Abstract
Objective
One potential benefit of greater electronic health information exchange is a reduction in the effort required for patients to switch between providers. We therefore assessed whether hospital participation in health information organizations (HIOs) led to increased patient sharing.
Data Sources
Secondary data from 2010 to 2016.
Study Design
Using hospital‐pair and year fixed effects regression models, we assessed change in patient sharing volume following HIO participation by hospitals and compared the effect by the level of market competition and by hospital size.
Data Extraction Methods
We used national data on hospital participation in HIOs from the American Hospital Association Information Technology Supplement and data on the volume of Medicare patients shared between pairs of hospitals from 2010 to 2016.
Principal Findings
The volume of patients shared between hospitals increased by 2.6 percent when both hospitals participated in a health information organization (P = .008, 95% CI: 0.7%‐4.5%). This increase was greater in competitive markets (3.1 percent increase, P = .03 95% CI: 0.3%‐5.9%) and between large hospitals (4.3 percent increase, P = .007 95% CI: 1.2%‐7.3%). Participation by only one hospital in a pair had no effect on patient sharing.
Conclusions
Our results suggest that an important policy goal motivating the investment in health information exchange has been at least partially achieved. However, our results also support hospital concerns about the competitive implications of engaging in health information exchange. HIO participation appears to facilitate patient movement between hospitals, likely by lowering switching costs and resulting in greater competition.
Keywords: competition, health information exchange, health information technology, hospitals, interoperability
What This Study Adds.
Hospital engagement in electronic health information exchange (HIE) has increased over the last decade but lags behind other types of health information technology.
One proposed reason for slow growth in HIE is provider concerns that sharing information with other providers could lead their patients to seek care elsewhere. However, from a patient perspective greater HIE would facilitate improved patient choice of providers.
When we examined whether HIE results in greater patient sharing, we found greater patient sharing between hospitals after joint HIE participation, suggesting greater patient choice.
The effect is especially pronounced among hospitals in completive markets and hospitals that are both large, underscoring provider concerns about competitive implications and the benefits of HIE for patient choice.
1. INTRODUCTION
Over the past decade, a wide array of public and private sector efforts have sought to increase the level of electronic health information exchange (HIE) between health care providers.1, 2 One key approach is the development of health information organizations (HIOs), independent or state‐convened organizations intended to foster HIE between potentially competing health care providers.3, 4 A common challenge cited by HIOs is provider concerns about the competitive implications of joining and enabling other provider organizations to access their patient data.5, 6 Prior work reveals that provider organization decisions to participate in HIOs are driven in part by the business case for HIE, including how it might affect their market share.7, 8 However, little empirical evidence demonstrates whether and how HIE impacts patient movement between providers.
Health information organization participation has the potential to increase the flow of patients between unaffiliated hospitals. HIE lowers switching costs for patients—that is, without functional HIE, patients who have been previously treated at specific hospitals and health systems face a cost to switching to other unaffiliated providers outside of the system and on a different EHR. Seeking treatment at an outside, unaffiliated hospital often requires work by patients to ensure the necessary medical information follows them—the time, effort, and financials costs associated with moving medical information to a potential new site of care may reduce the rate at which patients switch providers. Patients are often asked to bring paper records, CDs with images, and other pieces of information when making a new appointment and would therefore become aware of HIO connectivity when it allows for retrieval of that information without patient effort.9 Economic theory indicates that the presence of switching costs is beneficial for providers at the cost of patients, imposing monopoly‐like conditions.10 The introduction of HIE could reduce these costs by making it easier to transfer medical information between organizations, allowing patients more free choice of provider and reducing friction in the health care market. While this argument assumes that increased patient sharing from hospital HIO participation is driven by patient‐mediated mechanisms, it may be that lower switching costs drive providers to more routinely refer patients to outside hospitals when that transition is most appropriate. For instance, tertiary care hospitals may be more willing to refer their patients to community hospitals for routine follow‐up care when HIO connectivity facilitates information transfer,11 also increasing the volume of shared patients.
