Abstract
Objective
To examine the effect of the 2010 Affordable Care Act (ACA) extended dependent coverage and no cost‐sharing provisions on human papillomavirus (HPV) vaccination in relation to sexual orientation identity among U.S. women.
Data Sources
2006‐2010 and 2011‐2015 National Survey of Family Growth.
Study Design
We used an interrupted time series design and multivariable Poisson regression to assess differences in HPV vaccination initiation before (2007‐2010) and after (2011‐2015) the 2010 ACA provisions among heterosexual, bisexual, and lesbian U.S. women aged 15‐25 years (N = 7033), adjusting for temporal trends and demographic factors.
Data Collection
Computer‐assisted personal interview and audio computer‐assisted self‐interview questionnaires.
Principal Findings
The adjusted prevalence of HPV vaccination initiation was significantly higher among lesbian and bisexual women after compared to before the 2010 ACA—at 19.1 (95% confidence interval [CI]: 5.4, 32.9) and 15.7 (95% CI: 4.4, 27.1) percentage points in 2015 compared to 2007‐2010, respectively. We observed no association between the 2010 ACA provisions and HPV vaccination initiation among heterosexual women after adjusting for temporal trends and demographic factors.
Conclusions
The 2010 ACA provisions may have improved HPV vaccination initiation among lesbian and bisexual women. Policies and programs that increase access to health insurance and provide HPV vaccines at no cost to patients may facilitate HPV vaccine uptake in these marginalized populations.
Keywords: Affordable Care Act, health inequities, human papillomavirus vaccination, sexual orientation, women
1. INTRODUCTION
Human papillomavirus (HPV) is the most common sexually transmitted infection (STI) in the United States.1 Each year, approximately 7 million U.S. women are newly infected with HPV,2 and about 17 000 develop a new cervical or other HPV‐related cancer.3 Sexual minority women (SMW; eg, lesbians, bisexual women) are at risk of acquiring HPV from various sexual behaviors with sexual partners of any sex or gender.4 Using 2003‐2012 National Health and Nutrition Examination Survey data, researchers found that bisexual women were at particularly elevated risk of HPV infection, with a prevalence of 57.7 percent relative to 41.1 percent among heterosexual women and 35.5 percent among lesbians.5 Additionally, while no data on the incidence of cervical and other HPV‐related cancers in relation to sexual orientation currently exist,6 research suggests that the prevalence of cervical cancer may be higher among bisexual women relative to their heterosexual and lesbian counterparts.7 Moreover, studies indicate that lesbians who acquire HPV may be at higher risk of developing cervical cancer relative to heterosexual women because of a lower prevalence of regular Pap testing,8 higher prevalence of smoking,9 and lower prevalence of health insurance and access to health care.10 Between 2006 and 2019, HPV vaccination, which effectively prevents cervical cancer,11 was recommended for girls aged 11 and 12 years and unvaccinated young women aged 13‐26 years regardless of sexual orientation.12 However, research suggests that lesbians may have significantly lower odds of initiating and completing the 3‐dose HPV vaccine series relative to their heterosexual counterparts.13, 14
The Affordable Care Act (ACA) is a federal health policy that was enacted in 2010 and provides coverage to young adults up to 26 years of age under their parents' health insurance plan as well as coverage of preventive health services, including HPV vaccines, by private health plans with no cost sharing from patients.15, 16 Studies indicate that the 2010 implementation of the ACA was associated with a statistically significant increase in HPV vaccination initiation and completion among young U.S. women.17 However, no study of which we are aware has examined the effect of the ACA on HPV vaccination disparities, including in relation to sexual orientation, which is critical to promoting not only population health but also health equity. Indeed, given that SMW are more likely to be poor and medically underserved than heterosexual women,10, 18 it is possible that the ACA disproportionately increased access to high‐cost HPV vaccines in this population and helped mitigate sexual orientation disparities in HPV vaccination among young U.S. women.19
Thus, using an interrupted time series study design,20 we examined the effect of the 2010 ACA extended dependent coverage and no cost‐sharing provisions on HPV vaccination initiation among heterosexual, bisexual, and lesbian U.S. women using a large national probability sample. Our analyses provide new information on the association between the ACA and HPV vaccine uptake across sexual orientation identity groups, thus contributing to the small but growing evidence base examining the effect of this federal health policy on health disparities. Additionally, the present study may help inform the development of policies, programs, and practices that facilitate HPV vaccination and help prevent cervical and other HPV‐related cancers among SMW, a marginalized and underserved population.
