult Clin Psychol 74, 317–326. [DOI] [PubMed] [Google Scholar]
- Wilson AD, Bravo AJ, Pearson MR, Witkiewitz K, 2016. Finding success in failure: using latent profile analysis to examine heterogeneity in psychosocial functioning among heavy drinkers following treatment. Addiction 111, 2145–2154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Wilson AD, Pearson MR, Montes KS, Kirouac M, Roos CR, Hallgren KA, Maisto SA, 2019. Profiles of recovery from alcohol use disorder at three years following treatment: Can the definition of recovery be extended to include high functioning heavy drinkers? Addiction 114, 69–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood AM, Kaptoge S, Butterworth AS, Willeit P, Warnakula S, Bolton T, Paige E, Paul DS, Sweeting M, Burgess S, Bell S, Astle W, Stevens D, Koulman A, Selmer RM, Verschuren WMM, Sato S, Njølstad I, Woodward M, Salomaa V, Nordestgaard BG, Yeap BB, Fletcher A, Melander O, Kuller LH, Balkau B, Marmot M, Koenig W, Casiglia E, Cooper C, Arndt V, Franco OH, Wennberg P, Gallacher J, de la Cámara AG, Völzke H, Dahm CC, Dale CE, Bergmann MM, Crespo CJ, van der Schouw YT, Kaaks R, Simons LA, Lagiou P, Schoufour JD, Boer JMA, Key TJ, Rodriguez B, Moreno-Iribas C, Davidson KW, Taylor JO, Sacerdote C, Wallace RB, Quiros JR, Tumino R, Blazer DG, Linneberg A, Daimon M, Panico S, Howard B, Skeie G, Strandberg T, Weiderpass E, Nietert PJ, Psaty BM, Kromhout D, Salamanca-Fernandez E, Kiechl S, Krumholz HM, Grioni S, Palli D, Huerta JM, Price J, Sundström J, Arriola L, Arima H, Travis RC, Panagiotakos DB, Karakatsani A, Trichopoulou A, Kühn T, Grobbee DE, Barrett-Connor E, van Schoor N, Boeing H, Overvad K, Kauhanen J, Wareham N, Langenberg C, Forouhi N, Wennberg M, Després J-P, Cushman M, Cooper JA, Rodriguez CJ, Sakurai M, Shaw JE, Knuiman M, Voortman T, Meisinger C, Tjønneland A, Brenner H, Palmieri L, Dallongeville J, Brunner EJ, Assmann G, Trevisan M, Gillum RF, Ford I, Sattar N, Lazo M, Thompson SG, Ferrari P, Leon DA, Smith GD, Peto R, Jackson R, Banks E, Di Angelantonio E, Danesh J, Wood AM, Kaptoge S, Butterworth A, Willeit P, Warnakula S, Bolton T, Paige E, Paul DS, Sweeting M, Burgess S, Bell S, Astle W, Stevens D, Koulman A, Selmer RM, Verschuren M, Sato S, Njølstad I, Woodward M, Veikko S, Nordestgaard BG, Yeap BB, Flecther A, Melander O, Kuller LH, Balkau B, Marmot M, Koenig W, Casiglia E, Cooper C, Arndt V, Franco OH, Wennberg P, Gallacher J, Gómez de la Cámara A, Völzke H, Dahm CC, Dale CE, Bergmann M, Crespo C, van der Schouw YT, Kaaks R, Simons LA, Lagiou P, Schoufour JD, Boer JM, Key TJ, Rodriguez B, Moreno-Iribas C, Davidson KW, Taylor JO, Sacerdote C, Wallace RB, Quiros JR, Rimm EB, Tumino R, Blazer DG III, Linneberg A, Daimon M, Panico S, Howard B, Skeie G, Salomaa V, Strandberg T, Weiderpass E, Nietert PJ, Psaty BM, Kromhout D, Salamanca-Fernandez E, Kiechl S, Krumholz HM, Grioni S, Palli D, Huerta JM, Price J, Sundström J, Arriola L, Arima H, Travis RC, Panagiotakos DB, Karakatsani A, Trichopoulou A, Kühn T, Grobbee DE, Barrett-Connor E, van Schoor N, Boeing H, Overvad K, Kauhanen J, Wareham N, Langenberg C, Forouhi N, Wennberg M, Després J-P, Cushman M, Cooper JA, Rodriguez CJ, Sakurai M, Shaw JE, Knuiman M, Voortman T, Meisinger C, Tjønneland A, Brenner H, Palmieri L, Dallongeville J-P, Brunner EJ, Assmann G, Trevisan M, Gillumn RF, Ford IF, Sattar N, Lazo M, Thompson S, Ferrari P, Leon DA, Davey Smith G, Peto R, Jackson R, Banks E, Di Angelantonio E, Danesh J, 2018. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 391, 1513–1523. [DOI] [PMC free article] [PubMed] [Google Scholar]