It is possible, however, that HIO participation could fail to drive increased patient sharing. Patients are unlikely to directly know that hospitals are connected through an HIO and hospitals may choose not make it clear to patients that HIOs can ease the transfer of information, limiting their agency to switch sites of care. Hospitals may also engage with HIOs in ways that impede seamless sharing of information (eg, by not integrating into frontline provider workflow) or fail to refer patients even in the face of lower switching costs because of the revenue losses they would incur. Finally, lower switching costs would only be incurred when multiple hospitals participate in an HIO; by definition, if only one hospital participates, switching costs remain high and would fail to increase patient sharing. This scenario may even reduce interhospital patient sharing if the HIO facilitates exchange between the participating hospital and associated ambulatory providers without facilitating exchange between hospitals.8, 12
Even if HIO participation does increase patient sharing between unaffiliated hospitals, the impact of this change on any given hospital is ambiguous. Increased mobility of patient information via HIO participation may lead to a loss of customers for some hospitals because patients are now more easily able to seek care elsewhere, but these patients still must receive care from somewhere, potentially resulting in a gain to other hospitals. Given this ambiguity and lack of empirical data on these questions, we sought to assess the impact of HIO participation on patient sharing between unaffiliated hospitals by examining changes in the volume of shared patients between hospitals following participation in a HIO from 2010 to 2016, a period of rapid HIO growth. To do so, we combined data on the volume of Medicare fee‐for‐service patients treated at multiple hospitals over this time period with national survey data on hospital HIO participation to identify how the volume of shared patients between pairs of hospitals changed once both participated in an HIO. We first examined the extent to which the HIO status of pairs of hospitals that shared patients changed over this time period and the proportion of patients that were shared between hospitals that both participated in an HIO. We then specifically measured whether joining an HIO changed the total volume of patients shared with other hospitals that participated in the HIO (likely through lower switching costs) and compared this to changes in patient sharing volume with other hospitals that did not participate in an HIO. To examine whether there was a differential impact across hospitals, we stratified our analysis by the level of hospital competition in the market and size of hospitals.
2. METHODS
2.1. Data
We created a panel of hospital pairs that shared patients from DocGraph's 180‐day “Root NPI Data” files from 2010 to 2014 and 2014 to 2016 HOP teaming data.13 Both files are derived from national Medicare fee‐for‐service claims; DocGraphs transitioned to a new approach beginning in 2014 and renamed the dataset. In the former files, sharing between hospitals occurs when they “participate in the delivery of health services to the same patient within 180 days … after another organization or provider participated in providing health services to the same patient.”13 In the HOP files, shared patients are defined by counting the number of unique transactions between providers over the course of one year (https://careset.com/docgraph-hop-teaming/). To ensure that our results are not driven by differences in the Root NPI and HOP files, we examined the correlation between values derived from each file in the one year (2014) when data are available using both methodologies and found a Pearson correlation of 0.93 and a Spearman rank correlation of 0.89. We report the over‐time correlation matrix in supporting information; correlations were >0.88 across all years, and the shift in methodology is not apparent from the reported correlations (Table S1).
We combined data on the number of shared patients between hospitals with the 2009‐2017 American Hospital Association's Information Technology Supplement, a detailed national survey of hospitals about their use of information technology, to identify pairs of hospitals that participated in HIOs in each year. We selected a longer period for survey data to more reliably measure HIO participation as described below. We combined these data with the AHA Annual Survey to capture hospital characteristics including membership in the same multihospital system (to limit our analyses to sharing that occurs across unaffiliated hospitals), hospital size, market competition, and other control variables.
2.2. Population
The population under study is all acute care, nonfederal hospitals in the United States. We combined this sample with data on the annual number of Medicare beneficiaries shared between hospitals, resulting in a hospital‐pair‐based dataset. Due to Medicare's cell‐size rule for public data, to be included in the HOP dataset, hospital pairs had to treat at least 11 shared patients over the course of the year. We further limited our sample to hospital pairs that were never in the same multihospital system to focus on the effect of HIO participation on patient sharing between unaffiliated hospitals (n = 2139 hospitals and 26 609 pairs).
2.3. Volume of shared patients
The Root NPI and HOP data files capture all types of Medicare fee‐for‐service claims. Each observation in the data includes the national provider identifier of the two treating providers and the number of unique patients that both treated over the course of the year. Hospital NPIs appear in the claim for patients in which the hospital is listed as the organizational NPI. These data therefore reflect treatment for inpatient and emergent care at the hospital as well as hospital‐based outpatient clinics. These data are directed, such that there are two observations for each pair of hospitals, one representing the volume of patients first seen at hospital A and then seen at hospital B and the other representing the volume first seen at hospital B and then seen at hospital A. However, we chose not to examine the data by directionality because the volume of shared patients flowing from hospital A to hospital B and from hospital B to hospital A is highly correlated (Pearson's correlation = 0.95).