2. METHODS
2.1. Study participants
We analyzed data from the 2006‐2010, 2011‐2013, and 2013‐2015 waves of the National Survey of Family Growth (NSFG), which provides a national probability sample of the U.S. civilian, noninstitutionalized population aged 15‐44 years.21, 22, 23 Response rates were 77 percent in 2006‐2010, 73 percent in 2011‐2013, and 69 percent in 2013‐2015.21, 22, 23 Our analysis was restricted to women surveyed in July 2007 or later and aged 15‐24 years at screening, as women surveyed before July 2007 and those aged 25 years and above at screening were not asked about HPV vaccination. Additionally, we excluded women missing data on HPV vaccination initiation (n = 120; 1.7 percent) and those who did not answer or responded “don't know” or “something else” to the sexual orientation identity question (n = 83; 1.2 percent). Thus, our analytic sample consisted of 7033 heterosexual, bisexual, and lesbian U.S. women aged 15‐24 years (at screening), including 3205 women in 2007‐2010 and 3828 women in 2011‐2015.
2.2. Measures
The dichotomous outcome of interest was HPV vaccination initiation (≥1 dose). In 2007‐2010, participants were asked: “Before today, have you ever heard of the cervical cancer vaccine, HPV shot, or Gardasil?” Women aged 15‐24 years (at screening) who responded “yes” were asked: “Have you received the cervical cancer vaccine, also known as the HPV shot or Gardasil?” In 2011‐2015, all women aged 15‐24 years (at screening) were asked whether they had ever received the HPV vaccine. Response options included “yes,” “no,” and “don't know.” Participants who reported never having heard of the HPV vaccine in 2007‐2010 (n = 555; 17.1 percent) were coded as not having initiated vaccination. A response of “don't know” in 2007‐2015 (n = 120; 1.7 percent—including n = 6, 0.2 percent in 2007‐2010, and n = 114, 2.9 percent in 2011‐2015) was coded as missing. The primary predictor was the implementation of two ACA provisions—namely, extended dependent coverage and preventive services coverage by private health plans with no patient cost sharing. Both ACA provisions went into effect in September 2010, which coincided with the June 2010‐September 2011 gap between NSFG waves. Thus, we created a dichotomous variable where the 2011‐2015 NSFG wave was coded as 1 (post‐2010 ACA provisions) and the 2006‐2010 NSFG wave was coded as 0 (pre‐2010 ACA provisions).
We conceptualized sexual orientation identity as a potential effect modifier of the relationship between the 2010 ACA provisions and HPV vaccination initiation among U.S. women. We selected sexual orientation identity as our measure of sexual orientation because of its relevance to individuals' health care access and experiences24 and to facilitate comparisons with other research on the effect of the ACA on lesbian, gay, bisexual, and transgender (LGBT) health.25 Sexual orientation identity was assessed using the question “Do you think of yourself as…,” to which participants could respond “heterosexual or straight” (henceforth, heterosexual), “homosexual, gay, or lesbian” (henceforth, lesbian), or “bisexual.” Participants who did not answer the question or responded “don't know” or “something else” were coded as missing (n = 83, 1.2 percent).
Covariates were selected a priori based on the scientific literature and included demographic factors (ie, age, race/ethnicity, nativity, place of residence, and relationship status), which we conceptualized as potential confounders (see Appendix Table 1 for their categorization). Age was dichotomized as 15‐18 years and 19‐25 (inclusive) years given that the ACA's extended dependent coverage pertained to young adults aged 19‐26 years (ie, until their 26th birthday). For each of these demographic covariates, the proportion of missing data in the original responses was small (≤1 percent). These variables were imputed by NSFG staff using regression‐based imputation, resulting in no missing covariate data in the present analysis.26
Table 1.
Percentage distribution of demographic, socioeconomic, and health care factors before (2007‐2010) and after (2011‐2015) the 2010 Affordable Care Act provisions overall and in relation to sexual orientation identity among U.S. women aged 15‐25 y (N = 7033)
| Variable (%) | Pre‐2010 ACA provisions (2007‐2010) | Post‐2010 ACA provisions (2011‐2015) | ||||||
|---|---|---|---|---|---|---|---|---|
| Total | Heterosexual | Bisexual | Lesbian | Total | Heterosexual | Bisexual | Lesbian | |
| N = 3205 | n = 2911 (91.5%) | n = 232 (6.6%) | n = 62 (1.9%) | N = 3828 | n = 3359 (87.7%) | n = 382 (10.0%) | n = 87 (2.3%) | |
| Age (y) | ||||||||
| 15‐18 | 37.9 | 38.3 | 36.6 | 24.3 | 36.6 | 36.3 | 40.5 | 34.0 |