Because the volume of shared patients is highly skewed and contains a few outliers, we used the logarithm of the volume of patients shared between hospitals and excluded pairs of hospitals above the ninety‐ninth percentile, which could unduly influence statistical analyses.
2.4. HIO participation
The AHA IT Supplement includes a question on HIO participation that asks, “Please indicate your level of participation in a state, regional, and/or local health information exchange (HIE) or health information organization (HIO).” Hospitals were coded as participating in an HIO if they selected the response, “HIE/HIO is operational in my area and we are participating and actively exchanging data in at least one HIE/RHIO” in a given year. Hospitals were also coded as participating if data were missing in a given year but the hospital indicated participating in an HIO in both the preceding year and the following year. Hospitals were coded as not participating in an HIO if they indicated that they were not participating in an HIO, or that no HIO was available. Hospitals that did not respond in a given year were coded as not participating in an HIO if they indicated not participating in an HIO in either the prior or following year and did not indicate participating in an HIO in either year.
For each pair of hospitals, we created two indicator variables, one of which indicated whether only one (but not both) hospital participated in an HIO, and the other indicating if both hospitals participated in an HIO.
2.5. Covariates and stratifying variables
To account for the potential that contemporary changes in other hospital characteristics could bias our results, we included characteristics of each hospital in the pair in all models. These characteristics included whether the hospital was a general acute care facility or specialty facility, whether the hospital was a member of a multihospital system or network, teaching status (none, minor, major), size (small < 100 beds; medium (100‐399 beds) or large > 400 beds), ownership type (government, nonprofit, for‐profit), market share, and market concentration. To facilitate examination of the effect of HIO participation in markets with different levels of competition, we created a binary measure of competition by splitting the measure of market concentration at the median (those with hospital bed‐based Herfindahl‐Hirschman indices above/below 0.146).
2.6. Analysis
We first described growth in hospital‐level HIO participation from 2010 to 2016. We then describe growth in hospital‐pair HIO participation by dividing pairs into three groups: pairs in which neither hospital, only one hospital, or both hospitals participated. We report the proportion of all shared patients that were shared by pairs of hospitals in each group in each year.
To examine whether the volume of shared patients between hospitals changed following hospital HIO participation, we created a hospital‐pair fixed effect model estimating the total log‐volume of Medicare patients shared between each pair of hospitals based on the HIO participation status of the two hospitals. We included year fixed effects and characteristics of each hospital as covariates and used multiway clustering to cluster the standard errors by both hospitals in each pair.
We would find evidence supporting our primary hypothesis that joint HIO participation was associated with increased shared patients if the coefficient on the indicator for both hospital participating was positive. No association between the indicator that only one hospital participates in the HIO and patient sharing volume would provide further support for our proposed causal mechanism—that HIO connectivity through both hospitals participating is driving switching—while a negative, statistically significant coefficient would indicate that patient 'stickiness' increased when one hospital joined an HIO but the other did not.
Next, we added an interaction between HIO participation and a binary indicator of high or low market competition to examine relative change in patient sharing following HIO participation in more and less competitive markets. Finally, to identify differences in patient sharing by hospital market position, we included a three‐way interaction term between HIO participation status, and the size of both hospitals in each pair (eg, small‐small, small‐large).
We conducted four additional tests to further validate the observed trends. First, we conducted a falsification test to examine whether our findings could be driven by ongoing differences in the rate of increase in patient sharing among hospitals that both joined an HIO and those that did not participate in an HIO that could have occurred prior to the HIO participation decision due to a secular trend or another reason unrelated to HIO participation. Second, we recreated our primary model using hospitals that were not in the data in all years. We first recreated the panel including all hospitals with data in at least five of the seven years from 2010 to 2016 and then recreated the panel including all hospitals with any data in that time period. Third, we divided our sample to hospital pairs that were less than 100 miles from one another and hospitals that were over 100 miles from one another. Because most HIOs are regional, we would only expect to see an association between HIO participation and hospitals in the same region. A null result in the “over 100 miles” model would provide evidence that this was not simply due to hospitals participating in an HIO exhibiting homophily regardless of connectivity.
Finally, we limited our sample to less volatile markets by characterizing hospital referral regions by three characteristics: (a) the rate of change in nonfederal acute care hospitals within each HRR from 2010 to 2016, defined as the difference between the maximum and minimum number of such hospitals in the HRR and divided by the average number in the HRR, (b) the proportion of hospitals in the HRR that participated in an ACO by 2016, and (c) change in hospital system affiliation from 2010 to 2016, measured as changes in each hospital in each HRR's system affiliation, divided by the average number of hospitals in the HRR. We then defined relatively stable markets as those below the 75th percentile on all three measures. This divided the sample into approximately two halves. We then examined whether the relationship between HIO participation and volume of shared patients remained in more stable markets.
3. RESULTS
Our balanced panel included 26 609 hospital pairs each year, representing 2139 unique hospitals. Characteristics of the balanced panel relative to all acute care, nonfederal hospitals in the AHA Annual Survey (n = 4599) are reported in Table 1. Relative to all hospitals, hospitals in the balanced panel are more likely to be large (12.4 percent compared to 9.8 percent of all hospitals), more likely to be major teaching hospitals (7.2 percent compared to 5.2 percent) and less likely to be members of a system (58.0 percent compared to 63.6 percent). Included and excluded hospitals were similar across other measures, such as network membership, market share, and market concentration.
Table 1.
Hospital sample characteristics (2016)
| In balanced panel (n = 2139); % | Not in panel (n = 2460); % | All hospitals (n = 4599); % | P‐value | |
|---|---|---|---|---|
| HIO participation | 48.9 | 64.4a | 55.6 | P < .001 |
| Size | ||||
| Small | 49.7 | 54.3 | 52.1 | |
| Medium | 37.9 | 38.2 | 38.1 | P < .001 |
| Large | 12.4 | 7.5 | 9.8 | |
| Ownership | ||||
| Government | 25.3 | 17.6 | 21.4 | |
| Nonprofit | 60.4 | 59.7 | 60.0 | P < .001 |
| For‐profit | 14.4 | 22.7 | 18.9 | |
| Organizational status | ||||
| System member | 58.0 | 68.4 | 63.6 | P < .001 |
| Network member | 37.8 | 34.8 | 36.2 | P = .033 |
| Teaching Status | ||||
| Non‐teaching hospital | 68.3 | 72.0 | 70.3 | P < .001 |
| Minor teaching hospital | 24.5 | 24.5 | 22.9 | P = .98 |
| Major teaching hospital | 7.2 | 3.5 | 5.2 | P < .001 |
| Market | ||||
| Hospital system market concentration | 0.18 | 0.18 | 0.18 | 0.887 |
| Hospital system market share | 13.1 | 14.7 | 13.9 | P = .001 |
| General acute care hospital | 97.6 | 92.0 | 96.0 | P < .001 |
Estimate based on all respondents to the AHA IT Supplement Survey in 2016, n = 1621.
In our sample, hospital participation in HIOs increased markedly over the course of the study period (Figure 1), which translated to a greater proportion of patients that were shared between unaffiliated hospitals that both participated in an HIO. Specifically, in 2010, 5 percent of patients that moved from one hospital to another were shared by hospitals that both participated in an HIO. By 2016, the percent of patients that transitioned between hospitals that both participated in an HIO increased to 41 percent. Meanwhile, the percent of patients shared by hospitals where only one hospital participated in an HIO increased from 26 percent to a high of 48 percent in 2013 and then declined to 41 percent in 2016, and the percent moving between hospitals where neither hospital participated decreased from 69 percent in 2010 to 18 percent 2016. The proportion of hospital pairs connected by HIO participation without regard to patient volume was similar and is reported in Figure S1. Trends were also similar when we compared our sample to the unbalanced sample (Figure S2).
Figure 1.