| 19‐25 | 62.1 | 61.7 | 63.4 | 75.7 | 63.4 | 63.7 | 59.5 | 66.0 |
| Race/ethnicity | ||||||||
| White | 58.7 | 58.0 | 66.2 | 61.7 | 53.6 | 54.3 | 50.4 | 36.9 |
| Black | 14.8 | 14.9 | 10.6 | 20.1 | 14.7 | 14.6 | 13.2 | 29.0 |
| Latina | 17.2 | 17.7 | 11.6 | 14.4 | 21.4 | 21.2 | 21.7 | 29.9 |
| Another race/ethnicity or multiracial | 9.4 | 9.3 | 11.6 | 3.7 | 10.3 | 10.0 | 14.7 | 4.1 |
| U.S.‐born: yes | 90.4 | 90.4 | 92.2 | 82.9 | 91.4 | 91.0 | 95.2 | 94.0 |
| MSA status | ||||||||
| MSA, central city | 35.5 | 35.1 | 41.6 | 36.3 | 36.1 | 35.7 | 40.5 | 35.2 |
| MSA, other | 46.7 | 46.9 | 39.9 | 60.6 | 48.7 | 49.2 | 43.6 | 48.3 |
| Non‐MSA | 17.7 | 18.0 | 18.5 | 3.1 | 15.2 | 15.1 | 15.8 | 16.5 |
| Relationship statusa | ||||||||
| Never married | 78.4 | 78.4 | 74.7 | 89.8 | 77.0 | 76.7 | 75.2 | 100.0 |
| Currently married | 8.0 | 8.2 | 8.6 | 0.7 | 7.6 | 8.2 | 3.7 | 0.0 |
| Living with a partner | 11.9 | 11.8 | 15.9 | 4.5 | 14.3 | 14.2 | 18.1 | 0.0 |
| Separated, divorced or widowed | 1.7 | 1.7 | 0.8 | 5.0 | 1.0 | 0.9 | 3.0 | 0.0 |
| Educational attainment | ||||||||
| < HS diploma | 41.8 | 41.9 | 44.1 | 27.9 | 34.8 | 34.3 | 41.5 | 27.8 |
| HS diploma or GED | 22.9 | 22.6 | 22.7 | 36.4 | 25.4 | 24.6 | 31.9 | 33.9 |
| Some college or Associates degree | 27.0 | 26.8 | 30.9 | 25.5 | 31.1 | 31.7 | 23.5 | 37.6 |
| Bachelor's degree or higher | 8.3 | 8.7 | 2.3 | 10.2 | 8.7 | 9.4 | 3.2 | 0.7 |
| Household federal poverty level (%) | ||||||||
| <100 | 29.2 | 28.9 | 36.2 | 21.3 | 35.4 | 35.1 | 38.5 | 38.3 |
| 100‐199 | 25.3 | 25.3 | 26.5 | 18.9 | 22.9 | 22.1 | 30.9 | 24.5 |
| 200‐299 | 17.8 | 17.6 | 18.7 | 24.5 | 15.9 | 16.2 | 11.4 | 20.6 |
| ≥300 | 27.7 | 28.2 | 18.6 | 35.3 | 25.8 | 26.6 | 19.2 | 16.6 |
| Employment status | ||||||||
| Working | 51.8 | 52.0 | 42.4 | 71.0 | 53.8 | 54.9 | 45.5 | 40.2 |
| Not working | 25.5 | 24.8 | 38.6 | 16.3 | 20.4 | 19.7 | 25.8 | 30.9 |
| Student | 22.7 | 23.2 | 18.9 | 12.7 | 25.8 | 25.5 | 28.7 | 28.9 |
| Health insurance status | ||||||||
| Private insurance | 55.8 | 57.2 | 36.7 | 54.2 | 55.0 | 56.1 | 43.7 | 55.7 |
| Public insurance | 24.5 | 23.7 | 37.0 | 19.6 | 29.7 | 29.2 | 36.1 | 20.3 |
| Uninsured or underinsuredb | 19.7 | 19.0 | 26.3 | 26.2 | 15.3 | 14.6 | 20.2 | 24.0 |
Percentages (%) account for the complex survey design and may not add to 100% due to rounding error.
Abbreviation: MSA, Metropolitan Statistical Area.
Pertains to male partners only.
Covered by a single‐service plan or the Indian Health Service only.
2.3. Statistical analysis
Using sample weights to produce nationally representative estimates based on the NSFG's sampling strategy, we estimated the distribution of demographic, socioeconomic, and health care factors among U.S. women aged 15‐25 years, overall and in relation to sexual orientation identity, before (2007‐2010) and after (2011‐2015) the implementation of the 2010 ACA provisions. We then estimated the prevalence of HPV vaccination initiation, overall in relation to sexual orientation identity, in 2007‐2010 and 2011‐2015 and assessed differences between each time period (reference: 2007‐2010) within each sexual orientation identity group using the adjusted Wald test.
We assessed the effect of the 2010 ACA extended dependent coverage and no cost‐sharing provisions on the probability of HPV vaccination initiation among heterosexual, bisexual, and lesbian women using Poisson regression modeling (with a robust variance estimator), which allowed us to directly estimate risk ratios (RR).27 Post‐ vs pre‐2010 ACA differences in HPV vaccination initiation were estimated for each sexual orientation identity group using an interaction term between the 2010 ACA provisions and sexual orientation identity. This interaction model was adjusted for the main effect of sexual orientation identity as well as temporal trends. Time was modeled continuously in years because estimating interaction terms between time modeled using indicator variables and sexual orientation identity left no remaining variation from which to estimate the interaction between the 2010 ACA provisions and sexual orientation identity (ie, there was perfect collinearity). The slopes of the temporal trends were allowed to vary across sexual orientation identity groups by including interaction terms between year and sexual orientation identity. Further, our model was also adjusted for demographic factors, including age, race/ethnicity, nativity, Metropolitan Statistical Area (MSA) status, and relationship status (see Appendix Table S1).28 As a sensitivity analysis, we also estimated a linear regression model including the same variables as the Poisson regression model.
We used the Poisson regression model to estimate RR in order to ascertain differences in the adjusted prevalence of HPV vaccination initiation associated with the 2010 ACA provisions within each sexual orientation identity group relative to each group's level of HPV vaccination initiation in 2007‐2010. For heterosexual women, the RR was obtained by exponentiating the coefficient for the 2010 ACA provisions main effect. For bisexual and lesbian women, RR were obtained by exponentiating the sum of the 2010 ACA main effect coefficient and the coefficient for the interaction term between the 2010 ACA provisions and corresponding sexual orientation identity group. For each post‐2010 ACA survey year (ie, 2011‐2015), we also used the Poisson regression model to calculate risk differences (RD) in order to assess the percentage point difference in HPV vaccination initiation prevalence associated with the 2010 ACA provisions for each sexual orientation identity group. Because RD from Poisson regression models depend on the level of the other covariates included in the model, we estimated weighted average marginal effects (ie, we calculated RD for each observation and took a weighted average using sampling weights).29, 30 Standard errors for RD were calculated using the delta method.29 Lastly, we also used the Poisson regression model to estimate predicted HPV vaccination initiation probabilities for each sexual orientation identity group in each year from 2007 to 2015. All analyses were conducted in R version 3.4.1 and accounted for the complex survey design.31, 32
3. RESULTS
Table 1 shows that in 2011‐2015 (post‐2010 ACA provisions), U.S. women aged 15‐25 years were more likely to identify as Latina and bisexual, have obtained a high school diploma or GED, live in a household with an income below 100 percent of the federal poverty level (FPL), be employed, and have public insurance and less likely to be uninsured or underinsured compared to their counterparts in 2007‐2010 (pre‐2010 ACA provisions). In 2007‐2010, lesbians were more likely to be older than 18 years, have a high school diploma or GED, live above 300 percent of the FPL, be employed, and be uninsured or underinsured and less likely to be U.S.‐born, live in a non‐MSA, and be married to a male partner compared to heterosexual women. Further, relative to heterosexual women, bisexual women were less likely to be employed and have a bachelor's degree or higher and more likely to be living in a MSA, central city, with a male partner, and under 100 percent FPL and to be uninsured or underinsured. The distribution of covariates across sexual orientation identity groups was similar in 2011‐2015. However, in 2011‐2015, lesbians were just as likely as heterosexual women to live in a non‐MSA and less likely to live above 300 percent FPL and be employed relative to their heterosexual counterparts (Table 1).
Table 2 shows that the unadjusted prevalence of HPV vaccination initiation was significantly higher in 2011‐2015 compared to 2007‐2010 among U.S. women aged 15‐25 years in general (45.7 vs 24.1 percent, P < .0001) and among heterosexual (46.4 vs 24.1 percent, P < .0001), bisexual (46.6 vs 30.6 percent, P = .0089), and lesbian (27.1 vs 4.6 percent, P = .0012) women in particular. Further, lesbians were significantly less likely to have initiated HPV vaccination compared to their heterosexual counterparts in both 2007‐2010 (4.6 vs 24.1 percent, P = .0004) and 2011‐2015 (27.1 vs 46.4 percent, P = .011). In contrast, bisexual women had a similar unadjusted prevalence of HPV vaccination initiation as heterosexual women before (30.6 vs 24.1 percent, P = .18) and after (46.6 vs 46.4 percent, P = .95) the 2010 ACA provisions (Table 2).
Table 2.
Distribution of human papillomavirus vaccination initiation before (2007‐2010) and after (2011‐2015) the 2010 Affordable Care Act provisions overall and in relation to sexual orientation identity among U.S. women aged 15‐25 y (N = 7033)
| Variable | Pre‐2010 ACA provisions (2007‐2010) | Post‐2010 ACA provisions (2011‐2015) | ||||
|---|---|---|---|---|---|---|
| n | % | 95% CI | n | % | 95% CI | |
| Total | 3205 | 24.1 | 21.2, 27.2 | 3828 | 45.7* | 43.2, 48.3 |
| Sexual orientation identity | ||||||
| Heterosexual (reference) | 2911 | 24.1 | 21.2, 27.4 | 3359 | 46.4* | 43.7, 49.1 |
| Bisexual | 232 | 30.6 | 21.9, 40.9 | 382 | 46.6* | 40.3, 52.9 |
| Lesbian | 62 | 4.6 | 1.4, 14.1** | 87 | 27.1*, ** | 15.9, 42.2 |
Prevalence estimates (%) and 95% confidence intervals (CIs) account for the complex survey design. P‐values are based on the adjusted Wald test.