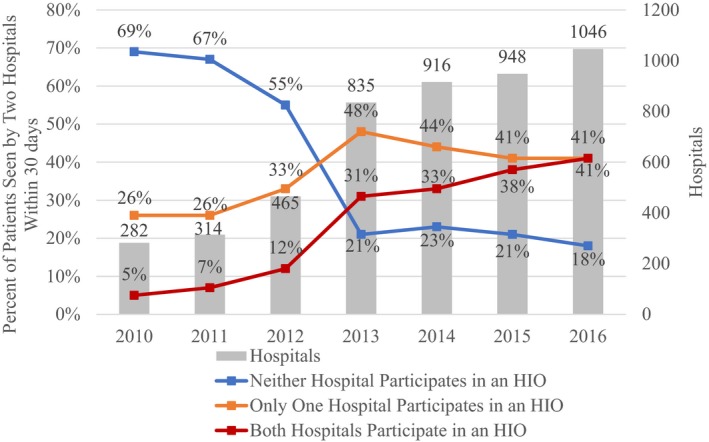
Trend in volume of shared patients treated by two hospitals within 30 days, by hospital‐pair HIO participation status. Error bars represent 95% confidence intervals. Data from 2009‐2016 American Hospital Association Information Technology Supplement and 2010‐2013 medicare physician shared patient patterns files and 2014‐2016 HOP files [Color figure can be viewed at http://wileyonlinelibrary.com]
We observed no change in the total volume of shared patients between hospitals when one hospital participated in an HIO and the other did not participate. In contrast, we observed a statistically significant increase in patient sharing when both hospitals participated in an HIO of approximately 2.6 percent (representing an increase from 78 to 80 shared patients per pair, P = .008, Figure 2; full regression results available as Table S2, column 1). In more competitive markets, we found a consistent, statistically significant increase in patient sharing when both hospitals participated in a HIO of 3.1 percent (P = .030). The association between both hospitals participating and patient sharing in markets below the median in competition was 2.0 percent (P = .029). Finally, when we examined the effect of HIO participation on patient sharing for hospitals of different sizes (Figure 3), we did not observe statistically significant changes when one hospital in the pair participated in an HIO. However, we did observe statistically significant increases in shared patients when pairs comprised of two small or two large hospitals both participated in an HIO (increase of 3.7 percent, P = .016 for small hospitals and 4.3 percent, P = .007 for large hospitals).
Figure 2.
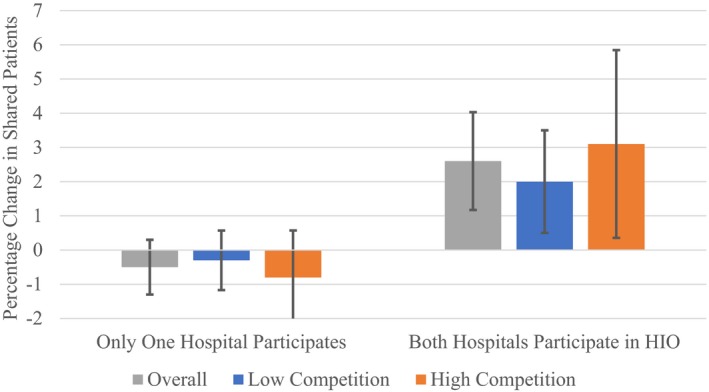
Association between hospitals joining a HIO and change in interhospital patient sharing. Error bars represent 95% confidence intervals. Data from 2009‐2016 American Hospital Association Information Technology Supplement and 2010‐2013 medicare physician shared patient patterns files and 2014‐2016 HOP files [Color figure can be viewed at http://wileyonlinelibrary.com]
Figure 3.
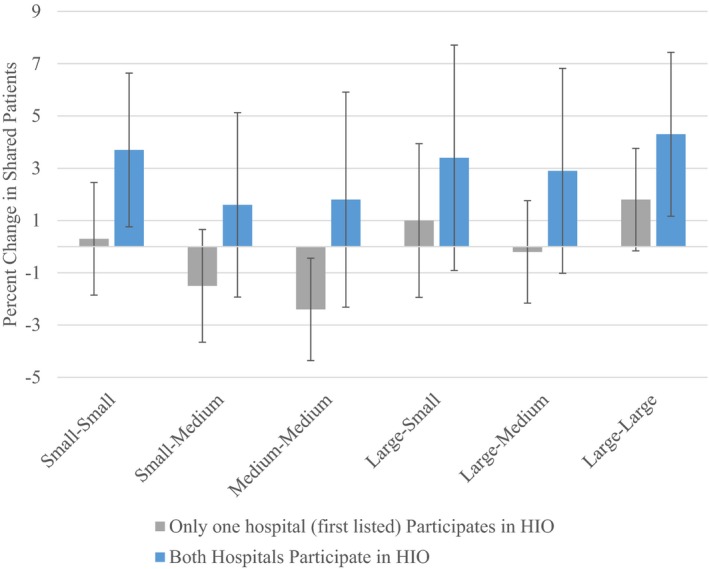
Association between hospital size, hospitals joining a HIO, and change in interhospital patient flow. Error bars represent 95% confidence intervals. Data from 2009‐2016 American Hospital Association Information Technology supplement and 2010‐2013 medicare physician shared patient patterns files and 2014‐2016 HOP files [Color figure can be viewed at http://wileyonlinelibrary.com]
In our falsification test, in which HIO status from the following year was used, we did not observe an association between only one or both hospitals participating in an HIO and the volume of shared patients (P = .25 and P = .13, respectively; Table S2, column 2). Our findings were robust to including hospital pairs that were missing one year of data (n = 337 559); however, when we recreated the model and included all available observations (n = 648 085), the association in our primary model was no longer observed (P = .322) and the point estimate of the association was small, likely due to noise introduced by missing data in some years (Table S2, columns 3 and 4). When we limited our sample to hospital pairs within 100 miles of one another (which made up 75 percent of pairs), we observed an association between both hospitals participating in an HIO and sharing of patients that was slightly stronger than our primary model of 3.2 percent (P = .001). There was no association between HIO participation and patient sharing among hospitals that were over 100 miles away from one another. When we limited our sample to hospitals in more stable markets (n = 92 820, or 50 percent of the full sample), we observed a continued association similar in magnitude to our main result (2.3 percent, P = .028).