Abbreviation: ACA, Affordable Care Act.
Statistically significant (P < .05) difference between 2011‐2015 and 2007‐2010 (reference).
Statistically significant (P < .05) difference between sexual orientation identity groups (reference: heterosexual).
Table 3 presents RR and RD for HPV vaccination initiation after (2011‐2015) compared to before (2007‐2010) the 2010 ACA provisions among heterosexual, bisexual, and lesbian U.S. women aged 15‐25 years. After adjusting for sexual orientation identity group‐specific HPV vaccination initiation temporal trends and demographic factors, the RR for the probability of HPV vaccination initiation after compared to before the 2010 ACA provisions were 4.4 (95% confidence interval [CI]: 0.7, 29.8) among lesbian women and 1.7 (95% CI: 0.9, 3.2) among bisexual women. While the magnitude of these RR suggested a positive association between the 2010 ACA provisions and HPV vaccination initiation among both lesbian and bisexual women, they were not statistically significant at the 0.05 level. Further, the RR for the probability of HPV vaccination initiation after compared to before the 2010 ACA provisions was 1.0 (95% CI: 0.8, 1.3) among heterosexual women after adjusting for temporal trends and demographic factors.
Table 3.
Adjusted risk ratios and risk differences for the association between the 2010 Affordable Care Act provisions and human papillomavirus (HPV) vaccination initiation among heterosexual, bisexual, and lesbian U.S. women aged 15‐25 y (N = 7033)
| n | RR (95% CI) | RD (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | |||
| Heterosexual | 6270 | 1.0 (0.8, 1.3) | 0.4 (−6.7, 7.6) | 0.5 (−7.7, 8.6) | 0.5 (−8.7, 9.8) | 0.6 (−10.0, 11.2) | 0.7 (−11.4, 12.8) |
| Bisexual | 614 | 1.7 (0.9, 3.2) | 17.4 (−1.6, 36.3) | 16.9 (0.1, 33.7) | 16.5 (1.7, 31.3) | 16.1 (3.1, 29.1) | 15.7 (4.4, 27.1) |
| Lesbian | 149 | 4.4 (0.7, 29.8) | 15.3 (−7.8, 38.4) | 16.2 (−4.0, 36.4) | 17.1 (−0.2, 34.5) | 18.1 (3.2, 33.0) | 19.1 (5.4, 32.9) |
Risk ratios (RR) and risk differences (RD) and 95% confidence intervals (CIs) were generated from a Poisson regression model, account for the complex survey design, and are adjusted for the HPV vaccination initiation temporal trend in each sexual orientation identity group and demographic factors (ie, age, race/ethnicity, nativity, MSA status, and relationship status). RD are expressed as percentage point differences in HPV vaccination initiation in a given year after (2011‐2015) compared to before (2007‐2010) the 2010 ACA provisions. Bolded values represent parameter estimates with 95% CIs that exclude 1 (for RR) and 0 (for RD).
Moreover, among bisexual women, we observed statistically significant percentage point differences in the adjusted prevalence of HPV vaccination initiation after compared to before the 2010 ACA provisions—ranging from 16.9 (95% CI: 0.1, 33.7) percentage points in 2012 to 15.7 (95% CI: 4.4, 27.1) percentage points in 2015. Among lesbians, we found statistically significant percentage point differences in HPV vaccination initiation after compared to before the 2010 ACA provisions in 2014 (RD = 18.1; 95% CI: 3.2, 33.0) and 2015 (RD = 19.1; 95% CI: 5.4, 32.9). Among heterosexual women, we noted no statistically significant percentage point difference in HPV vaccination initiation after compared to before the 2010 ACA provisions in any year between 2011 and 2015 after adjusting for the increasing HPV vaccination initiation temporal trend in this group and demographic factors (Table 3). Further, Figure 1 shows that adjusting for temporal trends and demographic factors, the predicted probability of HPV vaccination initiation was higher among lesbian and bisexual women after compared to before the 2010 ACA. Of note, some of the statistically significant results from the Poisson regression model were not statistically significant in the linear regression model, although point estimates were similar in both models (Appendix Table S2).28
Figure 1.
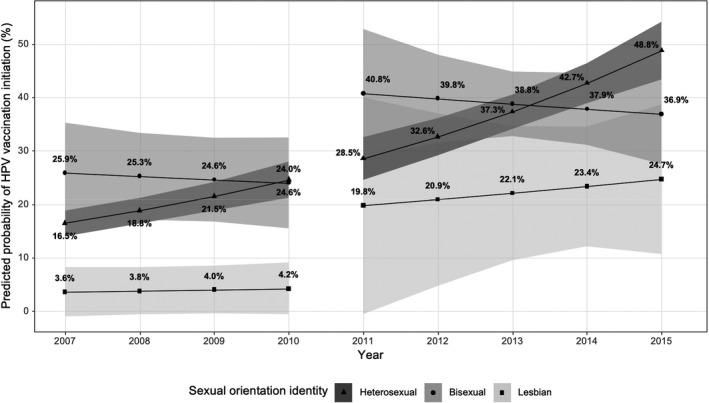
Adjusted predicted probability of human papillomavirus (HPV) vaccination initiation before (2007‐2010) and after (2011‐2015) the 2010 Affordable Care Act provisions among heterosexual, bisexual, and lesbian U.S. women aged 15‐25 y (N = 7033).
Note. Predicted probabilities account for the complex survey design and are based on a multivariable Poisson regression model adjusted for sexual orientation identity group–specific temporal trends in HPV vaccination initiation and demographic factors (ie, age, race/ethnicity, nativity, MSA status, and relationship status)
4. DISCUSSION
To our knowledge, the present study is the first to examine the effect of the 2010 ACA provisions—namely extended dependent coverage and preventive services coverage by private health plans with no cost sharing from patients—on HPV vaccination disparities, including in relation to sexual orientation, among U.S. women. Similarly to the few other studies that assessed the impact of the ACA on HPV vaccine uptake among women overall,17, 33 we found that the unadjusted prevalence of HPV vaccination initiation was significantly higher after compared to before the implementation of the 2010 ACA provisions among young U.S. women in general. Additionally, our study contributes to the existing literature by showing that the unadjusted prevalence of HPV vaccination initiation was higher not only among U.S. women overall but also in each sexual orientation identity group (ie, heterosexual, bisexual, and lesbian). Moreover, among lesbian and bisexual women, we observed a higher probability of HPV vaccination initiation after (2011‐2015) compared to before (2007‐2010) the 2010 ACA provisions on both the RR and RD scales after adjusting for group‐specific HPV vaccination initiation temporal trends and demographic factors. However, only the RDs were statistically significant at the 0.05 level. Of note, the large but nonstatistically significant RR among lesbians may be due to the small number of lesbians in our sample. In contrast, among heterosexual women, we no longer observed any difference in the probability of HPV vaccination initiation after compared to before the 2010 ACA provisions after adjusting for increasing temporal trends in this group and demographic factors.
It is possible that the 2010 ACA extended dependent coverage and no cost‐sharing provisions were associated with a considerably higher adjusted probability of HPV vaccination initiation among lesbians on the RR scale (albeit not statistically significant, possibly because of the small number of lesbians in our sample) because of the particularly low prevalence of HPV vaccination initiation in this marginalized and underserved population prior to the ACA.34 Additionally, other research suggests that the 2010 ACA provisions may have had a statistically significant positive effect on the adjusted prevalence of HPV vaccination initiation among lesbian and bisexual women on the RD scale because they directly addressed barriers to HPV vaccines (ie, health insurance, cost) that are especially pronounced in these disproportionately poor,18 uninsured,10 and medically underserved10 populations.19, 35
Our findings should be interpreted in light of some limitations. First, all data were self‐reported, and HPV vaccination initiation was not confirmed using medical records. However, while reporting error may affect the accuracy of prevalence estimates, we do not believe that it influenced our estimation of the magnitude of the ACA effect among sexual orientation identity groups as there is no evidence that reporting of HPV vaccine uptake differs before and after the ACA. Additionally, all data were cross‐sectional; thus, we cannot establish temporality between sexual orientation identity, HPV vaccination initiation, and potential confounders. It is also possible that unmeasured changes in the composition of each sexual orientation identity group between the pre‐ and post‐2010 ACA periods accounted for the differences we identified. Moreover, due to the small number of lesbians in our sample, many meaningful effect estimates did not reach statistical significance at the 0.05 level. Further, because of the small sample size for lesbians, we were unable to stratify our data by age (ie, 15‐18 years, only affected by preventive services coverage provision, vs 19‐25 years, affected by both extended dependent coverage and preventive services coverage provisions) to disentangle the effects of the extended dependent coverage and preventive services coverage provisions on HPV vaccination initiation. Moreover, we were not able to include an interaction term between sexual orientation identity, ACA implementation, and private health insurance due to the small number of lesbians in our study, which may have hindered our ability to fully capture the effect of the 2010 ACA provisions, which applied only to private health plans.