4. DISCUSSION
In this study, we used data on the volume of Medicare patienst shared between hospitals to generate the first national quantitative evidence on the impact of HIE on sharing of patients between hospitals. Over the years of the study, the proportion of hospital pairs that both participated in an HIO increased notably as did the sharing of patients between hospital pairs that both participated in an HIO. When both hospitals in a pair participated in an HIO, the volume of patients shared between them increased, and this relationship was of greater magnitude in competitive markets where patients are more likely to have multiple choices of hospitals. By reducing the “cost” of switching providers, HIOs may reduce providers' economic advantage while facilitating greater choice among patients.
By 2016, 41 percent of patients shared between hospitals were shared by hospitals that both participated in an HIO, representing a notable increase from 5 percent of shared patients in 2010. The overall moderate level of connectivity indicates that, by 2016, work to foster hospital participation in HIOs remained incomplete. The relatively large volume of shared patients in which only one hospital participated in an HIO in 2016 (also 41 percent) further indicates that continued growth in HIO participation is needed. Given the frequency with which one half of a pair of hospitals participates in an HIO, increased adoption is likely to shift hospital pairs from only one using an HIO (which, for that pair, is likely the same as neither using it) to both hospitals participating in an HIO. Since 2013, when the volume of patients shared between pairs in which only one hospital used HIO was at a maximum, increased HIO participation has been more likely to lead to both hospitals participating in an HIO. Continued policy incentives to increase connectivity, such as those included as part of the Promoting Interoperability Program and Information Blocking rule, are likely necessary to encourage greater levels of exchange. Even with connectivity, impactful use of exchanged information will likely depend on financial incentives linked to quality and efficiency that make such use beneficial to hospitals and providers who, in turn, will demand highly usable exchange technologies.
Our central finding—that HIO participation increases the volume of patients shared between hospitals—points toward a societal benefit of information exchange that complements documented improvements in the efficiency and quality of health care.14, 15, 16, 17 While competition is often conceptualized and measured as the number of providers in a market area,18, 19 the ability for patients to switch providers can be limited by switching costs that impose barriers to changing providers. These switching costs are not directly financial and instead take the form of time, effort, and potential distress caused by barriers to accessing and transferring health information across providers. In the presence of high switching costs, the real competition between hospitals may be lower than it appears because patients, as consumers, are only motivated to switch when the benefits of doing so exceed the costs.20 By lowering these costs, HIOs have the potential to make the provider market more competitive.
For patients, employers, payers, and others concerned about free choice of provider and the price and quality of health care, this is likely a welcome development. Recent policy changes focused on eliminating information blocking and increasing information sharing by providers and health insurers have been explicitly motivated by the goal to “empower patients,” and the higher level of sharing we observe indicates that HIOs may be fulfilling at least part of that policy goal.21 However, the small magnitude of our findings makes the real benefit of decreased switching costs through information exchange somewhat uncertain—it may be that marginal benefits are small relative to the overall costs of care. On the other hand, greater levels of connectivity over time and increasing patient knowledge of the ease of transferring information (as it becomes more widespread and taken for granted) may lead to much larger effects than those observed in these data.
For hospitals and providers, this may introduce some complexity to patient and population management, which may be only partially mitigated by information exchange. For instance, Accountable Care Organization (ACOs) might find it more challenging to ensure quality and efficiency of care if patients are more apt to seek care outside the ACO.22, 23 Also relevant to hospitals and providers, our results validate their concerns about the competitive implications of electronic health information sharing. Our finding that HIO participation was associated with increased patient sharing helps to explain prior findings that hospitals do not preferentially develop HIE with hospitals with which they share many patients (with whom they may compete),24 that larger hospital system sizes are associated with decreased likelihood of HIE,7 and that hospitals prioritize HIE within their system at the expense of HIE with unaffiliated hospitals.25 That is, hospitals and hospital systems may be less inclined to engage in HIE in order to retain market power through preserving high switching costs. Furthermore, stratified analyses indicated that the overall increase in shared patients between hospitals following HIO participation is driven by hospitals of the same size and in more competitive markets. This reinforces the concern that patients may switch to similar hospitals that are often viewed as the predominant competitor (ie, those that occupy a similar market position) if they are in a competitive market with choice of hospital.