The present study has important implications for future research. First, additional studies are needed to examine the effect of the 2010 ACA provisions on not only the initiation but also the completion of the HPV vaccine series in relation to both identity‐ and behavior‐based measures of sexual orientation (with larger samples of lesbians) as well as race/ethnicity, socioeconomic position (SEP), nativity, and geography among both U.S. women and men. Second, while past studies have focused on the 2010 ACA provisions, research that investigates how other ACA provisions (eg, state Medicaid expansions) influence HPV vaccine uptake among young U.S. women and men in general and in relation to sexual orientation and other dimensions of social inequality is needed to capture the full effect of the ACA on HPV vaccination in the U.S. population. Lastly, future research should investigate the effect of various ACA provisions on access to and utilization of other preventive health services among U.S. women and men in relation to sexual orientation. Indeed, while studies have assessed whether the ACA improved the use of various preventive health services within and between racial/ethnic and socioeconomic groups,36, 37 no study of which we are aware examined its impact on health and health care in relation to sexual orientation, a key social determinant of health.24
The present study also has important implications for public health practice. Indeed, our findings suggest that national, state, local, and institutional policies and programs that facilitate access to health insurance and provide HPV vaccines at no cost to patients may improve HPV vaccine uptake among adolescent and young adult lesbian and bisexual women and help decrease sexual orientation disparities in HPV vaccination among young U.S. women. It is possible that these policies and programs will also facilitate HPV vaccination among other groups of disproportionately poor, uninsured, and underserved young people and help mitigate HPV vaccination disparities related to other dimensions of social inequality, including race/ethnicity, SEP, nativity, and geography. Ensuring that adolescent and young adult SMW and other marginalized and underserved groups of young people have access to HPV vaccines is essential for not only meeting overall Healthy People 2020 objectives38 but also achieving equity in HPV vaccination and, ultimately, HPV‐related diseases in the United States.
Supporting information
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: We thank the National Center for Health Statistics and 2006‐2010 and 2011‐2015 National Survey of Family Growth participants for the data used in this study. The preparation of this manuscript was supported by American Cancer Society grant 128863‐PF‐15‐149‐01‐CPHPS, awarded to M Agénor.
Agénor M, Murchison GR, Chen JT, et al. Impact of the Affordable Care Act on human papillomavirus vaccination initiation among lesbian, bisexual, and heterosexual U.S. women. Health Serv Res. 2020;55:18–25. 10.1111/1475-6773.13231
REFERENCES
- 1. Dunne EF, Markowitz LE, Saraiya M, et al. CDC Grand Rounds: reducing the burden of HPV‐associated cancer and disease. MMWR Morb Mortal Wkly Rep. 2014;63(4):69‐72. [PMC free article] [PubMed] [Google Scholar]
- 2. Satterwhite LC, Torrone FE, Meites BE, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013;40(3):187‐193. [DOI] [PubMed] [Google Scholar]
- 3. Jemal A, Simard E, Dorell C, et al. Annual report to the nation on the status of cancer, 1975–2009, featuring the burden and trends in human papillomavirus (HPV)‐associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst. 2013;105(3):175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gorgos LM, Marrazzo JM. Sexually transmitted infections among women who have sex with women. Clin Infect Dis. 2011;53(suppl 3):S84. [DOI] [PubMed] [Google Scholar]
- 5. Reiter P, McRee AL. HPV infection among sexual minority women: does it matter how sexual orientation is measured? Cancer Epidemiol Biomarkers Prev. 2016;25(3):559‐560. [Google Scholar]
- 6. Bowen DJ, Boehmer U. The lack of cancer surveillance data on sexual minorities and strategies for change. Cancer Causes Control. 2007;18(4):343‐349. [DOI] [PubMed] [Google Scholar]
- 7. Boehmer U, Miao X, Ozonoff A. Cancer survivorship and sexual orientation. Cancer. 2011;117(16):3796‐3804. [DOI] [PubMed] [Google Scholar]
- 8. Agénor M, Krieger N, Austin S, Haneuse S, Gottlieb B. Sexual orientation disparities in Papanicolaou test use among US women: the role of sexual and reproductive health services. Am J Public Health. 2014;104(2):E68‐E73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cochran SD, Bandiera FC, Mays VM. Sexual orientation‐related differences in tobacco use and secondhand smoke exposure among US adults aged 20 to 59 years: 2003–2010 National Health and Nutrition Examination Surveys. Am J Public Health. 2013;103(10):1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cochran SD, Mays VM, Bowen D, et al. Cancer‐related risk indicators and preventive screening behaviors among lesbians and bisexual women. Am J Public Health. 2001;91(4):591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Saslow D, Castle PE, Cox JT, et al. Cancer Society guideline for human papillomavirus (HPV) vaccine use to prevent cervical cancer and Its precursors. CA Cancer J Clin. 2008;57(1):7‐28. [DOI] [PubMed] [Google Scholar]
- 12. Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER. Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2007;56(RR‐2):1‐24. [PubMed] [Google Scholar]