Our results suggest that current policy efforts, particularly those under the Trusted Exchange Framework and Cooperative Agreement (TEFCA) and Information Blocking regulations, which aim to ensure that health care providers exchange information with a broad group of other providers, are likely to result in greater ability of patients to move across providers.26 TEFCA in particular envisions a single “on‐ramp” in which a provider that joins a given HIO can engage in HIE with providers that have chosen to connect to other HIOs. While our results cannot specifically address the extent to which hospitals refrain from HIO participation when their primary competitor(s) have joined, or choose to join an HIO that differs from the one that their primary competitor(s) have joined, TEFCA will help curb such strategic pursuit of HIE. A key outcome may be that the magnitude of change in shared patient volume from joint HIO participation, which was modest in our study, increases, reflecting even greater ability of patients to seek care from multiple providers.
4.1. Limitations
Our study is subject to several limitations. One important limitation of this analysis is that we are not able to directly measure whether two hospitals that share patients and both report HIO participation are participating in the same HIO. There are some markets in which multiple HIOs are operational, but this is not common. Further, even if two hospitals participate in different HIOs, our estimate of the effect of joint HIO participation on shared patients would represent an underestimate, since the effect of joint participation is biased downwards by the effect of participation in different HIOs. A second limitation is that we only examined HIO participation when there are other available forms of HIE that could allow two hospitals to share patient information.27 However, there is not a data source that allows us to measure hospital engagement in these other forms of HIE over our study period. This limitation is likely to bias the association between HIO and patient sharing to the null because comparator hospitals may engage in other forms of HIE. A third limitation is that we focus on the association between HIO participation and patient movement between unaffiliated hospitals: Because hospitals in the same system may share the same EHR or otherwise ease information transfer, our findings may not be generalizable to hospital pairs in the same system. A fourth limitation of our study is that our measure of shared patients reflects all patients treated by the two hospitals regardless of the length of their medical history at a given hospital. Any observed effect may be more pronounced for patients with long histories at a given hospital, for whom the cost of switching may be higher. In addition, our analysis is focused on hospitals only and may not apply to other care settings, or to non‐Medicare patients.
5. CONCLUSION
In this study, we provide quantitative evidence that HIOs facilitate patient sharing between hospitals, likely by making it easier to move health information from one hospital to another. For patients, this dynamic is clearly positive: It likely represents a facilitation of greater choice of hospital while reducing the economic advantage of providers. From a provider perspective, this same effect could be unwelcome if it reduces their economic advantage and increases competition. Combined with our observation that, as more hospitals participate in an HIO, each new participant is able to exchange informaton for a larger proportion of their shared patients, these findings provide additional motivation for public policy efforts that support HIOs to enhance patient choice and competition between hospitals.
Supporting information
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under award number R01AG062563.
Disclosures: None.
Everson J, Adler‐Milstein J. Sharing information electronically with other hospitals is associated with increased sharing of patients. Health Serv Res. 2020;55:128–135. 10.1111/1475-6773.13240
REFERENCES
- 1. Kuperman GJ. Health‐information exchange: why are we doing it, and what are we doing? J Am Med Inform Assoc. 2011;18(5):678‐682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Patel V, Henry J, Pylypchuk Y, Searcy T. Interoperability among U.S. Non‐federal Acute Care Hospitals in 2015; 2016. https://www.healthit.gov/sites/default/files/briefs/onc_data_brief_36_interoperability.pdf. Accessed August 21, 2019.
- 3. Adler‐Milstein J, Bates DW, Jha AK. US Regional health information organizations: progress and challenges. Health Aff. 2009;28(2):483‐492. [DOI] [PubMed] [Google Scholar]
- 4. Patel VN, Dhopeshwarkar RV, Edwards A, Barrón Y, Sparenborg J, Kaushal R. Consumer support for health information exchange and personal health records: a regional health information organization survey. J Med Syst. 2012;36(3):1043‐1052. [DOI] [PubMed] [Google Scholar]
- 5. Adler‐Milstein J, Pfeifer E. Information blocking: is it occurring and what policy strategies can address it? Milbank Q. 2017;95(1):117‐135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. The Office of the National Coordinator for Health Information Technology . 2015 Report to Congress on Health Information Blocking; 2015.