- 13. Agenor M, Peitzmeier S, Gordon AR, Haneuse S, Potter JE, Austin SB. Sexual orientation identity disparities in awareness and initiation of the human papillomavirus vaccine among U.S. women and girls: a national survey. Ann Intern Med. 2015;163(2):99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Agenor M, Peitzmeier SM, Gordon AR, et al. Sexual orientation identity disparities in human papillomavirus vaccination initiation and completion among young adult US women and men. Cancer Causes Control. 2016;27(10):1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kaiser Family Foundation . Preventive services covered by private health plans under the Affordable Care Act [Internet]. San Francisco, CA: Kaiser Family Foundation; 2015. https://www.kff.org/health-reform/fact-sheet/preventive-services-covered-by-private-health-plans/. Accessed December 1, 2018. [Google Scholar]
- 16. Rosenbaum S. The Patient Protection and Affordable Care Act: implications for public health policy and practice. Public Health Rep. 2011;126(1):130‐135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lipton BJ, Decker SL. ACA provisions associated with increase in percentage of young adult women initiating and completing the HPV vaccine. Health Aff. 2015;34(5):757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Badgett M, Durso L, Schneebaum A. New patterns of poverty in the lesbian, gay, and bisexual community [Internet]. Los Angeles, CA: The Williams Institute; 2013. https://escholarship.org/uc/item/8dq9d947. Accessed December 1, 2018. [Google Scholar]
- 19. Baker KE, Durso LE, Cray A. Moving the needle: the impact of the Affordable Care Act on LGBT communities [Internet]. Washington, DC: Center for American Progress; 2014. https://cdn.americanprogress.org/wp-content/uploads/2014/11/LGBTandACA-report.pdf. Accessed December 1, 2018. [Google Scholar]
- 20. Shadish W, Cook T, Campbell D. Experimental and Quasi‐Experimental Designs for Generalized Causal Inference. Boston, MA: Houghton Mifflin; 2002:xxi. [Google Scholar]
- 21. National Center for Health Statistics . 2006–2010 National Survey of Family Growth public use data and documentation [Internet]. Hyattsville, MD: CDC National Center for Health Statistics; 2011. https://www.cdc.gov/nchs/data/nsfg/NSFG_2006-2010_UserGuide_MainText.pdf. Accessed December 1, 2018. [Google Scholar]
- 22. National Center for Health Statistics . 2011–2013 National Survey of Family Growth public use data and documentation [Internet]. Hyattsville, MD: CDC National Center for Health Statistics; 2014. December. https://www.cdc.gov/nchs/data/nsfg/NSFG_2011-2013_UserGuide_MainText.pdf. Accessed December 1, 2018. [Google Scholar]
- 23. National Center for Health Statistics . 2013–2015 National Survey of Family Growth public use data and documentation [Internet]. Hyattsville, MD: CDC National Center for Health Statistics; 2016. October. https://www.cdc.gov/nchs/nsfg/nsfg_2013_2015_puf.htm. Accessed December 1, 2018. [Google Scholar]
- 24. Institute of Medicine Committee on Lesbian, Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities . The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 25. Durso L, Baker K, Cray A. Communities and the Affordable Care Act: findings from a national survey [Internet]. Washington, DC: Center for American Progress; 2013. https://www.americanprogress.org/issues/lgbt/reports/2013/10/10/76693/lgbt-communities-and-the-affordable-care-act/. Accessed December 1, 2018. [Google Scholar]
- 26. Lepkowski JM, Mosher WD, Davis KE, Groves RM, Van Hoewyk J. The 2006–2010 National Survey of Family Growth: sample design and analysis of a continuous survey. Vital Health Stat. 2010;150:1‐36. [PubMed] [Google Scholar]
- 27. Barros A, Hirakata VN. Alternatives for logistic regression in cross‐sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 29. Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model‐adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 2010;171(5):618. [DOI] [PubMed] [Google Scholar]
- 30. Kleinman LC, Norton EC. What's the risk? A simple approach for estimating adjusted risk measures from nonlinear models including logistic regression. Health Serv Res. 2009;44(1):288‐302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lumley T. Analysis of complex survey samples. J Stat Softw. 2004;9(1):1‐19. [Google Scholar]
- 32. R Core Team . A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2017. [Google Scholar]
- 33. Corriero R, Gay JL, Robb SW, Stowe EW. Human papillomavirus vaccination uptake before and after the Affordable Care Act: variation according to insurance status, race, and education (NHANES 2006–2014). J Pediatr Adolesc Gynecol. 2018;31(1):23‐27. [DOI] [PubMed] [Google Scholar]
- 34. McCauley HL, Silverman JG, Decker MR, et al. Sexual and reproductive health indicators and intimate partner violence victimization among female family planning clinic patients who have sex with women and men. J Womens Health. 2015;24(8):621‐628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Skopec L, Long SK. Lesbian, gay, and bisexual adults making gains in health insurance and access to care. Health Aff. 2015;34(10):1769‐1773. [DOI] [PubMed] [Google Scholar]
- 36. Abdus S, Mistry KB, Selden TM. Racial and ethnic disparities in services and the Patient Protection and Affordable Care Act. Am J Public Health. 2015;105(S5):S668‐S675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cooper GS, Kou TD, Dor A, Koroukian SM, Schluchter MD. Cancer preventive services, socioeconomic status, and the Affordable Care Act. Cancer. 2017;123(9):1585‐1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. U.S. Department of Health and Human Services . Immunization and Infectious Diseases [Internet]. Washington, DC: U.S. Department of Health and Human Services; 2018. https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives. Accessed December 1, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