- 7. Miller AR, Tucker C. Health information exchange, system size and information silos. J Health Econ. 2014;33:28‐42. [DOI] [PubMed] [Google Scholar]
- 8. Grossman JM, Bodenheimer TS, McKenzie K. Hospital‐physician portals: the role of competition in driving clinical data exchange. Health Aff. 2006;25(6):1629‐1636. [DOI] [PubMed] [Google Scholar]
- 9. Parry C, Coleman EA, Smith JD, Frank J, Kramer AM. The care transitions intervention: a patient‐centered approach to ensuring effective transfers between sites of geriatric care. Home Health Care Serv Q. 2003;22(3):1‐17. [DOI] [PubMed] [Google Scholar]
- 10. Klemperer P. Markets with consumer switching costs. Q J Econ. 1987;102(2):375‐394. [Google Scholar]
- 11. Bates WD. Health information technology and care coordination: the next big opportunity for informatics? Yearb Med Inform. 2015;24(01):11‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Eftekhari S, Gopal R, Ramesh R. Impact of Health Information Exchange Adoption on Physician's Referral Behavior; 2016.
- 13. Center for Medicare and Medicaid Services . Physician Shared Patient Patterns Technical Requirements. https://www.nber.org/physician-shared-patient-patterns/docs/physician_shared_patient_patterns_technical_requirements.pdf. Accessed August 21, 2019.
- 14. Menachemi N, Rahurkar S, Harle CA, Vest JR. The benefits of health information exchange: an updated systematic review. J Am Med Inform Assoc. 2018;25(9):1259‐1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Adjerid I, Adler‐Milstein J, Angst C. Reducing Medicare spending through electronic health information exchange: the role of incentives and exchange maturity. Inform Syst Res. 2018;29(2):341‐361. [Google Scholar]
- 16. Lammers EJ, Adler‐Milstein J, Kocher KE. Does health information exchange reduce redundant imaging? Evidence from emergency departments. Med Care. 2014;52(3):227‐234. [DOI] [PubMed] [Google Scholar]
- 17. Frisse ME, Holmes RL. Estimated financial savings associated with health information exchange and ambulatory care referral. J Biomed Inform. 2007;40(6):S27‐S32. [DOI] [PubMed] [Google Scholar]
- 18. Austin DR, Baker LC. Less physician practice competition is associated with higher prices paid for common procedures. Health Aff. 2015;34(10):1753‐1760. [DOI] [PubMed] [Google Scholar]
- 19. Baker LC. Measuring competition in health care markets. Health Serv Res. 2001;36(1 Pt 2):223. [PMC free article] [PubMed] [Google Scholar]
- 20. Burnham TA, Frels JK, Mahajan V. Consumer switching costs: A typology, antecedents, and consequences. J Acad Mark Sci. 2003;31(2):109‐126. [Google Scholar]
- 21. U.S. Department of Health and Human Services. Proposes New Rules to Improve the Interoperability of Electronic Health Information. https://www.hhs.gov/about/news/2019/02/11/hhs-proposes-new-rules-improve-interoperability-electronic-health-information.html. Accessed August 12, 2019.
- 22. Everson J, Adler‐Milstein J, Ryan AM, Hollingsworth JM. Hospitals strengthened relationships with close partners after joining accountable care organizations. Med Care Res Rev. 2018. 10.1177/1077558718818336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Barnett ML, McWilliams JM. Changes in specialty care use and leakage in Medicare accountable care organizations. Am J Manag Care. 2018;24(5):e141‐e149. [PMC free article] [PubMed] [Google Scholar]
- 24. Everson J, Adler‐Milstein J. Gaps in health information exchange between hospitals that treat many shared patients. J Am Med Inform Assoc. 2018;25(9):1114‐1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Vest JR, Simon K. Hospitals' adoption of intra‐system information exchange is negatively associated with inter‐system information exchange. J Am Med Inform Assoc. 2018;25(9):1189‐1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Technology OotNCfHI . Draft Trusted Exchange Framework; 2018.
- 27. Everson J. The implications and impact of 3 approaches to health information exchange: community, enterprise, and vendor‐mediated health information exchange. Learn Health Syst. 2017;1(2):e10021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


